Академический Документы
Профессиональный Документы
Культура Документы
Thyroid Dysfunction in Pregnancy: Motha MBC, Palihawadana TS, Dias TD
Загружено:
Kristian Lihardo GirsangИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Thyroid Dysfunction in Pregnancy: Motha MBC, Palihawadana TS, Dias TD
Загружено:
Kristian Lihardo GirsangАвторское право:
Доступные форматы
www.slcog.
lk/sljog Leading Article
Thyroid dysfunction in pregnancy
Motha MBC1, Palihawadana TS1, Dias TD1
Introduction
Maternal thyroid state is an important of Sri Lanka a decade ago, found as normal for our pregnant women.
predictor of pregnancy outcome. Both the prevalence of thyroglobulin Symptoms of thyroid dysfunction
hyperthyroidism and hypothyroidism autoantibody (TgAb) to be markedly are generally vague and non specific,
have been shown to have an adverse raised at 14.3% in 11 year olds and and could easily be attributed to the
impact on pregnancy. There is a wide 69.7% among 16 year old girls7. physiological changes that occur in
range in the prevalence of thyroid Thyroid autoantibodies are known pregnancy. The clinical presentation of
dysfunction worldwide. In the to be associated with thyroid hyperthyroidism may not be obvious
USA which is considered an iodine dysfunction, mainly hypothyroidism. because symptoms of tachycardia,
replete country, 2%–3% of apparently These observations raise the sweating, dyspnoea, and nervousness
healthy, non pregnant women of possibility of a high prevalence of are seen in normal pregnancy.
childbearing age have an elevated thyroid dysfunction among pregnant Generalised body aches, arthralgia,
serum TSH with the majority in the women of Sri Lanka, which needs to constipation and excessive sleepiness
subclinical range12. In southern Iran, be confirmed by studies. which are features of hypothyroidism
the prevalence of hypothyroidism too could be easily attributed to the
among pregnant women was hormonal changes of pregnancy. A
shown to be 13.7%3. In a study Changes in thyroid high index of suspicion is therefore
carried in India, the prevalence of
homeostasis in pregnancy required for timely identification and
thyroid dysfunction was high with appropriate treatment. Palpitations
subclinical hypothyroidism found in Transfer of thyroxine transplacentally,
which are frequent and distressing,
6.47% and overt hypothyroidism found increased maternal renal clearance of
excessive sweating, increased
in 4.58% of pregnant women4. iodine and changes in thyroid binding
bowel frequency, fine tremor of the
Hyperthyroidism is less commonly globulin disturb thyroid homeostasis
outstretched hands, tachycardia and
encountered in pregnancy with a in pregnancy. Thyroid hormone
exaggerated deep tendon reflexes
prevalence of 0.2- 0.6%5. production which is iodine dependant
suggest thyrotoxicosis. Distressing
gradually declines if the increase on
There is lack of data on the magnitude arthralgia and myalgia, especially
iodine demand placed by the pregnant
and different forms of thyroid proximal myopathy, should prompt
state, which averages 250 micrograms
dysfunction among pregnant women examination of the pulse rate for
per day, is not met.
of Sri Lanka. Few studies have looked bradycardia and slow relaxing ankle
at the prevalence of iodine deficiency The reference range for serum thyroid jerks which are highly suggestive of
and autoimmune thyroid disease stimulating hormone (TSH) and hypothyroidism.
which are the two leading causes free thyroxine (FT4 ) are different
of hypothyroidism in pregnancy. during pregnancy, reflecting the
In a cross sectional, nationally physiological changes described Screening for thyroid
representative sample of pregnant above. The reference range for TSH dysfunction in pregnancy
women in Sri Lanka, median urinary is lower than outside pregnancy, At present, an aggressive case finding
iodine level was 113.7 μg/l, which was while FT4 levels are highest in the approach rather than universal
far below the WHO recommendation first trimester due to the stimulatory screening is advocated for detection
of a level between 150 and 249 μg/l, effect of serum beta hCG on the of thyroid dysfunction in pregnancy
indicating inadequate iodine status TSH receptors. Until reference inspite of the significant impact
of pregnant women in Sri Lanka6. A ranges are available for Sri Lankan thyroid dysfunction exerts on
study looking at the prevalence of women, the following reference range pregnancy. This is due to the Absence
thyroid autoantibodies in schoolgirls shown in box 1 could be adopted of consistent results on benefit of
levothyroxine replacement in women
1
Senior Lecturer, Dept of Obstetrics & Box 1- Referance range for thyroid function tests in pregnancy
Gynaecology, Faculty of Medicine, University
of Kelaniya, Sri Lanka. Trimester Serum TSH (µIU/mL) FT4 (pg/ml)
First 0.1-2.5 0.83-1.27
Correspondence: Dr. Motha MBC
Second 0.2-3.0 0.71-1.05
No 6, Thalagolla road, Ragama. Sri Lanka
Third 0.3-3.0 0.72-1.06
E-mail: cmotha6@gmail.com
Competing interests: None
March 2015 Sri Lanka Journal of Obstetrics and Gynaecology 1
Leading Article www.slcog.lk/sljog
with subclinical hypothyroidism, birth, gestational hypertension, cheap and devoid of significant
which forms the majority of thyroid low birth weight and fetal loss are side effects, most authorities incline
dysfunction. However, a target known complications of maternal towards prescribing levothyroxine
case finding approach appears hypothyroidismii. 8 9 The fetus requires for SCH even in the absence of
ineffective as the prevalence of adequate thyroxine for central nervous thyroid autoantibodies. Isolated
SCH and overt hypothyroidism system maturation in early gestation hypothyroxinaemia (normal TSH with
have found to be equal in targeted and is totally dependant on maternal low FT4) does not need to be treated.
thyroid tested and untested women, thyroxine due to the inability of its The aim of treatment should be
while in another study testing only thyroid gland to synthesize thyroxine maintenance of TSH within the
women in the high risk group was until early second trimester10. trimester specific reference range.
shown to miss a third of those with Maternal hypothyroidism is therefore Serum TSH is adequate for monitoring
overt/subclinical hypothyroidism associated with the much feared maternal thyroid status and should
. The cost effectiveness of a universal complication of neurodevelopmental be assessed every 4 weeks during
screening program has also delay in the offspring11. pregnancy.
been demonstrated based on the Subclinical hypothyroidism (SCH)
assumption that treatment of SCH In women with pre existing
defined as elevated TSH (based on hypothyroidism contemplating
has an effect on IQ of the offspring, trimester specific reference range)
though studies are yet to confirm this pregnancy, periconceptional care
with normal free T4 level too appears should ensure that TSH is maintained
. Until the results of such studies shed to have an adverse impact on the
new light, a case finding approach is within the reference range for the
pregnancy with increased incidence first trimester (ie TSH < 2.5 µiu/ml).
currently recommended. of miscarriage, gestational diabetes It also important to increase chances
All pregnant women should be mellitus, gestational hypertension of conception as infertility is known
assessed with serum TSH at the and pre eclampsia. 12. The association to be associated with SCH. In case of
booking visit if any one of the features between maternal SCH and impaired unplanned pregnancy, the dose of
listed in Box 2 is found to be present. If neuropsychological development in thyroxine should be increased by 25-
TSH is abnormal (high or low) free T4 the offspring is less consistent than for 30% of the preconception dosage as
should be assessed. overt hypothyroidism. early as possible while awaiting the
Levothyroxine is used to treat overt result of TSH. In all other women
hypothyroidism. The benefits of seen at any other time in pregnancy,
Thyroid dysfunction- levothyroxine therapy on subclinical a TSH should be performed as soon
hypothyroidism hypothyroidism is less convincing as possible and maintained within
Worldwide, iodine deficiency is the with some studies failing to show the trimester specific referance range.
commonest cause of hypothyroidism, a significant benefit in the absence In a woman newly diagnosed to have
while chronic autoimmune of thyroid autoantibodies 8 13. A overt hypothyroidism, the usual
thyroiditis remains the leading prospective randomized controlled starting dose of thyroxine is 2µg/
cause in the developed world. Overt trial by the National Institute of Child Kg/d (maximum of 2.5 µg /Kg/d).
hypothyroidism is defined as an Health and Human Development – TSH performed at 4 weeks should
elevated serum TSH and low free T4 USA and similar studies which are help in titrating the dose thereafter.
(FT4) or TSH> 10µIU/ml irrespective underway, will hopefully enlighten The woman should be advised on
of the FT4 level. Miscarriage, preterm us this area in the near future. Given general measures that enhance the
the fact that levothyroxine is relatively
Box 2- Clinical features that require thyroid assessment in pregnancy
■ A family history of autoimmune thyroid disease, hypothyroidism or hyperthyroidism
■ Presence of a goitre
■ Presence of thyroid antibodies, primarily thyroid peroxidase antibodies (TPOAb)
■ Symptoms or clinical signs suggestive of hypothyroidism or hyperthyroidism
■ Women with type 1 diabetes mellitus, or other autoimmune disorders
■ Women with a history of infertility
■ Women with a prior history of miscarriage or preterm delivery
■ Women with prior therapeutic head or neck irradiation or prior thyroid surgery
■ Women currently receiving Levothyroxine replacement
■ Women living in a region presumed to be iodine deficient
2 Sri Lanka Journal of Obstetrics and Gynaecology March 2015
www.slcog.lk/sljog Leading Article
absorption of thyroxine. Taking The usual starting dose for
Fetal wellbeing could be affected in
thyroxine on an empty stomach upon Propylthiouracil is 100-300mg daily
the presence of elevated TRAb and in
waking in the morning with a lapse in divided doses and for Carbimazole
poorly controlled hyperthyroidism16.
of at least half an hour until a drink it is 10-15mg daily in divided doses.
or meal and avoiding taking iron and Antithyroid drugs have no place in Ultrasonography appearance of fetal
calcium supplements concomitantly managing thyrotoxicosis associated tachycardia (>170 bpm, persistent
should be advised upon. with hyperemesis gravidarum, for over 10 minutes), fetal growth
though beta blockers could be used restriction, fetal goiter, accelerated
Thyroxine is safe during breast
if troublesome hypermetabolic bone maturation, signs of congestive
feeding. Women with pre existing
symptoms are present. heart failure, and fetal hydrops may
hypothyroidism could be maintained
suggest potential underlying fetal
on their pre pregnancy dose of The aim of treatment in thyrotoxicosis
hyperthyroidism17.
thyroxine with serum TSH reviewed is to maintain FT4 in the upper
at 6 weeks postpartum. Neonatal TSH normal range using the smallest dose American thyroid association
should be tested within the first week. of antithyroid drug. This reduces recommends to offer serial fetal
the risk of fetal hypothyroidism. wellbeing assessment in women who
Beta adrenergic blocking agents (Eg have uncontrolled hyperthyroidism
Thyroid dysfunction- Propranolol 20-40 mg 6 hourly ) may and/or women with high TRAb levels
hyperthyroidism be used for controlling troublesome (greater than three times the upper
‘Transient thyrotoxicosis of pregnancy’ hypermetabolic symptoms such as limit of normal). These women should
occur due to the stimulatory effect of palpitations and tremulousness, be managed under a maternal–fetal
serum β hCG on the TSH receptor and with the dose reduced as early as medicine specialist and monitoring
the commonest cause of thyrotoxicosis possible in view of risk of fetal should include ultrasound for heart
in pregnancy which is known to affect growth restriction, fetal bradycardia rate, growth, amniotic fluid volume,
1-3% of pregnancies. Graves disease and neonatal hypoglycaemia. In the and fetal goiter 18.
remains the commonest pathological vast majority of cases, beta blockers
cause of maternal hyperthyroidism could be discontinued in 1-2 weeks.
in pregnancy14. Complications of Thyroidectomy is rarely indicated Postpartum thyroid
maternal hyperthyroidism include to control hyperthyroidism and if dysfunction
miscarriage, gestational hypertension, required, is usually performed in the Autoimmune thyroiditis is
preterm birth, fetal growth restriction, second trimester. Radioactive iodine characterised by thyroid inflammation
stillbirth, low birth weight, thyroid is contraindicated during pregnancy. caused by autoantibodies. Thyroid
storm, and maternal congestive heart A woman with pre-existing peroxidase antibodies (TPO Ab) and
failure. High levels of maternal thyroid hyperthyroidism, should be rendered thyroglobulin antibodies (TgAb) are
receptor stimulating antibodies euthyroid before attempting the two most important autoantibodies
(TRAb) which characterises Graves pregnancy with TSH maintained described. These antibodies when
disease, is associated with an increased within the reference range for the first present in high titres could cause
risk of fetal/neonatal thyrotoxicosis, trimester. If radioactive iodine has a destructive thyroiditis which
which although transient can cause been used to achieve euthyroidism, classically results in hyperthyroidism
significant morbidity15. conception should be delayed for a due to release of preformed hormones
Overt hyperthyroidism is minimum of 6 months. followed by hypothyroidism due to
characterised by depressed serum exhaustion of thyroid reserve and
Women with Graves disease may finally euthyroidism. In the western
TSH and high levels of free T4. Overt experience disease flares in the
hyperthyroidism can be treated world, 10-20% of pregnant euthyroid
first trimester, though a gradual women were found to have thyroid
though there is a lack of evidence of improvement is expected as
benefit in treatment of subclinical autoantibodies in first trimester.
pregnancy advances. Discontinuation There is a growing body of evidence
hyperthyroidism ( depressed TSH of all antithyroid therapy is feasible
levels with normal FT4) or isolated linking adverse pregnancy outcomes
in 20%–30% of patients in the third with autoimmune thyroiditis even in
hyperthyroxinaemia (normal levels trimester. The exceptions are women
of TSH with elevated FT4) in the absence of thyroid dysfunction.
with high levels of thyroid receptor Development of overt or subclinical
pregnancy. Antithyroid drugs are the stimulating antibodies (TRAb), in
mainstay of management of maternal hypothyroidism, miscarriage,
whom it is needed to be continued preterm delivery, placental abruption,
hyperthyroidism. Propylthoiuracil until delivery. Maternal serum TRAb
should be used in the first trimester postpartum depression and reduced
levels should be determined between IQ in the offspring are some of the
of pregnancy due to lesser risk of 24 to 28 weeks in women with active
teratogenicity while Carbimazole adverse associations described19. In the
hyperthyroidism, those with a history only prospective interventional trial
may be commenced from the second of thyroidectomy for treatment of
trimester onwards. This will reduce to date, levothyroxine replacement in
hyperthyroidism, those treated with TPOAb positive women has shown
the risk of liver toxicity associated with radioiodine and in women who have
prolonged use of Propylthiouracil. to significantly reduce the rate of
had an infant with hyperthyroidism.
March 2015 Sri Lanka Journal of Obstetrics and Gynaecology 3
Leading Article www.slcog.lk/sljog
preterm delivery20. thyroid dysfunction in the postpartum positive TPO Ab detected in the first
Downregulation of the maternal period, which is termed postpartum trimester22.
immune system is pertinent for fetal thyroid dysfunction (PPTD). The The classical course of PPTD is a
survival. The maternal immune incidence of PPTD ranges from 4%- thyrotoxic phase which occurs around
system which is suppressed during 9%21. It is characterised by elevated 1-4 months following delivery,
pregnancy, rebounds back to thyroid peroxidase (TPOAb) and/ followed by a hypothyroid state
normalacy in the postpartum period. or thyroglobulin antibodies (TgAb) around 4-8 months and finally a state
It has been shown that autoantibodies and is the result of an autoimmune of euthyroidism. A hyperthyroid
seen in women in the first trimester destructive process that lies relatively phase followed by return to
gradually wane due to the immune quiescent in the antenatal period. normalacy and a hypothyroid phase
tolerance of pregnancy and increase There is lymphocytic infiltration of the alone are also identified. Although
in the postpartum period, at times thyroid gland and hypoechogenicity clinical and biochemical abnormalities
overshooting the normal level. This of the gland on ultrasound scanning. are transient in the majority, 20-30%
autoimmune process could lead to PPTD has been shown to occur in of women will remain permanently
as much as 33-50% of women with
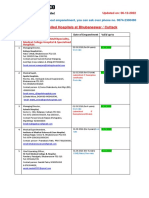
Figure 1 – Management of postpartum thyroid dysfunction
Figure 1. Management of postpartum thyroid dysfunction
Hypothyroidism
Hyperthyroidism
Asymptomatic
If symptomatic
Do not treat
Treat with propranolol
Monitor thyroid
No place for ATD
functions 6 weekly
Euthyroid
See if,
Symptomatic
TSH >10 µIU/mL
Breast feeding
Attempting pregnancy and
TSH >2.5-10 µIU/mL
If any of the
If none of the above present
above present
Do not treat
Start treatment
• Continue treatment until 6-12 months
Repeat TSH every 2 months until 1 year • Attempt weaning by halving the dose and
postpartum repeating TSH in 6-8 weeks
• Do not attempt weaning if patient is pregnant,
breast feeding, or attempting to conceive
Yearly TSH measurement in women who had PPTD and returned to the euthyroid state
4 Sri Lanka Journal of Obstetrics and Gynaecology March 2015
www.slcog.lk/sljog Leading Article
hypothyroid at one year postpartum outcome.Int J Endocrinol Metab. 2014 14. Patil-Sisodia K, Mestman JH 2010 Graves
while long term follow up studies Oct 1;12(4): hyperthyroidism and pregnancy: a clinical
reveal that nearly 50% of those 4. Sahu MT(1), Das V, Mittal S, Agarwal update. Endocr Pract 16:118–129.
whose thyroid function recovers A, Sahu M. Overt and subclinical thyroid 15. Zimmerman D 1999 Fetal and neonatal
after an episode of PPTD will become dysfunction among Indian pregnant hyperthyroidism. Thyroid 9:727–733.
hypothyroid at seven years 23. PPTD women and its effect on maternal and 16. Davis LE, Lucas MJ, Hankins GD, Roark
which is a treatable condition causes fetal outcome.Arch Gynecol Obstet. ML, Cunningham FG Thyrotoxicosis
significant maternal morbidity 2010;281(2):215-20. complicating pregnancy. Am J Obstet
in the new mother but often goes 5. Nambiar V, Jagtap VS, Sarathi V, Lila Gynecol 1989;160:63–70
unrecognised as the symptoms are AR Prevalence and Impact of Thyroid 17. Polak M, Le Gac I, Vuillard E,
blamed on maternal depression or Disorders on Maternal Outcome in Asian- Guibourdenche J, Leger J, Toubert
anxiety that are known to occur Indian Pregnant Women Journal of ME, Madec AM, Oury JF, Czernichow
following childbirth. Thyroid Research 2011. P, Luton D Fetal and neonatal thyroid
Certain risk factors have been 6. Jayatissa R, Gunathilaka M M , Ranbanda function in relation to maternal Graves’
identified for the development of J M , Peiris P et al (2013) Iodine status of disease. Best Pract Res Clin Endocrinol
PPTD. A history of autoimmune pregnant women in Sri Lanka Sri Lanka Metab 2004;18:289–302.
thyroid illness, other autoimmune Journal of Diabetes, Endocrinology and 18. Stagnaro-Green A, Abalovich M,
disease and history of PPTD are some Metabolism 3: 4-7. Alexander E, Azizi F, Mestman J,
of these. Identification of risk factors 7. L D K E Premawardhana, A B Parkes, Negro R, Nixon A, Pearce EN, Soldin
for PPTD should lead to screening with P PA Smyth1, C N Wijeyaratne et al OP, Sullivan S, Wiersinga W; American
serum TSH and timely intervention, Increased prevalence of thyroglobulin Thyroid Association Taskforce on
while routine monitoring thereafter antibodies in Sri Lankan schoolgirls ± is Thyroid Disease During Pregnancy and
will enable early identification of iodine the cause? European Journal of Postpartum. Guidelines of the American
permanent hypothyroidism. (Figure Endocrinology (2000) 143 185-188. Thyroid Association for the diagnosis and
1) 8. Abalovich M, Gutierrez S, Alcaraz management of thyroid disease during
G, Maccallini G, Garcia A, Levalle pregnancy and postpartum Thyroid. 2011
Thyroid dysfunction exerts a major O 2002 Overt and subclinical ;21(10):1081-125.
impact on the mother, fetus, neonate hypothyroidismcomplicating pregnancy. 19. Li Y, Shan Z, Teng W, Yu X, Li Y, Fan
and child. Inspite of evidence of Thyroid 12:63–68. C, Teng X, Guo R, Wang H, Li J, Chen
significant disease burden, there 9. Leung AS, Millar LK, Koonings PP, Y, Wang W, Chawinga M, Zhang L,Yang
is currently no rigorous screening Montoro M, Mestman JH 1993 Perinatal L, Zhao Y, Hua T 2010 Abnormalities
program to detect thyroid dysfunction outcome in hypothyroid pregnancies. of maternal thyroid function during
in pregnancy and postpartum period Obstet Gynecol 81:349–353. pregnancy affect neuropsychological
in Sri Lanka. One major reason behind 10. de Escobar GM, Obregón MJ, del Rey development of their children at 25–30
this is inadequate awareness on the FE. Maternal thyroid hormones early in months. Clin Endocrinol (Oxf) 72:825–
magnitude and forms of thyroid pregnancy and fetal brain development. 829.
dysfunction in pregnant women in Sri Best Pract Res Clin Endocrinol Metab 20. Negro R, Schwartz A, Gismondi R, Tinelli
Lanka due to paucity of data, which 2004;18:225-48. A, Mangieri T,Stagnaro-Green A 2010
needs to be addressed immediately. 11. Haddow JE, Palomaki GE, Allan WC, Universal screening versus case finding
Williams JR, Knight GJ, Gagnon J, O’Heir for detection and treatment of thyroid
CE, Mitchell ML, Hermos RJ, Waisbren hormonal dysfunction during pregnancy.
References SE, Faix JD, Klein RZ 1999 Maternal J Clin Endocrinol Metab 95:1699–1707.
thyroid deficiency during pregnancy 21. Stagnaro-Green A 2004 Postpartum
1. Casey BM, Dashe JS, Wells CE, McIntire
and subsequent neuropsychological thyroiditis. Best Pract Res Clin Endocrinol
DD, Byrd W, Leveno KJ, Cunningham FG
development of the child. N Engl J Med Metab 18:303–316.
(2005) Subclinical hypothyroidism and
341:549–555. 22. Smallridge RC 2000 Postpartum thyroid
pregnancy outcomes. Obstet Gynecol
12. Negro R, Schwartz A, Gismondi R, Tinelli disease: a model of immunologic
105:239–245.
A, Mangieri T, Stagnaro-Green A 2010 dysfunction. Clin Appl Immunol Rev
2. Allan WC, Haddow JE, Palomaki
Increased pregnancy loss rate in thyroid 1:89–103.
GE, Williams JR, Mitchell ML, et al
antibody negative women with TSH 23. Premawardhana LD, Parkes AB, Ammari
(2000) Maternal thyroid deficiency and
levels between 2.5 and 5.0 in the first F, et al. Postpartum thyroiditis and long-
pregnancy complications: implications
trimester of pregnancy. J Clin Endocrinol term thyroid status: prognostic influence
for population screening. J Med Screen
Metab 95:E44–8. of thyroid peroxidase antibodies and
7:127–130.
13. John H. Lazarus, M.D., Jonathan P. ultrasound echogenicity. J Clin Endocrinol
3. Saki F, Dabbaghmanesh MH, Ghaemi
Bestwick, M.Sc., Sue Channon Antenatal Metab 2000;85:71–5.
SZ, Forouhari S, Ranjbar Omrani
Thyroid Screening and Childhood
G, Bakhshayeshkaram M. Thyroid
Cognitive Function N Engl J Med 2012;
dysfunction in pregnancy and it’s
366:493-501.
influences on matetrnal and fetal
March 2015 Sri Lanka Journal of Obstetrics and Gynaecology 5
Вам также может понравиться
- Astm D2000 PDFДокумент38 страницAstm D2000 PDFMariano Emir Garcia OdriozolaОценок пока нет
- Hypothyroidism and InfertilityДокумент19 страницHypothyroidism and Infertilitysandeepdogra5357Оценок пока нет
- Acog Practice Bulletin TiroidesДокумент10 страницAcog Practice Bulletin TiroidesMerpi Alvarez Goris100% (1)
- Complementary and Alternative Medical Lab Testing Part 9: GynecologyОт EverandComplementary and Alternative Medical Lab Testing Part 9: GynecologyОценок пока нет
- Scrum Handbook: Scrum Training Institute PressДокумент66 страницScrum Handbook: Scrum Training Institute PressFranky RiveroОценок пока нет
- The Role of Maternal Thyroid Status On Pregnancy Outcome For Motherand NewbornДокумент36 страницThe Role of Maternal Thyroid Status On Pregnancy Outcome For Motherand NewbornRahmayantiYuliaОценок пока нет
- Review Thyroid Disease in PregnancyДокумент7 страницReview Thyroid Disease in PregnancydnnivОценок пока нет
- Thyroid and InfertilityДокумент36 страницThyroid and InfertilitySairindri SahooОценок пока нет
- Route Clearence TeamДокумент41 страницаRoute Clearence Teamctenar2Оценок пока нет
- Hypothyroidism in PregnancyДокумент14 страницHypothyroidism in PregnancyShajia ZafarОценок пока нет
- Congenital HypothyroidismДокумент21 страницаCongenital HypothyroidismDanna GarcíaОценок пока нет
- 148 Thyroid Disease in PregnancyДокумент10 страниц148 Thyroid Disease in Pregnancyobgin uiОценок пока нет
- Graves' Hyperthyroidism in Pregnancy: A Clinical ReviewДокумент22 страницыGraves' Hyperthyroidism in Pregnancy: A Clinical ReviewAnisa Dinda NurlianaОценок пока нет
- Thyroid Disease in PregnancyДокумент70 страницThyroid Disease in PregnancyRajeev Sood100% (1)
- Thyroid Disease in PregnancyДокумент6 страницThyroid Disease in PregnancyCindy KestyОценок пока нет
- Thyroid Dysfunction During Pregnancy: A Review of The Current GuidelinesДокумент7 страницThyroid Dysfunction During Pregnancy: A Review of The Current GuidelinesSSR-IIJLS JournalОценок пока нет
- Preconception Counseling For Thyroid DisordersДокумент7 страницPreconception Counseling For Thyroid DisordersLiya AnjelinaОценок пока нет
- Hipertiroidismo en El Embarazo-The LANCETДокумент12 страницHipertiroidismo en El Embarazo-The LANCETNEIDER11Оценок пока нет
- Thyroid Hormone Therapy of Hypothyroidism in PregnancyДокумент8 страницThyroid Hormone Therapy of Hypothyroidism in PregnancySoul DreamОценок пока нет
- Hypothyroidism Pregnancy BrochureДокумент2 страницыHypothyroidism Pregnancy BrochureNungky KusumaОценок пока нет
- Prevalence of Thyroid Dysfunction in Pregnancy and Its Outcome: The Indian ScenarioДокумент6 страницPrevalence of Thyroid Dysfunction in Pregnancy and Its Outcome: The Indian ScenarioArshiya BegumОценок пока нет
- Assessment and Treatment of Thyroid Disorders in Pregnancy and The Postpartum PeriodДокумент14 страницAssessment and Treatment of Thyroid Disorders in Pregnancy and The Postpartum PeriodErick HernandezОценок пока нет
- Thyroid Physiology and Common Diseases in Pregnancy: Review of LiteratureДокумент8 страницThyroid Physiology and Common Diseases in Pregnancy: Review of LiteratureMarijeimy Alejandra Ortíz FerroОценок пока нет
- Enfermedad Tiroides y Embarazo ACOGДокумент10 страницEnfermedad Tiroides y Embarazo ACOGDairo PintoОценок пока нет
- Negro 2014Документ10 страницNegro 2014stone riverОценок пока нет
- Thyroid Disorders During Pregnancy and A PDFДокумент6 страницThyroid Disorders During Pregnancy and A PDFtania jannah100% (1)
- Thyroid Disorders in PregnancyДокумент3 страницыThyroid Disorders in PregnancyZoel Nikonian100% (1)
- TiroidopatiasДокумент10 страницTiroidopatiasArantza PelaezОценок пока нет
- Management of Hypothyroidism and Hypothyroxinemia During Pregnancy-AaceДокумент8 страницManagement of Hypothyroidism and Hypothyroxinemia During Pregnancy-Aacegu mailОценок пока нет
- Good Clinical Practice Advice: Thyroid and PregnancyДокумент5 страницGood Clinical Practice Advice: Thyroid and Pregnancyjuan carlos pradaОценок пока нет
- Toag 5 4 204 26919 PDFДокумент4 страницыToag 5 4 204 26919 PDFAshnaОценок пока нет
- TOG Thyroid Dysfunction and Reproductive HealthДокумент7 страницTOG Thyroid Dysfunction and Reproductive HealthMarОценок пока нет
- Hyperthyroidism During Pregnancy: Etiology, Diagnosis and ManagementДокумент9 страницHyperthyroidism During Pregnancy: Etiology, Diagnosis and ManagementAdi PratamaОценок пока нет
- Sub Clinical Hypothyroidism in Early Pregnancy in A North Indian Population.Документ12 страницSub Clinical Hypothyroidism in Early Pregnancy in A North Indian Population.locus1Оценок пока нет
- Thyroid Dysfunction and Women's Reproductive Health: Thyroid Volume 14, Supplement 1, 2004 © Mary Ann Liebert, IncДокумент11 страницThyroid Dysfunction and Women's Reproductive Health: Thyroid Volume 14, Supplement 1, 2004 © Mary Ann Liebert, IncAnanda PutraОценок пока нет
- Hypothyroidism and Pregnancy Vol.2Документ9 страницHypothyroidism and Pregnancy Vol.2RakhiОценок пока нет
- Gestational Transient Thyrotoxicosis: M. Taha Albaar, John MF AdamДокумент6 страницGestational Transient Thyrotoxicosis: M. Taha Albaar, John MF AdamMaulana Rahmat HidayatullahОценок пока нет
- Screenshot 2022-10-07 at 5.51.47 AMДокумент14 страницScreenshot 2022-10-07 at 5.51.47 AMManuel PuertaОценок пока нет
- Thyroid Disease in Pregnancy v3.6Документ9 страницThyroid Disease in Pregnancy v3.6nino.matasОценок пока нет
- Comparison of The American Thyroid Association With The Endocrine Society Practice Guidelines For The Screening and Treatment of Hypothyroidism During PregnancyДокумент7 страницComparison of The American Thyroid Association With The Endocrine Society Practice Guidelines For The Screening and Treatment of Hypothyroidism During PregnancySus ArОценок пока нет
- Thyroid & WomenДокумент51 страницаThyroid & Womennitin ranjan guptaОценок пока нет
- Enfermedades Tiroideas en El EmbarazoДокумент14 страницEnfermedades Tiroideas en El EmbarazoMelissa Gómez CruzОценок пока нет
- Эндокринологическая патология и беременность 2018Документ50 страницЭндокринологическая патология и беременность 2018Med PoxОценок пока нет
- Grave DiseaseДокумент6 страницGrave DiseaseFakrocev Charlie GuloОценок пока нет
- Update of Newborn Screening and Therapy For Congenital HypothyroidismДокумент14 страницUpdate of Newborn Screening and Therapy For Congenital HypothyroidismMauricio HurtadoОценок пока нет
- Precocious Puberty With Primary Hypothyroidism Due To Autoimmune ThyroiditisДокумент3 страницыPrecocious Puberty With Primary Hypothyroidism Due To Autoimmune ThyroiditisShohel RanaОценок пока нет
- A Case Report On Intrahepatic Cholestasis of PregnancyДокумент4 страницыA Case Report On Intrahepatic Cholestasis of PregnancyEditor IJTSRDОценок пока нет
- Thyroid Dysfunction and Reproductive Health: ReviewДокумент7 страницThyroid Dysfunction and Reproductive Health: ReviewAnca CucuОценок пока нет
- Etj 0003 0076Документ19 страницEtj 0003 0076ayssa witjaksonoОценок пока нет
- Levothyroxine Treatment in Pregnancy Indications Efficacy and Terapeutic RegimenДокумент12 страницLevothyroxine Treatment in Pregnancy Indications Efficacy and Terapeutic RegimenjacquelineОценок пока нет
- Thyroid Function in Pre EcclampsiaДокумент3 страницыThyroid Function in Pre EcclampsiaIOSRjournalОценок пока нет
- Prevalence of Subclinical and Undiagnosed Overt Hypothyroidismin Habitual AbortionДокумент7 страницPrevalence of Subclinical and Undiagnosed Overt Hypothyroidismin Habitual AbortionIJAR JOURNALОценок пока нет
- 10 11648 J JFMHC 20220801 13Документ4 страницы10 11648 J JFMHC 20220801 13dkhatri01Оценок пока нет
- Tiroid Disease 14 HalamanДокумент14 страницTiroid Disease 14 HalamanDevi SuryandariОценок пока нет
- Bioscientific Review (BSR)Документ10 страницBioscientific Review (BSR)UMT JournalsОценок пока нет
- Hyperprolactinemia and Its Comparision With Hypothyroidism in Infertile WomenДокумент7 страницHyperprolactinemia and Its Comparision With Hypothyroidism in Infertile WomenIJAR JOURNALОценок пока нет
- The Prevalence of Thyroid Dysfunction and HyperproДокумент8 страницThe Prevalence of Thyroid Dysfunction and HyperproHannaОценок пока нет
- Wassner 2018Документ18 страницWassner 2018brendavanessameraaОценок пока нет
- Thyroid-Stimulating Hormone Receptor Antibodies in Pregnancy: Clinical RelevanceДокумент11 страницThyroid-Stimulating Hormone Receptor Antibodies in Pregnancy: Clinical Relevanceocah lakaОценок пока нет
- IndianJEndocrMetab163466-7944218 220402Документ3 страницыIndianJEndocrMetab163466-7944218 220402Raiiad MihaОценок пока нет
- Hyperthyroidism PregnancyДокумент3 страницыHyperthyroidism PregnancySyahfiq IsmailОценок пока нет
- Ijrb 14 677Документ10 страницIjrb 14 677agathaОценок пока нет
- Pregnancy Thyroid Disease 508Документ12 страницPregnancy Thyroid Disease 508Ankush RanaОценок пока нет
- Helipal Tbs Powercube ManualДокумент29 страницHelipal Tbs Powercube Manualoualid zouggarОценок пока нет
- Bathinda - Wikipedia, The Free EncyclopediaДокумент4 страницыBathinda - Wikipedia, The Free EncyclopediaBhuwan GargОценок пока нет
- Reproduction in PlantsДокумент12 страницReproduction in PlantsAnand Philip PrasadОценок пока нет
- UBMM1011 Unit Plan 201501Документ12 страницUBMM1011 Unit Plan 201501摩羯座Оценок пока нет
- Compact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightДокумент2 страницыCompact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightStanley Ochieng' OumaОценок пока нет
- Advantages Renewable Energy Resources Environmental Sciences EssayДокумент3 страницыAdvantages Renewable Energy Resources Environmental Sciences EssayCemerlang StudiОценок пока нет
- Cheerios Media KitДокумент9 страницCheerios Media Kitapi-300473748Оценок пока нет
- 2.1 DRH Literary Translation-An IntroductionДокумент21 страница2.1 DRH Literary Translation-An IntroductionHassane DarirОценок пока нет
- LSL Education Center Final Exam 30 Minutes Full Name - Phone NumberДокумент2 страницыLSL Education Center Final Exam 30 Minutes Full Name - Phone NumberDilzoda Boytumanova.Оценок пока нет
- DLI Watchman®: Vibration Screening Tool BenefitsДокумент2 страницыDLI Watchman®: Vibration Screening Tool Benefitssinner86Оценок пока нет
- Gmail - ICICI BANK I PROCESS HIRING FOR BACKEND - OPERATION PDFДокумент2 страницыGmail - ICICI BANK I PROCESS HIRING FOR BACKEND - OPERATION PDFDeepankar ChoudhuryОценок пока нет
- Investigative JournalismДокумент8 страницInvestigative JournalismMitchie LlagasОценок пока нет
- Case Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Документ15 страницCase Study To Find Tank Bulging, Radial Growth and Tank Settlement Using API 650Jafer SayedОценок пока нет
- Advanced Physiotherapeutic SyllabusДокумент1 страницаAdvanced Physiotherapeutic SyllabusAnup SharmaОценок пока нет
- FHHR 013 Red Tag Procedure PDFДокумент5 страницFHHR 013 Red Tag Procedure PDFN3N5YОценок пока нет
- SahanaДокумент1 страницаSahanamurthyarun1993Оценок пока нет
- D. Das and S. Doniach - Existence of A Bose Metal at T 0Документ15 страницD. Das and S. Doniach - Existence of A Bose Metal at T 0ImaxSWОценок пока нет
- Asu 2019-12Документ49 страницAsu 2019-12janineОценок пока нет
- English For General SciencesДокумент47 страницEnglish For General Sciencesfauzan ramadhanОценок пока нет
- Switching Lab-05b Configuring InterVLAN RoutingДокумент2 страницыSwitching Lab-05b Configuring InterVLAN RoutingHernan E. SalvatoriОценок пока нет
- Reading Stressful Jobs 1 4Документ4 страницыReading Stressful Jobs 1 4Ivana C. AgudoОценок пока нет
- KiSoft Sort & Pack Work Station (User Manual)Документ41 страницаKiSoft Sort & Pack Work Station (User Manual)Matthew RookeОценок пока нет
- Abc Uae Oil and GasДокумент41 страницаAbc Uae Oil and GasajayОценок пока нет
- CUET 2022 General Test 6th October Shift 1Документ23 страницыCUET 2022 General Test 6th October Shift 1Dhruv BhardwajОценок пока нет
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Документ19 страницEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uОценок пока нет
- AppcДокумент71 страницаAppcTomy lee youngОценок пока нет
- Modified Airdrop System Poster - CompressedДокумент1 страницаModified Airdrop System Poster - CompressedThiam HokОценок пока нет