Академический Документы
Профессиональный Документы
Культура Документы
Infodatin Ibu
Загружено:
chintyamontang0 оценок0% нашли этот документ полезным (0 голосов)
21 просмотров39 страницca servix
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документca servix
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
21 просмотров39 страницInfodatin Ibu
Загружено:
chintyamontangca servix
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 39
Hanggoro Tri Rinonce, MD, PhD - Department of Anatomical Pathology, Faculty of Medicine, Gadjah Mada University
Normal anatomy of female
reproductive system
INTRODUCTION
• Most tumors of the cervix
– epithelial origin
– caused by oncogenic strains of human papillomavirus
(HPV).
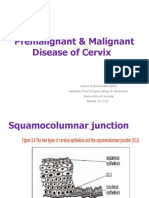
• During development, the columnar, mucus-secreting
epithelium of the endocervix is joined to the squamous
epithelial covering of the exocervix at the cervical os.
• Onset of puberty
– the squamocolumnar junction eversion columnar
epithelium to become visible on the exocervix.
• The exposed columnar cells undergo squamous
metaplasia transformation zone.
Development of the cervical transformation zone
PATHOGENESIS
• HPV has a tropism for the immature
squamous cells of the transformation zone.
• Most HPV infections are transient and are
eliminated within months by an acute and
chronic inflammatory response.
• A subset of infections persists cervical
intraepithelial neoplasia (CIN) invasive
cervical carcinomas.
• HPV is detectable in nearly all cases of CIN and
cervical carcinoma.
• Important risk factors for the development of CIN
and invasive carcinoma thus are directly related
to HPV exposure and include
– Early age at first intercourse
– Multiple sexual partners
– Male partner with multiple previous sexual partners
– Persistent infection by high-risk strains of
papillomavirus
• Although HPV infection occurs in the most immature
squamous cells of the basal layer, replication of HPV DNA
takes place in more differentiated overlying squamous cells.
• Squamous cells at this stage of maturation do not normally
replicate DNA, but HPV-infected squamous cells do, as a
consequence of expression of two potent oncoproteins
encoded in the HPV genome called E6 and E7.
• The E6 and E7 proteins bind and inactivate two critical
tumor suppressors, p53 and Rb, respectively, and in doing
so promote growth and increased susceptibility to
additional mutations that may eventually lead to
carcinogenesis.
• Recognized serotypes of HPV can be classified as high-risk or low-risk
types based on their propensity to induce carcinogenesis.
• High-risk HPV infection is the most important risk factor for the
development of CIN and carcinoma. Two highrisk HPV strains, types
16 and 18, account for approximately
• 70% of cases of CIN and cervical carcinoma. In general, infections
with high-risk HPV serotypes are more likely to persist, which is a risk
factor for progression to carcinoma.
• These HPV subtypes also show a propensity to integrate into the host
cell genome, an event that is linked to progression.
• Low-risk HPV strains (e.g., types 6 and 11), on the other hand, are
associated with development of condylomas of the lower genital
tract and do not integrate into the host genome, remaining instead
as free episomal viral DNA.
• Despite the strong association of HPV infection with cancer of the
cervix, HPV is not sufficient to drive the neoplastic process. As
mentioned below, several HPV-infected highgrade precursor lesions
do not progress to invasive cancer.
Possible consequences of
human papillomavirus (HPV)
infection. Progression is
associated with integration
of virus and acquisition of
additional mutations. CIN,
cervical intraepithelial
neoplasia.
Cervical Intraepithelial Neoplasia (CIN)
• HPV-related carcinogenesis begins with the precancerous epithelial change termed CIN, which
usually precedes the development of an overt cancer by many years, sometimes decades.
• CIN peaks in incidence at about 30 years of age, whereas invasive carcinoma peaks at about 45
years of age.
• Low-grade dysplasia (CIN I) moderate dysplasia (CIN II) severe dysplasia (CIN III).
• The higher the grade of CIN, the greater the likelihood of progression
• Because decisions about patient management are two-tiered (i.e., observation versus surgical
treatment), this three-tiered grading system has recently been simplified to a two-tiered system,
with CIN I renamed low-grade squamous intraepithelial lesion (LSIL) and CIN II and CIN III
combined into one category referred to as high-grade squamous intraepithelial lesion (HSIL).
• As shown in Table 18–1, the decision to treat HSIL and to observe LSIL is based on differences in the
natural histories of these two groups of lesions.
Natural History of Squamous Intraepithelial Lesions (SILs)
• CIN I
– dyplastic changes in the lower third of the squamous epithelium
– koilocytotic change in the superficial layers of the epithelium.
• CIN II
– Dysplasia extends to the middle third of the epithelium and
takes the form of delayed keratinocyte maturation.
– Some variation in cell and nuclear size, heterogeneity of nuclear
chromatin, and presence of mitoses above the basal layer
extending into the middle third of the epithelium.
– The superficial layer of cells shows some differentiation and
occasionally demonstrates the koilocytotic changes described.
• CIN III
– almost complete loss of maturation
– greater variation in cell and nuclear size
– chromatin heterogeneity
– disorderly orientation of the cells
– normal or abnormal mitoses
– affect virtually all layers of the epithelium
– koilocytotic change usually is absent
Spectrum of cervical intraepithelial neoplasia (CIN), with normal
squamous epithelium for comparison: CIN I with koilocytotic atypia;
CIN II with progressive atypia in all layers of the epithelium; and CIN III
(carcinoma in situ) with diffuse atypia and loss of maturation.
Wart virus infection with CIN
Carcinoma in situ (CIN III)
Carcinoma in situ (CIN III)
Cytologic features of cervical intraepithelial neoplasia (CIN) in a Papanicolaou smear.
Superficial squamous cells may stain either red or blue.
A. Normal exfoliated superficial squamous epithelial cells.
B. CIN 1—low-grade squamous intraepithelial lesion (LSIL).
C and D. CIN II and CINIII, respectively—both high-grade squamous intraepithelial lesions
(HSILs).
Note the reduction in cytoplasm and the increase in the nucleus-to-cytoplasm ratio as the
grade of the lesion increases. This observation reflects the progressive loss of cellular
differentiation on the surface of the cervical lesions from which these cells are exfoliated .
SIGNS AND SYMTOMS
DIAGNOSIS
Invasive Carcinoma of the Cervix
• The most common cervical carcinomas are squamous
cell carcinomas (75%), followed by adenocarcinomas
and mixed adenosquamous carcinomas (20%) and
small cell neuroendocrine carcinomas (less than 5%).
• All of these types of carcinomas are caused by HPV.
• Of interest, the relative proportion of adenocarcinomas
has been increasing in recent decades owing to the
decreasing incidence of invasive squamous carcinoma
and suboptimal detection of glandular lesions by Pap
smear.
WHO histological classification of tumor of the uterine cervix
SQUAMOUS CELL CARCINOMA
• Squamous cell carcinoma has a peak incidence at the age of
about 45 years, some 10 to 15 years after detection of
precursor CIN.
• Progression of CIN to invasive carcinoma is variable and
unpredictable and requires HPV infection as well as
mutations in genes such as LKB.
• Risk factors for progression include cigarette smoking and
human immunodeficiency virus (HIV) infection, the latter
finding suggesting that immune surveillance has a role in
holding CIN in check.
• Although risk factors may help stratify patients who are
likely to progress from CIN to carcinoma, the only reliable
way to monitor the disease course is with frequent physical
examinations coupled with biopsy of suspicious lesions.
Cervical os with
surrounding,
invasive, exophytic
cervical carcinoma.
• Invasive carcinomas of the cervix develop in the
transformation zone and range from microscopic foci of
stromal invasion to grossly conspicuous exophytic tumors.
• Tumors encircling the cervix and penetrating into the
underlying stroma produce a barrel cervix, which can be
identified by direct palpation.
• Extension into the parametrial soft tissues can affix the
uterus to the surrounding pelvic structures.
• The likelihood of spread to pelvic lymph nodes correlates
with the depth of tumor invasion and the presence of
tumor cells in vascular spaces.
• The risk of metastasis increases from less than 1% for
tumors under 3 mm in depth
ADENOCARCINOMA IN SITU
ADENOCARCINOMA
• 5-15% of invasive cervical carcinomas, higher percentage in Jewish women
• Incidence increasing in US, now up to 25% of cervical cancers, due to decreasing rates of squamous
cell carcinoma and difficulty in diagnosis using current screening methods; increased frequency in
young women (Cancer 2004;100:1035)
• Usually associated with in-situ adenocarcinoma (mean 5 year interval, which is less than for SIL)
• Suspected but still unproven association with oral contraceptives
• Endocervical adenocarcinoma is associated with ovarian mucinous adenocarcinoma and ovarian
endometrioid adenocarcinoma
• 30-50% false negative reports by cytology
• p16 may be sensitive/specific for diagnosing adenocarcinoma (invasive or in-situ) by histology or
Thin-Prep (Am J Surg Pathol 2003;27:187, but see Hum Pathol 2002;33:899)
• Often vaginal bleeding, pelvic pain
• Spreads first to pelvic structures, then pelvic lymph nodes; metastases to ovaries, upper abdomen,
distant organs
• Mixed if there is 10% or more of a second component
• Survival by stage: I-79%, II-37%, III/IV-less than 9%
• Poor prognostic factors: high stage (including depth > 5 mm, Int J Gynecol Cancer 2004;14:104),
angiolymphatic invasion, high grade (Gynecol Oncol 2004;92:262); also HER2 overexpression,
elevated serum CA125
• Gross description
– Exophytic mass, ulcerated plaque or barrel-shaped cervix (diffuse
enlargement)
• Micro description
– Often well differentiated with endocrine morphology and mucin that
may leak into stroma; may also be poorly differentiated, papillary,
endometrioid or have psammoma bodies
– Microscopic invasion: individual cells or incomplete glands lined by
malignant cells at a stromal interface or malignant glands surrounded
by a desmoplastic host response
– Other evidence of invasion is architecturally complex, branching, or
small glands, which grow confluently or in a labyrinthine pattern;
cribriform growth pattern of malignant epithelium devoid of stroma
within a single gland profile; and the presence of glands below the
deep margin of normal glands; rare findings are focal cilia (Acta Cytol
2005;49:187)
• Tumor grade of adenocarcinoma (for classical adenocarcinoma, not
variants; not universally accepted):
• Grade 1: well-differentiated (10% or less solid growth); tumor contains
well-formed regular glands with papillae; cells are elongate and columnar
with uniform oval nuclei; minimal stratification (fewer than three cell
layers in thickness); infrequent mitotic figures
• Grade 2: moderately differentiated (11% to 50% solid growth); tumor
contains complex glands with frequent bridging and cribriform formation;
solid areas up to 50% of tumor; nuclei more rounded and irregular; small
nucleoli present; mitoses more frequent
• Grade 3: poorly differentiated (over 50% solid growth); sheets of
malignant cells; few glands are discernible; cells are large and irregular
with pleomorphic nuclei; occasional signet cells are present; mitoses are
abundant with abnormal forms; marked desmoplasia; necrosis is common
well-differentiated
moderately differentiated
poorly differentiated
CLINICAL COURSE
• Invasive cervical cancer most often is seen in women who have
never had a Pap smear or who have not been screened for many
years.
• In such cases, cervical cancer often is symptomatic, with patients
coming to medical attention for unexpected vaginal bleeding,
leukorrhea, painful coitus (dyspareunia), or dysuria.
• Treatment is surgical by hysterectomy and lymph node dissection;
small microinvasive carcinomas may be treated with cone biopsy.
• Mortality is most strongly related to tumor stage and, in the case of
neuroendocrine carcinomas, to cell type.
• Most patients with advanced disease die as a result of local invasion
rather than distant metastasis.
• In particular, renal failure stemming from obstruction of the urinary
bladder and ureters is a common cause of death.
Вам также может понравиться
- Praktikum Reproduksi 2Документ46 страницPraktikum Reproduksi 2Andika Tatag100% (1)
- Pathology of Breast CancerДокумент22 страницыPathology of Breast CancerfadoОценок пока нет
- 10a.cervical CancerДокумент49 страниц10a.cervical CancerRagone MseraОценок пока нет
- 9.cancer of The Female Genital Tract.Документ58 страниц9.cancer of The Female Genital Tract.vichramОценок пока нет
- 1 - Cervical CancerДокумент87 страниц1 - Cervical Cancerzuzuyasi65Оценок пока нет
- Premalignant & Malignant Disease of CervixДокумент64 страницыPremalignant & Malignant Disease of CervixDegefaw BikoyОценок пока нет
- 1 Benign and Malignant Lesions of The CervixДокумент46 страниц1 Benign and Malignant Lesions of The CervixRohitОценок пока нет
- Etiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsДокумент33 страницыEtiopathogenesis and Natural History of Carcinoma Cervix: Human Papilloma Virus High Risk FactorsNatasya Ayusandra MahersaputriОценок пока нет
- Milla Kviatkovsky, OMS-III, April 2013Документ23 страницыMilla Kviatkovsky, OMS-III, April 2013api-210786702Оценок пока нет
- Cervical Intraepithelial Neoplasia and Cervical CancerДокумент28 страницCervical Intraepithelial Neoplasia and Cervical CancerNatnael100% (1)
- Lesson Plan On Cervical Cancer Vaccines: Mini ProjectДокумент11 страницLesson Plan On Cervical Cancer Vaccines: Mini ProjectGargi MPОценок пока нет
- 24 - Pathology of CervixДокумент19 страниц24 - Pathology of CervixRyubusa HayabusaОценок пока нет
- Pre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5Документ147 страницPre Malignant and Malignant Lesions of Cervix: Gynaec Unit 5FarazОценок пока нет
- 8-Cervical CancerДокумент45 страниц8-Cervical CancerBekeОценок пока нет
- Abnormal Cervical CytologyДокумент21 страницаAbnormal Cervical CytologyNatalia HaikaliОценок пока нет
- Benign and Malignant Tumors of CervixДокумент37 страницBenign and Malignant Tumors of CervixFirifan DiribaОценок пока нет
- Cervical CancerДокумент36 страницCervical CancerDebabrata SatapathyОценок пока нет
- Learning Unit 8 - Neoplasia of The Female Genital TractДокумент28 страницLearning Unit 8 - Neoplasia of The Female Genital TractMarelize ErasmusОценок пока нет
- CACXДокумент34 страницыCACXMax ZealОценок пока нет
- Summary of Data: Cervical Cancer and ScreeningДокумент10 страницSummary of Data: Cervical Cancer and Screeningpalomazul007Оценок пока нет
- Pre Mal Dis of CervixДокумент44 страницыPre Mal Dis of CervixnoreenfatimamaanОценок пока нет
- 10 Cervical NeoplasiaДокумент33 страницы10 Cervical NeoplasiaDawit g/kidanОценок пока нет
- CCSP - NewДокумент69 страницCCSP - NewasdfОценок пока нет
- Disease of Female Reproductive System: Maria Picu, MDДокумент66 страницDisease of Female Reproductive System: Maria Picu, MDAbanoub AwadallaОценок пока нет
- Premalignant Lesions of The Uterine Cervix - Sundhed - DKДокумент7 страницPremalignant Lesions of The Uterine Cervix - Sundhed - DKPavel BerlinschiОценок пока нет
- KarsinomaДокумент12 страницKarsinomaWahyudi Pratama HarliОценок пока нет
- Screenshot 2022-10-26 at 7.27.40 PMДокумент36 страницScreenshot 2022-10-26 at 7.27.40 PMhamdacawad22Оценок пока нет
- Septiya Agestin Cahyaningrum - Malignancy in Reproductive Health System - WordДокумент30 страницSeptiya Agestin Cahyaningrum - Malignancy in Reproductive Health System - WordSepty KawaiОценок пока нет
- Cervical CancerДокумент3 страницыCervical CancernoblefxОценок пока нет
- Case StudyДокумент18 страницCase StudyKristine Joy RevañoОценок пока нет
- Pathologic Types: o o o oДокумент2 страницыPathologic Types: o o o orexzordОценок пока нет
- Malignant Diseases of BreastДокумент70 страницMalignant Diseases of BreastdranjupradhanОценок пока нет
- BreastДокумент50 страницBreastعلي عليОценок пока нет
- Colorectal CancersДокумент162 страницыColorectal CancersSomto NwabuezeОценок пока нет
- Aetiology, Pathogenesis, and Pathology of Cervical NeoplasiaДокумент9 страницAetiology, Pathogenesis, and Pathology of Cervical NeoplasiaKamilah NasarОценок пока нет
- Cervical Cancer: Emedicine Specialties Obstetrics and Gynecology Gynecologic OncologyДокумент19 страницCervical Cancer: Emedicine Specialties Obstetrics and Gynecology Gynecologic OncologyFatah Abdul YasirОценок пока нет
- 1.female Genital SystemДокумент114 страниц1.female Genital Systemأسود / BlackОценок пока нет
- Benign and Premalignant Disease of The CervixДокумент23 страницыBenign and Premalignant Disease of The CervixJ.V. Siritt ChangОценок пока нет
- Diseases of Female Reproductive SystemДокумент13 страницDiseases of Female Reproductive SystemSalon LamichhaneОценок пока нет
- Penile Cancer - ClinicalKeyДокумент11 страницPenile Cancer - ClinicalKeyDenisse MejiaОценок пока нет
- Cervical Intraepithilial NeoplasiaДокумент41 страницаCervical Intraepithilial Neoplasiadrtasmiaakter100% (1)
- Female Genital PathologyДокумент62 страницыFemale Genital PathologySingitan SiyoumОценок пока нет
- Endometrial Malignancies 1Документ41 страницаEndometrial Malignancies 1jerrydanfordfxОценок пока нет
- Phyllodes TumorДокумент20 страницPhyllodes TumorManuela KarinaaОценок пока нет
- Breast Pathology: Lecturer: Hanina Hibshoosh, M.DДокумент35 страницBreast Pathology: Lecturer: Hanina Hibshoosh, M.DPaulo MartinsОценок пока нет
- Cervic Tumour - SummaryДокумент9 страницCervic Tumour - SummaryRUDOLF YUSON BM20110052Оценок пока нет
- Cervical Cancer - A Global Health CrisisДокумент9 страницCervical Cancer - A Global Health Crisispb.nakulaОценок пока нет
- Cervical Intraepithelial NeoplasiaДокумент16 страницCervical Intraepithelial Neoplasiaalejandro fernandezОценок пока нет
- Pathology of The OvaryДокумент7 страницPathology of The OvaryLorMD34Оценок пока нет
- Carcinoma BreastДокумент8 страницCarcinoma BreastYeshvi s100% (1)
- Cervical Cancer: Dr. Vijay PrakashДокумент23 страницыCervical Cancer: Dr. Vijay PrakashVijay PrakashОценок пока нет
- 7.4 Malignant Conditions of ChildhoodДокумент9 страниц7.4 Malignant Conditions of ChildhoodΜατθαίος ΠαππάςОценок пока нет
- Uterine Body Carcinoma - DRJДокумент35 страницUterine Body Carcinoma - DRJJyoti MishraОценок пока нет
- HSILДокумент7 страницHSILYudha GanesaОценок пока нет
- Naspub Ca VulvaДокумент8 страницNaspub Ca VulvaLisa Raihan LutfiaОценок пока нет
- Data Persalinan & Kematian Ibu Tahun 2017Документ32 страницыData Persalinan & Kematian Ibu Tahun 2017HansОценок пока нет
- Cervical DysplasiaДокумент4 страницыCervical DysplasiaCarleta StanОценок пока нет
- Female Reproductive SystemДокумент12 страницFemale Reproductive SystemAli KhanОценок пока нет
- Neoplasms of TestisДокумент26 страницNeoplasms of TestisFeddyFebriyantoManurungОценок пока нет
- Infectious Causes of Cancer: A Guide for Nurses and Healthcare ProfessionalsОт EverandInfectious Causes of Cancer: A Guide for Nurses and Healthcare ProfessionalsОценок пока нет
- Psychotropic - TransquilizerДокумент45 страницPsychotropic - Transquilizerchintyamontang100% (1)
- Drug Use During Pregnancy and LactationДокумент50 страницDrug Use During Pregnancy and LactationchintyamontangОценок пока нет
- DR Santy Fisiologi Penglihatan UNTADДокумент45 страницDR Santy Fisiologi Penglihatan UNTADchintyamontangОценок пока нет
- Cerebral Spinal Fluid & The MeningesДокумент25 страницCerebral Spinal Fluid & The MeningeschintyamontangОценок пока нет
- Management of Stroke: Dr. Isnaniah, Sp. SДокумент80 страницManagement of Stroke: Dr. Isnaniah, Sp. SchintyamontangОценок пока нет
- TransductionДокумент14 страницTransductionArchana RakibeОценок пока нет
- Evaluation of Bacterial Antagonists of Ralstonia Solanacearum, CausalДокумент6 страницEvaluation of Bacterial Antagonists of Ralstonia Solanacearum, CausalHvzem MohammedОценок пока нет
- Acute Hematogenous Osteomyelitis in Children: Pathogenesis, Diagnosis, and TreatmentДокумент10 страницAcute Hematogenous Osteomyelitis in Children: Pathogenesis, Diagnosis, and TreatmentMerlin MuktialiОценок пока нет
- Microcarrier Cell Culture HandbookДокумент140 страницMicrocarrier Cell Culture HandbookDolphing100% (1)
- Biology Investigatory ProjectДокумент11 страницBiology Investigatory ProjectAkileshОценок пока нет
- Types of Specimens 4.1Документ21 страницаTypes of Specimens 4.1Maxwell C Jay KafwaniОценок пока нет
- Cerevisiae and Other Fungi: Principles of Gene Manipulation by Liuzengran Hebei University of Economics and BusinessДокумент81 страницаCerevisiae and Other Fungi: Principles of Gene Manipulation by Liuzengran Hebei University of Economics and BusinessManuel DíazОценок пока нет
- Mutations of Voltage-Gated Sodium Channel Genes SCN1A and SCN2A in Epilepsy, Intellectual Disability, and AutismДокумент19 страницMutations of Voltage-Gated Sodium Channel Genes SCN1A and SCN2A in Epilepsy, Intellectual Disability, and Autismyasmin al ammariОценок пока нет
- Cobb. Tech Focus2024.avian InfuenzaДокумент18 страницCobb. Tech Focus2024.avian Infuenzaikram chohanОценок пока нет
- June 2008 QP - Paper 1 CIE Biology A-LevelДокумент20 страницJune 2008 QP - Paper 1 CIE Biology A-LevelDamien SibandaОценок пока нет
- Model MBBS Syllabus (DR Apurba Sastry, DR Sandhya Bhat) PDFДокумент22 страницыModel MBBS Syllabus (DR Apurba Sastry, DR Sandhya Bhat) PDFmajoragarwal1195Оценок пока нет
- Chapter 2 History of MicrobiologyДокумент39 страницChapter 2 History of MicrobiologyChristian AbordoОценок пока нет
- Ilovepdf MergedДокумент25 страницIlovepdf Mergedyufm2008Оценок пока нет
- Ihc PDFДокумент28 страницIhc PDFJean Bosco ByendaОценок пока нет
- 1SC0 1BF Que 20190515Документ16 страниц1SC0 1BF Que 20190515Thasanya AlgamaОценок пока нет
- Humoral Immunity 2022 MBBSДокумент58 страницHumoral Immunity 2022 MBBSCraft Hachz By dhiyaОценок пока нет
- Covid 19 Vaccines An Australian ReviewДокумент18 страницCovid 19 Vaccines An Australian ReviewLMCG DocketОценок пока нет
- SANOFI Brochure PartneringДокумент26 страницSANOFI Brochure PartneringÉtoile JolieОценок пока нет
- SURFING National Biology 4 Maitaing Internal Sample PDFДокумент21 страницаSURFING National Biology 4 Maitaing Internal Sample PDFelamОценок пока нет
- Adverse Drug Events in The Oral Cavity PDFДокумент13 страницAdverse Drug Events in The Oral Cavity PDFdaruОценок пока нет
- (October 2019) NMAT Study Guide Ver. 1.BДокумент75 страниц(October 2019) NMAT Study Guide Ver. 1.Bmikhaela saboОценок пока нет
- ADN Descubrimiento 2018Документ37 страницADN Descubrimiento 2018Paul Suarez MaldonadoОценок пока нет
- AVN HCCC ReplyДокумент27 страницAVN HCCC Replyd-fbuser-31847459Оценок пока нет
- LAB 11 Biochemical TestsДокумент15 страницLAB 11 Biochemical TestsDeena Hajj QasemОценок пока нет
- Asepsis 1Документ52 страницыAsepsis 1严子明 Renz Ryan SevillenoОценок пока нет
- T Lymphocytes and Macrophages in The Intestinal Tissues of Dogs Infected With Leishmania InfantumДокумент12 страницT Lymphocytes and Macrophages in The Intestinal Tissues of Dogs Infected With Leishmania InfantumWillОценок пока нет
- Hormones and Behavior and The Integration of Brain-Body ScienceДокумент7 страницHormones and Behavior and The Integration of Brain-Body SciencePerla Arguelles CastroОценок пока нет
- Paper Pet ProjectДокумент27 страницPaper Pet Projectapi-406104878Оценок пока нет
- Light and Immunomodulation: Joan E. RobertsДокумент11 страницLight and Immunomodulation: Joan E. RobertsBhavani U KulkarniОценок пока нет
- OTITIS Concept MapДокумент7 страницOTITIS Concept MapElleОценок пока нет