Академический Документы
Профессиональный Документы
Культура Документы
Jamaotolaryngology Maxwell 2017 Oi 160147
Загружено:
Benny KurniawanАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Jamaotolaryngology Maxwell 2017 Oi 160147
Загружено:
Benny KurniawanАвторское право:
Доступные форматы
Research
JAMA Otolaryngology–Head & Neck Surgery | Original Investigation
Association of Preoperative Calcium and Calcitriol Therapy
With Postoperative Hypocalcemia After Total Thyroidectomy
Anne K. Maxwell, MD; David C. Shonka Jr, MD; Derek J. Robinson, MD; Paul A. Levine, MD
IMPORTANCE Hypocalcemia is the most common complication after total thyroidectomy and
can result in prolonged hospital admissions and increased hospital charges.
OBJECTIVE To determine the effectiveness of preoperative calcium and calcitriol
supplementation in reducing hypocalcemia following total thyroidectomy.
DESIGN, SETTING, AND PARTICIPANTS A retrospective cohort study was conducted at a
tertiary care center in 65 patients undergoing total thyroidectomy by a single surgeon.
Patients were divided into 2 groups: those receiving preoperative as well as postoperative
supplementation with calcium carbonate, 1000 to 1500 mg, 3 times daily and calcitriol, 0.25
to 0.5 μg, twice daily, and those receiving only postoperative supplementation with those
agents at the same dosages. Data on patients who underwent surgery between January 1,
2008, and December 31, 2011, were acquired, and data analyses were conducted from March
through June 2012, and from October through December 2016.
INTERVENTIONS Calcium and calcitriol therapy.
MAIN OUTCOMES AND MEASURES Postoperative serum calcium levels and development of
postoperative hypocalcemia.
RESULTS Of the 65 patients who underwent total thyroidectomy 27 (42%) were men; mean
(SD) age was 49.7 (16.7) years. Thirty-three patients received preoperative calcium and
calcitriol supplementation, and 32 patients received only postoperative therapy. In the
preoperative supplementation group, 15 of 33 (45%) patients underwent complete central
compartment neck dissection and 11 of 33 (33%) had lateral neck dissection, compared with
16 of 32 (50%) and 12 of 32 (38%), respectively, patients without preoperative
supplementation. The mean measured serum calcium level in those without preoperative
supplementation vs those with supplementation are as follows: preoperative, 9.6 vs 9.4
mg/dL (absolute difference, 0.16; 95% CI, −0.12 to 0.49 mg/dL); 12 hours postoperative, 8.3
vs 8.6 mg/dL (absolute difference, −0.30; 95% CI, −0.63 to 0.02 mg/dL); and 24 hours
postoperative, 8.4 vs 8.5 mg/dL (absolute difference, −0.13; 95% CI, −0.43 to 0.16 mg/dL).
In patients not receiving preoperative supplementation, 5 of 32 (16%) individuals became
symptomatically hypocalcemic vs 2 of 33 (6%) in the preoperative supplementation group;
an absolute difference of 10% (95% CI, −6.6% to 26.3%). Compared with the group not
receiving preoperative supplementation, the mean [SD] length of stay was significantly
shorter in the preoperative supplementation group (3.8 [1.8] vs 2.9 [1.4] days; absolute Author Affiliations: University of
difference, −0.9; 95% CI, −1.70 to −0.105 days). Preoperative supplementation resulted in an Virginia School of Medicine,
estimated $2819 savings in charges per patient undergoing total thyroidectomy. University of Virginia Health System,
Charlottesville (Maxwell); Now with
Department of Otolaryngology,
CONCLUSIONS AND RELEVANCE Preoperative calcium and calcitriol supplementation, in University of Colorado, Denver
addition to routine postoperative supplementation, was associated with a reduced incidence (Maxwell); Department of
of symptomatic hypocalcemia, length of hospital stay, and overall charges following total Otolaryngology–Head and Neck
Surgery, University of Virginia Health
thyroidectomy. System, Charlottesville (Shonka,
Robinson, Levine).
Corresponding Author: David C.
Shonka Jr, MD, Department of
Otolaryngology–Head and Neck
Surgery, University of Virginia Health
JAMA Otolaryngol Head Neck Surg. 2017;143(7):679-684. doi:10.1001/jamaoto.2016.4796 System, Box 800713, Charlottesville,
Published online April 13, 2017. VA 22908 (dcs5z@virginia.edu).
(Reprinted) 679
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Research Original Investigation Preoperative Calcium and Calcitriol and Hypocalcemia After Thyroidectomy
H
ypocalcemia is the most frequent complication of total
thyroidectomy. It can be defined either biochemi- Key Points
cally or clinically. There is no universal agreement on
Question Does preoperative calcium and calcitriol
the serum calcium level that constitutes biochemical hypo- supplementation decrease the incidence of hypocalcemia
calcemia, but many studies define this as a measured serum following total thyroidectomy?
calcium level less than 8.0 mg/dL (to convert to millimoles per
Findings In this cohort study of 65 patients, preoperative
liter, multiply by 0.25). Patients with clinical hypocalcemia ex-
supplementation with calcium and calcitriol was associated with a
hibit symptoms of perioral or fingertip numbness or tingling, reduced incidence of symptomatic hypocalcemia, length of
or presence of the Chvostek sign in the setting of biochemical hospital stay, and overall costs following total thyroidectomy.
hypocalcemia. Hypocalcemia may also be categorized tempo-
Meaning This study supports the use of preoperative calcium and
rally as transient or permanent. In transient hypocalcemia, se-
calcitriol supplementation for patients undergoing total
rum calcium levels reach a nadir from 24 to 48 hours postop- thyroidectomy.
eratively, but subsequently return to the reference range within
6 months.1-3 Permanent hypocalcemia is defined as hypocal-
cemia persisting beyond 6 months postoperatively and is due vitamin D (ie, calcitriol) is immediately bioavailable and is theo-
to permanent hypoparathyroidism. It is less frequent, occur- retically beneficial within a few days of initiating therapy. The
ring in 2% to 8% of patients, compared with transient hypo- hypothesis of this study is that preoperative supplementation
calcemia, which occurs in up to half of patients.3-6 Persistent with calcium and calcitriol would result in decreased postthy-
symptomatic hypocalcemia, intravenous calcium require- roidectomy hypocalcemia and a shorter hospital stay. To our
ments, and laboratory monitoring often prolong hospital stay knowledge, there are no published prospective studies to date
and delay recovery after total thyroidectomy.1 More severe risks comparing preoperative and postoperative calcitriol and calcium
to the patient who experiences significant hypocalcemia in- supplementation with postoperative supplementation alone.
clude hypotension, tetany, seizure, and arrhythmia. The pa-
tients also bear additional financial burdens when they expe-
rience this complication, including hospital charges for
repletion, laboratory testing, and increased length of hospi-
Methods
tal stay. A retrospective cohort study was conducted of patients un-
Calcium absorption is regulated primarily via parathy- dergoing total thyroidectomy at the University of Virginia De-
roid hormone and vitamin D. Vitamin D3 (cholecalciferol) is partment of Otolaryngology–Head and Neck Surgery be-
acquired via diet or photon-stimulated conversion of tween January 1, 2008, and December 31, 2011. Data analyses
precursors in the skin. In the liver, it is hydroxylated to 25- were conducted from March through June 2012, and from Oc-
hydroxyvitamin D3 (calcifediol), which, due to its half-life of tober through December 2016. This study was approved by the
2 to 3 weeks, is the most useful measure of vitamin D levels. University of Virginia Institutional Review Board with waiver
When stimulated by parathyroid hormone, the enzyme 1α- hy- of informed consent. There was no financial compensation.
droxylase in the kidney further hydroxylates 25-OHD3 to the Patients were included in the study if they had a total thy-
active form 1,25-dihydroxyvitamin D3 (calcitriol).1,7 Acti- roidectomy performed by the senior author (P.A.L.), if they
vated vitamin D increases calcium absorption from the intes- were treated with routine postoperative calcium and cal-
tine. Vitamin D deficiency is a known independent risk factor citriol supplementation, and if the presence or absence of pre-
for postthyroidectomy hypocalcemia.1,8,9 Previous research has operative calcium and calcitriol supplementation was clearly
identified 15 ng/mL as the threshold below which patients ex- documented in the medical record. Patients were analyzed in
perience an increased risk of transient postoperative 2 groups: (1) those who received 5 days of preoperative oral cal-
hypocalcemia.8,10 Underlying secondary hyperparathyroid- cium carbonate, 1000 to 1500 mg, 3 times daily and cal-
ism due to low calcium and vitamin D levels is thought to be citriol, 0.25 to 0.5 μg twice daily supplementation and (2) those
the mechanism behind the increased risk of hypocalcemia in who did not receive preoperative supplementation. Both
patients with vitamin D deficiency.8 groups received routine postoperative calcium and calcitriol
Previous studies have demonstrated the efficacy of routine supplementation at dosages the same as those described above.
postoperative calcium and vitamin D supplementation as a pro- The decision to treat patients with preoperative calcium and
phylactic strategy for preventing hypocalcemia in patients un- calcitriol supplementation was made by the senior author at
dergoing total thyroidectomy, but evaluations of preoperative the time of the preoperative workup in clinic. Although this
supplementation are limited.2,11-14 Preoperative supplementa- was not designed as a prospective trial, during the time of this
tion with vitamin D in inactivated forms (ergocalciferol, chole- study there was a gradual transition from never using preop-
calciferol) is unlikely to be beneficial because this can require up erative calcium and calcitriol supplementation to the routine
to two 8-week courses of supplementation, which is unrealistic use of preoperative supplementation. During this transition in
in the preoperative setting.15 One single-arm study of preopera- clinical practice, the senior author randomly treated patients
tive and postoperative supplementation with calcium and inac- with preoperative supplementation without regard to labora-
tivated vitamin D in patients undergoing total thyroidectomy tory results or planned extent of surgery.
showed rates of symptomatic hypocalcemia and biochemical hy- For patients who met the inclusion criteria, data collected
pocalcemia of 6% and 10%, respectively.16 Alternatively, activated from the electronic medical record included age, sex, diagnosis,
680 JAMA Otolaryngology–Head & Neck Surgery July 2017 Volume 143, Number 7 (Reprinted) jamaotolaryngology.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Preoperative Calcium and Calcitriol and Hypocalcemia After Thyroidectomy Original Investigation Research
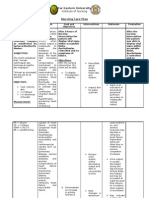
Table 1. Patient Demographics
No. (%)
Characteristic No Preoperative Supplement Preoperative Supplement Effect Size (95% CI), %
Patients, No. 32 33
Men 16 (50) 11 (33)
17 (−7 to 38)
Women 16 (50) 22 (67)
Age, mean (SD), y 47 (16) 52 (17) 5.2 (−3.1 to 13.4)
Diagnosis
Cancer 26 (81) 29 (88)
7 (−11 to 25)
Benign 6 (19) 4 (12)
Central ND 16 (50) 15 (45) 5 (−19 to 27)
Lateral ND 12 (38) 11 (33) 4 (−18 to 26)
Abbreviation: ND, neck dissection.
procedure performed (with or without a concomitant neck dis-
section), preoperative and postoperative calcium levels, symp- Results
tomatic hypocalcemia, intravenous calcium repletion, length
of hospital stay, and readmissions or emergency department vis- Demographics
its that were related to hypocalcemia. Patients who under- Between January 1, 2008, and December 31, 2011, 65 patients
went a subtotal thyroidectomy or completion thyroidectomy (mean [SD] age, 49.7 [16.7] years) underwent total thyroidec-
were excluded. During the postoperative hospitalization, se- tomy performed by the senior author and met inclusion cri-
rum calcium levels were checked every 12 hours. All patients teria for analysis. Of those, 33 patients received preoperative
received the same postoperative regimen of oral calcium and and postoperative calcium and calcitriol supplementation and
calcitriol supplementation. Intravenous calcium was given if se- 32 patients received only postoperative therapy. In the preop-
rum calcium levels dropped below 7.5 mg/dL or if the patient erative supplementation group, 22 of 33 patients (67%) were
developed symptoms of hypocalcemia (perioral numbness and women; in the group not receiving preoperative supplemen-
tingling, paresthesias, cramps or spasms of the hands and feet, tation 16 of 32 (50%) were women for a difference in sex be-
and/or the Chvostek sign) in the setting of serum calcium lev- tween the 2 treatment groups of 17% (95% CI, −7% to 38%). A
els lower than 8.0 mg/dL. similar number of patients in each group underwent thyroid-
Primary outcome measures were postoperative calcium ectomy for cancer: 29 of 33 (88%) of the preoperative supple-
levels and the development of postoperative hypocalcemia (cal- mentation group and 26 of 32 (81%) of those not receiving
cium levels <8.0 mg/dL). Secondary outcome measures were supplementation.
development of symptomatic hypocalcemia (calcium level In the group receiving preoperative supplementation, 15
<8 mg/dL with symptoms), length of hospital stay, and re- of 33 patients (45%) underwent central compartment neck dis-
quirements for intravenous calcium. section and 11 of 33 (33%) underwent lateral neck dissection.
An analysis of hospital and pharmacy charges was per- Of those without preoperative supplementation, 16 of 32 (50%)
formed for patients in both groups using the mean number of and 12 of 32 (38%) patients had central compartment and lat-
days each patient spent in the hospital postoperatively ($3042 eral neck dissections, respectively. There was no statistically
per day) and mean number of intravenous calcium gluconate significant difference in the demographic data between the 2
doses required ($121 per 2-g dose). For patients receiving pre- groups (Table 1).
operative calcitriol and calcium supplementation, the charges
for 5 days of calcitriol ($1.20 per 0.25-μg tablet; dosage 0.5 μg Biochemical Calcium Status
twice daily) and 5 days of oral calcium carbonate ($0.12 per Serum calcium levels were measured and recorded preopera-
500-mg tablet; dosage 1500 mg 3 times daily) were calcu- tively and again at 12 and 24 hours postoperatively. The mean
lated. These charges were then summed to determine the mean measured serum calcium level in patients without preopera-
total difference in charges per patient. tive supplementation vs those with preoperative supplemen-
tation were as follows: preoperative, 9.6 vs 9.4 mg/dL (abso-
Statistical Analysis lute difference, 0.16; 95% CI, −0.12 to 0.49); 12 hours
The frequency of hypocalcemia is presented as the number and postoperative, 8.3 vs 8.6 mg/dL (absolute difference, −0.30;
percentage of patients in each group who experienced that 95% CI, −0.63 to 0.02); and 24 hours postoperative, 8.4 vs 8.5
complication. The length of hospital stay is presented as the mg/dL (absolute difference, −0.13; 95% CI, −0.43 to 0.16)
mean (SD). Calcium levels in each group are presented as the (Figure 1). The decrease in serum calcium levels from base-
mean preoperatively and at approximately 12 and 24 hours line to 12 hours postoperative was significantly greater in the
postoperatively. Group differences were analyzed using the χ2 group that received postoperative supplementation only (ab-
test. Statistical analysis was performed with SPSS, version 20.0 solute difference, −0.36 mg/dL; 95% CI, −0.6 to −0.05)
(IBM Corp), using 2-tailed, paired and unpaired t tests and the (Figure 2). At 24 hours postoperatively, 5 of 33 (15%) patients
Fisher exact test, where indicated. in the preoperative supplementation group had serum cal-
jamaotolaryngology.com (Reprinted) JAMA Otolaryngology–Head & Neck Surgery July 2017 Volume 143, Number 7 681
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Research Original Investigation Preoperative Calcium and Calcitriol and Hypocalcemia After Thyroidectomy
Figure 1. Preoperative, 12-Hour Postoperative, and 24-Hour Figure 2. Change in Serum Calcium Levels From Baseline
Postoperative Serum Calcium Levels
10.0
12 Without preoperative
supplementation
9.5
With preoperative
11 supplementation
Calcium Level, mg/dL
9.0
10
Calcium, mg/dL
8.5
9
Without preoperative
supplementation
8 8.0
With preoperative
supplementation
7
7.5
Preoperative 12-h Postoperative
6
Preoperative 12 24 To convert calcium levels to millimoles per liter, multiply by 0.25.
Time, h
To convert calcium levels to millimoles per liter, multiply by 0.25. The bar within
patient not receiving preoperative supplementation (mean
the quartile boxes represents the median value; error bars indicate 95% CIs; hospital stay, 3.8 [1.8] days) was $11 503. Both groups
dots indicate outliers. received similar routine postoperative oral calcium and cal-
citriol supplementation, so these charges were not calcu-
cium levels below 8.0 mg/dL vs 10 of 32 (31%) patients who lated in the analysis. Thus, preoperative supplementation
did not receive preoperative supplementation for an absolute resulted in an estimated $2819 savings in charges per patient
difference between the 2 groups of 16% (95% CI, −4% to 35%) undergoing total thyroidectomy (Table 3).
(Table 2).
Complications of Treatment
Clinical Calcium Status No patient in either group experienced symptoms of hyper-
During their postoperative course, 2 of 33 (6%) of the preop- calcemia. No patients experienced adverse effects of cal-
erative supplementation group became symptomatically hy- citriol and/or calcium supplementation. All patients reported
pocalcemic, compared with 5 of 32 (16%) in the group with- adherence to prescribed dosing and none reported adverse
out preoperative supplementation for an absolute difference symptoms.
of 9.6% (95% CI, −6.6% to 26.3%). No patients receiving pre-
operative supplementation were readmitted to the hospital or
visited the emergency department. In the group without pre-
operative supplementation, 3 of 32 (9%) patients required re-
Discussion
admission or were seen in the emergency department for symp- Transient hypocalcemia is a common complication follow-
toms of hypocalcemia (absolute difference, 9%; 95% CI, −3% ing total thyroidectomy, occurring in up to one-half of
to 24%). Those who received preoperative supplementation patients, 3,5 and serum calcium levels reach their nadir
had a mean postoperative hospital stay of 2.9 (1.4) days, which approximately 24 hours postoperatively. Calcitriol increases
was significantly shorter by 0.9 days compared with those with- calcium absorption by promoting expression of calcium-
out preoperative supplementation who stayed a mean of 3.8 binding protein in intestinal cells, thus increasing intestinal
(1.8) days (95% CI, 0.11 to 1.70) (Table 2). calcium transport across the mucosa into the blood.7 This
effect on calcium absorption requires several days. There-
Hospital/Pharmacy Charge Analysis fore, preoperative supplementation in patients undergoing
Preoperative supplementation with calcium and calcitriol thyroidectomy with calcitriol would be expected to increase
resulted in charges of $29 per patient, based on the dosage of the efficacy of routine calcium supplementation in the
1500 mg of oral calcium carbonate 3 times daily and 0.5 μg immediate postoperative period, thereby mitigating the
of calcitriol twice daily starting 5 days before surgery. The extent of transient hypocalcemia.
group receiving preoperative supplementation required a The aim of this study was to examine the effect of 5 days
total of 10 doses of intravenous calcium gluconate, which of preoperative supplementation with calcium and calcitriol
resulted in a mean charge of $37 (83) per patient. The group on the incidence of postthyroidectomy hypocalcemia. In this
without supplementation required a total of 37 doses of study, patients in the preoperative supplementation group re-
intravenous calcium, with a mean charge of $140 (246) per ceived a straightforward regimen of calcium and calcitriol for
patient. Assuming a hospital charge of $3042 per day, the 5 days immediately prior to surgery. The short time-frame al-
mean charge for the hospital stay per patient receiving pre- lows preoperative supplementation to be accomplished with-
operative supplementation (mean hospital stay, 2.9 [1.4] out unduly delaying definitive surgical treatment of the un-
days) was $8757. The mean charge of the hospital stay per derlying thyroid disorder. The low pharmacy charge of
682 JAMA Otolaryngology–Head & Neck Surgery July 2017 Volume 143, Number 7 (Reprinted) jamaotolaryngology.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Preoperative Calcium and Calcitriol and Hypocalcemia After Thyroidectomy Original Investigation Research
Table 2. Results
No. (%)
Characteristic No Preoperative Supplement Preoperative Supplement Effect Size % (95% CI)
Biochemical
Calcium level <8.0 at 24 h 10 of 32 (31) 5 of 33 (15) 16 (−4.5 to 35.4)
Clinically symptomatic 5 of 32 (16) 2 of 33 (6) 9.6 (−6.6 to 26.3)
IV calcium repletion Abbreviations: ED, emergency
Required 11 of 32 (34) 7 of 33 (21) 13.2 (−8.5 to 33.4) department; IV, intravenous.
No. of dosesa 37 10 SI conversion factor: To convert
calcium to millimoles per liter,
Readmissions/ED visits 3 of 32 (9) 0 of 33 9.4 (−2.7 to 24.2)
multiply by 0.25.
Length of stay, mean (SD), d 3.8 (1.8) 2.9 -0.90 (-1.70,-0.11) a
Effect size, 27 doses.
Table 3. Hospital/Pharmacy Charge Analysis
Charges per Patient, Mean (SD), $
Characteristic No Preoperative Supplement Preoperative Supplement Difference (95% CI)
IV calcium repletion 139.91 (246.08) 36.67 (82.76) 103.24 (12.80 to 193.68)
Length of stay 11 502.56 (5394.00) 8757.27 (4352.66) 2745.29 (319.49 to 5171.09)
Preoperative supplementation 0 29.40 (0) −29.40 (−29.40)
Total 11 642.47 (5512.97) 8823.34 (4388.22) 2819.13 (353.31 to 5284.95)
Abbreviation: IV, intravenous.
supplementation ($29 per patient), twice-daily dosing, and ab- As a result, the patient population in this study may be at
sence of reported adverse effects in this study can encourage greater risk of postoperative hypocalcemia and receive greater
adherence to the treatment. benefit from preoperative supplementation compared with a
This study demonstrated a significant decrease in post- more typical patient population. Second, patients were not ran-
operative hospital stay for patients receiving preoperative domized to their respective treatment groups and preopera-
supplementation (2.9 days) compared with those who did not tive supplementation was provided at the discretion of the sur-
(3.8 days)—a mean decrease of nearly 1 full day. Although se- geon. Although the surgeon did not use preoperative laboratory
rum calcium levels in both groups decreased from baseline lev- results or the planned extent of surgery to decide to prescribe
els postoperatively, the decrease was 0.36 mg/dL greater in pa- preoperative supplementation, because the study was not de-
tients who did not receive preoperative supplementation, signed as a randomized trial, there may have been a selection
which was statistically and clinically significant. These data bias with patients presumed to be at greater risk of postopera-
also demonstrate a decreased incidence of both biochemical tive hypocalcemia receiving preoperative supplementation.
and clinical hypocalcemia, need for intravenous calcium reple- This bias would result in a diminished observed effect of pre-
tion, and hospital readmissions with the upper bound of the operative supplementation. Presumably the selection bias was
95% CI consistent with as much as a 35%, 26%, 33%, and 24% minimal since the patient characteristics (cancer incidence and
reduction, respectively, in each of these factors associated with extent of surgery) of the 2 groups were similar. Nonetheless,
preoperative supplementation. These differences translated future studies would benefit from randomized analysis. Third,
into significant savings in charges for the preoperative supple- vitamin D levels were not routinely measured preopera-
mentation group. Based on these results, preoperative supple- tively. Because patients with low vitamin D levels are more
mentation, in addition to routine postoperative supplemen- likely to develop postoperative hypocalcemia, a preponder-
tation, should be considered for patients undergoing total ance of these patients in either group would be expected to
thyroidectomy. affect the results. Finally, to more precisely quantify the im-
pact of preoperative supplementation, future studies may ben-
Limitations efit from an increased sample size.
This study contains limitations. First, the patient population
may not be representative of a typical thyroidectomy prac-
tice. This is demonstrated by the high percentage of study pa-
tients undergoing thyroidectomy for cancer (85%) and under-
Conclusions
going a complete central compartment neck dissection (46%) Preoperative calcium and calcitriol supplementation
and/or lateral neck dissection (35%) in addition to total thy- resulted in increased postoperative serum calcium levels,
roidectomy. The incidence of temporary hypocalcemia has lower postoperative intravenous calcium repletion require-
been shown to be much higher in patients with a diagnosis of ment, and less symptomatic hypocalcemia in this cohort of
cancer undergoing central compartment neck dissections or patients undergoing total thyroidectomy. Direct patient ben-
lateral neck dissections at the time of total thyroidectomy.17,18 efits include fewer symptoms, significantly decreased length
jamaotolaryngology.com (Reprinted) JAMA Otolaryngology–Head & Neck Surgery July 2017 Volume 143, Number 7 683
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Research Original Investigation Preoperative Calcium and Calcitriol and Hypocalcemia After Thyroidectomy
of hospital stay, decreased hospital readmissions, and associated with postthyroidectomy hypocalcemia, this study
decreased charges. Benefits to society include reduction in supports the use of preoperative supplementation in addi-
health care costs. Weighing the safety of a short course of tion to postoperative supplementation for patients undergo-
calcium and calcitriol supplementation against the risks ing total thyroidectomy.
ARTICLE INFORMATION 3. Testa A, Fant V, De Rosa A, et al. Calcitriol plus calcium and vitamin D supplements in patients with
Accepted for Publication: December 24, 2016. hydrochlorothiazide prevents transient differentiated papillary thyroid carcinoma
post-thyroidectomy hypocalcemia. Horm Metab Res. undergoing total thyroidectomy plus central neck
Published Online: April 13, 2017. 2006;38(12):821-826. dissection. Cancer. 2009;115(2):251-258.
doi:10.1001/jamaoto.2016.4796
4. Mehanna HM, Jain A, Randeva H, Watkinson J, 12. Sanabria A, Dominguez LC, Vega V, Osorio C,
Author Contributions: Drs Maxwell and Shonka Shaha A. Postoperative hypocalcemia—the Duarte D. Routine postoperative administration of
contributed equally to the study, had full access to difference a definition makes. Head Neck. 2010;32 vitamin D and calcium after total thyroidectomy:
all the data in the study, and take responsibility for (3):279-283. a meta-analysis. Int J Surg. 2011;9(1):46-51.
the integrity of the data and the accuracy of the
data analysis. 5. Reeve T, Thompson NW. Complications of 13. Tartaglia F, Giuliani A, Sgueglia M, Biancari F,
Study concept and design: Shonka, Levine. thyroid surgery: how to avoid them, how to manage Juvonen T, Campana FP. Randomized study on oral
Acquisition, analysis, or interpretation of data: them, and observations on their possible effect on administration of calcitriol to prevent symptomatic
Maxwell, Shonka, Robinson. the whole patient. World J Surg. 2000;24(8):971-975. hypocalcemia after total thyroidectomy. Am J Surg.
Drafting of the manuscript: Maxwell, Shonka. 6. Jacobs JK, Aland JW Jr, Ballinger JF. Total 2005;190(3):424-429.
Critical revision of the manuscript for important thyroidectomy: a review of 213 patients. Ann Surg. 14. Bellantone R, Lombardi CP, Raffaelli M, et al.
intellectual content: Shonka, Robinson, Levine. 1983;197(5):542-549. Is routine supplementation therapy (calcium and
Statistical analysis: Maxwell, Shonka, Robinson. 7. Bringhurst FR, Demay MB, Krane SM, vitamin D) useful after total thyroidectomy? Surgery.
Supervision: Shonka, Levine. Kronenberg HM. Bone and mineral metabolism in 2002;132(6):1109-1112.
Conflict of Interest Disclosures: All authors have health and disease. In: Longo DL, Fauci AS, Kasper 15. Bordelon P, Ghetu MV, Langan RC. Recognition
completed and submitted the ICMJE Form for DL, Hauser SL, Jameson JL, Loscalzo J, eds. and management of vitamin D deficiency. Am Fam
Disclosure of Potential Conflicts of Interest and Harrison's Principles of Internal Medicine. 18th ed. Physician. 2009;80(8):841-846.
none were reported. New York: McGraw-Hill; 2012. 16. Docimo G, Tolone S, Pasquali D, et al. Role of
Meeting Presentation: This study was presented 8. Kirkby-Bott J, Markogiannakis H, Skandarajah A, pre and post-operative oral calcium and vitamin D
as a poster at the Combined Sections Meeting, Cowan M, Fleming B, Palazzo F. Preoperative supplements in prevention of hypocalcemia after
Triological Society; January 25, 2013; Scottsdale, vitamin D deficiency predicts postoperative total thyroidectomy. G Chir. 2012;33(11-12):374-378.
Arizona. hypocalcemia after total thyroidectomy. World J Surg. 17. Shindo M, Stern A. Total thyroidectomy with
2011;35(2):324-330. and without selective central compartment
REFERENCES 9. Erbil Y, Ozbey NC, Sari S, et al. Determinants of dissection: a comparison of complication rates.
1. Erbil Y, Bozbora A, Ozbey N, et al. Predictive postoperative hypocalcemia in vitamin D–deficient Arch Otolaryngol Head Neck Surg. 2010;136(6):
value of age and serum parathormone and vitamin Graves’ patients after total thyroidectomy. Am J Surg. 584-587.
D3 levels for postoperative hypocalcemia after total 2011;201(5):685-691. 18. Roh JL, Park JY, Park CI. Total thyroidectomy
thyroidectomy for nontoxic multinodular goiter. 10. Erbil Y, Barbaros U, Temel B, et al. The impact of plus neck dissection in differentiated papillary
Arch Surg. 2007;142(12):1182-1187. age, vitamin D3 level, and incidental thyroid carcinoma patients: pattern of nodal
2. Roh JL, Park CI. Routine oral calcium and vitamin parathyroidectomy on postoperative hypocalcemia metastasis, morbidity, recurrence, and
D supplements for prevention of hypocalcemia after total or near total thyroidectomy. Am J Surg. postoperative levels of serum parathyroid
after total thyroidectomy. Am J Surg. 2006;192(5): 2009;197(4):439-446. hormone. Ann Surg. 2007;245(4):604-610.
675-678. 11. Roh JL, Park JY, Park CI. Prevention of
postoperative hypocalcemia with routine oral
684 JAMA Otolaryngology–Head & Neck Surgery July 2017 Volume 143, Number 7 (Reprinted) jamaotolaryngology.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: on 01/22/2019
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Pathogenesis and Management of Hepatolithiasis: A Report of Two CasesДокумент3 страницыPathogenesis and Management of Hepatolithiasis: A Report of Two CasesBenny KurniawanОценок пока нет
- Risk Factors, Complications and Outcome of Cholelithiasis in Children: A Retrospective, Single-Centre ReviewДокумент6 страницRisk Factors, Complications and Outcome of Cholelithiasis in Children: A Retrospective, Single-Centre ReviewBenny KurniawanОценок пока нет
- Comparison of Laparoscopic Versus Open Left Hemihepatectomy For Left-Sided HepatolithiasisДокумент7 страницComparison of Laparoscopic Versus Open Left Hemihepatectomy For Left-Sided HepatolithiasisBenny KurniawanОценок пока нет
- Body Mass Index, Abdominal Fatness and The Risk of Gallbladder DiseaseДокумент11 страницBody Mass Index, Abdominal Fatness and The Risk of Gallbladder DiseaseBenny KurniawanОценок пока нет
- Spontaneous Passage of Bile Duct Stones: Frequency of Occurrence and Relation To Clinical PresentationДокумент4 страницыSpontaneous Passage of Bile Duct Stones: Frequency of Occurrence and Relation To Clinical PresentationBenny KurniawanОценок пока нет
- Babaian 2001Документ4 страницыBabaian 2001Benny KurniawanОценок пока нет
- Head and Neck Surgery: Pressure Ulcer Prevention Strategies in Prolonged SurgeryДокумент2 страницыHead and Neck Surgery: Pressure Ulcer Prevention Strategies in Prolonged SurgeryBenny KurniawanОценок пока нет
- Spinning Protons Presents: The Basics of MRI: T1 vs. T2Документ26 страницSpinning Protons Presents: The Basics of MRI: T1 vs. T2Benny KurniawanОценок пока нет
- DhirendraДокумент3 страницыDhirendraBenny KurniawanОценок пока нет
- Cover LetterДокумент3 страницыCover LetterBenny KurniawanОценок пока нет
- Hydrosefalus: Benny Nanda Kurniawan Oktatika PratiwiДокумент22 страницыHydrosefalus: Benny Nanda Kurniawan Oktatika PratiwiBenny KurniawanОценок пока нет
- Aromatase InhibitorДокумент10 страницAromatase InhibitorBenny KurniawanОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Review of Antibacterial Medicines For The Treatment of Enteric Fever For The WHO Model List of Essential Medicines 2019 UpdateДокумент19 страницReview of Antibacterial Medicines For The Treatment of Enteric Fever For The WHO Model List of Essential Medicines 2019 UpdateSundas EjazОценок пока нет
- Multimorbidity and Its Associated Risk Factors Among Adults in Northern Sudan: A Community-Based Cross-Sectional StudyДокумент7 страницMultimorbidity and Its Associated Risk Factors Among Adults in Northern Sudan: A Community-Based Cross-Sectional StudyOwais SaeedОценок пока нет
- Irda Non Payable ListДокумент21 страницаIrda Non Payable ListMUKESH SINGHОценок пока нет
- Dental EssayДокумент3 страницыDental Essayvaleriana calaniОценок пока нет
- Diabetes Home Health RubricДокумент13 страницDiabetes Home Health Rubricapi-372924050Оценок пока нет
- Midwifery KitДокумент3 страницыMidwifery KitRitzel CreusОценок пока нет
- National Health AccountsДокумент4 страницыNational Health AccountsMyat MinОценок пока нет
- 5th ReflectionДокумент2 страницы5th Reflectionapi-478150357Оценок пока нет
- Engel 1980 The Clinical Application of of The Biopsychosocial Model PDFДокумент10 страницEngel 1980 The Clinical Application of of The Biopsychosocial Model PDFDiego Almanza HolguinОценок пока нет
- Congenital Adrenal HyperplasiaДокумент30 страницCongenital Adrenal HyperplasiaIrene Jordan100% (1)
- Conversion DisorderДокумент27 страницConversion DisorderKhalil Ullah100% (1)
- Case 1 - Pneumonia (Final)Документ4 страницыCase 1 - Pneumonia (Final)Joegie ArioОценок пока нет
- EclampsiaДокумент14 страницEclampsiaUmi PulunganОценок пока нет
- Form 2 Reporting Form Revision 1Документ1 страницаForm 2 Reporting Form Revision 1Cha Tuban DianaОценок пока нет
- Lemos 2016Документ32 страницыLemos 2016wendyjemmy8gmailcomОценок пока нет
- DrugДокумент13 страницDrugkhesler BacallaОценок пока нет
- SRM Case Studys C05-007Документ8 страницSRM Case Studys C05-007Aqfaq UdeenОценок пока нет
- Institute of Nursing: Far Eastern UniversityДокумент3 страницыInstitute of Nursing: Far Eastern UniversityaleccespirituОценок пока нет
- Selective Awareness TherapyДокумент10 страницSelective Awareness TherapyHashem Al AttasОценок пока нет
- Surgery Songbook CompressedДокумент69 страницSurgery Songbook CompressedBrandon HayashiОценок пока нет
- LA Union: PDRRM OДокумент32 страницыLA Union: PDRRM OEnash RidОценок пока нет
- LDN Information PackДокумент17 страницLDN Information PackkindheartedОценок пока нет
- Ferraris M La HermeneuticaДокумент310 страницFerraris M La HermeneuticaantoniomarkusОценок пока нет
- Contagious Bovine PyelonephritisДокумент26 страницContagious Bovine PyelonephritisMuhammad Hamza AlviОценок пока нет
- Anna Giuliani - Assisted Peritoneal Dialysis - Ren Replace Ther 2022Документ7 страницAnna Giuliani - Assisted Peritoneal Dialysis - Ren Replace Ther 2022francescoОценок пока нет
- Artsanto R, Doso Sutiyono, Witjaksono : Bagian Anestesiologi Dan Terapi Intensif FK Undip/ RSUP Dr. Kariadi, SemarangДокумент12 страницArtsanto R, Doso Sutiyono, Witjaksono : Bagian Anestesiologi Dan Terapi Intensif FK Undip/ RSUP Dr. Kariadi, SemarangAdhyОценок пока нет
- Sush Unity Corrected EMERGENCY1700Документ76 страницSush Unity Corrected EMERGENCY1700Dr-Jahanzaib GondalОценок пока нет
- Albuterol, Accuneb Drug CardДокумент2 страницыAlbuterol, Accuneb Drug Carddnw876Оценок пока нет
- Quantum Techniques Client ManualДокумент42 страницыQuantum Techniques Client ManualVeres Beatrix100% (4)
- Paper-Organ DonationДокумент7 страницPaper-Organ Donationapi-400417633Оценок пока нет