Академический Документы
Профессиональный Документы
Культура Документы
Progressive Multiple Sclerosiss
Загружено:
Muhammad Imam NoorАвторское право
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документProgressive Multiple Sclerosiss
Загружено:
Muhammad Imam NoorSeries
Multiple sclerosis 3
Progressive multiple sclerosis: prospects for disease therapy,
repair, and restoration of function
Daniel Ontaneda, Alan J Thompson, Robert J Fox, Jeffrey A Cohen
Multiple sclerosis is a major cause of neurological disability, which accrues predominantly during progressive forms of Lancet 2017; 389: 1357–66
the disease. Although development of multifocal inflammatory lesions is the underlying pathological process in Published Online
relapsing-remitting multiple sclerosis, the gradual accumulation of disability that characterises progressive multiple November 23, 2016
http://dx.doi.org/10.1016/
sclerosis seems to result more from diffuse immune mechanisms and neurodegeneration. As a result, the 14 anti-
S0140-6736(16)31320-4
inflammatory drugs that have regulatory approval for treatment of relapsing-remitting multiple sclerosis have little or
This is the third in a Series of
no efficacy in progressive multiple sclerosis without inflammatory lesion activity. Effective therapies for progressive three papers about multiple
multiple sclerosis that prevent worsening, reverse damage, and restore function are a major unmet need. In this Series sclerosis
paper we summarise the current status of therapy for progressive multiple sclerosis and outline prospects for Mellen Center for Multiple
the future. Sclerosis Treatment and
Research, Neurological
Institute, Cleveland Clinic,
Introduction exhibit gradually worsening disability, most often motor Cleveland, OH, USA
Multiple sclerosis is a chronic immune-mediated disease impairment with a pattern suggesting a myelopathy, but (D Ontaneda MD,
of the CNS. The global prevalence of multiple sclerosis also progressive hemiparesis, ataxia, visual dysfunction, Prof R J Fox MD,
Prof J A Cohen MD); and
was estimated to be 2·3 million people in 2013,1 an or cognitive impairment. Although the onset of
Department of Brain Repair
increase of 0·2 million from 5 years earlier. This progression most often occurs at age 40–50 years in both and Rehabilitation, University
prevalence is likely an underestimate and does not fully groups, secondary progressive multiple sclerosis follows College London, Institute of
account for the number of patients with multiple an initial relapsing-remitting multiple sclerosis phase Neurology, Faculty of Brain
Sciences, London, UK
sclerosis in large Asian countries. About 15% of patients typically lasting 10–15 years. Primary progressive multiple
(Prof A J Thompson MD)
begin with a progressive disease course from onset, sclerosis has an equal sex ratio, whereas secondary
Correspondence to:
termed primary progressive multiple sclerosis, and about progressive multiple sclerosis affects women more Dr Jeffrey A Cohen, Mellen Center
70% develop progression 10–15 years after an initial frequently than men. A small proportion of patients with for Multiple Sclerosis Treatment
relapsing-remitting course, termed secondary pro radiologically isolated syndrome (MRI findings typical of and Research, Neurological
multiple sclerosis without clinical manifestations) have Institute, Cleveland Clinic,
gressive multiple sclerosis. Thus, at least 1·3 million
Cleveland, OH 44195, USA
people have progressive multiple sclerosis. clinical conversion manifested as gradual progression of cohenj@ccf.org
Disability in multiple sclerosis accrues predominantly disability.4 The proportion with progression as the initial
in the progressive forms of the disease, creating a clinical manifestation, as well as demographics, sex ratio,
substantial health-care burden at individual, family, and clinical characteristics, and frequency of spinal cord
community levels. Although great progress has been lesions in these patients, are similar to those of primary
made in the treatment of relapsing-remitting multiple progressive multiple sclerosis. At present the consensus
sclerosis (14 drugs have regulatory approval), is that primary progressive multiple sclerosis is
development of therapies that prevent or reverse biologically part of the multiple sclerosis spectrum, and
progression has been slower. International efforts such that clinical, imaging, and pathological differences
as the International Progressive MS Alliance are between primary and secondary progressive multiple For the International Progressive
increasing the focus on progressive multiple sclerosis sclerosis are more relative than absolute. Therefore, in MS Alliance see http:\\www.
progressivemsalliance.org
and identifying specific research areas to target.2 In this, much of this Series paper, primary and secondary
the third paper in a Series about multiple sclerosis, we progressive multiple sclerosis will be discussed together
summarise the current status of therapy for progressive as progressive multiple sclerosis.
multiple sclerosis and outline prospects for the future.
Pathogenesis of progressive multiple sclerosis Search strategy and selection criteria
The pathogenic mechanisms underlying progression are This paper is based on the cumulative literature archives of
incompletely understood. Moreover, since the division the authors. Additionally, we searched PubMed for articles
25 years ago of what previously was called chronic published in English up to April 1, 2016, with the search terms
progressive multiple sclerosis into primary progressive “multiple sclerosis”, “epidemiology”, “pathology”,
multiple sclerosis and secondary progressive multiple “inflammation”, “neurodegeneration”, “demyelination”,
sclerosis, there have been questions about whether they “remyelination”, “outcome measures”, “magnetic resonance
represent overlapping or distinct entities.3 Patients with imaging”, “clinical trial”, “stem cell”, and “rehabilitation”.
primary and secondary progressive multiple sclerosis
www.thelancet.com Vol 389 April 1, 2017 1357
Series
IV).8 Cortical histopathology includes microglial
Mitochondrial dysfunction Chronic axonal demyelination
• Impaired mitochondrial transport • Loss of trophic support for axon
activation, demyelination, neuritic transection, neuronal
• Mitochondrial DNA mutations • Loss of saltatory conduction death, and reduced presynaptic terminals, but tends not
• Susceptibility to ROS • Loss of myelin insulation to include perivascular lymphocytic cuffs typical of white
• Increased production of ROS ↑ Exposure to inflammatory mediators
• Amplification of oxidative injury ↑ Exposure to ROS matter lesions.8 Subpial lesions can be associated with
Increased expression
• Histotoxic hypoxia
Reversed operation of of sodium channels meningeal infiltrates of T and B lymphocytes, plasma
ROS
the Na –Ca exchanger
+ 2+
cells, and macrophages,6 which in some cases of
Damaged ROS Energetic secondary progressive multiple sclerosis form structures
mitochondrion ROS Ca2+ failure
Fe Na+ Na+ resembling lymphoid follicles.9 The severity of cortical
K+
Fe
ROS
Na+ ATP
demyelination correlates with the extent of meningeal
Na+ inflammation in progressive multiple sclerosis, suggesting
Na+ Na
+
Ca overload
2+ Fe
a pathogenic role.10
Fe ROS
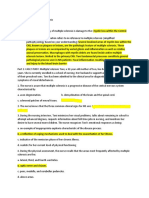
Myelin Axon Several potential mechanisms are hypothesised to lead
Proteases Lipases NOS to neurodegeneration in progressive multiple sclerosis
(figure 1),11 many of which are potential therapeutic
Lesion formation
targets. Demyelinated axons are abundant in long-
ROS Neuron Antegrade/retrograde degeneration standing multiple sclerosis and are hypothesised to be
susceptible to chronic injury.6 In addition to loss of
myelin’s structural and trophic support, chronic
Oxidative injury
Inflammation demyelination might permit increased exposure to toxic
B lymphocytes
species in the micro-environment such as inflammatory
mediators, and reactive oxygen and iron species. In
some demyelinated axons, saltatory nerve-impulse
T lymphocytes
conduction is replaced by continuous conduction, which
restores function but increases energy demand and
Microglia sodium accumulation in the axonal cytoplasm. Resultant
ROS Oligodendrocyte reverse operation of sodium–calcium exchanger to
Fe restore ionic gradients could lead to cytoplasmic calcium
accumulation, activation of calpains, and proteolysis of
cytoskeleton.
Although remyelination can be seen in some lesions,
the failure of remyelination in other areas is postulated
Figure 1: Pathogenesis of neurodegeneration in progressive multiple sclerosis
to cause axonal degeneration and disease progression.
ROS=reactive oxygen species. Fe=iron. NOS=nitric oxide synthase. Thus, remyelination is a potential therapeutic goal. The
abundance of oligodendrocyte precursors in some
The pathological mechanisms that cause tissue damage chronic lesions suggests that scarcity of such cells
in relapsing-remitting multiple sclerosis and progressive does not explain failure of remyelination.12 Rather,
multiple sclerosis overlap, but differ quantitatively. In the the absence of factors necessary for successful
early stages, pathology is dominated by focal inflammatory remyelination or the presence of inhibitory factors is
lesions with perivenular accumulation of T and B more likely to be responsible. This concept has
lymphocytes, blood–brain barrier disruption, demye- important implications for potential repair-promoting
lination, and acute axonal transection.5 Although focal strategies.
lesions sometimes develop in progressive multiple Axonal injury also is a major contributor to irreversible
sclerosis, new lesion activity becomes less frequent over disability. Injury is believed to occur through a
time. By contrast, diffuse pathology in grossly normal combination of acute inflammatory damage,
appearing white and grey matter with microglial activation degeneration of chronically demyelinated axons in
and neurodegeneration are more prominent.6 These white and grey matter, and antegrade and retrograde
features are found in early multiple sclerosis as well, but trans-synaptic degeneration due to distal axonal
increase with age and disease duration. transection.13 Mitochondrial dysfunction in axons seems
The clinical importance of grey matter pathology to result from impaired mitochondrial transport,
involving cortex, deep structures, cerebellum, and spinal susceptibility to oxidative injury, and mutations in
cord is increasingly recognised in progressive multiple mitochondrial DNA, all of which lead to impaired
sclerosis.7 Several types of cortical lesions have been energy production and generation of reactive oxygen
distinguished: leukocortical (subcortical lesions affecting species. The net effect of these processes is accumulation
adjacent white and grey matter), intracortical, and of various toxic species, increased cellular energy
subpial (spanning long distances in the subpial ribbon demand, failure of energy production, and virtual
and extending from the surface to cortical layers II or hypoxia resulting in neurodegeneration.
1358 www.thelancet.com Vol 389 April 1, 2017
Series
Active (clinical) with Active (MRI/clinical) without Active (MRI) with progression Not active with progression Not active without progression
progression progression
Secondary progressive MS Primary progressive MS MRI activity—new or enhancing lesions
Figure 2: Categorisation of patients with progressive MS
MS=multiple sclerosis.
Revised classification of multiple sclerosis neurological functions, permitting comparison between
phenotype individuals or groups on a 0–10 scale. Despite limitations,
Increasing recognition that relapses and MRI-identified the EDSS is likely to continue to be used as a measure of
lesion activity occur in some patients with progressive multiple sclerosis-related disability. An alternative
multiple sclerosis (mainly in the early stages) led to approach, the Multiple Sclerosis Functional Composite
recent revision of the phenotypic categories of progressive (MSFC), uses quantitative neuroperformance tests
multiple sclerosis (figure 2).14 The new scheme still covering four neurological domains: timed 25-Foot Walk
differentiates progression at disease onset (primary (T25FW; short-distance walking speed), Nine-Hole Peg
progressive multiple sclerosis) from progression after an Test (9HPT; upper-extremity function), Sloan Low-
initial relapsing-remitting course (secondary progressive Contrast Letter Acuity (SLCLA; vision), and Paced
multiple sclerosis), but adds two qualifiers: presence or Auditory Serial Addition Test or Symbol Digit Modalities
absence of clinical relapses or new MRI lesions (active or Test (PASAT or SDMT; cognitive processing speed and
not active, respectively), and presence or absence of sustained attention). Anticipated advantages of the MSFC
gradual worsening disability independent of relapses compared with the EDSS are ease of administration,
(with progression or without progression, respectively). more meaningful contribution from several neurological
These qualifiers are intended to be reassessed over domains, improved reliability, and greater sensitivity in
time (eg, every year), with patients potentially changing some populations. The Multiple Sclerosis Outcome
category based on recent disease course. Assessments Consortium comprising multiple sclerosis
The new classification will have noteworthy benefits clinical researchers from academia and industry is
in recognising two relatively separate facets of pro- working to develop the MSFC approach further and
gressive multiple sclerosis—ie, inflammatory lesion obtain formal regulatory qualification for use in multiple
activity and gradual progression. The classification will sclerosis trials.16 The INFORMS trial of fingolimod in
be especially helpful for selection of clinical trial primary progressive multiple sclerosis17 used a composite
participants. The presence of recent relapses or active outcome measure combining EDSS, T25FW, and 9HPT.
MRI lesions is an important determinant of efficacy of Although the trial did not show efficacy, the composite
drugs with predominantly anti-inflammatory effects. It endpoint detected events in 69% of participants, more
is hoped that phenotypic classification will incorporate than its components.
additional imaging and non-imaging biomarkers, Several automated measurement devices to capture
genetic markers, and epigenetic factors to categorise function in multiple sclerosis are under development. The
patients more comprehensively. Multiple Sclerosis Performance Test is a battery of
quantitative neuroperformance assessments modelled
Clinical measures of disability after the MSFC designed for supervised or self-admin-
Clinical outcome measures must take into account istration using a suite of iPad apps.18 Several smartphone
heterogeneous clinical manifestations, unpredictable and wearable motion sensors have been developed, which
course, and the generally slow rate of worsening in provide the ability to measure community-based
progressive multiple sclerosis. The current measures ambulation and physical activity. How such data can be
address these issues in different ways.15 The Kurtzke used to assess therapies in clinical trials or to make
Expanded Disability Status Scale (EDSS) is based on therapeutic decisions in practice is unclear at present.
neurological examination and assesses a range of Nevertheless, it is expected that multiple sclerosis disability
www.thelancet.com Vol 389 April 1, 2017 1359
Series
assessment will undergo further refinement to include more diffuse (presumably due to damage to afferent or
various performance measures. Methods to capture large efferent connections).29,30 Similar to whole-brain atrophy
segments of data using the electronic medical record will measures, regional atrophy measures need substantial
also expand in the future. image post-processing, making them more suitable for
research studies than for clinical practice.
The role of imaging in progressive multiple
sclerosis Advanced MRI techniques
Standard MRI Several MRI techniques can provide improved pathological
MRI is a key diagnostic method for all forms of multiple specificity and, thus, better correlation with clinical
sclerosis. The greater sensitivity of MRI compared with disability: diffusion tensor imaging (DTI; which quantifies
clinical outcome assessment has made it a standard the 3D diffusion of water),31 magnetisation transfer
approach in the development of anti-inflammatory imaging (which quantifies tissue integrity through the
therapies for relapsing-remitting multiple sclerosis, with interaction of protons bound to molecular structures and
MRI lesion activity used in phase 2 trials to predict free water),32 magnetic resonance spectroscopy (which
benefit on relapses in subsequent phase 3 trials.19 Such a quantifies tissue metabolites),33 and techniques such as
marker is lacking for progressive multiple sclerosis in magnetic resonance fingerprinting.34 These techniques
which lesion activity is less common and disability often can be applied to the whole brain, or selectively to grey or
worsens without lesion accrual. Moreover, because of its white matter lesions or regions that appear normal on
low pathological specificity, standard MRI does not seem standard MRI. All of these techniques show promise, but
to detect the pathological processes that underlie require further validation to determine their pathological
disability progression. Several imaging approaches specificity.
under development show promise to meet this need.
Spinal cord imaging
Brain volume measures Spinal cord atrophy correlates with clinical measures
Whole-brain atrophy, which reflects aggregate tissue of disability.35 Quantitative and more pathologically
injury, is more severe in progressive multiple sclerosis specific MRI measures of the spinal cord are difficult
than in relapsing-remitting multiple sclerosis, even because of low spatial resolution, pulsation artifact,
though the rate of volume loss is relatively constant over cerebrospinal fluid partial-volume averaging, and
the course of the disease.20 Whole-brain atrophy challenges in registration. Nevertheless, assessment of
correlates with physical20 and cognitive21 impairment. the spinal cord using DTI,36 magnetisation transfer
Treatment effects on brain atrophy predict effects on ratio,37 and spectroscopy38 could provide important
disability, at least in relapsing-remitting multiple insights in progressive multiple sclerosis.
sclerosis.22 Methods to measure whole-brain volume are
reasonably established, and published sample size PET and optical coherence tomography
estimates for progressive multiple sclerosis trials based PET markers for activated microglia39 and myelin40 could
on whole-brain atrophy are feasible.23 The main assess disease status in progressive multiple sclerosis.
disadvantage as a phase 2 trial outcome is the rather The main shortcoming of this technique is its limited
slow rate of change, prolonging trial duration. spatial resolution.
Additionally, precise whole-brain volume measurement Optical coherence tomography is a rapid, non-invasive
is technically challenging and subject to substantial technique that provides high-resolution quantification of
biological variability, making it difficult to implement in the retinal nerve fibre layer (the axons that extend to the
clinical practice. optic nerve) and the corresponding neuronal cells bodies
in the ganglion cell layer. These measures directly reflect
Methods to detect grey matter pathology the axonal integrity of the optic nerves and correlate with
Conventional MRI does not detect cortical lesions, an overall clinical disability41 and brain MRI measures.42
important site of multiple sclerosis injury. Specialised
sequences such as double-inversion recovery24 and ultra- Disease therapy for progressive multiple sclerosis
high-field (7 T) MRI25 allow identification of some, but Anti-inflammatory strategies
not all, cortical lesions. Because of the insensitivity of Most drugs approved for relapsing-remitting multiple
current techniques to show cortical pathology directly, sclerosis have been tested in progressive multiple
some studies have measured cortical thickness or volume sclerosis (table). Interferon beta-1 therapies were
to quantify pathology indirectly. Cortical atrophy is evaluated in secondary progressive multiple sclerosis
prominent in progressive multiple sclerosis26 and shortly after their efficacy was shown in relapsing-
correlates with physical27 and cognitive28 impairment. remitting multiple sclerosis. Although two trials were
Atrophy of deep grey structures (thalamus, caudate, and positive,50,51 several others were negative.52–54 Similarly, a
hippocampus) also occurs in progressive multiple phase 3 trial of glatiramer acetate in primary progressive
sclerosis and can be focal (presumably due to lesions) or multiple sclerosis was negative.47 Subsequent analysis
1360 www.thelancet.com Vol 389 April 1, 2017
Series
Population Treatment arms Follow-up Mean age Participants Primary outcome Results
duration of with
population gadolinium-
(years) enhancing
lesions at
baseline (%)
Anti-inflammatory strategies
ASCEND43 Secondary progressive Natalizumab (n=439) 96 weeks 47·2 24% 6 month CDW based on a 4% increase in CDW; OR 0·86 (95% CI
multiple sclerosis and placebo (n=448) composite of EDSS, T25FW, 0·66–1·13), p=0·287
and 9HPT
INFORMS17 Primary progressive Fingolimod (n=336) 3 years 49 13% 3 month CDW based on a 5·05% reduction in CDW; HR 0·95
multiple sclerosis and placebo (n=487) composite of EDSS, T25FW, (95% CI 0·80–1·12), p=0·544
and 9HPT
MAESTRO44 Secondary progressive MPB8298 (n=305) and 2 years 49·9 NA 6 month CDW based on EDSS 2·9% increase in CDW in DR2-positive/
multiple sclerosis placebo (n=307) DR4-positive subgroup (p=0·527);
7·5% reduction in CDW in DR2-negative/
DR4-negative subgroup, (p=0·055)
OLYMPUS45 Primary progressive Rituximab (n=292) and 96 weeks 49·9 24·5% 3 month CDW based on EDSS 8·3% reduction in CDW, HR 0·77, 95% CI
multiple sclerosis placebo (n=147) 0·55–1·09; p=0·144
ORATORIO46 Primary progressive Ocrelizumab (n=488) 120 weeks 44·6 years 26% 3 month CDW based on EDSS 24% reduction in CDW, HR=0·76, 95% CI
multiple sclerosis and placebo (n=244) 0·50–0·98; p=0·03
PROMiSe47 Primary progressive Glatiramer acetate 36 months 50·4 14·1% 3 month CDW based on EDSS HR 0·87, 95% CI 0·71–1·07; p=0·175
multiple sclerosis (n=627) and placebo
(n=316)
Neuroprotective or repair-promoting strategies
CUPID48 Primary and secondary Dronabinol (n=329) 36 months 52·2 NA 6 month CDW based on EDSS, 0·1% reduction in CDW; HR 0·92, 95% CI
progressive multiple and placebo (n=164) change in MSIS-29 PHYS 0·68–1·23, p=0·57
sclerosis
MS-SPI49 Primary and secondary Biotin (n=103) and 12 months 51·4 NA Proportion with disability 12·6% of participants in biotin arm
progressive multiple placebo (n=51) improvement based on EDSS improved compared with 0 in the placebo arm;
sclerosis and T25FW at 9 months p=0·005
confirmed at 12 months
CDW=confirmed disability worsening. EDSS=Expanded Disability Status Scale. T25FW=Timed 25-Foot Walk. 9HPT=Nine-Hole Peg Test. OR=odds ratio. HR=hazard ratio. NA=not applicable.
MSIS-29 PHYS=physical impact subscale of the 29-item Multiple Sclerosis Impact Scale.
Table: Recent phase 3 clinical trials in progressive multiple sclerosis
found that trials enriched with participants with recent worsening of disability measured by a composite
relapses and MRI lesion activity tended to show benefit outcome similar to that used in the trial of fingolimod,
from interferon beta.55 Similar results were seen with although benefit was seen on 9HPT.43 The absence of
other anti-inflammatory therapies in progressive benefit on progression with natalizumab, one of the
multiple sclerosis. more potent anti-inflammatory therapies for relapsing-
Fingolimod reduced relapses, MRI lesion activity, and remitting multiple sclerosis, underscores the importance
brain volume loss in three phase 3 trials in relapsing- of mechanism of action in determining efficacy.
remitting multiple sclerosis.56–58 Fingolimod readily Because of the potent efficacy of anti-CD20 monoclonal
enters the brain and has direct effects on several CNS cell antibodies in relapsing-remitting multiple sclerosis, there
types mediated by sphingosine 1-phosphate receptors, is increased recognition of the multifaceted role of B
suggesting it might be beneficial in progressive multiple lymphocytes in multiple sclerosis pathogenesis beyond
sclerosis.59 A phase 3 trial of fingolimod in primary antibody production.60 In a phase 3 trial of patients with
progressive multiple sclerosis showed reduction in new primary progressive multiple sclerosis, rituximab
MRI lesions, but not the risk of confirmed disability treatment slowed the change in lesion volume relative to
worsening measured by a composite outcome that placebo, but did not decrease the risk of confirmed
included EDSS, T25FW, and 9HPT.17 These results disability progression.45 In planned subgroup analyses,
indicate that entry of a drug into the CNS and direct participants younger than 50 years and those with
actions there do not ensure efficacy in progressive gadolinium-enhancing lesions at baseline showed benefit
multiple sclerosis. on disability progression. Based on those results, a
Another highly effective anti-inflammatory therapy, the humanised anti-B lymphocyte monoclonal antibody,
anti-β1 integrin monoclonal antibody natalizumab, was ocrelizumab, was evaluated in patients with primary
evaluated in a phase 3 trial of patients with secondary progressive multiple sclerosis. This phase 3 trial
progressive multiple sclerosis. Natalizumab did not slow demonstrated that ocrelizumab reduced the risk of
www.thelancet.com Vol 389 April 1, 2017 1361
Series
disability progression by 24%.46 This trial enrolled many essential carboxylases and, in high doses, is
relatively young participants (mean age 44·6 years; hypothesised to enhance cellular energy production
maximum age 55 years), with short disease duration with resultant improved axonal function, decreased
(mean 6·4 years; maximum 15 years), and a relatively neurodegeneration, and enhanced remyelination.65 A
high proportion of participants had gadolinium- placebo-controlled phase 3 trial evaluated whether
enhancing lesions at baseline (26%). The subgroup with high-dose biotin (300 mg/day) improved disability in
gadolinium-enhancing lesions at baseline seemed to have patients with primary and secondary progressive
a greater reduction in risk of disability progression, multiple sclerosis.49 12·6% of treated participants had
although the difference was not significant (hazard ratio improvement in measures of disability, compared with
0·65 [95% CI 0·40–1·06] for those with enhancing lesions none in the placebo group.
vs 0·84 [0·62–1·13] for those without enhancing lesions).61
The different results obtained in trials of progressive Repair-promoting strategies
multiple sclerosis seem not to relate to differences in LINGO-1 is a protein expressed by oligodendrocytes and
anti-inflammatory potency. Instead, the results suggest neurons that inhibits remyelination.66 Treatment of
that trials that enrol a study population with younger patients with acute optic neuritis with the LINGO-1-
age, shorter disease duration, and more ongoing blocking monoclonal antibody BIIB033 did not improve
inflammatory lesion activity tend to show greater benefit. recovery of visual evoked potential latency, a measure of
Conversely, older patients without lesion activity gain optic nerve conduction, in the primary analysis but was
little if any benefit as a group. In addition to study effective in a post-hoc per-protocol analysis.67 Negative
population, mechanism of action might also be relevant, results were recently announced for a phase 2 trial that
although this requires further study. These observations assessed whether BIIB033 improved disability in patients
provide valuable guidance for both the characteristics of with relapsing-remitting or secondary progressive
participants to enrol in future trials and the choice of multiple sclerosis (NCT01864148).68
therapies to study in progressive multiple sclerosis. Cell-based repair-promoting strategies have received
much attention as a potential therapeutic approach for
Neuroprotective therapeutic strategies progressive multiple sclerosis. Oligodendrocyte progenitor
The limited success of anti-inflammatory drugs in cells (OPCs) can be isolated from fetal human brain and,
treatment of progressive multiple sclerosis suggests that when injected intracerebrally into hypomyelinating
other therapeutic approaches, such as neuroprotective or shiverer mice, lead to widespread myelination and reversal
repair-promoting strategies, will be necessary. A phase 2 of the clinical phenotype.69 A phase 1 dose-escalation trial
study assessed the cytoprotective properties of simvastatin is planned to evaluate the feasibility and safety of
in patients with secondary progressive multiple sclerosis.62 intracerebral injections of these cells in patients with
Simvastatin produced a 43% reduction in whole-brain secondary progressive multiple sclerosis.70
volume loss and a slowing in disability worsening An intriguing related approach involves using OPCs71
measured by EDSS (absolute difference in means of or OPC-like induced pluripotent stem cells72 as the basis
0·25 points). Another trial investigated a repurposed for high-throughput screening of available drugs for
sodium-channel blocker, phenytoin, to assess whether it their ability to stimulate remyelination. Molecules
protects axons from acute inflammatory injury in acute identified in the initial screens were further evaluated by
optic neuritis.63 Phenytoin treatment within 2 weeks of increasingly stringent in-vitro and in-vivo testing,
onset led to a 30% decrease in loss of retinal nerve fibre identifying the muscarinic antagonist benzatropine, the
layer thickness relative to placebo. This success contrasts antihistamine clemastine, the imidazole antifungal
that from trials of another sodium-channel blocker, miconazole, and the topical steroid clobetasol as
lamotrigine, which did not slow brain volume loss in potential candidates for further testing. A pilot study of
patients with secondary progressive multiple sclerosis.64 clemastine showed improvement on visual evoked
This discrepancy could relate to a pseudoatrophy effect potentials in participants with multiple sclerosis-related
seen in the first year of the lamotrigine study, which chronic optic neuropathy.73
might have obscured a potential benefit. Similarly, the Mesenchymal stem cell (MSC) transplantation has been
neuroprotective effects of cannabinoids in preclinical assessed as a potential repair-promoting strategy for
studies were not confirmed in a trial of the synthetic multiple sclerosis.74 MSCs are pluripotent precursor cells
cannabinoid dronabinol in patients with primary and that can be isolated from bone marrow, adipose tissue,
secondary progressive multiple sclerosis. Treatment did and numerous other tissues, and propagated in culture to
not reduce disability worsening over 3 years.48 The low increase cell yield and purity. They have numerous
progression rate in the placebo group decreased the immunomodulatory, tissue-protective, and repair-
power of this study to demonstrate benefit. promoting properties.74 After several preliminary studies
Cellular energy metabolism seems to be abnormal in showing good safety and tolerability, the ongoing
progressive multiple sclerosis11 and is another potential MESEMS phase 2 trial (NCT01854957) should provide
therapeutic target. The vitamin biotin is a coenzyme for more definitive evidence concerning safety and efficacy.
1362 www.thelancet.com Vol 389 April 1, 2017
Series
However, important methodological questions remain, priority by the International Progressive MS Alliance.2
including preferred source (bone marrow vs adipose Although most studies of physiotherapy and multi-
tissue), cell production protocol to optimise yield and disciplinary rehabilitation have focused on relapsing-
potency, whether the cells can be cryopreserved or need to remitting multiple sclerosis, some evidence suggests that
be administered immediately, best route of administration these approaches can improve ability, participation, and
(intravenous, intrathecal, or intra-arterial), appropriate health-related quality of life and coping skills in patients
dose and dosing schedule, and whether the cells should be with progressive multiple sclerosis.76 However, a recent
derived from patients (autologous) or people without systematic review found that, although 13 studies showed
multiple sclerosis (allogeneic).74 benefit in at least one outcome measure, all were either
under-powered or had methodological issues.76 Adequately
Future directions designed clinical trials will be necessary to advance
The largely disappointing results of studies of anti- rehabilitation for progressive multiple sclerosis.
inflammatory drugs in patients with progressive multiple There is some evidence to suggest that exercise,
sclerosis indicate that therapies that target other incorporating endurance or resistance training, is feasible
mechanisms will be necessary. One obstacle to in patients with multiple sclerosis,77 and improving
development of such strategies is the incomplete physical fitness benefits not only physical function but
understanding of the pathophysiology of progression. also cognitive function.78 Addressing the multiplicity of
Therefore, the range of approaches under investigation symptoms in progressive multiple sclerosis could need a
remains relatively broad and without clear pattern of combination of approaches and use a range of outcomes.
success. MS-SMART (NCT01910259) is applying an A recent pilot trial used three forms of exercise and
adaptive trial design to evaluate three putative demonstrated benefit in both mobility and cognition.79
neuroprotective agents, amiloride, riluzole, and Similarly, a 2016 study showed augmented benefit from
fluoxetine. A second noteworthy obstacle is the lack of a combining exercise with symptomatic therapy.80 For
validated phase 2 trial methodology that reliably predicts patients with greater disability, robotics are useful to
success of neuroprotective and repair-promoting augment the power and precision of voluntary movements
strategies in phase 3 studies. Two general approaches of limbs with impaired motor function.81 Results for gait
have been explored: recovery from an acute lesion and balance training have been encouraging, although
involving an eloquent pathway (eg, the optic nerve), or an trial sizes were relatively small. Some benefits were also
imaging biomarker (eg, whole-brain atrophy). The seen for upper limb function.
eloquent pathway approach has the advantage of Several studies have demonstrated neuroplasticity in
sensitivity, but the relevance of improving recovery from a patients with multiple sclerosis, measured with functional
focal acute inflammatory lesion to lessening damage in imaging and, more recently, physiological techniques at
progressive multiple sclerosis is uncertain. Conversely, the synaptic level.82,83 Functional reorganisation after
assessing whole-brain or regional volume loss seems relapse is shown to help to restore function. At a cellular
more likely to measure preservation of tissue integrity level, synaptic plasticity seems to make an important
relevant to progressive multiple sclerosis but could be contribution to recovery in multiple sclerosis. Long-term
insufficiently sensitive for a phase 2 trial. In addition to potentiation of synaptic transmission might functionally
testing the efficacy of ibudilast in patients with primary compensate for neuronal loss through increasing synaptic
and secondary progressive multiple sclerosis, the excitability of denervated neurons. This phenomenon has
SPRINT-MS trial (NCT01982942) is evaluating the relative been demonstrated after relapse, but not yet in progression.
sensitivity of whole-brain and regional atrophy measures, The challenge will be to incorporate approaches that target
DTI, magnetisation transfer imaging, and optical these mechanisms into active rehabilitation programmes.
coherence tomography to detect neuroprotection for use This issue is compounded in progressive multiple sclerosis
in proof-of-concept clinical trials. However, the population by smaller cognitive and motor reserve.
most likely to benefit from neuroprotective or repair- Management of progressive multiple sclerosis presents
promoting strategies and the optimum trial design to a number of other challenges. The population is older
demonstrate benefit have yet to be defined. with increased likelihood of comorbidities.84 Recognition
and treatment of disorders such as musculoskeletal
Restorative and rehabilitation approaches disorders, diabetes, cardiac disease, and respiratory
People with progressive multiple sclerosis must manage dysfunction are necessary to maximise levels of ability
increasing disability from a wide range of complex and participation. Additionally, awareness of the factors
interacting symptoms, with impairments of gait, vision, that lead to falls (inevitably associated with increasing
and cognition considered the most relevant for those who disability and therefore more common in progressive
have lived with multiple sclerosis for longer than 15 years.75 multiple sclerosis), and preventive measures to avoid
Given the paucity of pharmacological treatments for these them, is essential.85
symptoms, restorative and rehabilitation approaches form Over and above all of these approaches, embracing a
the mainstay of their management; highlighted as a key holistic concept of wellness and encouraging lifestyle
www.thelancet.com Vol 389 April 1, 2017 1363
Series
choices across physical, emotional, social, intellectual, 7 Calabrese M, Poretto V, Favaretto A, et al. Cortical lesion load
occupational, and spiritual dimensions is a key element associates with progression of disability in multiple sclerosis.
Brain 2012; 135: 2952–61.
of a comprehensive management plan and one that is 8 Peterson JW, Bo L, Mork S, Chang A, Trapp BD.
strongly advocated by people with multiple sclerosis.86 Transected neurites, apoptotic neurons, and reduced inflammation
This approach serves to underline the importance of self- in cortical multiple sclerosis lesions. Ann Neurol 2001; 50: 389–400.
9 Serafini B, Rosicarelli B, Magliozzi R, Stigliano E, Aloisi F.
management at all stages of multiple sclerosis. Detection of ectopic B-cell follicles with germial centers in the
meninges of patients with secondary progressive multiple sclerosis.
Conclusions and future perspectives Brain Pathol 2004; 14: 164–74.
10 Howell OW, Reeves CA, Nicholas R, et al. Meningeal inflammation
The pathogenic mechanisms underlying acute relapses is widespread and linked to cortical pathology in multiple sclerosis.
and progression differ, although both processes probably Brain 2011; 134: 2755–71.
coexist to varying degrees throughout the course of 11 Mahad DH, Trapp BD, Lassmann H. Progressive multiple sclerosis
multiple sclerosis. Therapies approved for relapsing- 1. Pathological mechanisms in progressive multiple sclerosis.
Lancet Neurol 2015; 14: 183–93.
remitting multiple sclerosis have little or no benefit in 12 Chang A, Tourtellotte WW, Rudick RA, Trapp BD.
patients with progressive multiple sclerosis in the absence Premyelinating oligodendrocytes in chronic lesions of multiple
of ongoing inflammatory lesion activity. Therapies are sclerosis. N Engl J Med 2002; 346: 165–73.
13 Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mork S, Bo L.
needed that prevent progression independent of acute Axonal transection in the lesions of multiple sclerosis. N Engl J Med
inflammatory pathology. Approaches are also needed to 1998; 338: 278–85.
restore function, both through promoting tissue repair 14 Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical
course of multiple sclerosis: the 2013 revisions. Neurology 2014;
and improving function of damaged tissue. Successful 83: 278–86.
development of new therapies for progressive multiple 15 Cohen JA, Reingold SC, Polman CH, Wolinsky JS, for the
sclerosis will need improved understanding of the International Advisory Committee on Clinical Trials in Multiple
Sclerosis. Disability outcome measures in multiple sclerosis trials:
pathogenesis of progression and more sensitive clinical current status and future prospects. Lancet Neurol 2012; 11: 467–76.
and imaging outcome measures. 16 Rudick RA, LaRocca N, Hudson LD, MSOAC. Multiple Sclerosis
Contributors Outcome Assessments Consortium: Genesis and initial project
DO drafted the sections on phenotype classification and imaging and plan. Mult Scler J 2014; 20: 12–17.
provided modifications to the text in all other sections. AJT drafted the 17 Lublin F, Miller DH, Freedman MS, et al. Oral fingolimod in primary
introduction and sections on restorative and rehabilitation approaches, progressive multiple sclerosis (INFORMS): a phase 3, randomised,
double-blind, placebo-controlled trial. Lancet 2016; 387: 1075–84.
and provided modifications to the text in all other sections. RJF drafted
the sections on disease and neuroprotective therapeutic strategies, and 18 Rudick RA, Miller D, Bethoux F, et al. The Multiple Sclerosis
Performance test (MSPT): an iPad-based disability assessment tool.
provided modifications to the text in all other sections. JAC drafted the
J Vis Exp 2014; 30: e51318.
sections on pathogenesis, measures of disability, and repair-promoting
19 Sormani MP, Bruzzi P. MRI lesions as a surrogate for relapses in
therapeutic strategies; provided modifications to the text in all other
multiple sclerosis: a meta-analysis of randomised trials.
sections; and did the final editing before submission. Lancet Neurol 2013; 12: 669–76.
Declaration of interests 20 De Stefano N, Giorgio A, Battaglini M, et al. Assessing brain
DO reports personal fees from Acorda Therapeutics, Alkermes, Biogen, atrophy rates in a large population of untreated multiple sclerosis
Genentech, Genzyme, Mallinkrodt, and Teva; and grants from Genzyme subtypes. Neurology 2010; 74: 1868–76.
and Novartis. AJT reports fees paid to his institution from Biogen, Esai, 21 Zivadinov R, Sepcic J, Nasuelli D, et al. A longitudinal study of
MedDay, Novartis, Teva; honoraria from EXCEMED, Remedica, and brain atrophy and cognitive disturbances in the early phase of
Sage; and travel support for serving on the Scientific Advisory Board relapsing-remitting multiple sclerosis. J Neurol Neurosurg Psychiatry
from International Progressive MS Alliance. RJF reports personal fees 2001; 70: 773–80.
from Actelion, Biogen, Genentech, Mallinckrodt, MedDay, Novartis, 22 Sormani MP, Arnold DL, De Stefano N. Treatment effect on brain
Teva, and XenoPort. JAC reports personal fees from Genentech, atrophy correlates with treatment effect on disability in multiple
sclerosis. Ann Neurol 2014; 75: 43–49.
Genzyme, Novartis, Receptos, and Teva and an honorarium from Sage.
23 Altmann DR, Jasperse B, Barkhof F, et al. Sample sizes for brain
Acknowledgments atrophy outcomes in trials for secondary progressive multiple
DO is supported by grant KL2 TR000440, and RJF is supported by grant sclerosis. Neurology 2009; 72: 595–601.
1U01NS082329 from the US National Institutes of Health. We thank 24 Seewann A, Kooi EJ, Roosendaal SD, et al. Postmortem verification of
Amanda Mendelsohn who helped to create the figures. MS cortical lesion detection with 3D DIR. Neurology 2012; 78: 302–08.
25 Mainero C, Benner T, Radding A, et al. In vivo imaging of cortical
References
pathology in multiple sclerosis using ultra-high field MRI.
1 Browne P, Chandraratna D, Angood C, et al. Atlas of multiple
Neurology 2009; 73: 941–48.
sclerosis 2013: a growing global problem with widespread inequity.
Neurology 2014; 83: 1022–24. 26 Fisher E, Lee J-C, Nakamura K, Rudick RA. Gray matter atrophy in
multiple sclerosis: a longitudinal study. Ann Neurol 2008; 64: 255–65.
2 Fox RJ, Thompson A, Baker D, et al. Setting a research agenda for
progressive multiple sclerosis: the International Collaborative on 27 Chen JT, Narayanan S, Collins DL, Smith SM, Matthews PM,
Progressive MS. Mult Scler J 2012; 18: 1534–40. Arnold DL. Relating neocortical pathology to disability progression
in multiple sclerosis using MRI. Neuroimage 2004; 23: 1168–75.
3 Miller DH, Leary SM. Primary-progressive multiple sclerosis.
Lancet Neurol 2007; 6: 903–12. 28 Calabrese M, Rinaldi F, Grossi P, Gallo P. Cortical pathology and
cognitive impairment in multiple sclerosis. Expert Rev Neurother
4 Kantarci OH, Lebrun C, Siva A, et al. Primary progressive multiple
2011; 11: 425–32.
sclerosis evolving from radiologically isolated syndrome.
Ann Neurol 2016; 79: 288–94. 29 Anderson VM, Fisniku LK, Khaleeli Z, et al. Hippocampal atrophy
in relapsing-remitting and primary progressive MS: a comparative
5 Lucchinetti CF, Parisi J, Bruck W. The pathology of multiple
study. Mult Scler 2010; 16: 1083–90.
sclerosis. Neurol Clin 2005; 23: 77–105.
30 Mesaros S, Rocca MA, Pagani E, et al. Thalamic damage predicts
6 Lucchinetti CF, Popescu BFG, Bunyan RF, et al.
the evolution of primary-progressive multiple sclerosis.
Inflammatory cortical demyelination in early multiple sclerosis.
AJNR Am J Neuroradiol 2011; 32: 1016–20.
N Eng J Med 2011; 365: 2188–97.
1364 www.thelancet.com Vol 389 April 1, 2017
Series
31 Fox RJ, Cronin T, Lin J, et al. Measuring myelin repair and axonal 52 Secondary Progressive Efficacy Clinical Trial of Recombinant
loss with diffusion tensor imaging. AJNR Am J Neuroradiol 2011; Interferon-beta-1a in MS (SPECTRIMS) Study Group.
32: 85–91. Randomized controlled trial of interferon-beta-1a in secondary
32 Fisniku LK, Altmann DG, Cercignani M, et al. progressive MS. Clinical results. Neurology 2001; 56: 1496–504.
Magnetization transfer ratio abnormalities reflect clinically relevant 53 The North American Study Group on Interferon Beta-1b in
grey matter damage in multiple sclerosis. Mult Scler 2009; 15: 668–77. Secondary Progressive MS. Interferon beta-1b in secondary
33 MacMillan EL, Tam R, Zhao Y, et al. Progressive multiple sclerosis progressive MS: results from a three-year controlled study.
exhibits decreasing glutamate and glutamine over two years. Neurology 2004; 63: 1788–95.
Mult Scler J 2016; 22: 112–16. 54 Andersen O, Elovaara I, Farkkila M, et al. Multicentre, randomised,
34 Ma D, Gulani V, Seiberlich N, et al. Magnetic resonance double blind, placebo controlled, phase III study of weekly, low
fingerprinting. Nature 2013; 495: 187–92. dose, subcutaneous interferon beta-1a in secondary progressive
35 Bieniek M, Altmann DR, Davies GR, et al. Cord atrophy separates multiple sclerosis. J Neurol Neurosurg Psychiatry 2004; 75: 706–10
early primary progressive and relapsing remitting multiple 55 Kappos L, Weinshenker B, Pozzilli C, et al. Interferon beta-1b in
sclerosis. J Neurol Neurosurg Psychiatry 2006; 77: 1036–39. secondary progressive MS. A combined analysis of the two trials.
36 von Meyenburg J, Wilm BJ, Weck A, et al. Spinal cord Neurology 2004; 63: 1779–87.
diffusion-tensor imaging and motor-evoked potentials in multiple 56 Kappos L, Radue E-W, O’Connor P, et al. A placebo-controlled trial
sclerosis patients: microstructural and functional asymmetry. of oral fingolimod in relapsing multiple sclerosis. N Engl J Med
Radiology 2013; 267: 869–79. 2010; 362: 387–401.
37 Charil A, Caputo D, Cavarretta R, Sormani MP, Ferrante P, 57 Cohen JA, Barkhof F, Comi G, et al. Oral fingolimod or
Filippi M. Cervical cord magnetization transfer ratio and clinical intramuscular interferon for relapsing multiple sclerosis.
changes over 18 months in patients with relapsing-remitting N Engl J Med 2010; 362: 402–15.
multiple sclerosis: a preliminary study. Mult Scler 2006; 12: 662–65. 58 Calabresi PA, Radu EW, Goodin D, et al. Safety and efficacy of
38 Marliani AF, Clementi V, Albini Riccioli L, et al. fingolimod in patients with relapsing-remitting multiple sclerosis
Quantitative cervical cord 3T proton MR spectroscopy in multiple (FREEDOMS II): a double-blind, randomised, placebo-controlled,
sclerosis. AJNR Am J Neuroradiol 2010; 31: 180–84. phase 3 trial. Lancet Neurol 2014; 13: 545–56.
39 Oh U, Fujita M, Ikonomidou VN, et al. Translocator protein PET 59 Groves A, Kihara Y, Chun J. Fingolimod: direct CNS effects of
imaging for glial activation in multiple sclerosis. sphingosine 1-phosphate (S1P) receptor modulation and implications
J Neuroimmune Pharmacol 2011; 6: 354–61. in multiple sclerosis therapy. J Neurol Sci 2013; 328: 9–18.
40 Wu C, Zhu J, Baeslack J, et al. Longitudinal positron emission 60 McFarland HF. The B cell—old player, new position on the team
tomography imaging for monitoring myelin repair in the spinal (editorial). N Engl J Med 2008; 358: 664–65.
cord. Ann Neurol 2013; 74: 688–98. 61 Wolinsky JS, Arnold D, Bar-Or A, et al. Efficacy of ocrelizumab in
41 Martinez-Lapiscina EH, Arnow S, Wilson JA, et al. patients with PPMS with and without T1 gadolinium-enhancing
Retinal thickness measured with optical coherence tomography lesions at baseline in a phase III placebo-controlled trial (LB148).
and risk of disability worsening in multiple sclerosis: a cohort Mult Scler J 2016; 22: 67–68.
study. Lancet Neurol 2016; 15: 574–84. 62 Chataway J, Schuerer N, Alsanousi A, et al. Effect of high-dose
42 Saidha S, Al-Louzi O, Ratchford JN, et al. Optical coherence simvastatin on brain atrophy and disability in secondary progressive
tomography reflects brain atrophy in multiple sclerosis: multiple sclerosis (MS-STAT): a randomised, placebo-controlled,
a four-year study. Ann Neurol 2015; 78: 801–13. phase 2 trial. Lancet 2014; 383: 2213–21.
43 Steiner D, Arnold D, Freedman M, et al. Natalizumab versus 63 Raftopoulos R, Hickman SJ, Toosy A, et al. Phenytoin for
placebo in patients with secondary progressive multiple sclerosis neuroprotection in patients with acute optic neuritis: a randomised,
(SPMS): results from ASCEND, a multicenter, double-blind, placebo-controlled, phase 2 trial. Lancet Neurol 2016; 15: 259–69.
placebo-controlled, randomized phase 3 clinical trial. Annual 64 Kapoor R, Furby J, Hayton T, et al. Lamotrigine for neuroprotection in
Meeting of the American Academy of Neurology; April 15–21, 2016; secondary progressive multiple sclerosis: a randomised, double-blind,
Vancouver, BC, Canada. abstr ES1.009. placebo-controlled, parallel-group study. Lancet Neurol 2010; 9: 681–88.
44 Freedman MS, Bar-Or A, Oger J, et al. A phase III study evaluating 65 Sedel F, Bernard D, Mock DM, Tourbah A. Targeting demyelination
the efficacy and safety of MBP8298 in secondary progressive MS. and virtual hypoxia with high-dose biotin as a treatment for
Neurology 2011; 77: 1551–60. progressive multiple sclerosis. Neuropharmacology 2015; published
45 Hawker K, O’Connor P, Freedman MS, et al. Rituximab in patients online Sept 5. DOI: 10.1016/j.neuropharm.2015.08.028.
with primary progressive multiple sclerosis. Results of a 66 Mi S, Pepinsky RB, Cadavid D. Blocking LINGO-1 as a therapy to
randomized double-blind placebo-controlled multicenter trial. promote CNS repair: from concept to the clinic. CNS Drugs 2013;
Ann Neurol 2009; 66: 460–71. 27: 493–503.
46 Montalban X, Hemmer B, Rammohan K, et al. Efficacy and safety 67 Cadavid D, Balcer L, Galetta S, et al. Efficacy analysis of the
of ecrelizumab in primary progressive multiple sclerosis—results Anti-LINGO-1 monoclonal antibody BIIB033 in acute optic neuritis:
of the placebo-controlled, double-blind, phase III ORATORIO study the RENEW trial. Neurology 2015; 84 (suppl 14): P7.202.
(Abstract 228). Mult Scler J 2015; 23: 780–81. 68 Cadavid D, Edwards KR, Hupperts R, et al. Efficacy analysis of
47 Wolinsky JS, Narayana PA, O’Connor P, et al. Glatiramer acetate opicinumab in relapsing multiple sclerosis: the phase 2b SYNERGY
in primary progressive multiple sclerosis: results of a trial (abstract 192). Mult Scler J 2016; 22 (suppl 3): 66.
multinational, multicenter, double-blind, placebo-controlled trial. 69 Windrem MS, Schanz SJ, Guo M, et al. Neonatal chimerization
Ann Neurol 2007; 61: 14–24. with human glial progenitor cells can both remyelinate and rescue
48 Zajicek J, Ball S, Wright D, et al. Effect of dronabinol on progression the otherwise lethally hypomyelinated shiverer mouse.
in progressive multiple sclerosis (CUPID): a randomised, Cell Stem Cell 2008; 2: 553–65.
placebo-controlled trial. Lancet Neurol 2013; 12: 857–65. 70 Goodman AD. Stem cell therapy for MS. Mult Scler J 2016;
49 Tourbah A, Lebrun-Frenay C, Edan G, et al, for the MS-SPI study 22 (suppl 1): 8.
group. MD1003 (high-dose biotin) for the treatment of progressive 71 Mei F, Fancy SPJ, Shen Y-AA, et al. Micropillar arrays as a
multiple sclerosis: a randomised, double-blind, placebo-controlled high-throughput screening platform for therapeutics in multiple
study. Mult Scler 2016; published online Sept 1. DOI: sclerosis. Nat Med 2014; 20: 954–60.
10.1177/1352458516667568. 72 Najm FJ, Madhavan M, Zaremba A, et al. Drug-based modulation
50 European Study Group on Interferon β-1b in Secondary of endogenous stem cells promotes functional remyelination in
Progressive MS. Placebo-controlled multicentre randomised trial vivo. Nature 2015; 522: 216–20.
of interferon β-1b in treatment of secondary progressive multiple 73 Green A, Gelfand J, Cree B, et al. Positive phase II double-blind
sclerosis. Lancet 1998; 352: 1491–97. randomized placebo-controlled crossover trial of clemastine
51 Cohen JA, Cutter GR, Fischer JS, et al. Benefit of interferon β-1a fumarate for remyelination of chronic optic neuropathy in MS.
on MSFC progression in secondary progressive MS. Neurology Annual Meeting of the American Academy of Neurology;
2002; 59: 679–87. April 15–21, 2016; Vancouver, BC, Canada. abstr ES1.008.
www.thelancet.com Vol 389 April 1, 2017 1365
Series
74 Cohen JA. Mesenchymal stem cell transplantation in multiple 81 Feys P. Potential of robot-assisted therapy for disabled persons with
sclerosis. J Neurol Sci 2013; 333: 43–49. MS. Mult Scler J 2016; 22: 264–65.
75 Heesen C, Bohm J, Reich C, Kasper J, Goebel M, Gold SM. 82 Tomassini V, Matthews PM, Thompson AJ, et al. Neuroplasticity and
Patient perception of bodily functions in multiple sclerosis: gait and functional recovery in multiple sclerosis. Nature Rev Neurol 2012;
visual function are the most valuable. Mult Scler 2008; 14: 988–91. 8: 635–46.
76 Campbell E, Coulter EH, Mattison PG, Miller L, McFadyen A, 83 Weiss S, Mori F, Rossi S, Centonze D. Disability in multiple sclerosis:
Paul L. Physiotherapy rehabilitation for people with progressive when synaptic long-term potentiation fails. Neurosci Biobehav Rev
multiple sclerosis: a systematic review. Arch Phys Med Rehabil 2016; 2014; 43: 88–99.
97: 141–51. 84 Marrie RA, Cohen J, Stuve O, et al. A systematic review of the
77 Dalgas U, Stenager E. Exercise and disease progression in multiple incidence and prevalence of comorbidity in multiple sclerosis:
sclerosis: can exercise slow down the progression of multiple overview. Mult Scler J 2015; 21: 263–81.
sclerosis? Ther Adv Neurol Disord 2012; 5: 81–95. 85 Nilsagard Y, Gunn H, Freeman J, et al. Falls in people with MS—
78 Beier M, Bombardier CH, Hartoonian N, Motl RW, Kraft GH. an individual data meta-analysis from studies from Australia,
Improved physical fitness correlates with improved cognition in Sweden, United Kingdom and the United States. Mult Scler J 2015;
multiple sclerosis. Arch Phys Med Rehabil 2014; 95: 1328–34. 21: 92–100.
79 Briken S, Gold SM, Patra S, et al. Effects of exercise on fitness and 86 Dunn M, Bhargava P, Kalb R. Your patients with MS have set
cognition in progressive MS: a randomized, controlled pilot trial. wellness as a high priority—and the National MS Society is
Mult Scler J 2014; 20: 382–90. responding. Multiple Sclerosis Special Report. US Neurology 2015;
80 Hupperts R, Lycke J, Short C, et al. Prolonged-release fampridine 11: 80–86.
and walking and balance in MS: randomised controlled MOBILE
trial. Mult Scler J 2016; 22: 212–21.
1366 www.thelancet.com Vol 389 April 1, 2017
Вам также может понравиться
- A Meningioma Is AДокумент20 страницA Meningioma Is ASherry KingОценок пока нет
- Case Report Esophageal AtresiaДокумент3 страницыCase Report Esophageal Atresiaadriani lawrenciaОценок пока нет
- Sleep Deprivation Informational EssayДокумент15 страницSleep Deprivation Informational EssayPEYTON KNIGHTОценок пока нет
- Final Research EssayДокумент11 страницFinal Research Essayapi-609081297Оценок пока нет
- Neonatal EncephalopahtyДокумент17 страницNeonatal EncephalopahtyRebeca Tapia RsОценок пока нет
- Pediatric Case 6: Eva Madison (Complex) : Guided Reflection QuestionsДокумент3 страницыPediatric Case 6: Eva Madison (Complex) : Guided Reflection QuestionsKathy ArenasОценок пока нет
- Sleep Duration, Sleep Quality, and The Development of Non Alcoholic Fatty Liver Disease A Cohort StudyДокумент9 страницSleep Duration, Sleep Quality, and The Development of Non Alcoholic Fatty Liver Disease A Cohort StudyReynaldy Anggara SaputraОценок пока нет
- Research Proposal Atrial Septal DefectДокумент28 страницResearch Proposal Atrial Septal DefectIzharIsmailОценок пока нет
- Surgical Therapies For Parkinson DiseaseДокумент13 страницSurgical Therapies For Parkinson DiseaseAnali Durán CorderoОценок пока нет
- Red Eye: A Guide For Non-Specialists: MedicineДокумент14 страницRed Eye: A Guide For Non-Specialists: MedicineFapuw Parawansa100% (1)
- Guillain-Barré Syndrome: Clinical ManifestationsДокумент7 страницGuillain-Barré Syndrome: Clinical Manifestationseagame gamersОценок пока нет
- The Effectiveness of Educational Program On Nurses' Competencies Regarding Pre-Eclampsia Care in Three Hospitals in Sudan2021Документ6 страницThe Effectiveness of Educational Program On Nurses' Competencies Regarding Pre-Eclampsia Care in Three Hospitals in Sudan2021International Journal of Innovative Science and Research Technology100% (1)
- Child's HerniaДокумент13 страницChild's HerniaKreshnik HAJDARIОценок пока нет
- Vomiting in Children 2018 PDFДокумент19 страницVomiting in Children 2018 PDFSamuel DiazОценок пока нет
- Neuroanesthesiology UpdateДокумент23 страницыNeuroanesthesiology UpdateAhida VelazquezОценок пока нет
- Nathália Becker - Sleep Quality and Stress - A Literature Review 2015Документ10 страницNathália Becker - Sleep Quality and Stress - A Literature Review 2015gilangОценок пока нет
- E148 FullДокумент17 страницE148 Fullpatricx10100% (1)
- InTech-Pathophysiology of Gestational Diabetes Mellitus The Past The Present and The FutureДокумент25 страницInTech-Pathophysiology of Gestational Diabetes Mellitus The Past The Present and The FuturefahlevyОценок пока нет
- Brain Storming in Brain TraumaДокумент4 страницыBrain Storming in Brain TraumamatisrocksОценок пока нет
- Tos CronicaДокумент13 страницTos CronicaFlavio GuillenОценок пока нет
- Neonatalhypoglycemia: Is There A Sweet Spot?Документ14 страницNeonatalhypoglycemia: Is There A Sweet Spot?karisman kadirОценок пока нет
- Care Following Cesarean Birth 4 Hours To 3 Days PostpartumДокумент20 страницCare Following Cesarean Birth 4 Hours To 3 Days PostpartumAntonella VitaleОценок пока нет
- Progressive Myoclonic Epilepsies - Practical Neurology 2015. MalekДокумент8 страницProgressive Myoclonic Epilepsies - Practical Neurology 2015. MalekchintanОценок пока нет
- PLACENTA PREVIA CASE STUDY IntroДокумент53 страницыPLACENTA PREVIA CASE STUDY IntrojeremiahОценок пока нет
- Chapter 2 Inflamation (B)Документ86 страницChapter 2 Inflamation (B)مختبرات ابوسارةОценок пока нет
- Angle Closure GlaucomaДокумент6 страницAngle Closure GlaucomaRick van DewОценок пока нет
- Case Study-Molar PregnancyДокумент14 страницCase Study-Molar Pregnancysimbarashe tangwadzana100% (1)
- Subdural HematomaДокумент12 страницSubdural HematomaDeby AnditaОценок пока нет
- Krok Key WordsДокумент50 страницKrok Key WordsKeller 0Оценок пока нет
- The Pathophysiology and Treatment of GlaucomaДокумент11 страницThe Pathophysiology and Treatment of GlaucomaelisaОценок пока нет
- Acute Bronchiolitis Assessment and Management in Urgent CareДокумент25 страницAcute Bronchiolitis Assessment and Management in Urgent CareAna Belén Viteri luzuriagaОценок пока нет
- Annotated BibliographyДокумент10 страницAnnotated Bibliographyapi-273829037Оценок пока нет
- Guillain Barrésyndrome (GBS) DisabilityScore NeurologicalScalesДокумент1 страницаGuillain Barrésyndrome (GBS) DisabilityScore NeurologicalScalesSutama ArtaОценок пока нет
- National TB ProgramДокумент34 страницыNational TB ProgramASTR4 BABY100% (1)
- Amyotrophic Lateral SclerosisДокумент6 страницAmyotrophic Lateral SclerosisJohnjohn MateoОценок пока нет
- All ExhibitsДокумент16 страницAll ExhibitsJuwel KobirОценок пока нет
- Dengue Infection - Case AnalysisДокумент58 страницDengue Infection - Case AnalysisLevi AckerManОценок пока нет
- Neurologic ExamДокумент6 страницNeurologic ExamMDNIC100% (1)
- Management of Obstructive Sleep Apnea in Adults - UpToDateДокумент19 страницManagement of Obstructive Sleep Apnea in Adults - UpToDateJuan Carrillo AguilarОценок пока нет
- Assessing Knowledge, Attitude, and Practice of Diabetes Type 2 Patients Attending Keruguya Referral HospitalДокумент10 страницAssessing Knowledge, Attitude, and Practice of Diabetes Type 2 Patients Attending Keruguya Referral HospitalInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- 1 - Neuro Assessment 2021 - 336Документ30 страниц1 - Neuro Assessment 2021 - 336HADI BADWAN100% (2)
- Diagnosing Patients With Acute-Onset Persistent DizzinessДокумент7 страницDiagnosing Patients With Acute-Onset Persistent DizzinessMuhammed ElgasimОценок пока нет
- Maternal Mortality PDFДокумент101 страницаMaternal Mortality PDFCamille Joy BaliliОценок пока нет
- Nuchal Cord and Its ImplicationsДокумент12 страницNuchal Cord and Its ImplicationsNiecole Gayle LedesmaОценок пока нет
- MOG Antibody-Associated DiseasesДокумент3 страницыMOG Antibody-Associated DiseasesYassmin ElNazerОценок пока нет
- Neurology 4 PDF-mergedДокумент358 страницNeurology 4 PDF-mergedAnuraag YadavОценок пока нет
- 2011 Corrigan - Nutrition in Stroke PatientsДокумент11 страниц2011 Corrigan - Nutrition in Stroke PatientsAmy100% (1)
- Presented by Group 3-B Evangelista, Joe Ana Marie Fonte, Chelsey Kate Frane, Liezl Honrada, Gleadhies Macaraig, BernadetteДокумент30 страницPresented by Group 3-B Evangelista, Joe Ana Marie Fonte, Chelsey Kate Frane, Liezl Honrada, Gleadhies Macaraig, Bernadettekhate fonteОценок пока нет
- Expectatant Management of Cesarean Scar Ectopic PregnancyДокумент5 страницExpectatant Management of Cesarean Scar Ectopic PregnancyEricОценок пока нет
- Superior Oblik PalsyДокумент13 страницSuperior Oblik PalsyYunita ManurungОценок пока нет
- Research PropsalДокумент4 страницыResearch Propsalapi-490644641Оценок пока нет
- Glaucoma: Mohd Roslee Bin Abd GhaniДокумент42 страницыGlaucoma: Mohd Roslee Bin Abd GhaniSaha DirllahОценок пока нет
- Herpes Zoster OphthalmicusДокумент29 страницHerpes Zoster Ophthalmicuspurvi333Оценок пока нет
- 4 HemophiliaДокумент5 страниц4 HemophiliaMary Rose F. MalaluanОценок пока нет
- Introduction RevisionДокумент50 страницIntroduction RevisionGracie S. VergaraОценок пока нет
- Family Case PresentationДокумент32 страницыFamily Case PresentationMay Chelle Erazo0% (2)
- PregnancyДокумент11 страницPregnancyLyra IsraelОценок пока нет
- FAHS Thesis Pattern 2019Документ102 страницыFAHS Thesis Pattern 2019falak chaudharyОценок пока нет
- Systemic Lupus ErythematosusДокумент3 страницыSystemic Lupus ErythematosuspoliututuОценок пока нет
- Diagnosis of Multiple Sclerosis Progress and ChallengesДокумент11 страницDiagnosis of Multiple Sclerosis Progress and Challengessarawu9911Оценок пока нет
- Ophthalmologic Manifestations and Retinal Findings in Children With Down SyndromeДокумент6 страницOphthalmologic Manifestations and Retinal Findings in Children With Down SyndromeMuhammad Imam NoorОценок пока нет
- Research Article: Detection of Diabetic Retinopathy Using Bichannel Convolutional Neural NetworkДокумент7 страницResearch Article: Detection of Diabetic Retinopathy Using Bichannel Convolutional Neural NetworkMuhammad Imam NoorОценок пока нет
- The Role of Head Elevation in Treatment of Vitreous HaemorrhageДокумент7 страницThe Role of Head Elevation in Treatment of Vitreous HaemorrhageMuhammad Imam NoorОценок пока нет
- Jurnal 2Документ6 страницJurnal 2RizkyОценок пока нет
- Assessment of Tear-Evaporation Rate in Thyroid-Gland PatientsДокумент5 страницAssessment of Tear-Evaporation Rate in Thyroid-Gland PatientsMuhammad Imam NoorОценок пока нет
- Shabto 2020Документ8 страницShabto 2020Muhammad Imam NoorОценок пока нет
- Reoperations For Complications Within 90 Days After Glaucoma SurgeryДокумент3 страницыReoperations For Complications Within 90 Days After Glaucoma SurgeryMuhammad Imam NoorОценок пока нет
- Jurnal Reading 2Документ6 страницJurnal Reading 2Muhammad Imam NoorОценок пока нет
- Jurnal Mata 3Документ6 страницJurnal Mata 3Muhammad Imam NoorОценок пока нет
- Management of KeratitisДокумент12 страницManagement of KeratitisSeptian Harry WibowoОценок пока нет
- Jurnal Mata 1Документ4 страницыJurnal Mata 1Muhammad Imam NoorОценок пока нет
- Association Between Electronic Cigarette Use and Smoking Reduction in FranceДокумент8 страницAssociation Between Electronic Cigarette Use and Smoking Reduction in FranceMuhammad Imam NoorОценок пока нет
- Jurnal Reading 3Документ11 страницJurnal Reading 3Muhammad Imam NoorОценок пока нет
- Efficacy of 0.5% Levofloxacin and 5.0% Povidone-Iodine Eyedrops in Reducing Conjunctival Bacterial FloraДокумент9 страницEfficacy of 0.5% Levofloxacin and 5.0% Povidone-Iodine Eyedrops in Reducing Conjunctival Bacterial FloraMuhammad Imam NoorОценок пока нет
- E-Cigarettes Use Behavior and Experience of AdultsДокумент7 страницE-Cigarettes Use Behavior and Experience of AdultsMuhammad Imam NoorОценок пока нет
- Bremond Gignac2010Документ5 страницBremond Gignac2010Muhammad Imam NoorОценок пока нет
- Clinical Manifestations, Diagnosis, and Surgery of Inferior Oblique Muscle EctopiaДокумент5 страницClinical Manifestations, Diagnosis, and Surgery of Inferior Oblique Muscle EctopiaMuhammad Imam NoorОценок пока нет
- Clinical Study: Systemic Factors Associated With Treatment Response in Diabetic Macular EdemaДокумент6 страницClinical Study: Systemic Factors Associated With Treatment Response in Diabetic Macular EdemaMuhammad Imam NoorОценок пока нет
- Research Article: Detection of Diabetic Retinopathy Using Bichannel Convolutional Neural NetworkДокумент7 страницResearch Article: Detection of Diabetic Retinopathy Using Bichannel Convolutional Neural NetworkMuhammad Imam NoorОценок пока нет
- Research Article: The Adverse Impact of Glaucoma On Psychological Function and Daily Physical ActivityДокумент8 страницResearch Article: The Adverse Impact of Glaucoma On Psychological Function and Daily Physical ActivityMuhammad Imam NoorОценок пока нет
- Vent Rig Lio 2017Документ2 страницыVent Rig Lio 2017Muhammad Imam NoorОценок пока нет
- A Comparison of Daily Versus Weekly Electronic Cigarette Users in Treatment For Substance AbuseДокумент7 страницA Comparison of Daily Versus Weekly Electronic Cigarette Users in Treatment For Substance AbuseMuhammad Imam NoorОценок пока нет
- Punia 2019Документ2 страницыPunia 2019Muhammad Imam NoorОценок пока нет
- Acanthamoeba Keratitis in Noncompliant Soft Contact Lenses UsersДокумент7 страницAcanthamoeba Keratitis in Noncompliant Soft Contact Lenses UsersMuhammad Imam NoorОценок пока нет
- Social Media Use and Conduct Problems in Emerging Adults: Apid OmmunicationsДокумент5 страницSocial Media Use and Conduct Problems in Emerging Adults: Apid OmmunicationsindahОценок пока нет
- Bidirectional Associations Between Child Sleep Problems and Internalizing and Externalizing Difficulties From Preschool To Early AdolescenceДокумент8 страницBidirectional Associations Between Child Sleep Problems and Internalizing and Externalizing Difficulties From Preschool To Early AdolescenceMuhammad Imam NoorОценок пока нет
- Psychiatric Comorbidity in Adolescent Electronic and Conventional Cigarette UseДокумент19 страницPsychiatric Comorbidity in Adolescent Electronic and Conventional Cigarette UseMuhammad Imam NoorОценок пока нет
- Urosepsis-Etiology, Diagnosis, and Treatment: Continuing Medical EducationДокумент14 страницUrosepsis-Etiology, Diagnosis, and Treatment: Continuing Medical EducationMuhammad Imam NoorОценок пока нет
- Diagnosis and Management For UrosepsisДокумент8 страницDiagnosis and Management For UrosepsisMuhammad Imam NoorОценок пока нет
- 878Wag2015MS Urosepsis OverviewДокумент20 страниц878Wag2015MS Urosepsis OverviewMuhammad Imam NoorОценок пока нет
- Multiple Sclerosis AANN-ARN-IOMSN-MS-Guideline - FINAL PDFДокумент49 страницMultiple Sclerosis AANN-ARN-IOMSN-MS-Guideline - FINAL PDFCyntia Theresia LumintangОценок пока нет
- DMT Consensus MS CoalitionДокумент73 страницыDMT Consensus MS CoalitionDeepaОценок пока нет
- Multiple SclerosisДокумент35 страницMultiple SclerosisJc SeguiОценок пока нет
- Cidp Nejm PDFДокумент14 страницCidp Nejm PDFFebrianaОценок пока нет
- Ubogu - Inflammatory NeuropathiesДокумент24 страницыUbogu - Inflammatory NeuropathiesMarcelo BedoyaОценок пока нет
- Multiple Sclerosis Research Paper OutlineДокумент6 страницMultiple Sclerosis Research Paper Outlinevbbcvwplg100% (1)
- Ms PresДокумент17 страницMs Presapi-278737325Оценок пока нет
- Handbook of Multiple Sclerosis 4th Ed - S. Cook (Taylor and Francis, 2006) WW PDFДокумент546 страницHandbook of Multiple Sclerosis 4th Ed - S. Cook (Taylor and Francis, 2006) WW PDFGigiEnergie100% (1)
- Assessment of Bone Marrow-Derived Cellular Therapy in Progressive Multiple Sclerosis (ACTiMuS) - Full Text View - ClinicalTrialsДокумент4 страницыAssessment of Bone Marrow-Derived Cellular Therapy in Progressive Multiple Sclerosis (ACTiMuS) - Full Text View - ClinicalTrialsAnonymous 0qYv7WpgОценок пока нет
- NeuroДокумент317 страницNeuroNela Popa100% (2)
- Multiple Sclerosis: BY: Ridhima Daga MPT-2 YearДокумент130 страницMultiple Sclerosis: BY: Ridhima Daga MPT-2 YearDurga BhavaniОценок пока нет
- Acquired Demyelinating SyndromesДокумент13 страницAcquired Demyelinating SyndromesfbonillaОценок пока нет
- Multiple SclerosisДокумент2 страницыMultiple Sclerosisplethoraldork100% (5)
- MMNCB Distribution of Demyelination and Axonal DegenerationДокумент7 страницMMNCB Distribution of Demyelination and Axonal DegenerationShauki AliОценок пока нет
- Ayurpharm 393Документ6 страницAyurpharm 393Rahul KirkОценок пока нет
- An Illustrated Pocketbook of Multiple SclerosisДокумент98 страницAn Illustrated Pocketbook of Multiple SclerosisMskola Karlovac100% (1)
- Fatty Liver and MSДокумент16 страницFatty Liver and MSAljon Anies100% (1)
- Perez-Cerdá - Inflammation Neurodegeneration Multiple SclerosisДокумент8 страницPerez-Cerdá - Inflammation Neurodegeneration Multiple SclerosisinesОценок пока нет
- AP 1 Transcription Factor As Precursor of PostZika and MS SymptomsДокумент22 страницыAP 1 Transcription Factor As Precursor of PostZika and MS SymptomsElton MatsushimaОценок пока нет
- Ljunggren-Rose Et Al., 2020 PDFДокумент9 страницLjunggren-Rose Et Al., 2020 PDFAna paula CamargoОценок пока нет
- Multiple SclerosisДокумент4 страницыMultiple SclerosisnasibdinОценок пока нет
- Study Guide For Lorenzo S OilДокумент20 страницStudy Guide For Lorenzo S Oilthe_wise_oneОценок пока нет
- Worksheet 16Документ2 страницыWorksheet 16Aleksei CuadraОценок пока нет
- BSR 39 bsr20181335 PDFДокумент11 страницBSR 39 bsr20181335 PDFFelipe MОценок пока нет
- MS in Focus 20 Is It MS EnglishДокумент28 страницMS in Focus 20 Is It MS EnglishDeepaОценок пока нет
- Chronic Inflammatory Demyelinating PolyradiculoneuropathДокумент13 страницChronic Inflammatory Demyelinating Polyradiculoneuropathrafael rocha novaesОценок пока нет
- Health Problems Philosophical Puzzles About The Nature of Health Elizabeth Barnes Full ChapterДокумент67 страницHealth Problems Philosophical Puzzles About The Nature of Health Elizabeth Barnes Full Chaptersteven.kincaid536100% (4)
- Pathologi GbsДокумент8 страницPathologi GbssandykumalaОценок пока нет
- Multiple Sclerosis Lancet 2018Документ15 страницMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoОценок пока нет
- Multiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskДокумент39 страницMultiple Sclerosis: Saadia Perwaiz, PT BSPT, M. Phil-MskArslan Aslam100% (2)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!От EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Рейтинг: 5 из 5 звезд5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisОт EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerОт EverandGut: the new and revised Sunday Times bestsellerРейтинг: 4 из 5 звезд4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 3.5 из 5 звезд3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningОт EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningРейтинг: 4 из 5 звезд4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)От EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Рейтинг: 4 из 5 звезд4/5 (378)
- To Explain the World: The Discovery of Modern ScienceОт EverandTo Explain the World: The Discovery of Modern ScienceРейтинг: 3.5 из 5 звезд3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlОт EverandThe Marshmallow Test: Mastering Self-ControlРейтинг: 4.5 из 5 звезд4.5/5 (58)