Академический Документы
Профессиональный Документы
Культура Документы
Bittencourt, Lucena-Santos, Moraes, & Oliveira, 2012
Загружено:
Ana Sofia AlmeidaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Bittencourt, Lucena-Santos, Moraes, & Oliveira, 2012
Загружено:
Ana Sofia AlmeidaАвторское право:
Доступные форматы
Trends
in Psychiatry and Psychotherapy Original Article
Anxiety and depression symptoms in women
with and without binge eating disorder enrolled
in weight loss programs
Sintomas de ansiedade e depressão em mulheres com e sem compulsão
alimentar participantes de programas de redução de peso
Simone Armentano Bittencourt,1 Paola Lucena-Santos,2 João Feliz Duarte Moraes,3 Margareth da Silva Oliveira4
Abstract Resumo
Objectives: 1) To investigate the association between binge Objetivos: 1) Investigar a associação entre escores de compul-
eating scores, anxiety and depression symptoms, and body são alimentar, sintomas de ansiedade e de depressão e índice de
mass index (BMI), and 2) to assess the presence of differences in massa corporal (IMC); e 2) verificar se existe diferença na inten-
severity of anxiety symptoms, severity of depression symptoms, sidade dos sintomas de ansiedade, dos sintomas depressivos e
and BMI in women with and without binge eating disorder. no IMC em mulheres com e sem compulsão alimentar.
Method: The sample comprised 113 women aged between 22 Método: A amostra foi composta de 113 mulheres com idade
and 60 years (39.35±10.85) enrolled in weight loss programs entre 22 e 60 anos (39,35±10,85), participantes de programas
in Porto Alegre, southern Brazil. The following instruments were de redução de peso na cidade de Porto Alegre, sul do Brasil.
used: structured interview, Brazilian Economic Classification Foram aplicados os seguintes instrumentos: entrevista estrutu-
Criteria, Beck Anxiety Inventory, Beck Depression Inventory, and rada, Critérios de Classificação Econômica Brasil, Inventário de
Binge Eating Scale. Data were analyzed using descriptive and Ansiedade de Beck, Inventário de Depressão de Beck e Escala
inferential statistics. de Compulsão Alimentar Periódica. Os dados foram analisados
Results: A positive association was found between binge eating utilizando-se estatística descritiva e inferencial.
scores and the severity of anxiety symptoms (p < 0.001) and Resultados: Houve associação positiva entre os escores de
depression symptoms (p < 0.001). No significant association compulsão alimentar e a intensidade dos sintomas de ansieda-
was observed between BMI and binge eating scores (p = 0.341). de (p < 0,001) e de depressão (p < 0,001). Não foi observada
There were significant differences between women with and associação significativa (p = 0,341) entre IMC e escores de com-
without binge eating disorder with regard to severity of anxiety pulsão alimentar. Houve diferença significativa entre mulheres
symptoms (p < 0.001) and severity of depression symptoms (p com e sem co mpulsão alimentar com relação à intensidade dos
< 0.001). Conversely, no significant differences were observed sintomas de ansiedade (p < 0,001) e depressão (p < 0,001).
between the groups concerning BMI (p = 0.103). Não foi encontrada diferença significativa entre os grupos com
Conclusion: Our findings showed that binge eating is associated relação ao IMC (p = 0,103).
with symptoms of anxiety and depression, but not with BMI. Conclusão: Os achados deste estudo mostraram que a com-
Keywords: Anxiety, depression, feeding behavior, compulsive pulsão alimentar está associada a sintomas de ansiedade e de
behavior. depressão, porém não está associada ao IMC.
Descritores: Ansiedade, depressão, comportamento alimentar,
comportamento compulsivo.
1
Doutora, Psicologia, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. 2 Acadêmica de Psicologia, PUCRS. Bolsista
de Iniciação Científica, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). 3 Doutor, Gerontologia Biomédica, PUCRS. Professor adjunto,
Faculdades de Matemática, PUCRS e Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil. 4 Doutora, Ciências da Saúde, Universidade
Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil. Professora adjunta, Programa de Pós-Graduação em Psicologia, PUCRS. Bolsista de Produtividade em
Pesquisa Nível 1D, CNPq.
Financial support: Grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Submitted Oct 19 2010, accepted for publication Aug 22 2011. No conflicts of interest declared concerning the publication of this article.
Suggested citation: Bittencourt SA, Lucena-Santos P, Moraes JF, Oliveira MS. Anxiety and depression symptoms in women with and without binge eating disorder
enrolled in weight loss programs. Trends Psychiatry Psychother. 2012;34(2):87-92.
© APRS Trends Psychiatry Psychother. 2012;34(2) – 87-92
Anxiety and depression in binge eating patients – Bittencourt et al.
Introduction increase the risk of cardiovascular disease, which
seems to suggest that the association between obesity
Obesity is a condition in which excess fat accumulates and depression could further increase the incidence of
to the extent of having adverse effects on health. In cardiovascular conditions. With regard to the quality of
2006, there were approximately 1 billion and 600 life of obese individuals, the review conducted by Kushner
million people aged 15 years and older with overweight & Foster,13 which had the aim of analyzing the impact of
worldwide, and at least 400 million adults with obesity. obesity on quality of life, found that obesity has negative
It is estimated that, by 2015, the number of overweight consequences on quality of life, both in terms of physical
adults will reach approximately 2 billion and 300 million, aspects and of psychosocial functioning.
and over 700 million adults will be obese. Overweight Finally, a high prevalence of severe binge eating
and obesity were originally considered diseases of disorders (BEDs) is also observed in obese populations.
developed countries, however their rates have been In fact, BED patients account for the majority of people
drastically increasing in developing countries, especially seeking assistance at health care services that offer
in urban areas.1 weight loss programs.6
Overweight and obesity cause serious consequences BED is characterized by recurrent episodes of
to health, once a high body mass index (BMI) is an compulsive eating behavior in the absence of other
important risk factor for a variety of chronic conditions, compensatory behaviors aimed at avoiding weight
such as: cardiovascular disease (cardiopathies and gain. During a binge episode, the subject experiences a
stroke), which is the main cause of death worldwide, feeling of loss of control combined with the intake of high
with 17 million of deaths every year; diabetes, which amounts of food, even when not really hungry, resulting
has become a worldwide epidemic, with estimates in great discomfort. Binge episodes are followed by
of a 50% increase in deaths from diabetes by 2015; strong subjective ill-being, characterized by feelings of
cancer (endometrium, breast, and colon), in addition to anguish, sadness, guilt, shame, and self-loathing.14,15
locomotor conditions (e.g. arthrosis).1 BED has been widely studied, with a special focus on
Obese adults and adolescents are openly discriminated binge episodes, which are the main manifestation and
in their professional and academic lives, increasing the form of evaluation of the disease, frequently accompanied
risk for the development of psychiatric conditions in this by hyperphagia and social isolation.16
population, e.g. depression, anxiety disorders, drug abuse, In Brazil, the prevalence of BED in the general
and eating behaviors.2 population ranges from 1.8 to 4.6%; in contrast,
Several studies have been conducted with the aim approximately 30% of obese individuals seeking weight
of improving our understanding of obesity.3-5 The wide loss treatment present the disorder.15 In the majority
interest in the topic is justified by the alarming rates of of cases, obese patients with BED do not lose clinically
obesity in the general population, by the risks associated significant amounts of weight with conventional weight
with the condition, and by the economic costs imposed loss therapies,16 which may be explained, to a great
on society.6 The impacts of obesity are strong, once extent, by the comorbidities associated with the disorder.
eating behaviors are multidetermined, regulated by Individuals with BED seem to present psychopathological
interactions among physiologic, psychological, genetic conditions at higher rates when compared with individuals
and environmental factors to which each individual without the disorder.16,17
is exposed.7 In view of the multifactorial nature of The combination of binge eating and food restriction
obesity, treatment is difficult, and the patient’s physical behaviors is frequent among obese patients, and
and mental health and quality of life are frequently can explain, at least in part, the recurrent failure of
compromised. This is why most studies on obesity interventions aimed at treating obesity. Moreover, some
include the assessment of comorbidities and associated other psychological aspects that also regulate feeding
variables.8 behaviors, e.g. depressive mood and anxiety, are
Obesity is knowingly associated with high rates of frequently present and can influence treatment results.18
psychopathologies, including depression, anxiety, eating A prospective study covering a 4-year follow-
disorders, personality disorders,9 and schizophrenia.10 For up period aimed to investigate the impact of anxiety,
example, it has long been known that the prevalence of depression, and binge eating behaviors on weight loss in
people with overweight or obesity among patients with obese individuals submitted to different therapies (obese
unipolar or bipolar depression is higher than in the general patients submitted to bariatric surgery, obese patients
population, reaching 20 to 45% higher frequencies enrolled in a conventional weight loss program, and a
among obese patients.11 Tapia & Masson12 have pointed group of control obese patients). The study reached the
out to the fact that obesity and depression independently following conclusions: 1) there was a tendency toward
88 – Trends Psychiatry Psychother. 2012;34(2)
Anxiety and depression in binge eating patients – Bittencourt et al.
weight gain in the control group among obese individuals Instruments
with current depressive or anxiety disorder, whereas
individuals in the same group without mental disorders A structured interview was specifically designed for
lost some weight at the beginning of treatment; 2) the present study to collect sample characteristics.
obese patients submitted to bariatric surgery and with The Brazilian Economic Classification Criteria were
a current diagnosis of depressive or anxiety disorder used to determine the economic status of participants.21
lost significantly less weight when compared with obese A questionnaire was applied and yielded a score that
patients in the same group without a diagnosis of mental determined the economic status of each individual
disorder; and 3) patients presenting with binge eating at according to the following categories (from higher to
baseline did not lose weight after 4 years of follow-up.19 lower income): A1, A2, B1, B2, C, D, and E.
These results underscore the importance of developing a The Brazilian version of the Beck Depression Inventory
better understanding of binge eating and related anxiety was used to measure severity of depression.22,23 The
and/or depression symptoms in patients seeking weight instrument comprises 21 questions, each one with four
loss treatment, especially in view of the strong influence answer options. Subjects should choose the answer that
these symptoms have on treatment success. best described them. The total score is a sum of the
Considering all the damage that obesity can scores obtained at each individual item. The following
potentially cause, the loss of weight comes up as a cutoff points have been established for psychiatric
possible solution for the problem. Losing weight can patients in Brazil: 0-11 (minimal depression), 12-19
significantly reduce the risk for the development of most (mild), 20-35 (moderate), and 36-63 (severe).
comorbidities associated with obesity,5 and it is therefore The Brazilian version of the Beck Anxiety Inventory
important that therapies specifically targeted at obesity was used to assess the severity of anxiety among
be developed and implemented in the public health care participants.23,24 This scale also comprises 21 items that
system in Brazil.20 subjects should rate using a four-point scale so as to
Moreover, for the development and implementation reflect their symptoms. Again, the total score is a sum of
of effective therapies specifically aimed at weight loss, the scores obtained at each individual item. The following
it becomes extremely important to study in detail the cutoff points have been established for psychiatric
psychiatric comorbidities most frequently associated with patients: 0-10 (minimal anxiety), 11-19 (mild), 20-30
obesity in the literature. Attention should be given not (moderate), and 31-63 (severe).
only to the identification of behavioral and psychological Finally, the Binge Eating Scale25 was used to assess
variables, but also to the implementation of interventions the presence and severity of binge episodes. The
tailored to the specific characteristics of this population, instrument has been translated into Brazilian Portuguese
taking into consideration the high prevalence of such and validated for use in Brazil.26 The scale is a Likert-
comorbidities. Appropriate interventions will have greater style instrument comprising 62 statements arranged in
chances of succeeding and consequently reducing the 16 items. Subjects should select the response option
risks associated with the obesity epidemic. that best describes their perception. Each statement is
Taking into consideration the wide range of aspects assigned scores from 0 to 3, which correspond to total
related with obesity, the high prevalence of BED among absence (score 0) up to presence of severe compulsion
patients enrolled in weight loss programs, and also (score 3). The total score (sum of individual scores) is
the difficulties faced by binge eaters while trying to interpreted according to the following classification25: ≤
lose weight, the aims of the present study were 1) to 17, absence of compulsive behavior (participants in this
investigate the association between binge eating scores, score category were allocated to the control/non-binging
anxiety and depression symptoms, and body mass index group); 18-25, moderate binging; ≥ 26, severe binging
(BMI), and 2) to assess the presence of differences in (participants in the two latter categories were allocated
severity of anxiety symptoms, severity of depression to the group with BED).
symptoms, and BMI in women with and without BED. The following inclusion criteria were taken into
consideration: being enrolled in weight loss programs
in the municipality of Porto Alegre, southern Brazil,
Method female sex (given the higher prevalence of eating
disorders among females27; the male:female ratio has
This is a cross-sectional and quantitative study. Data been reported to range from 1:10 up to 1:2028), age
analysis was performed using descriptive and inferential between 18 and 60 years,1 and at least 5 years of formal
statistics. The association between variables was also education. Patients presenting with acute psychotic
assessed. episodes or any other conditions that could interfere with
Trends Psychiatry Psychother. 2012;34(2) – 89
Anxiety and depression in binge eating patients – Bittencourt et al.
the understanding of the instruments used in the study For the subsequent analyses, the sample was
were excluded from the sample. divided into two groups: patients with binge episodes
and patients without binge episodes. The chi-square
Ethical considerations test showed that both groups were homogeneous with
regard to the number of subjects (p = 0.301).
The present study was nested in a broader research Approximately 18.6% (21 patients) of the sample
project submitted and approved by the Research Ethics was not attending school; 76.1% (86) were working.
Committee of Pontifícia Universidade do Rio Grande Again, according to the chi-square test, both groups were
do Sul (protocol no. 364/05-CEP). Prior to inclusion in statistically similar with regard to education (p = 0.459) and
the study, all patients were asked to sign an informed working status (p = 0.421). Also, no significant differences
consent form containing the objectives of the study. All were observed between the groups in terms of marital
participants were informed of the purpose of the research status, education level, and economic status (Table 1).
project and were given guarantees of confidentiality and
anonymity by the research team. Table 1 – Sociodemographic characteristics
of patients with and without BED
Following presentation and approval of the study
No BED BED
at the different participating centers, the instruments Frequency % n (%) n (%) p
included in the research protocol were applied individually Marital status
by previously trained research team members. Single 39 34.5 14 (35.9) 25 (64.1)
Married 63 55.8 33 (52.4) 30 (47.6)
Statistical analysis Divorced 11 9.7 4 (36.4) 7 (63.6) 0.221*
Education level
Elementary school 9 8 2 (22.2) 7 (77.8)
Data were entered into the Statistical Package for High school 45 39.8 19 (42.2) 26 (57.8)
the Social Sciences (SPSS) version 17.0. Descriptive and College 59 52.2 30 (50.8) 29 (49.2) 0.272†
inferential analyses were conducted using the following Economic status
statistical tests: Kolmogorov-Smirnov, Fisher’s exact A 16 14.2 11 (68.8) 5 (31.3)
B 41 36.3 19 (46.3) 22 (53.7)
test, Pearson’s chi-square test, Mann-Whitney test, and
C 41 36.3 16 (39.0) 25 (61)
Spearman’s correlation. Significance was set at 5%. D 15 13.3 5 (33.3) 10 (66.7) 0.165*
BED = binge eating disorder.
* Pearson’s chi-square test.
† Fisher’s exact test.
Results
The following variables were tested for normality
The sample comprised 113 women enrolled in
in both groups using the Kolmogorov-Smirnov test:
weight loss programs in the municipality of Porto Alegre,
age, anxiety, depression, and BMI (Table 2). Abnormal
southern Brazil. Mean age was 39.35±10.85 years, and
distributions were observed for all variables in at least
it ranged from 22 to 60 years.
one of the groups. Therefore, the Mann-Whitney test
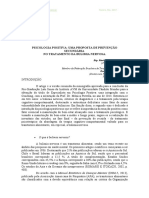
Based on the scores of the Binge Eating Scale,
was used to compare groups, and Spearman correlation
patients were first classified as non-binging, moderate
to assess associations between variables.
binging, or severe binging (Figure 1).
Table 2 – Kolmogorov-Smirnov’s normality test
45.1% Variable No BED (p) BED (p)
Age 0.163 0.005
Anxiety (total BAI score) 0.001 0.200*
Depression (total BDI score) 0.007 0.200*
27.4% 27.4% BMI 0.200* 0.011
BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; BED = binge
eating disorder; BMI = body mass index.
* p value ≥ 0.200.
The Mann-Whitney test revealed statistically
significant differences between patients with and without
No binging Moderate binging Severe binging binge episodes in terms of severity of anxiety symptoms
and severity of depression symptoms. Conversely, no
Figure 1 – Classification of binge eating symptoms
in a sample of women enrolled in weight loss programs significant differences were observed in BMI between
in Porto Alegre, southern Brazil patients with and without binge episodes (Table 3).
90 – Trends Psychiatry Psychother. 2012;34(2)
Anxiety and depression in binge eating patients – Bittencourt et al.
Table 3 – Relationship between presence/absence BED showed higher levels of both depression and anxiety
of BED and severity of anxiety symptoms, severity
of depression symptoms, and BMI when compared with women without BED.
Variable/group n Mean rank p In our study, significant differences were also
Anxiety observed between the groups in relation to anxiety
No BED 51 37.73 levels: higher anxiety levels were associated with
BED 62 72.85 0.000* increased binge eating scores. A previous study34 also
Depression found significant differences between individuals with
No BED 51 34.01
and without BED with regard to depression (p < 0.001)
BED 62 75.91 0.000*
BMI and anxiety levels (p < 0.008), in both male and female
No BED 51 51.45 patients, with higher levels among binge eaters than
BED 62 61.56 0.103* among controls.
BED = binge eating disorder; BMI = body mass index. Total BMI did not differ between patients with and
* Mann-Whitney’s test.
without BED, and no significant association was observed
Spearman correlation revealed a positive association between BMI and binge eating scores. This findings
between binge eating scores and severity of anxiety suggest that a higher BMI is not necessarily associated
symptoms (r = 0.598; p < 0.001) and severity of with BED, which is in accordance with the report by Jirik-
depression symptoms (r = 0.766; p < 0.001). No Babb & Norring,34 who also did not observe differences
significant association was found between BMI and binge between patients with and without BED in relation to
eating scores (r = 0.104; p = 0.082). BMI.
Binge eaters account for a substantial part of the
patients seeking weight loss programs. In this sense, the
Discussion findings of the present study underscore the paramount
importance of assessing anxiety and depression
Of the total sample, 54.8% presented binge episodes: symptoms in BED patients, as well as of defining
27.4% showed moderate binging, and 27.4% showed intervention strategies to deal specifically with these
severe binging. These results are similar to those of a symptoms, which seem to affect treatment results.
previous study29 conducted with morbidly obese patients, Further studies are warranted to further investigate
which observed an overall BED prevalence of 56.7%, these populations, preferably follow-up studies designed
namely 25.4% with moderate binging and 31.3% with to investigate possible predictive factors of feeding
severe binging. In turn, higher rates of BED have been behaviors, aimed at establishing causal relationships
reported for patients seeking weight loss treatment,30 and broadening our scientific knowledge of the variables
which is compatible with the characteristics of our associated with eating disorders.
sample.
Significant differences were observed in our study
between patients with and without BED with relation
to severity of depression symptoms. Also, higher BED References
scores were associated with more severe depression
symptoms. Similar results have been reported in a 1. Organización Mundial de la Salud. Obesidad y sobrepeso.
previous study designed to assess the prevalence of 2006. (Nota Descritiva n. 311). http://www.who.int/media-
centre/factsheets/fs311/es/index.html Accessed 2010 Jul 26.
psychiatric disorders according to the presence of
2. Cordas TA, Ascecio RF, editores. Tratamento comportamental
absence of BED in morbidly obese patients.29 In that da obesidade. Einstein (São Paulo). 2006;4(supl 1):S44-8.
study, the group with BED showed a high prevalence of 3. Costa AC, Ivo ML, Cantero WB, Rognini JR. Obesidade em
major depression (42.1%), with a significant difference pacientes candidatos a cirurgia bariátrica. Acta Paul Enferm.
(p = 0.001) between patients with and without the 2009;22:55-9.
4. Pi-Sunver FX. The medical risks of obesity. Postgrad Med.
disorder.29 Another study31 carried out with obese patients
2009;121:21-33.
enrolled in weight loss programs found an association 5. Mattos RS. Nasci de novo: sobrevivendo ao estigma da gor-
between depression and a higher chance of having BED dura. Um estudo de caso sobre obesidade [dissertação]. Rio
(57%) when compared with patients without depression de Janeiro: Universidade do Estado do Rio de Janeiro; 2008.
(21%), also at a statistically significant difference (p 6. Mancini MC, Aloe F, Tavares S. Apnéia do sono em obesos.
Arq Bras Endocrinol Metab. 2000;44:81-90.
= 0.001). Moreover, Geliebter et al.32 concluded that
7. Quaioti TC, Almeida SS. Determinantes psicobiológicos do
patients with BED presented higher depression scores comportamento alimentar: uma ênfase em fatores am-
when compared with patients without the disorder, and bientais que contribuem para a obesidade. Psicol USP.
Jirik-Babb & Geliebter33 observed that obese women with 2005;17:193-211.
Trends Psychiatry Psychother. 2012;34(2) – 91
Anxiety and depression in binge eating patients – Bittencourt et al.
8. Baptista MN, Vargas JF, Baptista AS. Depressão e qualidade de 22. Beck AT, Steer RA. Beck depression inventory manual. San
vida em uma amostra brasileira de obesos mórbidos. Aval Antonio: Psychology Corporation; 1993.
Psicol. 2008;7:235-47. 23. Cunha JA. Manual da versão em português das escalas Beck.
9. Pull CB. Current psychological assessment practices in obe- São Paulo: Casa do Psicólogo; 2001.
sity surgery programs: what to assess and why. Curr Opin 24. Beck AT, Steer RA. Beck anxiety inventory manual. San An-
Psychiatry. 2010;23:30-6. tonio: Psychological Corporation; 1993.
10. Allison DB, Newcomer JW, Dunn AL, Blumenthal JA, Fabrica- 25. Gormally J, Black S, Daston S, Rardin D. The assessment of
tore AN, Daumit GL, et al. Obesity among those with mental binge eating severity among obese persons. Addict Behav.
disorders: a National Institute of Mental Health meeting re- 1982;7:47-55.
port. Am J Prev Med. 2009;36:341-50. 26. Freitas S, Lopes CS, Coutinho W, Appolinario JC. Tradução e
11. Rihmer Z, Purebl G, Faludi G, Halmy L. Association of adaptação para o português da Escala de Compulsão Alimen-
obesity and depression. Neuropsychopharmacol Hung. tar Periódica. Rev Bras Psiquiatr. 2001;23:215-20.
2008;10:183-9. 27. Saikali CJ, Soubhia CS, Scalfara BM, Cordás TA. Imagem
12. Tapia SA, Masson SL. Detección de síntomas depresivos corporal nos transtornos alimentares. Rev Psiquiatr Clin.
en pacientes con sobrepeso y obesidad. Rev Chil Nutr. 2004;31:164-6.
2006;33:162-9. 28. Klein DA, Walsh BT. Eating disorders: clinical features and
13. Kushner RF, Foster GD. Obesity and quality of life. Nutrition. pathophysiology. Physiol Behav. 2004;81:359-74.
2000;16:947-52. 29. Petribu K, Ribeiro ES, Oliveira FM, Braz CI, Gomes ML, Araujo
14. American Psychiatric Association. Diagnostic and Statistical DE, et al. Transtorno da compulsão alimentar periódica em
Manual of Mental Disorders - 4th edition (DSM-IV). Washing- uma população de obesos mórbidos candidatos a cirurgia
ton: APA; 1994. bariátrica do Hospital Universitário Oswaldo Cruz, em Recife-
15. Duchesne M, Appolinário JC, Rangé BP, Freitas S, Papel- PE. Arq Bras Endocrinol Metab. 2006;50:901-8.
baum M, Coutinho W. Evidências sobre a terapia cognitivo- 30. Pinheiro AP, Sullivan PF, Bacaltchuck J, Prado-Lima PA, Bu-
comportamental no tratamento de obesos com transtorno lik CM. Genética em transtornos alimentares: ampliando os
da compulsão alimentar periódica. Rev Psiquiatr Rio Gd Sul. horizontes de pesquisa. Rev Bras Psiquiatr. 2006;28:218-25.
2004;26:47-51. 31. Pagoto S, Bodenlos JS, Kantor L, Gitkind M, Curtin C, Ma Y.
16. Dobrow IJ, Kamenetz C, Devlin MJ. Aspectos psiquiátricos da Association of major depression and binge eating disorder
obesidade. Rev Bras Psiquiatr. 2002;24:63-7. with weight loss in a clinical setting. Obesity (Silver Spring).
17. Napolitano MA, Head S, Babyak MA, Blumenthal JA. Binge 2007;15:2557-9.
eating disorder and night eating syndrome: psychological and 32. Geliebter A, Hassid G, Hashim SA. Test meal intake in obese
behavioral characteristics. Int J Eat Disord. 2001;30:193-203. binge eaters in relation to mood and gender. Int J Eat Disord.
18. Bernardi F, Cichelero C, Vitolo MR. Comportamento de re- 2001;29:488-94.
strição alimentar e obesidade. Rev Nutr. 2005;18:85-93. 33. Jirik-Babb P, Geliebter A. Comparison of psychological char-
19. Legenbauer T, De Zwann M, Benecke A, Muhlhans B, Pe- acteristics of binging and nonbinging obese, adult female
trak F, Herpertz S. Depression and anxiety: their predictive outpatients. Eat Weight Disord. 2003;8:173-7.
function for weight loss in obese individuals. Obes Facts. 34. Jirik-Babb P, Norring C. Gender comparisons in psychologi-
2009;2:227-34. cal characteristics of obese, binge eaters. Eat Weight Disord.
20. Sampaio VL. Overweight, obesity and mouth compulsion 2005;10:101-4.
among low income women in the city of Carapicuíba-SP
[tese]. São Paulo: Secretaria da Saúde do Estado de São
Paulo; 2009. Correspondence
21. Associação Nacional de Empresas de Pesquisa. Critério de Margareth da Silva Oliveira
Classificação Econômica Brasil. 2008. www.anep.org.br. Ac- Av. Ipiranga, 6681 - Porto Alegre, RS - Brazil
cessed 2010 Jul 26. E-mail: marga@pucrs.br
92 – Trends Psychiatry Psychother. 2012;34(2)
Вам также может понравиться
- Obesidade Desvendada: Explorando as Raízes e Estratégias para um Estilo de Vida SaudávelОт EverandObesidade Desvendada: Explorando as Raízes e Estratégias para um Estilo de Vida SaudávelОценок пока нет
- Obesidade e TCCДокумент16 страницObesidade e TCCDaniel Nuno Vancetto BorgesОценок пока нет
- Fatores Psicologicos Da Obesidade e Alguns Apontamentos Baseada Na Terapia Do EsquemaДокумент14 страницFatores Psicologicos Da Obesidade e Alguns Apontamentos Baseada Na Terapia Do EsquemaThaís ZancanaroОценок пока нет
- 1613-5630-2-PB Fator Emocional Na ObesidadeДокумент10 страниц1613-5630-2-PB Fator Emocional Na ObesidadegrandemeioОценок пока нет
- 13975Документ5 страниц13975Ana Raíza OliveiraОценок пока нет
- Prevalência e Associação Entre Obesidade e Transtornos MentaisДокумент10 страницPrevalência e Associação Entre Obesidade e Transtornos MentaisLuciene PaivaОценок пока нет
- Bulimia Nervosa - Psicologia Aplicada À NutriçãoДокумент33 страницыBulimia Nervosa - Psicologia Aplicada À NutriçãoSamara IF Técnico NutriçãoОценок пока нет
- PAPER Obesidade e Transtornos MentaisДокумент7 страницPAPER Obesidade e Transtornos MentaisDaniela MouraОценок пока нет
- 24244-Texto Do Artigo-59832-1-2-20231106Документ5 страниц24244-Texto Do Artigo-59832-1-2-20231106Werla SantosОценок пока нет
- Depressao e DisbioseДокумент7 страницDepressao e Disbioseadriele nascimentoОценок пока нет
- Fatores Psicológicos Da Obesidade e Alguns Apontamentos Baseada Na Terapia Do EsquemaДокумент15 страницFatores Psicológicos Da Obesidade e Alguns Apontamentos Baseada Na Terapia Do EsquemaleoziinstyflandoОценок пока нет
- Mcrar, Archi v7 n2 7 - 2018Документ5 страницMcrar, Archi v7 n2 7 - 2018Diana PereiraОценок пока нет
- OriginalESTADO NUTRICIONAL E QUALIDADE DE VIDA EM ADULTOS E IDOSOS COM DEPRESSÃOДокумент12 страницOriginalESTADO NUTRICIONAL E QUALIDADE DE VIDA EM ADULTOS E IDOSOS COM DEPRESSÃOMICHELLY RHAYSSA FREITAS RODRIGUESОценок пока нет
- DownloadДокумент8 страницDownloadcarlaОценок пока нет
- Ansiedade e Impacto NutricionalДокумент7 страницAnsiedade e Impacto Nutricionalkethelen fernandaОценок пока нет
- Aspectos Psicológicos Da Obesidade Mórbida PDFДокумент16 страницAspectos Psicológicos Da Obesidade Mórbida PDFFelipeОценок пока нет
- Estado Nutricional, Comportamento Alimentar e A Prevalencia de Ansiedade e Depressão em Praticantes de Pole Dance - Giovana Figueiredo TCCДокумент25 страницEstado Nutricional, Comportamento Alimentar e A Prevalencia de Ansiedade e Depressão em Praticantes de Pole Dance - Giovana Figueiredo TCCgiovanaОценок пока нет
- Ambulatório Interdisciplinar para o Tratamento Da Obesidade em Pacientes Com Compulsão AlimentarДокумент9 страницAmbulatório Interdisciplinar para o Tratamento Da Obesidade em Pacientes Com Compulsão AlimentarVanessa MarsdenОценок пока нет
- 1982-Texto Do Artigo-8085-1-10-20221117Документ12 страниц1982-Texto Do Artigo-8085-1-10-20221117Fabiane OliveiraОценок пока нет
- Contribuições Da Psicologia e Nutrição para A Mudança Do Comportamento HumanoДокумент9 страницContribuições Da Psicologia e Nutrição para A Mudança Do Comportamento Humanoerica fernandesОценок пока нет
- TCC 2023 O Impacto Dos Transtornos Alimentares em Mulheres AdultasДокумент18 страницTCC 2023 O Impacto Dos Transtornos Alimentares em Mulheres Adultasjoanapassos94Оценок пока нет
- 3086-Texto Do Artigo-8387-12360-10-20210531Документ20 страниц3086-Texto Do Artigo-8387-12360-10-20210531Brenda ChaconОценок пока нет
- TCC NCДокумент23 страницыTCC NCCíntia De Lima De LiraОценок пока нет
- Artigo - CONTRIBUIÇÕES DA PSICOLOGIA EM UM GRUPO DE EMAGRECIMENTO EДокумент15 страницArtigo - CONTRIBUIÇÕES DA PSICOLOGIA EM UM GRUPO DE EMAGRECIMENTO EKelly LiraОценок пока нет
- Perfil Psicológico de Indivíduos Submetidos À Cirurgia BariátricaДокумент20 страницPerfil Psicológico de Indivíduos Submetidos À Cirurgia BariátricaGeremias Soares dos SantosОценок пока нет
- MonografiaДокумент38 страницMonografiaTainara d O P E SantoОценок пока нет
- Modulo 1 - Introducao Da Avaliacao Do EstДокумент14 страницModulo 1 - Introducao Da Avaliacao Do EstDaniОценок пока нет
- Preparação para Cirurgia Bariátrica (R)Документ12 страницPreparação para Cirurgia Bariátrica (R)Antonio Lima0% (1)
- Ansiedade, Tensão Emocional e Consumo PDFДокумент3 страницыAnsiedade, Tensão Emocional e Consumo PDFAna Maria De LimaОценок пока нет
- Depressão e Cirurgia Bariátrica - A Conexão Que ExisteДокумент10 страницDepressão e Cirurgia Bariátrica - A Conexão Que ExistemilafraserОценок пока нет
- TCC e Transtornos AlimentaresДокумент15 страницTCC e Transtornos AlimentaresMilena CristinaОценок пока нет
- E Possibilidades Na Terapia Cognitivo-Comportamental: Um Estudo de Caso de Anorexia Nervosa: DesafiosДокумент13 страницE Possibilidades Na Terapia Cognitivo-Comportamental: Um Estudo de Caso de Anorexia Nervosa: DesafiosLaura SuelenОценок пока нет
- A Importância Da Alimentação Balanceada para o Controle Da Ansiedade e Compulsão AlimentarДокумент26 страницA Importância Da Alimentação Balanceada para o Controle Da Ansiedade e Compulsão AlimentarGlauber RochaОценок пока нет
- Mcrar, Archi v9 n4 - 16 - 2020 - Comunicação RápidaДокумент2 страницыMcrar, Archi v9 n4 - 16 - 2020 - Comunicação Rápidabarbara.araujo57Оценок пока нет
- Percepções de Obesos DeprimidosДокумент20 страницPercepções de Obesos DeprimidosVanessa MaiaОценок пока нет
- Avaliação Clínica Nas Doenças Do Comportamento AlimentarДокумент14 страницAvaliação Clínica Nas Doenças Do Comportamento AlimentarValériaОценок пока нет
- Disturbios Alimentares - DefiniçãoДокумент1 страницаDisturbios Alimentares - DefiniçãoFelipe HerdyОценок пока нет
- A Atuação Do Nutricionista em Grupos de EmagrecimentoДокумент206 страницA Atuação Do Nutricionista em Grupos de EmagrecimentoEliane MoreiraОценок пока нет
- TCC NutriçãoДокумент22 страницыTCC NutriçãoAdm JONN GUILHERME100% (1)
- TCC Nutrição e Dietetica FinalizadoДокумент24 страницыTCC Nutrição e Dietetica FinalizadoBruno RochaОценок пока нет
- TCC 1 Parte (1) .Docx.2.1Документ21 страницаTCC 1 Parte (1) .Docx.2.1Victor HugoОценок пока нет
- TCC e ObesidadeДокумент15 страницTCC e ObesidadeLuara nery costaОценок пока нет
- Renata Patrícia Pinheiro Leite - 0007270 - Thaís Magalhães Diniz - 0006371Документ13 страницRenata Patrícia Pinheiro Leite - 0007270 - Thaís Magalhães Diniz - 0006371Dessa CorreaОценок пока нет
- Diabetes, Perturbações Alimentares e Imagem Corporal em Jovens Adultos: Estudo Exploratório Sobre A DiabulimiaДокумент88 страницDiabetes, Perturbações Alimentares e Imagem Corporal em Jovens Adultos: Estudo Exploratório Sobre A DiabulimiaJuliano BagatinОценок пока нет
- TCC Nutrologia v2Документ18 страницTCC Nutrologia v2Simone Prada KanashiroОценок пока нет
- EstigmaДокумент27 страницEstigmakikaОценок пока нет
- Artigo Imc e RCQДокумент6 страницArtigo Imc e RCQViviane Vilanova RodriguesОценок пока нет
- Depressão, Ansiedade e Estresse e o Comportamento Alimentar: Depression, Anxiety and Stress and Eating BehaviorДокумент8 страницDepressão, Ansiedade e Estresse e o Comportamento Alimentar: Depression, Anxiety and Stress and Eating Behaviorgabriel steffenОценок пока нет
- PDF Bulimia 2018 - Razera Trabalho de Conclusão Da Pós Graduação em PSICOLOGIA POSITIVAДокумент19 страницPDF Bulimia 2018 - Razera Trabalho de Conclusão Da Pós Graduação em PSICOLOGIA POSITIVAGraçaMariaRazeraОценок пока нет
- TCC Psicologia 2023Документ19 страницTCC Psicologia 2023sofiaОценок пока нет
- Psychological Aspects Related To Obesity: Case Report: Aspectos Psicológicos Relacionados À Obesidade: Relato de CasoДокумент8 страницPsychological Aspects Related To Obesity: Case Report: Aspectos Psicológicos Relacionados À Obesidade: Relato de CasoLiliОценок пока нет
- 750-Texto Do Artigo-2902-1-10-20150531 PDFДокумент14 страниц750-Texto Do Artigo-2902-1-10-20150531 PDFAnonymous fPQaCe8Оценок пока нет
- Ativ. Fis., Nutri. Farm. Obes. Rev, Lit.Документ17 страницAtiv. Fis., Nutri. Farm. Obes. Rev, Lit.André P. Lemos FariaОценок пока нет
- Diabetes Mellitus e Transtornos Alimentares: Uma Revisão SistemáticaДокумент11 страницDiabetes Mellitus e Transtornos Alimentares: Uma Revisão Sistemáticarhayssa.vitoriaa09Оценок пока нет
- YASMINДокумент18 страницYASMINcristifeitenОценок пока нет
- Caso Clínico Anorexia NervosaДокумент16 страницCaso Clínico Anorexia NervosaPedro Jardel CoppetiОценок пока нет
- Revista Brasileira de Obesidade, Nutrição e Emagrecimento: ISSN 1981-9919Документ12 страницRevista Brasileira de Obesidade, Nutrição e Emagrecimento: ISSN 1981-9919adriele nascimentoОценок пока нет
- TCC NutriçãoclinicaДокумент12 страницTCC NutriçãoclinicaPriscila VieiraОценок пока нет
- Tese de Mestrado - Catarina Do Carmo Tomas PDFДокумент63 страницыTese de Mestrado - Catarina Do Carmo Tomas PDFMika Sant'anaОценок пока нет
- FICHA Handbook of Emotion RegulationДокумент9 страницFICHA Handbook of Emotion RegulationAna Sofia AlmeidaОценок пока нет
- Tese Univ. Minho - Filipa Vaz 2009Документ134 страницыTese Univ. Minho - Filipa Vaz 2009Ana Sofia AlmeidaОценок пока нет
- A14v27n4 PDFДокумент7 страницA14v27n4 PDFAna Sofia AlmeidaОценок пока нет
- Prada & Garrido 2013 - APAДокумент37 страницPrada & Garrido 2013 - APAantoniojgteixeiraОценок пока нет
- Oliveira, Francisco, & Novo, 2015Документ12 страницOliveira, Francisco, & Novo, 2015Ana Sofia AlmeidaОценок пока нет
- Tic CriançaДокумент12 страницTic CriançaVânia AlvesОценок пока нет
- Desenho Da Árvore - Folha de Registo PDFДокумент1 страницаDesenho Da Árvore - Folha de Registo PDFAna Sofia AlmeidaОценок пока нет
- Teste Do Desenho Família (Louis Corman) + AnexoДокумент15 страницTeste Do Desenho Família (Louis Corman) + AnexoNathalie Ferraz Marques95% (19)
- Era Uma VezДокумент55 страницEra Uma VezAna Sofia AlmeidaОценок пока нет
- Teste Do Desenho Da CasaДокумент18 страницTeste Do Desenho Da CasaAna Sofia Almeida100% (8)
- Folha de Registo CompletaДокумент8 страницFolha de Registo CompletaAna Sofia AlmeidaОценок пока нет
- SGS IiДокумент3 страницыSGS IiAna Sofia Almeida100% (1)
- Teste Do Desenho Da ÁrvoreДокумент34 страницыTeste Do Desenho Da ÁrvoreAna Sofia Almeida100% (7)
- Desenho Da Casa - QuestõesДокумент1 страницаDesenho Da Casa - QuestõesAna Sofia AlmeidaОценок пока нет
- Desenho Da Figura Humana - ManualДокумент58 страницDesenho Da Figura Humana - ManualAna Sofia Almeida92% (25)
- Questionário Desenho Da PessoaДокумент2 страницыQuestionário Desenho Da PessoaAna Sofia AlmeidaОценок пока нет
- Pata Negra - As PranchasДокумент2 страницыPata Negra - As PranchasAna Sofia Almeida100% (2)
- Teste FH - Folha de CorreçãoДокумент6 страницTeste FH - Folha de CorreçãoAna Sofia Almeida100% (1)
- Anorexia Nervosa e Bulimia NervosaДокумент7 страницAnorexia Nervosa e Bulimia NervosalinhamarquesОценок пока нет
- InstruçõesДокумент2 страницыInstruçõesAna Sofia AlmeidaОценок пока нет
- Tic CriançaДокумент12 страницTic CriançaVânia AlvesОценок пока нет
- Analise Do Teste Da Familia PDFДокумент1 страницаAnalise Do Teste Da Familia PDFAna Sofia AlmeidaОценок пока нет
- Manual Práticas Positivas e Colaborativas 2014Документ200 страницManual Práticas Positivas e Colaborativas 2014Catarina RiveroОценок пока нет
- V21s1a03 PDFДокумент6 страницV21s1a03 PDFAninha AraujoОценок пока нет
- Prada & Garrido 2013 - APAДокумент37 страницPrada & Garrido 2013 - APAantoniojgteixeiraОценок пока нет
- APA 6º EdiçãoДокумент28 страницAPA 6º Ediçãosoniae40% (1)
- Competências SociaisДокумент1 страницаCompetências SociaisAna Sofia AlmeidaОценок пока нет
- O Medo A Ansiedade e Suas Pertubações PDFДокумент11 страницO Medo A Ansiedade e Suas Pertubações PDFhercules1111Оценок пока нет
- Anorexia Nervosa e Bulimia NervosaДокумент7 страницAnorexia Nervosa e Bulimia NervosalinhamarquesОценок пока нет
- TCC Apresentaçao - Drywall - Guilherme Candido FerreiraДокумент9 страницTCC Apresentaçao - Drywall - Guilherme Candido FerreiraGustavo SilvaОценок пока нет
- Exercícios de ANOVA Modelo de Blocos AleatóriosДокумент4 страницыExercícios de ANOVA Modelo de Blocos AleatóriosHelcio RochaОценок пока нет
- Análise de DocumentosДокумент2 страницыAnálise de Documentosteresaamatos100% (1)
- Fontes de Informação CredíveisДокумент2 страницыFontes de Informação CredíveislilapОценок пока нет
- Ir 005 - Alfa Laval - PC 4509436955Документ4 страницыIr 005 - Alfa Laval - PC 4509436955Marcelo PiresОценок пока нет
- Exercícios Ias 38Документ3 страницыExercícios Ias 38janaina.limacontabeis12Оценок пока нет
- Un 4 - EntomologiaДокумент4 страницыUn 4 - EntomologiaEmmanuel CecchettoОценок пока нет
- Descrição de CargosДокумент5 страницDescrição de CargosJoão Vitor GodinhoОценок пока нет
- Análise de Documentos Enviados para Pós (Candidatos (As) )Документ58 страницAnálise de Documentos Enviados para Pós (Candidatos (As) )Luan SantosОценок пока нет
- Residuo de UvaДокумент27 страницResiduo de UvaBeatriz MirandaОценок пока нет
- Conceitos de Caminhabilidade e Estudo Aplicado em Praça Pública de Palmas TOДокумент64 страницыConceitos de Caminhabilidade e Estudo Aplicado em Praça Pública de Palmas TOFabricio Cicero Nunes da SilvaОценок пока нет
- Tic - Técnicas Dos Incidentes Críticos - Rev01Документ11 страницTic - Técnicas Dos Incidentes Críticos - Rev01Izabel Maria GoulartОценок пока нет
- Tese Ariel Tavares PereiraДокумент345 страницTese Ariel Tavares PereiraAriel Tavares Pereira100% (1)
- Texto 1 - Ética em Pesquisa CientíficaДокумент13 страницTexto 1 - Ética em Pesquisa CientíficaComoCuОценок пока нет
- Ementa Completa - Matecraftrando ProntoДокумент3 страницыEmenta Completa - Matecraftrando Prontorecarbeda100% (1)
- The Power of FeedbackДокумент32 страницыThe Power of FeedbackAna Claudia Candido de OliveiraОценок пока нет
- 469-Texto Do Artigo-1530-1-10-20190424Документ23 страницы469-Texto Do Artigo-1530-1-10-20190424Maria Eugênia Alvares Mantovani SneiderisОценок пока нет
- TrabmodeloДокумент3 страницыTrabmodelogabrirlОценок пока нет
- SLIDE PRONTO - Controle EstratégicoДокумент35 страницSLIDE PRONTO - Controle EstratégicoAna VictóriaОценок пока нет
- PG Damec 2018 1 19Документ57 страницPG Damec 2018 1 19Luana PereiraОценок пока нет
- Monografia - David CaetanoДокумент109 страницMonografia - David CaetanoDavid CaetanoОценок пока нет
- Aula3 PDFДокумент10 страницAula3 PDFIngryd BraynerОценок пока нет
- Pesquisa Qualitativa - AtividadeДокумент6 страницPesquisa Qualitativa - AtividadeAlexandre Henrique ProcópioОценок пока нет
- Deivy Ferreira Carneiro - Maíra Ines Vendrame - Espaços, Escalas e Práticas Sociais Na Micro-História italiana-FGV Editora (2021)Документ284 страницыDeivy Ferreira Carneiro - Maíra Ines Vendrame - Espaços, Escalas e Práticas Sociais Na Micro-História italiana-FGV Editora (2021)Larisse EliasОценок пока нет
- Quais As Métrica Sutilizadas Pelos RobôsДокумент2 страницыQuais As Métrica Sutilizadas Pelos RobôsTiago RibeiroОценок пока нет
- CegosurdezДокумент337 страницCegosurdezCamila CostaОценок пока нет
- Conservação de Colecoes Indigenas Mara Lucia CarretДокумент335 страницConservação de Colecoes Indigenas Mara Lucia CarretHelena SouzaОценок пока нет
- Você É o Problema, Você É A Solução - Ricardo AlvesДокумент129 страницVocê É o Problema, Você É A Solução - Ricardo AlvesMARCO PEREIRAОценок пока нет
- Eduardo Fonseca Maciel - A. Seeger: Uma Criança No MundoДокумент1 страницаEduardo Fonseca Maciel - A. Seeger: Uma Criança No MundoEduardo F. MacielОценок пока нет
- Ética Humanista e Educação Do AmorДокумент53 страницыÉtica Humanista e Educação Do Amorgasantos7Оценок пока нет