Академический Документы
Профессиональный Документы
Культура Документы
Aspergillus, Cryptococcus, and Pneumocystis) .: Small Animal Internal Medicine For Veterinarian Technisi
Загружено:
Anonymous wU5gfKUОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Aspergillus, Cryptococcus, and Pneumocystis) .: Small Animal Internal Medicine For Veterinarian Technisi
Загружено:
Anonymous wU5gfKUАвторское право:
Доступные форматы
Pneumonia
Pneumonia is defined as an inflammatory disease of the terminal airways and pulmonary interstitium. It is
important to recognize that pneumonia has many etiologies. Too often, the term “pneumonia” is used
inappropriately as a synonym for bacterial pneumonia, and clinical findings indicative of pneumonia are
erroneously ascribed to bacterial infection. Infectious agents that may cause pneumonia include bacteria
(including rickettsial agents), viruses (canine distemper virus, canine influenza virus, CAV-2, canine PIV,
feline herpesvirus, feline calicivirus), protozoa (Toxoplasma, Neospora), respiratory parasites
(Paragonimus, Aelurostrongylus, Filaroides), and fungi (Blastomyces, Histoplasma, Coccidioides,
Aspergillus, Cryptococcus, and Pneumocystis).
Some viral agents predispose to secondary bacterial pneumonia (canine distemper virus, canine PIV,
FeLV, and FIV). Noninfectious forms of pneumonia include aspiration pneumonia, pneumonia secondary
to smoke inhalation, and lipid pneumonia (exogenous lipid pneumonia from aspiration of fatty substances
or endogenous lipid pneumonia related to lipid release from breakdown of pulmonary tissues).
Appropriate treatment of pneumonia requires identification of the specific etiology, including identification
of specific organisms and their antimicrobial sensitivities in bacterial disease.
Bacterial pneumonia is considered a secondary condition that is established following some other
pathological insult that impairs the natural defense mechanisms of the lung. Infection is usually
associated with resident respiratory flora, although hematogenous spread is another potential source of
bacteria (Enterococcus), and most cases of pneumonia involve more than one bacterial agent
(polymicrobial). Common agents include Streptococcus, Staphylococcus, E. coli, Pasteurella, Klebsiella
Pseudomonas, Bordetella, and Mycoplasma. Samples for bacterial culture and sensitivity can be
collected by TTW, BAL, or lung aspirate. Empiric antibacterial therapy using broad-spectrum drugs with
good respiratory distribution should be initiated pending culture results. A combination of (1) an
aminopenicillin or a first-generation cephalosporin and (2) a fluoroquinolone or an aminoglycoside
provides a rational empiric choice. Parenteral administration of drugs is advised for patients with severe
hypoxemia that may secondarily impair gut function and absorption of orally administered drugs. Aerosol
administration of antibiotics is not recommended. Response to treatment is monitored by sequential
thoracic radiographs ± ABG determination and antibacterial drugs are continued until 1–2 weeks past
resolution of clinical and radiographic evidence of disease.
Other forms of infectious pneumonia are also treated as indicated for the specific causative agent (i.e.,
long-term [months] administration of oral antifungal drugs with or without a course of injectable antifungal
drug for fungal pneumonia; clindamycin or trimethoprim–sulfa with or without pyrimethamine for protozoal
pneumonia). Patients with infectious or noninfectious pneumonia will often require general treatment
measures such as oxygen supplementation, fluid therapy, nebulization, and coupage. Use of
bronchodilators and mucolytics in the treatment of pneumonia is controversial.
Small animal internal medicine for veterinarian technisi
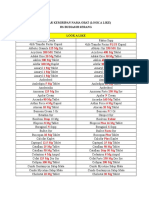
Вам также может понравиться
- Microbiology NotesДокумент3 страницыMicrobiology NotesAthena Huynh100% (1)
- Chapter 19 Practice Multiple ChoiceДокумент8 страницChapter 19 Practice Multiple Choicekiden300% (1)
- The Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis ResearchДокумент29 страницThe Professional Assassination of Autism Expert Lisa Blakemore-Brown Medical Misdiagnosis Researchapi-246003035Оценок пока нет
- Capture D'écran . 2021-08-15 À 09.21.56Документ108 страницCapture D'écran . 2021-08-15 À 09.21.56Juan VasquezОценок пока нет
- Pneumonia 3Документ8 страницPneumonia 3janinecasilenОценок пока нет
- Pneumonia With Pleural EffusionДокумент24 страницыPneumonia With Pleural EffusionMund CheleОценок пока нет
- Mechanism of Action For Each Class of AntiДокумент146 страницMechanism of Action For Each Class of AntiReynaldo RiveraОценок пока нет
- Microbial Diseases of The Respiratory SystemДокумент30 страницMicrobial Diseases of The Respiratory SystemChristopher Eria Santiañez0% (1)
- Roosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results SurveyДокумент4 страницыRoosendaal Study of Vaccinated vs. Unvaccinated Children in The Netherlands: Results Surveythomas_austin_189% (9)
- Case Study PcapДокумент3 страницыCase Study PcapClaire PalaciosОценок пока нет
- Chapter 1Документ30 страницChapter 1Ayro Business CenterОценок пока нет
- PneumoniaДокумент79 страницPneumoniaEjiro OnoroОценок пока нет
- Pneumonia CHN Case ReportДокумент6 страницPneumonia CHN Case ReportRhaine MagtotoОценок пока нет
- Definition of PneumoniaДокумент4 страницыDefinition of PneumoniaEmylia Ananda PutriОценок пока нет
- Addis Ababa University: Collage of Health Science Pediatrics and Neonatology On PneumoniaДокумент21 страницаAddis Ababa University: Collage of Health Science Pediatrics and Neonatology On PneumoniaCheru DugaseОценок пока нет
- Bacterial Pneumonia in Cattle - Respiratory System - Veterinary ManualДокумент4 страницыBacterial Pneumonia in Cattle - Respiratory System - Veterinary ManualMutiara DarisОценок пока нет
- PneumoniaДокумент5 страницPneumoniasamtaynbОценок пока нет
- Probiotics in Respiratory Virus Infections: ReviewДокумент14 страницProbiotics in Respiratory Virus Infections: ReviewErik Jaya GunawanОценок пока нет
- Pneumonia, BronchiolitisДокумент65 страницPneumonia, BronchiolitisYemata HailuОценок пока нет
- LRTI and KDДокумент14 страницLRTI and KDjomerdalonaОценок пока нет
- Practice Essentials: Essential Update: Telavancin Approved For Bacterial PneumoniaДокумент12 страницPractice Essentials: Essential Update: Telavancin Approved For Bacterial PneumoniaAnnette CraigОценок пока нет
- Lec 9 Respiratory Disorders Part 2Документ11 страницLec 9 Respiratory Disorders Part 2iam2117Оценок пока нет
- CH 11 PneumoniaДокумент18 страницCH 11 PneumoniaBader AljarboaОценок пока нет
- Acute PharyngitisДокумент3 страницыAcute PharyngitisMohammed Taha Al-nuaimyОценок пока нет
- Bacterial Atypical (Interstitial) PneumoniaДокумент24 страницыBacterial Atypical (Interstitial) Pneumoniamailkammar967Оценок пока нет
- 2 Microbial Disease of The Respiratory SystemДокумент63 страницы2 Microbial Disease of The Respiratory Systemrandom stuffОценок пока нет
- Epidemiology, Pathogenesis, and Microbiology of Community-Acquired Pneumonia in AdultsДокумент19 страницEpidemiology, Pathogenesis, and Microbiology of Community-Acquired Pneumonia in AdultsRubén RodríguezОценок пока нет
- Guidelines For The Evaluation and Treatment of PneumoniaДокумент19 страницGuidelines For The Evaluation and Treatment of PneumoniaBayu Suryadi100% (1)
- Pneumonia (Handout) EditДокумент27 страницPneumonia (Handout) EditEveline YОценок пока нет
- MICROMIDTERMSLABДокумент27 страницMICROMIDTERMSLABmicaellaabedejosОценок пока нет
- CommunityДокумент2 страницыCommunityRonald Anthony TobiasОценок пока нет
- 04 Acute Bronchitis and Pneumonia in ChildrenДокумент58 страниц04 Acute Bronchitis and Pneumonia in ChildrenMi PatelОценок пока нет
- Pneumonia Is An: ClinicalДокумент13 страницPneumonia Is An: ClinicaldfgsfsfssdОценок пока нет
- Etiology: M Tuberculosis Is A Slow-Growing, Obligate Aerobe and A Facultative, Intracellular Parasite. TheДокумент5 страницEtiology: M Tuberculosis Is A Slow-Growing, Obligate Aerobe and A Facultative, Intracellular Parasite. TheFerdi StefiyanОценок пока нет
- tmp7F77 TMPДокумент9 страницtmp7F77 TMPFrontiersОценок пока нет
- PneumoniaДокумент2 страницыPneumoniaMargaret EricksonОценок пока нет
- Pneumonia: Anjitha JosephДокумент43 страницыPneumonia: Anjitha JosephanjithaОценок пока нет
- Classification of PneumoniaДокумент3 страницыClassification of PneumoniaRobelОценок пока нет
- PneumoniaДокумент18 страницPneumoniaFryam Bells100% (1)
- Mycoplasma Infect The Upper Respiratory Tract and Can Cause Pneumonia. Pneumonia Is AnДокумент11 страницMycoplasma Infect The Upper Respiratory Tract and Can Cause Pneumonia. Pneumonia Is AnJenny TaylorОценок пока нет
- Consequences of Cov-19 Infection 2Документ15 страницConsequences of Cov-19 Infection 2MustafaОценок пока нет
- PneumoniaДокумент8 страницPneumoniaCostescu ClaudiaОценок пока нет
- Pneumonia 1Документ17 страницPneumonia 1Jonathan katanaОценок пока нет
- Updated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHДокумент42 страницыUpdated: Dec 07, 2016 Author: Justina Gamache, MD Chief Editor: Guy W Soo Hoo, MD, MPHgita suci arianiОценок пока нет
- Microbiology:: Parasites (Parasitic Pneumonia)Документ5 страницMicrobiology:: Parasites (Parasitic Pneumonia)9t6vx7psm5Оценок пока нет
- Listeria Monocytogenes Escherichia Coli: Signs and SymptomsДокумент15 страницListeria Monocytogenes Escherichia Coli: Signs and SymptomsPuput's BourboneОценок пока нет
- Aspiration PneumoniaДокумент16 страницAspiration PneumoniaFeni DianiОценок пока нет
- Pediatric Community-Acquired Pneumonia: Nelson 20 EdДокумент43 страницыPediatric Community-Acquired Pneumonia: Nelson 20 EdRazel Kinette AzotesОценок пока нет
- PneumoniaДокумент5 страницPneumoniaAbubakr AurangzebОценок пока нет
- Upper Respiratory Tract InfectionДокумент3 страницыUpper Respiratory Tract Infectionmcvirgo014100% (1)
- Lec. 3 Pulmonary Infections. SaifДокумент19 страницLec. 3 Pulmonary Infections. Saifs2111110520Оценок пока нет
- Bacterial PneumoniaДокумент6 страницBacterial PneumoniaIrsa SevenfoldismОценок пока нет
- Respiratory Specimen Collection and ProcessingДокумент20 страницRespiratory Specimen Collection and ProcessingJose Adan Vazquez MoralesОценок пока нет
- Respiratory Tract Bacterial Infection Etiological Agents and Susceptibility TestingДокумент8 страницRespiratory Tract Bacterial Infection Etiological Agents and Susceptibility TestingDoyoxОценок пока нет
- Wae'l Hayajneh: PneumoniaДокумент14 страницWae'l Hayajneh: PneumoniaRashed ShatnawiОценок пока нет
- Nosocomial InfectionДокумент57 страницNosocomial InfectionFaith Ho100% (1)
- Nosocomial Pneumonia Nosocomial PneumoniaДокумент37 страницNosocomial Pneumonia Nosocomial PneumoniaAjay AgrawalОценок пока нет
- Bacteria Infection of The Respiratory TractДокумент8 страницBacteria Infection of The Respiratory TractChidi EmmanuelОценок пока нет
- Pneumonia Definations & ClassificationsДокумент29 страницPneumonia Definations & ClassificationsJimitОценок пока нет
- Clinical Presentation and Diagnosis of Pneumocystis Pulmonary Infection in HIVДокумент42 страницыClinical Presentation and Diagnosis of Pneumocystis Pulmonary Infection in HIVmariano villavicencioОценок пока нет
- An Overview of Respiratory Diseases in Pets: Review ArticleДокумент3 страницыAn Overview of Respiratory Diseases in Pets: Review ArticlerianperoОценок пока нет
- Jurnal Bahasa InggrisДокумент12 страницJurnal Bahasa InggrisVanessa Angelica SitepuОценок пока нет
- Micro Chap 19Документ30 страницMicro Chap 19Farah ZahidОценок пока нет
- Primer-Hypersensitivity PneumonitisДокумент19 страницPrimer-Hypersensitivity PneumonitisMary CogolloОценок пока нет
- Reading Article (Pedia)Документ2 страницыReading Article (Pedia)Babon , Christelle Anne S.Оценок пока нет
- How Soon Can You Drink Alcohol After Getting Your Covid-19 Vaccine - SA Corona Virus Online PortalДокумент1 страницаHow Soon Can You Drink Alcohol After Getting Your Covid-19 Vaccine - SA Corona Virus Online PortalArjay GudoyОценок пока нет
- Laboratory Associated Infections: Tania Chintya IKD BiomedikДокумент16 страницLaboratory Associated Infections: Tania Chintya IKD BiomedikTania Chintya Dewi KarimaОценок пока нет
- Brazilian Case Study PCV-2 Vaccine Plus DenagardДокумент4 страницыBrazilian Case Study PCV-2 Vaccine Plus Denagardnick224Оценок пока нет
- Managing Acute Meningitis: HistoryДокумент37 страницManaging Acute Meningitis: HistoryMhelshy VillanuevaОценок пока нет
- 1418Документ19 страниц1418mehanakjafhhaifhiassfОценок пока нет
- Upsc CMS 2008Документ52 страницыUpsc CMS 2008Vaibhav BharatОценок пока нет
- Premera Preventative Benefits PDFДокумент5 страницPremera Preventative Benefits PDFlindytindylindtОценок пока нет
- Certificate For COVID-19 Vaccination: Beneficiary DetailsДокумент1 страницаCertificate For COVID-19 Vaccination: Beneficiary DetailsaravindОценок пока нет
- JKNKLKLДокумент10 страницJKNKLKLCyntia AndrinaОценок пока нет
- 9700 w14 QP 22Документ16 страниц9700 w14 QP 22rashmi_harryОценок пока нет
- AssessmentДокумент2 страницыAssessmentelishaОценок пока нет
- Taguibo HighlightsДокумент160 страницTaguibo HighlightsMitzi LabisОценок пока нет
- Kansas KCI Form B Medical ExemptionДокумент1 страницаKansas KCI Form B Medical ExemptionDonnaОценок пока нет
- Urn Uvci 01 Ro 230dmyqx5erjr4dg9xj719kv6wop8l#Документ2 страницыUrn Uvci 01 Ro 230dmyqx5erjr4dg9xj719kv6wop8l#dianabanuОценок пока нет
- Infection Control Guidance For EMS ProvidersДокумент41 страницаInfection Control Guidance For EMS ProvidersNicholaiCabadduОценок пока нет
- 3RD Quarter - Melc 2Документ5 страниц3RD Quarter - Melc 2Jennica Roz Fronda-CastroОценок пока нет
- Pathogenesis of Type 1 Diabetes MellitusДокумент28 страницPathogenesis of Type 1 Diabetes MellitusJuan Diego Fernández MurielОценок пока нет
- In Re Strahilevitz - Uses of Example in SpecificationДокумент7 страницIn Re Strahilevitz - Uses of Example in SpecificationJorel Andrew FlautaОценок пока нет
- EprДокумент68 страницEprAnonymous 6OPLC9UОценок пока нет
- List High AlertДокумент11 страницList High Alertputiasri85Оценок пока нет
- Fast Chicken Pox Cure PDF-eBook, Stefan HallДокумент46 страницFast Chicken Pox Cure PDF-eBook, Stefan HallCyrusОценок пока нет
- Swine ErysipelasДокумент31 страницаSwine Erysipelaslea0% (1)
- Fever and RashДокумент14 страницFever and RashwirdahajaОценок пока нет
- Bulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Документ6 страницBulacan State University College of Nursing: Bulsu-Op-Con-23F15 Revision: 0Richmon SantosОценок пока нет