Академический Документы
Профессиональный Документы
Культура Документы
Original Research Paper: Gastroenterology
Загружено:
Afkar30Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Original Research Paper: Gastroenterology
Загружено:
Afkar30Авторское право:
Доступные форматы
Volume : 3 | Issue
VOLUME-6, : 11 | JULY-2017
ISSUE-7, November 2014 • ISSN
• ISSN No 2277
No 2277 - 8179
- 8160 IF : 4.547 | IC Value 80.26
Original Research Paper Gastroenterology
POST CHOLECYSTECTOMY SYNDROME AFTER LAPAROSCOPIC
CHOLECYSTECTOMY- A PROSPECTIVE STUDY
Additional Professor, Department of General Surgery, Government Medical
Dr Sulfekar M S College, Trivandrum
Dr Azeem Mohamed Senior Resident, Department of General Surgery, Government Medical College,
Bashir Trivandrum
Dr Aravind S Junior Resident, Department of General Surgery, Government Medical College,
Ganapath Trivandrum
ABSTRACT Post cholecystectomy syndrome has been used to signify the heterogeneous group of disorders affecting patients
who continue to complain of symptoms after cholecystectomy. It is not really a syndrome and the term is
confusing. Today it has become a melting pot of various postoperative syndromes of mostly obscure origin. In about half the cases treated
by cholecystectomy, cholecystectomy leaves certain problems of digestive dysfunction (dyspeptic-pain syndrome) unresolved. This study
was done to study Symptoms of postcholecystectomy syndrome in patients after laparoscopic cholecystectomy and to nd the proportion
of patients get cured of the pre operative symptoms after surgery. Patients admitted in surgical wards of Government Medical College
Trivandrum for laparoscopic cholecystectomy fo a period of one year were enrolled into the study. The mean age of the patients was
42.8years. There were 23 females and 9 male giving a ratio 1: 2.5. The most common symptoms preoperatively were abdominal pain, pain
related to food intake, nausea, dyspepsia, and vomiting. Symptom of dyspepsia, abdominal bloating and increased atulence were present
in only half the patients. In all, none of the patients suffered from jaundice. All the preoperative symptoms were signi cantly improved after
laparoscopic cholecystectomy. 23 patients had complete absence of symptoms postoperatively. The most common symptoms post
operatively were pain related to food, abdominal pain, nausea and bloating. There were no new symptoms developed after laparoscopic
cholecystectomy.
KEYWORDS : - post cholecystectomy syndrome, laparoscopic cholecystectomy
Introduction PCS is also the development of symptoms, such as gastritis and
Laparoscopic cholecystectomy is the standard treatment for diarrhea, caused by removal of the gallbladder3. It is thought to be
symptomatic gall stone disease1. This study aimed to assess the the cause of PCS in patients with mild gastro duodenal symptoms or
effect of the operation on patients' symptoms. diarrhea. Removal of the reservoir function of the gallbladder alters
bile ow and the enterohepatic circulation of bile5.
Since its introduction by Eric Muhe in 1987, laparoscopic
cholecystectomy has rapidly gained in popularity and is now Absence of the gallbladder, on its own, i.e., cholecystectomy per se
considered the treatment of choice for symptomatic gallstone has not been reported to impair intestinal digestion or absorption.
disease. The advantages over laparoscopic cholecystectomy As a matter of fact there is a congenital anomaly known as agenesis
include reduced postoperative hospitalization, reduced pain and of the gallbladder and cystic duct which does occur, although
morbidity, better cosmesis and considerable nancial savings. uncommonly, and patients with this anomaly have not been
reported to suffer any digestive or absorption problems. It is a well
Gallstones are associated with a wide variety of symptoms. These known fact that the gallbladder acts as a volume reservoir,
include abdominal pain, pain related to fatty foods, nausea and collecting the bile produced by the liver and releasing it when
vomiting as well as dyspepsia, required, i.e. after a meal. Functional consequences related to this
property are rare following cholecystectomy because the loss of the
abdominal bloating and increased atulence2. A few patients gallbladder is compensated for by the biliary tree which has been
continue to have gastrointestinal symptoms after laparoscopic shown to be dilated following cholecystectomy.
cholecystectomy. The term 'postcholecystectomy syndrome' has
been used to describe this condition although the term 'persistent Gallstone patients have a higher tendency to duodenogastric re ux
postcholecystectomy symptoms' is a more accurate description3. of bile acid. This tendency is further increased by removal of a
The repor ted incidence of persistent symptoms af ter functioning gallbladder (but not a nonfunctioning gallbladder). The
cholecystectomy varies widely. Studies on the symptomatic overall incidence of positive endoscopic and histopathologic
outcome after laparoscopic cholecystectomy have reported changes in stomach of cholecystectomized patients is 20-30%
successful relief of symptoms in 70% to 95% of patients but the especially signi cant is the atrophic type of gastritis. With the
characteristics of patients who continue to experience pain passage of time following cholecystectomy, manifestations of
after surgery is poorly de ned4.In 1947, Womack and Crider rst chronic duodenal obstruction become advanced. This results in an
described PCS, de ning it as the presence of symptoms after increase in the incidence of gastroduodenal re ux and decreased
cholecystectomy. These symptoms may actually represent either acid forming function of the stomach.
(1) the continuation of symptoms that had been interpreted as Only 30% of patients with gallstones come to surgery6, which
resulting from pathology of the gallbladder means that asymptomatic gallstones are common. Chronic
or cholecystitis, the commonest indication for cholecystectomy, it is
found that the only symptom entirely characteristic of chronic
(2) the development of new symptoms that might normally be cholecystitis is biliary colic 11 . If all patients with gallstones are
attributed to the gallbladder. operated on, we will surely end up with a high incidence of PCS.
Those with no symptoms at all may complain of symptoms related
The usual and most common cause of PCS is incorrect preoperative to the operation or its complications and those with symptoms of
diagnosis. other systems will continue to complain of their initial symptoms
14 X GJRA - GLOBAL JOURNAL FOR RESEARCH ANALYSIS
IF : 4.547 | IC Value 80.26 Volume : 3 | Issue
VOLUME-6, : 11 | November
ISSUE-7, 2014
JULY-2017 • ISSN
• ISSN NoNo 2277- 8160
2277 - 8179
and all will be considered PCS. 1. McNemarChi – square test
2. Paired T- test
ERCP manometry is recommended in postcholecystectomy Sample size
patients with unexplained abdominal pain of pancreaticobiliary Sample size was calculated using the formula
origin . Some have shown that patients with PCS have hypertonic N = (Za/2 + Z1-b)2 [P1(100-P1) +P2(100-P2)
dyskinesia of the sphincter of Oddi, i.e. deep and wide waves (P1 - P2)2
superimposed on high basal pressures of the sphincter. Endoscopic P1= proportion of patients having the symptoms pre operatively
manometry at the sphincter of Oddi enabled many of the P2 = proportion of patients having the same symptom post
unclari ed postcholecystectomy symptoms to be identi ed. In up operatively
to 30% of cases of PCS, functional disturbances of the sphincter are (Za/2 + Z1-b)2 =7.9 , if a = 0.05
responsible for the clinical picture . While others insist that patients , b = 0.2
with sphincter of Oddi dysfunction have no greater pressure rise in
the CBD after morphine than do asymptomatic cholecystectomized The symptom with least prevalence is taken, to get maximum
controls and a given rise in pressure might precipitate pain in a sample size.
patient with sphincter of Oddi dysfunction but not in a normal
control subject which means that these patients might have a The study 'Postcholecystectomy Syndrome After
greater pain sensitivity to a given rise in pressure in the CBD . Laparoscopic Cholecystectomy' by M Akthar Quresi et al conducted
among 100 cases of patients under went laparoscopic
Treatment of this condition is a controversial area with lack of cholecystectomy showed the symptom with least prevalence was
de nitive evidence for cure by any form of treatment. Medical atulence . Proportion of patients who had atulence pre-
treatment includes cisapride, ursodeoxy cholic acid, sublingual operatively ( P1 ) was 39 and proportion of patients who had the
nitroglycerine, nifedipine, endoscopic sphincterotomy and same symptom post operatively ( P2 ) was 10.
sphincteroplasty.
Using these values in the formula Sample size, N = 31
Aims of the study
PRIMARY: VARIABLES STUDIED
1. To study Symptoms of postcholecystectomy syndrome in 1. Age
patients after laparoscopic cholecystectomy . 2. Sex
3. History of addictions (smoking, alcoholism, iv abuser)
2. To nd the proportion of patients get cured of the pre operative 4. Any other comorbities present
symptoms after surgery. 5. History of previous surgery
6. Treatment history, intake of oral contraceptive pills
SECONDARY 7. Vital signs
To study the duration of each symptoms following laparoscopic
cholecystectomy. Results
All the patients contacted agreed to participate in the study.
Methodology The mean age of the patients was 42.8years. There were 23 females
Research design: Hospital based Prospective cohort study and 9 male giving a ratio 1: 2.5.
Study setting :
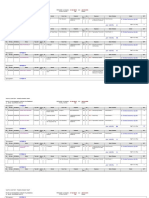
The results in the table no:1 summarize the pre and post operative
Department of General surgery Government medical college, symptoms of 32 patients in the study.
Thiruvananthapuram
The most common symptoms preoperatively were abdominal pain,
Study population : pain related to food intake, nausea, dyspepsia, and vomiting.
Pa t i e n t s a d m i t t e d i n s u rg i c a l w a rd s fo r l a p a ro s c o p i c
cholecystectomy Study period : 12 months after getting clearance Symptom of dyspepsia, abdominal bloating and increased
from the Ethical committee atulence were present in only half the patients.
Inclusion criteria: In all, none of the patients suffered from jaundice. All the
All patients admitted in general surgery ward for laparoscopic preoperative symptoms were signi cantly improved after
cholecystectomy laparoscopic cholecystectomy. 23 patients had complete absence
of symptoms postoperatively. The most common symptoms post
Exclusion criteria : operatively were pain related to food, abdominal pain, nausea and
Patients not giving consent bloating.
Patient Undergoing open cholecystectomy
There were no new symptoms developed after laparoscopic
Study Tools : cholecystectomy.
Structured proforma
Informed consent Gallbladder specimen examination:
Histology of the gallbladder showed that 85% had chronic and 10%
Study Procedure : sub acute in ammation while 5% were normal. Bacteriology was
Patients ful lling the inclusion criteria were enrolled into the study not done. Stone type was not examined.
and evaluation and recording in a preformed proforma of the Symptoms Improvement after 6weeks
following were done after getting a written informed consent.
Abdominal pain 87.96%
Statistical analysis : Pain on food intake 91.93%
1. Qualitative data was analysed using proportions Nausea 92.25%
Vomiting 100%
2. Quantitative data was analysed using mean, median and standard
deviation Statistical methods applied : Dyspepsia 100%
GJRA - GLOBAL JOURNAL FOR RESEARCH ANALYSIS X 15
Volume : 3 | Issue
VOLUME-6, : 11 | JULY-2017
ISSUE-7, November 2014 • ISSN
• ISSN No 2277
No 2277 - 8179
- 8160 IF : 4.547 | IC Value 80.26
Bloating 93.39%
atulence 100%
Jaundice 100%
Fever 100%
Rigor 100%
TABLE:1 IMPROVEMENT OF SYMPTOMS AFTER 6 WEEKS
Discussion
The result of this analysis demonstrate that laparoscopic
cholecystectomy is an effective treatment for symptomatic gall
stone disease , 78.1% of patients were completely free of symptoms
after laparoscopic cholecystectomy. Of the 22% patients who had
persistence of symptoms only few had one symptom which did not
interfere with their lifestyle. Thus 85% of patients had good
outcome after laparoscopic cholecystectomy in this study.
The symptoms described by the patients with gall stones also occur
in a number of other conditions such as peptic ulcer, re ux
oesophagitis, pancreatitis and irritable bowel syndrome. Thus it may
be difficult to attribute the patients symptoms conclusively to gall
stone and persistence of symptoms has been documented in 30%to
50% of patients after classical cholecystectomy is followed by a
persistence of symptoms in a similar manner.
Removal of gall bladder is associated with several physiological
change in the upper gastrointestinal tract which may account for
the persistence of symptoms or the development of new symptoms
after cholecystectomy. The cholecystosphincter of oddi re ex
,cholecystoantral re ex and cholecysto-oesophageal re ex are all
disrupted and a number of local upper gastrointestinal hormonal
changes also occur after cholecystectomy. Thus there is an
increased incidence of gastritis,alkaline guodenogastric re ux and
gastro esophageal re ux after cholecystectomy.
In all, patients who continued to have at least two symptoms
postoperatively and this correlates with patient satisfaction with the
procedure. Most patients returned to full activity within 6 weeks:
however this did not correlate with number of postoperative
symptoms .
Histology of the gallbladder showed that 85% had chronic and 10%
subacute in ammation while 5% were normal. Bacteriology was not
done. Stone type was not examined.
Conclusion
Laparoscopic cholecystectomy is an effective treatment for
symptomatic gall stone disease. 85% of patients had good outcome
after laparoscopic cholecystectomy in this study. Most patients
returned to full activity within 6 weeks.
Bibliography
1. Maingot's Abdominal Operations, 11th edition
2. Bailey and Love's Short Practice of Surgery 25th edition .
3. Sabiston Text Book of Surgery 19th edition.
4. Barthet M., Affriat C., Bernard J.P. et al. Is biliary lithiasis associated with
pancreatographic changes? Gut. 1995; 36(5): 761-765.
5. Schmalz MJ, Geenen JE, Hogan WJ, Dodds WJ, Venu RP, Johnson GK. Pain on
common bile duct injection during ERCP: does it indicate sphincter of Oddi
dysfunction? Gastrointest Endosc 199036(5):458-61.
6. Tanaka M, Ikeda S, Nakayama F. Change in bile duct pressure responses after
cholecystectomy: Loss of gallbladder as a pressure reservoir. Gastroenterology
1984;87(5):1154-9.
16 X GJRA - GLOBAL JOURNAL FOR RESEARCH ANALYSIS
Вам также может понравиться
- Acute Intestinal ObstructionДокумент9 страницAcute Intestinal ObstructionRoxana ElenaОценок пока нет
- Adhesive Small Bowel Adhesions Obstruction: Evolutions in Diagnosis, Management and PreventionДокумент24 страницыAdhesive Small Bowel Adhesions Obstruction: Evolutions in Diagnosis, Management and PreventionEunikeSetiyantoWijayaОценок пока нет
- Peustow ArticleДокумент6 страницPeustow ArticleAjay GujarОценок пока нет
- 20 Iunie 2017Документ3 страницы20 Iunie 2017Radu MiricaОценок пока нет
- Complicacion Enteros Clinics 2015Документ13 страницComplicacion Enteros Clinics 2015Yoeli Marisa Escandon EspinozaОценок пока нет
- Annals of Medicine and Surgery: Case ReportДокумент4 страницыAnnals of Medicine and Surgery: Case ReportDimas ErlanggaОценок пока нет
- A Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionДокумент6 страницA Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionSantosh BabuОценок пока нет
- Surgery Case Write UpДокумент8 страницSurgery Case Write UpKaarthigan RamaiahОценок пока нет
- Volume 15, Number 5 May 2011Документ188 страницVolume 15, Number 5 May 2011Nicolai BabaliciОценок пока нет
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueДокумент3 страницыGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghОценок пока нет
- Minimally Invasive Surgery: Amar Shah and Anirudh ShahДокумент5 страницMinimally Invasive Surgery: Amar Shah and Anirudh ShahKadelsy BristolОценок пока нет
- Atlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueОт EverandAtlas of Laparoscopic Gastrectomy for Gastric Cancer: High Resolution Image for New Surgical TechniqueОценок пока нет
- Chronic Gastric Volvulus With Diaphragmatic 2024 International Journal of SДокумент5 страницChronic Gastric Volvulus With Diaphragmatic 2024 International Journal of SRonald QuezadaОценок пока нет
- Dr.R.Durai Ms Assisstant Professor Department of General Surgery MgmcriДокумент45 страницDr.R.Durai Ms Assisstant Professor Department of General Surgery Mgmcrimarinacretu1Оценок пока нет
- Management For PancreatolithiasisДокумент13 страницManagement For PancreatolithiasisAhmad Fakhrozi HelmiОценок пока нет
- SOP Open Access Endoscopy Updated30AprilДокумент29 страницSOP Open Access Endoscopy Updated30AprilmungicideОценок пока нет
- Articol Colectiiintraabd2013Документ8 страницArticol Colectiiintraabd2013Miha ElaОценок пока нет
- Rectal Prolapse: Rare Presentation and Complication: Case ReportДокумент3 страницыRectal Prolapse: Rare Presentation and Complication: Case Reportadi tiarmanОценок пока нет
- Acalasia 10 AnosДокумент6 страницAcalasia 10 Anosgabriel martinezОценок пока нет
- Laparoscopy in The Acute AbdomenДокумент15 страницLaparoscopy in The Acute AbdomenDragoiu AlexandraОценок пока нет
- Complicated Small-Bowel Diverticulosis: A Case Report and Review of The LiteratureДокумент3 страницыComplicated Small-Bowel Diverticulosis: A Case Report and Review of The LiteratureYeudiel SuroОценок пока нет
- Articulo HC CG IIrДокумент6 страницArticulo HC CG IIrKelly F RuizОценок пока нет
- Pancreatic PseudocystДокумент16 страницPancreatic PseudocystSpandan KadamОценок пока нет
- Laparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyДокумент4 страницыLaparoscopic Versus Open Cystogastrostomy For Pancreatic Pseudocysts A Comparative StudyInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Gossypiboma - A Rare Cause of Gastric Outlet ObstructionДокумент3 страницыGossypiboma - A Rare Cause of Gastric Outlet ObstructionJuniper PublishersОценок пока нет
- Raj KamalДокумент5 страницRaj KamalBhavani Rao ReddiОценок пока нет
- Journal ReadingДокумент8 страницJournal ReadingAnonymous Uh2myPxPHОценок пока нет
- Oesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractДокумент12 страницOesophagocoloplasty For Corrosive Oesophageal Stricture: AbstractSpandan KadamОценок пока нет
- Cureus 0013 00000014175Документ6 страницCureus 0013 00000014175qweqweqwОценок пока нет
- Kunio Et Al. - 2015 - Short EsophagusДокумент12 страницKunio Et Al. - 2015 - Short EsophagusDaniel PredaОценок пока нет
- Pancreatitis AgudaДокумент19 страницPancreatitis AgudaSamuel MedinaОценок пока нет
- Gastrojejunostomy For Gastric Outlet Obstruction in Patients With Gastric CarcinomaДокумент4 страницыGastrojejunostomy For Gastric Outlet Obstruction in Patients With Gastric CarcinomacindyОценок пока нет
- Cholecystectomy: Cholecystectomy Is The Surgical Removal of The Gallbladder. It Is The Most CommonДокумент3 страницыCholecystectomy: Cholecystectomy Is The Surgical Removal of The Gallbladder. It Is The Most CommonkiellrОценок пока нет
- Minimally Invasive SurgeryДокумент6 страницMinimally Invasive SurgerycarmenОценок пока нет
- Materi DR Budi WidodoДокумент44 страницыMateri DR Budi WidodoAnna Maria UlfaОценок пока нет
- Gastric Resection: General Surgical and Anesthetic ConsiderationsДокумент26 страницGastric Resection: General Surgical and Anesthetic ConsiderationsBlanchette ChОценок пока нет
- Nuclear Medicine GuideДокумент3 страницыNuclear Medicine GuidejeffsunilОценок пока нет
- Floppy Dor Fundoplication After Esophagocardiomyotomy For AchalasiaДокумент8 страницFloppy Dor Fundoplication After Esophagocardiomyotomy For AchalasiaDaniel FloreaОценок пока нет
- JJ Intus Post RNY HJДокумент29 страницJJ Intus Post RNY HJRajesh MenonОценок пока нет
- Technical Modification For Sleeve GastrectomyДокумент5 страницTechnical Modification For Sleeve GastrectomyJorge SalazarОценок пока нет
- Referat EndosДокумент29 страницReferat EndosShenaquitaIvandraОценок пока нет
- Gallbladder Disorders: Group 3Документ51 страницаGallbladder Disorders: Group 3Mae GabrielОценок пока нет
- Patophsyiology GerdДокумент17 страницPatophsyiology Gerdanon_873909596Оценок пока нет
- Editorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystДокумент4 страницыEditorial What Is The Best Endoscopic Treatment For Pancreatic PseudocystLogical MonsterОценок пока нет
- 139-Article Text-416-1-10-20180204Документ3 страницы139-Article Text-416-1-10-20180204Kriti KumariОценок пока нет
- Van Der Aa July 2012Документ8 страницVan Der Aa July 2012ValОценок пока нет
- Recurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Документ2 страницыRecurrent Infected Mesenteric Cyst A Rare Cause of Surgical Abdomen - September - 2022 - 6310790226 - 8312714Motivational SpeechОценок пока нет
- J Epsc 2015 05 012Документ4 страницыJ Epsc 2015 05 012Hanung PujanggaОценок пока нет
- Surgical Endoscopy 6Документ102 страницыSurgical Endoscopy 6Saibo BoldsaikhanОценок пока нет
- Background: Endoscopic Retrograde Cholangiopancreatography (ERCP)Документ4 страницыBackground: Endoscopic Retrograde Cholangiopancreatography (ERCP)Resci Angelli Rizada-NolascoОценок пока нет
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryДокумент31 страницаRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaОценок пока нет
- An Evidence-Based Manual For Abdominal Paracentesis: Grant I. Chen Sander Veldhuyzen Van ZantenДокумент9 страницAn Evidence-Based Manual For Abdominal Paracentesis: Grant I. Chen Sander Veldhuyzen Van ZantenIULIAN LUPUОценок пока нет
- Nissen Fundoplication - StatPearls - NCBI BookshelfДокумент9 страницNissen Fundoplication - StatPearls - NCBI BookshelfAndres Neira QuezadaОценок пока нет
- Ileus Obstruksi PDFДокумент20 страницIleus Obstruksi PDFherfikaОценок пока нет
- Laparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8Документ4 страницыLaparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8ciuca bogdanОценок пока нет
- Entero Cutaneous FistulaДокумент35 страницEntero Cutaneous FistulaNikhil PanjiyarОценок пока нет
- Bologna Guidelines Asbo 2013Документ19 страницBologna Guidelines Asbo 2013Gina Kristina NanginОценок пока нет
- Artículo 2Документ10 страницArtículo 2edunapedОценок пока нет
- Cis v2 Id1838Документ6 страницCis v2 Id1838Raqqi PujatmikoОценок пока нет
- Gallstone Disease and The Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Observational StudiesДокумент7 страницGallstone Disease and The Risk of Cardiovascular Disease: A Systematic Review and Meta-Analysis of Observational StudiesAfkar30Оценок пока нет
- FS PustakaДокумент4 страницыFS PustakaAfkar30Оценок пока нет
- Outcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisДокумент9 страницOutcomes of Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-AnalysisAfkar30Оценок пока нет
- Prospective Clinical Study: Mass Closure Versus Layer Closure of Abdominal WallДокумент6 страницProspective Clinical Study: Mass Closure Versus Layer Closure of Abdominal WallAfkar30Оценок пока нет
- DR Kiki Lukman Patofisiologi Acute CholangitisДокумент36 страницDR Kiki Lukman Patofisiologi Acute CholangitisAfkar30Оценок пока нет
- Dr. Wifanto-Management Liver Metastasis CRCДокумент46 страницDr. Wifanto-Management Liver Metastasis CRCAfkar30Оценок пока нет
- Guidelines For Surgery in The HIV Patient: Samuel Smit, MB CHB, M Med (Surg)Документ8 страницGuidelines For Surgery in The HIV Patient: Samuel Smit, MB CHB, M Med (Surg)Afkar30Оценок пока нет
- Salah Satu Syarat Guna Memperoleh Gelar Dokter Spesialis BedahДокумент1 страницаSalah Satu Syarat Guna Memperoleh Gelar Dokter Spesialis BedahAfkar30Оценок пока нет
- Announcement BSS GP PDFДокумент2 страницыAnnouncement BSS GP PDFAfkar30Оценок пока нет
- Imaging Correlation of The Degree of Degenerative L4-5 Spondylolisthesis With The Corresponding Amount of Facet FluidДокумент6 страницImaging Correlation of The Degree of Degenerative L4-5 Spondylolisthesis With The Corresponding Amount of Facet FluidAfkar30Оценок пока нет
- Abses Hepar 2014Документ2 страницыAbses Hepar 2014Afkar30Оценок пока нет
- Esofageal Stenosis - DR AnungДокумент26 страницEsofageal Stenosis - DR AnungAfkar30Оценок пока нет
- Bun, Creatinin & CCTДокумент1 страницаBun, Creatinin & CCTAfkar30Оценок пока нет
- Rekap Visite Dokter Pasien R.Inap: Periode Layanan: S.D TGL Cetak. Rumah Sakit Dr. Mohammad Hoesin Palemban Hal.Документ8 страницRekap Visite Dokter Pasien R.Inap: Periode Layanan: S.D TGL Cetak. Rumah Sakit Dr. Mohammad Hoesin Palemban Hal.Afkar30Оценок пока нет
- Visit DR SI Feb 2017Документ4 страницыVisit DR SI Feb 2017Afkar30Оценок пока нет
- Poli Maret 2017Документ1 страницаPoli Maret 2017Afkar30Оценок пока нет
- Visit DR TT Feb 2017Документ3 страницыVisit DR TT Feb 2017Afkar30Оценок пока нет
- P P P P P P P P P: Jumlah 28 HR TH 0-6 HR PERSEN (%)Документ1 страницаP P P P P P P P P: Jumlah 28 HR TH 0-6 HR PERSEN (%)Afkar30Оценок пока нет
- Denah Meja VIPДокумент4 страницыDenah Meja VIPAfkar30Оценок пока нет
- Acalculous Cholecystitis CaseДокумент35 страницAcalculous Cholecystitis CaseSaada Enok MedtamakОценок пока нет
- C 10 + 11 GALLBLADDER AND BILIARY TRACT Part1Документ45 страницC 10 + 11 GALLBLADDER AND BILIARY TRACT Part1mikaaa00050% (2)
- TEST-8 Gallstones: Part AДокумент178 страницTEST-8 Gallstones: Part Akuriakose mathewОценок пока нет
- 4 Series CPTДокумент13 страниц4 Series CPTPraviiОценок пока нет
- August 2023 (P2) - 1Документ309 страницAugust 2023 (P2) - 1Sherpao khan100% (1)
- KoledokolitiasisДокумент6 страницKoledokolitiasisnadya nazwinnОценок пока нет
- Differential Diagnosis Pain Right HypochondriumДокумент35 страницDifferential Diagnosis Pain Right HypochondriumDrArish Mahmood100% (1)
- LiverДокумент20 страницLiversekiannОценок пока нет
- Subdiaphragmatic Abscess V: PeterДокумент12 страницSubdiaphragmatic Abscess V: Petersyahrul ridengОценок пока нет
- Surgery Question From AbeideДокумент44 страницыSurgery Question From Abeide69xXALModr3EMXx69 McAnusОценок пока нет
- UWORLD Notes April 29 2016 (Usmle Grassroots)Документ80 страницUWORLD Notes April 29 2016 (Usmle Grassroots)Bhuvana Usmle100% (3)
- CholangitisДокумент4 страницыCholangitisNarianne Mae Solis Bedoy100% (1)
- Surgery Oral ExamДокумент46 страницSurgery Oral ExamM Patel100% (9)
- Interventional Approaches Gallbladder DiseaseДокумент9 страницInterventional Approaches Gallbladder DiseaseAntônio GoulartОценок пока нет
- Ms Questions2Документ12 страницMs Questions2laniОценок пока нет
- Week2Handout - NDT - Liver, Gallbladder, and PancreasДокумент7 страницWeek2Handout - NDT - Liver, Gallbladder, and PancreasMegumi S.Оценок пока нет
- IcdДокумент30 страницIcdSuryaAtmajayaОценок пока нет
- Surgery Sep+Oct+NovДокумент122 страницыSurgery Sep+Oct+Novﻋﻤﻴﺪ ﺍﻟﺸﻤﻴﺮﻱОценок пока нет
- JAUNDICE and CHOLECYSTITISДокумент109 страницJAUNDICE and CHOLECYSTITISSarah Racheal AkelloОценок пока нет
- Choledocholithiasis: Prevalence IncidenceДокумент9 страницCholedocholithiasis: Prevalence IncidenceMike GОценок пока нет
- 5 Obstructive Jaundice EditedДокумент33 страницы5 Obstructive Jaundice EditedNadhirah ZulkifliОценок пока нет
- NP3 SET A With AnswersДокумент11 страницNP3 SET A With AnswersMiss GОценок пока нет
- Standard Treatment Guidelines General Surgery: Ministry of Health & Family Welfare Govt. of IndiaДокумент73 страницыStandard Treatment Guidelines General Surgery: Ministry of Health & Family Welfare Govt. of IndiaiuytrerОценок пока нет
- EMQs For Medical Students Volume 2 2eДокумент30 страницEMQs For Medical Students Volume 2 2ePasTestBooks50% (2)
- Advance Managament of Acute Cholecystitis and CholangitisДокумент43 страницыAdvance Managament of Acute Cholecystitis and CholangitisWi HardiyantiОценок пока нет
- Visceral Pain Somatic Pain Referred Pain: 9. Acute AbdomenДокумент4 страницыVisceral Pain Somatic Pain Referred Pain: 9. Acute AbdomenLenard BangugОценок пока нет
- GB Cancer - Radiologic-Pathologic CorrelationДокумент20 страницGB Cancer - Radiologic-Pathologic CorrelationSamuel WidjajaОценок пока нет
- Answers For Oral FinalДокумент139 страницAnswers For Oral FinalIris BakerОценок пока нет
- Practical MCQ Question For 4-YearДокумент39 страницPractical MCQ Question For 4-Yearkhuzaima9100% (2)
- Dannangxue (M-Le-23) : Gallbladder PointДокумент1 страницаDannangxue (M-Le-23) : Gallbladder Pointray72roОценок пока нет