Академический Документы
Профессиональный Документы
Культура Документы
Pro67-C-15 Sput Digestion Decont For Mycobact Cultv1 1
Загружено:
sjamsul bahriОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Pro67-C-15 Sput Digestion Decont For Mycobact Cultv1 1
Загружено:
sjamsul bahriАвторское право:
Доступные форматы
SMILE
Johns Hopkins University
Baltimore, MD USA
Specimen Digestion/Decontamination for Mycobacteriology Culture-
Guidelines
Author: Peggy Coulter Document Number: Pro67-C-15-G
Effective (or Post) Date: 10 Feb 09
Review History Version V 1.1
Revised Date: 13 May 2013
Date of last review 14 May 2013 Reviewed by: Heidi Hanes
SMILE Comments: This document is provided as an example only. It must be revised to accurately reflect your lab’s
specific processes and/or specific protocol requirements. Users are directed to countercheck facts when considering
their use in other applications. If you have any questions contact SMILE.
CAP Accreditation Checklist:
Question pertaining to Mycobacteriology Culture can be found under Mycobacteriology –
Concentration, Inoculation, Incubation Section of the CAP Accreditation Laboratory
Microbiology Checklist.
Background Information:
Specimens submitted for Mycobacteriology culture are most frequently obtained from body sites
where other pathogens and/or normal flora reside. Because mycobacteria are slow growing and
require long incubation times these contaminating organisms can overgrow in cultures, blocking
the ability to detect the presence of the mycobacteria. Digestion and decontamination procedures
are used in processing sputum for examination and culture of sputum specimens. This step
performs two major functions: 1) sputum is liquefied (digestion), permitting the mycobacteria to
be released from the thick sputum so that they can be subsequently concentrated by
centrifugation, and 2) contaminating normal flora is preferentially killed (decontamination).
Unfortunately, it must be recognized that the strong alkaline reagent usually used for the
decontamination step is also toxic to mycobacteria. The degree to which the mycobacteria in the
specimen are killed is a function of the concentration of the alkali used, the length of time over
which the organisms are exposed, and the temperature at which the exposure occurs.
Appropriate digestion and decontamination procedures, culture media, and conditions of
incubation must be selected to facilitate optimal recovery of the mycobacteria. These
considerations are especially important for paucibacillary disease, i.e. sputum from patients who
present with non-cavitary disease, who excrete only small numbers of organisms in their sputum.
These populations include patient with early infections, and those who are HIV-infected.
The success of digestion/decontamination depends upon the following considerations:
The concentration of organisms present in a given specimen;
The resistance of tubercle bacilli to the concentration of the strongly alkaline or acidic
digesting solutions used;
The length of time the mycobacteria are exposed to the digestant;
The temperature of the room, in which the exposure is carried out
The amount of heat generated by the specimen centrifugation step; and
The efficiency of the centrifuge used in the sedimentation step.
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Several methods are available for digestion and decontamination of sputum specimens for
culturing of Mycobacteria, but not all are acceptable for all specimens or for all systems used to
culture for mycobacteria subsequently. The choice must be based upon technical capability, and
upon the quality and type of equipment, supplies and reagents available. Optimally for quality
control reasons, only a single method should be used in a given laboratory. Whichever method is
used, meticulous care must be taken to prevent laboratory cross-contamination of specimens
during processing. Risk of contamination occurs especially when digestant and/or buffer are
added subsequently to a batch of tubes. A single positive culture for M. tuberculosis can lead to
diagnosis of tuberculosis and a false-positive culture affects not only clinical management of the
patient, but also epidemiological investigations and public health controls.
Major Liquefaction/Decontamination Processing Method:
N-Acetyl-L-Cysteine-Sodium Hydroxide (NALC-NaOH) Method
NALC (a mucolytic agent) combined with sodium hydroxide is the preferred method for the
digestion step because it is the least toxic to the mycobacteria, and therefore provides the highest
yield of positives. NALC perform the liquefaction step, and permits the use of a lower, (1%)
concentration of NaOH than that required when NALC is omitted. Sodium citrate is also
included to bind heavy metal ions, which, if present in the specimen, can inactivate the acetyl-
cysteine. The digestant must be made fresh daily due to the rapid loss of acetyl-cysteine activity
when the compound is in solution.
A variety of specimen types may be processed using this method, making it particularly useful
for processing specimens from patients with few organisms, as seen in non cavitary disease
which includes patients with concurrent HIV infections. This is the manufacturer approved
method for processing specimens using the BD BBL™ MGIT™ Mycobacteria Growth Indicator
Tube.
Resources
1. Cernoch, P.L. et al. (1994). Cumitech 16A: Laboratory diagnosis of the Mycobacterioses.
ASM Press. Washington, DC.
2. Forbes, B.A., et al (2007). Laboratory detection and identification of mycobacteria; Proposed
guideline. CLSI document M48-P. Clinical and Laboratory Standards Institute, Wayne, PA.
3. Kent , P.T. and Kubica, G. P. (1985). Public Health Mycobacteriology. A Guide for the Level
III Laboratory. U.S. Dept. Health and Human Services. Center for Disease Control.
4. SA Healthinfo, Tuberculosis Part III: Culture homogenization and decontamination. Obtained
from the World Wide Web on 14 March 2007 at HREF="http://www.sahealthinfo.org/tb"
5. Weitzman, I. (2007) p 7.1.2.1-7.1.2.9. In H.D. Isenberg (ed.) Clinical Microbiology
Procedures Handbook American Society for Microbiology, Washington, D.C.
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Specimen Digestion/Decontamination for Mycobacteriology Culture - SOP
Peggy Coulter MDE, MT (HEW) Document Effective
Author(s), Name & International QA/QC Coordinator Number Date
Title Pro67-C-15 13 May 2013
Approved By Name, Title Signature Date
SOP Annual Name, Title Signature Date
Review
Version # [0.0] Revision Date Description (notes)
Revision [dd/mm/yy]
History
Distributed Name (or location) # of copies Name (or location) # of copies
Copies to
Associated Forms:
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Purpose
There are different approved methods for processing specimens from various body sites. The one
used for processing sputum outlined below can be used for the BD BBL MGIT (Mycobacteria
Growth Indicator Tube) liquid and solid culture media.
Pre-analytic Procedure
Refer to the following procedures:
1. Mycobacteriology Laboratory Specimen Collection/Receiving
2. Safety in the BSL-3 Laboratory
3. Use of the Bio-Safety Hood in the Mycobacteriology Laboratory
Abbreviations Used:
AFB = Acid Fast Bacilli
BSC = Bio-Safety Cabinet
SOP = Standard Operating Procedure
Specimen Information:
Specimen collection- Refer to Mycobacteriology Laboratory Specimen Collection/Receiving
SOP.
Analytic Procedure
Specimen types
Specimens that require decontamination include sputum, bronchial secretions, washings, or
biopsies, skin, soft tissue, gastric lavage, stool specimens, urines and all other specimens
from sites contaminated with normal microbial flora.
o Gastric aspirates
If the volume is greater than 10 ml, concentrate by centrifugation.
Re-suspend sediment in about 5ml of sterile water and then decontaminate.
Add a small amount of NALC powder if the specimen is thick or mucoid.
o Stool
Suspend 1 g of feces in 5ml of Middlebrook broth.
Agitate the suspension on a vortex mixer for 5 s.
Precede to the procedure steps below.
Sterile sites not requiring decontamination include CSF, bone marrow, blood, pleural fluid,
and sterile biopsy sites. These should be processed following specimen handling in the
Mycobacteriology Culture SOP.
When a specimen is determined to be unacceptable, a repeat specimen must be requested.
o Unacceptable specimens include unlabeled or inadequately identified specimens, dry
swabs, and those received in previously used containers, containers that are non-
sterile or cannot be tightly sealed.
o Specimens held unrefrigerated prior to processing for greater than one hour may lead
to bacterial overgrowth at levels that prevent detection of mycobacteria
o Sputum specimens collected at different times must never be pooled as this greatly
increases the contamination rates.
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Specimen storage
Specimens should be delivered to the laboratory as soon as possible to avoid overgrowth by
contaminants and normal respiratory flora.
Specimens not processed within one hour of collection must be refrigerated at 2 – 8° C.
If gastric lavage specimens are to take longer than 4 hours prior to processing, 100 mg. of
sodium carbonate must be added to the container to neutralize the high acidity of the
specimen.
Reagents/Media:
Reagents used for digestion/decontamination are dependent on precise adherence to the required
procedures.
1. Fresh working NALC-NaOH Solution - Directions for preparing NALC-NaOH Solution or
alternatively BD BBL™ MycoPrep™ Specimen Digestion/Decontamination Kit are included
in Appendix A
2. Phosphate buffer solution (pH 6.8)
3. BBL™ MGIT™ Mycobacteria Growth Indicator Tube
4. BACTEC™ MGIT™ 960 Supplement Kit including:
a. BACTEC MGIT Growth Supplement
b. BBL MGIT PANTA Antibiotic Mixture vial
Required Supplies:
1. 50 ml sterile conical centrifuge tubes
2. Vortex mixer
3. Centrifuge- capable of speed 3,000–3,500 x g, fixed angle rotor with aerosol-free safety
centrifuge cups
4. Funnel and waste container filled 1/3 full with an approved disinfectant solution
5. Disposable sterile pipettes
6. Slide warmer set between 65 and 75°C
7. Glass microscope slides (a frosted end for labeling with a pencil is useful)
Quality Control:
Negative - Process a negative water or buffer control with each run of specimens.
Positive - Sputum spiked with a mycobacterial species should be processed as a positive control
once per week.
Each new lot or shipment of MGIT tubes may be parallel tested using the following strains and
dilutions. The test culture should not be more than 15 days old. Prepare a suspension from
growth on solid medium, which is well dispersed, free of large clumps, and with a turbidity of
0.5 McFarland standard. When 0.5 mL of diluted suspension is inoculated into an MGIT tube
supplemented with enrichment, it should be detected as instrument positive within the time frame
shown below:
M. tuberculosis (ATCC 27294) 1:500 within 6-10 days
M. kansasii (ATCC 12478) 1:50,000 within 6-11 days
M. fortuitum (ATCC 6841) 1:5,000 within 1-3 days
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Record Quality Control growth results on a weekly basis.
Digestion, Decontamination and Concentration Procedure Steps:
Follow laboratory bio-safety practices for all procedure steps.
1. Prepare fresh working digestant/decontamination solution or BD BBL™ MycoPrep™
Specimen Digestion/Decontamination Kit as described in Appendix A.
2. Prepare the BSC for use following the Use of the Bio-Safety Hood in the Mycobacteriology
Laboratory SOP.
3. Reconstitute a lyophilized vial of BBL MGIT PANTA Antibiotic Mixture with 15 mL of
BACTEC MGIT Growth Supplement.
*Once reconstituted, the PANTA mixture must be stored at 2 – 8°C and used within 5 days.
4. Label the MGIT tubes with the specimen number.
5. Unscrew the cap and aseptically add 0.8 mL of Growth Supplement/MGIT PANTA
Antibiotic Mixture to each labeled MGIT tube.
*For best results, the addition of Growth Supplement/MGIT PANTA Antibiotic Mixture
should be made just prior to specimen inoculation.
6. If the specimen was not collected in a sterile, labeled 50 ml disposable centrifuge tube,
transfer the entire specimen to a labeled 50 ml conical tube.
*No more than 10 ml of specimen may be processed per conical tube. The remaining sample
should be transferred to second tube and processed. Repeat for all patient specimens.
7. Stagger the tubes in the rack to prevent cross contamination.
*Do not process more specimens in a batch than the centrifuge will hold.
8. Opening only one tube at a time, to the first specimen tube add an equal amount of fresh
working NACL-NaOH solution, rotate and invert the tube, ensuring the mixture coats the
entire interior surface. Vortex the mixture for 10-15 seconds. Repeat this step for each
specimen in the batch.
*Start the timer for 15 minutes after adding the solution to the first tube in the batch.
9. Allow the specimens to stand the entire 15 minutes. During the incubation time check each
specimen by slightly tilting the tube and observing for liquefaction.
*If a specimen is very mucoid with no change during these checks, add a small amount of
NALC directly to the tube, vortex and allow to stand until the end of this incubation time.
10. After the digestant has remained in the first tube for 15 minutes, begin with the first
specimen and fill the first tube to the 50 ml mark with phosphate buffer by slowly pouring
the buffer down the side of the tube avoiding splashing or contamination. Tighten the cap and
wipe the outside of each tube with the disinfectant soaked towel, then invert the tube several
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
times to mix thoroughly. Repeat this step on each of the remaining specimens in the batch,
mixing well after each addition.
11. Load tubes in aerosol-free safety centrifuge cups. Centrifuge tubes for 15 minutes at 3,000 -
3,500 x g. Allow aerosols to settle a few minutes before removing tubes from the centrifuge
cups.
12. Opening one tube at a time, pour off the supernatant into a waste container filled 1/3 full with
approved disinfectant solution. Wipe the lip of the conical tube with a disinfectant soaked
towel and then recap.
*The use of a funnel is preferred. (Pour slowly so as not to disturb the pellet and be sure to
not touch the funnel while pouring.
13. Using a sterile disposable transfer pipette, re-suspend the pellet by adding 1-2 mL of
phosphate buffer. Gently mix the tube contents.
14. Add 0.5 mL of the concentrated specimen suspension to the prepared BBL™ MGIT™
Mycobacteria Growth Indicator Tube. Also add a drop (0.1 - .25 mL) of specimen to a
Lowenstein-Jensen agar slant or other conventional solid medium.
*Refer to the Mycobacteriology Culture SOP.
15. With the same pipette, place a drop of the suspension onto a clean, labeled glass microscope
slide. Prepare a smear over an area of 1 by 2 cm of the slide.
*Refer to the AFB smear SOP.
16. Tightly recap the MGIT tube and mix well. Leave the inoculated tubes at room temperature
for 30 minutes before loading in to the MGIT system.
*Refer to the Mycobacteriology Culture SOP.
17. Load inoculated BBL™ MGIT™ Mycobacteria Growth Indicator Tube into the instrument
following manufacturers’ instructions for the duration of the recommended 42 day testing
protocol.
18. For specimens in which mycobacteria with different incubation requirements are suspected, a
duplicate MGIT tube can be set up and incubated at the appropriate temperature; e.g., 30 or
42°C. Inoculate and incubate at the required temperature. These tubes must be manually read
(refer to the BACTEC MGIT Instrument User’s Manual).
Post-analytic Procedure
Specimen Retention:
Store processed specimens in AFB refrigerator for as long as space allows (approximately two
weeks).
Calculations:
Quality monitors are compiled monthly to monitor the digestion process of the lab.
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
Expected Values:
Contamination rates of 8 - 10% are considered to be acceptable for solid culture
media.
Liquid culture media will have a higher contamination rate which will be monitored
for acceptability.
A contamination rate of less than 5% suggests overly harsh decontamination.
A contamination rate of greater than 10% growth suggests inadequate
decontamination, incomplete digestion, reagent and/or media contamination or
environmental contamination.
Interpretation of Results:
Contamination rates higher than 10% on solid media will be investigated to determine whether
equipment, reagent or personnel are causing the high rates. Data is included in the monthly
quality assurance report.
Method Limitations:
The procedure is dependant on strict adherence to recommended techniques, timing,
temperature, and biochemical requirements. Any deviation from the SOP will not provide
appropriate clinical care.
The NaOH procedure is very robust and may kill up to 60% of tubercle bacilli in clinical
specimens, and may give a false negative result, especially in cases of paucibacillary disease
as seen in early disease, or in many HIV positive patients.
Additional contributory factors such as heat build-up in the centrifuge step may also kill
tubercle bacilli.
Appendix
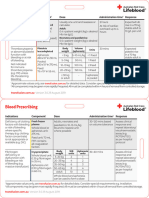
Appendix A -NALC-NaOH Method Reagent
References:
1. Cernoch, P.L. et al. (1994). Cumitech 16A: Laboratory diagnosis of the Mycobacterioses.
ASM Press. Washington, DC.
2. Clinical Laboratory Standards Institute (CLSI). Clinical Laboratory Technical Procedure
Manuals; Fourth Edition. CLSI Document GP2-A4 (ISBN 1-56238-458-9). Clinical and
Laboratory Standards Institute, Wayne, PA
3. Forbes, B.A., et al (2007). Laboratory detection and identification of mycobacteria; Proposed
guideline. CLSI document M48-P. Clinical and Laboratory Standards Institute, Wayne, PA.
4. Kent , P.T. and Kubica, G. P. (1985). Public Health Mycobacteriology. A Guide for the Level
III Laboratory. U.S. Dept. Health and Human Services. Center for Disease Control.
5. SA Healthinfo, Tuberculosis Part III: Culture homogenization and decontamination. Obtained
from the World Wide Web on 14 March 2007 at HREF="http://www.sahealthinfo.org/tb"
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
SMILE
Johns Hopkins University
Baltimore, MD USA
6. Weitzman, I. (2007) p 7.1.2.1-7.1.2.9. In H.D. Isenberg (ed.) Clinical Microbiology
Procedures Handbook American Society for Microbiology, Washington, D.C.
7. BBL™ MGIT™ Mycobacteria Growth Indicator Tube with BACTEC™ MGIT™ 960
Supplement Kit package insert, Becton, Dickinson and Company, 2011.
Digestion Decontamination for Mycobacterial Cultures V1.1 SMILE Document
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Emergency Room 100 ItemsДокумент33 страницыEmergency Room 100 ItemsJillian EsquivelОценок пока нет
- Jawaban PBL Diare Nomer 3Документ2 страницыJawaban PBL Diare Nomer 3sjamsul bahriОценок пока нет
- Jawaban PBL No 6Документ1 страницаJawaban PBL No 6sjamsul bahriОценок пока нет
- Jawaban PBL NMR 3 Modul KuningДокумент3 страницыJawaban PBL NMR 3 Modul Kuningsjamsul bahriОценок пока нет
- Normal ROMДокумент1 страницаNormal ROMsjamsul bahriОценок пока нет
- Sasa TugasДокумент2 страницыSasa Tugassjamsul bahriОценок пока нет
- 47 IrradiationДокумент1 страница47 Irradiationsjamsul bahriОценок пока нет
- 44 Congenital Heart DiseaseДокумент2 страницы44 Congenital Heart Diseasesjamsul bahriОценок пока нет
- Chapter 12 - Scoliosis: Expert ConsultДокумент2 страницыChapter 12 - Scoliosis: Expert Consultsjamsul bahriОценок пока нет
- Aloe VeraДокумент39 страницAloe VeraAyush TiwariОценок пока нет
- Metastases Bone DiseaseДокумент59 страницMetastases Bone Diseasemuhammad rustamОценок пока нет
- An Investigatory Project ProposalДокумент13 страницAn Investigatory Project ProposalJeg B. Israel Jr.Оценок пока нет
- Basic Life Support PresentationДокумент34 страницыBasic Life Support PresentationMona ElhassanОценок пока нет
- A Patient of Poisoning in ICU (Ankit Jain)Документ48 страницA Patient of Poisoning in ICU (Ankit Jain)SharryОценок пока нет
- Bhoomi PatelДокумент9 страницBhoomi PatelPooja PanchalОценок пока нет
- Daily Inspiration: Powered by Crystallive™Документ8 страницDaily Inspiration: Powered by Crystallive™douglaszimbaОценок пока нет
- Cognitive Rehab For StrokeДокумент19 страницCognitive Rehab For StrokeAisyah IcahОценок пока нет
- Liver CancerДокумент16 страницLiver CancerMark James MelendresОценок пока нет
- Cardioplegia Types and Methods of AdministrationДокумент59 страницCardioplegia Types and Methods of Administrationgovind_soni_150% (2)
- Guide To Dilution and Administration of Iv Medications: AcyclovirДокумент29 страницGuide To Dilution and Administration of Iv Medications: AcyclovirCiara Marjorie HannaОценок пока нет
- 05 Lanyard Cards - Blood Prescribing Card v3.2 FINALДокумент2 страницы05 Lanyard Cards - Blood Prescribing Card v3.2 FINALAbdul RaufОценок пока нет
- Ascorbic Acid (Vitamin C) - Side Effects, Interactions, Warning, Dosage & UsesДокумент4 страницыAscorbic Acid (Vitamin C) - Side Effects, Interactions, Warning, Dosage & UsesMuhammad ZuhriОценок пока нет
- Concepts of Diet Therapy and The Role of The NurseДокумент18 страницConcepts of Diet Therapy and The Role of The NurseHartiem FarrellОценок пока нет
- The Mind Body Interaction in DiseaseДокумент8 страницThe Mind Body Interaction in DiseaseYuli MSОценок пока нет
- ESSAYДокумент2 страницыESSAYBokОценок пока нет
- Surgery Surgical Nursing Objs With AnsДокумент136 страницSurgery Surgical Nursing Objs With AnsmintahmeshackbenjaminОценок пока нет
- Name of Patient: E.J.P Ward/Room/Bed #: Pedia Ward/G.I./Bed 1 Age & Sex: 2 Y.o/ Female Diagnosis: Urinary Tract InfectionДокумент1 страницаName of Patient: E.J.P Ward/Room/Bed #: Pedia Ward/G.I./Bed 1 Age & Sex: 2 Y.o/ Female Diagnosis: Urinary Tract InfectionSALMA M. TUANOОценок пока нет
- Journal of Clinical Neuroscience: Imran Ahmad, Farooq Azam RathoreДокумент5 страницJournal of Clinical Neuroscience: Imran Ahmad, Farooq Azam RathorekhairaniОценок пока нет
- Pa Tho Physiology of Diabetes InsipidusДокумент4 страницыPa Tho Physiology of Diabetes InsipidusteynsОценок пока нет
- Chapter 46 Antianginal AgentsДокумент14 страницChapter 46 Antianginal AgentsJewel SantosОценок пока нет
- Differences in Left Ventricular and Left Atrial FuДокумент10 страницDifferences in Left Ventricular and Left Atrial FueugeniaОценок пока нет
- Komplikasi AnestesiДокумент34 страницыKomplikasi Anestesiyurie_ameliaОценок пока нет
- Factors Influencing Compliance To Dietary Regimen Among Diabetic Patient in Ladoke Akintola University of Technology Teaching Hospital Osogbo. by Folaranmi Basirat TemitopeДокумент98 страницFactors Influencing Compliance To Dietary Regimen Among Diabetic Patient in Ladoke Akintola University of Technology Teaching Hospital Osogbo. by Folaranmi Basirat TemitopeOMOLOLA ADAMS OLATAYOОценок пока нет
- Department of Molecular Virology: COVID-19 (Corona) VirusДокумент1 страницаDepartment of Molecular Virology: COVID-19 (Corona) VirusMuhammad YahyaОценок пока нет
- VACCINESДокумент8 страницVACCINESzilikajainОценок пока нет
- White Blood Cells TugasДокумент6 страницWhite Blood Cells TugasanisaОценок пока нет
- Ectopic Pregnancy: DR .Urmila KarkiДокумент27 страницEctopic Pregnancy: DR .Urmila KarkiBasudev chОценок пока нет
- 9c5ff54e-92aa-4393-8350-218e91c128d2Документ6 страниц9c5ff54e-92aa-4393-8350-218e91c128d2Zarbakht AliОценок пока нет