Академический Документы
Профессиональный Документы
Культура Документы
Injuria Renală Acută Corectat
Загружено:
Caraiman LarisaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Injuria Renală Acută Corectat
Загружено:
Caraiman LarisaАвторское право:
Доступные форматы
Prevention and Management of Acute Kidney Injury Guideline
1 Introduction
Acute Kidney Injury (AKI), previously known as acute renal failure, is
characterised by a sudden decline in kidney function.
AKI can occur without symptoms and is detected through a routine blood
test (serum creatinine) and/or a decrease in urine output (KDIGO, 2012).
AKI is associated with an increased risk of death, length of hospital stay,
risk of chronic kidney disease (CKD) and cost to the NHS.
It is likely that early AKI currently goes unrecognised and a number of AKI
cases in at risk groups / high-risk scenarios are preventable.
Early detection and appropriate management of AKI can minimise further
injury.
1.1 Recognise AKI
AKI is defined according to the KDIGO criteria (KDIGO, 2012) and relies
primarily on assessing the change in serum creatinine measurement from a
previous baseline.
Depending on the availability of previous creatinine measurements, in order of
preference, ‘Baseline creatinine’ is defined as:
a) The lowest serum creatinine measurement in the preceding 7 days
b) The average (mean) of all serum creatinine measurements over the
preceding year
c) The upper limit of the age specific reference interval for serum
creatinine.
In addition, urine output <0.5 ml/kg/h for ≥8h may indicate AKI and should
prompt further investigation.
AKI severity Serum creatinine
Stage 1 1.5–1.9× baseline
OR
≥26 μmol/l increase
Stage 2 2.0–2.9× baseline
Prevention and Management of Acute Kidney Injury
Stage 3 3.0× baseline
OR
Increase in serum creatinine to ≥354 μmol/l)
OR
Initiation of renal replacement therapy
OR
Decrease in estimated glomerular filtration rate (eGFR – see
Appendix A for calculation) to <35 ml/min per 1.73 m2
2 Prevention of AKI
2.1 Identify patients at risk for AKI
An audit at Alder Hey identified that our leading causes of AKI are cardiac
bypass surgery and nephrotoxic medications.
The BAPN recommends that children meeting any of the following criteria
should be considered at risk of AKI:
Children at high risk of AKI include those with:
Nephro-urological, cardiac or liver disease
Malignancy and/or a bone marrow transplant
Dependence on others for access to fluids (e.g. gastrostomy fed)
History of taking medication that may adversely affect renal function
(ACEI / ARB, NSAIDs, aminoglycosides, calcineurin inhibitors)
Scenarios in which children can be at high risk of AKI include:
History of reduced urine output
Sepsis
Hypoperfusion or dehydration
History of exposure to drugs or toxin that may adversely affect renal
function
Renal disease or urinary tract obstruction
Major surgery
2.2 Prevention: 3Ms
Monitor the following daily in children at high risk of AKI:
Serum creatinine and electrolytes
Urinalysis
Weight
Fluid balance (including urine output)
PEWS including blood pressure
Maintain circulation
adequate treatment of hypoperfusion
February 2019 Page 2 of 6
Prevention and Management of Acute Kidney Injury
Minimise kidney insults
Review, monitor and adjust potentially nephrotoxic medications
o Calculate eGFR (see Appendix A)
o Review medication list in liaison with pharmacist
o Consider risk of radiocontrast for CT scans (if essential, ensure
adequate hydration)
3 Management of confirmed AKI
3.1 Aims
Recognise AKI early
Minimise further kidney injury
Identify and treat the underlying cause
3.2 Management: 4Ms
Monitor the following daily in children at high risk of AKI:
Serum creatinine and electrolytes
Urinalysis
Weight
Fluid balance (including urine output)
PEWS including blood pressure
Maintain circulation
adequate treatment of hypoperfusion
Minimise kidney insults
Review, monitor and adjust potentially nephrotoxic medications
o Calculate eGFR (see Appendix A)
o Review medication list in liaison with pharmacist
o Consider risk of radiocontrast for CT scans (if essential, ensure
adequate hydration)
Management
Initial investigations:
o Repeat creatinine & electrolytes (including bicarbonate)
o Bone profile
o FBC
o Urine dipstick
o Urine microscopy
Urgent review by a senior member of the patient’s primary clinical team.
Urinary tract ultrasound scan, usually within 24 hours (primarily to exclude
urinary tract obstruction)
Further investigations if clinically relevant:
o C3 / C4
o ASOT
o ANA
o ANCA
o Anti-GBM antibodies
February 2019 Page 3 of 6
Prevention and Management of Acute Kidney Injury
o Immunoglobulins
o Blood film
o LDH
o CK
3.3 Paediatric Nephrology Referral (excluding patients on Intensive Care)
AKI Stage 1 Consider discussion with nephrology team
AKI Stage 2 Discuss with nephrology team
AKI Stage 3 Refer to nephrology team:
Notify patient’s lead consultant
Telephone referral to Nephrology team (Registrar
bleep 184, Out-of-hours contact on-call consultant via
switchboard)
Also complete Meditech Nephrology referral
Criteria for immediate discussion with nephrology team in any stage of AKI:
Pre-existing renal condition (e.g. existing CKD 4 or 5 or renal transplant)
AKI associated with multisystem disease or suspected intrinsic renal
disease (e.g. haemolytic uraemic syndrome)
Potassium >5.5mmol/l (free-flowing, non-haemolysed sample)
Oligoanuria and/or plasma sodium <125mmol/l
Pulmonary oedema or hypertension
Rising plasma urea >20mmol/l unresponsive to fluid challenge
3.4 Referral of patients on Intensive Care to Paediatric Nephrology Team
We recognise that AKI often occurs as part of multisystem illness in critically ill
patients, and will usually be managed independently by the intensive care
team.
The Nephrology team should be routinely informed of any patient with AKI
stage 2 or more for 2 days or more.
Some patients may benefit from additional Paediatric Nephrology input,
including:
Where there is diagnostic uncertainty
Where intrinsic renal disease is suspected
Where the patient is likely to require ongoing renal input following
stepdown from intensive care.
4 Discharge after AKI
AKI stage 2 or more
For 2 days or more
= Refer for Nephrology AKI follow-up
February 2019 Page 4 of 6
Prevention and Management of Acute Kidney Injury
4.1 Discharge summary
Document AKI episode (including stage and dates) on discharge summary
Document the likely cause of AKI (e.g. nephrotoxic (state causative agent),
dehydration, sepsis, cardiac surgery, etc.)
Request AKI follow-up with nephrology team for all patients with AKI stage
2 or 3 for 2 days or more:
o State ‘Nephrology AKI follow-up clinic in 3 months’ in discharge
summary plan
o Inform Nephrology team of discharge (bleep 184)
4.2 Follow-up
All patients with AKI stage 2 or 3 for 2 days or more will be followed-up by the
paediatric nephrology team 3 months after the episode.
5 Contributors
Caroline Jones, Consultant Paediatric Nephrologist
Richard Holt, Consultant Paediatric Nephrologist
Henry Morgan, Consultant Paediatric Nephrologist
Louise Oni, Consultant Paediatric Nephrologist
Tolu Awogbemi, Consultant General Paediatrician
6 References
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury
Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury.
Kidney inter., Suppl. 2012; 2: 1–138
Think Kidneys. Guidance for clinicians managing children at risk of, or with,
acute kidney injury. UK Renal Registry, 2017.
www.thinkkidneys.nhs.uk/aki/wp-content/uploads/sites/2/2018/11/Nov-19-AKI-
Guidance-for-paediatrics.pdf Accessed 27/12/2018
Appendix A – Calculation of estimated glomerular filtration rate (eGFR)
40 ∗ [𝐻𝑒𝑖𝑔ℎ𝑡 (𝑐𝑚)]
𝑒𝐺𝐹𝑅(𝑚𝑙/𝑚𝑖𝑛/1.73𝑚2 ) =
𝑠𝑒𝑟𝑢𝑚 𝑐𝑟𝑒𝑎𝑡𝑖𝑛𝑖𝑛𝑒
Appendix B – BAPN AKI Management Recommendations
alderhey.nhs.uk/AKI
February 2019 Page 5 of 6
Prevention and Management of Acute Kidney Injury
Document Control Sheet
Prevention and Management of Acute Kidney Injury
Version: 1
Ratified by: Clinical Development Evaluation Group
Date ratified: 15/02/2019
Name of originator/author: Stephen McWilliam
Approved by: Nephrology Team
Date approved: 10/02/2019
Key search words: Acute, kidney, injury, AKI
Date issued: February 2019
Review date: February 2022
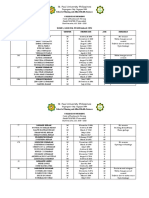
Version Control Table
Version Date Author Status Comment
1 February Stephen McWilliam, Current
2019 Paediatric
Nephrologist
Review & Amendment Log
Record of changes made to document since last approved version
Section Page Change/s made Reason for change
Number Number
February 2019 Page 6 of 6
Вам также может понравиться
- Ultrasound in Acute Kidney InjuryДокумент70 страницUltrasound in Acute Kidney InjuryaandakuОценок пока нет
- Understanding Chronic Kidney Disease: A guide for the non-specialistОт EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistРейтинг: 4 из 5 звезд4/5 (3)
- Obstetrics and Gynaecology Case ProformaДокумент13 страницObstetrics and Gynaecology Case Proformamd maaz100% (4)
- Homeopathy Answer KeyДокумент16 страницHomeopathy Answer Keyokta yuliawatiОценок пока нет
- Nephrology DR ZeinabДокумент101 страницаNephrology DR ZeinabZeinab Muhammad100% (1)
- Community OphthalmologyДокумент33 страницыCommunity OphthalmologyVarun BoddulaОценок пока нет
- Picu Protocol AiimsДокумент78 страницPicu Protocol AiimsMrinmayeeDeshmukh0% (1)
- Integrated Therapeutics II: January 2020Документ700 страницIntegrated Therapeutics II: January 2020Seyoum Tumsa100% (1)
- Kidney Biomarkers: Clinical Aspects and Laboratory DeterminationОт EverandKidney Biomarkers: Clinical Aspects and Laboratory DeterminationSeema S. AhujaОценок пока нет
- Integrated Therapeutics-Ii For 3 Year STS: Chapter-1Документ69 страницIntegrated Therapeutics-Ii For 3 Year STS: Chapter-1Geleta GalataaОценок пока нет
- Integrated Therapeutics IiДокумент165 страницIntegrated Therapeutics IiSalahadinОценок пока нет
- End Stage Renal Disease Case StudyДокумент8 страницEnd Stage Renal Disease Case StudyNikko Dela CruzОценок пока нет
- Critical Care-Sepsis Case StudyДокумент25 страницCritical Care-Sepsis Case Studyapi-378305067Оценок пока нет
- Differential Diagnosis of Head and SwellingДокумент41 страницаDifferential Diagnosis of Head and Swellingmachine318Оценок пока нет
- Acute Kidney InjuryДокумент21 страницаAcute Kidney InjuryyinyangdongОценок пока нет
- Acute Kidney Injury: KDIGO 2012 Clinical Practice GuidelineДокумент40 страницAcute Kidney Injury: KDIGO 2012 Clinical Practice GuidelineAbedDabajaОценок пока нет
- Recognition and Management of Acute Kidney Injury: Thomas Oates and Shabbir MoochhalaДокумент5 страницRecognition and Management of Acute Kidney Injury: Thomas Oates and Shabbir MoochhalaIntan NoaОценок пока нет
- Clinical Guidance: Acute Kidney InjuryДокумент25 страницClinical Guidance: Acute Kidney Injuryfahad nokiaОценок пока нет
- Acute Kidney Injury: Current Concepts and New Insights: Key WordsДокумент5 страницAcute Kidney Injury: Current Concepts and New Insights: Key WordsIHОценок пока нет
- Síndrome Hepatorrenal Cirrosis Eur Gast J 2021Документ9 страницSíndrome Hepatorrenal Cirrosis Eur Gast J 2021Anabel GonzalezОценок пока нет
- Aki GuidlineДокумент5 страницAki GuidlineFii Fathayati PutriОценок пока нет
- Renal DisorderДокумент102 страницыRenal DisorderIbsaa UsmanОценок пока нет
- The Definition of Acute Kidney Injury and Its Use in PracticeДокумент12 страницThe Definition of Acute Kidney Injury and Its Use in PracticewelinОценок пока нет
- Overview of The Management of Acute Kidney Injury in Adults - UpToDateДокумент13 страницOverview of The Management of Acute Kidney Injury in Adults - UpToDateDaniely FreitasОценок пока нет
- Acute Kidney InjuryДокумент15 страницAcute Kidney Injurykuchaibaru90Оценок пока нет
- Renal DisordersДокумент164 страницыRenal Disorderspblinder1319Оценок пока нет
- Causes of Acute Deterioration in Chronic Kidney DiseaseДокумент3 страницыCauses of Acute Deterioration in Chronic Kidney DiseaseSitLus ChannelОценок пока нет
- Acute Renal Failure in The ICU PulmCritДокумент27 страницAcute Renal Failure in The ICU PulmCritchadchimaОценок пока нет
- Acute Renal Failure and Cardiac SurgeryДокумент9 страницAcute Renal Failure and Cardiac Surgeryserena7205Оценок пока нет
- Acut Kidney InjuryДокумент12 страницAcut Kidney InjuryorriОценок пока нет
- Chew, Dennis - Acute - Kidney - Disease - Cats - STYLEDДокумент7 страницChew, Dennis - Acute - Kidney - Disease - Cats - STYLEDPatricia QueroОценок пока нет
- Gagal Ginjal Akut - Bhs InggrisДокумент27 страницGagal Ginjal Akut - Bhs InggrisAgustinusОценок пока нет
- Novel Aspects of Pharmacological Therapies For Acute Renal FailureДокумент16 страницNovel Aspects of Pharmacological Therapies For Acute Renal FailureproluvieslacusОценок пока нет
- Prevention and Management AKIДокумент24 страницыPrevention and Management AKIZulhendraОценок пока нет
- The Definition of Acute Kidney Injury and Its Use in PracticeДокумент12 страницThe Definition of Acute Kidney Injury and Its Use in PracticeErwin SiahaanОценок пока нет
- Aetiology: Save Time & Improve Your PDP On Patient - Co.ukДокумент9 страницAetiology: Save Time & Improve Your PDP On Patient - Co.ukBaihaqi SaharunОценок пока нет
- Joacp 28 386Документ11 страницJoacp 28 386KrisztinaОценок пока нет
- Lecture 2. Acute Renal FailureДокумент85 страницLecture 2. Acute Renal FailurePharmswipe KenyaОценок пока нет
- Acute Kidney Injury and Chronic Kidney DiseaseДокумент44 страницыAcute Kidney Injury and Chronic Kidney DiseaseshihochanОценок пока нет
- Perioperative Acute Kidney Injury: DR Mukul Kapoor Director Anesthesia, Max Smart Super Specialty Hospital, Saket, DelhiДокумент46 страницPerioperative Acute Kidney Injury: DR Mukul Kapoor Director Anesthesia, Max Smart Super Specialty Hospital, Saket, DelhiChiragОценок пока нет
- Kdoki y KdigoДокумент24 страницыKdoki y KdigoIsrael Armida SodanargОценок пока нет
- AKI Perioperatif 3Документ6 страницAKI Perioperatif 3Kevin JohanesОценок пока нет
- Renal Management in The Critically Ill PatientДокумент16 страницRenal Management in The Critically Ill PatientAbygail RHОценок пока нет
- Acute Kidney Injury 2Документ15 страницAcute Kidney Injury 2Manish VijayОценок пока нет
- Acute Kidney Injury An UpdateДокумент9 страницAcute Kidney Injury An Updatekarol fernandezОценок пока нет
- Acute Renal Failure in NeonatesДокумент15 страницAcute Renal Failure in NeonatesSomendra Mohan ShuklaОценок пока нет
- Acute Kidney InjuryДокумент17 страницAcute Kidney InjuryCha-cha UzumakiОценок пока нет
- ACUTE KIDNEY INJURY by Dr. Monday Jacob ZaccheausДокумент70 страницACUTE KIDNEY INJURY by Dr. Monday Jacob ZaccheausDr. Amb. Monday ZaccheausОценок пока нет
- Surgery in The Patient With Renal DysfunctionДокумент11 страницSurgery in The Patient With Renal DysfunctionAps CnjОценок пока нет
- Pulsenotes - Chronic Kidney Disease NotesДокумент12 страницPulsenotes - Chronic Kidney Disease NotesElay PedrosoОценок пока нет
- Pharmacotherapy of Renal DisordersДокумент231 страницаPharmacotherapy of Renal DisordersTewodros GetahunОценок пока нет
- Essential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsДокумент5 страницEssential Update: FDA Approves First Test To Predict AKI in Critically Ill PatientsRika Ariyanti SaputriОценок пока нет
- A Comparison of The RIFLE and AKIN Criteria For Acute Kidney InjuryДокумент6 страницA Comparison of The RIFLE and AKIN Criteria For Acute Kidney InjuryFranciana AzêdoОценок пока нет
- Acute Kidney InjuryДокумент29 страницAcute Kidney InjuryElison J PanggaloОценок пока нет
- Kidney Injury: AcuteДокумент14 страницKidney Injury: AcutealfredoibcОценок пока нет
- NHS England AKI Webinar Final Version AaaaaaaaaaaaaadsadadaДокумент18 страницNHS England AKI Webinar Final Version AaaaaaaaaaaaaadsadadaAlmen Pandangan AdjulОценок пока нет
- Acute Kidney Injury: On Completion of This Chapter, The Learner Will Be Able ToДокумент9 страницAcute Kidney Injury: On Completion of This Chapter, The Learner Will Be Able TojhcacbszkjcnОценок пока нет
- Primary Care Approach To Management of CKD: February 2018Документ15 страницPrimary Care Approach To Management of CKD: February 2018AbedDabajaОценок пока нет
- Problem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureДокумент48 страницProblem 3.12 Study Guide 1 Causes of Renal Failure 1. Discuss The Causes of Acute (Pre-Renal, Renal and Post-Renal) and Chronic Renal FailureAnishilОценок пока нет
- Managing Chronic Kidney Disease PrimaryДокумент18 страницManaging Chronic Kidney Disease Primaryhusnaforever100% (1)
- Global Epidemiology and Outcomes of Acute Kidney InjuryДокумент19 страницGlobal Epidemiology and Outcomes of Acute Kidney Injuryredouane bennaiОценок пока нет
- Acute Kidney Injury: Diagnosis and ManagementДокумент8 страницAcute Kidney Injury: Diagnosis and ManagementfadelОценок пока нет
- Emergencydepartment Managementofacute Kidneyinjury, Electrolyte Abnormalities, Andrenal Replacementtherapyinthe CriticallyillДокумент13 страницEmergencydepartment Managementofacute Kidneyinjury, Electrolyte Abnormalities, Andrenal Replacementtherapyinthe CriticallyillAlejandro OlivaОценок пока нет
- Pediatric Acute Kidney Injury: Focusing On Diagnosis and ManagementДокумент8 страницPediatric Acute Kidney Injury: Focusing On Diagnosis and ManagementIrkania PasangkaОценок пока нет
- Restoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisОт EverandRestoring Chronic Kidney Disease : Restoring, Preserving, and Improving CKD to Avoid DialysisОценок пока нет
- Campinha Bacote ModelДокумент2 страницыCampinha Bacote ModelApril Jane PanchoОценок пока нет
- Daftar Diagnosis Dan Kode BPJSДокумент18 страницDaftar Diagnosis Dan Kode BPJSeginagirsangОценок пока нет
- Annotated BibliographyДокумент20 страницAnnotated Bibliographyapi-347153077Оценок пока нет
- Labial Access For Lower TeethДокумент3 страницыLabial Access For Lower TeethHarish ChowdaryОценок пока нет
- Reading New E2 PDFДокумент50 страницReading New E2 PDFMary Jis100% (1)
- Abbott Alinity S FactSheetДокумент1 страницаAbbott Alinity S FactSheetInayat UllahОценок пока нет
- INTEGRIS COVID19Interpreting COVID19 Test Results7720Документ2 страницыINTEGRIS COVID19Interpreting COVID19 Test Results7720nellyОценок пока нет
- Or-Indicator Measure Profile-Kpi-6.4 Day Surgery Conversion To AdmissionДокумент2 страницыOr-Indicator Measure Profile-Kpi-6.4 Day Surgery Conversion To Admissionangeli punoОценок пока нет
- Prenatal and Postnatal: DevelopmentДокумент22 страницыPrenatal and Postnatal: DevelopmentenergygapОценок пока нет
- A Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyДокумент9 страницA Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Drug-Addiction-Biology ProjectДокумент37 страницDrug-Addiction-Biology ProjectAhalya Bai SahooОценок пока нет
- Personal Development Plan Learner TemplateДокумент2 страницыPersonal Development Plan Learner TemplateDhaval VaghaniОценок пока нет
- Shah 2000Документ4 страницыShah 2000Ardian AshadiОценок пока нет
- Tutorial Questions 1Документ1 страницаTutorial Questions 1Kaite walker MutaleОценок пока нет
- Adult CardДокумент4 страницыAdult CardagelsantosОценок пока нет
- s1299 Can Alpha Feto Protein Level Be Used As A.1299Документ2 страницыs1299 Can Alpha Feto Protein Level Be Used As A.1299Chia Diamante NegroОценок пока нет
- Choosing WiselyДокумент4 страницыChoosing WiselyCarlos R. CantaleОценок пока нет
- Essentials of Medical Writing: Drug Discovery and Clinical ResearchДокумент15 страницEssentials of Medical Writing: Drug Discovery and Clinical ResearchanuОценок пока нет
- DR Sandeep Dewan Webinar InvitationДокумент3 страницыDR Sandeep Dewan Webinar InvitationShehbaz ThakurОценок пока нет
- Mono Propolis - Oral EnglishДокумент8 страницMono Propolis - Oral EnglishTom DelongeОценок пока нет
- Icao Health-Related DocumentsДокумент30 страницIcao Health-Related DocumentsVitor Hugo FreitasОценок пока нет
- IDS - Tuberculosis (Dr. Sy)Документ5 страницIDS - Tuberculosis (Dr. Sy)Renrenz PayumoОценок пока нет
- St. Paul University Philippines: School of Nursing and Allied Health SciencesДокумент12 страницSt. Paul University Philippines: School of Nursing and Allied Health SciencesKarina MadriagaОценок пока нет
- Research On Social Work Practice: PurposeДокумент10 страницResearch On Social Work Practice: PurposeMAHESH KOUJALAGIОценок пока нет
- CV SafiaДокумент4 страницыCV Safiaarshi khanОценок пока нет