Академический Документы
Профессиональный Документы
Культура Документы
Final Copy of Lesson Plan 1st Topic
Загружено:
manish dafdaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Final Copy of Lesson Plan 1st Topic
Загружено:
manish dafdaАвторское право:
Доступные форматы
Lesson plan
Name of the student teacher : Ms. Pooja Rana
Topic : Teaching on Dermatitis
Group : 2nd year B.sc Nursing
Method of teaching : lecture cum discussion
Teaching Aids : power point presentation, black board, chart
Date : 3//2017
Time : 10am to 11am
Duration of Teaching : 60 min
Venue : 2nd year B.sc. Nursing class room
General Objective : After the completion of the topic, the students will be able to understand about Dermatitis
Specific objectives:
1) Introduce of the topic
2) Explain the definition of the dermatitis.
3) Describe the main causes and signs and symptoms of dermatitis.
4) Explain about medical management of dermatitis.
5) Discuss about the prevention and nursing care of the patient with dermatitis.
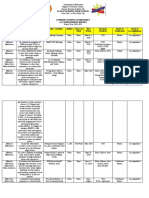
TIME ACTIVITES A.V. EVALUATION
SPECIFIC
CONTENT
(MINUTES) OBJECTIVES Teacher Student AIDS
INRODUCTION:-
1min Introduce the topic Lecture Listening Powerpoint What you think
method carefully and chalkboard about
1. Dermatitis is a general term for skin dermatitis?
inflammation. The skin will typically look dry,
swollen and red. The condition can have many
causes but its not contagious. Dermatitis can
have many causes and occurs in many forms.
It usually involves an itchy rash on swollen,
reddened skin.
2. Skin affected by dermatitis may blister, ooze,
develop a crust or flake off. Examples of
dermatitis include atopic dermatitis (eczema),
dandruff and rashes caused by contact with
any of a number of substances such as poison,
.
soap and jewellery with nickel in it.
Lecture Listening powerpoint
2min Definition of the • A medical condition in which the skin becomes
method carefully What is the
dermatitis red, swollen, sore, and sometimes with small
definition of
blisters resulting from direct irritation of the
dermatitis?
skin by an external agent or an allergic reaction
to it.
5mins Causes of • ENVIRONMENTAL Lecture cums Listen Powerpoint, Causes of
dermatitis discussion carefully and chalkboard and dermatitis?
• GENETIC participate in chart
discussion
Signs and Lecture cums Listen
5mins symptoms of 1: Redness discussion carefully and Powerpoint Signs and
dermatitis. 2; Itching participate in presentation symptoms of
discussion dermatitis?
3: Swelling
4: Painful cracks
5: Blisters
3mins Diagnostic methods • HISTORY COLLECTION
• PHYSICAL EXAMINATION Diagnostic
Lecture cums methods of
discussion Listen Powerpoint
• SKIN BIOPSY dermatitis?
carefully and presentation
participate in
discussion
• ATOPIC: Atopic dermatitis is an allergic
disease believed to have a hereditary to have a
10min Common types of hereditary component and often runs in
dermatitis. families whose members have asthma. Itchy
rash is particularly noticeable on head and
scalp, neck, inside of elbows, behind knees, Lecture cums Participate in Powerpoint Types of
and buttocks. It is very common in developed Discussion discussion and chalkboard dermatitis?
countries, and rising. Irritant contact dermatitis method
is sometimes misdiagnosed as atopic dermatitis
CONTACT: Contact dermatitis is of two
types:
Allergic: Resulting from a delayed
reaction to an allergen, such as poison
ivy, nickel, or balsam of peru .
Irritant: Resulting from direct reaction
to a detergent, such as sodium lauryl
sulphate, for example.
• SEBORRHEIC: Is a condition sometimes
classified as a form of eczema that is closely
related to dandruff. It causes a thick, yellow,
crusty scalp rash called cradle cap, which seems
related to lack of biotin and is often curable.
Age: Dermatitis can occur at any age, but atopic
dermatitis (eczema) usually begins in infancy.
10min Risk factors
Allergies and asthma: People who have a
personal or family history of eczema, allergies, Lecture cums Listening and Powerpoint Risk factors of
hay fever or asthma are more likely to develop discussion participate in and chalkboard dermatitis?
atopic dermatitis. method. discussion
Occupation: Jobs that put you in contact with
certain metals, solvents or cleaning supplies
increase your risk of contact dermatitis. Being a
health care worker is linked to hand eczema.
Health conditions: You may be at increased
risk of seborrheic dermatitis if you have one of
a number of conditions, such as congestive heart
failure, Parkinson's disease and HIV.
Complications: Scratching the itchy rash
associated with dermatitis can cause open sores,
which may become infected. These skin
infections can spread and may very rarely
become life-threatening.
Avoiding dry skin may be one factor in helping
you prevent dermatitis. These tips can help you
minimize the drying effects of bathing on your
skin:
10min Prevention of Take shorter baths or showers. Limit your baths
dermatitis. and showers to 5 to 10 minutes. And use warm,
rather than hot, water. Bath oil also may be helpful.
Use nonsoap cleansers or gentle soaps. Choose Discussion Participate in Powerpoint How can we
fragrance-free nonsoap cleansers or mild soaps. method. discussion and chalkboard prevent
Some soaps can dry your skin. dermatitis?
Dry yourself carefully. After bathing, brush your
skin rapidly with the palms of your hands, or gently
pat your skin dry with a soft towel.
Moisturize your skin. While your skin is still
damp, seal in moisture with an oil or a cream. Try
different products to find one that works for you.
Ideally, the best one for you will be safe, effective,
affordable and unscented.
• There is no known cure for some types of
dermatitis, with treatment aiming to control
symptoms by reducing inflammation and
relieving itching. Contact dermatitis is treated
by avoiding what is causing it.
• Lifestyle: Bathing once or more a day is
recommended, usually for five to ten minutes in
warm water. Soaps should be avoided as they
10mins tend to strip the skin of natural oils and lead to Discussion
excessive dryness. method.
• Moisturizers: Low-quality evidence indicates
that moisturizing agents may reduce eczema
severity and lead to fewer flares. Products that
contain dyes, perfumes, or peanuts should not be
used.
• Medications: There is little evidence
for antihistamine; they are thus not generally
recommended. Sedative antihistamines, such
as diphenhydramine, may be tried in those who
are unable to sleep due to eczema. Topical
immunosuppresants like pimecrolimus and
tacrolimus may be better in the short term and
appear equal to steroids after a year of use. Their
use is reasonable in those who do not respond to
or are not tolerant of steroids.
• DEFINITION
5mins • SIGNS AND SYMPTOMS
• CAUSES
• DIAGNOSIS
• COMMON TYPES
• RISK FACTORS
• PREVENTION
• MANAGEMENT
Вам также может понравиться
- Lession Plan of DermatitisДокумент5 страницLession Plan of Dermatitismanish dafdaОценок пока нет
- Teaching Plan Scabies 11Документ4 страницыTeaching Plan Scabies 11umar khan0% (1)
- Lesson Plan ON Benign Prostatic HyperplasiaДокумент26 страницLesson Plan ON Benign Prostatic HyperplasiaBlessy Madhuri75% (4)
- Diet in HypertensionДокумент9 страницDiet in Hypertension421Karanbir Kaur100% (1)
- Lesson Plan ON Diabetes Mellitus: Presented by Swatilekha DasДокумент6 страницLesson Plan ON Diabetes Mellitus: Presented by Swatilekha Dasramzan aliОценок пока нет
- Lession Plan For PracticalsДокумент12 страницLession Plan For PracticalsBHUKYA USHARANI100% (2)
- Lesson Plan Colostomy IrigationДокумент18 страницLesson Plan Colostomy IrigationAnuradha Maurya67% (3)
- Orientation Report of UHTCДокумент7 страницOrientation Report of UHTCDiksha chaudhary100% (1)
- Breast Cancer Lesson PlanДокумент20 страницBreast Cancer Lesson PlanBharat Singh Banshiwal100% (2)
- MT - Maleria (1) Rupesh KumarДокумент12 страницMT - Maleria (1) Rupesh KumarTopeshwar TpkОценок пока нет
- Lesson PlanДокумент29 страницLesson PlanSiva072680% (5)
- Unit Plan CHNДокумент3 страницыUnit Plan CHNParampal KaurОценок пока нет
- Peptic Ulcer LPДокумент8 страницPeptic Ulcer LPAnonymous 0C4OZmR100% (2)
- Lesson Plan On TumorsДокумент19 страницLesson Plan On TumorsPuneetОценок пока нет
- Seminar On Biomedical Waste Management: By:-Gamit NikitaДокумент29 страницSeminar On Biomedical Waste Management: By:-Gamit Nikitahiral mistryОценок пока нет
- Lesson Plan MIДокумент14 страницLesson Plan MIAnand Bhawna100% (1)
- Ear InstillationДокумент2 страницыEar InstillationTrisha Apillanes100% (2)
- Lesson Plan On PeritonitisДокумент12 страницLesson Plan On PeritonitisDimpal Choudhary100% (7)
- Lesson Plan ON AneurysmДокумент8 страницLesson Plan ON AneurysmAnusikta PandaОценок пока нет
- Lesson Plan On Lung CancerДокумент10 страницLesson Plan On Lung CancerPankaj Jena100% (1)
- Time Specific Objective Content Teachin G Learning Activity Av Aids EvaluationДокумент7 страницTime Specific Objective Content Teachin G Learning Activity Av Aids Evaluationrittika dasОценок пока нет
- Case Presentation 3 DR Oscar Laryngitis TBДокумент33 страницыCase Presentation 3 DR Oscar Laryngitis TBmarajuu50% (2)
- Lesson Plan On Wound CareДокумент5 страницLesson Plan On Wound CareA J Fathima0% (1)
- Cataracts Teaching PlanДокумент4 страницыCataracts Teaching PlanShaina Diya100% (1)
- Nursing Procedure Checklist: Administering An Eye IrrigationДокумент1 страницаNursing Procedure Checklist: Administering An Eye IrrigationOrl Trinidad100% (1)
- Lesson Plan MSN 1Документ14 страницLesson Plan MSN 1SHREE SWAMINARAYAN NURSING COLLEGE CHIKHLIОценок пока нет
- Lesson Plan On Myocardial Infarction: TimeДокумент17 страницLesson Plan On Myocardial Infarction: TimeRio Rio100% (1)
- Nursing Education Lesson Plan On Intradermal InjectionДокумент12 страницNursing Education Lesson Plan On Intradermal InjectionNisha MwlzОценок пока нет
- LP ArfДокумент7 страницLP ArfAnonymous 0C4OZmRОценок пока нет
- Health Talk On BSFДокумент11 страницHealth Talk On BSFjyoti singh100% (1)
- Cirrhosis of Liver New Lesson PlaneДокумент17 страницCirrhosis of Liver New Lesson PlaneKrini Tandel100% (6)
- LESSON PLAN ON Hand WashingДокумент3 страницыLESSON PLAN ON Hand Washinganimesh panda50% (2)
- Sno Specific Objectives Duratio N Content Teacher /learning Av Aids B/B Activity EvaluationДокумент9 страницSno Specific Objectives Duratio N Content Teacher /learning Av Aids B/B Activity Evaluationjasmine100% (2)
- Tracheostomy Care Lesson PlanДокумент26 страницTracheostomy Care Lesson PlanShubha JeniferОценок пока нет
- Bed BathДокумент11 страницBed Bathramtenki sreelekha100% (1)
- Class 2 Lesson PlanДокумент16 страницClass 2 Lesson PlanArjun Neupane100% (1)
- TubercolosisДокумент8 страницTubercolosisNitesh Bhura100% (1)
- Lesson Plan On Ryle'S Tube FeedingДокумент9 страницLesson Plan On Ryle'S Tube FeedingPriyanka Nilewar100% (5)
- Hypothyroidism Lesson PlanДокумент20 страницHypothyroidism Lesson PlanDimpal Choudhary50% (2)
- Lesson Plan ON "Hernias" Child Health Nursing: Submitted To: Submitted byДокумент13 страницLesson Plan ON "Hernias" Child Health Nursing: Submitted To: Submitted byNitesh sharma100% (6)
- Leukemia Lesson PlanДокумент3 страницыLeukemia Lesson PlanIshika Roy75% (4)
- Abdominal ParacentesisДокумент5 страницAbdominal ParacentesisSivaprasad S100% (1)
- Demo Eye IrrigationДокумент5 страницDemo Eye IrrigationSachin Dwivedi100% (4)
- Lesson Plan Chemo CHNДокумент31 страницаLesson Plan Chemo CHNGiri Siva100% (2)
- Lesson Plan Lumbar PunctureДокумент19 страницLesson Plan Lumbar PunctureLoma Waghmare (Jadhav)Оценок пока нет
- LESSON PLAN - Peptic Ulcer - MDДокумент11 страницLESSON PLAN - Peptic Ulcer - MDmohamad dildar100% (3)
- MT Vitals Signs - RespirationДокумент11 страницMT Vitals Signs - RespirationpriyankaОценок пока нет
- GlaucomaДокумент15 страницGlaucomapreethijojo20035582100% (5)
- Filaria - Final 4Документ14 страницFilaria - Final 4Arun Jv100% (1)
- Micro Teaching 2Документ15 страницMicro Teaching 2kathyayani arraОценок пока нет
- LESSON PLAN ON Hand Washing ProcedureДокумент19 страницLESSON PLAN ON Hand Washing ProcedurePrabh Gill75% (4)
- Types of Reconstructive & Cosmetic SurgeryДокумент28 страницTypes of Reconstructive & Cosmetic SurgerySimon JosanОценок пока нет
- Av AidsДокумент10 страницAv AidsMadhu Bala100% (1)
- Lesson Plan On Intestinal ObstructionДокумент41 страницаLesson Plan On Intestinal ObstructionLoma Waghmare (Jadhav)100% (1)
- Lesson Plan of HepatitisДокумент8 страницLesson Plan of HepatitisAshish Gupta100% (1)
- 3.FIRST AID Snakebite LESSON PLANДокумент8 страниц3.FIRST AID Snakebite LESSON PLANdew2375% (4)
- Nursing Management of Patients Occupational and Industrial DisordersДокумент11 страницNursing Management of Patients Occupational and Industrial DisordersNandini VermaОценок пока нет
- EczemaДокумент13 страницEczemaCollective123Оценок пока нет
- Diagnosis Banding EritrasmaДокумент7 страницDiagnosis Banding EritrasmaIde Yudis TiyoОценок пока нет
- Refka-Fixed Drug EruptionДокумент11 страницRefka-Fixed Drug EruptionSandiОценок пока нет
- Learning PDFДокумент2 страницыLearning PDFmanish dafdaОценок пока нет
- Acute and Chronic Renal FailureДокумент15 страницAcute and Chronic Renal Failuremanish dafdaОценок пока нет
- Polycystic KidneyДокумент10 страницPolycystic Kidneymanish dafdaОценок пока нет
- 3rd Year Academic CalenderДокумент1 страница3rd Year Academic Calendermanish dafdaОценок пока нет
- COPDДокумент50 страницCOPDmanish dafdaОценок пока нет
- Common COldДокумент17 страницCommon COldmanish dafdaОценок пока нет
- Bronchitisori 131023102922 Phpapp01Документ13 страницBronchitisori 131023102922 Phpapp01manish dafdaОценок пока нет
- Nursing MGT of Patient With Immunological Problems: By: Pooja RanaДокумент8 страницNursing MGT of Patient With Immunological Problems: By: Pooja Ranamanish dafdaОценок пока нет
- Endocrine SystemДокумент1 страницаEndocrine Systemmanish dafdaОценок пока нет
- ASTHMAДокумент72 страницыASTHMAmanish dafdaОценок пока нет
- By: Miss - Pooja Rana Clinical InstructorДокумент33 страницыBy: Miss - Pooja Rana Clinical Instructormanish dafdaОценок пока нет
- Child Guidance ClinicДокумент12 страницChild Guidance Clinicmanish dafda0% (1)
- Acute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, HubliДокумент22 страницыAcute Respiratory Distress Syndrome (ARDS) : MR Sanjay. M. Peerapur, Principal, KLES Institute of Nursing Sciences, Hublimanish dafdaОценок пока нет
- SomnabulismДокумент18 страницSomnabulismmanish dafdaОценок пока нет
- With A Healthy Heart, The Beat Goes On.Документ4 страницыWith A Healthy Heart, The Beat Goes On.manish dafdaОценок пока нет
- Caste Study of NephritisДокумент25 страницCaste Study of Nephritismanish dafdaОценок пока нет
- Final Copy of Lesson Plan 1st TopicДокумент9 страницFinal Copy of Lesson Plan 1st Topicmanish dafdaОценок пока нет
- Rooming in and KMCДокумент10 страницRooming in and KMCmanish dafdaОценок пока нет
- Demographic DataДокумент7 страницDemographic Datamanish dafdaОценок пока нет
- Most Important Electrical Engineering NTS Based Short QuestionsДокумент63 страницыMost Important Electrical Engineering NTS Based Short QuestionsnageenОценок пока нет
- 1101259L 580.752830 Pressure Washer ManualДокумент64 страницы1101259L 580.752830 Pressure Washer Manualgork1roguesОценок пока нет
- NWO Plans Exposed by Insider in 1969Документ36 страницNWO Plans Exposed by Insider in 1969Stig Dragholm100% (3)
- Savage Inequalities Reading ReflectionДокумент2 страницыSavage Inequalities Reading Reflectionapi-367127133Оценок пока нет
- La Paz National High SchoolДокумент19 страницLa Paz National High SchoolBon Ivan FirmezaОценок пока нет
- The Assignment Vol.4 - The Pain - Mike Murdock PDFДокумент168 страницThe Assignment Vol.4 - The Pain - Mike Murdock PDFEmmanuel Temiloluwa67% (3)
- LPG PropertiesДокумент2 страницыLPG Propertiesvvk557Оценок пока нет
- Megapower: Electrosurgical GeneratorДокумент45 страницMegapower: Electrosurgical GeneratorAnibal Alfaro VillatoroОценок пока нет
- Jurnal Aquaponik Jada BahrinДокумент36 страницJurnal Aquaponik Jada BahrinbrentozОценок пока нет
- Numerical Modelling of Brine Dispersion in Shallow Coastal WatersДокумент13 страницNumerical Modelling of Brine Dispersion in Shallow Coastal WatersIAEME PublicationОценок пока нет
- Blotter EntryДокумент2 страницыBlotter EntryCharline Khie Silvestra PortemCamposanoОценок пока нет
- TD-XT-D004-003 V2.00 20131204 XG1.UCD-135M185M300M Operation Manual PDFДокумент47 страницTD-XT-D004-003 V2.00 20131204 XG1.UCD-135M185M300M Operation Manual PDFStan TC100% (1)
- Excel HysysДокумент11 страницExcel HysysAndrie Kurniawan IndraОценок пока нет
- 06 - Flexible Operation of Thermal Power Plants - OEM Perspective and Experiences PDFДокумент22 страницы06 - Flexible Operation of Thermal Power Plants - OEM Perspective and Experiences PDFRavishankarОценок пока нет
- Basic Electrical Engineering Mcqs Unit 1Документ13 страницBasic Electrical Engineering Mcqs Unit 1shubha christopherОценок пока нет
- World Wide Emission Free E-Motercycle ProjectДокумент20 страницWorld Wide Emission Free E-Motercycle ProjectAkshay SharmaОценок пока нет
- Dialysis and ElectrodialysisДокумент32 страницыDialysis and ElectrodialysisJuan CarvajalОценок пока нет
- Production of AcetaldehydeДокумент124 страницыProduction of AcetaldehydeAdilaAnbreen80% (5)
- Tibia Bone Segmentation in X-Ray Images - A Comparative AnalysisДокумент8 страницTibia Bone Segmentation in X-Ray Images - A Comparative AnalysisSuzanaPetrovicОценок пока нет
- English 10-1 Personal Response EssayДокумент2 страницыEnglish 10-1 Personal Response Essayapi-467840192Оценок пока нет
- SOP-M-003 Device Master Record Rev AДокумент3 страницыSOP-M-003 Device Master Record Rev AAnil Chowadary Anil ChowadaryОценок пока нет
- Cell Division-Mitosis Notes: 2 New CellsДокумент21 страницаCell Division-Mitosis Notes: 2 New CellsCristina MariaОценок пока нет
- 6 Human Diseases That Cause by VirusesДокумент7 страниц6 Human Diseases That Cause by VirusesJefry JapОценок пока нет
- Michigan Clinic 2008 NotesДокумент10 страницMichigan Clinic 2008 NotesCoach Brown100% (3)
- Winchester Model 9422 Lever Action Rifle Owner's Manual: LicenseeДокумент0 страницWinchester Model 9422 Lever Action Rifle Owner's Manual: Licenseecarlosfanjul1Оценок пока нет
- Premium Connections Catalogue ENGДокумент134 страницыPremium Connections Catalogue ENGsubzwarijОценок пока нет
- 2nd Comprehensive ExamДокумент15 страниц2nd Comprehensive ExamLoala SMDОценок пока нет
- Assignment PSДокумент2 страницыAssignment PSMohsin Islam RifatОценок пока нет
- Bai Tap Anh 9 Tuan 19202122 - 2032023135013Документ21 страницаBai Tap Anh 9 Tuan 19202122 - 2032023135013Duy HoangОценок пока нет
- API 16C ErrataДокумент1 страницаAPI 16C ErrataDinesh KumarОценок пока нет