Академический Документы
Профессиональный Документы
Культура Документы
Nsaids For Chronic Low Back Pain: Jama Clinical Evidence Synopsis
Загружено:
tanyasisОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Nsaids For Chronic Low Back Pain: Jama Clinical Evidence Synopsis
Загружено:
tanyasisАвторское право:
Доступные форматы
Clinical Review & Education
JAMA Clinical Evidence Synopsis
NSAIDs for Chronic Low Back Pain
Wendy T. M. Enthoven, MD, PhD; Pepijn D. Roelofs, PhD; Bart W. Koes, PhD
CLINICAL QUESTION Arenonsteroidalanti-inflammatorydrugs(NSAIDs)associatedwithgreaterpain
relief than placebo, other drugs, and nondrug treatments for patients with chronic low back pain?
BOTTOM LINE Compared with placebo, NSAIDs are associated with a small but significant
improvement in pain and disability in patients with chronic low back pain, although this
difference became nonsignificant when studies with high risk for bias were excluded. The
associated benefits were smaller than the minimal clinically important difference.
Introduction low-quality evidence that NSAIDs were associated with greater ben-
Chroniclowbackpain(lasting>3months)isacommonhealthproblem. efit than placebo for the outcome of disability. The mean difference
Nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most from baseline was −0.85 (95% CI, −1.30 to −0.40) on a 0-to-24 visual
prescribedmedicationsandarefrequentlyusedbypatientswithchronic analog scale. The minimal clinically important change was 3.5 points.7
lowbackpain.1,2 Clinicalpracticeguidelinesrecommendshort-termuse Six studies reported adverse events. NSAIDs were not associ-
ofNSAIDsforpainreliefinpatientswithchroniclowbackpain,buttheir ated with higher rates of adverse events vs placebo (735 vs 619 events;
efficacy is still unclear.3,4 This JAMA Clinical Evidence Synopsis summa- relative risk [RR], 1.04, 95% CI, 0.92 to 1.17). When randomized clini-
rizes a Cochrane review5 on the association of NSAIDs with pain relief cal trials (RCTs) with high risk of bias were excluded, the associated
and adverse events for patients with chronic low back pain. benefits were smaller and the difference was not statistically signifi-
cant (pain: −5.03 [95% CI, −10.37 to 0.32]; disability: −0.41 [95% CI,
Summary of Findings
−1.04 to 0.23]). Three studies comparing different types of NSAIDs
Sixofthe13studiescomparedNSAIDswithplacebo(n = 1354)(Figure).
and studies comparing NSAIDs with paracetamol (acetaminophen)
There was low-quality evidence based on the Grades of Recommen-
(n = 30) and pregabalin (n = 36) were too heterogeneous for a
dation, Assessment, Development and Evaluation assessment6 that
quantitative meta-analysis. All reported no associated differences in
NSAIDswereassociatedwithstatisticallysignificantgreaterbenefitthan
pain and disability. One trial showed a better overall improvement
placeboforpainintensity.Themeandifferencefrombaselinewas−6.97
in pain from baseline, favoring celecoxib vs tramadol (508 of 798 pa-
(95% CI, −10.74 to −3.19) on a 0-to-100 visual analog scale and the
tients [64%] vs 412 of 785 patients [52%] improved by ⱖ30%, re-
median follow-up was 56 days (interquartile range, 13 to 91 days). For
spectively; RR, 1.20 [95% CI, 1.11 to 1.32]). One trial compared NSAIDs
patientswithchronicbackpain,theminimalclinicallyimportantchange
with home-based exercise (n = 201) and disability improved more in
was at least 20 mm.7 Four studies measured disability. There was
participants who exercised, but the pain scores were not different.
Discussion
Evidence Profile
TheresultsshowedthatNSAIDswereassociatedwithgreaterimprove-
No. of randomized clinical trials: 13 ment in pain intensity and disability compared with placebo. However,
Study years: 1981-2011 (conducted); 1982-2013 (published) the magnitude of the association was small, the quality of the evidence
Last search date: June 24, 2015 was low, and the statistical heterogeneity was high. There were no as-
No. of patients: 4807 sociations between type of NSAID and pain scores, although the num-
Men: 2067 (43%) Women: 2740 (57%) ber of trials was small. Two trials used an enriched enrollment design,
in which only participants who responded well to NSAIDs before ran-
Race/ethnicity: Not reported
domization were enrolled. These trials may overestimate the associa-
Age, mean: 49.7 years
tion of NSAIDs with benefit and reduce the external validity.
Clinical settings: General practice and outpatient Almost all RCTs mentioned adverse events. However, trials
Countries: Australia, Belgium, Brazil, Canada, Costa Rica, Czech lacked statistical power and follow-up periods were too short to in-
Republic, Denmark, Ecuador, Finland, France, Germany, Hong vestigate serious adverse events. Therefore, conclusions regard-
Kong, Hungary, Italy, Japan, New Zealand, Norway, Peru, Portugal,
ing the association of NSAIDs with adverse events cannot be made.
Russian Federation, Singapore, Sweden, Taiwan, Thailand, United
Arab Emirates, United Kingdom, United States, Venezuela The literature search was updated on September 16, 2016. One
study was identified that compared celecoxib with paracetamol
Comparison: NSAIDs vs placebo, paracetamol/acetaminophen, other
types of NSAIDs, pregabalin, tramadol, and home-based exercise (acetaminophen) in 50 participants.8 In this trial,8 celecoxib improved
pain and disability compared with paracetamol. No other trials in the
Primary outcome measures: Pain intensity, global measure
(eg, overall improvement), back pain–specific functional Cochrane review compared celecoxib with paracetamol. One trial in-
status (eg, Roland Disability Questionnaire), adverse events cluded in the Cochrane review reported no difference in outcomes
between the NSAID diflunisal compared with paracetamol.
jama.com (Reprinted) JAMA June 13, 2017 Volume 317, Number 22 2327
© 2017 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936301/ by a University of Massachusetts Amherst User on 06/13/2017
Clinical Review & Education JAMA Clinical Evidence Synopsis
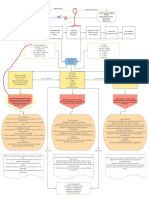
Figure. Associations of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) With Pain and Disability for Chronic Low Back Pain vs Placebo
A Mean change in pain intensity from baseline on 100-mm visual analog scalea
NSAID Placebo
Total No. of Total No. of Mean Difference Favors Favors
Source Participants Mean (SD) Participants Mean (SD) (95% CI)b NSAID Placebo Weight, %
Allegrini, 2009 60 –28 (31.7) 59 –16.5 (31.7) –11.50 (–22.89 to –0.11) 8.4
Berry, 1982 37 –11.5 (34) 37 9.4 (34) –20.90 (–36.39 to –5.41) 5.1
Birbara, 2003 107 –7.5 (23.3) 109 0 (23.3) –7.50 (–13.71 to –1.29) 18.2
Coats, 2004 148 –41.9 (27.7) 143 –31.1 (27.7) –10.80 (–17.17 to –4.43) 17.7
Katz, 2011 88 –2.4 (11.6) 41 0 (11.6) –2.40 (–6.70 to 1.90) 24.5
Kivitz, 2013 295 –4.1 (22.3) 230 0 (22.3) –4.10 (–7.94 to –0.26) 26.1
Total 735 619 –6.97 (–10.74 to –3.19) 100.0
–40 –30 –20 –10 0 10 20
Mean Difference (95% CI)
B Mean change in disability from baseline on 24-item Rowland-Morris Disability Questionnairec
NSAID Placebo
Total No. of Total No. of Mean Difference Favors Favors
Source Participants Mean (SD) Participants Mean (SD) (95% CI)d NSAID Placebo Weight, %
Birbara, 2003 107 –2.1 (5.3) 109 0 (5.3) –2.10 (–3.51 to –0.69) 10.1
Coats, 2004 148 –1.1 (3.1) 143 0 (3.1) –1.10 (–1.81 to –0.39) 39.7
Katz, 2011 88 –0.6 (3.1) 41 0 (3.1) –0.60 (–1.75 to 0.55) 15.3
Kivitz, 2013 295 –0.32 (4.4) 230 0 (4.4) –0.32 (–1.08 to 0.44) 35.0
Total 638 523 –0.85 (–1.30 to –0.40) 100.0
–4 –3 –2 –1 0 1 2
Mean Difference (95% CI)
c
The error bars indicate the 95% CIs. The size of the data markers corresponds Score range is 0 to 24; a higher number indicates more disability.
with the weight of the study. Follow-up was 16 weeks or shorter. d
A fixed-effects model was used for the analyses.
a
Score range is 0 to 100 mm; a higher number indicates more pain.
b
A random-effects model was used for the analyses.
Limitations American Pain Society guidelines on chronic back pain recommend
Strict inclusion criteria were used regarding the duration of back pain, the shortest duration possible.3,4 In the Cochrane review,5 there was
meaning that only trials reporting the results for patients with chronic low-quality evidence that NSAIDs are associated with improve-
low back pain were included. ment in pain and disability compared with placebo; however, the
strength of the association is small and clinically not meaningful.
Comparison of Findings With Current Practice Guidelines
Because of possible adverse effects, the European Guidelines of the Areas in Need of Future Study
Management of Chronic Low Back Pain recommend using NSAIDs Future research is needed to identify patients who are most likely
for up to 3 months, and the American College of Physicians and the to respond well to NSAIDs.
ARTICLE INFORMATION REFERENCES 5. Enthoven WT, Roelofs PD, Deyo RA, et al.
Author Affiliations: Department of General 1. Gore M, Tai KS, Sadosky A, et al. Use and costs of Non-steroidal anti-inflammatory drugs for chronic
Practice, Erasmus Medical Center, Rotterdam, the prescription medications and alternative low back pain. Cochrane Database Syst Rev. 2016;2:
Netherlands (Enthoven, Koes); Research Centre treatments in patients with osteoarthritis and CD012087.
Innovations in Care, Rotterdam University of chronic low back pain in community-based settings. 6. Cochrane. The GRADE approach.
Applied Sciences, Rotterdam, the Netherlands Pain Pract. 2012;12(7):550-560. http://handbook.cochrane.org/chapter_12/12_2_1
(Roelofs). 2. Piccoliori G, Engl A, Gatterer D, et al. _the_grade_approach.htm. Accessed March 31, 2017.
Corresponding Author: Wendy T. M. Enthoven, Management of low back pain in general practice. 7. Ostelo RW, de Vet HC. Clinically important
MD, PhD, Erasmus Medical Center, PO Box 2040, BMC Fam Pract. 2013;14:148. outcomes in low back pain. Best Pract Res Clin
3000 CA Rotterdam, the Netherlands 3. Airaksinen O, Brox JI, Cedraschi C, et al. Chapter Rheumatol. 2005;19(4):593-607.
(w.enthoven@erasmusmc.nl). 4. Eur Spine J. 2006;15(suppl 2):S192-S300. 8. Bedaiwi MK, Sari I, Wallis D, et al. Clinical efficacy
Section Editor: Mary McGrae McDermott, MD, 4. Chou R, Qaseem A, Snow V, et al. Diagnosis and of celecoxib compared to acetaminophen in chronic
Senior Editor. treatment of low back pain. Ann Intern Med. nonspecific low back pain. Arthritis Care Res
Conflict of Interest Disclosures: The authors have 2007;147(7):478-491. (Hoboken). 2016;68(6):845-852.
completed and submitted the ICMJE Form for
Disclosure of Potential Conflicts of Interest and
none were reported.
2328 JAMA June 13, 2017 Volume 317, Number 22 (Reprinted) jama.com
© 2017 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/936301/ by a University of Massachusetts Amherst User on 06/13/2017
Вам также может понравиться
- Kapandji EEIIДокумент244 страницыKapandji EEIIMarisa Piazze83% (6)
- President CEO Healthcare Administrator in Nashville TN Resume Kerry GillihanДокумент4 страницыPresident CEO Healthcare Administrator in Nashville TN Resume Kerry GillihanKerryGillihanОценок пока нет
- Critical Care Nurse Skills ChecklistДокумент4 страницыCritical Care Nurse Skills ChecklistMichael Silva0% (1)
- EXERCISE Stress Testing FOR HEARTДокумент52 страницыEXERCISE Stress Testing FOR HEARTBenjamin GonzalezОценок пока нет
- Hong-Geun JUNG (Eds.) - Foot and Ankle Disorders - An Illustrated Reference-Springer-Verlag Berlin Heidelberg (2016)Документ633 страницыHong-Geun JUNG (Eds.) - Foot and Ankle Disorders - An Illustrated Reference-Springer-Verlag Berlin Heidelberg (2016)tanyasisОценок пока нет
- Hong-Geun JUNG (Eds.) - Foot and Ankle Disorders - An Illustrated Reference-Springer-Verlag Berlin Heidelberg (2016)Документ633 страницыHong-Geun JUNG (Eds.) - Foot and Ankle Disorders - An Illustrated Reference-Springer-Verlag Berlin Heidelberg (2016)tanyasisОценок пока нет
- AtracuriumДокумент2 страницыAtracuriumFederico Andales50% (2)
- Animals Should Not Be Used As A Laboratory ToolsДокумент6 страницAnimals Should Not Be Used As A Laboratory ToolsLuisa Castillo100% (1)
- Diagnostic Criteria Decision Tree PDFДокумент2 страницыDiagnostic Criteria Decision Tree PDFNor Nadia ZakariaОценок пока нет
- HyllestedДокумент16 страницHyllestedJennifer GОценок пока нет
- JRMS 18 43Документ4 страницыJRMS 18 43Ricardo PietrobonОценок пока нет
- Non-Steroidal Anti-In Ammatory Drugs For Spinal Pain: A Systematic Review and Meta-AnalysisДокумент11 страницNon-Steroidal Anti-In Ammatory Drugs For Spinal Pain: A Systematic Review and Meta-AnalysistanyasisОценок пока нет
- Aines en Onco ResumenДокумент3 страницыAines en Onco ResumenEdgar P. Aguirre MilachayОценок пока нет
- Jama Busse 2018 Oi 180142Документ13 страницJama Busse 2018 Oi 180142Oumaima MoustahsineОценок пока нет
- 1516-3180-spmj-133-04-00383 Azka PDFДокумент1 страница1516-3180-spmj-133-04-00383 Azka PDFagustiawan28Оценок пока нет
- Tennis Elbow TreatmentДокумент3 страницыTennis Elbow TreatmentMurty MОценок пока нет
- JurnalДокумент2 страницыJurnalHamba AllahОценок пока нет
- Immunocal Children Cancer Page 11Документ14 страницImmunocal Children Cancer Page 11api-3714923Оценок пока нет
- สัมนาาาДокумент7 страницสัมนาาาBook AmornwadeeОценок пока нет
- Jama Krebs 2018 Oi 180013Документ11 страницJama Krebs 2018 Oi 180013Yeison UrregoОценок пока нет
- The Role of CBT in Relapse Prevention of SchizophreniaДокумент2 страницыThe Role of CBT in Relapse Prevention of SchizophreniaKorn IbraОценок пока нет
- Anterior Approach: Evidence SummaryДокумент6 страницAnterior Approach: Evidence SummaryAhmed DRIDIОценок пока нет
- Facet Joint Pain-Advances in Patient Selection and TreatmentДокумент16 страницFacet Joint Pain-Advances in Patient Selection and TreatmentthiagoОценок пока нет
- J Explore 2013 08 013Документ4 страницыJ Explore 2013 08 013ankitabhitale2000Оценок пока нет
- ArticuloДокумент15 страницArticuloGloria Villalpando SosaОценок пока нет
- 02 - Viscosupplementation For Knee Osteoarthritis - Systematic Review and Meta-Analysis (BMJ 2022)Документ14 страниц02 - Viscosupplementation For Knee Osteoarthritis - Systematic Review and Meta-Analysis (BMJ 2022)Nicolas ReyesОценок пока нет
- CATIENNTEditorialRegardingCITROME KERWIN IntJClinPract2006Документ2 страницыCATIENNTEditorialRegardingCITROME KERWIN IntJClinPract2006Leslie CitromeОценок пока нет
- Bai 2017Документ4 страницыBai 2017kurnia fitriОценок пока нет
- Benefits and Harms of Spinal Manipulative Therapy For The Treatment of Chronic Low Back PainДокумент15 страницBenefits and Harms of Spinal Manipulative Therapy For The Treatment of Chronic Low Back PainRachel PutriОценок пока нет
- Association Between Pain Control and Patient Satisfaction Outcomes in The Emergency Department SettingДокумент7 страницAssociation Between Pain Control and Patient Satisfaction Outcomes in The Emergency Department SettingSri Wahyuni YkОценок пока нет
- Effects of Acupuncture For The Treatment of Endometriosis-Related Pain: A Systematic Review and Meta-AnalysisДокумент15 страницEffects of Acupuncture For The Treatment of Endometriosis-Related Pain: A Systematic Review and Meta-AnalysisjjОценок пока нет
- 904nm - Bmjopen-2019-031142Документ13 страниц904nm - Bmjopen-2019-031142Gino DammiuncrodinoОценок пока нет
- 10 1056@nejm200105243442106 PDFДокумент9 страниц10 1056@nejm200105243442106 PDFRafael BomfimОценок пока нет
- The Effect of Vitamin D On Nonspecific Low Back Pain: Original ArticleДокумент5 страницThe Effect of Vitamin D On Nonspecific Low Back Pain: Original ArticleأبومحمدالزياتОценок пока нет
- Bmjopen 2021 051073Документ12 страницBmjopen 2021 051073Eugênio AraújoОценок пока нет
- (10920684 - Neurosurgical Focus) Novel Technique For Trialing Peripheral Nerve Stimulation - Ultrasonography-Guided StimuCath TrialДокумент7 страниц(10920684 - Neurosurgical Focus) Novel Technique For Trialing Peripheral Nerve Stimulation - Ultrasonography-Guided StimuCath TrialSebastiano SerraОценок пока нет
- No.6 Tzellos2008Документ8 страницNo.6 Tzellos2008harasthaОценок пока нет
- A Drug Burden Index To Define The Functional Burden of Medications in Older PeopleДокумент7 страницA Drug Burden Index To Define The Functional Burden of Medications in Older PeopleRidzqie DibyantariОценок пока нет
- The Following Abstracts of Articles From Leading Journals Have Been Selected On The Basis of Their Importance To The Practice of Obstetrics and GynecologyДокумент3 страницыThe Following Abstracts of Articles From Leading Journals Have Been Selected On The Basis of Their Importance To The Practice of Obstetrics and GynecologythereberryОценок пока нет
- We Wege 2018Документ11 страницWe Wege 2018Rocio SilleroОценок пока нет
- 2024 Clinical Relevance of Resistance Training in Women With FibromyalgiaДокумент16 страниц2024 Clinical Relevance of Resistance Training in Women With FibromyalgiaLina M GarciaОценок пока нет
- Part 5 VolДокумент6 страницPart 5 VolMoopsОценок пока нет
- Abstracts S13: A07 Guidelines, Systematic Reviews, and Meta-AnalysisДокумент1 страницаAbstracts S13: A07 Guidelines, Systematic Reviews, and Meta-AnalysiselianaОценок пока нет
- Pharmacotherapy For Diabetic Peripheral Neuropathy Pain and Quality of LifeДокумент11 страницPharmacotherapy For Diabetic Peripheral Neuropathy Pain and Quality of LifeAF KoasОценок пока нет
- 2022 - Lingyu - Acupuncture For The Treatment of Diarrhea-Predominant - EcaДокумент11 страниц2022 - Lingyu - Acupuncture For The Treatment of Diarrhea-Predominant - EcaesmargarОценок пока нет
- Journal Reading SarafДокумент10 страницJournal Reading SarafRifa RoazahОценок пока нет
- The Effect of Non-Steroidal Anti-Inflammatory Drugs On Severity of Acute Pancreatitis and Pancreatic NecrosisДокумент4 страницыThe Effect of Non-Steroidal Anti-Inflammatory Drugs On Severity of Acute Pancreatitis and Pancreatic NecrosisAracelyAcostaОценок пока нет
- Articles: BackgroundДокумент13 страницArticles: Backgroundaku siapaОценок пока нет
- Hershman2018 PDFДокумент10 страницHershman2018 PDFAndrie WigunaОценок пока нет
- 2015 Do Over The Counter Remedies Relieve Cough in Acute Upper Respiratory InfectionsДокумент2 страницы2015 Do Over The Counter Remedies Relieve Cough in Acute Upper Respiratory InfectionsDaniela Güiza ArgüelloОценок пока нет
- Gedin 2022 Oi 221233 1668781352.25734Документ12 страницGedin 2022 Oi 221233 1668781352.25734Dragutin PetrićОценок пока нет
- Intramuscular and Intravenous Opioid Pain Relieving Drugs in LabourДокумент2 страницыIntramuscular and Intravenous Opioid Pain Relieving Drugs in LabourFarhana KanakanОценок пока нет
- Original Research Article: Anurag Bijalwan, Pradeep Singhal, Syed AltamashДокумент7 страницOriginal Research Article: Anurag Bijalwan, Pradeep Singhal, Syed Altamashagus sukarnaОценок пока нет
- Safety and Efficacy of Pregabalin in Patients With Central Post - Stroke PainДокумент6 страницSafety and Efficacy of Pregabalin in Patients With Central Post - Stroke Painfahri azwarОценок пока нет
- Translate JurnalДокумент4 страницыTranslate JurnalnomustaОценок пока нет
- NIH Public Access: Acupuncture For Chronic PainДокумент8 страницNIH Public Access: Acupuncture For Chronic Painmazh21Оценок пока нет
- Pedoman Pelayanan Kefarmasian Untuk Terapi AntibiotikДокумент8 страницPedoman Pelayanan Kefarmasian Untuk Terapi AntibiotikWidya LestariОценок пока нет
- Jamapsychiatry Weiser 2019 Oi 190042Документ9 страницJamapsychiatry Weiser 2019 Oi 190042Bella LifindraОценок пока нет
- Evaluating The Effectiveness of Antidepressant Therapy Adjuvant To Gabapentin and Pregabalin For Treatment of SCI-related Neuropathic PainДокумент8 страницEvaluating The Effectiveness of Antidepressant Therapy Adjuvant To Gabapentin and Pregabalin For Treatment of SCI-related Neuropathic Painnur aini rahmawatiОценок пока нет
- Jurnal LBP PDFДокумент7 страницJurnal LBP PDFdiadiadia88Оценок пока нет
- Jurnal JossДокумент6 страницJurnal JosskurolivОценок пока нет
- Brignardello Petersen2018Документ1 страницаBrignardello Petersen2018Daniella NúñezОценок пока нет
- Wilhelm 2012Документ9 страницWilhelm 2012Paola Avila DíazОценок пока нет
- Comparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainДокумент15 страницComparative Effectiveness and Safety of Analgesic Medicines For Adults With Acute Non-Specific Low Back PainRachel PutriОценок пока нет
- Intrathecal Ziconotide in The Treatment of Refractory Pain in Patients With Cancer or AIDSДокумент8 страницIntrathecal Ziconotide in The Treatment of Refractory Pain in Patients With Cancer or AIDSSérgio TavaresОценок пока нет
- Harri Es 2014Документ2 страницыHarri Es 2014Amer WasimОценок пока нет
- Onmam 4Документ1 страницаOnmam 4Jose IgnacioОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 15: MusculoskeletalОт EverandComplementary and Alternative Medical Lab Testing Part 15: MusculoskeletalОценок пока нет
- Complementary and Alternative Medical Lab Testing Part 17: OncologyОт EverandComplementary and Alternative Medical Lab Testing Part 17: OncologyОценок пока нет
- Injury: Andrew H. SchmidtДокумент4 страницыInjury: Andrew H. SchmidttanyasisОценок пока нет
- Impact of Ulnar Styloid Fractures On The Treatment Effect of Distal Radius Fractures With Volar Plate Fixation: A Case Control StudyДокумент8 страницImpact of Ulnar Styloid Fractures On The Treatment Effect of Distal Radius Fractures With Volar Plate Fixation: A Case Control StudytanyasisОценок пока нет
- Main PDFДокумент5 страницMain PDFtanyasisОценок пока нет
- Kneeling After Total Knee Arthroplasty: Raj M. Amin, MD Vikram Vasan Julius K. Oni, MDДокумент6 страницKneeling After Total Knee Arthroplasty: Raj M. Amin, MD Vikram Vasan Julius K. Oni, MDtanyasisОценок пока нет
- Research Article: Anatomical Consideration of The Anterolateral Ligament of The KneeДокумент6 страницResearch Article: Anatomical Consideration of The Anterolateral Ligament of The KneetanyasisОценок пока нет
- Effect of Dislocation Timing Following Primary Total Hip Arthroplasty On The Risk of Redislocation and RevisionДокумент7 страницEffect of Dislocation Timing Following Primary Total Hip Arthroplasty On The Risk of Redislocation and RevisiontanyasisОценок пока нет
- Currentconceptsof Femoroacetabular Impingement: Aria Ghaffari,, Ivan Davis,, Troy Storey,, Michael MoserДокумент18 страницCurrentconceptsof Femoroacetabular Impingement: Aria Ghaffari,, Ivan Davis,, Troy Storey,, Michael MosertanyasisОценок пока нет
- Informed Consent: Guidance For ApplicantsДокумент7 страницInformed Consent: Guidance For ApplicantstanyasisОценок пока нет
- Letter To The Editor: Antibiotic Prophylaxis Regimens in Trauma and Orthopaedic SurgeryДокумент3 страницыLetter To The Editor: Antibiotic Prophylaxis Regimens in Trauma and Orthopaedic SurgerytanyasisОценок пока нет
- 2013jul SepInformedconsentIssuesandchallenges JAPTR43134 140Документ8 страниц2013jul SepInformedconsentIssuesandchallenges JAPTR43134 140tanyasisОценок пока нет
- Informed ConsentДокумент7 страницInformed ConsenttanyasisОценок пока нет
- A Protocol For The Management of Adhesive Small Bowel ObstructionДокумент9 страницA Protocol For The Management of Adhesive Small Bowel ObstructiontanyasisОценок пока нет
- Femoro Acetabular Impingement Clinical Research: Is A Composite Outcome The Answer?Документ7 страницFemoro Acetabular Impingement Clinical Research: Is A Composite Outcome The Answer?tanyasisОценок пока нет
- Wong2015 PDFДокумент28 страницWong2015 PDFtanyasisОценок пока нет
- (J. K. Rowling, Mary GrandPré) Harry Potter HardcДокумент376 страниц(J. K. Rowling, Mary GrandPré) Harry Potter HardcDiego RobertОценок пока нет
- Venous Thromboembolism in Over 16s Reducing The Risk of Hospitalacquired Deep Vein Thrombosis or Pulmonary Embolism PDF 1837703092165Документ43 страницыVenous Thromboembolism in Over 16s Reducing The Risk of Hospitalacquired Deep Vein Thrombosis or Pulmonary Embolism PDF 1837703092165tanyasisОценок пока нет
- Ankle Sprains: Evaluation, Rehabilitation, and Prevention: Raining Revention AND EhabilitationДокумент7 страницAnkle Sprains: Evaluation, Rehabilitation, and Prevention: Raining Revention AND EhabilitationtanyasisОценок пока нет
- DiniДокумент10 страницDiniMuhammad Yasdar BahriОценок пока нет
- Aines 2008Документ85 страницAines 2008tanyasisОценок пока нет
- Osteomyelitis-Bojan Rafaj (2012) PDFДокумент188 страницOsteomyelitis-Bojan Rafaj (2012) PDFtanyasisОценок пока нет
- Respiratory Tract Virus Infections in The Elderly With PneumoniaДокумент11 страницRespiratory Tract Virus Infections in The Elderly With PneumoniatanyasisОценок пока нет
- Riete & CapriniДокумент2 страницыRiete & CaprinitanyasisОценок пока нет
- Intestinal Dysbiosis in Preterm Infants Preceding N eДокумент15 страницIntestinal Dysbiosis in Preterm Infants Preceding N etanyasisОценок пока нет
- Stan Nard 2014Документ2 страницыStan Nard 2014tanyasisОценок пока нет
- Risk Factors For N e in NeonatesДокумент9 страницRisk Factors For N e in NeonatestanyasisОценок пока нет
- Senior CapstoneДокумент6 страницSenior Capstoneapi-313278667Оценок пока нет
- Danish Mask StudyДокумент1 страницаDanish Mask StudyJuana AtkinsОценок пока нет
- VTR 214 PDFДокумент2 страницыVTR 214 PDFKimberly AndrzejewskiОценок пока нет
- Marijuana and EpilepsyДокумент17 страницMarijuana and EpilepsyOmar AntabliОценок пока нет
- Efficacy of Glimepiride/metformin Combination Versus Glibenclamide/ Metformin in Patients With Uncontrolled Type 2 Diabetes MellitusДокумент4 страницыEfficacy of Glimepiride/metformin Combination Versus Glibenclamide/ Metformin in Patients With Uncontrolled Type 2 Diabetes Mellitusfannia nabillaОценок пока нет
- Mechanical Therapy: by Nikola TeslaДокумент2 страницыMechanical Therapy: by Nikola TeslaRommy RahmansyahОценок пока нет
- Pga R3Документ71 страницаPga R3Samruddhi PataitОценок пока нет
- LINKSERVE Training MaterialsДокумент15 страницLINKSERVE Training MaterialslisingynnamaeОценок пока нет
- Prescription PsychologyДокумент7 страницPrescription PsychologyJose LuisОценок пока нет
- CS 5 - Duchenne Muscular Dystrophy - EditedДокумент3 страницыCS 5 - Duchenne Muscular Dystrophy - EditedKarishmaK.Dhanani100% (1)
- Actinic KeratosisДокумент19 страницActinic KeratosisDajour CollinsОценок пока нет
- Tumors of The Orbit by Dr. Jonathan Del Prado 082708Документ3 страницыTumors of The Orbit by Dr. Jonathan Del Prado 082708CitrusОценок пока нет
- A Rural Mental Health CrisisДокумент13 страницA Rural Mental Health CrisisKeri StrahlerОценок пока нет
- SBARДокумент2 страницыSBARNabiela Aswaty 2011125083Оценок пока нет
- Rundown ISMI Hotti 2016Документ5 страницRundown ISMI Hotti 2016Wahyu PurnomoОценок пока нет
- 1-Diabetes Package - PO2693771771-269Документ6 страниц1-Diabetes Package - PO2693771771-269KishoreОценок пока нет
- S: "Masakit Ang Ulo at Tiyan Niya" As Verbalized byДокумент2 страницыS: "Masakit Ang Ulo at Tiyan Niya" As Verbalized bydenise-iceОценок пока нет
- Drugs and Pharmaceutical Technology Question BankДокумент7 страницDrugs and Pharmaceutical Technology Question BankVanitha EОценок пока нет
- Multiple Pregnancy: Prof Uma SinghДокумент53 страницыMultiple Pregnancy: Prof Uma Singhpok yeahОценок пока нет
- CKD + HPN Concept Map DRAFTДокумент1 страницаCKD + HPN Concept Map DRAFTInah Floresta BesasОценок пока нет
- Systemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsДокумент4 страницыSystemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsRandom PersonОценок пока нет
- 09 Cystic FibrosisДокумент12 страниц09 Cystic FibrosisYwagar YwagarОценок пока нет
- Media File 4: PathophysiologyДокумент1 страницаMedia File 4: PathophysiologyhazeeeОценок пока нет
- RabdoДокумент7 страницRabdoErik Ulises Teolotitla RoslaesОценок пока нет