Академический Документы
Профессиональный Документы
Культура Документы
Full
Загружено:
Anonymous IwWqtsyeОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Full
Загружено:
Anonymous IwWqtsyeАвторское право:
Доступные форматы
BRIEF REPORT
Association between medical cannabis laws and
opioid overdose mortality has reversed over time
Chelsea L. Shovera,1 , Corey S. Davisb , Sanford C. Gordonc , and Keith Humphreysa,d
a
Department of Psychiatry and Behavioral Sciences, Stanford University, Stanford, CA 94305; b The Network for Public Health Law, Carrboro, NC 27516;
c
Wilf Family Department of Politics, New York University, New York, NY 10012; and d Center for Innovation to Implementation, Veterans Affairs Health Care
System, Palo Alto, CA 94304
Edited by Kenneth W. Wachter, University of California, Berkeley, CA, and approved May 16, 2019 (received for review February 27, 2019)
Medical cannabis has been touted as a solution to the US opi- also increased dramatically over that time period (8). Using the
oid overdose crisis since Bachhuber et al. [M. A. Bachhuber, same methods as Bachhuber et al. (1), we revisited the ques-
B. Saloner, C. O. Cunningham, C. L. Barry, JAMA Intern. Med. 174, tion with seven more years of data. To investigate how newer
1668–1673] found that from 1999 to 2010 states with medical cannabis laws may be associated with changes in the association
cannabis laws experienced slower increases in opioid analgesic between cannabis laws and opioid overdose mortality, we also
overdose mortality. That research received substantial attention created a model with additional terms to account for presence
in the scientific literature and popular press and served as a talk- of a recreational cannabis law or a low-THC restriction. Because
ing point for the cannabis industry and its advocates, despite none of the states with low-THC laws operate medical dispen-
caveats from the authors and others to exercise caution when saries and many limit access to a small number of indications, the
using ecological correlations to draw causal, individual-level con- levels of access can be approximated as highest for recreational,
clusions. In this study, we used the same methods to extend then “comprehensive” medical with dispensaries, and lowest for
states with low-THC only. If broader access to cannabis writ
SOCIAL SCIENCES
Bachhuber et al.’s analysis through 2017. Not only did findings
from the original analysis not hold over the longer period, but large, rather than medical cannabis specifically, is the latent fac-
the association between state medical cannabis laws and opi- tor associated with lower opioid overdose mortality, we would
oid overdose mortality reversed direction from −21% to +23% expect to see the most negative association in states with recre-
and remained positive after accounting for recreational cannabis ational laws and the least negative association (or even positive)
laws. We also uncovered no evidence that either broader (recre- association in states with low-THC-only laws.
ational) or more restrictive (low-tetrahydrocannabinol) cannabis
laws were associated with changes in opioid overdose mortal- Results
MEDICAL SCIENCES
ity. We find it unlikely that medical cannabis—used by about
For the original 1999–2010 time period, we obtained estimates
2.5% of the US population—has exerted large conflicting effects
similar to Bachhuber et al. (1), with slight differences likely
on opioid overdose mortality. A more plausible interpretation
due to missing values for 30 state/year combinations. Whereas
is that this association is spurious. Moreover, if such rela-
Bachhuber et al. (1) estimated a 24.8% reduction in deaths
tionships do exist, they cannot be rigorously discerned with
per 100,000 population associated with a medical cannabis law’s
aggregate data. Research into therapeutic potential of cannabis
introduction, we estimated a statistically indistinguishable 21.1%
should continue, but the claim that enacting medical cannabis
decrease. As in the original model, none of the four time-varying
laws will reduce opioid overdose death should be met with
covariates (annual state unemployment rate and presence of
skepticism.
the following: prescription drug monitoring program, pain man-
agement clinic oversight laws, and law requiring or allowing
medical cannabis | opioid overdose | public policy
pharmacists to request patient identification) were significantly
associated with opioid overdose mortality (Table 1). Using the
A 2014 study by Bachhuber et al. (1) created a sensation by
showing that state medical cannabis laws were associated
with lower-than-expected opioid overdose mortality rates from
full 1999–2017 dataset, we found that the sign reversed for medi-
cal cannabis laws, such that states passing a medical cannabis law
experienced a 22.7% increase, 95% CI (2.0, 47.6) in overdose
1999 to 2010. Cited by more than 350 scientific articles to date, deaths. As an additional robustness test, we estimated models
the study attracted national and international media attention including state-specific linear time trends as well as state and
and was hailed by many activists and industry representatives as year fixed effects. As with the analysis reported above, the sign
proof that expanding medical cannabis would reverse the opi- of the effect of medical cannabis law switched from negative
oid epidemic (1). Despite the authors’ cautions about drawing to positive once the data were extended to 2017; however, the
firm conclusions from ecological correlations, and similar warn- magnitude was diminished and in neither specification was the
ings from other scientists (2), many such conclusions were drawn, estimate statistically significant.
to the point where medical cannabis has now been approved by The direction of the association between medical cannabis
several states as a treatment for opioid use disorder (3, 4). Sub- laws and opioid overdose mortality was sensitive to the study’s
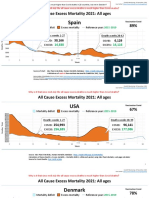
sequently published papers also found that cannabis access and endpoint (Fig. 1). For end dates between 2008 and 2012, the
indices of opioid-related harm were negatively correlated in the
aggregate, with some attributing this less to medical cannabis
laws per se than to increased access to any form of cannabis Author contributions: C.L.S., S.C.G., and K.H. designed research; C.L.S. and C.S.D. per-
(including recreational) (5–7). formed research; C.L.S. and S.C.G. analyzed data; C.L.S. and K.H. wrote the paper; C.S.D.
Given mounting deaths from opioid overdose, replicating provided legal review; and C.S.D. and S.C.G. critically revised the paper.y
the Bachhuber et al. (1) finding is a worthy task, especially The authors declare no conflict of interest.y
in light of the changing policy landscape. Between 2010 and This open access article is distributed under Creative Commons Attribution-NonCommercial-
2017, 32 states enacted medical cannabis laws, including 17 that NoDerivatives License 4.0 (CC BY-NC-ND).y
allowed only medical cannabis with low levels of the psychoactive 1
To whom correspondence may be addressed. Email: clshover@stanford.edu.y
tetrahydrocannabinol (THC) and high levels of the nonpsychoac- This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.
tive component cannabidiol. Eight states enacted recreational 1073/pnas.1903434116/-/DCSupplemental.y
cannabis laws during this period. Opioid overdose deaths have
www.pnas.org/cgi/doi/10.1073/pnas.1903434116 PNAS Latest Articles | 1 of 3
Table 1. Age-adjusted opioid overdose death rate per 100,000 population
Independent variables Bachhuber et al. (1999–2010) Replication (1999–2010) Extension (1999–2017) Expanded model (1999–2017)
Medical cannabis law −24.8 (−37.5 to −9.5) −21.1 (−35.7, −3.0) 22.7 (2.0, 47.6) N/A
Prescription drug
monitoring program 3.7 (−12.7 to 23.3) −2.8 (−16.7, 13.3) −2.7 (−15.9, 12.5) −4.0 (−17.1, 11.1)
Law requiring or allowing
pharmacists to request patient
identification 5.0 (−10.4 to 23.1) 2.8 (−12.6, 20.9) 11.8 (−7.7, 35.5) 8.8 (−10.2, 31.9)
Increased state oversight of
pain management clinics −7.6 (−19.1 to 5.6) −6.9 (−18.4, 6.2) 9.0 (−15.6, 40.8) 13.7 (−11.2, 45.5)
Annual state unemployment rate 4.4 (−0.3 to 9.3) 4.4 (−0.3, 9.3) 1.4 (−2.7, 5.5) 0.7 (−3.1, 4.6)
Types of cannabis laws
Recreational and medical
cannabis law N/A N/A N/A −14.7 (−43.6, 29.0)
Medical cannabis only N/A N/A N/A 28.2 (1.2, 62.4)
Low-THC–only medical
cannabis law N/A N/A N/A −7.1 (−29.1, 21.7)
All models also included year and state fixed effects. N/A denotes not applicable because variable was not included in model.
association was negative as reported in Bachhuber et al. (1). Sub- the individual level and (ii) the relationship is causal. The first
sequently, the association became statistically indistinguishable conclusion is frequently incorrect across many research fields
from zero before turning positive in 2017. owing to the ecological fallacy (9). Ecological correlations can-
In the expanded model with indicators for different types of not establish individual-level relationships and indeed may run
cannabis laws, having a comprehensive medical cannabis law in the directly opposite direction (e.g., higher rates of smoking
was associated with a 28.2%, 95% CI (1.2, 62.4) higher opi- in French regions with lower rates of esophageal cancer should
oid overdose mortality, while estimates for other laws were not be interpreted as evidence of a protective effect of smok-
nonsignificant. The association between having a recreational ing) (10). In this case, compelling evidence exists that violates
cannabis law and opioid overdose mortality was −14.7%, 95% the first assumption: A study of a nationally representative sam-
CI (−43.6, 29.0). Having a low-THC-only medical cannabis law ple of individuals shows that use of medical cannabis is positively
was associated with −7.1%, 95% CI (−29.1, 21.7) lower opioid correlated both with use and misuse of prescription pain relievers
overdose mortality. For both of these laws, the wide CIs include (11). This positive correlation does not at all prove that medical
strong positive, strong negative, and null associations, indicating cannabis causes individuals to use opioids because correlation of
compatibility with a large range of true associations. nonexperimentally gathered data does not establish causation,
a general principle that all parties to the current debate should
Discussion bear in mind.
We replicated Bachhuber et al.’s (1) finding of a negative asso- When multiple studies using similar methods generate a par-
ciation between medical marijuana and opioid overdose deaths ticular result, and for the first time one of those studies fails to
from 1999 to 2010. However, the association did not hold when replicate with more extensive data, there are multiple ways to
more extensive data through 2017 were analyzed. Had the anal- explain the discrepancy. It could be that by bad luck the only
ysis’ endpoint been between 2008 and 2012, the results would one of those studies whose initial findings would not stand up
have been comparable to those obtained by Bachhuber et al. (1). to reanalysis with more recent data happened to be the one
However, the association became equivocal in 2013; by 2017 it
had reversed such that a study conducted in that year might lead
some to conclude that medical cannabis laws were compounding
opioid overdose mortality. 60
The mechanism theorized to describe a causal relationship 50
between medical cannabis laws and opioid overdose mortality
Point Estimate and 95% Confidence Interval
40
rests on several premises: (i) Cannabis is more available in states
30
with medical cannabis laws; (ii) people in these states substitute
20
cannabis for opioids, whether for pain management, intoxica-
tion, or both; and (iii) this substitution occurs on a large enough 10
scale to impact the population-level overdose mortality esti- 0
mates. Under this model, states with highly restrictive medical -10
cannabis laws limited to low-THC products would be expected to -20
have a weaker association than states with comprehensive med-
-30
ical cannabis, while states with recreational cannabis would be
expected to have a stronger association. Our results do not sup- -40
port this, as after adjusting for more and less restrictive types of -50
2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
cannabis law (recreational and medical or low-THC only), states Study Endpoint
with comprehensive medical cannabis laws still had a positive
association with opioid overdose mortality.
Fig. 1. Changes in point estimate and 95% CI of association between
The Bachhuber et al. (1) study is one of several that find medical cannabis law and age-adjusted opioid overdose death rate by the
the rate of cannabis access and some index of opioid-related last year included in the analysis since 1999. Fixed (year and state) and
harm are negatively correlated in the aggregate (1, 5–7). Pol- time-varying effects (prescription drug monitoring program, state unem-
icy that expands access to cannabis based on these findings ployment, pain management clinic oversight laws, and prescription drug
assumes that (i) the same negative relationship is present at identification laws) were also adjusted for.
2 of 3 | www.pnas.org/cgi/doi/10.1073/pnas.1903434116 Shover et al.
BRIEF REPORT
that was reexamined and every other similar study in that area icy areas. Corporate actors (e.g., the medical cannabis industry)
would survive such an analysis (even though, as in this case, with deep pockets have substantial ability to promote congenial
they explicitly build on the nonreplicated finding). However, we results, and suffering people are desperate for effective solutions.
think a nonreplication should at least raise the possibility in Cannabinoids have demonstrated therapeutic benefits (13), but
the minds of scientists that the similar findings of other, sim- reducing population-level opioid overdose mortality does not
ilar studies in this area might also not replicate with a longer appear to be among them.
time series.
We are more cautious than others have been in drawing causal Materials and Methods
conclusions from ecological correlations and conclude that the Opioid analgesic overdose deaths were extracted from Centers for Dis-
observed association between these two phenomena is likely spu- ease Control and Prevention’s Wide-ranging Online Data for Epidemiologic
rious rather than a reflection of medical cannabis saving lives Research (CDC WONDER) and independent variables were obtained from
the sources cited in the original paper and are included in the associated
10 y ago and killing people today. Medical cannabis users are dataset for ref. 1. For rates with 95% CIs in CDC WONDER but no point
about 2.5% of the population, making it unlikely that they estimate (those with 10 to 20 deaths in a state and year) we smoothed the
can significantly alter population-wide indices (12). Unmeasured data by averaging the confidence limits. Medical cannabis laws were coded
variables likely explain both associations (e.g., state incarcera- as 0 for years preimplementation and 1 for years postimplementation. As
tion rates and practices, naloxone availability, and the extent of applicable, we included a fraction for the year the law went into effect
insurance and services) (2). (e.g., 0.5 for a law implemented on July 1). A generalized linear model with
Our expanded analysis does not support the interpretation robust standard errors was specified with year and state as fixed effects.
We reviewed the legal literature to assess the effects of potential inaccura-
that broader access to cannabis is associated with lower opioid
cies in the original sources (14); coefficient of the independent variable was
overdose mortality. The CIs for both recreational cannabis laws insensitive to these differences. We ran the main model with end years from
and low-THC laws are wide due to the comparatively small num- 2002 to 2017 and plotted the adjusted association. To assess the association
ber of state/year combinations with these laws. Importantly, the between new cannabis laws implemented since 2010, we specified a model
CIs are compatible with a strong positive or strong negative cor- that included indicator variables for three kinds of cannabis laws: (i) pres-
SOCIAL SCIENCES
relation, as well as no correlation. Future estimates may be more ence of a recreational cannabis law and medical cannabis law, (ii) medical
precise (i.e., have narrower CIs) as data accumulate over time, cannabis only with no restriction on THC content, and (iii) medical cannabis
and we caution scientists who conduct these analyses to note but only low-THC. Data are available in Dataset S1.
that, at present, states with recreational cannabis laws (Alaska, ACKNOWLEDGMENTS. C.L.S. was supported by National Institute on Drug
California, Colorado, Massachusetts, Maine, Oregon, Washing- Abuse of the National Institutes of Health Award T32 DA035165 and the
ton, Vermont, and the District of Columbia) form a group that Wu Tsai Neurosciences Institute. K.H. was supported by a Senior Career
is qualitatively different from the rest of the United States on a Research Scientist Award from the Veterans Health Administration, Wu Tsai
Neurosciences Institute, and the Esther Ting Memorial Professorship at Stan-
number of metrics that may confound estimates.
MEDICAL SCIENCES
ford University. The content is solely the responsibility of the authors and
The nonrobustness of the earlier findings also highlights the does not necessarily represent the official views of the NIH or the authors’
challenges of controlling scientific messages in controversial pol- employers.
1. M. A. Bachhuber, B. Saloner, C. O. Cunningham, C. L. Barry, Medical cannabis laws 8. L. Scholl, P. Seth, K. Mbabazi, N. Wilson, G. Baldwin, Drug and opioid-involved over-
and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA dose deaths, United States, 2013-2017. Morb. Mortal. Weekly Rep. 67, 1419–1427
Intern. Med. 174, 1668–1673 (2014). (2018).
2. W. Hall et al., It is premature to expand access to medicinal cannabis in hopes of 9. W. Robinson, Ecological correlations and the behavior of individuals. Am. Sociol. Rev.
solving the us opioid crisis. Addiction 113, 987–988 (2018). 15, 351–357 (1950).
3. K. Humphreys, R. Saitz, Should physicians recommend replacing opioids with 10. J. W. Finney, K. Humphreys, D. R. Kivlahan, A. H. Harris, Why health care process per-
cannabis? JAMA 321, 639–640 (2019). formance measures can have different relationships to outcomes for patients and
4. New York State Department of Health, New York State Department of Health hospitals: Understanding the ecological fallacy. Am. J. Public Health 101, 1635–1642
announces opioid replacement now a qualifying condition for medical marijuana. (2011).
https://www.health.ny.gov/press/releases/2018/2018-07-12 opioid replacement.htm. 11. T. L. Caputi, K. Humphreys, Medical marijuana users are more likely to use prescription
Accessed 24 February 2019. drugs medically and nonmedically. J. Addict. Med. 12, 295–299 (2018).
5. D. Powell, R. L. Pacula, M. Jacobson, Do medical marijuana laws reduce 12. T. L. Caputi, Medical marijuana, not miracle marijuana: Some well-publicized studies
addictions and deaths related to pain killers? J. Health Econ. 58, 29–42 about medical marijuana don’t pass a reality check. Addiction 114, 1128–1129 (2019).
(2018). 13. National Academies of Sciences, Engineering, and Medicine, The Health Effects of
6. A. C. Bradford, W. D. Bradford, Medical marijuana laws may be associated with a Cannabis and Cannabinoids: The Current State of Evidence and Recommendations
decline in the number of prescriptions for Medicaid enrollees. Health Aff. 36, 945–951 for Research (The National Academies Press, Washington, DC, 2017).
(2017). 14. J. Horwitz, C. S. Davis, L. S. McClelland, R. S. Fordon, E. Meara, The problem of data
7. H. Wen, J. M. Hockenberry, Association of medical and adult-use marijuana laws quality in analyses of opioid regulation: The case of prescription drug monitor-
with opioid prescribing for Medicaid enrollees. JAMA Intern. Med. 178, 673–679 ing programs, NBER Working Paper 24947 (National Bureau of Economic Research,
(2018). Cambridge, MA, 2018).
Shover et al. PNAS Latest Articles | 3 of 3
Вам также может понравиться
- Revised Should Marijuana Be Legalized in The USДокумент24 страницыRevised Should Marijuana Be Legalized in The USBailey DeitchОценок пока нет
- Physician Guide To Cannabis-Assisted Opioid Reduction (Distributed by EB)Документ2 страницыPhysician Guide To Cannabis-Assisted Opioid Reduction (Distributed by EB)Lisa Rough100% (6)
- IEC ShipsДокумент6 страницIEC ShipsdimitaringОценок пока нет
- Argumentative Essay Medical MarijuanaДокумент7 страницArgumentative Essay Medical MarijuanaMaxim Dahan100% (1)
- Sindi and Wahab in 18th CenturyДокумент9 страницSindi and Wahab in 18th CenturyMujahid Asaadullah AbdullahОценок пока нет
- Fusion Implementing Offerings Using Functional Setup Manager PDFДокумент51 страницаFusion Implementing Offerings Using Functional Setup Manager PDFSrinivasa Rao Asuru0% (1)
- Grade 7 ExamДокумент3 страницыGrade 7 ExamMikko GomezОценок пока нет
- DQ Vibro SifterДокумент13 страницDQ Vibro SifterDhaval Chapla67% (3)
- Medical Cannabis: A Guide for Patients, Practitioners, and CaregiversОт EverandMedical Cannabis: A Guide for Patients, Practitioners, and CaregiversРейтинг: 5 из 5 звезд5/5 (1)
- Role of Losses in Design of DC Cable For Solar PV ApplicationsДокумент5 страницRole of Losses in Design of DC Cable For Solar PV ApplicationsMaulidia HidayahОценок пока нет
- Medical Cannabis Laws and Opioid Analgesic Overdose Mortality in The United States, 1999-2010Документ6 страницMedical Cannabis Laws and Opioid Analgesic Overdose Mortality in The United States, 1999-2010AlonsoCaceresОценок пока нет
- ASAM 2020 Public Policy Statement On Cannabis PDFДокумент13 страницASAM 2020 Public Policy Statement On Cannabis PDFJoseph PreisterОценок пока нет
- FinalthesisofficialДокумент29 страницFinalthesisofficialapi-674809646Оценок пока нет
- The Effect of Medical Cannabis Dispensaries On Opioid and Heroin Overdose MortalityДокумент2 страницыThe Effect of Medical Cannabis Dispensaries On Opioid and Heroin Overdose MortalityCato InstituteОценок пока нет
- 2292 Final PaperДокумент14 страниц2292 Final Paperseanchiu0812Оценок пока нет
- Reiman Et Al 2017 Cannabis As A Substitute For Opioid Based Pain Medication Patient Self ReportДокумент7 страницReiman Et Al 2017 Cannabis As A Substitute For Opioid Based Pain Medication Patient Self ReportfelipepretelmktОценок пока нет
- HHS Public Access: Cannabis Use, Attitudes, and Legal Status in The U.S.: A ReviewДокумент25 страницHHS Public Access: Cannabis Use, Attitudes, and Legal Status in The U.S.: A Reviewyeremias setyawanОценок пока нет
- Cara PaperДокумент11 страницCara Paperapi-392400343Оценок пока нет
- Final Paper WordДокумент8 страницFinal Paper Wordapi-357159376Оценок пока нет
- Cannabis and MH 2019 ReviewДокумент23 страницыCannabis and MH 2019 Reviewbosko888Оценок пока нет
- Nihms 1696800Документ54 страницыNihms 1696800Fabíola ManoОценок пока нет
- PIIS0012369215506375Документ11 страницPIIS0012369215506375Rodrigo OlivoОценок пока нет
- Medical Cannabis Access, Use, and Substitution For Prescription Opioids and Other Substances: A Survey of Authorized Medical Cannabis PatientsДокумент6 страницMedical Cannabis Access, Use, and Substitution For Prescription Opioids and Other Substances: A Survey of Authorized Medical Cannabis PatientsAnonymous f3w70b6emrОценок пока нет
- PIIS1556086418300388Документ8 страницPIIS1556086418300388Michael UОценок пока нет
- Marijuanaandlaw FinalДокумент11 страницMarijuanaandlaw Finalapi-283892872Оценок пока нет
- HESA Submission - Toxic Drug Crisis - Jan 2024Документ10 страницHESA Submission - Toxic Drug Crisis - Jan 2024CDPCОценок пока нет
- Legalization of Medical Marijuana in The United StatesДокумент12 страницLegalization of Medical Marijuana in The United StatesTeresa SmithОценок пока нет
- An Assessment of The Benefits of Marijuana LegalizationДокумент9 страницAn Assessment of The Benefits of Marijuana LegalizationChris BatesОценок пока нет
- The Implications of Marijuana Decriminalization and Legalization On Crime in The United StatesДокумент23 страницыThe Implications of Marijuana Decriminalization and Legalization On Crime in The United Statesctoma7Оценок пока нет
- Mortality and Socioeconomic Consequences of Prescription Opioids: Evidence From State PoliciesДокумент2 страницыMortality and Socioeconomic Consequences of Prescription Opioids: Evidence From State PoliciesCato InstituteОценок пока нет
- Opioides en UrgenciasДокумент6 страницOpioides en UrgenciasSandra Milena ZuletaОценок пока нет
- DPA Fact Sheet CBD Aug2015 PDFДокумент3 страницыDPA Fact Sheet CBD Aug2015 PDFwebmaster@drugpolicy.org100% (1)
- Overdosing On RegulationДокумент21 страницаOverdosing On Regulation02quantum.beagleОценок пока нет
- Estudio Uso THCДокумент16 страницEstudio Uso THCMax Möller ZamoranoОценок пока нет
- Medical Cannabis Users' Comparisons Between Medical Cannabis and Mainstream MedicineДокумент7 страницMedical Cannabis Users' Comparisons Between Medical Cannabis and Mainstream MedicineMoises BocanegraОценок пока нет
- Medical Marijuana: "Take A Deep Breath"Документ26 страницMedical Marijuana: "Take A Deep Breath"MarkОценок пока нет
- Appi Ajp 2021 21111134 PDFДокумент4 страницыAppi Ajp 2021 21111134 PDFSteve aokiОценок пока нет
- Cannabis Use and Cannabis Use DisordersДокумент2 страницыCannabis Use and Cannabis Use DisordersGustavo FigueroaОценок пока нет
- DEA 2022 0120 0217 - Attachment - 1Документ7 страницDEA 2022 0120 0217 - Attachment - 1Tim BrownОценок пока нет
- Articulo Cientifico InglessДокумент13 страницArticulo Cientifico InglessKarla MontañoОценок пока нет
- Therapeutic Effects of Cannabis and Cannabinoids - The Health Effects of Cannabis and Cannabinoids - NДокумент50 страницTherapeutic Effects of Cannabis and Cannabinoids - The Health Effects of Cannabis and Cannabinoids - NCesar VargasОценок пока нет
- PuffpuffpassДокумент9 страницPuffpuffpassapi-251251694Оценок пока нет
- DD 3Документ14 страницDD 3westernmsa.marketingОценок пока нет
- Maconha Como Substituicao para Medicamentos PrescritosДокумент10 страницMaconha Como Substituicao para Medicamentos PrescritosMarcellaОценок пока нет
- Artigo Secundaìrio 1Документ9 страницArtigo Secundaìrio 1Victoria AlmeidaОценок пока нет
- The Debate On The Legalization of MarijuanaДокумент4 страницыThe Debate On The Legalization of MarijuanakelleybrawnОценок пока нет
- Oregon DWDA 10-Year ExperienceДокумент12 страницOregon DWDA 10-Year ExperienceNicholasОценок пока нет
- Cannabis Use and Substantial Reduction in Premature Deaths in The United States.Документ53 страницыCannabis Use and Substantial Reduction in Premature Deaths in The United States.Monterey Bud100% (2)
- 15 Annotated Bibliography (Final)Документ8 страниц15 Annotated Bibliography (Final)ethanОценок пока нет
- Final Annotated BibliographyДокумент11 страницFinal Annotated Bibliographyapi-358143741Оценок пока нет
- The Unintended Consequences of Marijuana LegislationДокумент5 страницThe Unintended Consequences of Marijuana LegislationMaldini NyachОценок пока нет
- The Crimes and Constitutional Deficiencies of Our Criminal Justice System: Why Depriving Prisoners with Opioid Use Disorder Access to Medicated-Assisted Treatment is Cruel, Criminal, and Unconstitutional - Sarah GadДокумент25 страницThe Crimes and Constitutional Deficiencies of Our Criminal Justice System: Why Depriving Prisoners with Opioid Use Disorder Access to Medicated-Assisted Treatment is Cruel, Criminal, and Unconstitutional - Sarah GadSarah_GadОценок пока нет
- Cns 765 Assignment 3Документ8 страницCns 765 Assignment 3api-664836263Оценок пока нет
- Revised Annotated BibliographyДокумент16 страницRevised Annotated BibliographyBailey DeitchОценок пока нет
- Journal International of The Opioid-Overdose PUTRI INDRIANIДокумент22 страницыJournal International of The Opioid-Overdose PUTRI INDRIANIPutri IndrianiОценок пока нет
- Pinto 2019Документ7 страницPinto 2019Cadu SantanaОценок пока нет
- Olfson Et Al 2017 Cannabis Use and Risk of Prescription Opioid Use Disorder in The United StatesДокумент7 страницOlfson Et Al 2017 Cannabis Use and Risk of Prescription Opioid Use Disorder in The United StatesfelipepretelmktОценок пока нет
- Association Between Cannabis Use Disorder and Self and Other Directed AggressionДокумент10 страницAssociation Between Cannabis Use Disorder and Self and Other Directed Aggressionsamer.elhayekОценок пока нет
- PrimaryДокумент3 страницыPrimaryapi-358143741Оценок пока нет
- Reimagining U.S. Drug Policy Post-PandemicДокумент10 страницReimagining U.S. Drug Policy Post-PandemicOscar YanezОценок пока нет
- Reasearch Paper 610Документ16 страницReasearch Paper 610Q-MT Branch HQ 497 OM&MОценок пока нет
- KanabisДокумент8 страницKanabisFadil MuhammadОценок пока нет
- HHS Public AccessДокумент20 страницHHS Public Accessirribarra.nlopez3046Оценок пока нет
- 2017 08 08ajpmopiatesДокумент9 страниц2017 08 08ajpmopiatesZerohedgeОценок пока нет
- Nihms 1608915Документ26 страницNihms 1608915bohicah384Оценок пока нет
- Opioid CrisisДокумент5 страницOpioid CrisisLorine IchingwaОценок пока нет
- LEIA Home Lifts Guide FNLДокумент5 страницLEIA Home Lifts Guide FNLTejinder SinghОценок пока нет
- Rule 113 114Документ7 страницRule 113 114Shaila GonzalesОценок пока нет
- User S Manual AURORA 1.2K - 2.2KДокумент288 страницUser S Manual AURORA 1.2K - 2.2KEprom ServisОценок пока нет
- Review1 ScheduleДокумент3 страницыReview1 Schedulejayasuryam.ae18Оценок пока нет
- Classifications of AssessmentsДокумент11 страницClassifications of AssessmentsClaire CatapangОценок пока нет
- Sam Media Recruitment QuestionnaireДокумент17 страницSam Media Recruitment Questionnairechek taiОценок пока нет
- Application Activity Based Costing (Abc) System As An Alternative For Improving Accuracy of Production CostДокумент19 страницApplication Activity Based Costing (Abc) System As An Alternative For Improving Accuracy of Production CostM Agus SudrajatОценок пока нет
- Companyprofil E: Erfanconstructionsolut IonДокумент14 страницCompanyprofil E: Erfanconstructionsolut IonNurin AleesyaОценок пока нет
- Module 1: Overview of Applied Behaviour Analysis (ABA)Документ37 страницModule 1: Overview of Applied Behaviour Analysis (ABA)PriyaОценок пока нет
- SMR 13 Math 201 SyllabusДокумент2 страницыSMR 13 Math 201 SyllabusFurkan ErisОценок пока нет
- Tetralogy of FallotДокумент8 страницTetralogy of FallotHillary Faye FernandezОценок пока нет
- What Is TranslationДокумент3 страницыWhat Is TranslationSanskriti MehtaОценок пока нет
- Laboratory Manual (CIV 210) Engineering Surveying (2018-19) (For Private Circulation Only)Документ76 страницLaboratory Manual (CIV 210) Engineering Surveying (2018-19) (For Private Circulation Only)gyanendraОценок пока нет
- Agnes de MilleДокумент3 страницыAgnes de MilleMarie-Maxence De RouckОценок пока нет
- Business Plan 3.3Документ2 страницыBusiness Plan 3.3Rojin TingabngabОценок пока нет
- Week 7Документ24 страницыWeek 7Priyank PatelОценок пока нет
- Mastertop 1230 Plus PDFДокумент3 страницыMastertop 1230 Plus PDFFrancois-Оценок пока нет
- Radiation Safety Densitometer Baker PDFДокумент4 страницыRadiation Safety Densitometer Baker PDFLenis CeronОценок пока нет
- Huawei R4815N1 DatasheetДокумент2 страницыHuawei R4815N1 DatasheetBysОценок пока нет
- Retailing in IndiaДокумент11 страницRetailing in IndiaVinod MalkarОценок пока нет
- Chemistry Test 1Документ2 страницыChemistry Test 1shashankОценок пока нет
- Traveling Salesman ProblemДокумент11 страницTraveling Salesman ProblemdeardestinyОценок пока нет
- Countries EXCESS DEATHS All Ages - 15nov2021Документ21 страницаCountries EXCESS DEATHS All Ages - 15nov2021robaksОценок пока нет
- Dialogue Au Restaurant, Clients Et ServeurДокумент9 страницDialogue Au Restaurant, Clients Et ServeurbanuОценок пока нет