Академический Документы
Профессиональный Документы
Культура Документы
2802 3498
Загружено:
Cleofe Lagura DiazОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
2802 3498
Загружено:
Cleofe Lagura DiazАвторское право:
Доступные форматы
HOME PREVIOUS NEXT
ARTICLE
A Closer Look at Substance Use and Suicide
Michael Esang, M.B.B.Ch., M.P.H., Saeed Ahmed, M.D.
Suicide is the tenth leading cause of disorders, more suicide attempts, and that 24.5% of people aged 60–69 and
death in the United States across all age more frequent hospitalizations than pa- 13% of people aged 70–79 had consumed
groups. A total of 44,193 suicides occur tients with bipolar disorder alone (7). alcohol before attempting suicide (13).
each year, or 121 suicides per day (1). The Substance use independently in- Older persons use alcohol as a palliative
Centers for Disease Control and Preven- creases the risk of suicidal behavior (8). measure in response to pain, losses, and
tion defines suicide as “death caused by Acute and chronic drug abuse may im- affective changes. This often leads to a
self-inflicted injuries with the intention pair judgment, weaken impulse control, damaging cycle of alcohol use to self-
of dying from the result of such actions” and interrupt neurotransmitter path- medicate symptoms of depression, wors-
(1). Substance use is a risk factor for both ways, leading to suicidal tendencies ening the situation. For this reason, alco-
fatal and nonfatal overdoses, suicide at- through disinhibition (9). Additionally, hol use disorder has been reported to be
tempts, and death by suicide. Compared physiological and metabolic stress re- the second most common psychiatric
with the general population, individuals sulting from drug abuse can lead to neu- disorder associated with elderly suicide,
with alcohol dependence and persons rotoxic damage and other severe medical second only to depression (10, 13).
who use drugs have a 10–14 times greater complications. This is particularly sig-
risk of death by suicide, respectively (2), nificant in older populations who are less
OPIOID USE DISORDER AND
and approximately 22% of deaths by sui- physiologically resilient due to increased
SUICIDE
cide have involved alcohol intoxication chronic medical comorbidities and neu-
(2). Furthermore, one study found that rodegenerative diseases (10). In older Opioid-related suicides have doubled in
opiates were present in 20% of suicide populations, suicide is closely linked first the last 15 years. This increase has paral-
deaths, marijuana in 10.2%, cocaine in with psychiatric illness and subsequently leled the massive increase in drug over-
4.6%, and amphetamines in 3.4% (2). with substance use disorders, particu- dose deaths, particularly those involving
Among the reported substances, alco- larly alcohol use disorder. Therefore, prescription opioids. Prescribed opioid
hol and opioids are associated with the persons in this patient population have use nearly doubled between 1999 (116
greatest risks of suicidal behavior. a higher risk of suicidal behavior com- million) and 2011 (219 million) (14) and
Psychiatric disorders have a strong pared with younger individuals (9). has been noted to be a risk factor for sui-
association with suicide. Ninety percent cide by overdose. In 2015 alone, the Cen-
of people who die by suicide have one or ters for Disease Control and Prevention
ALCOHOL USE DISORDER AND
more concomitant psychiatric disorders reported a total of 52,000 drug overdose-
SUICIDE
(3). Suicide risk is highest among patients related deaths, with 63.1% involving a
with bipolar disorder (odds ratio=7.77) Drinking alcohol at an early age, binge or prescription or illicit opioid (15). The
and unipolar affective disorder (odds heavy drinking, and drinking behaviors rates increased to 72.2% for synthetic
ratio=6.67), followed by schizophrenia that meet criteria for mild, moderate, or opioids and were 20.6% for heroin. A
(odds ratio=6.55) and anxiety disorders severe alcohol use disorder can all lead meta-analysis by Wilcox and colleagues
(odds ratio=3.57–6.64) (4). The risk of to increased suicidal ideation. Persons (2) showed that heroin use increased the
suicide increases further when psychi- with heavy alcohol use are five times risk of suicide by 13.5 times compared
atric disorders are comorbid with sub- more likely to die by suicide than social with the 10-fold increase with alcohol
stance use disorders. Research shows drinkers (11). use disorder. Another study investigat-
that men with comorbid depression and In 2015, a survey conducted by the ing the association between prescription
alcohol use have the highest long-term Substance Abuse and Mental Health opioid use and suicide among patients
suicide risk (16.2%) (5). The prevalence Services Administration showed that with chronic noncancer pain revealed
of lifetime suicide attempts among pa- 9.8 million people ≥18 years old seri- that an increased opioid dose was related
tients with alcohol use disorder and bi- ously considered suicide in the past 12 to an increased risk of suicide, even after
polar disorder is reported to be between months, with 1.4 million making nonfa- controlling for demographic and clinical
21% and 42% (6). Similarly, patients tal suicide attempts (12). Young adults factors (16). The recent increase in drug
with bipolar disorder and comorbid sub- aged 18–25 were also more likely to have overdose-related suicides highlights the
stance use disorder have earlier-onset serious thoughts of suicide or suicide at- importance of assessing suicide risk in
mood symptoms, higher rates of anxiety tempts. One study of the elderly found patients receiving opioids.
The American Journal of Psychiatry Residents’ Journal | June 2018 6
HOME PREVIOUS NEXT
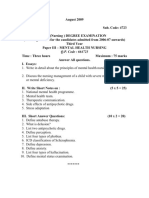
BOX 1. Dynamic and Static Risk Factors Associated With Suicide and Protective Factorsa
Dynamic and Acute Risk Factors Static and Long-Term Risk Factors Protective Factors
Current suicidal ideation Family history Reasons for living
Current suicidal plan Caucasian race Being clean and sober
Preparation for suicide Unmarried status Attending 12-step support groups
Acute symptoms of mental disorder Living alone Religious attendance and/or internalized spiritual
Severe psychic anxiety Lack of social support teachings against suicide
Anxious ruminations Medical illness Presence of a child in the home and/or childrearing
Global insomnia Unemployment responsibilities
Psychosis with delusions of poverty or doom Fall in social or economic status Intact marriage
Active or recent alcohol abuse Rejection by spouse or partner Trusting relationship with a counselor, physician, or
Previous suicide attempts other service provider
Anniversary of important losses Employment
a For further details, see Simon (19).
OTHER SUBSTANCES, MULTIPLE The literature suggests numerous to make the patient aware of the process
SUBSTANCE USE, AND SUICIDE schemas to assist in evaluating individu- of rehabilitation. In the case of opioid use
als for potential suicide risks. One schema disorder, this can involve methadone and
Almost all substance use disorders are
categorizes risk factors as either dynamic buprenorphine treatments, which have
associated with an increase in suicide
(acute) or static (long-term) (see box). been shown to protect against suicide.
risk. Research shows that the suicide
Regarding patients who are suicidal and Methadone treatment in particular has
hazard ratio is 1.35 for cocaine use, 2.10
have a concurrent substance use disorder, been shown to make patients 20% less
for psychostimulant use, 3.83 for benzo-
clinicians should pay attention to dynamic likely to commit suicide (21). When treat-
diazepine use, 3.89 for cannabis use, and
risk factors that affect the individual’s life. ing patients with alcohol use disorder, a
11.36 for sedative use (8). Additionally,
These factors can change rapidly but are multilevel model of protection is recom-
marijuana use, cocaine use, alcohol use,
easy to target for treatment intervention. mended. This includes protecting against
and cigarette smoking were all found to
They include current misuse of alcohol biological, behavioral, environmental,
be independently related to suicide, even
and other drugs, concomitant depression, and cultural factors. Effective clinical
after controls for sociodemographic fac-
criminality, and difficulties in controlling care for patients with alcohol use disor-
tors (17). Tobacco use and smoking ap-
aggression and impulsivity. der as well as other psychiatric and med-
pear to contribute to deaths by suicide
The goal of intervention is to treat ical disorders will mitigate suicide risk,
(18). Current smokers are at the highest
acute, modifiable risk factors and to con- given the preponderance of evidence
risk of suicidal ideation, plans, and at-
tinuously ensure the patient’s safety (19). linking alcohol use disorder and suicidal
tempts, followed by past smokers, with
Patients at high risk for suicide should behavior. In addition, easy access to a va-
nonsmokers carrying the lowest risk.
be hospitalized as a precaution, and de- riety of clinical and nonpharmacological
Genetic vulnerabilities in the serotoner-
toxification treatment should be started interventions can be helpful. These in-
gic system may predispose a smoker to
immediately. Subsequently, it is crucial terventions may include psychotherapy,
suicide, although the exact mechanisms
have yet to be elucidated (18).
KEY POINTS/CLINICAL PEARLS
RISK ASSESSMENT AND • Collectively, substance use disorders confer a risk of suicide that is 10–14 times
MANAGEMENT greater than that of the general population; deaths related to substance use are
highest among persons with alcohol use disorders followed by persons who
Currently, no single rating scale or clini-
abuse opiates.
cal algorithm can accurately predict the
risk of suicide, because suicidal behavior • Patients with comorbid alcohol use disorder and a mood disorder have a great-
emanates from a convergence of multiple er risk of suicide attempts compared with patients with a mood disorder alone.
predisposing and concurrent risk factors. • Ongoing suicide risk assessment allows for an integrated treatment plan that
Even if all the scales were combined into enables the clinician to continuously address acute and modifiable suicide risk
a single risk assessment form, other clini- factors, such as preparatory behavior or acute psychosis, while identifying pro-
cal risk factors would be omitted (19). tective factors, which include spirituality, an intact marriage, and child-rearing
Furthermore, suicide is difficult to pre- responsibilities.
dict, as shown in one report suggesting
• The use of methadone and buprenorphine should be prioritized within an in-
that 83% of deaths by suicide were un-
tegrated treatment plan for patients with opioid use disorder to protect against
expected or unavoidable (20). Therefore, suicide; similarly, patients with alcohol use disorder require a multilevel ap-
reasonable clinical assessment and judg- proach, such as detoxification, attendance of rehabilitation programs, and en-
ment is key. gagement in recovery through follow-up programs.
The American Journal of Psychiatry Residents’ Journal | June 2018 7
HOME PREVIOUS NEXT
motivational interviewing, cultural and Drs. Esang and Ahmed are third-year resi- 11. Harris EC, Barraclough B: Suicide as an out-
family engagement, fostering spiritual dents in the Department of Psychiatry at come for mental disorders: a meta-analysis.
Nassau University Medical Center, East Br J Psychiatry 1997; 170:205–228
beliefs, and limiting access to alcohol at
Meadow, N.Y. 12. Piscopo K, Lipari RN, Cooney J, et al: Sui-
the community level. Additionally, clini- cidal thoughts and behavior among adults:
cians should address coexisting smoking results from the 2015 National Survey on
The authors thank Dr. Anna Kim for her as-
addiction, because people with psychiat- Drug Use and Health. Rockville, Md, Sub-
sistance with this article.
ric disorders often have a truncated life stance Abuse and Mental Health Services
Administration, 2016
span due to smoking related diseases and
13. Frierson RL: Suicide attempts by the old and
premature mortality, compared with the REFERENCES
the very old. Arch Intern Med 1991;
general population. Furthermore, nico- 1. Centers for Disease Control and Prevention: 151:141–145
tine use has been shown to contribute to Increase in suicide in the United States, 14. Volkow N: Prescription Opioid Abuse and
deaths by suicide (18, 22). Patients who 1999–2014, National Center for Health Sta- Heroin: Hearings before the House Com-
are reluctant to adopt pharmacological tistics Data Brief. Atlanta, Centers for Dis- mittee on Energy and Commerce Subcom-
ease Control and Prevention, 2016 mittee on Oversight and Investigations,
recommendations should be referred for
2. Wilcox HC, Conner KR, Caine ED, et al: As- 113th Congress, 2nd Session (statement of N.
nonpharmacological treatment modali- sociation of alcohol and drug use disorders Volkow, April 29, 2014).
ties as described above. and completed suicide: an empirical review 15. Rudd RA: Increases in drug and opioid-in-
Taking a closer look at family engage- of cohort studies. Drug Alcohol Depend volved overdose deaths—United States,
ment as an intervention in substance 2004; 76:S11–S19 2010–2015. MMWR 2016; 65:1445–1452
use disorders, the clinician should en- 3. Bertolote JM, Fleischmann A, De Leo D, et 16. Ilgen MA, Bohnert ASB, Ganoczy D, et al:
al: Psychiatric diagnoses and suicide: revis- Opioid dose and risk of suicide. Pain 2016;
gage the patient’s family and friends in
iting the evidence. Crisis 2004; 25:147–155 157:1079–1084
forming a crisis plan. For example, a cri- 4. Nordentoft M, Mortensen PB, Pedersen CB: 17. Brener N, Hassan S, Barrios L, et al: Suicidal
sis plan for a person who abuses opioids Absolute risk of suicide after first hospital ideation among college students in the
should include education and naloxone, contact in mental disorder. Arch Gen Psy- United States. J Consult Clin Psychol 1999;
particularly for those with a high risk chiatry 2011; 68:1058–1064 67:1004–1008
of reattempting suicide via opioid over- 5. Holmstrand C, Bogren M, Mattisson C, et al: 18. Malone KM, Waternaux C, Haas GL, et al:
Long-term suicide risk in no, one or more Cigarette smoking, suicidal behavior, and se-
dose. Such individuals include those tak-
mental disorders: the Lundby Study 1947– rotonin function in major psychiatric disor-
ing high-dose prescription opiates for 1997. Acta Psychiat Scand 2015; 132:459–469 ders. Am J Psychiatry 2003; 160(4):773–779
chronic pain, those recently discharged 6. Oquendo MA, Currier D, Liu S, et al: In- 19. Simon RI: Suicide risk: assessing the unpre-
from the hospital for opioid intoxication creased risk for suicidal behavior in comorbid dictable, in The American Psychiatric Pub-
or overdose, and those recently released bipolar disorder and alcohol use disorders. J lishing Textbook of Suicide Assessment and
from prison with a history of opioid use Clin Psychiatry 2010; 71:902–909 Management, 1st ed. Edited by Simon RI,
7. Nery FG, Soares JC: Comorbid bipolar dis- Hales RE. Washington, DC, American Psy-
disorder (19).
order and substance abuse: evidence-based chiatric Publishing, 2006, pp 1–32
Because patients with substance use options. Curr Psychiatry 2018; 10:57–67 20. Mays D: Structured assessment methods
disorders are prone to suicidal ideation 8. Bohnert KM, Ilgen MA, Louzon S, et al: Sub- may improve suicide prevention. Psychiatr
and attempts, clinicians need to screen stance use disorders and the risk of suicide Annal 2004; 34:366–372
such patients for suicidal thoughts and mortality among men and women in the US 21. Maxwell JC, Pullum TW, Tanner K, et al:
behaviors routinely and continuously Veterans Health Administration. Addiction Deaths of clients in methadone treatment in
2017; 112:1193–1201 Texas: 1994–2002. Drug Alcohol Depend
throughout treatment. Collaboration be-
9. Pompili M, Serafini G, Innamorati M, et al. 2005; 78:73–81
tween substance use treatment provid- Suicidal behavior and alcohol abuse. Int J En- 22. Ahmed S, Stanciu CN: Addiction and sui-
ers, other health care practitioners, fam- viron Res Public Health 2010; 7:1392–1431 cide: an unmet public health crisis. Am J
ily members, and community resources 10. Blow FC, Brockmann LM, Barry KL, et al: Psychiatry Res J 2017; 12(12):3–6
is imperative to the successful rehabili- Role of alcohol in late-life suicide. Alcohol
tation of patients with substance use Clin Exp Res 2004; 28:S48–S56
disorders.
The American Journal of Psychiatry Residents’ Journal | June 2018 8
Вам также может понравиться
- 1109 1176 PDFДокумент68 страниц1109 1176 PDFCleofe Lagura DiazОценок пока нет
- ENG PCIPolicyFrameworkДокумент28 страницENG PCIPolicyFrameworkAdria Putra FarhandikaОценок пока нет
- Understanding SuicideДокумент2 страницыUnderstanding Suicideapi-355166390Оценок пока нет
- TR 228 PDFДокумент234 страницыTR 228 PDFCleofe Lagura DiazОценок пока нет
- SuicideДокумент6 страницSuicideZildian Gem SosaОценок пока нет
- Suicide in America:: Frequently Asked QuestionsДокумент6 страницSuicide in America:: Frequently Asked QuestionsCleofe Lagura DiazОценок пока нет
- 6th Central Pay Commission Salary CalculatorДокумент15 страниц6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Suicide PDFДокумент184 страницыSuicide PDFWilbert Barzola HuamanОценок пока нет
- Understanding Substances & Their Uses PDFДокумент92 страницыUnderstanding Substances & Their Uses PDFmajdОценок пока нет
- Ten Keys To Happier Living - GuidebookДокумент28 страницTen Keys To Happier Living - Guidebookferranuk100% (2)
- Know The Facts About DrugsДокумент20 страницKnow The Facts About DrugszipzapdhoomОценок пока нет
- How To Write An Effective Research ReportДокумент33 страницыHow To Write An Effective Research Reportharshalp1212Оценок пока нет
- 20 Simple Tips To Be Happy Now PDFДокумент11 страниц20 Simple Tips To Be Happy Now PDFLaura OtiОценок пока нет
- 7 Ways PDFДокумент5 страниц7 Ways PDFCleofe Lagura DiazОценок пока нет
- Recovering KeysДокумент28 страницRecovering KeysCleofe Lagura DiazОценок пока нет
- Howtobehappyeveryday LWC PDFДокумент12 страницHowtobehappyeveryday LWC PDFCleofe Lagura Diaz100% (1)
- Annual Review 2016Документ26 страницAnnual Review 2016Cleofe Lagura DiazОценок пока нет
- Neom Happiness Ebook PDFДокумент19 страницNeom Happiness Ebook PDFCleofe Lagura Diaz100% (1)
- Annual Review 2016Документ26 страницAnnual Review 2016Cleofe Lagura DiazОценок пока нет
- Love Yourself Louise HayДокумент1 страницаLove Yourself Louise HayCleofe Lagura DiazОценок пока нет
- Love Yourself Louise HayДокумент1 страницаLove Yourself Louise HayCleofe Lagura DiazОценок пока нет
- Depression Developing Plan To OvercometДокумент13 страницDepression Developing Plan To OvercometCleofe Lagura DiazОценок пока нет
- Annual Review 2016Документ26 страницAnnual Review 2016Cleofe Lagura DiazОценок пока нет
- Apa Style Sample PaperДокумент12 страницApa Style Sample Paperjoerunner407Оценок пока нет
- Coping With DepressionДокумент39 страницCoping With DepressionaldiОценок пока нет
- Love Yourself Louise Hay PDFДокумент1 страницаLove Yourself Louise Hay PDFCleofe Lagura DiazОценок пока нет
- Love Yourself Louise Hay PDFДокумент1 страницаLove Yourself Louise Hay PDFCleofe Lagura DiazОценок пока нет
- Love Yourself Louise HayДокумент12 страницLove Yourself Louise HayCleofe Lagura DiazОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- 1992 Eysenck - The Definition and Measurement of Psychoticism Personality andДокумент29 страниц1992 Eysenck - The Definition and Measurement of Psychoticism Personality andAnoop AnandОценок пока нет
- Psychiatric Medication Use in Pregnancy and BreastfeedingДокумент19 страницPsychiatric Medication Use in Pregnancy and BreastfeedingYamiletRomeroVillaОценок пока нет
- L4 Chapter 4 Mood DisordersДокумент9 страницL4 Chapter 4 Mood DisordersHui Li TehОценок пока нет
- Theory For MassageДокумент16 страницTheory For MassageAnnaya KhanОценок пока нет
- The Kraepelinian Dichotomy - Going, Going - . - But Still Not GoneДокумент4 страницыThe Kraepelinian Dichotomy - Going, Going - . - But Still Not GoneAgustin307Оценок пока нет
- Teen DepressionДокумент6 страницTeen DepressionEmma WatsonОценок пока нет
- Mood Disorders DR Jean-Claude YazbekДокумент167 страницMood Disorders DR Jean-Claude YazbekDaniel GhosseinОценок пока нет
- Bipolar DisorderДокумент30 страницBipolar Disorderapi-401906698Оценок пока нет
- The Association Between Depression and Marital DissatisfactionДокумент22 страницыThe Association Between Depression and Marital DissatisfactionZuluaga LlanedОценок пока нет
- Cannabis Effect On Mental HealthДокумент5 страницCannabis Effect On Mental Healthammaramaryam6463Оценок пока нет
- Basic Concepts of Psychiatric Mental Health Nursing 8th Edition Shives Test BankДокумент8 страницBasic Concepts of Psychiatric Mental Health Nursing 8th Edition Shives Test Bankclaraninht5sqdj100% (29)
- What's New With DSM 5? (Formerly Known As DSM V) : 1 Credit Continuing Education CourseДокумент15 страницWhat's New With DSM 5? (Formerly Known As DSM V) : 1 Credit Continuing Education CourseTodd Finnerty44% (9)
- Homeopathic Alternatives To Conventional Drug TherapiesДокумент239 страницHomeopathic Alternatives To Conventional Drug Therapiesmr.mukundОценок пока нет
- Portofolio Ppds-I Psikiatri Fakultas Kedokteran Universitas Airlangga Rsud Dr. Soetomo - SurabayaДокумент14 страницPortofolio Ppds-I Psikiatri Fakultas Kedokteran Universitas Airlangga Rsud Dr. Soetomo - SurabayaDedy SavradinataОценок пока нет
- Comorbidity Psychiatric Disorders Posttraumatic StressДокумент11 страницComorbidity Psychiatric Disorders Posttraumatic StressReka Jakab-FarkasОценок пока нет
- Anxiety and Sports Performance in Young FemalesДокумент11 страницAnxiety and Sports Performance in Young FemalesGuille monsterОценок пока нет
- Oppositional Defiant Disorder - StatPearls - NCBI BookshelfДокумент5 страницOppositional Defiant Disorder - StatPearls - NCBI BookshelfalexandraОценок пока нет
- Grace Under Pressure Overcoming Depression 1Документ36 страницGrace Under Pressure Overcoming Depression 1Lordivino T. MesinaОценок пока нет
- I Have Never Been (Un) HappierДокумент64 страницыI Have Never Been (Un) HappierSanaa Moledina89% (9)
- Pshcology AssignmentДокумент5 страницPshcology AssignmentAbdul MoizОценок пока нет
- Committee For Proprietary Medicinal Products (CPMP) : London, 26 April 2001 CPMP/EWP/567/98Документ10 страницCommittee For Proprietary Medicinal Products (CPMP) : London, 26 April 2001 CPMP/EWP/567/98uli nadapdapОценок пока нет
- 664723KUДокумент26 страниц664723KUTAMILAN XEROX VtmОценок пока нет
- Mood Disorders Lesson PlanДокумент17 страницMood Disorders Lesson Planapi-2841042060% (1)
- A Guide To What Works For DepressionДокумент96 страницA Guide To What Works For DepressionLynda HernandezОценок пока нет
- Understanding Anger Disorders PDFДокумент429 страницUnderstanding Anger Disorders PDFadaknow100% (2)
- Psychiatry Case Study 1Документ26 страницPsychiatry Case Study 1Sibelle Bou NassifОценок пока нет
- Antidepressants (ME216) 20 5Документ40 страницAntidepressants (ME216) 20 5Dineish MurugaiahОценок пока нет
- Psychology Handicapped MCQДокумент25 страницPsychology Handicapped MCQMohamed Abd ElnaserОценок пока нет
- Rorschach Inkblot TestДокумент16 страницRorschach Inkblot TestAbhishek PatelОценок пока нет
- Schizophrenia Spectrum and Other Psychotic DisordersДокумент84 страницыSchizophrenia Spectrum and Other Psychotic DisordersJara YumiОценок пока нет