Академический Документы
Профессиональный Документы
Культура Документы
Acute Midshaft Clavicular Fracture PDF
Загружено:
Diana Marcela Benítez HernándezОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Acute Midshaft Clavicular Fracture PDF
Загружено:
Diana Marcela Benítez HernándezАвторское право:
Доступные форматы
Acute Midshaft
Clavicular Fracture
Kyle J. Jeray, MD Abstract
Clavicular fractures represent 2.6% to 5% of all fractures, and
middle third fractures account for 69% to 82% of fractures of the
clavicle. The junction of the outer and middle third is the thinnest
part of the bone and is the only area not protected by or reinforced
with muscle and ligamentous attachments. These anatomic
features make it prone to fracture, particularly with a fall on the
point of the shoulder, which results in an axial load to the clavicle.
Optimal treatment of nondisplaced or minimally displaced
midshaft fracture is with a sling or figure-of-8 dressing; the
nonunion rate is very low. However, when midshaft clavicular
fractures are completely displaced or comminuted, and when they
occur in elderly patients or females, the risk of nonunion, cosmetic
deformity, and poor outcome may be markedly higher. Thus, some
surgeons propose surgical stabilization of a complex midshaft
clavicular fracture with either plate-and-screw fixation or
intramedullary devices. Further randomized, prospective trials are
needed to provide better data on which to base treatment decisions.
Dr. Jeray is Program Director,
T he clavicle is one of the most
commonly fractured bones; cla-
vicular fractures represent 2.6% to
practically impossible to maintain,
and a certain amount of deformity is
to be expected, generally compatible
Orthopaedic Surgery Education,
5% of all fractures.1,2 The incidence with satisfactory return of function
Greenville Hospital System, Greenville,
of clavicular fracture in adults is es- in the shoulder.”6 The same text-
SC.
timated to be 71 in 100,000 for men book states that even completely
Neither Dr. Jeray nor the department and 30 in 100,000 for women, with displaced fractures “generally do
with which he is affiliated has received the incidence of midshaft fractures well with non-operative manage-
anything of value from or owns stock in a decreasing with increasing age. Mid- ment....”6
commercial company or institution shaft fractures account for 69% to However, most previous studies
related directly or indirectly to the 82% of all clavicular fractures.1-5 describing the results of clavicular
subject of this article. Midshaft fractures are more common fracture have used surgeon-based or
Reprint requests: Dr. Jeray, Greenville in children and young adults. The in- radiographic outcome measures that
Hospital System, University Medical cidence of high-energy clavicular equate union with success. Very few
Center, Orthopaedic Surgery Education, fractures with comminution, dis- studies on clavicular fracture have
701 Grove Road, 2nd Floor ERC placement, and shortening appears to been published using patient-based
Support Tower, Greenville, SC 29605. be increasing.2 outcomes such as the Medical Out-
Traditionally, fractures of the comes Study 36-Item Short Form
J Am Acad Orthop Surg 2007;15:239-
clavicle have been treated with (QualityMetric, Lincoln, RI) or the
248
closed reduction. More than 200 Disabilities of the Arm, Shoulder
Copyright 2007 by the American methods have been described for and Hand questionnaire (DASH; In-
Academy of Orthopaedic Surgeons. closed reduction, yet a classic text- stitute for Work and Health, Toron-
book recognizes that “reduction is ta, Canada, and the American Acad-
Volume 15, Number 4, April 2007 239
Acute Midshaft Clavicular Fracture
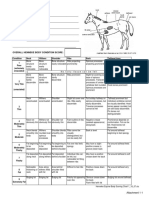
Figure 1 noclavicular (SC) joint cartilage, the
oblique fibers of the costoclavicular
ligaments, and the subclavius mus-
cle. The clavicle is S-shaped and
double-curved, concave ventrally on
its lateral half and convex ventrally
on its medial half. The cross-
sectional geometry changes from flat
laterally to tubular centrally to trian-
gular medially (Figure 1).
The shape of the clavicle and the
ligamentous and muscle attach-
ments play a role in fracture pat-
terns. The junction of the outer and
middle thirds is the thinnest part of
the bone and is the only area not pro-
tected by or reinforced with muscle
and ligamentous attachments, there-
by rendering it prone to fracture, par-
ticularly with axial loading.12 This
helps to explain why the middle
third is the most common site of
fracture, occurring at the junction
Anatomy and cross-sectional geometry of the clavicle. (Adapted with permission
where the bone geometry changes
from Craig EV: Fractures of the shoulder: Part II. Fractures of the clavicle, in
Rockwood CA, Green DP, Bucholz RW [eds]: Rockwood and Green’s Fractures from flat to tubular.
in Adults, ed 3. Philadelphia, PA: JB Lippincott, 1991, vol 1, pp 928-990.) The motion of the clavicle is ulti-
mately linked to the surrounding
motion of the scapula because of the
emy of Orthopaedic Surgeons only the supraclavicular nerves cross- anatomic attachment to the scapula
[AAOS]). Recent studies have indi- ing the bone. However, several fascial through the AC joint and to the ster-
cated that outcomes are not always layers and muscles attach to the bone num through the SC joint. Motion of
excellent, particularly in high- itself and help to create the predict- the clavicle occurs with elevation
energy fractures.7-11 These studies able deformity seen with fractures. and abduction of the arm. During el-
raise the question whether acute The proximal fragment is pulled su- evation, with respect to the SC joint,
midshaft clavicular fractures should periorly and posteriorly by the ster- the clavicle undergoes elevation of
be internally fixed. nocleidomastoid muscle. The distal 11° to 15°, retraction of 15° to 29°,
segment sags forward and rotates in- and posterior long-axis rotation of
feriorly because of the weight of the 15° to 31°, with the magnitude and
Anatomy and Function
upper extremity and, to a lesser ex- planes varying among subjects.13
The clavicle is the first bone to ossify tent, the pull of the pectoralis mus- Other studies suggest that rotation
in the fifth week of fetal life, and it cle on the humerus. may be as much as 50° and elevation
is the only long bone to ossify by in- The clavicle is a strut that con- as high as 30°.14 More importantly,
tramembranous ossification. Initial nects the upper extremity to the clavicle rotation is relatively small
growth up to age 5 years arises from trunk and is the only link to the ax- until humeral elevation exceeds 90°;
the ossification center in the central ial skeleton. It also provides protec- thus, early rehabilitation that avoids
portion of the clavicle, with contin- tion for the adjacent axillary and over-the-shoulder activity will sig-
ued growth occurring at the epiphy- subclavicular neurovascular struc- nificantly limit rotational forces at
seal plates at the medial and lateral tures and the apex of the lungs. Lat- the site of a clavicular fracture.15
ends of the bone. The medial growth erally, the clavicle is secured by the
plate, typically the only plate seen ra- acromioclavicular (AC) and coraco- Mechanism of Injury
diographically, accounts for up to clavicular ligaments where it articu- Midshaft clavicular fractures
80% of longitudinal growth. The me- lates with the acromion. Medially, have traditionally been thought to
dial growth plate is the last physis to the clavicle articulates with the ster- occur from a fall on an outstretched
close, generally at age 22 to 25 years. num and is strongly secured to the hand. However, a biomechanical
The clavicle is subcutaneous, with first rib by the intra-articular ster- analysis of the forces demonstrated
240 Journal of the American Academy of Orthopaedic Surgeons
Kyle J. Jeray, MD
that a direct injury from the shoul- Figure 2
der (rather than the hand) that pro-
duces a force equal to the body
weight would exceed the critical
buckling load and result in a mid-
shaft clavicular fracture.16 Several
studies have demonstrated that a di-
rect fall or blow onto the point of the
shoulder accounts for 85% to 94% of
the injuries.2,3,5,16,17 When the forces
are transmitted through the arm, as
with a fall on an outstretched hand,
the forces are not directly delivered
to the clavicle; thus, they are unlike-
ly to produce a midshaft fracture.
This mechanism accounts for 2% to
5% of all midshaft fractures. A direct
blow to the clavicle, such as from a
hockey stick or a seat belt shoulder-
strap injury, also may produce a frac-
ture and accounts for 10% to 13% of
midshaft fractures in most stud-
ies.16 Although rare, direct force on
the top of the shoulder may drive the
midshaft clavicle against the first
rib, resulting in a fracture.
Robinson’s classification system for midshaft clavicular fractures. (Reproduced with
Classification permission from Robinson CM: Fractures of the clavicle in the adult: Epidemiology
Clavicular fractures have been and classification. J Bone Joint Surg Br 1998;80:476-484.)
classified by Allman18 into three ana-
tomic regions, with the middle third
being group I. The classification sys- classification system will reliably motion at the fracture site. A non-
tem of the Orthopaedic Trauma As- predict treatment and functional displaced or minimally displaced
sociation separates diaphyseal cla- outcomes. fracture may be suspected when pain
vicular fractures into three types: and/or skin changes are present over
06-A (simple), 06-B (wedge) and 06-C the clavicle.
Clinical Evaluation
(complex).19 Each type is further bro- Because middle third fractures
ken down into three groups. Often with clavicular fracture, a frequently occur with high-energy
The system developed by Robin- bruise or abrasion is seen, either over trauma, a complete examination
son3 divides midshaft clavicular frac- the point of the shoulder (indicating should be performed to avoid miss-
tures into type 2A (cortical align- a direct blow) or over the midline ing associated injuries. Skeletal inju-
ment fracture) and type 2B (displaced (suggesting a seat belt shoulder-strap ries include fracture-dislocations of
fracture). In an effort to provide di- injury). The shoulder has a droop, the SC and AC joints or, in younger
rection for treatment and prognosis, the scapula appears slightly internal- patients, physeal injuries. Chest wall
Robinson further divides these into ly rotated, and the shoulder appears trauma may result in high rib frac-
subgroup types 2A1 (nondisplaced), shortened relative to the opposite tures, scapular neck and body frac-
2A2 (angulated), 2B1 (simple or side. This characteristic deformity is tures, and a pneumothorax or he-
wedge comminuted), and 2B2 (isolat- produced by the pull of muscles at- mothorax. Although acute brachial
ed or comminuted segmental) (Fig- tached to the clavicle. Immediate plexus injury is rare, the ulnar nerve
ure 2). Robinson’s classification sys- swelling may obscure the deformity is at highest risk because of its loca-
tem has demonstrated satisfactory of the bone, which will be seen on tion adjacent to the middle third of
levels of interobserver and intraob- radiographs if the fracture is dis- the clavicle. When a nerve injury is
server reliability and reproducibility. placed. Palpation over the area will identified, a thorough vascular ex-
However, additional studies are reveal tenderness, and gentle manip- amination and evaluation of the
needed to determine whether this ulation may produce crepitus and scapulothoracic articulation should
Volume 15, Number 4, April 2007 241
Acute Midshaft Clavicular Fracture
Figure 3
Standard radiographic anteroposterior view (A) and 45° cephalic tilt view (B). Both are necessary to determine the extent of
fracture displacement.
be undertaken to avoid missing an treatment. Displacement without preinjury level. By allowing the clav-
associated injury. Penetrating trau- bony contact, especially with a icle to heal with minimal deformity,
ma is typically the cause of vascular transversely displaced fragment, is a loss of motion and pain can be min-
injury. However, vascular injury can risk factor strongly predictive of imized. Indications for nonsurgical
occur from blunt trauma, resulting long-term sequelae.7 Additional ra- treatment include a nondisplaced or
in spasm or thrombosis of the sub- diographic parameters predictive of minimally displaced midshaft clav-
clavian vessels. increased risk for pain, limitation of icular fracture. Indications for surgi-
motion, or nonunion include an cal treatment include open fractures
overall displacement of the fracture and fractures associated with skin
Radiographic
ends >1.5 cm. This displacement in- compromise or with neurologic or
Evaluation
cludes shortening, distraction, or vascular injury.
To determine the fracture pattern separation of the ends in the anteri- Relative surgical indications in-
and displacement, radiographs in or or posterior direction in any radio- clude certain multiple-system trau-
two projections are necessary. A graphic view.20-22 A second view, at matized patients, a floating shoulder,
standard anteroposterior view should least 45° off plane from the first, and a painful malunion or nonunion.
be accompanied by a 45° cephalic tilt helps to further delineate the dis- More recently, relative indications
view (Figure 3). The shoulder girdle placement. Often, the displacement for surgical treatment have been ex-
and upper lung fields should be is difficult to assess on a single radio- panded to include high-energy closed
carefully assessed to avoid missing graph. For example, as seen in Figure fractures with >15 to 20 mm of
associated fractures or a subtle pneu- 3, both views reveal distraction at shortening, fractures with complete
mothorax. The radiographic evalua- the fracture site of at least 1.5 cm. displacement, and fractures with
tion should assess the fracture pat- comminution.23-26 Although these re-
tern, presence of comminution, cently adopted indications have re-
Management
displacement, and shortening or dis- ceived attention in the current liter-
traction of the fracture. Indications ature, articles dating as far back as
Several radiographic findings can The primary goal in treatment is the 1960s have described similar sur-
help guide the surgeon’s choice of to restore shoulder function to the gical indications—including Neer’s
242 Journal of the American Academy of Orthopaedic Surgeons
Kyle J. Jeray, MD
article,17 which is often cited as sup- Figure 4
port for nonsurgical management.
Randomized controlled trials, one of
which has recently been complet-
ed,11 and another that is currently
under way, are necessary to deter-
mine whether these relative indica-
tions should be considered routine
and, if so, in which patients with
which fracture types.
Nonsurgical Treatment
Historically, nonsurgical treat-
ment has been the mainstay for
clavicular fractures. It has varied
from plaster shoulder spica casts to
benign neglect. Most commonly, a
sling or figure-of-8 brace is applied
in the acute setting. With either de-
vice, immobilization is typically for
2 to 6 weeks, based on the patient’s
Anteroposterior radiograph demonstrating clavicle plating in the anterosuperior
level of comfort. Often, mild dis- position, using a 3.5-mm limited-contact dynamic compression plate.
comfort can linger in adults for
3 months. Return to athletics or
heavy labor is permitted 4 to 6 tion. Traditionally, a skin incision is anteroinferior position, although
weeks after clinical and radiograph- made over the clavicle following less favorable biomechanically,29 al-
ic union has occurred. Light work Langer’s lines, as the skin permits. A lows for drilling in a direction away
with restricted overhead activity newly described alternative is to in- from the subclavian vessels and
can begin once the patient’s comfort cise the inferior skin after pulling it lung. It also keeps the plate from be-
allows, usually in 2 to 4 weeks after over the fracture site.28 As the skin is ing placed under the incision. This
fracture healing. released, it will fall 1 to 2 cm below position theoretically is less likely to
In a prospective, randomized the clavicle and prevent the wound cause irritation, thereby decreasing
study,27 26% of patients treated with from being in contact with the plate the need for plate removal. However,
a figure-of-8 bandage were dissatis- on the clavicle. The aim is to im- the anteroinferior position demands
fied compared with 7% of those prove cosmesis and prevent wound additional soft-tissue stripping and a
treated with a sling. The patients complications. The dissection is more difficult contouring of the
treated with a sling reported less dis- taken down to bone with care to plate compared with the anterosupe-
comfort. There was no difference in identify the cutaneous supraclavic- rior position.
overall healing and alignment of the ular nerves. When necessary, they Ideally, a 3.5-mm dynamic com-
fractures, indicating that a figure- can be sacrificed. It is important to pression plate or plate of similar
of-8 bandage does little to obtain or inform the patient before surgery of strength should be used, with at
maintain reduction. the possibility of a patch of numb- least six cortices on each side. Semi-
ness in the skin inferior to the clav- tubular plates are not as rigid and
Surgical Techniques icle. should not be used.24,31 Reconstruc-
Plates Minimizing subperiosteal strip- tion plates are more easily contoured
Open reduction and internal fixa- ping with gentle handling of the skin and have been used with success;
tion using plates and screws can be and soft tissue helps avoid complica- however, they account for several
done with the patient in either the tions. The plate usually is placed on failures to obtain union and would
supine or the beach-chair position, the tension side of the bone—for the not be the author’s first choice.24,31
with the head and neck tilted away clavicle, the anterosuperior position Precontoured plates of suitable
from the surgical site. A bump is (Figure 4). Biomechanically, this thickness offer the advantage of ease
placed behind the scapula to aid in position provides the best stabili- of placement without manipulation
the reduction. The arm is prepped in ty.29 However, clinically successful of the plate. Locked plates are not
the field to allow for traction and treatment with anteroinferior place- necessary for the acute plating of
manipulation to assist in the reduc- ment also has been described.30 The nonosteoporotic clavicular fractures;
Volume 15, Number 4, April 2007 243
Acute Midshaft Clavicular Fracture
Figure 5 fracture is reduced, and the pin is ad-
vanced antegrade across the fracture
into the medullary canal of the me-
dial segment. The Rockwood Clavi-
cle Pin (DePuy Orthopaedics, War-
saw, IN) has two nuts that go over
the threaded end of the inserted pin
posterolaterally. Once the pin is
across the fracture, the first nut is in-
serted posterolaterally, compressing
the fracture, followed by the second
nut, which is cold-welded to the
first. Figure 5 shows the Rockwood
Clavicle Pin in place. Some of the IM
techniques vary slightly depending
on the device, and not all of the tech-
niques allow for fracture compres-
sion.
Patients are allowed to begin
Anteroposterior radiograph demonstrating the Rockwood Clavicle Pin (DePuy shoulder motion immediately post-
Orthopaedics). Note that the anteromedial cortex is not violated, preventing the pin operatively. When rotational stabil-
from migrating medially. ity is a concern, forward elevation
should be restricted to 90° and ab-
duction to 90° for the first 4 weeks.
there is no significant advantage fixation compared with plate fixa- The Rockwood pin should be re-
over conventional plating, and the tion include less soft-tissue stripping moved at 8 to 14 weeks. In some sit-
cost is higher. at the fracture site, better cosmesis uations, this can be done under local
Once plating is completed, the with a smaller skin incision, easier anesthesia in the office; however,
fascia is repaired over the plate, if hardware removal, and less weak- most Rockwood pins need to be re-
possible, and the skin incision is ness of the bone after hardware re- moved in the operating room. Some
closed. Suture closure is preferable moval. Biomechanically, however, of the other IM devices, such as Her-
to staples. With a sufficiently stable the ability to resist torsional forces bert screws, do not need to be re-
construct, unrestricted shoulder mo- with IM fixation is much less than moved.
tion is allowed, with the exception that with a plate. Migration of the As with plating, a major benefit is
of overhead lifting for 6 weeks. Of- pins also has been a major concern. early return to activities. Several
ten, the pain relief associated with Newer designs, which include lock- studies have reported athletes’ re-
stabilizing the fracture is dramatic, ing nuts on the lateral end of the IM turning to their sport activities by
and efforts to limit the patient’s ac- devices, prevent medial pin migra- 2 to 3 weeks.35,37
tivity may be needed. Pain relief is tion. Newer techniques that avoid
cited as one of the potential benefits penetration of the medial fragment
Complications
of surgical intervention. cortex also prevent medial migration
of the devices.34 Complications can occur from non-
Intramedullary Fixation Patient positioning is similar to surgical treatment as well as surgical
An alternative to plating is in- that for plate fixation. A small inci- treatment. Both can produce a cos-
tramedullary (IM) fixation. Many sion is made over the fracture site, metic deformity (Figure 6). Both can
variations of IM implants have been exposing the fracture ends. The me- result in malunion, nonunion, pain,
described over the past 40 years, in- dial segment is prepared by drilling local tenderness or irritation, and
cluding Hagie pins, modified Hagie into the medullary canal, but the an- limitation of motion. Other rare
pins, Knowles pins, Herbert screws, terior medial cortex is not violated. complications following surgical or
Steinmann pins, elastic nails, can- The distal segment is drilled retro- nonsurgical treatment are residual
cellous screws, and Kirschner grade through the canal, exiting the nerve paresthesia; subclavian ves-
wires.32-36 Modifications in the tech- posterior lateral cortex. The pin is sel compression, thrombosis, and
nique have led to a resurgence of in- inserted retrograde through the ca- pseudoaneurysm; thoracic outlet
terest in IM fixation of these frac- nal and exits through the posterolat- syndrome; and brachial plexus neu-
tures. The potential benefits of IM eral hole and out the skin. Next, the ropathy.
244 Journal of the American Academy of Orthopaedic Surgeons
Kyle J. Jeray, MD
Figure 6
A, Healed clavicular fracture managed nonsurgically. The bump, shortened shoulder width, and subtle droop are evident.
B, A healed clavicular fracture treated with plate and screws, showing prominence of the anterior-superior–positioned plate.
Some complications are unique union rate of 3.7% in patients who
Results
to surgical intervention, such as in- underwent surgery compared with
fection and hardware problems. In- Whether treated nonsurgically or 0.8% in those treated without sur-
fection rates vary from 0% to 18%, surgically, most clavicular fractures gery. Neer17 reported nonunion rates
with the lower rates reported in the heal without incident when length of 0.1% with nonsurgical treatment
more recent studies.24,31,37,38 Painful, and alignment are maintained. Ac- and 4.6% with surgical treatment.
irritating hardware requiring plate or ceptable cosmetic and functional re- Neer17 suggested that the most im-
pin removal is reported to be as high sults should be expected. Satisfacto- portant causal factor for nonunion of
as 50% to 100%.24,39 Following plate ry results occur less consistently a midshaft clavicular fracture is im-
removal, the risk for refracture rang- when the fracture fails to heal or proper open surgery. This may be
es from 0% to 8%.24,31 Adhesive cap- heals with a significant deformity. true to some extent; aggressive soft-
sulitis of the shoulder has been re- tissue stripping, inability to reduce
ported with surgical treatment in Nonunion the fracture, and inadequate internal
0% to 7% of cases.24,28 Most cases of nonunion are symp- fixation all can lead to poor results.
IM devices are associated with tomatic, presenting with pain, loss Several recent studies have re-
unique complications, including mi- of function, neurologic changes, ported high union rates with surgical
gration of the pin and hardware irri- and/or unsightly clavicular deformi- intervention using a variety of inter-
tation, resulting in local skin break- ty. Although clavicular nonunion nal fixation devices, including plat-
down that often requires antibiotics has not been clearly defined in the ing and IM pin or rod fixation.39,40 In
and, ultimately, hardware remov- literature, most authors concur that addition, there is evidence that the
al.39 Figure 7 illustrates skin break- nonunion is present when healing nonunion rate after nonsurgical treat-
down from an IM pin. Although has not occurred by 16 weeks. ment may be higher than previously
most of these complications are rare, Traditional thinking is that cla- reported, particularly in certain frac-
a second surgery for plate or pin re- vicular fractures treated nonsurgical- ture types and in certain patients. In
moval is sufficiently frequent to be ly almost always heal and that surgi- their review of 581 nonsurgically
considered when reviewing treat- cal treatment increases the risk of treated fractures, Robinson et al20 re-
ment choices. nonunion. Rowe4 reported a non- ported an overall nonunion rate of
Volume 15, Number 4, April 2007 245
Acute Midshaft Clavicular Fracture
Figure 7
Healed clavicular fracture treated with intramedullary pinning. A, Note incision size and location over fracture and posterolateral
prominence. B, Early breakdown of the skin resulting from a prominent pin at the posterolateral insertion site.
4.5% for diaphyseal fractures. Strat- were from evidence-based level III, ment. Symptomatic patients help
ification of Robinson’s data revealed IV, and V studies (ie, observational, define the malunion. Symptoms in-
that women with displaced diaphy- retrospective, case series, and expert clude weakness and pain in the in-
seal fractures had a nonunion rate opinion studies) rather than from volved shoulder, loss of shoulder
ranging from 19% to 33%. When level I and II studies (ie, randomized, motion, loss of endurance, neurolog-
comminution was combined with prospective studies). ic symptoms consistent with thorac-
displacement, the nonunion rate in Surgical treatment of nonunion ic outlet syndrome and brachial
women increased to a range of 33% has a high success rate. Techniques plexus impingement, and cosmetic
to 47%.41 In addition to fracture frag- include plate fixation with bone deformity.46
ment displacement, female sex, and graft, IM pin fixation with bone In 1986, Eskola et al21 noted in
comminution, other risk factors graft, and external fixation. Union 89 patients that shortening >12 mm
identified with nonunion include ad- rates with each method have been was associated with increased pain.
vancing age, lack of cortical apposi- reported to be >92% and as high as Wick et al22 concluded in a retrospec-
tion, severity of the initial trauma, 100%.42-45 Plate fixation has the tive study that shortening of 2 cm in
the extent of fracture fragment dis- largest support in the literature and midshaft clavicular fractures was as-
placement,25 and, arguably, soft- is currently the most predictable sociated with an increased risk of
tissue interposition.42 Early mobiliza- and recommended treatment for pain, limitation of motion, or non-
tion has not been associated with the symptomatic nonunion. Other union. McKee et al9 assessed func-
development of a nonunion, whether methods may be successful in the tional outcome following displaced
treated surgically or nonsurgically. hands of an experienced surgeon. clavicular fractures and noted signif-
A recently published systematic icantly inferior scores for both the
review of the literature on nonunion Malunion upper extremity–specific (DASH)
after treatment of midshaft clavicu- Most nonsurgically treated cla- outcome scores (P = 0.02) and the
lar fractures revealed a 5.9% non- vicular fractures heal with some de- Constant scores (P = 0.01) compared
union rate in nonsurgically managed formity. The literature does not with the general population. They
fractures.8 In the completely dis- clearly define when a deformity is concluded that fractures with >2 cm
placed fractures, the rate increased to considered to be a malunion; howev- of shortening tended to be associated
15.1%. In surgically treated displaced er, the evidence strongly suggests with decreased abduction strength
fractures, plating of 460 fractures re- that some clavicular deformities re- and greater patient dissatisfaction.
sulted in a nonunion rate of 2.2%, sult in unsatisfactory outcomes. The Hill et al25 reported on completely
and IM fixation of 152 fractures re- deformity is a three-dimensional displaced middle third clavicular
sulted in a nonunion rate of 2.0%.8 problem; the most consistent char- fractures and concluded that final
These data should be interpreted acteristic is shortening with inferior shortening ≥2 cm was associated
with caution, however, because most displacement of the medial frag- with an unsatisfactory result but not
246 Journal of the American Academy of Orthopaedic Surgeons
Kyle J. Jeray, MD
with nonunion. After closed treat- tion with a plate and screws resulted ized, prospective studies are needed
ment, 31% of patients were dissatis- in an improved functional outcome to determine whether the benefits of
fied with the final result, 54% were and a lower rate of malunion and surgical fixation outweigh the risks
unhappy with the appearance, and nonunion compared with nonsurgi- and, if so, in which types of patients
15% of fractures failed to unite. Us- cal treatment at 1 year.11 and for which types of midshaft cla-
ing the same subjective patient ques- Treatment of a malunion consists vicular fracture.
tionnaire as that used by Hill et of surgical correction to restore
al,25 Lazarides and Zafiropoulos10 re- length, angular deformity, and rota- References
ported that final clavicular shorten- tion of the clavicle. Treatment may
ing >18 mm in males and >14 mm in or may not involve an intercalary Evidence-based Medicine: Level I/II
females was associated with unsatis- bone graft. Often, after removing the prospective studies are references
factory results and with increased callus of the malunion, it is possible 5, 7, 8, and 27. The remaining refer-
patient symptoms. to identify the proximal and distal ences are level III/IV case-control co-
Ledger et al47 showed the effect of fragments in order to anatomically hort studies or level V, expert opinion.
clavicular shortening >15 mm on reconstruct the clavicle.46,48 The ben-
Citation numbers printed in bold
biomechanical parameters of the efit of this technique is that there is
type indicate references published
shoulder. They found a significant no donor-site morbidity for a bone
within the past 5 years.
increase in upward angulation graft. When difficulty in determining
(mean, 10.7°; P < 0.005) of the SC the length of the malunited clavicle 1. Postacchini F, Gumina S, De Santis P,
joint on the injured side compared is anticipated, a preoperative radio- Albo F: Epidemiology of clavicle frac-
with the uninjured side. The muscle graphic image of both clavicles is tures. J Shoulder Elbow Surg 2002;
11:452-456.
torque of the injured arm was signif- helpful. Both IM devices and plates
2. Nordqvist A, Petersson C: The inci-
icantly weaker than that of the unin- have been used successfully to treat dence of fractures of the clavicle.
jured arm in extension (P < 0.05), ad- malunions.46,48-50 Treatment of symp- Clin Orthop Relat Res 1994;300:127-
duction (P < 0.05), and internal tomatic malunions has resulted in 132.
rotation (P < 0.05).47 improvement of the function of the 3. Robinson CM: Fractures of the clavi-
These studies indicate that al- cle in the adult: Epidemiology and
upper extremity, decreased pain, and
classification. J Bone Joint Surg Br
though clavicular deformities are increased patient satisfaction.46,50 1998;80:476-484.
complex and hard to assess, shorten- 4. Rowe CR: An atlas of anatomy and
ing of 1.5 to 2 cm, which results in an treatment of midclavicular fractures.
Summary Clin Orthop Relat Res 1968;58:29-
increased incidence of clinical symp-
42.
toms, is one parameter that can be The frequency of comminuted and
5. Nowak J, Mallmin H, Larsson S: The
measured. Further investigation is displaced midshaft clavicular frac- aetiology and epidemiology of clavic-
needed to clearly define the patients tures that result from high-energy ular fractures: A prospective study
as well as the fracture deformity that injuries is increasing. Nondisplaced during a two-year period in Uppsala,
is likely to be symptomatic with a and minimally displaced fractures Sweden. Injury 2000;31:353-358.
6. Neer CS: Fractures of the clavicle, in
clavicular malunion. In this way, should be treated nonsurgically,
Rockwood CA, Green DP (eds): Frac-
acute surgical treatment could be of- preferably with a sling for patient tures in Adults, ed 2. Philadelphia,
fered to the patients who are most comfort; the rates of nonunion, pain, PA: JB Lippincott, 1981, pp 707-713.
likely to benefit. In addition, compar- cosmetic deformity, and loss of func- 7. Nowak J, Holgersson M, Larsson S:
ative trials are necessary to establish tion are low. However, for specific Can we predict long-term sequelae af-
ter fractures of the clavicle based on
that patients with clavicular frac- groups of patients, the risk of com-
initial findings? A prospective study
tures that predictably result in defor- plications from nonsurgical manage- with nine to ten years of follow-up.
mity have better outcomes when ment may be significantly higher. J Shoulder Elbow Surg 2004;13:479-
treated surgically rather than nonsur- These patients include those with 486.
gically. Several randomized trials cur- completely displaced and commi- 8. Zlowodzki M, Zelle BA, Cole PA,
Jeray K, McKee MD, Evidence-Based
rently are under way, and one has nuted fractures and, possibly, those
Orthopaedic Trauma Working Group:
been completed, assessing the surgi- who are female or of advanced age. Treatment of acute midshaft clavicle
cal versus nonsurgical management The current literature suggests that fractures: Systematic review of 2144
of acute displaced midshaft clavicu- surgical stabilization, with either fractures. On behalf of the Evidence-
lar fractures. The Canadian Ortho- plates and screws or with an IM de- Based Orthopaedic Trauma Working
Group. J Orthop Trauma 2005;19:
paedic Trauma Society has shown in vice, should be considered as the pre-
504-507.
a multicenter randomized trial of 132 ferred treatment option for these 9. McKee MD, Pedersen EM, Jones C, et
patients that for displaced fractures more complex acute midshaft cla- al: Deficits following nonoperative
of the clavicular shaft, surgical fixa- vicular fractures. Further random- treatment of displaced midshaft cla-
Volume 15, Number 4, April 2007 247
Acute Midshaft Clavicular Fracture
vicular fractures. J Bone Joint Surg Scheele A, Petersson CJ: Shortening of 2-7 years. Acta Orthop Scand 2002;
Am 2006;88:35-40. clavicle after fracture: Incidence and 73:134-139.
10. Lazarides S, Zafiropoulos G: Conser- clinical significance, a 5-year follow- 37. Verborgt O, Pittoors K, Van Glabbeek
vative treatment of fractures at the up of 85 patients. Acta Orthop Scand F, Declercq G, Nuyts R, Somville J:
middle third of the clavicle: The rele- 1997;68:349-351. Plate fixation of middle-third clavicle
vance of shortening and clinical out- 24. Böstman O, Manninen M, Pihlajama- fractures in the semi-professional ath-
come. J Shoulder Elbow Surg 2006; ki H: Complications of plate fixation lete. Acta Orthop Belg 2005;71:17-
15:191-194. in fresh displaced midclavicular frac- 21.
11. Canadian Orthopaedic Trauma Soci- tures. J Trauma 1997;43:778-783. 38. Wu CC, Shih CH, Chen WJ, Tai CL:
ety: Nonoperative treatment com- 25. Hill JM, McGuire MH, Crosby LA:
Treatment of clavicular aseptic non-
pared with plate fixation of displaced Closed treatment of displaced middle-
union: Comparison of plating and
midshaft clavicular fractures: A mul- third fractures of the clavicle gives
intramedullary nailing techniques.
ticenter, randomized clinical trial. poor results. J Bone Joint Surg Br
J Trauma 1998;45:512-516.
J Bone Joint Surg Am 2007;89:1-10. 1997;79:537-539.
12. Ljunggren AE: Clavicular function. 26. Oroko PK, Buchan M, Winkler A, 39. Ali Khan MA, Lucas HK: Plating of
Acta Orthop Scand 1979;50:261-268. Kelly IG: Does shortening matter af- fractures of the middle third of the
13. Ludewig PM, Behrens SA, Meyer SM, ter clavicular fractures? Bull Hosp Jt clavicle. Injury 1978;4:263-267.
Spoden SM, Wilson LA: Three- Dis 1999;58:6-8. 40. Zenni EJ Jr, Krieg JK, Rosen MJ: Open
dimensional clavicular motion during 27. Andersen K, Jensen PO, Lauritzen J: reduction and internal fixation of
arm elevation: Reliability and de- Treatment of clavicular fractures: clavicular fractures. J Bone Joint Surg
scriptive data. J Orthop Sports Phys Figure-of-eight versus a simple sling. Am 1981;63:147-151.
Ther 2004;34:140-149. Acta Orthop Scand 1987;58:71-74. 41. Brinker MR, Edwards TB, O’Connor
14. Simpson NS, Jupiter JB: Clavicular 28. Coupe BD, Wimhurst JA, Indar R, DP: Estimating the risk of nonunion
nonunion and malunion: Evaluation Calder DA, Patel AD: A new approach following nonoperative treatment of a
and surgical management. J Am for plate fixation of midshaft clavicu- clavicular fracture. J Bone Joint Surg
Acad Orthop Surg 1996;4:1-8. lar fractures. Injury 2005;36:1166- Am 2005;87:676-677.
15. Fung M, Kato S, Barrance PJ, et al: 1171. 42. Manske DJ, Szabo RM: The operative
Scapular and clavicular kinematics 29. Iannotti MR, Crosby LA, Stafford P, treatment of mid-shaft clavicular
during humeral elevations: A study Grayson G, Goulet R: Effects of plate non-unions. J Bone Joint Surg Am
with cadavers. J Shoulder Elbow Surg location and selection on the stability 1985;67:1367-1371.
2001;10:278-285. of midshaft clavicle osteotomies: A 43. Jupiter JB, Leffert RD: Non-union of the
16. Stanley D, Trowbridge EA, Norris SH: biomechanical study. J Shoulder clavicle: Associated complications and
The mechanism of clavicular frac- Elbow Surg 2002;11:457-462. surgical management. J Bone Joint
ture: A clinical and biomechanical 30. Kloen P, Sorkin AT, Rubel IF, Helfet Surg Am 1987;69:753-760.
analysis. J Bone Joint Surg Br 1988; DL: Anterioinferior plating of mid 44. Karaharju E, Joukainen J, Peltonen J:
70:461-464. shaft clavicular nonunions. J Orthop Treatment of pseudarthrosis of the
17. Neer CS II: Nonunion of the clavicle. Trauma 2002;16:425-430. clavicle. Injury 1982;13:400-403.
JAMA 1960;172:1006-1011. 31. Poigenfürst J, Rappold G, Fischer W: 45. Boehme D, Curtis RJ Jr, DeHaan JT,
18. Allman FL Jr: Fractures and ligamen- Plating of fresh clavicular fractures: Kay SP, Young DC, Rockwood CA Jr:
tous injuries of the clavicle and its ar- Results of 122 operations. Injury Non-union of fractures of the mid-
ticulation. J Bone Joint Surg Am 1992;23:237-241. shaft of the clavicle: Treatment with a
1967;49:774-784. 32. Ngarmukos C, Parkpian V, Patradul modified Hagie intramedullary pin
19. Fracture and dislocation compendi- A: Fixation of fractures of the mid- and autogenous bone-grafting. J Bone
um: Orthopaedic Trauma Association shaft of the clavicle with Kirschner Joint Surg Am 1991;73:1219-1226.
Committee for Coding and Classifica- wires: Results in 108 patients. J Bone 46. McKee MD, Wild LM, Schemitsch
tion. J Orthop Trauma 1996;10(suppl Joint Surg Br 1998;80:106-108. EH: Midshaft malunions of the clavi-
1):1-154. 33. Grassi FA, Tajana MS, D’Angelo F: cle. J Bone Joint Surg Am 2003;85:
20. Robinson CM, Court-Brown CM, Management of midclavicular frac- 790-797.
McQueen MM, Wakefield AE: Esti- tures: Comparison between nonoper- 47. Ledger M, Leeks N, Ackland T, Wang
mating the risk of nonunion following ative treatment and open intramedul- A: Short malunions of the clavicle:
nonoperative treatment of a clavicu- lary fixation in 80 patients. J Trauma An anatomic and functional study.
lar fracture. J Bone Joint Surg Am 2001;50:1096-1100. J Shoulder Elbow Surg 2005;14:349-
2004;86:1359-1365. 34. Leppilahti J, Jalovaara P: Migration of 354.
21. Eskola A, Vainionpää S, Myllynen P, Kirschner wires following fixation of 48. Basamania CJ: Abstract: “Claviculo-
Pätiälä H, Rokkanen P: Outcome of the clavicle: A report of 2 cases. Acta plasty” and intramedullary fixation of
clavicular fracture in 89 patients. Orthop Scand 1999;70:517-519. malunited, shortened clavicle fractures.
Arch Orthop Trauma Surg 1986;105: 35. Jubel A, Andemahr J, Bergmann H, J Shoulder Elbow Surg 1999;8:540.
337-338. Prokop A, Rehm KE: Elastic stable in- 49. Bosch U, Skutek M, Peters G, Tscherne
22. Wick M, Müller EJ, Kollig E, Muhr G: tramedullary nailing of midclavicular H: Extension osteotomy in malunited
Midshaft fractures of the clavicle with fractures in athletes. Br J Sports Med clavicular fractures. J Shoulder
a shortening of more than 2 cm pre- 2003;37:480-484. Elbow Surg 1998;7:402-405.
dispose to nonunion. Arch Orthop 36. Chu CM, Wang SJ, Lin LC: Fixation of 50. Chan KY, Jupiter JB, Leffert RD,
Trauma Surg 2001;121:207-211. mid-third clavicular fractures with Marti R: Clavicle malunion. J Shoul-
23. Nordqvist A, Redlund-Johnell I, von Knowles pins: 78 patients followed for der Elbow Surg 1999;8:287-290.
248 Journal of the American Academy of Orthopaedic Surgeons
Вам также может понравиться
- FxClavícula PDFДокумент7 страницFxClavícula PDFPenélope CrespoОценок пока нет
- FX Pelvic Rim Injury17Документ8 страницFX Pelvic Rim Injury17Antonio PáezОценок пока нет
- Complex Elbow InstabilityДокумент9 страницComplex Elbow InstabilityAristoteles Plato SocratesОценок пока нет
- Midshaft Clavicle Fractures AДокумент9 страницMidshaft Clavicle Fractures AFreddyChandraNainggolanОценок пока нет
- Current Concepts Tibial Plateau FXДокумент14 страницCurrent Concepts Tibial Plateau FXOrtho 20172100% (1)
- Current Concepts in Elbow Fracture Dislocation: Adam C Watts, Jagwant Singh, Michael Elvey and Zaid HamoodiДокумент8 страницCurrent Concepts in Elbow Fracture Dislocation: Adam C Watts, Jagwant Singh, Michael Elvey and Zaid HamoodiJoão Artur BonadimanОценок пока нет
- 2008 - Elbow Dislocation - OCNAДокумент7 страниц2008 - Elbow Dislocation - OCNAharpreet singhОценок пока нет
- Elbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Документ15 страницElbow Fractures: Distal Humerus: The American Society For Surgery of The Hand.)Radu UrcanОценок пока нет
- Common Pediatric Elbow Fractures: Erin S. Hart Allison Turner Maurice Albright Brian E. GrottkauДокумент7 страницCommon Pediatric Elbow Fractures: Erin S. Hart Allison Turner Maurice Albright Brian E. GrottkauFino SopianОценок пока нет
- Managementofdistal Femurfracturesinadults: An Overview of OptionsДокумент12 страницManagementofdistal Femurfracturesinadults: An Overview of OptionsDoctor's BettaОценок пока нет
- 2001 - Cartilage Substitutes - Overview of Basic Science and Treatment OptionsДокумент16 страниц2001 - Cartilage Substitutes - Overview of Basic Science and Treatment Optionsgrofecbio1Оценок пока нет
- Fractures of The Radial Head (2013)Документ9 страницFractures of The Radial Head (2013)Say MamenОценок пока нет
- Calcaneal Fractures Where Are We NowДокумент11 страницCalcaneal Fractures Where Are We NowfunmugОценок пока нет
- Hombro Inlges PDFДокумент6 страницHombro Inlges PDFOscar Segun DoОценок пока нет
- Hand Clin 2007 23 (2) 165Документ13 страницHand Clin 2007 23 (2) 165Juan Del rosalОценок пока нет
- Clavicula FractureДокумент6 страницClavicula Fracturedrian pamungkasОценок пока нет
- Fractures of The Cervical Spine: ReviewДокумент7 страницFractures of The Cervical Spine: ReviewMeri Fitria HandayaniОценок пока нет
- Fraser MoodieДокумент11 страницFraser MoodieWiindaОценок пока нет
- Tompkins, JPOSNA ARTICLE 172 - FINAL UPDATEDДокумент13 страницTompkins, JPOSNA ARTICLE 172 - FINAL UPDATEDTania RahamanОценок пока нет
- Toorthj 7 329 PDFДокумент5 страницToorthj 7 329 PDFmuhammad robyОценок пока нет
- Femoral Neck Fractures in Young Patients State Of.3Документ5 страницFemoral Neck Fractures in Young Patients State Of.3Rizwan Ahamed T AОценок пока нет
- Complex Elbow Instability: Matthew Dipaola, MD, William B. Geissler, MD, A. Lee Osterman, MDДокумент14 страницComplex Elbow Instability: Matthew Dipaola, MD, William B. Geissler, MD, A. Lee Osterman, MDAndrea Z MilanoОценок пока нет
- Fractures of The Condylar ProcessДокумент15 страницFractures of The Condylar Processmargarita mogollonОценок пока нет
- Distal Radius FractureДокумент16 страницDistal Radius FractureDeneishMuruОценок пока нет
- Anexo 01 Clase 04 Unidad IiДокумент9 страницAnexo 01 Clase 04 Unidad IiSebastiánCandiaОценок пока нет
- Perioperative Management of Distal Radius Fractures: Jiang An Lim, Bryan LC Loh, George Sylvestor and Wasim KhanДокумент5 страницPerioperative Management of Distal Radius Fractures: Jiang An Lim, Bryan LC Loh, George Sylvestor and Wasim Khansuci triana putriОценок пока нет
- Pediatric Supracondylar Fractures of The Distal Humerus: Provided by Springer - Publisher ConnectorДокумент7 страницPediatric Supracondylar Fractures of The Distal Humerus: Provided by Springer - Publisher ConnectorBison_sonОценок пока нет
- Humeral Non UnionДокумент12 страницHumeral Non Unionmmqk122Оценок пока нет
- Art 1Документ10 страницArt 1Danilo LlumitasigОценок пока нет
- Fractura Cadera 1Документ22 страницыFractura Cadera 1Júlia LedesmaОценок пока нет
- Sacral Alae S1 and S2Документ11 страницSacral Alae S1 and S2Aysiah AzhariОценок пока нет
- Monteggia Fractures - Pearls and PitfallsДокумент9 страницMonteggia Fractures - Pearls and PitfallsdrdabielmaderacОценок пока нет
- 17 - Distal Radius FracturesДокумент78 страниц17 - Distal Radius FracturesFlorin PanduruОценок пока нет
- Occlusal Schemes in FPDДокумент6 страницOcclusal Schemes in FPDPadmini ReddyОценок пока нет
- Humerus FractureДокумент5 страницHumerus FracturecyahiminОценок пока нет
- Sarver PDFДокумент8 страницSarver PDFanon_768201406Оценок пока нет
- GaleazziДокумент11 страницGaleazzijuanitiusОценок пока нет
- 11.clavicle Fractures REVДокумент11 страниц11.clavicle Fractures REVRika Yulizah GobelОценок пока нет
- Currentmanagementof Metacarpalfractures: Rafael Diaz-Garcia,, Jennifer F. WaljeeДокумент12 страницCurrentmanagementof Metacarpalfractures: Rafael Diaz-Garcia,, Jennifer F. WaljeeHarry CenОценок пока нет
- Reconstruction of Posttraumatic Disorders of The ForearmДокумент12 страницReconstruction of Posttraumatic Disorders of The Forearmsinung bawonoОценок пока нет
- Manejo de Fracturas Mediales de Cadera 2015 Femoral Neck Fractures - Current ManagementДокумент9 страницManejo de Fracturas Mediales de Cadera 2015 Femoral Neck Fractures - Current ManagementSergio Tomas Cortés MoralesОценок пока нет
- 2022 Fracturas Mandibulares de CondiloДокумент14 страниц2022 Fracturas Mandibulares de CondiloPaola AlcocerОценок пока нет
- Distal Clavicle Fracture Radiography and Treatment: A Pictorial EssayДокумент9 страницDistal Clavicle Fracture Radiography and Treatment: A Pictorial EssayAdella Maharani SОценок пока нет
- Stav SoucasnyДокумент14 страницStav SoucasnyTommysОценок пока нет
- Subtrochanteric Femur Fractures: Asheesh Bedi, MD, T. Toan Le, MDДокумент11 страницSubtrochanteric Femur Fractures: Asheesh Bedi, MD, T. Toan Le, MDMd.Shafiul EzazОценок пока нет
- Cia 5 337Документ9 страницCia 5 337Shahid HussainОценок пока нет
- Classification of Pelvic Fractures and Its Clinical RelevanceДокумент6 страницClassification of Pelvic Fractures and Its Clinical RelevanceMohamed AzeemОценок пока нет
- Fractures of Clavicle AserДокумент44 страницыFractures of Clavicle AserHeba ElgoharyОценок пока нет
- Spinal Cord Injury: Causation & PathophysiologyДокумент10 страницSpinal Cord Injury: Causation & Pathophysiologycpradheep100% (3)
- Ac Joint Seperation Clavicle FractureДокумент5 страницAc Joint Seperation Clavicle Fractureapi-356829966Оценок пока нет
- Evidence-Based Review of Distal Radius Fractures: Benjamin M. Mauck,, Colin W. SwiglerДокумент12 страницEvidence-Based Review of Distal Radius Fractures: Benjamin M. Mauck,, Colin W. SwiglerOrtopedia HGMОценок пока нет
- Fractures Radial Head & Neck. JBJS. 2013Документ10 страницFractures Radial Head & Neck. JBJS. 2013C Martin TraumatoОценок пока нет
- Acute Distal Radioulnar Joint InstabilityДокумент13 страницAcute Distal Radioulnar Joint Instabilityyerson fernando tarazona tolozaОценок пока нет
- Misra 2019Документ3 страницыMisra 2019Jawhar DhiafОценок пока нет
- Mandibulasr Truma ManagementДокумент18 страницMandibulasr Truma Managementjoal510Оценок пока нет
- Surgery Management of Fractures, Dislocations, and Traumatic Instability of The ElbowДокумент17 страницSurgery Management of Fractures, Dislocations, and Traumatic Instability of The ElbowErvaldi IlhamОценок пока нет
- Galeazzi-Fracture 6Документ14 страницGaleazzi-Fracture 6MIGUEL ANGEL MEJIA FERNANDEZОценок пока нет
- Fractures Pathophysiology Treatment and Nursing CareДокумент9 страницFractures Pathophysiology Treatment and Nursing Careaddica0% (1)
- Acromioclavicular Joint Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandAcromioclavicular Joint Injury, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Acetabular Fractures in Older Patients: Assessment and ManagementОт EverandAcetabular Fractures in Older Patients: Assessment and ManagementTheodore T. MansonОценок пока нет
- Pain Therapy in Children and Adolescents: Boris Zernikow, Tanja HechlerДокумент17 страницPain Therapy in Children and Adolescents: Boris Zernikow, Tanja HechlerNUR AIDAОценок пока нет
- The Use of MRI in Evaluating Knee Pain in Patients Aged 40 Years and OlderДокумент7 страницThe Use of MRI in Evaluating Knee Pain in Patients Aged 40 Years and OlderDiana Marcela Benítez HernándezОценок пока нет
- Management of Fractures of The Proximal UlnaДокумент12 страницManagement of Fractures of The Proximal UlnaDiana Marcela Benítez HernándezОценок пока нет
- Terrible Triad Injury of He ElbowДокумент15 страницTerrible Triad Injury of He Elbowbarbara liuva chia policarpoОценок пока нет
- Trauma en Pediatria. Evaluacion. J Emerg Crit Care Med 2018 2:3Документ8 страницTrauma en Pediatria. Evaluacion. J Emerg Crit Care Med 2018 2:3Diana Marcela Benítez HernándezОценок пока нет
- Management of The Floating Knee.Документ8 страницManagement of The Floating Knee.barbara liuva chia policarpoОценок пока нет
- Treatment of Distal Radius Fractures.7 PDFДокумент10 страницTreatment of Distal Radius Fractures.7 PDFHayudhiaОценок пока нет
- Journal Orthopedi 3Документ5 страницJournal Orthopedi 3Nur SulistiyaningsihОценок пока нет
- Fractura Tercio Medio ClavíДокумент5 страницFractura Tercio Medio ClavíDiana Marcela Benítez HernándezОценок пока нет
- Metabolic Syndrome and Sistemic Inflammation in Patients With COPDДокумент5 страницMetabolic Syndrome and Sistemic Inflammation in Patients With COPDDiana Marcela Benítez HernándezОценок пока нет
- B Blockers and Their Mortality Benefits Underprescribed in Heart Failure and Chronic Obstructive Pulmonary DiseaseДокумент12 страницB Blockers and Their Mortality Benefits Underprescribed in Heart Failure and Chronic Obstructive Pulmonary DiseaseDiana Marcela Benítez HernándezОценок пока нет
- Immunologic Correlates of The AbscopalДокумент7 страницImmunologic Correlates of The AbscopalDiana Marcela Benítez HernándezОценок пока нет
- Catalogue of Unlocking Plates Suzhou Youbetter Medical Apparatus Co., LTDДокумент9 страницCatalogue of Unlocking Plates Suzhou Youbetter Medical Apparatus Co., LTDazisaaiОценок пока нет
- How To Take and Read Hip Joint Radiographs in A Structured WayДокумент2 страницыHow To Take and Read Hip Joint Radiographs in A Structured WaySamantha Orozco PinedaОценок пока нет
- Bone TumorsДокумент15 страницBone Tumorssarguss1450% (2)
- IARC Technical Report No10-9 PDFДокумент89 страницIARC Technical Report No10-9 PDFTanОценок пока нет
- Gr6 Revision - PPT Ete 1Документ30 страницGr6 Revision - PPT Ete 1Doaa AlhussienyОценок пока нет
- II - 4.anterior Cranial FossaДокумент2 страницыII - 4.anterior Cranial FossaalllexissssОценок пока нет
- Anaphy GRAPHIC - ORGANIZERДокумент6 страницAnaphy GRAPHIC - ORGANIZERLuna ScorpiusОценок пока нет
- Muscles That Move The Pectoral GirdleДокумент65 страницMuscles That Move The Pectoral GirdleJennifer FirestoneОценок пока нет
- Lower Extremity Anatomy: Sari Tri Yulianti, S.FT., M.BiomedДокумент73 страницыLower Extremity Anatomy: Sari Tri Yulianti, S.FT., M.BiomedDindaОценок пока нет
- Henneke BCS ChartДокумент1 страницаHenneke BCS ChartLaviniaMenicucciОценок пока нет
- EMG Analysis of Latissimus Dorsi Erector Spinae and Middle TrapДокумент68 страницEMG Analysis of Latissimus Dorsi Erector Spinae and Middle TrapYuОценок пока нет
- Veterinary AcupunctureДокумент19 страницVeterinary AcupuncturekinezildiОценок пока нет
- Lumbarization of First Sacral VertebraДокумент4 страницыLumbarization of First Sacral VertebraangellisimalОценок пока нет
- 2009.10.09 Legg Calve Perthes Disease 2Документ43 страницы2009.10.09 Legg Calve Perthes Disease 2AnItaОценок пока нет
- TMJ Anatomy and Biomechanics-14Документ67 страницTMJ Anatomy and Biomechanics-14erfan mohammadiОценок пока нет
- Kütük Cubuk Uyum StandartlariДокумент2 страницыKütük Cubuk Uyum StandartlariÖZGÜRОценок пока нет
- Can Trendelenburg'S Sign Be Positive If The Hip Is Normal?Документ5 страницCan Trendelenburg'S Sign Be Positive If The Hip Is Normal?Juniarto PangestuОценок пока нет
- The Use of Locking Plates in Complex Midfoot Fractures: Orthopaedic SurgeryДокумент4 страницыThe Use of Locking Plates in Complex Midfoot Fractures: Orthopaedic Surgeryfebyan yohanesОценок пока нет
- Rachel Scott - Anatomy of Bone Joints Jan 2019Документ7 страницRachel Scott - Anatomy of Bone Joints Jan 2019idyogaОценок пока нет
- ANTRIAN OPERASI SPINE Update 29 MeiДокумент21 страницаANTRIAN OPERASI SPINE Update 29 MeiIbnu ImadudinОценок пока нет
- Jurnal Oa Pak Harto Dan Bu Suriani MWD & Rhytmical StabilisasiДокумент6 страницJurnal Oa Pak Harto Dan Bu Suriani MWD & Rhytmical StabilisasiErwynk EriantoОценок пока нет
- CSEC - Form 4 Human and Social Biology NotesДокумент4 страницыCSEC - Form 4 Human and Social Biology NotesLeon Abel80% (5)
- Back and Spine AnatomyДокумент7 страницBack and Spine AnatomyCarmela Beatriz Suelan100% (1)
- MCQ Ortho 1Документ18 страницMCQ Ortho 1Pradeep Kumar100% (3)
- Frog SkeletonДокумент2 страницыFrog SkeletonJermaine Joyce Arvesu-Lugada0% (2)
- 1.2.2.A SkeletonHuntДокумент3 страницы1.2.2.A SkeletonHuntHBSrocksОценок пока нет
- Extraoral RadiograhyДокумент7 страницExtraoral RadiograhyKanish AggarwalОценок пока нет
- 2.bones of Trunk & LimbsДокумент19 страниц2.bones of Trunk & LimbsRioОценок пока нет
- C 06 Bradford II Faunal AnalysisДокумент14 страницC 06 Bradford II Faunal AnalysisCraig ChartierОценок пока нет
- Upper Extremities Rad PosiДокумент12 страницUpper Extremities Rad PosiJoan GemotoОценок пока нет