Академический Документы
Профессиональный Документы
Культура Документы
A Complex Case of Bipolar Disorder Responding To Combined Drug Therapy
Загружено:
Nimesha WarnakulasooriyaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
A Complex Case of Bipolar Disorder Responding To Combined Drug Therapy
Загружено:
Nimesha WarnakulasooriyaАвторское право:
Доступные форматы
Caseorganicbipolar_Layout 1 30/01/2014 10:12 Page 1
Case notes z Bipolar disorder
A complex case of bipolar disorder
responding to combined drug therapy
Sikandar Kamlana MBBS, DPM, FRCPsych, Dip Psychother
The aetiology of bipolar affective disorder is complex and can involve genetic,
environmental, biochemical and organic factors. Here, Dr Kamlana describes a puzzling
case of bipolar disorder in a patient with brain scan abnormalities, who responded well
to combined treatment with mood stabilisers, an atypical antipsychotic and an SSRI
together with a programme of rehabilitation.
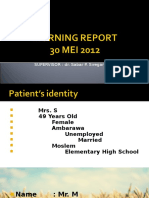
B i p o l a r
affective
disorder is a
drug therapy and a programme of
gradual rehabilitation.
depressed and expressed persecu-
tory delusions. She was also con-
vinced that she had cancer of the
common con- Presentation bowel. She was treated with ECT
dition which, A 47-year-old married woman was and her medications included mir-
among mental admitted to a specialist neuro - tazapine, olanzapine and diazepam.
illnesses, ranks psychiatric unit under Section 3 of She had two further admissions
second only to unipolar depres- the Mental Health Act. She pre- over the next three years, the most
sion as a cause of worldwide dis- sented with irritability, impulsivity, recent being two years prior to her
ability.1 Many patients have a poor disinhibition, distractibility, poor latest admission. At this time, she
outcome, a third suffer chronic concentration and worsening of showed marked behavioural distur-
symptoms and between 13 and 24 social functioning, and had been bance and mood fluctuations for
per cent develop rapid cycling dis- found wandering the streets in her which she was prescribed gaba-
order, in which four or more nightclothes and flagging vehicles. pentin. She repeatedly managed to
episodes occur within a year.2 She had approached strangers for abscond from the psychiatric unit,
Several organic factors have cigarettes and had no sense of was physically aggressive towards
been linked with bipolar disorder, road safety. staff and considered a risk to herself
particularly in patients whose illness She showed pressure of speech and others. She remained unman-
begins in older age (over 65 years). and increased energy and overactiv- ageable despite being on maximum
For example, non-dominant hemi- ity. Her sleep was disturbed and she dosages of amisulpride 500mg twice
sphere cerebrovascular accidents lacked insight. Her mood would daily and olanzapine 20mg daily as
can predispose to the development quickly change to feeling very well as gabapentin 600mg three
of mania, especially if there is either depressed with suicidal thoughts, times daily. Investigations at the time
a previous history of depression or and these changes could occur sev- included CT and MRI brain scans
family history of affective disorder. eral times a day. She was given a and an EEG, which were all
Other brain disorders (or systemic diagnosis of bipolar disorder. reported to be normal.
disease with cerebral involvement) There was no family history of The only other medical illness
can also present with mania or psychiatric illness. Her past psychi- of note in our patient was type 2
severe (often psychotic) depres- atric history included detoxification diabetes, which was stabilised on
sion. Accompanying the affective from lorazepam 17 years earlier. metformin 500mg three times daily
syndrome, there is usually evidence About 10 years after this, she con- and simvastatin 40mg at night.
of disorientation and other features sulted a GP for anxiety and depres- At her latest admission, a neuro-
of confusion along with visual hal- sion and another two years later psychiatric assessment showed sig-
lucinations, all of which are less (five years prior to the latest admis- nificant deterioration from her
common in primary bipolar illness. sion), she took an overdose and was estimated good average premorbid
Here, I present a complex case admitted to the Affective Disorder level of cognitive function across all
of bipolar affective disorder, with Unit under Section 3 and was diag- areas, which was particularly marked
a possible organic component, nosed with psychotic depression. At in relation to working memory with
which responded well to combined that time, she was severely significant impairment being pres-
26 Progress in Neurology and Psychiatry January/February 2014 www.progressnp.com
Caseorganicbipolar_Layout 1 30/01/2014 10:12 Page 2
Bipolar disorder z Case notes
ent in relation to new verbal learn- • Ensure compliance with present patient’s mood disturbances pre-
ing. An MRI brain scan was also per- drug therapy using the NOMAD dated the abnormal scan findings,
formed, which showed global monitored dosage system. and therefore organic bipolar dis-
atrophy. There was no marked atro- • A support, time and recover y order could not be verified.
phy of the caudate nuclei and no (STR) worker to visit the patient This case emphasises the diffi-
positive features to suggest a fronto- once a week at home culty distinguishing between
temporal predominance to the atro- • Follow-up at the outpatient clinic organic and non-organic psychi-
phy. These signs were considered to with a psychiatrist to monitor atric illness. Organic disorders
be possibly indicative of early progress and medication review often present with hallucinations
Alzheimer’s disease. The neuropsy- • Regular home support from a and disorientation; however, others
chiatric and scan results raised the community psychiatric nurse have symptomatology more typical
suspicion of an underlying organic • Social worker support, including of non-organic psychiatric illness.
component to the bipolar disorder a seven-day follow-up In our case, in addition to structural
but this could not be verified due to • Crisis team follow-up, initially brain changes, there were probably
her initial symptoms predating the once a month post-discharge also genetic, functional and bio-
scan abnormalities. • Telephone counselling once a chemical factors involved in the
The patient’s medications were month post-discharge aetiology of the bipolar disorder.
titrated to citalopram 20mg in the • Follow-up from her GP regarding Other examples of diagnostic diffi-
morning, gabapentin 400mg three physical healthcare. culty arising between organic and
times daily, quetiapine 300mg twice The patient was discharged suc- non-organic psychiatric disorders
daily and valproate semisodium cessfully and continues to make have been described by Lishman.4
1000mg twice daily. She remained good symptomatic recovery three In our case, despite the patient
an inpatient in the neuropsychiatric years later. Her cognitive function showing a history of resistance to
unit and gradually began to make has remained static. She has man- treatment, combined treatment
good symptomatic recovery over aged to gain employment in a pri- with mood stabilisers (gabapentin
the following 9-14 months, as meas- mar y school as a lunchtime and valproate semisodium), an
ured using the Health of the Nation assistant and she also does volun- atypical antipsychotic (quetiapine)
Outcome Scale (HoNOS). She was tary work at the local cattery. She and an SSRI (citalopram), together
compliant with her medications continues to remain well and com- with a programme of gradual reha-
and Section 17 leave. Her progress ply with her medications. bilitation following her most recent
was reviewed regularly in the multi- admission was surprisingly effective.
disciplinary ward rounds. She devel- Discussion According to the 2006 NICE
oped a strong therapeutic This report describes a complex guideline,5 key maintenance treat-
relationship with staff, and showed case of bipolar disorder, which ment of bipolar disorder is either a
no manifest symptoms of psychotic appeared to have an organic com- mood stabiliser or an atypical
depression or mania. Her insight ponent. According to ICD-10, the antipsychotic, which is started as
also improved. criterion for inclusion in the cate- monotherapy in order to achieve
This gradual process of rehabil- gory of organic mood (affective) complete symptom control of the
itation was carefully managed with disorders is the presumed direct index episode as well as sustained
the co-operation of her husband. causation by a cerebral or other remission and to prevent relapse. If
She began to resume a meaningful physical disorder whose presence monotherapy fails, there is evidence
life within and beyond the unit must either be demonstrated inde- to support combination therapy
and appeared to be enjoying her pendently, eg by means of appropri- with an atypical antipsychotic plus a
family and social life. However, she ate physical and laborator y mood stabiliser.6 The Consensus
expressed ambivalent feelings investigations, or assumed on the Group of the British Association for
towards her husband, who visited basis of an adequate history.3 The Psychopharma cology (BAP) 7
her at weekends in hospital. They mood disorder must follow on emphasised that in difficult to treat
had a nine-year-old son and her from the presumed organic factor cases, combination therapy is usually
husband also had a child from and be judged not to represent an necessary. There is also evidence to
another relationship. emotional response to the patient’s suggest that gabapentin is effective
A pre-discharge meeting was knowledge of having, or having the in refractory mood disorders.8
planned and the following after- symptoms of, a concurrent brain Regular monitoring of patients
care plan was implemented: disorder. In this case, however, the on combination therapy for bipo-
www.progressnp.com Progress in Neurology and Psychiatry January/February 2014 27
Caseorganicbipolar_Layout 1 30/01/2014 10:12 Page 3
Case notes z Bipolar disorder
lar disorder is important, includ- Declaration of interests Psychiatry 2000;48:445-7.
3. World Health Organization. ICD-10: Inter-
ing weight, waist, glucose, lipid, None declared. national Classification of Diseases, 10th Edn.
prolactin and blood pressure 4. Lishman WA. Neuropsychiatry. A delicate
measurements, in accordance with Dr Kamlana is Lead Consultant balance. Psychosomatics 1992;33:4-9.
5. NICE Clinical Guidelines No. 38. The
the NICE guidelines, and this was Psychiatrist/Psychotherapist, Medical Management of Bipolar Disorder in Adults,
the case with our patient. It is also Director and Honorary Clinical Children and Adolescents in Primary and
Secondary Care. NICE, July 2006.
important to remember that the Lecturer, Billingham Grange 6. Vieta E Suppes T, Eggens I, et al. Efficacy and
management of bipolar disorder is Independent Hospital, Stockton on Tees safety of quetiapine in combination with lithium
a long-term commitment between or divalproex for maintenance of patients with
bipolar I disorder. J Affect Dis 2008:109:251-63.
the patient, the GP, the psychiatrist References 7. Goodwin GM. Evidence-based guidelines for
and the patient’s family. Such col- 1. Murray CG, Lopez AD. Global mortality, dis- treating bipolar disorder: recommendations from
ability and the contribution of risk factors. the BAP. J Psychopharmacol 2003;17:149-73.
laborative working was of para-
Lancet 1997;349:1436-42. 8. Schaffer CB, Schaffer LC. Gabapentin in the
mount importance in the recovery 2. Angst J. Sellaro R. Historical perspectives treatment of bipolar disorder. Am J Psychiatry
of this refractory patient. and natural history of bipolar disorder. Biol 1997;154:291-2.
28 Progress in Neurology and Psychiatry January/February 2014 www.progressnp.com
Вам также может понравиться
- 114-116 SavithaДокумент3 страницы114-116 Savithamavriska.chairunnisaОценок пока нет
- Psychotropic Drug WithdrawalДокумент13 страницPsychotropic Drug WithdrawalViviani ReisОценок пока нет
- Archneur 23 3 001Документ8 страницArchneur 23 3 001Alo DeoОценок пока нет
- Toj 16 0001Документ3 страницыToj 16 0001novywardanaОценок пока нет
- Psychopharmacologic Agents Lec 2016Документ23 страницыPsychopharmacologic Agents Lec 2016roseanne_erikaОценок пока нет
- The Presentation, Recognition and Management of Bipolar Depression in Primary CareДокумент9 страницThe Presentation, Recognition and Management of Bipolar Depression in Primary CareJuan PerezОценок пока нет
- Recurrent Psychotic Episodes With A Near - Monthly CycleДокумент4 страницыRecurrent Psychotic Episodes With A Near - Monthly CycleNajia ChoudhuryОценок пока нет
- CASE Study SampleДокумент6 страницCASE Study SampleMary Shane Aragon MoraldeОценок пока нет
- Promazine in The Treatment of Delusional ParasitosisДокумент2 страницыPromazine in The Treatment of Delusional ParasitosisVictorson Leonardo ZegaОценок пока нет
- GROUP F Compilation PsychiaFinalДокумент20 страницGROUP F Compilation PsychiaFinalFrancis Raphael PitogoОценок пока нет
- Antipsycotic DrugДокумент21 страницаAntipsycotic DrugShashank SatheОценок пока нет
- Running Head: Mental Health Comprehensive Case Study 1Документ9 страницRunning Head: Mental Health Comprehensive Case Study 1api-741216417Оценок пока нет
- Abram Hoffer - Prousky - Niacinamide's Potent Role in Alleviating Anxiety With Its Benzodiazepine-Like Properties - TextДокумент8 страницAbram Hoffer - Prousky - Niacinamide's Potent Role in Alleviating Anxiety With Its Benzodiazepine-Like Properties - TextEbook PDF100% (1)
- Treatment Interictal PsychosisДокумент13 страницTreatment Interictal PsychosisJuan IgnacioОценок пока нет
- 17 Case Report 1Документ5 страниц17 Case Report 1neerajОценок пока нет
- Case StudyДокумент13 страницCase Studyapi-599558477Оценок пока нет
- Case Study Final DraftДокумент15 страницCase Study Final Draftapi-608049224Оценок пока нет
- 10 Page Case StudyДокумент11 страниц10 Page Case Studyapi-663754509Оценок пока нет
- Aripiprazole For Acute Mania in An Elderly Person: Balaji Bharadwaj, Shivanand Kattimani, Anuriddha MukherjeeДокумент4 страницыAripiprazole For Acute Mania in An Elderly Person: Balaji Bharadwaj, Shivanand Kattimani, Anuriddha MukherjeeMay GaamОценок пока нет
- Phobic Postural Vertigo: A Cognitive-Behavior ApproachДокумент2 страницыPhobic Postural Vertigo: A Cognitive-Behavior ApproachVa RissaОценок пока нет
- Psychiatric Mental Health Comprehensive Case StudyДокумент12 страницPsychiatric Mental Health Comprehensive Case Studyapi-739571122Оценок пока нет
- Tn. S Usia 35 Tahun Dengan Skizofrenia Episodik Berulang, Episode Kini AkutДокумент5 страницTn. S Usia 35 Tahun Dengan Skizofrenia Episodik Berulang, Episode Kini AkutHumaerah UumОценок пока нет
- Delirium and DementiaДокумент12 страницDelirium and DementiaSОценок пока нет
- A Rare Case of Early Onset Bipolar Affective Disorder During LockdownДокумент1 страницаA Rare Case of Early Onset Bipolar Affective Disorder During LockdownRupinder GillОценок пока нет
- Steroid-Induced PsychosisДокумент2 страницыSteroid-Induced Psychosisanisha batraОценок пока нет
- Manejo Depresion 1Документ10 страницManejo Depresion 1Luis HaroОценок пока нет
- Park, 2019 - NEJM - DepressionДокумент10 страницPark, 2019 - NEJM - DepressionFabian WelchОценок пока нет
- Oral Health and ODDДокумент4 страницыOral Health and ODDTiffany HanОценок пока нет
- Administrator, Journal Manager, 368-1206-1-CEДокумент3 страницыAdministrator, Journal Manager, 368-1206-1-CESameer KhanОценок пока нет
- Jamapsychiatry Brennan 2018 CG 180002Документ2 страницыJamapsychiatry Brennan 2018 CG 180002ZaiaОценок пока нет
- Psychosis and Seizure Disorder: Challenges in Diagnosis and TreatmentДокумент7 страницPsychosis and Seizure Disorder: Challenges in Diagnosis and TreatmentgreenanubisОценок пока нет
- A Rare Case of Early-Onset Bipolar Affective Disorder During LockdownДокумент1 страницаA Rare Case of Early-Onset Bipolar Affective Disorder During LockdownRupinder GillОценок пока нет
- Case Presentation 2Документ32 страницыCase Presentation 2TraceОценок пока нет
- MH Case StudyДокумент11 страницMH Case Studyapi-455565203Оценок пока нет
- Gardner 2011 PDFДокумент6 страницGardner 2011 PDFJarrod GottОценок пока нет
- Acute Neuropsychiatric Disorders in Adolecenst and Young Adults With Down Syndrome: Japanese Case ReportsДокумент7 страницAcute Neuropsychiatric Disorders in Adolecenst and Young Adults With Down Syndrome: Japanese Case ReportsPar DoОценок пока нет
- W3 Bipolar Disorder. Therapies. T2 2022-23Документ41 страницаW3 Bipolar Disorder. Therapies. T2 2022-23Nayanaa VarsaaleОценок пока нет
- Family Role On Schizoaffective Mixed Type Patient Treatment: Case ReportДокумент4 страницыFamily Role On Schizoaffective Mixed Type Patient Treatment: Case ReportAshОценок пока нет
- Case Report On Bipolar Affective Disorder: Mania With Psychotic SymptomsДокумент3 страницыCase Report On Bipolar Affective Disorder: Mania With Psychotic SymptomsmusdalifahОценок пока нет
- Case Study Mental HealthДокумент13 страницCase Study Mental Healthapi-738695053Оценок пока нет
- Case Study Project - Melissa MershimerДокумент15 страницCase Study Project - Melissa Mershimerapi-740498688Оценок пока нет
- Antidepresants Et Al2023Документ40 страницAntidepresants Et Al2023ABAJONG EMMANUELОценок пока нет
- Treatment Modules and Therapeutic Approaches For Inhalant Abuse A Case ReportДокумент5 страницTreatment Modules and Therapeutic Approaches For Inhalant Abuse A Case ReportSejahtera SurbaktiОценок пока нет
- Depression With Atypical Features: Diagnostic Validity, Prevalence, and TreatmentДокумент6 страницDepression With Atypical Features: Diagnostic Validity, Prevalence, and TreatmentIgnacioJoséCalderónPérezОценок пока нет
- Case Study For Mental Health 1Документ12 страницCase Study For Mental Health 1api-737888849Оценок пока нет
- Depression Treated With Imipramine and Ect: The Decarolis Study ReconsideredДокумент4 страницыDepression Treated With Imipramine and Ect: The Decarolis Study ReconsideredPsiholog Monica StănescuОценок пока нет
- Practicing Exorcism in Schizophrenia PDFДокумент3 страницыPracticing Exorcism in Schizophrenia PDFjackОценок пока нет
- Pseudoseizures and Dissociative DisordersДокумент5 страницPseudoseizures and Dissociative DisordersLaura AndreiОценок пока нет
- Meadows Paige Case StudyДокумент16 страницMeadows Paige Case Studyapi-607727110Оценок пока нет
- Epilepsia y PsicosisДокумент9 страницEpilepsia y PsicosisManuel Alejandro Pinzon OlmosОценок пока нет
- DocumentДокумент11 страницDocumentFairuds MamalintaОценок пока нет
- Case Report-Traducción LauraДокумент4 страницыCase Report-Traducción LauraPablo GuzmánОценок пока нет
- Mental HealthДокумент12 страницMental Healthapi-662585161Оценок пока нет
- Case Report On Bipolar Affective Disorder: Mania With Psychotic SymptomsДокумент2 страницыCase Report On Bipolar Affective Disorder: Mania With Psychotic SymptomskslhfwoiebvОценок пока нет
- Schizophrenia Case StudyДокумент3 страницыSchizophrenia Case StudyKumar Suryavanshi100% (1)
- 10 Page Mental HealthДокумент13 страниц10 Page Mental Healthapi-736365670Оценок пока нет
- BipolarДокумент27 страницBipolarSham Bundoc RosalОценок пока нет
- Obsessive-Compulsive Disorder in The ElderlyДокумент6 страницObsessive-Compulsive Disorder in The ElderlyZafira Ananda RaishaОценок пока нет
- A Case of Cycloid Psychotic Disorder: M C F, T S - F, B SДокумент2 страницыA Case of Cycloid Psychotic Disorder: M C F, T S - F, B Syeremias setyawanОценок пока нет
- Scl-90-R Symptom Checklist-90-Revised Interpretive Report: Leonard R. Derogatis, PHDДокумент5 страницScl-90-R Symptom Checklist-90-Revised Interpretive Report: Leonard R. Derogatis, PHDMuhammad Dadan KurniawanОценок пока нет
- Psychiatry Dr. Osama Mahmoud PDFДокумент59 страницPsychiatry Dr. Osama Mahmoud PDFRaouf Ra'fat SolimanОценок пока нет
- CasestudyДокумент12 страницCasestudyapi-354053517Оценок пока нет
- You Probably Have AdhdДокумент3 страницыYou Probably Have AdhdNur Amaleena GafarОценок пока нет
- 17Документ35 страниц17Gwen PhamОценок пока нет
- Mental HealthДокумент3 страницыMental HealthMary Jean Aguelo100% (1)
- DSM 5 and Child Psychiatric DisordersДокумент5 страницDSM 5 and Child Psychiatric Disordersfotinimavr94Оценок пока нет
- Gaf CamilleДокумент5 страницGaf CamilleAbby FernandezОценок пока нет
- Synthesis of ASD, ASR, and CSRДокумент8 страницSynthesis of ASD, ASR, and CSRKusnanto Penasehat Kpb RyusakiОценок пока нет
- Psychopathology NotesДокумент29 страницPsychopathology Notesmonster40lbsОценок пока нет
- Anti Maniac DrugsДокумент32 страницыAnti Maniac DrugsMohamad SamirОценок пока нет
- Mini Mental Status ExaminationДокумент13 страницMini Mental Status ExaminationAndrew Sabastian Geraldyno Paago100% (1)
- Autism 101 Webinar April 5, 2012Документ28 страницAutism 101 Webinar April 5, 2012The Autism NOW Center100% (1)
- Parental Substance AbuseДокумент8 страницParental Substance Abuseapi-458338612Оценок пока нет
- Excoriation (Skin Picking Disorder or Dermatillomania) : Diagnostic Criteria According To DSM VДокумент5 страницExcoriation (Skin Picking Disorder or Dermatillomania) : Diagnostic Criteria According To DSM VZarghoona inayatОценок пока нет
- First Rank Symptoms of SchizophreniaДокумент65 страницFirst Rank Symptoms of Schizophreniadrkadiyala2Оценок пока нет
- Acute Stress Disorder 1Документ22 страницыAcute Stress Disorder 1Seiska MegaОценок пока нет
- Body Image 2 1Документ9 страницBody Image 2 1api-460023508Оценок пока нет
- 201103check BipolarДокумент29 страниц201103check BipolarRumana AliОценок пока нет
- Needs Assessment Questionnaire For CaregiversДокумент4 страницыNeeds Assessment Questionnaire For CaregiversJasleen KaurОценок пока нет
- GP Mental State Exam OSCEДокумент2 страницыGP Mental State Exam OSCEJagdishVankarОценок пока нет
- CadabamsДокумент7 страницCadabamsLavanyaLNarayanОценок пока нет
- PMHNP Case Study - EditedДокумент7 страницPMHNP Case Study - EditedSoumyadeep BoseОценок пока нет
- Kring Abnormal Psychology Chapter 6 Anxiety NotesДокумент16 страницKring Abnormal Psychology Chapter 6 Anxiety NotesAnn Ross Fernandez50% (2)
- Postpartum Depression: Clinical PracticeДокумент11 страницPostpartum Depression: Clinical PracticeCasey Daisiu100% (1)
- ADHD Rating Scale-IV Home VersionДокумент2 страницыADHD Rating Scale-IV Home Versionrimpa29Оценок пока нет
- SUPERVISOR: Dr. Sabar P. Siregar SP - KJДокумент36 страницSUPERVISOR: Dr. Sabar P. Siregar SP - KJPuspita PrihatiniОценок пока нет
- Cns 771 Final Exam Suicide AssessmentДокумент4 страницыCns 771 Final Exam Suicide Assessmentapi-301673059Оценок пока нет
- Schizophrenia Final PaperДокумент6 страницSchizophrenia Final Paperchad5844Оценок пока нет
- Somatic Symptom Disorders and Personality DisordersДокумент15 страницSomatic Symptom Disorders and Personality Disordersapi-287575009Оценок пока нет