Академический Документы
Профессиональный Документы
Культура Документы
1 PB PDF
Загружено:
nico0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров4 страницыОригинальное название
56630-96898-1-PB.pdf
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
27 просмотров4 страницы1 PB PDF
Загружено:
nicoАвторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 4
CLINICAL FINDINGS AND MANAGEMENT OF CHRONIC
BLEPHARITIS IN A 25-YEAR OLD FEMALE -A CASE REPORT
BY
*OSAIYUWU, A. B. AND EBEIGBE, J. A.
DEPARTMENT OF OPTOMETRY, FACULTY OF LIFE SCIENCES,
UNIVERSITY OF BENIN, BENIN CITY, NIGERIA.
EMAIL: bosaiyuwu@yahoo.com
*Corresponding author
ABSTRACT
Blepharitis is an inflammation of the eyelid margins which sometimes leads to secondary changes in the
conjunctiva and cornea. Symptoms of blepharitis tend to be longstanding, thus, blepharitis is more of a
chronic condition than being acute and both eyes are usually affected, however, the symptoms can easily
be eased. Once symptoms have eased, daily 'eyelid hygiene' can usually keep the symptoms to a minimum.
Vision is rarely affected. This case report reviewed the management of blepharitis in a 25-year old girl the
clinical findings and treatment options were also discussed.
KEYWORDS: Blepharitis, Madarosis, Conjunctivitis, Keratitis, Staphylococcus auerus.
Received 03/03/2010 Accepted 04/06/2010
INTRODUCTION (OTC) drugs of which she could only remember
Historically, blepharitis has been divided into chloramphenicol eye drop as one of the drugs
anterior forms (affecting the anterior lid margin applied. The patient had never had an eye
and eyelashes) and posterior forms (affecting the examination prior to her visit to our clinic. The
meibomian glands) 1,2. Blepharitis is one of the patient also complained that the symptoms often
most common eyelid disorders often associated 'come and go' and that occasionally the symptoms
with tear film disruption and accompanying were so very severe and there were also long
symptoms of which the mainstay of management is periods without any symptoms. The patient's
meticulous lid hygiene not medicinal3. It is more medical and family history was negative.
common in young females4. One of the most
accompanying symptoms is madarosis of which CLINICALFINDINGS
infection due to Staphylococcus aureus is one of Her unaided visual acuity at distance was OD
the causes. Long-standing staphylococcal 6/6, OS 6/6 and OU 6/5+, while her unaided visual
infection is associated with madarosis, whitening acuity at near (0.4m) for OD and OS was N5.
(poliosis) and misdirection (trichiasis) of Colour vision testing with pseudoisochromatic
eyelashes5 . Blepharitis is characterized by plates was normal OU.
inflammation of the eyelid margins. It may cause Pupils were equally round and reactive to light,
redness of the eyes, itching and irritation of the
eyelids in one or both eyes. Its appearance is often no afferent pupil defect was noted OU.
confused with conjunctivitis and due to its Confrontation fields were full to finger count OU.
recurring nature; it is the most common cause of Extraocular muscles were unrestricted in all gazes
'recurrent conjunctivitis' in older people. It is also and the alternate cover test demonstrated both
often mistaken for 'dry eye' by patients due to the orthophoria at distance and near.
gritty sensation that may occur. Both eyes looked generally unhealthy in
appearance; the eyelids were inflamed and sore
CASE REPORT with the eyes having some discharge, irregularity
A 25-year old female patient, IU presented to and ulceration of the lid margins and madarosis and
our Optometry Clinic on 30 April 2008 with a
there was improper lid closure when the patient
history of irritation in both eyes since the past
eighteen months. She reported that the problem was instructed to close the eyes.
started mildly with occasional discharge and Slit lamp examination revealed the following:
itching, but progressed to a more copious Lashes: loss of lashes (madarosis), scanty and
discharge, itching, redness and almost a complete misdirection of lashes (trichiasis) and crusting of
loss of eyelashes (madarosis).She also reported lashes.
that she applied a couple of over-the-counter The meibomian orifices: crusting and plugging.
JNOA - VOL 16, 2010 26
PDF created with pdfFactory Pro trial version www.pdffactory.com
The conjunctiva: papillary injection. - The few misdirected lashes were epilated
Corneal findings: punctate epithelial erosions, after instillation of two drops of 0.05%
marginal infiltrates, pannus and phlyctenule novesine.
formation. - Tab. Vit. C, 2 tabs tds for 2weeks was also
prescribed.
Direct Ophthalmoscopy: no abnormality; both
crystalline lenses were transparent, there were The patient was again reminded to be drug
normal optic nerves with a cup-to-disc ratio of compliant and to return in 2 weeks time for follow
0.3/0.3 OU, neuroretinal rims were healthy, retinal up.
vessels were normal with an arterio-venous ratio of
2/3 OU and both eyes presented with normal FOLLOW UP# 2
macular findings. The patient returned for follow up on 19 May
2008. Her visual acuities remained the same and
Diagnosis: Chronic blepharitis she reported that she had been drug compliant. The
IU was counseled and instructed to go for a swab general appearance of the eyes looked improved
test and was scheduled to be seen on 5 May 2008. when compared to her first visit.
Slit lamp examination was conducted on her
FOLLOW UP#1 and findings were as listed;
IU returned on 5 May 2008 to review the swab Absence of misdirected lashes
result. The swab result revealed the causative There was reduced crusting of the lashes
organism as Staphylococcus aureus. Her visual There was a marked reduction of crusting and
acuity remained stable with unaided acuities of 6/6 plugging on the meibomian orifices
OD and OS and 6/5+ OU. Schirmer test was carried There was almost a total absence of
out on the patient and the result was quite conjunctival papillary injection.
favourable. The cornea still presented with some punctate
IU was counseled on the treatment regimen epithelial erosions, a few marginal infiltrates and
that would be given and that a strict compliance the pannus was resolving quietly as well as the
was all that would be needed for an effective phlyctenules.
treatment. She was also made to realize that the Direct op hthalmoscop y revealed no
treatment may span through months and thus she abnormality.
has to learn to be patient. She was instructed to The patient was encouraged to keep up with the
carry out the treatment thus: compliance as the prognosis was good. Her
Firstly, the application of heat to warm the medications were reviewed and she was advised
eyelid gland secretions and to promote thus:
evacuation and cleansing of the secretory
passages. Take: Cap. Doxycycline 100mg for another 2
Secondly, the eyelid margin should be washed weeks
mechanically to remove adherent materials Gutt Blephamide 1 drop bid for 2 weeks
such as collarettes and crusts and to clean the Oint. Erythromycin (0.5%) qid for 2 weeks
gland orifices, water often is used. Gentle Tab. Vit.C 2 tabs tds for 2 weeks
mechanical scrubbing of the eyelid margin is
all that is needed, vigorous scrubbing is not Patient was counseled to continue cleaning the
necessary and may be harmful. lids as instructed and generally maintain a very
Thirdly, the medications should be applied to good hygiene. IU was told to report again to the
the eyelid margin after it has been soaked and clinic in another 2 weeks time for follow up.
scrubbed.
FOLLOW UP# 3
The patient was placed on IU returned for follow up on 2 June 2008. Her
- Cap. Doxycycline 200mg stat,then 100mg for vision was unchanged and the eyes looked quite
2weeks. healthy. The patient said that she was happy with
- Ointment Erythromycin (0.5%), 0.5inch the drastic improvement of her eyes. Slit lamp
ribbon to be applied to lid margin qid for 2 examination revealed absence of misdirected
weeks. lashes, a few crusts on the lashes, a few crusts and
- Sulfacetamide sodium and prednisolone absence of plugging on the meibomian orifices,
acetate (Blephamide; 10% sulfacetamide; absence of conjunctival papillary injection, pannus
0.2% prednisolone), 1 drop qid for 2 weeks. and phlyctenules had completely resolved but the
27 JNOA - VOL 16, 2010
PDF created with pdfFactory Pro trial version www.pdffactory.com
cornea still presented with a few punctate epithelial patients with chronic blepharitis include
erosions and marginal infiltrates. Staphylococcal epidermidis, Propionibacterium
The patient was commended for not only being acnes , corynebacteria and Staphylococcus
drug compliant but also in maintaining good lid aureus.6,7. A staphylococcal infection normally
hygiene. Her medications were reviewed thus: presents predominantly in young women to
middle-aged women4. Collarettes or cuffs of fibrin
Take: Cap.Doxycycline 100mg for another 2 (matted, hard scales) extend from the base of and
weeks along lashes as a sleeve. Eyelid ulcerations are fine
Gutt Blephamide 1 drop daily for 2 weeks at the base of lashes. There is also the absence of
Oint. Erythromycin (0.5%) tds for 2 weeks eyelashes in staphylococcal infection; this
Tab. Vit. C 2 tabs tds for 2 weeks.
condition is very rare in seborrheic infection.
The management of blepharitis is a process
The patient was told to come for follow up in
which must be carried out for prolonged periods of
another 2 weeks time when we hoped the eyes
time, implying that even when symptoms have
would be fit enough to undergo the test for
subsided, the treatment should still continue but at
refraction.
reduced doses. Prognosis is usually good when the
FOLLOW UP# 4 patient is compliant to the instructions given as per
IU returned to the clinic on 16 June 2008. Her maintenance of proper lid hygiene3. The patient in
vision was unchanged and her eyes were looking this report was very compliant and it reflected in
really healthy. Slit lamp examination revealed no the prognosis report.
abnormality and there was also no abnormality Conjunctivitis and keratitis can result as a
detected on ophthalmoscopy. complication of blepharitis and requires additional
IU was so very grateful but she wanted to know treatment besides eyelid margin therapy.
if she would grow the lashes again. She was Antibiotic-corticosteroid solution can greatly
reassured that the lashes would re-grow but that it reduce inflammation and symptoms of
was not going to be spontaneous. We also conjunctivitis. Corneal infiltrates can be treated
counseled IU about referring her to an with antibiotic-corticosteroid drops1. Small
ophthalmologist to carry out lid repairs, but she marginal corneal ulcers can be treated empirically,
was not so enthusiastic about it and she rejected the but larger paracentral ulcers should be scraped and
idea of the referral. We also made her to realize that specimens sent for diagnostic slides and for culture
the treatment had not ended meaning that she and sensitivity testing4.
should still continue with the lid hygiene Overall the prognosis for patients with
religiously. We reviewed her medication by blepharitis is good to excellent. Patients with
placing her on the doxycycline, 100mg daily for unilateral or very asymmetric blepharitis may have
the next 2 weeks; she was to stop instilling the sebaceous cell carcinoma.An oculoplastics consult
blephamide but to continue with the ointment may be required for a lid biopsy4,7.
erythromycin to be applied twice a day for another This case demonstrates the role of patient
2 weeks. Her next follow up was in a month's time, history, clinical observation and swab study in the
16 July 2008. diagnosis of blepharitis. In most cases, the
diagnosis can confidently be made without a swab
The retinoscopic findings were: test, however, the information derived from the
OD +0.75 / -0.50 × 180 swab test is critical as knowledge of the causal
OS +0.75 / -0.25 × 180 organism would aid the optometrist into a pool of
medications that such organism(s) is (are)
The subjective refraction findings were same susceptible to. Although prognosis for patients
as retinoscopic findings. The patient was given with blepharitis is generally favourable, patients
another appointment to check her progress and should continue to self-monitor their vision even
possibly prescribe glasses, but she never returned. after resolution.
DISCUSSION
The most common organisms isolated from
JNOA - VOL 16, 2010 28
PDF created with pdfFactory Pro trial version www.pdffactory.com
REFERENCES
1. Jackson, B. W. (2008): Blepharitis: current Textbook of Ophthalmology. 1st Edn. Jaypee
strategies for diagnosis and management. Medical Publishers, pp. 67-9.
Can. J. Ophthalmol, 43:170-9. 5. Sachdeva, S. and Prasher, P. (2008):
2. Riordan-Eva, P. and Whitcher, J. P. (2004): Madarosis: A dermatological marker. India J.
Va u g h a n a n d A s b u r y ' s G e n e r a l Dermatol. Venereol. Leprol, 74:74-6.
Ophthalmology.16th Edn. McGraw Hill 6. Dougherty, J. M. and McCulley, J. P. (1984):
Company, Lange, pp. 19-26. Comparative bacteriology of chronic
3. Ron, M. and Randall, T. (2004): Blepharitis. blepharitis Bri. J. Ophthalmol, 68:524-8.
Clin. Refr. Optom, 15 (4):110-2. 7. McCulley, J. P. and Dougherty, J. M. (1986):
4. Sunita, A., Athiya, A., David, J. A., Lucio, B., Bacterial aspects of chronic blepharitis.
Jorge, L. A., Suresh, K. P. and Amar, A. (2002): Trans. Ophthalmol. Soc. UK, 105 (3):314-8.
29 JNOA - VOL 16, 2010
PDF created with pdfFactory Pro trial version www.pdffactory.com
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Malaysian Triage CategoryДокумент3 страницыMalaysian Triage CategoryHafiz Hamidi71% (7)
- 10 Introductory Questions Therapists Commonly Ask PDFДокумент4 страницы10 Introductory Questions Therapists Commonly Ask PDFsamir shah100% (1)
- Lion Air Eticket Itinerary / Receipt: Hutagaol/Nicolas Trivolta MRДокумент3 страницыLion Air Eticket Itinerary / Receipt: Hutagaol/Nicolas Trivolta MRnicoОценок пока нет
- Blepharitis 2934 2934 PDFДокумент10 страницBlepharitis 2934 2934 PDFnicoОценок пока нет
- Nicolas Trivolta Hutagaol-Pku-Mdvzcl-Kno-Flight - Originating PDFДокумент2 страницыNicolas Trivolta Hutagaol-Pku-Mdvzcl-Kno-Flight - Originating PDFnicoОценок пока нет
- Status OftalmikusДокумент2 страницыStatus OftalmikusnicoОценок пока нет
- Itchy Eyes Case Study: Eye Series - 17Документ2 страницыItchy Eyes Case Study: Eye Series - 17nicoОценок пока нет
- What Is The Best Treatment Approach For Severe Blepharitis?: Key Words: Blepharitis ClinicalДокумент3 страницыWhat Is The Best Treatment Approach For Severe Blepharitis?: Key Words: Blepharitis ClinicalnicoОценок пока нет
- Short Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSДокумент29 страницShort Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSErkoОценок пока нет
- A Ryan Case StudyДокумент6 страницA Ryan Case StudycryziaОценок пока нет
- HBN 07-01 FinalДокумент34 страницыHBN 07-01 FinalYahya Hammoudeh100% (1)
- Play TherapyДокумент4 страницыPlay TherapyAnita Hani ChristinaОценок пока нет
- HealthCare Industry AnalysisДокумент20 страницHealthCare Industry Analysisbinzidd00767% (3)
- Greening The Roadmap of The Philippine Pulp and Paper IndustryДокумент14 страницGreening The Roadmap of The Philippine Pulp and Paper IndustryJade LimbagoОценок пока нет
- PHD Thesis On Medical Tourism in IndiaДокумент4 страницыPHD Thesis On Medical Tourism in IndiaBuyingCollegePapersPittsburgh100% (1)
- TX Plan Goals Objectives 2Документ15 страницTX Plan Goals Objectives 2mysteryvan1981Оценок пока нет
- Dentine HypersensitivityДокумент32 страницыDentine Hypersensitivityitdoc100% (1)
- Ii 2015 1Документ266 страницIi 2015 1tuni santeОценок пока нет
- Batiquin v. Court of AppealsДокумент9 страницBatiquin v. Court of AppealsEnzo PerezОценок пока нет
- Roots 1 - 2015Документ60 страницRoots 1 - 2015Ovidiu100% (1)
- Pregnancy: Signs/Symptoms and Common Health ConcernsДокумент5 страницPregnancy: Signs/Symptoms and Common Health ConcernsTracy50% (2)
- Oncology Nursing: Detection and Prevention of CancerДокумент14 страницOncology Nursing: Detection and Prevention of CancerEdwin Delos Reyes AbuОценок пока нет
- Adhd ManualДокумент72 страницыAdhd ManualJuwita Pratiwi100% (1)
- Metabolic Encephalopathies and Delirium: Panayiotis N. Varelas, MD, PHDДокумент34 страницыMetabolic Encephalopathies and Delirium: Panayiotis N. Varelas, MD, PHDjorge_suoОценок пока нет
- TerminologyДокумент11 страницTerminologyMustafa SaßerОценок пока нет
- OmphaloceleДокумент3 страницыOmphaloceleAnonymous uI8yHXobYОценок пока нет
- Amlodipine CPДокумент2 страницыAmlodipine CPRose EchevarriaОценок пока нет
- 7x Premature EjaculationДокумент8 страниц7x Premature EjaculationTer AbОценок пока нет
- ModifiersДокумент8 страницModifiersKarna Palanivelu100% (6)
- Guidelines For Management of Endometrial CarcinomaДокумент41 страницаGuidelines For Management of Endometrial CarcinomaVeenaОценок пока нет
- Recent Patents On Biotechnology 2009, 3, 166-174Документ10 страницRecent Patents On Biotechnology 2009, 3, 166-174TehMarianОценок пока нет
- Major Catalogue CompletДокумент237 страницMajor Catalogue Complethenrycosta2009Оценок пока нет
- Surgical SkillsДокумент47 страницSurgical SkillsSamah SuhailОценок пока нет
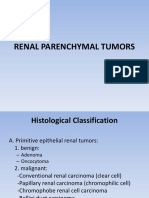
- Renal Parenchymal TumorsДокумент45 страницRenal Parenchymal TumorsDaniel100% (1)
- Lab 1 - Asepsis and Infection Control QuestionsДокумент3 страницыLab 1 - Asepsis and Infection Control QuestionsmlomiguenОценок пока нет
- 14 Exercises For Shoulder Pain Relief & Rehab (Printable PDFДокумент19 страниц14 Exercises For Shoulder Pain Relief & Rehab (Printable PDFlalita100% (1)