Академический Документы
Профессиональный Документы
Культура Документы
Fluid Balance Monitoring Poster
Загружено:
Sania okta0 оценок0% нашли этот документ полезным (0 голосов)
961 просмотров1 страницаFluid balance
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документFluid balance
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
961 просмотров1 страницаFluid Balance Monitoring Poster
Загружено:
Sania oktaFluid balance
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 1
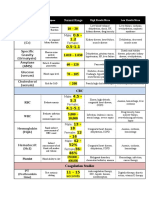
Fluid Balance Monitoring
WHAT IS FLUID BALANCE? WHO IS RESPONSIBLE: MONITORING AND ESCALATION
Fluid balance is a term used to describe In order to maintain homeostasis, the adult human body needs a fluid Trained Nurses Doctors
intake of 2-3 litres (25-30ml / kg per day), allowing it to keep a balance of
the balance of input and output of fluids in the nutrients, oxygen and water, which are necessary to preserve a stable • Identify patients who need fluid balance monitoring and communicate • Daily review:
the body, to allow metabolic processes to healthy internal environment. Output should be roughly equal, though via whiteboard behind bed, handover Indication for monitoring, is it still necessary?
Goal – document with special instructions such as restrictions or
function properly. ‘insensible losses’ may give a slightly positive balance on charts. • Clarify up-to-date plan with medical team and communicate to patient
frequency of monitoring
and visitors, wider MDT including HCAs: SALT, housekeeping, physio
What does water do for you? and any colleague who may assist with, provide or remove fluids Charts – current balance
Escalation plan or the need for it
Forms saliva Needed by the brain to • Ensure accuracy using charts and calculating cumulative
Human body is Although these fluid (digestion) manufacture hormones measurements 6 hourly
55-60% fluid compartments are classed as and neurotransmitters Patients
separate, water and fluids are Keeps mucosal • Escalate promptly to medical team in case of developing imbalance,
constantly moving between deterioration or concern • Must demonstrate capacity (understand information, retain and recall
membranes moist Regulates body
them all, powered by different when asked) concerning their fluid balance monitoring if they are to
temperature (sweating complete charts independently.
processes such as diffusion Allows body’s cells to and respiration)
2/3 total (movement of particles) grow, reproduce HCA’s and Student Nurses
1/3 is osmosis (movement of water)
• Trained nurses to calculate cumulative measurements
body fluid is and survive Acts as a shock
extracellular hydrostatic pressure (gravity • Teamwork, Communicating with MDT to ensure accurate
intracellular absorber for brain
and cardiac function) and measurements – eg SALT, housekeeping, physio
Flushes body waste, and spinal cord
oncotic pressure (proteins)
mainly in urine • Ensure chart is complete and accurate – use of appropriate equipment
Converts food to
This fluid consists of water and e.g. scales, urometers etc
electrolytes – particles which components needed
80% extracellular 20% extracellular Lubricates joints for survival - digestion • Inform trained staff or NIC with changes deterioration or concerns
carry an electrical charge – an Cup 160mls
fluid is fluid is in imbalance in these can cause
Glass 200mls Beaker 200mls Jug 750mls
interstital the plasma cardiac arrhythmias. Water is the major Helps deliver oxygen
component of most all over the body WHEN: INDICATIONS FOR FLUID BALANCE MONITORING
body parts
Increased fluid output Reduced urine output
WHY MONITOR FLUID BALANCE? HOW DO WE MONITOR FLUID BALANCE? Diarrhoea and vomiting – risk of dehydration, malnutrition and significant Oliguria – low urine output ↓0.5mls per kilogram per hour. Oliguria can be
Injury or Illness can alter fluid balance. Hypoperfusion of vital organs Knowing the signs and symptoms of Fluid Imbalance in the body is a electrolyte disturbances including hyperkalaemia an early sign of poor renal perfusion. Most common causes: hypotension
may occur with lower circulating volumes caused by dehydration, crucial aspect of hospital care and assessment. It is assessed in 3 ways: High urine output – polyuria -↑200mls /hr – leads to dehydration if or hypovolaemia. Anuria - absence of urine: ↓100mls over 24 hours.
or redistribution of within the body during an inflammatory response fluid balance charts, physical assessment of fluid balance and unmanaged. Common causes: diabetes, resolving AKI, excessive diuretics Acute Kidney Injury (AKI) /Chronic Kidney Disease
post trauma, in Cancer or during Sepsis, requiring fluid replacement. monitoring of blood results. Patients with raised creatnine blood levels combined with a low urine
High output stoma – increased frequency or ↑1 litre in 24 hrs
Alternatively an ‘overload’ may occur as a result of poor cardiac or renal output may have an AKI: the kidneys are not effectively filtering blood,
function, or excessive fluid intake orally or IV. Urinary catheter, convene, urostomy or irrigation – volumes must reabsorbing vital elements and excreting others. Prompt identification of
Overload may present with: tachycardia, hypertension, be measured. Incontinent patients may self-limit input in attempt to an AKI is crucial as it can lead to serious complications if left untreated.
Vital increased respiratory rate/effort/noise/moist cough. Fluid intake is regulated by manage problem.
Mucous membranes signs thirst – which is a natural Medications which increase risk of AKI (patients on these need fluid
dry/moist – mouth, Fluid depletion may present with hypotension, postural drop, response to fluid depletion. As Post-operative patients should be closely monitored balance monitoring)
Facial/
tongue, conjuntiva, a lowered ‘pulse pressure’, rapid, shallow respirations, rapid, the osmotic pressure of blood
oral
increases (due to higher ratio • Large open wounds: output should be estimated if an accurate output • Contrast medium – monitor fluid balance for 24 hrs before and
saliva – thick, sticky in weak thready pulse.
depletion or copious
assessment of molecules to H2O) water is is not possible after procedure
drawn from cells into blood.
and frothy in overload.
Osmoreceptors in the brain
• Drains: pleural, wound, ascitic • Chemotherapy – monitor Fluid Balance during therapy
Sunken facial features
particularly around
are dehydrated, and stimulate • Increased ‘insensible losses’: sweating, sustained pyrexia of 38°C or • Antibiotic therapy – many antibiotics can cause renal impairment
Physical Thirst release of anti-diuretic hormone a sustained respiratory ↑rpm. Each example can lead to a fluid loss of
eyes indicate severe (Check BNF). High risk are: Gentamycin, Aciclovir and Vancomycin.
depletion... or are there assessment and sensation of thirst. Adrenal
↑500 mls in any 24 hour period Fluid balance should be monitored throughout therapy and for 24hrs
glands produce Aldosterone
signs of oedema? of fluid status – stimulating reabsorbtion of post last dose
Skin elasticity – ‘tissue turgour’. sodium, and then water, from
the kidneys – less is excreted • ACE inhibitors and diuretics - often held in acute kidney injury
Skin • skin is dry and less elastic with dehydration
Weight • presence of oedema indicates overload Thirst is often a LATE indicator Unconcious
Capillary refill time of hydration, and this response patients
• good indicator of intravascular pressure/ volume becomes weaker and more
Patients
(and hydration). Blood should return to area delayed with increasing AGE. Diagnosis, Paralysis
Urine with
post gentle pressure in less than 2 seconds or at risk of
If serial weights same output • is skin warm, pink? impaired
malnutrition
time each day swallow
Jugular/venous pressure Decreased Poor memory Poor vision
• raised in overload
oral
intake Loss of
An imbalance of electrolytes in the blood can lead to fluid imbalance. FLUID BALANCE CHARTS NBM/
Impaired thirst
reflex - this can
independence
Laboratory blood tests such as urea and electrolytes, glucose, magnesium, restricted worsen with age and
calcium will determine discrepancies and lead to the right treatment. Identifying a postitive (↑input) or negative (↑ output) balance is essential, as diets increase risk
of dehydration
redressing any imbalance is vitally important. As well as aiding assessment,
Intravenous
LABORATORY RESULTS ASSOCIATED WITH together with other vital signs it allows us to evaluate and adapt our care,
fluids/enteral Stroke Delirium
replacing and restricting fluids appropriately to achieve stability. Maintaining an feeding
FLUID IMBALANCE accurate fluid chart can present challenges:
Communication with Patient Dementia
Fluid loss Fluid gain • Aware of plan, and any restriction to intake?
• Increased serum osmolality • Reduced plasma urea • Able to use equipment independently? Acute illness hypovolaemia. Generally caused by
• Compliant, possibly able to self document? Monitoring fluid balance helps monitor altered capilliary permeability (leaky blood
• High urine osmolality and • Reduced haematocrit acute illness or with early recognition of vessels) secondary to ischaemia, trauma
specific gravity Communication with MDT? further deterioration. In some illnesses or inflammation, conditions include: Heart failure
• MDT aware of monitoring? (SALT, Physio, volunteers) the fluid may move out of the vascular • Sepsis Acute Heart Failure (HF) is most commonly caused by cardiac dysfunction due to
• Raised haematocrit • Use whiteboard behind bed to convey any specific instructions system and into extracellular spaces • Bowel obstruction muscle damage, valvular dysfunction, or arrhythmias. The heart does not pump
• Increased plasma-urea outside the bloodstream. This fluid is • Acute pancreatitis (or acute on enough blood to meet all the needs of the body, and it can be complex to manage
Accuracy still in the body but no longer in a useful chronic) fluid balance for these patients. In acute new onset HF or acute decompensation of
concentration • Liver failure Chronic HF, renal function, weight and Fluid Balance should be closely and accurately
• Volumes measured specifically, awareness of volumes of different space and patients may develop low
drinking vessels urine output due to hypotension and • Malnutrition monitored, to ensure appropriate diuretic therapy or fluid management (NICE 2014).
• If patient is using pads these can be weighed with mg converted to ml
Clodagh Bannerman 2018
Вам также может понравиться
- SDL: Common Cardiac Drugs: Deala, Donna Marie Toledo Advanced Diploma in Medical Surgical-Group 1Документ13 страницSDL: Common Cardiac Drugs: Deala, Donna Marie Toledo Advanced Diploma in Medical Surgical-Group 1Donna Deala100% (2)
- Clinical Med CardsДокумент26 страницClinical Med CardsLila DanielsОценок пока нет
- Calculating Oral IntakeДокумент1 страницаCalculating Oral IntakeKassandra MerrillОценок пока нет
- Pharmacology Cheat Sheet - Generic Drug Stems - NurseslabsДокумент12 страницPharmacology Cheat Sheet - Generic Drug Stems - NurseslabsKc Mea Paran BorjaОценок пока нет
- Pharm PhalshДокумент206 страницPharm PhalshJohn MichealОценок пока нет
- Urinary CalculiДокумент4 страницыUrinary Calculirdowns100507Оценок пока нет
- Drug CardsДокумент11 страницDrug CardsLizShermanОценок пока нет
- Drugs WorksheetДокумент16 страницDrugs Worksheetninja-2001Оценок пока нет
- Dimensional Analysis For Nursing StudentsОт EverandDimensional Analysis For Nursing StudentsОценок пока нет
- Patho Physiology Bible: Over 70 Concept MapsДокумент139 страницPatho Physiology Bible: Over 70 Concept Mapslauramphs79100% (5)
- Cardiovascular Agents Group 1 Parmacology ReportingДокумент415 страницCardiovascular Agents Group 1 Parmacology ReportingMajestic RavenОценок пока нет
- Drug CardsДокумент19 страницDrug Cardslani83% (6)
- NURSING CARE OF ADULTS I: Passbooks Study GuideОт EverandNURSING CARE OF ADULTS I: Passbooks Study GuideОценок пока нет
- Ceces Study Guides Part 1Документ86 страницCeces Study Guides Part 1Patricia Mae Espinas100% (1)
- Ams 11Документ702 страницыAms 11CrazyОценок пока нет
- Disease Cheat SheetДокумент393 страницыDisease Cheat Sheetsurviving nursing school50% (2)
- Complete Drug GuideДокумент225 страницComplete Drug GuideJessica 'Baker' IsaacsОценок пока нет
- NCLEX Drug CardsДокумент136 страницNCLEX Drug CardsC Johnson100% (44)
- Med Surg Study GuideДокумент98 страницMed Surg Study Guideprogramgrabber100% (23)
- Common Medication Endings and Their ClassesДокумент1 страницаCommon Medication Endings and Their ClassesDesiree MorrisОценок пока нет
- Acid Base BalanceДокумент5 страницAcid Base BalanceTinaHo100% (4)
- Hypothyroidism Concept MapДокумент5 страницHypothyroidism Concept Mapnursing concept maps0% (1)
- Drug CardsДокумент4 страницыDrug CardsBrittany Lynn MyersОценок пока нет
- Ninja - Anti-HTN PDFДокумент6 страницNinja - Anti-HTN PDFErica Hyeyeon Lee100% (2)
- Generic Name: Acetaminophen Brand Name: Tylenol: ActionДокумент22 страницыGeneric Name: Acetaminophen Brand Name: Tylenol: Actionp_dawg100% (14)
- Patho Phlash Pathophysiology Flash Cards Download Free (EPUB, PDFДокумент4 страницыPatho Phlash Pathophysiology Flash Cards Download Free (EPUB, PDFHerman Orellana Mellado0% (3)
- m2 Pharmacology Handout 8-25-21Документ7 страницm2 Pharmacology Handout 8-25-21Sheila May SantosОценок пока нет
- Endocrine Disorders PDFДокумент6 страницEndocrine Disorders PDFShelleyОценок пока нет
- Basic Drug CardsДокумент13 страницBasic Drug Cardsnene lewis100% (2)
- 4x6 Module 6 Drug CardsДокумент10 страниц4x6 Module 6 Drug CardsQueennitaОценок пока нет
- Mnemonic S 2Документ9 страницMnemonic S 2Anj Shrestha100% (2)
- Electrolyte Mnemonic QuizletДокумент3 страницыElectrolyte Mnemonic QuizletA.h.Murad100% (2)
- Pharm ExamДокумент293 страницыPharm ExamTrish HồОценок пока нет
- Head to-Toe-Assessment Complete Guide - Nightingale CollegeДокумент1 страницаHead to-Toe-Assessment Complete Guide - Nightingale CollegeDabon RusselОценок пока нет
- This Study Resource WasДокумент2 страницыThis Study Resource WasKimberly WhitesideОценок пока нет
- MedSurg Nursing Clinical-Concept Map-2Документ3 страницыMedSurg Nursing Clinical-Concept Map-2adaezeОценок пока нет
- Nursing School Drug ChartДокумент13 страницNursing School Drug ChartEve Lester100% (3)
- Drug Cheat SheetДокумент2 страницыDrug Cheat SheetThomas Hart IIIОценок пока нет
- Med BundleДокумент36 страницMed Bundlejamie sealОценок пока нет
- Lab ValuesДокумент3 страницыLab Valuessurviving nursing school100% (1)
- Pharmacology Final Study GuideДокумент28 страницPharmacology Final Study GuideAnthony Palladeno100% (1)
- IV Solution Cheat Sheet: A Quick Reference Guide On The Different Intravenous SolutionsДокумент2 страницыIV Solution Cheat Sheet: A Quick Reference Guide On The Different Intravenous SolutionsMehdi SabeiОценок пока нет
- Fluid & Electrolytes Cheat Sheet v3Документ1 страницаFluid & Electrolytes Cheat Sheet v3faten100% (1)
- Med SurgДокумент9 страницMed SurgVanessaMUeller100% (1)
- Studying Patho For Nursing School - EasyДокумент1 страницаStudying Patho For Nursing School - EasyMarie J100% (1)
- Pharm 1.31 SOCK Method For Learning Pharm 1Документ1 страницаPharm 1.31 SOCK Method For Learning Pharm 1Angie Mandeoya100% (1)
- SimpleNursing Study GuidesДокумент5 страницSimpleNursing Study Guidessilgabernard100% (1)
- HESI Study GuideДокумент43 страницыHESI Study Guideharpay100% (12)
- Obstetrics - Cardiovascular Disease in PregnancyДокумент3 страницыObstetrics - Cardiovascular Disease in PregnancyJonathanОценок пока нет
- Lehne Flash CardsДокумент73 страницыLehne Flash Cardssarah_stover_1100% (11)
- NCLEX-PN Content Review Guide: Preparation for the NCLEX-PN ExaminationОт EverandNCLEX-PN Content Review Guide: Preparation for the NCLEX-PN ExaminationОценок пока нет
- Nursing Laboratory and Diagnostic Tests Demystified, Second EditionОт EverandNursing Laboratory and Diagnostic Tests Demystified, Second EditionОценок пока нет
- The Basics: A Comprehensive Outline of Nursing School ContentОт EverandThe Basics: A Comprehensive Outline of Nursing School ContentРейтинг: 5 из 5 звезд5/5 (3)
- CH 32 Gallbladder and Extrahepatic Biliary SystemДокумент33 страницыCH 32 Gallbladder and Extrahepatic Biliary SystemElisha BernabeОценок пока нет
- Covid-19: A Recommendation To Global Health PolicyДокумент5 страницCovid-19: A Recommendation To Global Health PolicyDr. Nur-E-Alam Rasel50% (2)
- Adult Isthmic SpondylolisthesisДокумент9 страницAdult Isthmic SpondylolisthesisAlex CortesОценок пока нет
- The Control and Prevention of MRSA in Hospitals and in The CommunityДокумент41 страницаThe Control and Prevention of MRSA in Hospitals and in The CommunityDimas RfОценок пока нет
- Myocardial Infraction ImprovedДокумент14 страницMyocardial Infraction Improvedvikram yadavОценок пока нет
- Cardiogenic ShockДокумент27 страницCardiogenic ShockMuhammad Ikbar100% (1)
- 03 Cutaneous MycosesДокумент30 страниц03 Cutaneous MycosesFelix AyornuОценок пока нет
- Epidemiology Sample QuestionsДокумент2 страницыEpidemiology Sample QuestionsMoff NyabutoОценок пока нет
- Livedoidna VaskulopatijaДокумент5 страницLivedoidna VaskulopatijaemirkurtalicОценок пока нет
- Lab Values: Interpreting Chemistry and Hematology For Adult PatientsДокумент36 страницLab Values: Interpreting Chemistry and Hematology For Adult PatientsBrian Johnson100% (1)
- Diazoxide 50mg Tab DCC SummeryДокумент1 страницаDiazoxide 50mg Tab DCC SummeryarifpharmjuОценок пока нет
- Injuria Renal Aguda PDFДокумент7 страницInjuria Renal Aguda PDFCaaarolОценок пока нет
- Oral Care ProtocolДокумент8 страницOral Care ProtocolQonitaNurMiladiОценок пока нет
- Biology Matters 3rd EditionДокумент272 страницыBiology Matters 3rd Editionotakukat763Оценок пока нет
- Albendazole - Drug Information PDFДокумент7 страницAlbendazole - Drug Information PDFjjjkkОценок пока нет
- TympanoplastyДокумент4 страницыTympanoplastyMelly Selvia AОценок пока нет
- DivocДокумент1 страницаDivocCarrackОценок пока нет
- Microbiology PneumoniaДокумент31 страницаMicrobiology PneumoniaKartika Rezky100% (1)
- 26 - Nonsurgical Treatment of Peyronies DiseaseДокумент4 страницы26 - Nonsurgical Treatment of Peyronies DiseaseNunuh SulaemanОценок пока нет
- Muscular Dystrophy and Its Ayurvedic PerspectivesДокумент149 страницMuscular Dystrophy and Its Ayurvedic PerspectivesMuktha ShenoyОценок пока нет
- A Huge Completely Isolated Duplication CystДокумент6 страницA Huge Completely Isolated Duplication CystNurlyanti RustamОценок пока нет
- Dizziness HXДокумент4 страницыDizziness HXbadmanОценок пока нет
- Topic 3 Environmental Risk AssessmentДокумент47 страницTopic 3 Environmental Risk Assessment郭思凱Оценок пока нет
- Affection of Salivary GlandsДокумент16 страницAffection of Salivary GlandsAdarshBijapurОценок пока нет
- Essential Intrapartum and Newborn Care: Health Science Department Southway College of TechnologyДокумент3 страницыEssential Intrapartum and Newborn Care: Health Science Department Southway College of TechnologyRowena AngelesОценок пока нет
- Kurva LubchencoДокумент3 страницыKurva LubchencoDanil Armand67% (3)
- American College of Women's Health PhysiciansДокумент16 страницAmerican College of Women's Health PhysiciansSex & Gender Women's Health CollaborativeОценок пока нет
- Research Paper On Organ DonationДокумент8 страницResearch Paper On Organ Donationsheeliya whiteОценок пока нет
- Tool For Bundling CalculationДокумент1 страницаTool For Bundling CalculationGladdy CabrezaОценок пока нет
- Immunofluorescence Techniques: Ian D. Odell and Deborah CookДокумент4 страницыImmunofluorescence Techniques: Ian D. Odell and Deborah CookbalamurugantОценок пока нет