Академический Документы
Профессиональный Документы
Культура Документы
Ninja - Adrenergic Drugs PDF
Загружено:
Erica Hyeyeon LeeОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ninja - Adrenergic Drugs PDF
Загружено:
Erica Hyeyeon LeeАвторское право:
Доступные форматы
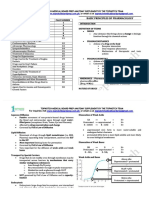
• if α is activated, baroreceptor will act
- vasculature increases DBP (main determinant of MAP)
- MAP determines if baroreceptor will act
• if ß1 and ß2 activated, baroreceptor inactive
- ß1 increases SBP no ∆MAP --> no baroreceptor
- ß2 decreases DBP
Direct Acting Adrenergic Agonists: Endogenous Catecholamines and D1 Agonists
Drug Name Receptor Uses/effect PK Adverse effects Other
High doses=potent vasopressor: ↑ BP [systolic>diastolic] → +ve
chronotropic and inotropic effects [β1] and vasoconstriction [α1] Synthesized from tyrosine in the
→ ↑CO [& ↑ O2 demand from heart] adrenal medulla
CNS disturbances:
Low doses → ↓ PVR [β2], rise in systolic and drop in diastolic BP
Restlessness, fear,
with the MAP staying the same [no reflex, β1]; tachycardia [β1] Rapid onset Polar molecule: does not enter
apprehension, headache
α & β2 Brief Duration CNS in therapeutic doses
and tremor [may be
Bronchodilation [β2]
secondary to effects
Low dose: β Relaxed GI smooth muscle with contracted sphincters Administered through IV in Metabolized by COMT and MAO
outside of CNS]
effects Relaxed detrusor [β2] and contracted sphincter [α1]! can lead emergencies → VMA and metanephrine
[vasodilation] to urinary retention
Epinephrine Intracranial hemorrhage
Prostatic smooth mm. contraction Other routes include SC, ET Hyperthyroidism may enhance
due to increased BP
High dose: α tube, inhalation, and CV actions due to upregulation of
effects Metabolic: hyperglycemia due to ↑ glycogenolysis and glucagon topically in the eye receptors
Cardiac arrhythmias –
[vasoconstriction] release [β2]; net inhibition of insulin secretion [α2 inhibits while
especially in patients on
β2 enhances secretion] Do not give orally due to Cocaine prevents re-uptake
digitalis
↑ Lipolysis through β3 activation [↑ cAMP and HSL] inactivation by intestinal
ß1 ≈ ß2 ≈ ß3 >> α1
enzymes Β-blockers cause predominate α
Pulmonary edema
DOC for patients in anaphylactic shock; cardiac arrest; asthma RAAS (ß1) + urinary retention (ß2)
effects such as ↑ TPR and BP
attacks combined with local anesthetics to increase duration; - ß with + a1
glaucoma [decreased production of aqueous humor] ß2
Vasoconstriction [α1] → increased PVR → ↑ SBP/DBP & MAP
Bradycardia due to decreased sympathetic outflow following
the baroreceptor response [indirect effect through M2] Baroreceptor reflex counteracts
local action which can be blocked
NE may cause kidney
Norepinephrine α & β1 > β2 Induces hyperglycemia [less potent than epi] by pretreatment with atropine…
shutdown
α1 ≈ α2 ≈ ß1 >> ß2 reveals direct effect of
Limited therapeutic value: can treat shock, but dopamine is tachycardia
better due to preservation of renal blood flow
Used to control BP and TXT of septic/cardiogenic shock
Central regulator of movement
CVS: low doses vasodilate through D1 receptors [cAMP]
especially at renal, mesenteric and coronary
Overdose causes
sympathomimetic
DOC for cardiogenic and hypovolemic shock: ↑GFR, renal blood
symptoms
flow and Na+ excretion → preservation of renal function
Ineffective when given
Dopamine D1 D & α & β
> ß1 > α1 orally due to metabolism Can cause nausea, HTN, & Dopamine does not cross BBB
Inotropic effect at intermediate concentration [β1] and
by MAO and COMT arrhythmia but it is short
increasing release of NE
lived due to rapid
metabolism to HVA
Increase in systolic BP &MAP
High concentration → α1 mediated vasoconstriction!↑BP
TXT for severe CHF
Peripheral vasodilation→ used in short term management of Give continuously via IV,
Fenoldopam D1
inpatient HTN not a bolus
(indirect)
(vasodilation)
Direct Acting Adrenergic Agonists: β-agonists
→ Major role in treatment of bronchoconstriction
Drug Name Receptor Uses/effect PK Other
CVS: ↑CO through rate and force of contraction [AV block or Cardiac arrest] via β1
↑lipolysis
↓TPR through vasodilation [β2] because there is no α1 opposing it
Slight ↑SBP; ↓MAP and ↓DBP, tachycardia (reflex)
Most reliable when given
Isoproterenol β1 & 2 Hyperglycemia!↑glycogenolysis Similar adverse effects compared to Epi
parenterally or inhaled
nonspecific
ß agonist
Bronchodilation and GI smooth muscle relaxation mediated by β2
Stimulate heart in emergency in pts. w/ bradycardia or heart lock + cardiogenic
shock
& cardiogenic Racemic mixture:
Acute management of congestive heart failure: increases contractility shock
Can build up tolerance -ve: α1 & weak β1 agonist;
Dobutamine β1 ↑ CO with little change in heart rate → O2 demands of the myocardium are not
with long term use +ve: α1 antagonist and potent β1 agonist
significantly affected gives it an advantage over other sympathomimetics & mild ß2 agonist
Net: selective β1
Resorcinol ring→ not
Bronchodilator metabolized by COMT Selectivity is lost at high concentrations
Terbutaline Emergency treatment of status asthmaticus giving it a longer duration
Reduces uterine contractions in premature labor :relaxes detrusor Used in treatment of asthma without having effects on
β2 Oral, Inhalation or SC the heart
Albuterol ß2 >> ß1 Inhalant bronchodilator; relief of symptoms in asthma
Slow onset, but Adverse effects: tremor, restlessness, apprehension and
Salmeterol Bronchodilator
prolonged action [12 anxiety
Formoterol Long acting → not used for prompt relief of bronchospasm
hours] after inhalation
Direct Acting Adrenergic Agonists: α-agonists
Drug Name Receptor MOA Uses/Effect/Actions PK Adverse Effects
Vasoconstrictor: ↑SBP and ↑DBP
Nasal decongestant
Mydriasis
Phenylephrine α1 Peripheral vasoconstriction TXT of supraventricular tachycardia Oral or topical
NO direct effect on heart, but does cause reflex
bradycardia after parenteral administration
Partial agonist: activation of central α2 Acute rise in BP due to transient Centrally acting antiadrenergic
Clonidine receptors suppresses sympathetic Antihypertensive vasoconstriction when given IV, drugs: SNS in CNS
outflow but not when given orally Sedation
Mental lassitude
Metabolized to α-methylnorepinephrine which causes effects similar to clonidine: ↓TPR
α2 • blocks α2
Impaired concentration
Methyldopa Central acting anti-HTN • no autoregulation and BP… prodrug
α2 ≈ central
• SNS AE: positive Coombs Xerostomia
DOC in pregnant patients with HTN [safety] (may cause hemolytic anemia) Lethargy
↓ aqueous humor production along with
Brimonidine ↓ intraocular pressure in glaucoma Ocular administration [topical]
increased outflow
Indirect Acting Adrenergic Agonists
→ Releasing Agents potentiate actions of endogenous NE by causing its release from presynaptic vesicles
Drug Name Receptor MOA Uses/Effect/Actions PK Adverse Effects
↑ BP through α1 and β effects
Little effect on Displaces catechol from storage vesicle Central stimulatory action:
Fatigue and depression following
Amphetamine post synaptic Weak inhibitor of MAO Alertness!insomnia
stimulation
α and β Blocks catecholamine reuptake ↓fatigue & appetite
causes presynaptic
cells to
release NE/E TXT of depression, narcolepsy and appetite suppression [in the past]
ADHD in children
Methylphenidate Structural analog of amphetamine
Narcolepsy
Byproduct of tyrosine Serious vasopressor episodes in
enters neuron via system L Not clinically useful, but is found in
Tyramine
induces hypersecretion metabolism, normally oxidized patients on MAO-I’s after release of
of catecholamines fermented foods [cheese and wine]
by MAO NE hypertensive crisis
Indirect Acting Adrenergic Agonists: Drugs That Act Presynaptically
→ All are Monoamine reuptake inhibitors
Drug Name Receptor MOA Uses Adverse Effects
DAT most potent against DET Sympathomimetic Therapeutic use: blockage of
Blocks dopamine [major effect], serotonin and NE Intense euphoria from blockage of dopamine reuptake in
Cocaine SERT voltage gated Na+ channels → local anesthetic
transporters→ potentiation and prolonged effects the limbic system & vasospasms in heart / brain
NET of the respiratory tract
Atomoxetine NET Selective NET inhibitor ADHD
NET Inhibit NE and Dopamine transporters!↑NE,
Modafinil Narcolepsy
DAT ↑Dopamine, ↑serotonin, ↑glutamate & ↓GABA
Adrenergic Agonists: Mixed Acting
Drug Name Receptor MOA Uses/Effects/Actions PK Adverse Effects Other
Vasoconstriction and cardiac stimulation → ↑ BP
^used in spinal anesthesia if hypotension is common NOT a catecholamine → poor
induce release
of catecholamines Bronchodilation [prophylactic TXT of asthma substrate for COMT and MAO→
and because it is slower onset and less potent than epi or longer duration of action Herbal supplements Induces release of NE and
stimulates
receptors
isoproterenol] banned in 2004 due to activates adrenergic receptors
Ephedrine Excellent oral absorption life-threatening
Synergistic effect with Anti-AChE in treatment of cardiovascular Use declining due to better drugs
α and β
myasthenia gravis Enters CNS reactions with fewer side effects
Mild CNS stimulation [alertness] and increased Eliminated unchanged in urine
athletic performance
Ephedrine
Pseudoephedrine Nasal decongestant with an H1 histamine antagonist
enantiomer
Adrenergic Antagonists: α-antagonists
→ Primary effect on blood pressure: vasculature is under tonic sympathetic control so blockade of these receptors reduces tone and decreases TPR
→ Epinephrine Reversal: all α-blockers inhibit Epi induced vasoconstriction, but not the β effect of vasodilation → ↓BP in response to Epi in the presence of phenoxybenzamine [NE is only
diminished] inhibit α1, but the ß1 & ß2 effects still occur (no reflex tachycardia)
→ Selective α1 blockers can cause dizziness, lack of energy, nasal decongestant, HA, drowsiness, orthostatic hypotension; tendency to retain Na+ and fluid→ give with a diuretic
Drug Name Receptor MOA Effects Uses Adverse Effects
Alkylation irreversibly CVS: prevents
DOC for pheochromocytoma: blocks effects of Postural hypotension
blocks receptor vasoconstriction of
excess catecholamines [may require a β blocker Nasal stuffiness
peripheral blood
to control tachycardia after α blockade is Nausea and vomiting
Slightly α1 selective vessels→ reflex
Phenoxybenzamine established] Inhibit ejaculation
Also blocks H1, M and 5-HT tachycardia [-α1]
[α1 > α2]
receptors
Historically used to lower BP, but was Contraindicated in pts with ↓ coronary
Presynaptic α2 [-α2]
unsuccessful [block presynaptic α2] perfusion due to reflex tachycardia
inhibits NET block→ ↑CO
Dx & control hypertensive episodes of
Nonselective
pheochromocytoma Phentolamine block test
α
Postural hypotension –baroreceptor reflex and
Prevents dermal necrosis when NE is released α2 blockade on cardiac nerves
Reversible α blocker
Phentolamine Antihypertensive in stimulant overdose Arrhythmia & angina
Serotonin blocker
used
during Muscarinic, H1 and H2 agonist
surgery Sudden withdrawal of sympatholytics Contraindicated in pts with ↓ coronary
[α1 ≈ α2] No autoregulatory reflex
[clonidine] perfusion
Interactions between MAO-Is and tyramine
↓TPR through relaxation of ↓ BP without reflex
Prazosin arterial and venous smooth tachycardia […α2]
muscle ^syncope Suppress sympathetic outflow from CNS
Selective α1 Not the DOC for primary HTN
↓ LDL/TAG, ↑HDL
Structural analog of prazosin →
Terazosin TXT of HTN, BPH
Useful in longer t1/2 → Less frequent First dose effect may cause exaggerated
Doxazosin Improves urinary
treatment of dosing hypotensive response and syncope [adjust 1st
blood flow
HTN dose ¼ of normal]
Relaxes
Selective for α1A receptor found Used in TXT of BPH with little effect on BP
Tamsulosin genitourinary
in genitourinary smooth muscle [reduced orthostatic HTN]
smooth muscle
α2 blocker→ indirect adrenergic TXT of erectile dysfunction, but has been Can reverse effects of α2 agonists like Clonidine
Yohimbine α2 ↑NE release→ ↑BP
agonist replaced by PDE-5 inhibitors [bad]
Adrenergic Antagonists: Partial Agonists
Drug Name Receptor MOA Uses/Effects
Causes a smaller reduction in resting HR and BP
Pindolol partial β β blocker with intrinsic sympathomimetic activity helps manage HTN
Preferred in pts with diminished cardiac reserve or propensity to bradycardia
Adrenergic Antagonists: β-antagonists
Drug Name Receptor MOA Effects/Uses Adverse Effects Other
used in chronic Does not induce postural
O2 demand of heart Bronchoconstriction→ Contraindicated in patients with
CVS: ↓ HR, ß1 stable angina hypotension because α1 receptors
COPD or asthma
↓contractility & remain active
Used in treatment of:
↑TPR [β2]
HTN [through ↓CO, not the DOC] Migraine [blocks Contraindicated in pts w/ variant angina
↓HDL and ↑LDL/TAGs [block ß3
vasodilation] Hyperthyroidism contraindicated in diabetics on insulin
Propranolol Metabolic: ↓ activation of HSL]! β1 selective
Chronic angina [↓O2 requirement] A-fib, MI Impair recovery from hypoglycemia in insulin dependent
[prototype] glycogenolysis and actually improve the lipid profile
[protective] patients→ syncope
glucagon
DOC for performance anxiety/stage fright *tachycardia seen in such episodes will mask the signs of
secretion→ severe Abrupt withdrawal→ HTN,
β1 & β2 Essential tremor hypoglycemia
hypoglycemia in pts tachycardia, ischemia d/t up
[ß1]: decrease RAAS
no reflex
on insulin regulation of β receptors after long
occurs CNS: sedation, dizziness, lethargy, fatigue, depression
term use
Longer duration of
Nadolol Long term treatment of angina and HTN
action
HTN [ ß2 vasodilation] DOC
Timolol
prophylaxis for migraines Glaucoma [open angle]
Management of HTN in pts with impaired pulmonary
Atenolol function or IDDM Less likely to induce bronchospasm! contraindicated in
Metoprolol asthmatics modest ß2 effects
Long term mgmt. of pts w/ angina pectoris/acute MI
β1
Useful in controlling arrhythmia [supraventricular or
Cardioselective PK: Ultra short acting: t1/2 is about 10
thyrotoxicosis]
minutes
Esmolol Associated with hepatic injury
Administered IV
Perioperative HTN :during surgery
Safer in critically ill patients
MI in acutely ill pts
Adrenergic Antagonists: Combined α1 and β-antagonists
Drug Name Receptor MOA Uses/Effects PK Adverse Effects
competitive Decrease in BP: HTN
More potent β antagonist
α1→ relaxation of arterial smooth muscle Orthostatic hypotension and
Labetalol Oral: chronic HTN
ß1 antagonist β1→ blocks sympathetic reflex dizziness [α1]
ß>α IV: emergencies
α1 & β
ß2 agonist β2→ sympathomimetic action contributes to vasodilation
α1 antagonist
Used on pts with CHF and HTN
Carvedilol More potent β antagonist
ß>α Antioxidant properties
Adrenergic Antagonists: Drugs Acting Presynaptically
Drug Name MOA Uses/Effects PK Other
α-methyltyrosine Blocks NE [& Epi] synthesis through competitive Used in adjuvant therapy with phenoxybenzamine in treatment of malignant
(metyrosine) inhibition of tyrosine hydroxylase pheochromocytoma [when surgery is not possible]
Unable to concentrate and store NE and dopamine in the vesicle→ continuous breakdown Slow onset and Historical TXT of
Reserpine Irreversible damage to VMAT→ ↓NE and dopamine
by MAO long duration HTN
[Obsolete] availability→ sympatholytic response -SNS
↓BP and ↓HR (gradual)
Reversible inhibitor of VMAT!↓catecholamines
Tetrabenzine Chorea associated with Huntington’s Disease
presynaptically
Вам также может понравиться
- Immunopharmacology PDFДокумент2 страницыImmunopharmacology PDFErica Hyeyeon LeeОценок пока нет
- Nsaids: Celecoxib, Meloxicam Aspirin, Diclofenac, Ibuprofen, Indomethacin Ketorolac, Naproxen, PiroxicamДокумент2 страницыNsaids: Celecoxib, Meloxicam Aspirin, Diclofenac, Ibuprofen, Indomethacin Ketorolac, Naproxen, PiroxicamErica Hyeyeon LeeОценок пока нет
- Opioids PDFДокумент2 страницыOpioids PDFErica Hyeyeon LeeОценок пока нет
- Asthma - Respiratory PDFДокумент1 страницаAsthma - Respiratory PDFErica Hyeyeon Lee0% (1)
- Ninja - Antihyperlipidemics PDFДокумент3 страницыNinja - Antihyperlipidemics PDFErica Hyeyeon Lee100% (1)
- GI Drugs PDFДокумент6 страницGI Drugs PDFErica Hyeyeon Lee100% (1)
- Ninja - Anemias PDFДокумент1 страницаNinja - Anemias PDFErica Hyeyeon LeeОценок пока нет
- Ninja - Anti-Coagulants PDFДокумент3 страницыNinja - Anti-Coagulants PDFErica Hyeyeon Lee100% (1)
- Pharmacogenomics PDFДокумент1 страницаPharmacogenomics PDFErica Hyeyeon LeeОценок пока нет
- Ninja - Antiarrhythmic Drugs PDFДокумент7 страницNinja - Antiarrhythmic Drugs PDFErica Hyeyeon Lee100% (1)
- Ninja - Drugs Heart Failure PDFДокумент4 страницыNinja - Drugs Heart Failure PDFErica Hyeyeon LeeОценок пока нет
- Ninja - Antianginal Drugs PDFДокумент2 страницыNinja - Antianginal Drugs PDFErica Hyeyeon LeeОценок пока нет
- Pharmacokinetics - Introduction To ANS PDFДокумент2 страницыPharmacokinetics - Introduction To ANS PDFErica Hyeyeon Lee100% (1)
- Ninja - Diuretics PDFДокумент3 страницыNinja - Diuretics PDFErica Hyeyeon Lee100% (1)
- Ninja - Anti-HTN PDFДокумент6 страницNinja - Anti-HTN PDFErica Hyeyeon Lee100% (2)
- Ninja - Cholinergic Drugs PDFДокумент4 страницыNinja - Cholinergic Drugs PDFErica Hyeyeon Lee100% (2)
- Ninja - Autacoids PDFДокумент3 страницыNinja - Autacoids PDFErica Hyeyeon LeeОценок пока нет
- 0.5. ANS Quicksheet PDFДокумент1 страница0.5. ANS Quicksheet PDFErica Hyeyeon LeeОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Medications Affecting The Nervous System: (Classifications)Документ110 страницMedications Affecting The Nervous System: (Classifications)susan2johnson-501300Оценок пока нет
- Bolo - Dakabadonebuli - Book 2Документ152 страницыBolo - Dakabadonebuli - Book 2sasa sasadzeОценок пока нет
- Module 3 - Frustration, Conflict and StressДокумент16 страницModule 3 - Frustration, Conflict and StressPadmaja PradeepОценок пока нет
- Controlling Your Dopamine For Motivation, FocusДокумент111 страницControlling Your Dopamine For Motivation, Focuswnd cОценок пока нет
- Case Study, NCP, and Drud Study For A Pt. With Diagnosis of Post ThoracostomyДокумент11 страницCase Study, NCP, and Drud Study For A Pt. With Diagnosis of Post Thoracostomynursejr24Оценок пока нет
- Final SK Golden 7+8 ErrataДокумент19 страницFinal SK Golden 7+8 ErrataHassam ZulfiqarОценок пока нет
- Pharmacological Interactions of VasoconstrictorsДокумент8 страницPharmacological Interactions of VasoconstrictorsValeska Farina EspinosaОценок пока нет
- Polygraph HandoutДокумент103 страницыPolygraph HandoutHEROWIN EDUARDOОценок пока нет
- Melanin Physics by NEB HERUДокумент241 страницаMelanin Physics by NEB HERUNeb Heru91% (81)
- HarmonesДокумент6 страницHarmonesbaskarОценок пока нет
- Pharma Final ModuleДокумент139 страницPharma Final ModuleQuantum XavierОценок пока нет
- Stress! Can Interfere With Endocrine SystemДокумент4 страницыStress! Can Interfere With Endocrine SystemInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Sem4 SylДокумент16 страницSem4 SylraviomjОценок пока нет
- The Development and Perceptions of GraffitiДокумент12 страницThe Development and Perceptions of Graffiticitra dewiОценок пока нет
- Intermittent Fasting Cheat Sheet PDFДокумент30 страницIntermittent Fasting Cheat Sheet PDFjong bariquit89% (9)
- Use of vasopressors and inotropes guideДокумент16 страницUse of vasopressors and inotropes guideIrving H Torres LopezОценок пока нет
- Physiology of ThermoregulationДокумент18 страницPhysiology of Thermoregulationsanti sidabalokОценок пока нет
- The Effects of Hospital Noise: Denise B. Choiniere, MS, RNДокумент7 страницThe Effects of Hospital Noise: Denise B. Choiniere, MS, RNAsal Salah100% (1)
- Biology: Board - ICSE Class-8 Topic - Endocrine and AdolescenceДокумент11 страницBiology: Board - ICSE Class-8 Topic - Endocrine and AdolescenceItu Dey100% (2)
- Neuropsychology of StressДокумент79 страницNeuropsychology of StressDr Nader KorhaniОценок пока нет
- BP402T - Med - Chem-I, 1st Sessional Que - PaperДокумент2 страницыBP402T - Med - Chem-I, 1st Sessional Que - PaperSajid khanОценок пока нет
- Adrenal ChromeДокумент1 страницаAdrenal Chromestormrunner002100% (1)
- Qdoc - Tips Topnotch Supplement Pharmacology HandoutДокумент57 страницQdoc - Tips Topnotch Supplement Pharmacology HandoutShehana MusahariОценок пока нет
- Physiological Responses To Exercise at Altitude: An UpdateДокумент8 страницPhysiological Responses To Exercise at Altitude: An UpdateMiguel Angel Ballen SeguraОценок пока нет
- Unit 6 - Week 3 - GE2020Документ13 страницUnit 6 - Week 3 - GE2020Giang NguyenОценок пока нет
- Bhaswati Bhattacharya Everyday Ayurveda DaiДокумент305 страницBhaswati Bhattacharya Everyday Ayurveda DaiRohit KumarОценок пока нет
- Drug-Receptor Interactions and PharmacodynamicsДокумент4 страницыDrug-Receptor Interactions and Pharmacodynamicshussam mazinОценок пока нет
- Anaphylaxis: Emergency Department TreatmentДокумент14 страницAnaphylaxis: Emergency Department TreatmentTom BiusoОценок пока нет
- Module Title: Teacher'S Education Program Bachelor of Elementary Education Third YearДокумент10 страницModule Title: Teacher'S Education Program Bachelor of Elementary Education Third YearRodrick RamosОценок пока нет
- Icu Masterclass - Inotropes and Vasopressors: Christopher R. Tainter, MDДокумент78 страницIcu Masterclass - Inotropes and Vasopressors: Christopher R. Tainter, MDHhaОценок пока нет