Академический Документы
Профессиональный Документы
Культура Документы
Ent Osce - Updated
Загружено:
HoneyАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ent Osce - Updated
Загружено:
HoneyАвторское право:
Доступные форматы
ENT OSCE - Solved
Station 01: CT SCAN of Para-nasal Sinuses
Structures can be seen:
Anomalies can be seen: Polyp, Mass, Foreign Body, Sinusitis
Views/Angels of CT for Paranasal Sinuses: Coronal View, Axial View, Lateral
View/Sagittal View
Station 02: Pleomorphic Adenoma of Parotid Gland
D/D: Warthin Tumor, Pleomorphic Adenoma, Oxyphil Adenoma, Squamous Cell Carcinoma of
Parotid Gland
Diagnosis: Pleomorphic Adenoma
Investigation to be performed: FNAC, CT/MRI
Treatment: Superficial Parotidectomy
Complications of Treatment: Nerve Dysfunction, Frey’s Syndrome, Numbness, Facial
Asymmetry, Necrosis near Incision, Reappearance of Tumor
Station 03: OTOSCOPE
Identify: Otoscope
Used for: Ear Examination – Gives view of Tympanic Membrane
and Ear Canal
Structures seen with it: Tympanic Membrane/Ear Drum – Cone
of Light, Posterior Malleal Fold, Lateral Process of Malleus,
Anterior Malleal Fold
Pathologies can seen with it: Discharge, Tympanic Membrane
Bulging, Tympanic Membrane Retraction, Tympanic Membrane
Perforation, Cerumen, Foreign Body, Exostoses
What is Serous Otitis Media? : Accumulation of non-purulent
fluid in Middle Ear Cleft
What age group it involves? : School Going Children
Why it happens? : Malfunction of Eustachian Tube, Allergy,
Viral Infection
What will you see on otoscope in it? : Dull opaque tympanic
membrane with loss of light reflex. Thin leash of blood vessels
may also be seen along the handle of malleus.
What color of tympanic membrane you will see in it? : Tympanic Membrane may appear
yellow, blueish or grey in color.
How will you treat it? : Medical Treatment includes decongestants, anti-allergic, antibiotics,
Middle Ear Aeration. Surgical Treatment includes Myringotomy and Aspiration of Fluid,
Grommet Insertion, Surgical Treatment of Causative Factor
What is Grommet? : Grommet is a tube surgically inserted to provide continued aeration of
middle ear.
Station 04: Nose Examination
Check Broadcast Msg, Link is provided for Examinations
Station 05: Perform Posterior
Rhinoscopy
Technique. Patient sits facing the examiner,
opens his mouth and breathes quietly from
the mouth. The examiner depresses the
tongue with a tongue depressor and
introduces posterior rhinoscopic mirror, which
has been warmed and tested on the back of
hand. The mirror is held like a pen and carried
behind the soft palate. Without touching it on
the posterior third of tongue to avoid gag
reflex, light from the head mirror is focussed
on the rhinoscopic mirror which further
illuminates the part to be examined. Patient’s relaxation is important so that soft palate does
not contract.
Station 06: Anterior Rhinoscopy
Name the Instrument: Thudicum Nasal
Speculum
In Which Surgery it is used? : Submucous
Resection of Nasal Septum (SMR)
What are the indications for SMR or
Septoplasty? : Deviated Nasal Septum,
Recurrent Epistaxis, To Correct External Nose
Deformity
What is little’s Area? : It is a vascular area in
anterioinferior part of nasal septum, where
anastomosis of arteries is present (Kiesselbach’s Plexus). Commonest site for epistaxis.
What arteries anastomose here? : Anterior ethmoidal, sphenopalatine, greater palatine and
septal branch of superior labial arteries and their corresponding veins form an anastomosis
here.
Station 07: Tracheostomy
Identify: Tracheostomy Tube for
Tracheostomy
What is Tracheostomy? : Tracheostomy is
making an opening in anterior wall of trachea
for ventilation or removing secretions.
Types of Tracheomstomy: Emergency
Tracheostomy, Elective Tracheostomy,
Permanent Tracheostomy, Percutaneous
Dilation tracheostomy and Mini
Tracheostomy
Indications: Respiratory obstructions,
Respiratory Insufficiency, Retained Secretions
Complications: Hemorrhage, Aponea, Tube Blockage, Injury to reccurent laryngeal nerve,
Laryngeal Stenosis, Tracheal Stenosis, Tracheo-esophageal Fistula
Station 08: Thyroid Nodule
D/D: Colloid Nodule, Adenoma,
Thyroid Cyst, Carcinoma,
Regeneration Nodule
Investigations to do: Fine Needle
Aspiration Cytology (FNAC), Thyroid
Function Test, Ultrasound
Treatment: Thyroidectomy
What are the complications of its
surgery? : Hematoma, Airway
Obstruction, Injury to recurrent
laryngeal nerve, Injury to Superior Laryngeal Nerve, Infection, Pneumothorax, Hypothyroidism,
Hypocalcemia.
Station 09: Peri-tonsillar Abscess (Quinsy)
D/D: Para-Pharyngeal Abscess, Neoplasm of Tonsil,
Retro-Pharyngeal Abscess, Peri-Tonsillar Abscess
Diagnosis: Peri-Tonsillar Abscess or Quinsy
Clinical Features: Pain usually unilateral,
Odynophagia, Hot Potato Voice (Thick and Muffled
Voice), Foul Breathe, Trismus
Treatment: Hospitalization, IV Fluids, Antibiotics,
Analgesics, Oral Hygiene, Incision and Drainage.
Station 10: Adenoidectomy
Identify: St. Clair Thompson adenoid
curette
Used for: Used in adenoidectomy
Indications: Adenoid Hypertrophy,
Recurrent Rhino-sinusitis, Chronic
Otitis Media with effusion associated
to Adenoid Hypertrophy, Dental
Malocclusion
Contraindications: Cleft Palate,
Hemorrhagic Diathesis, Acute
Infection of Upper Respiratory Tract
Complications of Adenoidectomy: Hemorrhage, Injury to Eustachian Tube opening, Injury to
pharyngeal musculature, Nasopharyngeal Stenosis, Recurrence
Station 11: Nasal Gauge – Killian’s nasal gouge (bayonet-shaped)
Name the Instrument: Nasal Gauge – Killian’s nasal gouge (bayonet-shaped)
Used for: Used for removal of septal spurs or bony crests and ridges in SMR operation
Name the Surgery: Submucous Resection of Nasal Septum (SMR)
Difference b/w Septoplasty and SMR:
Septoplasty SMR
Type of Procedure Conservative Destructive
Age Any Age Adults (>17 Years)
Mucoperichondrial One Side Both Sides
Flap
Risk of Tearing Low High
Flap
Risk of Septal Low High
Perforation
Contraindications Acute Nasal or Sinus Infection, Bleeding Age Below 17, Acute
Diatheses, Untreated Diabetes and Attack of Respiratory
Hypertension Infection, Bleeding
Diatheses, Untreated
Diabetes and Hypertension
Complications: Bleeding, Septal Hematoma, Septal Abscess, Perforation, Depression of Bridge,
Toxic Shock Syndrome, Persistence of Deviation
Station 12: Case of Mastoiditis
Diagnose: Mastoiditis
Clinical Findings for Diagnosis:
Symptoms – Pain Behind the Ear, Fever, Ear Discharge
Signs – Mastoid Tenderness, Sagging of Posteriosuperior Meatal Wall, Perforation of
Tympanic Membrane, Swelling over the mastoid, Conductive Hearing loss
Treatment: Hospitalization, Antibiotics, Myringotomy, Cortical Mastoidectomy if Indicated
Station 13: Aphthous Ulcer Case
Diagnosis: Aphthous Ulcer
Risk Factors: Nutritional Deficiency, Viral or Bacterial Infection, Food Allergies, Hormonal
Changes, Stress
Treatment: Topical Application of Steroids and cauterization with 10% Silver nitrate. Local Pain
can be relieved with Lignocaine Viscous.
Station 14: Tonsillectomy
Identify: Eve’s Tonsillar Snare
Uses: Used for tonsillectomy. After the tonsil has been dissected till its lower pole, snare is
passed round the tonsil to
engage the pedicle and
then firmly closed. It
crushes and cuts the
pedicle thereby
minimizing bleeding. Wire
used in snare is number
25 SWG.
Indications for Tonsillectomy:
Absolute Indications: Recurrent Infection of Throat, Peritonsillar Abscess, Tonsillitis,
Suspicious of Malignancy, Hypertrophy of Tonsils
Relative Indications: Unresponsive Diptheria Carriers, Chronic Tonsillitis, Streptococcal
Carriers, Recurrent Streptococcal Tonsillitis
Contraindications: Hb less than 10g, Acute infection of Upper Respiratory Tract, Under 3 year
age, Cleft Palate, Bleeding Disorder, Menses, Uncontrolled Systemic Disease
Station 15: Case of Angiofibroma
Diagnosis: Angiofibroma – Tumor of Adolescent Males, thought to be testosterone related
Clinical Findings:
Profuse, Recurrent, Spontaneous Epistaxis
Nasal Obstruction
Otitis Media with Effusion due to Eustachian tube blockage
Proptosis
Broadening of nasal bridge
Mass in Nasopharynx
Investigations: CT Scan of Nose and Paranasal Sinuses, both Coronal and Axial, Four Vessel
Angiography
Treatment: Surgical Removal of Angiofibroma
Station 16: Mastoidectomy
Identify: Mastoid Retractor
Used for: Used in mastoidectomy
to retract soft tissues after incision
and elevation of flaps. It is self-
retaining and haemostatic.
Define Mastoidectomy: A Surgical
Procedure to remove diseased
mastoid air cells when medical
treatment is not effective.
Types of Mastoidectomy:
Cortical: A Canal wall up
mastoidectomy which is an exenteration of all accessible mastoid air cells preserving the
posterior meatal wall.
Modified Radical: A canal wall down mastoidectomy in which the attic and mastoid are
exteriorized into the external auditory canal by removal of the posterior meatal and
lateral attic walls. Tympanic membrane remnant, functioning ossicles and the reversible
mucosa and function of the Eustachian tube are preserved and reconstructed.
Radical: A canal wall down mastoidectomy in which the tympanic membrane and
ossicles are not reconstructed, thus exteriorizing the middle ear and the mastoid.
Station 17: Indirect Laryngoscopy
Identify: Laryngeal Mirror, used to perform Indirect Laryngoscopy
What is Laryngoscopy? : An endoscopic procedure to get close view of larynx and other
surrounding structures.
Perform Indirect Laryngoscopy: Patient is seated opposite the examiner. He should sit erect
with the head and chest leaning slightly towards the examiner. He is asked to protrude his
tongue which is wrapped in gauze and held by the examiner between the thumb and middle
finger. Index finger is used to keep the upper lip or moustache out of the way. Gauze piece is
used to get a firm grip of the tongue and to protect it against injury by the lower incisors.
Laryngeal mirror (size 4–6) which has been warmed and tested on the back of hand is
introduced into the mouth and held firmly against the uvula and soft palate. Light is focused on
the laryngeal mirror and patient is asked to
breathe quietly. To see movements of the
cords, patient is asked to take deep
inspiration (abduction of cords), say “Aa”
(adduction of cords) and “Eee” (for
adduction and tension). Movements of
both the cords are compared.
Indications: Dysphonia, Hoarseness,
Foreign body sensation, Dysphagia
Structures seen on indirect laryngoscopy:
Epiglottis, arytenoid, Ring of trachea, vocal
cord, subglottis, pyriform fossa, ventricular
fold, Base of tongue, vallecular.
Station 18: Throat Instruments
Identify: Boyle-Davis mouth gag
Uses: Used for opening the mouth and retracting the
tongue anteriorly.
Indication: used for palate surgery, tonsillectomy, surgery
of soft palate, pharyngoplasty adenoidectomy, excision of
angiofibroma.
Identify: Doyen’s mouth gag
Uses: Used to keep the mouth open for intraoral surgery
when retraction of the tongue is not required or
desirable. Mostly used for tongue surgery.
Identify: Jenning’s mouth gag
Station 19: Laryngeal Papilloma
Diagnosis: Laryngeal Papillomatosis
(Juvenile Laryngeal Papillomatosis for
being more specific)
Findings: Glistering white lumpy
irregular growth, pedunculated or
sessile, bleed easily
Investigation: Direct Laryngoscope
Etiology: Viral – Human Papilloma Virus
Age group: Infants and Young Children
Give 4 Treatment Options: Interferon
Alpha 2, 13-cis-retinoic acid, CO2 Laser,
Endoscopic removal with cup forceps
Station 20: Aphthous Ulcer
Diagnosis: Aphthous Ulcer
Risk Factor: Autoimmune, Vitamin Deficiencies,
Young age
What time it takes to heal? : 2 weeks
Treatment: Self-limiting, Sometimes topical steroids
Station 21: Squamous Cell Carcinoma of Lip –
This is picture of 50 years old male patient,
chronic smoker having lesion at lip.
What is your probable diagnosis? : Squamous Cell Carcinoma
Who will you confirm your diagnosis? : Biopsy
(Histopathology)
What investigations you will advise to stage the disease? : CT
Scan head and neck with contrast
Station 22: Thudicum nasal Speculum
Identify: Thudicum Nasal Sepculum
To be Hold in: Left Hand
Used for: to examine anterior nasal cavity (Anterior
Rhinoscopy)
Structure seen: Nasal Vestibule, Nasal Septum, Inferior and
Middle Turbinate and floor of nasal cavity
Station 23: A 29 years old female patient
complaint of bilateral impairment of
hearing for the past 5 years. Examination
of tympanic membrane was normal and
tympanometry shows:
What type of Graph? : Type As tympanogram
Pathology causing this type of tympanogram:
Otosclerosis
Treatment of Otosclerosis: Stapedotomy
Station 24: Tympanogram
What Type of Tympanogram is this? : Type C
What pathology causing it? : Eustachian tube blockage (Negative
pressure in middle ear)
Station 25: Carcinoma of Tongue
Finding: Ulcer on Left lateral border of tongue –
Squamous Cell Carcinoma of Tongue
Clinical Features: Pain at lesion site, Ipsilateral Earache,
Lump in mouth, Dysphagia, Unable to protrude the
tongue
Investigations: Biopsy, MRI
Treatment: Surgery (Wide Local Excision) + Neck
Dissection
Rehab: Obturator Prosthesis
Station 26: Vocal Polyp
Identify: Polypoidal swelling at right vocal cord
Diagnosis: Vocal Polyp
Clinical Features: Hoarseness, difficulty in speech,
cough, sometime difficulty in breathing
Treatment: Micro-Laryngeal Excision
Station 27: X-Ray PNS
What X-Ray is this? : X Ray PNS
water’s view
What are the findings in this x-ray
marked with arrow? : Mucosal
Thickening in Right Maxillary Sinus
How will you manage this
patient? : Antibiotics,
Antihistamine, nasal
decongestants, anti-
inflammatory/anti-pyretic drugs
How many sinuses are visualized?
: Maxillary Sinus, Frontal Sinus,
Sphenoid Sinus
Station 28: Case of CSOM
Possible Diagnosis: Chronic Suppurative Otitis Media
Types:
Tubo-Tympanic : Without Cholesteatoma (Central Perforation)
Attico-Antral : With Cholesteatoma (Marginal Perforation)
Clinical Features:
Tubo-Tympanic: Mucopurulent Ear Discharge, Conductive Hearing Loss, Central
Perforation, Pale Polyp, Edematous and Swelled Middle Ear Mucose
Attico-Antral : Marginal perforation, retraction pocket, foul smelling discharge, Fleshy
Polyp, Hearing Loss (Conductive or Mixed)
Treatment:
Medical Management: Aural Toilet, Ear Drops, Systemic Antibiotics, Keep Ears Dry
Surgical Management: Tympanoplasty, Maryngioplasty, Cortical Mastoidectomy,
Radical Mastoidectomy, Modified Radical Mastoidectomy.
Station 29: Case of Polyp
DDx: Hypertrophied turbinate, Inverted Papilloma, Angiofibroma, Malignant Tumor
Two Types: Ethmoidal and Antro-Coanal
Ethmoidal:
Age: Common in adults
Laterality: Bilateral
Origin: Ethmoidal Sinus, Middle Turbinate, Middle Meatus
Etiology: Chronic Rhinosinusitis, Asthma, Aspirin intolerance, cystic fibrosis, Allergic
Fungal sinusitis
Investigation: CT Scan
Medical Treatment: Antihistamines, Steroids
Surgical Treatment: Polypectomy, Ethmoidectomy, Endoscopic Sinus Surgery
Antro-Coanal Polyp
Age: Common in Children
Laterality: Unilateral
Origin: Maxillary Sinus near the ostium
Etiology: Infections
Investigation: X-ray Lateral View, Posterior
Rhinoscopy
Treatment: Endoscopic Sinus Surgery, Caldwell-Luc
Operation
Station 30: Microscope from ENT OPD
Identify: ENT Microscope (Electron Microscope)
What can be seen with it? : Tympanic Membrane, External
Auditory Canal, Foreign Body, Ossicles, Middle Ear
What are the other methods to see membrane? : Otoscope,
Endoscopy, Ear Speculum
Normal Components of Membrane: Cone of Light, Umbo,
Lateral Head of Malleus, Pars Flaccida, Pars Tensa, Malleal
Folds
Station 31: Coin in Esophagus
What you see? : Foreign Body in Esophagus
Where is this foregin body? : At the level of thoracic Inlet –
C6 Cricopharynx
Clinical Features: Discomfort or Pain, Dysphagia, Drooling of
Saliva, Respiratory Distress
Complications: Respiratory Obstruction, Strictures,
Ulceration, Perioesophageal Cellulitis/Abscess
How will you remove it? : Endoscopic Removal
What other procedure if it is not deep? : Hypo-pharyngeal
speculum resembling direct laryngoscope
Station 32: Tilley’s Dressing Forceps
Identify: Tilley’s Dressing Forceps
Used for: Used for nasal packing, ear dressing, removal of
foreign bodies from the nose.
Difference b/w Septoplasty and SMR:
Septoplasty SMR
Type of Procedure Conservative Destructive
Age Any Age Adults (>17 Years)
Mucoperichondrial One Side Both Sides
Flap
Risk of Tearing Low High
Flap
Risk of Septal Low High
Perforation
Contraindications Acute Nasal or Sinus Infection, Bleeding Age Below 17, Acute
Diatheses, Untreated Diabetes and Attack of Respiratory
Hypertension Infection, Bleeding
Diatheses, Untreated
Diabetes and Hypertension
Complications: Bleeding, Septal Hematoma, Septal Abscess, Perforation, Depression of Bridge,
Toxic Shock Syndrome, Persistence of Deviation
Station 33: Myringotome
Identify: Myringotome
Used for: Used to make incison on tympanic membrane (Myringotomy)
Indications: Acute Suppurative Otitis Media, Serous Otitis Media, Aero-Otitis Media, Atelectatic
Ear
Disadvantage/Complications: Injury to Stapes, Injury to jugular bulb, Middle Ear Infection
Contraindication: Intra-tympanic Glomus Tumor
Station 34: Acute Epiglottitis Case
Diagnosis: Acute Epiglottitis
X-Ray Manifestation: Thumb’s Sign
Causative Organism: H Influenza
Differential Diagnosis: Laryngitis, Edema of Larynx, Acute
Laryngeo-tracheal Bronchitis, Foreign Body Aspiration
Clinical Findings: Sore throat, Dysphagia, Dyspnoea, Stridor,
Fever
Examination: Indirect Laryngoscopy will show edema and congestion of supraglottic structures,
Lateral View of X-ray will show thumb’s sign.
Treatment: Hospitalization, Antibiotics, Steroids, Adequate Hydration
Is tracheostomy required? : Yes, only in case of respiratory obstruction
Station 35: Case of Laryngeal Polyp – 30 year old smoker with history of
hoarseness, pedunculated mass on larynx
Diagnosis: Laryngeal Polyp
Causes: Allergy, Smoking, Vocal Abuse, Sudden shouting
Clinical Features: Hoarseness, Dyspnoea, Stridor, Intermittent Chocking, diplophonia
Investigation: Direct Laryngoscopy
Treatment: Surgical Excision
Station 36: Adenoid
Identify: adenoid mass obstructing the
nasopharyngeal airway
Structures can be seen: Cervical Spine,
Adenoids, Teeth, Skull
Pathology: Adenoid Hypertrophy
Where are adenoids? : At the junction of the
roof and posterior wall of the nasopharynx.
Function of Adenoids: Normally, in children, it
forms a soft mound in the roof and posterior
wall of the nasopharynx, just above and behind
the uvula. It provides immunity and form
antibodies.
Cause of adenoidal hypertrophy: Allergy,
Recurrent Attacks of Rhinitis, Sinusitis and
chronic tonsillitis.
Treatment: Decongestants Nasal Drops,
Antihistamine, Adenoidectomy – Removal of
Adenoids
Indication for Adenoidectomy: Adenoid
hypertrophy causing snoring, mouth breathing,
sleep apnoea syndrome or speech
abnormalities
Complications of Adenoidectomy: Hemorrhage, Injury to Eustachian tube opening, Injury to
pharyngeal musculature and vertebrae, Nasopharyngeal stenosis
At what age adenoids regress: Completely regress by age 20, while atrophy starts at puberty
Features of Adenoid Facies: An elongated face with dull expression, open mouth, prominent
and crowded upper teeth, hitched up upper lip and highly arched Hard Palate. Nose gives a
pinched in appearance.
Parts of Pharynx: Nasopharynx, Oropharynx, Hypopharynx/Laryngopharynx
Parts of Hypopharynx: Pyriform Sinus (Fossa), Posterior Pharyngeal Wall, Post-cricoid Region
Station 37: Ludwig’s Angina Case – Person with fever and mass in
submandibular area and dental infection
Possible Diagnosis: Ludwig’s Angina
Etiology: Dental Infections (80%), Submandibular Sialadenitis, injury to oral mucosa, fracture of
mandible
Organisms Involved: Mixed Infection of Aerobes and Anaerobes (Alpha-hemolytic streptococci,
Staphylococci, Bacteriods)
Investigations: Physical Examination, Blood Complete Picture
Treatment: Systemic Antibiotics, Incision and Drainage & Tracheostomy if there is airway
obstruction.
Station 38: Impedance Audiometry
Define: This is audiometry impedance, it
measures compliance of tympanic membrane
with a microphone reflects sound.
Types of tympanogram:
A—Normal
As—Reduced compliance at ambient
pressure (otosclerosis). ‘s’ stands for
shallow tympanogram but remember for
stiffness.
Ad—Increased compliance at ambient
pressure (ossicular discontinuity). ‘d’
stands for deep tympanogram.
Remember disruption of ossicular chain.
B—Flat or dome-shaped (fluid in middle ear).
C—Maximum compliance at pressures more than −200 mm H2O (negative pressure in
middle ear), e.g. eustachian tube obstruction or early stage of otitis media with effusion.
Type of Audiometry:
Subjective: Pure Tone Audiometry, Speech Audiometry
Objective: Impedance Audiometry, Brain Evoked Response Audiometry (BERA)
Define BERA: elicit brainstem responses to auditory stimulation by clicks or tone bursts. It is a
noninvasive technique to find the integrity of central auditory pathways. Done in Children
Station 39: Audiometry Graph showing conductive deafness
What is this? : Pure tone audiometry
Which type of hearing loss it is showing? : Conductive Hearing loss
Causes of Conductive hearing loss: Impacted wax, big foreign body,otomycosis, boil, tumor,
otitis media, trauma, otosclerosis, tympnosclerosis, ear drum perforation, dislocation of ear
ossicles.
Causes of sensorineural deafness: Congenital causes, genetic, labyrinthitis, perilymph fistula,
trauma to inner ear or cochlear nerve, blast injury, meniere’s disease, acoustic neuroma,
presbyacusis, ototoxicity.
Cause of Mixed Deafness: Otosclerosis
Last Resort for Patient with conductive deafness: Hearing Aid
Station 40: Septal Hematoma Case – Child with history of trauma, after 4
hours he presents with nasal obstruction and pain
Diagnosis: Septal Hematoma
Treatment: Incision and Drainage, Systemic Antibodies and Nasal Packing
Complication if left untreated: Permanent thickened septum, secondary infection causing
septal abscess, Necrosis of cartilage, Depression of nasal dorsum.
Station 41: Case of a man presenting with dysphagia, can’t swallow
saliva, high grade fever and there is grey white membrane over the
tonsils.
Diagnosis: Faucal Diphtheria
Organism causing this disease: Gram-positive bacillus, C. diphtheriae.
Treatment: Diphtheria Antitoxin, Antibiotics (Benzyl Penicillin or Erythromycin)
Complications: Myocarditis, Cardiac Arrhythmia, acute circulatory failure, Paralysis of soft
palate, paralysis of diaphragm and paralysis of ocular muscles
Station 42: Diffuse Midline Swelling of Neck
Differential Diagnosis:
Investigations: Sonogram, Ultrasound, CT, MRI, Fine Needle Aspiration
What will you if thyroid cancer is suspected? : FNAC, Ultrasound, CT, MRI, Thyroid Scan,
Thyroid Function Test
Station 43: Septal Hematoma Case
with Bilateral Red Nasal Swelling
and History of trauma 1 day back
Findings: Smooth rounded swelling in both
nasal fossae
Probable Diagnosis: Septal Hematoma
Treatment: : Incision and Drainage,
Systemic Antibodies and Nasal Packing
Complication if left untreated: Permanent
thickened septum, secondary infection
causing septal abscess, Necrosis of
cartilage, Depression of nasal dorsum.
Station 44: Laminated Picture of Enlarged Thyroid
Possible Diagnosis: Goiter
Differential Diagnosis: Iodine Deficiency, Goiter, Multinodular Goiter, Grave’s Disease, Thyroid
Adenoma
Initial Test: Ultrasound
Confirmatory Test: FNAC
Other Investigations: Thyroid Function Test, Thyroid Scan, Antibody Test, Biopsy
Station 45: Endotracheal tube
Identify: Endotracheal Tube
Define: is an emergency procedure that is often performed on people who are unconscious or
can’t breathe on their own. Given through mouth mostly but can be given through nose
Indication: To open airway to give oxygen, medication or anesthesia, For Mechanical
Ventilation, Suction in case of meconium aspiration,
Angioneuritc Edema
Complications: Mechanical Trauma to Tongue, Teeth, Palate,
Pharynx and Larynx, Pneumothorax, Pressure Necrosis,
Vasovagal Reflex
Types:
Cuffed E.Tube: For >8 Year , When Inflated maintain
E.Tube in proper position
Uncuffed E.Tube: For < 8 year, Narrow Subglottic area
prevents E.Tube form slipping
3 Ends:
Proximal: Connects to Ventilator
Central: Vocal Cord Opening
Distal: Prevents Complete blockage of E.Tube in case of secretions
Station 46: Myringotomy and Serous Otitis Media
Myringotomy: Incision in tympanic membrane to drain fluid from middle ear.
Serous Otitis Media: Accumulation of non-purulent fluid in Middle Ear Cleft
Cause: Malfunction of Eustachian Tube, Allergy, Viral Infection
DDx: Cholesteatoma, Otitis Externa, Acute Sinusitis
Clinical Findings: Hearing Impairment, Defective or Delayed Speech, Mild Earache
Otoscope Findings: Dull opaque tympanic membrane with loss of light reflex. Thin leash
of blood vessels may also be seen along the handle of malleus.
Conductive Hearing loss on tuning fork test
Treatment: Treat the underlying cause, Surgical Treatment – Myringotomy, Grommet Insertion
Station 47: Direct Laryngoscope
Identify: Direct Laryngoscope
Indication:
Diagnostic indications: 1.When indirect laryngoscopy is not possible (in infants and
young children), 2.When indirect laryngoscopy has not
been successful as in excessive gag reflex or over
hanging epiglottis obscuring a part of complete view of
larynx, 3.To examine base of tongue , valecullae, lower
part of pyriform fossa , infra hyoid epiglottis , anterior
commissure , ventricles and subglottic region, 4.To take
a biopsy and to find the extent of growth
Therapeutic indications: 1.Removal of benign lesions of
larynx (papilloma, fibroma, vocal nodule, polyp cyst),
2.Removal of foreign bodies from larynx and
hypopharynx, 3.Dilation of laryngeal strictures
Contraindications: Disease or Injury to Cervical Spine,
Respiratory Obstruction, Cardiac decompensation, Recent
coronary occlusion
Complications: Upper Airway trauma, Dental Trauma,
Aspiration
Station 48: Deviated Nasal Septum – X-ray PNS
Water’s View
Normal Structures can be seen:
Pathology: Deviated Nasal Septum
Treatment of DNS: Treatment is indicated only when it produces mechanical nasal obstruction
Septoplasty SMR
Type of Procedure Conservative Destructive
Age Any Age Adults (>17 Years)
Mucoperichondrial One Side Both Sides
Flap
Risk of Tearing Low High
Flap
Risk of Septal Low High
Perforation
Contraindications Acute Nasal or Sinus Infection, Bleeding Age Below 17, Acute
Diatheses, Untreated Diabetes and Attack of Respiratory
Hypertension Infection, Bleeding
Diatheses, Untreated
Diabetes and Hypertension
Complications of Treatment: Bleeding, Septal Hematoma, Septal Abscess, Perforation,
Depression of Bridge, Toxic Shock Syndrome, Persistence of Deviation
Which one is preferred now a days? : Septoplasty
Station 49: Barium Swallow
Name the Investigation: Barium Swallow
Purpose to do this investigation: To identify the abnormalities in Upper GI
Tract
Findings of this X-ray: Cardiac achalasia (megaoesophagus). There is a
failure of lower oesophageal sphincter to relax with dilatation of
oesophagus due to stasis of food.
Causes of Dysphagia: Esophageal Lumen Obstruction, Achalasia,
Scleroderma, Diffuse esophageal spasm, Hiatus Hernia, Hypopharyngeal
diverticulum, Thyroid Enlargement
Station 50: Pure Tone Audiogram
Type of Hearing Loss: Conductive
Causes of Conductive Hearing Loss: Congenital Atresia, Impacted wax, big
foreign body, otomycosis, boil, tumor, otitis
media, trauma, otosclerosis, tympnosclerosis,
ear drum perforation, dislocation of ear
ossicles.
Name the Procedure for External Auditory
Canal Atresia:
Types of Tympanoplasty:
Type I tympanoplasty is called
myringoplasty, and only involves the
restoration of the perforated eardrum
by grafting.
Type II tympanoplasty is used for
tympanic membrane perforations with
erosion of the malleus. It involves
grafting onto the incus or the remains of the malleus.
Type III tympanoplasty is indicated for destruction of two ossicles, with the stapes still
intact and mobile. It involves placing a graft onto the stapes, and providing protection
for the assembly.
Type IV tympanoplasty is used for ossicular destruction, which includes all or part of the
stapes arch. It involves placing a graft onto or around a mobile stapes footplate.
Type V tympanoplasty is used when the footplate of the stapes is fixed.
Station 51: Observe the Graph of 68 year old and answer the questions
Name of Investigation: Pure tone
audiometry/audiogram
These 2 lines show: Continuous line shows the
threshold of hearing of air conduction in that air
while dashed line shows the threshold for bone
conduction in that ear.
Findings in the graph: Both Bone conduction and Air
Conduction lines are below normal hearing
threshold, which is more marked in the higher
frequencies than lower frequencies. There is no
significant air-bone gap. There is sensorineural
hearing loss more marked in higher frequencies
Diagnosis: The findings are consistent with high
frequency sensorineural hearing loss. The most
probable cause is presbycusis or senile deafness.
Treatment Options: Reassurance, Hearing Aid, Auditory Rehab, Lip Reading
Station 52: Bronchoscopy
Identify: Bronchoscope
Type of Bronchoscopy:
Rigid and Flexible Fibroptic
Indication:
Diagnostic: To find
out the cause for
wheezing,
haemoptysis or
unexplained cough
persisting for more
than 4 weeks.
Collection of
bronchial
secretions for
culture and sensitivity tests, acid fast bacilli, fungus and malignant cells.
Therapeutic: Removal of Foreign Bodies or Retained secretions/mucus plug.
Complications: Injury to teeth and lips, Hemorrhage from biopsy side, Hypoxia, Cardiac Arrest,
Laryngeal edema
Station 53: Observe the graph and answer the questions
Name of Investigation: Pure Tone Audiometry
Write the meaning of two lines in the graph:
Continuous line shows the threshold of hearing of air
conduction in that air while dashed line shows the
threshold for bone conduction in that ear.
Describe the findings of this graph: Both the air
conduction and bone conduction lines are showing
normal hearing threshold i.e. up to 25 DB. There is no
significant air gap. The hearing of this person is within
normal limits.
Outline the classification of deafness according to its
severity:
Normal Hearing: Up to 25 dB
Mild deafness: 26 – 40 dB
Moderate Deafness: 41 – 55dB
Moderately Severe Deafness: 56 – 70dB
Severe Deafness: 71-90 dB
Profound deafness: >91dB
Station 54: Observe the graph and answer the questions
Name of Investigation: Pure Tone Audiometry
Describe the findings of this graph:
Air conduction line is much below the normal
threshold up to 60 dB in the lower frequencies
and up to 35 dB in the higher frequencies
Bone conduction line is in normal hearing
threshold except in 2000 Hz which is a dip,
known as Carhart’s notch.
There is conductive deafness more in the lower
frequencies.
What is the diagnosis in this patient: Findings are
typical of Otosclerosis
Enlist the treatment options in this case:
Medical Treatment: Fluoride therapy in active and cochlear Otosclerosis.
Surgical Treatment: Stapedotomy or Stapedectomy with insertion of prosthesis/piston
Hearing Aid and Rehab: In cases where surgery is not possible.
Station 55: Case of Branchial Cyst
Diagnosis: Branchial Cyst
Theories of origin: Branchial apparatus theory , cervical sinus theory , thymopharyngeal theory ,
inclusion theory
Complications: Fistula Formation, Sinus Formation
Treatment: Surgical Excision
Station 56: Case of Female 15 Year old, history of fever, Unilateral
Obstruction and Discharge, now presents with headache and epistaxis
Probable Diagnosis: Rhinolith
Investigations: Plan X-ray Nose Lateral View
Confirmatory Investigations: Clinical Examination, Water’s View X-ray
Treatment: removed under general anaesthesia. Most of them can be removed through
anterior nares. Large ones need to be broken into pieces before removal. Some particularly hard
and irregular ones require lateral rhinotomy.
Complications: Fistula Formation, Septal Perforation
Station 57: Case of a patient have pinna swelling after the trauma
Diagnosis: Hematoma Formation after the trauma
Mechanism of Hematoma Formation: Blunt trauma causes the vessels in the perichondrium to
be ruptured. Extravasated blood may clot and the organize resulting in a typical deformity called
cauliflower ear.
Complications: Perichondritis, Necrosis
Treatment: Treatment is aspiration of the haematoma under strict aseptic precautions and a
pressure dressing. When aspiration fails, incision and drainage should be done and pressure
applied by dental rolls tied with through and through sutures. All cases should receive
prophylactic antibiotics.
Station 58: Perform Indirect Laryngoscopy
Method: Patient is seated opposite the examiner. He should sit erect with the head and chest
leaning slightly towards the examiner. He is asked to protrude his tongue which is wrapped in
gauze and held by the examiner between the thumb and middle finger. Index finger is used to
keep the upper lip or moustache out of the way. Gauze piece is used to get a firm grip of the
tongue and to protect it against injury by the lower incisors. Laryngeal mirror (size 4–6) which
has been warmed and tested on the back of hand is introduced into the mouth and held firmly
against the uvula and soft palate. Light is focused on the laryngeal mirror and patient is asked to
breathe quietly. To see movements of the cords, patient is asked to take deep inspiration
(abduction of cords), say “Aa” (adduction of cords) and “Eee” (for adduction and tension).
Movements of both the cords are compared.
Indications: Dysphonia, Hoarseness, Foreign body sensation, Dysphagia
Structures seen on indirect laryngoscopy: Epiglottis, arytenoid, Ring of trachea, vocal cord,
subglottis, pyriform fossa, ventricular fold, Base of tongue, vallecular.
Can we see structures of hypopharynx through indirect laryngoscope? : No as these structures
of hidden structures of larynx which can be visualized by direct laryngoscope.
Causes of Hoarseness: Acute laryngitis, tuberculosis of larynx, papilloma, haemangioma,
chondroma, glottic carcinoma, contact ulcer, foreign bodies, intubation, paralysis of recurrent or
superior laryngeal nerve, arthritis, laryngeal web, laryngeocele.
Which carcinoma of larynx can cause hoarseness? : the glottic ca of larynx (hoarseness is the
major complain) and then the supraglottic (as hoarseness is this lesions late feature)
Station 59: Case of a patient with complaint of painful pussy ear
discharge and has fever. On examination
these were the findings
What findings can you see in this picture? : A
Large Boil in external Auditory canal
Diagnosis: Boil or Furuncle
Pathogenesis: A furuncle is a staphylococcal
infection of the hair follicle. As the hair are
confined only to the cartilaginous part of the
meatus, furuncle is seen only in this part of meatus.
Usually single, the furuncles may be multiple.
Treatment: In early cases without abscess:
systemic antibiotics, analgesics, and local heat, an
ear pack of 10% icthamol glycerin provides
splintage and reduces pain. With abscess
formation: incision and drainage.
Station 60: A School teacher presented with complain of hoarseness. On
examination there were two nodular swelling over her both vocal cords.
Diagnosis: Vocal Nodules
Causes: They are the result of vocal trauma when
person speaks in unnatural low tones for prolonged
periods or at high intensities.
Treatment: Early cases of vocal nodules can be
treated conservatively by educating the patient in
proper use of voice. Surgery is required for large
nodules or nodules of long standing in adults. They
are excised with precision under operating
microscope.
Station 61: On Otoscopy of male adult there
was foul smelling creamy debris in the ear
canal and a marginal perforation in
posterior-superior quadrant of ear drum was
seen.
Probable Diagnosis: Chronic Suppurative Otitis Media –
Atico-antral type
Investigations: Pus for Culture and Sensitivity, Pure tone
audiogram, Plain X-ray Mastoid (Law’s View), CT Scan of
Temporal Bone and Brain.
Treatment Options: Radical Mastoidectomy, Modified Radical Mastoidectomy, Cortical
Mastoidectomy and Tympanoplasty.
Station 62: A swimming champion
presented with complain of itching in
the ear. On Otoscopy, a wet bloating
paper like mass along with some
filamentous structures seen.
Diagnosis: Otomycosis
Mention the most common organism causing
this disease: Aspergillus is the most common
cause.
Investigation: Fungal Smear
Treatment: Ear Toilet, Anti-fungal, Keep Ear
Dry.
Station 63: Grommet
Name the device seen in this picture:
Grommet
Mention any two conditions while this
device neede: Acute Suppurative Otitis
media and Aero-otitis media
Вам также может понравиться
- ENTДокумент51 страницаENTBryan Paul Ramirez100% (1)
- OSCE Notes in Otology Surgery by DrtbaluДокумент85 страницOSCE Notes in Otology Surgery by DrtbaluDrAli JafarОценок пока нет
- Taking History Exam in ENTДокумент7 страницTaking History Exam in ENTLumos NoxОценок пока нет
- OSCE Review: by KP FerrarisДокумент86 страницOSCE Review: by KP Ferrarismahmoud azmyОценок пока нет
- Ent Past Years Question According To TopicsДокумент32 страницыEnt Past Years Question According To Topicsmohamed100% (1)
- ENT OSCE (Girls 1428-29)Документ9 страницENT OSCE (Girls 1428-29)Maria Monica De CastroОценок пока нет
- EntДокумент32 страницыEntaini natasha100% (3)
- ENT OsceДокумент14 страницENT OsceRj PolvorosaОценок пока нет
- 2012 ENT OSCE QuestionsДокумент4 страницы2012 ENT OSCE QuestionsFaiq Syukri Bin Saparudin50% (2)
- Ent Case 2Документ29 страницEnt Case 2Trina CardonaОценок пока нет
- Logan Turner's Diseases of the Nose, Throat and EarОт EverandLogan Turner's Diseases of the Nose, Throat and EarРейтинг: 4 из 5 звезд4/5 (2)
- Important Topics in OtologyДокумент94 страницыImportant Topics in OtologyDr. T. Balasubramanian100% (1)
- Ent Question PaperДокумент23 страницыEnt Question PaperGirish SubashОценок пока нет
- ENT NoseДокумент18 страницENT NosevkОценок пока нет
- ENTДокумент8 страницENTapi-19863548Оценок пока нет
- ENT Notes CrakДокумент52 страницыENT Notes CrakGrant KimОценок пока нет
- Round Cases (ENT) PDFДокумент9 страницRound Cases (ENT) PDFAmrAliTaha100% (2)
- ENT Lecture NotesДокумент190 страницENT Lecture NotesMizrab NadeemОценок пока нет
- Ent Solved Kmu Seqs by RMC StudentsДокумент68 страницEnt Solved Kmu Seqs by RMC StudentsAamir Khan100% (1)
- Ent ExaminationДокумент85 страницEnt ExaminationDevi Yusfita100% (1)
- 20.short Notes and Short Cases in ENT PDFДокумент116 страниц20.short Notes and Short Cases in ENT PDFpakistan100% (1)
- Osce Notes in OtolaryngologyДокумент94 страницыOsce Notes in OtolaryngologyDr. T. Balasubramanian92% (39)
- Ent Notes For PGДокумент12 страницEnt Notes For PGSHAKEEL1991Оценок пока нет
- Clinical Examination Techniques in OtologyДокумент44 страницыClinical Examination Techniques in OtologyDr. T. Balasubramanian100% (2)
- ENT Notes PDFДокумент66 страницENT Notes PDFBob Jenson100% (1)
- Clinicals ENTДокумент70 страницClinicals ENTMarrow Pg42Оценок пока нет
- ENT Paper 2Документ13 страницENT Paper 2John M. Hemsworth100% (1)
- Ent GuidelinesДокумент34 страницыEnt GuidelinesMuhammad IbrahimОценок пока нет
- E.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarДокумент3 страницыE.N.T-Otorhinolaryngology Instructions: Read Each Question Carefully and Then Select The Single Best Answer Part I: Otology/EarJohn M. Hemsworth100% (1)
- Practical View of ENTДокумент31 страницаPractical View of ENTAbouzr Mohammed ElsaidОценок пока нет
- Ent Cases MCQДокумент10 страницEnt Cases MCQDr-Firas Nayf Al-Thawabia100% (1)
- MS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionДокумент36 страницMS ENT Basic Sciences MGR University September 2009 Question Paper With SolutionDr. T. Balasubramanian67% (3)
- PT Wakode - Clinical Methods in ENT PDFДокумент171 страницаPT Wakode - Clinical Methods in ENT PDFRisya Nur Fadillah Sapitri100% (3)
- ENT Question PaperДокумент12 страницENT Question Paperasokk40% (5)
- MCQДокумент102 страницыMCQsalamred92% (13)
- MGR Medical University MS ENT Basic Sciences March 2009 Question Paper With SolutionДокумент44 страницыMGR Medical University MS ENT Basic Sciences March 2009 Question Paper With SolutionDr. T. Balasubramanian100% (4)
- Granulomatous Lesions of NoseДокумент15 страницGranulomatous Lesions of NoseDr. T. Balasubramanian100% (1)
- Osce - Nose & PnsДокумент19 страницOsce - Nose & Pnsaakash maanОценок пока нет
- Lecture On: Objective Structured Practical Examination (OSPE) in ENTДокумент34 страницыLecture On: Objective Structured Practical Examination (OSPE) in ENTEdward Smith100% (1)
- ENT Past Years CompilationДокумент7 страницENT Past Years CompilationYee Wei HoongОценок пока нет
- DOHNS Part II OSCE Glasgow May 2013Документ4 страницыDOHNS Part II OSCE Glasgow May 2013rizwan afzal100% (2)
- Otorhinolaryngology SBA'sДокумент22 страницыOtorhinolaryngology SBA'sJohn M. Hemsworth0% (1)
- Clinical Examination Techniques in Otology Edition IIДокумент43 страницыClinical Examination Techniques in Otology Edition IIDr. T. Balasubramanian100% (2)
- Endoscopic Anatomy of Nose and PNS FinalДокумент98 страницEndoscopic Anatomy of Nose and PNS FinalRahul Kurkure100% (2)
- DOHNS OSCE February 2014 LondonДокумент3 страницыDOHNS OSCE February 2014 LondonHamada Hassan Alloq100% (1)
- Osce Ear Nose N Telinga. P Throat!-From Siti Zarina. MueheheДокумент43 страницыOsce Ear Nose N Telinga. P Throat!-From Siti Zarina. MueheheiwennieОценок пока нет
- Ent NotesДокумент34 страницыEnt NotesJem JemОценок пока нет
- Dept ENT PDFДокумент117 страницDept ENT PDFPravee GaddeОценок пока нет
- Otalgia by DrtbaluДокумент13 страницOtalgia by DrtbaluDr. T. Balasubramanian100% (2)
- Ent Osce 2008Документ22 страницыEnt Osce 2008salamred100% (2)
- CSF RhinorrhoeaДокумент12 страницCSF RhinorrhoeaSuprit Sn100% (5)
- Revision Ent Instruments StyДокумент3 страницыRevision Ent Instruments StylubnatawilОценок пока нет
- Logan Turner's Diseases of the Nose, Throat and EarОт EverandLogan Turner's Diseases of the Nose, Throat and EarРейтинг: 3.5 из 5 звезд3.5/5 (4)
- Epistaxis (Nose Bleed), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandEpistaxis (Nose Bleed), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Management of Complications in Oral and Maxillofacial SurgeryОт EverandManagement of Complications in Oral and Maxillofacial SurgeryРейтинг: 2 из 5 звезд2/5 (2)
- Wa0005Документ22 страницыWa0005hassan qureshiОценок пока нет
- 18 Tonsil, Adenoid Notes Cumming Abd Key Topics (New Moe)Документ7 страниц18 Tonsil, Adenoid Notes Cumming Abd Key Topics (New Moe)osamaeОценок пока нет
- DEVS Epistaxis, Septum, & Sinonasal Tumors NewwДокумент24 страницыDEVS Epistaxis, Septum, & Sinonasal Tumors Newwyasin oumerОценок пока нет
- The Pharynx and Salivary GlandsДокумент21 страницаThe Pharynx and Salivary GlandsAce Ashley BaronОценок пока нет
- Stafilococo AureusДокумент15 страницStafilococo AureusJose MosqueraОценок пока нет
- Chapter 176. Superficial Cutaneous Infections and Pyodermas PDFДокумент36 страницChapter 176. Superficial Cutaneous Infections and Pyodermas PDFTresia SimalangoОценок пока нет
- Pigsa, Letteg Ken Busali... The Three BossДокумент8 страницPigsa, Letteg Ken Busali... The Three Bossjojazz74Оценок пока нет
- Pyoderma-NonPyoderma DR - Danny PDFДокумент89 страницPyoderma-NonPyoderma DR - Danny PDFPrayogaTantraОценок пока нет
- AbscessДокумент16 страницAbscessPlày GameОценок пока нет
- KatakatakaДокумент1 страницаKatakatakaLOUIE BORRALОценок пока нет
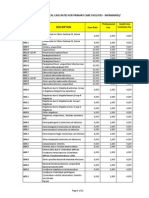
- PhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesДокумент22 страницыPhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesChrysanthus HerreraОценок пока нет
- Biological Warfare Agents - AgronДокумент129 страницBiological Warfare Agents - AgronMARK ARQUE LACANARIAОценок пока нет
- Common Bacterial InfectionsДокумент8 страницCommon Bacterial Infectionsmits98Оценок пока нет
- Infectious Dermatosis (Bacterial Skin Infections)Документ31 страницаInfectious Dermatosis (Bacterial Skin Infections)Melch PintacОценок пока нет
- Infection & Specific Wound InfectionsДокумент39 страницInfection & Specific Wound InfectionsAhmed ShorshОценок пока нет
- INFECTIONS Staphylococcal InfectionsДокумент48 страницINFECTIONS Staphylococcal InfectionsDr.P.NatarajanОценок пока нет
- 1) Localized Suppurative Inflammation: A) Abscess B) Special Type of AbscessДокумент8 страниц1) Localized Suppurative Inflammation: A) Abscess B) Special Type of AbscessAlaa SalmanОценок пока нет
- Healing PowersДокумент9 страницHealing PowersJack Key Chan AntigОценок пока нет
- FlucloxДокумент3 страницыFlucloxSultan MahmudОценок пока нет
- 2015 Handbook of TCM Herbal ApplicationsДокумент139 страниц2015 Handbook of TCM Herbal ApplicationsNANN LANG50% (2)
- Bacteriology - AmjedДокумент135 страницBacteriology - AmjedLola KhatimОценок пока нет
- Reviewer - Bacteriology FINALS - ANGELES, ANGELICДокумент38 страницReviewer - Bacteriology FINALS - ANGELES, ANGELICAngelic AngelesОценок пока нет
- FYP Proposal DraftДокумент17 страницFYP Proposal DraftKristen TeeОценок пока нет
- Identification and Classification According To Bergy's Manual of Systemic Bacteriology 2Документ46 страницIdentification and Classification According To Bergy's Manual of Systemic Bacteriology 2Cezar Alexander GuevaraОценок пока нет
- Samenvatting Infectie en InflammatieДокумент169 страницSamenvatting Infectie en InflammatiejeskevandiemenОценок пока нет
- Bacte Midterm Di TaposДокумент9 страницBacte Midterm Di TaposAL-HUSSEIN NAWABОценок пока нет
- Derm PathologyДокумент21 страницаDerm PathologyMaria GeorgeОценок пока нет
- Isolation and Identification of Microbes Responcible For Food Spoilage.Документ51 страницаIsolation and Identification of Microbes Responcible For Food Spoilage.nastaeenbaig1Оценок пока нет
- Kantor Cabang: BANJARMASIN - 1701 FKTP: Kertak Hanyar - 17040601Документ78 страницKantor Cabang: BANJARMASIN - 1701 FKTP: Kertak Hanyar - 17040601Ic-tika Siee ChuabbieОценок пока нет
- SurgeryДокумент6 страницSurgeryEthan HuntОценок пока нет
- Week 7: Canellie P. Canlas, RMT, MSMTДокумент30 страницWeek 7: Canellie P. Canlas, RMT, MSMTsophia salibaОценок пока нет
- StaphylococcusДокумент28 страницStaphylococcusAliyah SajaОценок пока нет
- Infectious DermatologyДокумент206 страницInfectious DermatologyAaron Christian Earl VillosoОценок пока нет
- Arnica Montana - FayazuddinДокумент13 страницArnica Montana - FayazuddinMohammad AtaОценок пока нет