Академический Документы
Профессиональный Документы
Культура Документы
Drug-Induced Renal Failure
Загружено:
Fiorella Mamani AceroИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Drug-Induced Renal Failure
Загружено:
Fiorella Mamani AceroАвторское право:
Доступные форматы
Drug-Induced Renal Failure: Update on New
Medications and Unique Mechanisms of
Nephrotoxicity
MARK A. PERAZELLA, MD
ABSTRACT: Medications cause renal failure through a ure. Several different drugs have been described to
variety of mechanisms. Hemodynamic renal failure may induce crystal nephropathy, including the antiparasitic
result from drugs that reduce renal prostaglandins and drug sulfadiazine, the antiviral agent acyclovir, and the
hence renal blood flow and glomerular filtration rate. A protease inhibitor indinavir. Finally, an unusual form of
relatively new group of drugs with this potential is the renal failure characterized by swollen, vacuolated prox-
cyclooxygenase-2 selective inhibitors. Direct renal tu- imal tubular cells can develop from hyperosmolar sub-
bular toxicity has also been described with a number of stances. Agents recently described to induce an “osmot-
new medications with unique effects on the epithelial ic nephrosis” include intravenous immunoglobulin and
cells of the kidney. These include the antiviral agents the plasma expander hydroxyethyl starch. KEY INDEX-
cidofovir, adefovir, and tenofovir as well as the bisphos- ING TERMS: Nephrotoxicity; Renal failure; Drugs; Med-
phonate pamidronate. Additionally, crystal deposition in ications; Crystal nephropathy; Osmotic nephrosis. [Am
the kidney may promote the development of renal fail- J Med Sci 2003;325(6):349–362.]
have been described to injure the kidney via various
T herapeutic agents have long been associated
with the development of iatrogenic renal fail-
ure. The mechanisms of drug toxicity can vary a
mechanisms of action.
great deal based on the pharmacologic action, me- Hemodynamic Renal Failure
tabolism, and ultimate pathway of excretion of the
agent administered. Altered renal hemodynamics, COX-2 Selective Inhibitors.
resulting in prerenal azotemia, is a common form of
A new class of selective nonsteroidal anti-inflam-
nephrotoxicity. It is often rapidly reversible upon
matory drugs (NSAIDs) was designed based on the
discontinuation of the culprit medication. Intrarenal
discovery of 2 cyclooxygenase (COX) isoforms
injury, especially in the renal tubular cells, may
(COX-1 and COX-2).1,2 The COX-2 selective inhibi-
result from treatment with certain types of drugs. tors are speculated to reduce end organ injury by
Nephrotoxic effects may develop in glomerular and
sparing homeostatic or “constitutive” COX-1 enzyme
tubular epithelial cells as a result of mechanisms
function.1– 4 In contrast, therapeutic effects result
that disrupt normal cellular functions (mitochon-
from the inhibition of the “inducible” COX-2 enzyme
dria, membrane integrity, etc), induce renal injury
that primarily mediates inflammatory processes.1,2
through intratubular obstruction (crystal deposi- Thus, COX-2 selective inhibitors target the produc-
tion), and promote cellular swelling and tubular tion of pro-inflammatory prostaglandins by COX-2
luminal occlusion (osmotic effects). without interrupting normal cell function mediated
This review will focus on a few new and/or unique by COX-1.1,2 This paradigm suggests that these
causes of drug-induced renal failure. It is not meant drugs can effectively reduce pain, fever and inflam-
to exhaustively review all potential agents but mation without disturbing homeostatic COX-1 en-
rather to highlight some of the medications that zyme function. In 1999, the COX-2 selective inhibi-
tors celecoxib and rofecoxib were introduced into
clinical practice to provide analgesia and anti-in-
From Section of Nephrology, Department of Medicine, Yale flammatory effects while also sparing end organ
University School of Medicine, New Haven, Connecticut. toxicity.3,4 In fact, treatment with these new drugs
Submitted November 1, 2002; accepted January 10, 2003. has resulted in therapeutic efficacy as well as a
Correspondence: Mark A. Perazella, M.D., FACP, Section of
Nephrology, Department of Medicine, Yale University School of significant reduction in gastrointenstinal toxicity.3,4
Medicine, LMP 2071, 333 Cedar Street, New Haven, CT 06520- Prostaglandins (PG) are the major products of
8029 (E-mail: mark.perazella@yale.edu). COX enzyme metabolism.5–7 The synthesis of pros-
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 349
Drug-Induced Nephrotoxicity
Table 1. Characteristics of COX-1 and COX-2 Enzymes Table 2. Clinical Syndromes Associated with Traditional
NSAIDs
COX-1 Enzyme COX-2 Enzyme
Acute
Chromosome 9 Chromosome 1 Acute vasomotor renal failure
22-kilobase gene 8-kilobase gene Hypertension, edema, CHF
Gene unresponsive to triggers Gene responds to triggers Hyponatremia
Constitutive Inducible (by cytokines, etc) Hyperkalemia/metabolic acidosis
Tissue expression Tissue expression Acute tubulointerstitial nephritis
GI tract Macrophages Acute papillary necrosis
Kidney Synoviocytes Chronic
Brain Cartilage Nephrotic syndrome (minimal change, membranous)
Vasculature Kidney Chronic papillary necrosis
Platelets Brain Analgesic nephropathy
Unchanged by Glucocorticoids Blocked by Glucocorticoids Renal cancer
GI, gastrointestinal. CHF, congestive heart failure.
taglandins from arachidonic acid is catalyzed by 2 sopressin, catecholamines] that would normally
different isomers of COX, COX-1 or COX-2 (Table 1). maintain systemic blood pressure at the expense of
These isozymes are approximately 65% identical in the renal circulation.5,6,12,13 Prostaglandin produc-
their amino acid sequences and nearly identical at tion is also increased in chronic kidney disease
their catalytic site.2,7 Conservation of their struc- (CKD).14,15 Up-regulation of PG synthesis in CKD is
tures at the catalytic site allows these isoforms to induced by intrarenal mechanisms activated to pro-
carry out similar enzymatic functions and produce mote perfusion of remnant nephrons.14,15 Impair-
similar prostaglandins. COX-1 is a 22-kilobase gene ment of PG production in this setting is associated
located on human chromosome 9, whereas the 8-ki- with short-term reductions in RBF and glomerular
lobase COX-2 gene resides on chromosome 1.2,7 The filtration rate (GFR). Renal PGs also importantly
COX isoforms can also be distinguished by their modulate salt and water homeostasis. In response to
respective patterns of gene transcription. The volume overload and salt loading, PG inhibition of
COX-2 DNA sequence identifies it as an “inducible” tubular NaCl reabsorption increases salt excre-
gene that has a number of sites that link its tran- tion.5,6,12,13 Antagonism of vasopressin effect on wa-
scription to the presence of appropriate protein trig- ter channels by these autocoids also facilitates ex-
gers, such as cytokines, growth factors, or hor- cretion of a water load.5,6,12,13 Regulation of
mones.2,7 In contrast, the gene sequence of COX-1 medullary blood flow by PGE2 also contributes to the
lacks the sites that are required to facilitate rapid kidney’s ability to modify renal solute excre-
protein transcription in response to stimuli, consis- tion.5,6,12,13 Taken together, these modulating effects
tent with a gene that expresses its constitutive prod- regulate intravascular volume status and plasma
uct protein without any prerequisite signal. The osmolality.
differences in gene regulation between the COX iso- In the same way that inhibition of COX enzyme by
mers provide a molecular basis for their purported NSAIDs produces therapeutic drug effects, disrup-
roles as “constitutive” (COX-1) and “inducible” tion of COX function also precipitates renal dysfunc-
(COX-2) enzymes. However, the COX-2 isoform is tion, leading to the well-described clinical syn-
also constitutively expressed and up-regulated in dromes of NSAID-associated nephrotoxicity (Table
the kidney and may reflect important homeostatic 2). ARF and disturbances in fluid and electrolyte
functions of this isoform.2,8 –11 Thus, the concern was balance induced by this class of drugs are the major
raised that inhibition of COX-2 may compromise acute effects of NSAIDs on the kidneys.
kidney function in a manner similar to that of tra- Despite the initial data that implied inducible
ditional NSAIDs. COX-2 formation was limited mainly to inflamma-
The major role of COX-derived prostaglandins is tory tissues, several animal models localize the
in the preservation of renal function when patho- COX-2 isoform to the healthy kidney. In fact, COX-2
logic states supervene and compromise physiologic mRNA and protein expression in the mammalian
processes in the kidney. Intravascular volume deple- kidney are among the highest observed in any tis-
tion, as seen with vomiting, diarrhea, and diuretic sues.16,17 COX-2 protein has been isolated from rat
therapy, stimulates PG synthesis to optimize renal medullary thick ascending limb cells and has been
blood flow.5,6,12,13 Also, effective decreases in renal induced by AII in cultured rat vascular smooth mus-
blood flow (RBF) as seen with congestive heart fail- cle cells.11,18,19 COX-2 has also been localized to the
ure (CHF), cirrhosis and nephrotic syndrome en- macula densa of the juxtaglomerular apparatus, the
hance compensatory PG production.5,6,12,13 PGI2 and adjacent thick cortical ascending limb cells, and to
PGE2 antagonize the local effects of circulating va- the medullary interstitial cells at the tip of the
soconstrictors [angiotensin II (AII), endothelin, va- papilla and outer medulla in rats.10,11,20 –22 Renal
350 June 2003 Volume 325 Number 6
Perazella et al
Table 3. Up-regulated Renal Expression of COX-2 Enzyme tomy specimens, providing critical insight into the
potential role of this isoform in human renal physi-
Stimulus Renal Localization ology.8 COX-2 enzyme was found in glomerular
podocytes and endothelial cells of arteries and veins
Salt restriction Renal cortex
Macula densa of these specimens. Using immunolocalization,
Thick ascending limb of Henle COX-2 expression was also demonstrated in the
ACE inhibitor/ARB Renal cortex macula densa in human kidney tissue from autopsy
Macula densa specimens procured from 10 elderly patients.31
Salt loading Renal medulla
Medullary interstitial cells COX-2 immunoreactivity was also noted in afferent
Water deprivation Medullary interstitial cells arterioles and medullary interstitial cells, with lim-
Experimental heart failure Renal medulla ited staining observed in the thick loops of Henle.
Kidney tissue from patients with Bartter-like syn-
ARB, angiotensin II receptor blocker. drome and CHF expressed COX-2 protein in the
macula densa.32 In contrast, control kidneys from
subjects without underlying renal or cardiovascular
expression of COX-2 is increased by a variety of disease did not have COX-2 protein in the macula
physiologic maneuvers (Table 3). Chronic salt re- densa, but it was detected in medullary interstitial
striction also enhanced COX-2 expression in the cells.
renal cortex and increased the number of COX-2 Evaluation of COX-2 selective inhibitors on renal
producing cells in both the macula densa and the function in human subjects has clarified the role of
adjacent thick ascending limb.10,20 Increases in rat the COX-2 isoform in the human kidney and pro-
cortical (macula densa) COX-2 expression were also vided insight into the effects of these drugs on GFR.
observed after administration of either angiotensin- Selective COX-2 and nonselective COX inhibition
converting enzyme (ACE) inhibitors or angiotensin was examined in 40 healthy male volunteers (GFR
receptor type 1 antagonists.23 In salt-restricted rats, ⬎ 100 mL/min) who were salt-restricted to induce
renin production by macula densa cells was stimu- prostaglandin dependence.33 The subjects were ran-
lated by COX-2– derived PGs; notably, renin release domized to receive 200 mg of celecoxib twice per day,
was inhibited by a COX-2–specific inhibitor.24 Salt 400 mg of celecoxib twice per day, 500 mg of
loading induced COX-2 expression in the medulla of naproxen twice per day, or placebo for 7 days. Tran-
rats, suggesting a role of this isoform in facilitating sient but clinically significant decreases in RBF (⬇
natriuresis.20 During water deprivation, COX-2 ex- ⫺100 mL/min) and GFR (⬇ ⫺20 mL/min) were
pression was stimulated to promote medullary in- noted after 1 day of therapy only in the 400-mg
terstitial cell survival during the hypertonic stress celecoxib group. Renal blood flow and GFR were
of dehydration.25,26 Finally, up-regulated expression decreased for both celecoxib and naproxen on day 7.
of medullary COX-2, but not COX-1, occurred in an A second study evaluating the effect of selective
experimental heart failure model in rats, suggesting COX-2 drugs on GFR was undertaken in a slightly
that this isoform produces PGs that maintain med- higher risk group. The renal effects of multiple doses
ullary blood flow and natriuresis in the face of de- of rofecoxib and indomethacin were studied in a
creased renal perfusion from CHF.27 group of salt-restricted elderly subjects.34 Sixty pa-
The important role of the renal COX-2 isoform and tients whose creatinine clearances ranged between
selective COX-2 inhibition in regulating RBF and 30 and 80 mL/min were randomized into 1 of 4
GFR, salt and water excretion, and renin secretion groups that received 12.5 mg of rofecoxib per day, 25
are noted in the following animal studies. Selective mg of rofecoxib per day, 50 mg of indomethacin three
COX-2 inhibition in sodium-restricted dogs pre- times per day, or placebo for 6 days. The 12.5- and
treated with norepinephrine induced a significant 25-mg rofecoxib doses significantly decreased glo-
decrease in RBF and GFR compared with dogs that merular filtration rate by 10.2 and 9.6 mL/min,
did not receive nimesulide.28 COX-2 inhibition with respectively, whereas indomethacin similarly de-
rofecoxib in rats treated with either furosemide or creased GFR by 7.8 mL/min. These data suggest
hydrochlorothiazide attenuated the diuresis and na- that salt-depleted subjects and patients with mild to
triuresis associated with these drugs compared with moderate CKD are at risk to develop a reduced GFR
rats administered vehicle.29 Celecoxib was also when treated with a COX-2 selective inhibitor, rem-
shown to raise systemic blood pressure and induce iniscent of traditional NSAID renal toxicity.
fluid retention in normotensive rats and exacerbate Clinically significant cases of nephrotoxicity from
hypertension in rats rendered hypertensive by long- COX-2 selective inhibitors have been published in
term nitric oxide inhibition.30 Thus, COX-2 stimu- the medical literature.35– 42 Celecoxib and rofecoxib
lated PGs play a key role in preserving normal were documented to cause acute renal failure (ARF)
cardiorenal physiology in animals. and hyperkalemia in 3 patients.35 It is notable that
COX-2 expression has also been demonstrated in all of these patients had multiple risk factors for
renal tissue obtained from adult human nephrec- NSAID-induced nephrotoxicity, including underly-
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 351
Drug-Induced Nephrotoxicity
ing chronic renal failure and true or “effective” vol- arteriolar tone through reduction in AII synthesis or
ume depletion. The acute deterioration in renal effect.
function returned to baseline after discontinuation
of COX-2 inhibitor and treatment of the associated Tubular Epithelial Cell Toxicity
intravascular volume disturbance. One patient re-
quired hemodialysis for severe hyperkalemia. Since As with hemodynamic renal failure, direct injury
this series of cases, several other reports of renal to the renal tubular epithelia occurs frequently after
failure and/or electrolyte disorders have been de- therapy with certain medications. This form of renal
scribed with the selective COX-2 inhibitors.36 – 42 failure is typically described as toxic acute tubular
Taken together, these cases suggest that ARF, hy- necrosis. A relatively new class of drugs employed to
perkalemia, and sodium retention can occur with treat various viral infections has been noted to have
selective COX-2 inhibitor therapy in high-risk pa- significant nephrotoxicity. The acyclic nucleoside
tients with prostaglandin-dependent disease states. phosphonates cidofovir and adefovir are antivirals
As evidenced by the expression of the COX-2 en- that possess significant nephrotoxicity. A structur-
zyme in animal and human kidneys as well as the ally similar agent, tenofovir disoproxil fumurate
current clinical data in humans, it seems that the (DF) has also been noted to cause ARF and tubular
COX-2 isoform is necessary to preserve kidney func- dysfunction. In addition, pamidronate, a drug that
tion in patients with prostaglandin-dependent has been employed widely to reduce hypercalcemia
states. The COX-2 inhibitors do not seem to have and modulate metastatic bone disease has also been
renal-sparing effects and should be considered associated with renal epithelial cell toxicity and re-
equivalently nephrotoxic as the traditional NSAIDs. nal failure. The renal effects of these drugs will be
These drugs should be used cautiously in patients reviewed.
with underlying risk for NSAID nephrotoxicity. Cidofovir, Adefovir, and Tenofovir DF. Cido-
fovir and adefovir cause direct proximal tubular
ACE Inhibitors/Angiotensin II Receptor Blockers. injury.45–51 A spectrum of injury ranging from iso-
lated proximal tubular defects (Fanconi-like syn-
Hemodynamic renal failure may also be a conse- drome) to severe acute tubular necrosis requiring
quence of therapy with medications that modulate renal replacement therapy has been described with
the renin-angiotensin system. Like NSAIDs, these both drugs.45–51 The structural similarity between
drugs precipitate a syndrome identical to prerenal these drugs and naturally occurring nucleotides is
azotemia from other causes. As a large body of lit- thought to underlie their nephrotoxic effects. Cido-
erature exists on this effect, this review will be fovir is a nucleotide analog of cytosine that forms
limited to a brief description of mechanism and risk cidofovir-phosphocholine, an analog of cytidine
factors for the development of ARF from these 5-diphosphocholine, within cells.45– 49 It is specu-
drugs.43,44 lated that cidofovir-phosphocholine interferes with
Activation of the angiotensin type 1 receptor on the normal synthesis and/or degradation of mem-
the efferent arteriole by AII raises intraglomerular brane phospholipids, resulting in proximal tubular
capillary pressure and augments GFR, particularly injury and, in extreme cases, cell necrosis. Adefovir
in situations in which where renal blood flow is is a nucleotide analog of adenine that undergoes
compromised.43 Also, AII constricts vessels in the mono and di-phosphorylation within cells.50,51 After
systemic circulation, raising arterial blood pressure phosphorylation, the analog interferes with a vari-
and promoting renal perfusion.43 In the absence of ety of ATP-related processes. Disruption of ATP
disease states that alter renal perfusion, blockade of synthesis, impairment of various ATP-dependent
AII formation or binding to angiotensin type 1 re- processes, and/or disturbed transport of adenine nu-
ceptors has little effect on renal function. Superim- cleotides in the Golgi apparatus and mitochondria
position of clinical situations that impair renal per- underlie this drug’s toxicity.50,51
fusion, such a critical renal artery stenosis, true It is apparent that the cytotoxicity of these drugs
volume contraction (vomiting, diarrhea, diuretics), for proximal tubular epithelia is related to their
effective volume depletion (cirrhosis, decompen- mode of excretion. Proximal tubular cells express an
sated heart failure, nephrosis), and severe nephro- organic anion transporter (human renal organic an-
sclerosis increase risk of hemodynamic renal failure ion transporter-1) that efficiently transports various
from ACE inhibitors and AII receptor blockers.44 acyclic nucleotide analogs, including cidofovir and
The simultaneous reduction in systemic blood pres- adefovir.52,53 This transporter resides on the baso-
sure and fall in transglomerular capillary pressure lateral membrane of proximal tubular cells and me-
(due to loss of efferent arteriolar vasoconstriction) diates active uptake of these drugs into the cells
precipitates a decline in GFR and renal failure. It from the peritubular circulation. Once these agents
seems that this effect is similar for both ACE inhib- accumulate in tubular cells, they interfere with var-
itors and AII receptor blockers, which is not unex- ious cell processes and are then secreted into the
pected, because they both ultimately blunt efferent tubular lumen via apical membrane carriers or
352 June 2003 Volume 325 Number 6
Perazella et al
channels.54,55 It is this pathway of drug elimination
by the kidney that fosters proximal tubular injury.
Based on these data, renal injury can be avoided or
reduced by employing the following guidelines.
Proper drug dosing for the prevailing level of renal
function, avoidance in patients with significant re-
nal impairment, and intravascular volume expan-
sion with intravenous fluids before drug initiation
will reduce ARF. In addition, administration of pro-
benecid, which competes with these agents for the
organic anion transporter and reduces proximal tu-
bular uptake of these analogs, decreases
nephrotoxicity.52
Tenofovir DF is a novel nucleotide analog that
also belongs to the class of acyclic nucleoside phos-
ponates.56,57 This new antiviral agent is a reverse
transcriptase inhibitor recently approved to treat
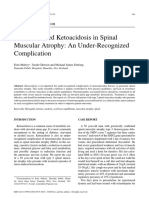
HIV infection.56,57 A few studies have documented Figure 1. Light microscopy reveals blebbing and necrosis (ar-
efficacy and safety with once daily dosing of this rows) of proximal tubular cells caused by treatment of HIV
infection with tenofovir DF.
drug.56,57 However, a persistent concern for tenofo-
vir DF is the potential for adverse renal effects. This
agent, like cidofovir and adefovir, has structural
similarities to naturally occurring nucleotides. Be- Fanconi syndrome has been reported in abstract
cause of these similarities, it is possible that tenofo- form.59 This patient developed renal disease after 4
vir DF can also interrupt cellular functions through months of therapy with tenofovir DF (300 mg/day).
the same mechanisms described for cidofovir and Renal biopsy demonstrated extensive necrosis and
adefovir. In addition, because tenofovir DF is an vacuolization of proximal tubular cells. Rapid im-
organic anion (like cidofovir and adefovir), active provement in renal function and tubular defects
uptake by the organic anion transporter in proximal occurred after discontinuation of tenofovir. These 2
tubular cells is also likely. In fact, pharmacokinetic cases suggest that administration of tenofovir DF
studies on tenofovir DF reveal that renal clearance can cause renal failure and proximal tubular injury
of the drug exceeds creatinine clearance, indicating in patients receiving the recommended dose of 300
active tubular secretion of the drug.56,57 Until re- mg per day. Patients with CKD are probably at more
cently, studies suggested that tenofovir DF is not risk and administration of tenofovir to these pa-
associated with severe nephrotoxicity.54,55 Only 1 tients should be avoided or undertaken with caution
patient of 18 who were receiving either 300 or 600 and close monitoring.
mg per day developed an increase in serum creati- Pamidronate. Pamidronate is employed fre-
nine after 35 days of therapy.57 None of the patients quently to treat malignancy-associated hypercalce-
receiving lower doses (75 and 150 mg per day) man- mia and osteolytic lesions.60 – 62 Recently, this widely
ifested a rise in serum creatinine. In yet another used bisphosphonate has been noted to cause neph-
study, evaluating tenofovir DF, 189 patients were rotoxicity in patients with multiple myeloma, meta-
randomized to placebo, 75, 150, or 300 mg per day.56 static breast cancer, and Langerhan histiocytosis.
The median serum creatinine values for the 4 orig- Dose-dependent nephrotoxicity has been previ-
inal dose groups remained constant (0.8 to 0.9 mg/ ously described in rats infused with relatively high
dL) through 48 weeks on treatment. Two patients doses (5–50 mg/kg) of pamidronate.63 High-dose
developed a 0.5 mg/dL or greater rise in serum therapy in rats was associated with an increase in
creatinine. These initial data suggested that tenofo- malate dehydrogenase, a sensitive marker of neph-
vir DF is minimally nephrotoxic. However, 2 cases of rotoxicity.63 Also, an elevation in serum urea con-
ARF and tubular injury have recently been centration was noted in these rats.63 Six patients
reported.58,59 with multiple myeloma, 1 patient with metastatic
The first patient described by Coca and Pera- breast cancer, and 1 patient with Langerhan histi-
zella58 had underlying CKD (baseline serum creati- ocytosis developed renal failure with relatively high
nine of 1.8 –2.0 mg/dL) and developed ARF after 6 doses and/or prolonged courses of pamidronate.64,65
weeks of therapy with tenofovir 300 mg per day. Doses ranging from 90 to 360 mg of pamidronate
Renal biopsy demonstrated blebbing and necrosis monthly were administered to 5 patients, whereas 1
limited to proximal tubular cells (Figure 1). Renal patient received 90 mg for 15 months, 1 received 90
function returned to baseline after discontinuation mg for 11 months, and 1 received 60 mg for 48
of tenofovir DF. A second case of tenofovir DF-asso- months. It is important to note that these patients
ciated ARF (serum creatinine of 2.2 mg/dL) and also received multiple potentially nephrotoxic che-
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 353
Drug-Induced Nephrotoxicity
Table 4. Drugs Associated with Crystal Nephropathy
Drug Type Prevention of ARF Treatment of Established ARF
Acyclovir Avoid rapid intravenous bolus Discontinue or reduce dose
Adjust dose for renal function Volume resuscitate to euvolemia
Establish euvolemia before therapy Establish high urine flow
Establish high urine flow Hemodialysis
Sulfonamides Adjust dose for renal function Discontinue or reduce dose
Establish euvolemia before therapy Volume resuscitate to euvolemia
Establish high urine flow Establish high urine flow
Alkalinize the urine (pH ⬎ 7.15) Alkalinize the urine (if possible)
Alleviate urinary obstruction
Hemodialysis
Methotrexate Adjust dose for renal function Discontinue or reduce dose
Establish euvolemia before therapy Volume resuscitate to euvolemia
Establish high urine flow Establish high urine flow
Alkalinize the urine (pH ⬎ 7.0) Alkalinize the urine (if possible)
High-flux hemodialysis
Leucovorin rescue
Indinavir Establish euvolemia before therapy Discontinue or reduce dose
Establish high urine flow Volume resuscitate to euvolemia
? Acidify the urine Establish high urine flow
Alleviate urinary obstruction
motherapeutic agents. ARF and nephrotic protein- feron-␥, driving local nephrotoxic effects in epithe-
uria developed in all patients; 5 of 8 required dialy- lial cells.64 Bisphosphonates may also promote renal
sis therapy. Renal biopsies in these patients were injury, particularly in glomerular epithelial cells,
pertinent for glomerular and tubular injury, al- through disruption of the cytoskeleton of these
though the glomerular disease was most prominent. cells.64 This effect is of particular interest given that
On light microscopy, the glomeruli exhibited collaps- disturbances in cell cycle control elements of these
ing focal and segmental glomerulosclerosis in 7 pa- cells can precipitate dedifferentiation of podocytes,
tients and minimal change in 1 patient.64,65 Exten- leading to injury and proteinuria as observed in
sive foot process effacement of the glomerular HIV-associated nephropathy.69 Patients receiving
podocytes (visceral epithelial cells) without dense either high doses or prolonged courses seem to be at
deposits on electron microscopy was present in all highest risk. Therefore, pamidronate therapy in
cases. On light microscopy, tubular changes were these patients should be regularly monitored for
diffuse and severe, with tubular atrophy, luminal changes in renal function and/or increases in uri-
ectasia, loss of brush border, cytoplasmic vacuoliza- nary protein excretion. Any change in these param-
tion, focal microcyst formation, and mild-to-severe eters should prompt discontinuation of pamidronate
interstitial fibrosis. Electron microscopy demon- and further evaluation.
strated extensive degenerative changes of the tu-
bules including epithelial simplification, loss of api- Crystal Nephropathy
cal brush border, and dilation of endoplasmic
reticulum. Immunofluorescence staining revealed Deposition of crystals in the kidneys can cause
minimal staining for C3 and IgM in 2 biopsies, with renal failure.67 The renal injury occurs from crystals
no evidence of light chain deposition. that, because of their relative insolubility in human
The literature has relatively little documentation urine, tend to precipitate in distal tubular lu-
of the nephrotoxicity of pamidronate and in general mens.70 –73 A number of routinely prescribed medi-
this drug is considered to be safe.66 – 68 The above cations (Table 4) cause crystal-induced renal dis-
reports support the notion that this drug can induce ease, termed crystal nephropathy.70 –73 Importantly,
injury in glomerular and tubular epithelial cells. characteristics common to patients who receive
The mechanism of renal epithelial cell toxicity in- these medications seem to predispose to the devel-
duced by pamidronate is speculated to involve inhi- opment of intratubular crystal deposition and tubu-
bition of ATP-dependent metabolic pathways lar obstruction.74
through incorporation of the drug into ATP ana- Among the factors that increase the likelihood of
logs.64 This effect would impair cell energetics and renal crystal deposition, severe volume contraction,
cause apoptosis and cell death. Pamidronate can from either “true” or “effective” causes, is the single
increase production of various cytokines and inter- most important.70,74 Patients who suffer from
354 June 2003 Volume 325 Number 6
Perazella et al
chronic diarrhea, anorexia with nausea/vomiting, ered clusters of echogenic material on renal
febrile illnesses, adrenal insufficiency, and renal ultrasonography in the setting of sulfadiazine
salt wasting commonly develop “true” intravascular therapy.78
volume depletion.70,74 “Effective” decreases in intra- Prevention of nephrotoxicity is possible if prompt
vascular volume will result from fluid sequestration correction of hypovolemia with an isotonic intrave-
in third-space compartments as seen with pancre- nous solution and induction of a generous diuresis
atitis, ascites, heart failure, and pleural effu- (100 to 150 mL/hour) is undertaken.75– 81 A loop
sions.70,74 These volume-related factors promote diuretic will promote high urine flow rates, with the
sluggish urine flow rates increasing the risk of crys- goal of matching fluid intake with urine output to
tal deposition within the tubules. Underlying renal achieve euvolemia. Maintaining a urine pH above
impairment is another important risk factor for the 7.15 with sodium bicarbonate increases the solubil-
development of crystal-induced ARF in these pa- ity of sulfadiazine by more than 20-fold and will
tients. Increased risk probably results from the ex- decrease crystal precipitation. Proper dosing of
posure of a fewer number of functioning nephrons to these drugs in relation to calculated GFR is also
the crystal-forming agent. Excessive drug dosing for important in the prevention of nephrotoxicity.75
the underlying glomerular filtration rate will also Daily monitoring of the urine for crystal formation
contribute to the development of ARF. Finally, met- will allow prompt adjustment of sulfadiazine dosing
abolic perturbations, including several forms of met- and more aggressive manipulation of both urinary
abolic acidoses or alkaloses, may also exacerbate pH and flow rates. In patients who have developed
intrarenal crystal deposition by causing either high ARF from sulfadiazine, treatment entails fluid re-
or low urinary pH.70,74 The importance of urine pH suscitation to achieve a vigorous diuresis in an at-
in this setting is dependent on the solubility char- tempt to clear crystals obstructing tubular lu-
acteristics of the culprit drug or endogenous crystal. mens.75– 81 Alkali therapy is reasonable if a good
As an example, medications that are weak acids urine flow rate is established. Discontinuation of the
(sulfadiazine) will precipitate in an acid urine, medication is usually required, at least initially, in
whereas a drug such as indinavir will precipitate in this setting. Occasionally, continued treatment with
an alkaline urine. sulfadiazine is tolerated with induction of high urine
Sulfadiazine. High-dose oral sulfadiazine is re- flow rates and urinary alkalinization. Ureteral cath-
quired to adequately treat infection with toxoplas- eterization or nephrostomy tube placement, followed
mosis. Therapy with sulfadiazine was 1 of the first by lavage with 5% bicarbonate solution, may dis-
therapeutic agents noted to cause crystal nephrop- solve stones in patients with total obstruction at the
athy.75– 81 Sulfadiazine is excreted in the urine (66 level of the renal pelvis or calyces.76,81 Dialysis,
%) as both parent compound and its metabolite which efficiently removes sulfadiazine may be nec-
acetylsulfadiazine.75 Because this drug is a weak essary in some cases.75
acid, it is relatively insoluble in an acid urine and Acyclovir. Intravenous acyclovir therapy is often
will tend to precipitate in tubular lumens when the required when infections with varicella zoster and
urine pH falls below 5.5.75 Precipitation in the kid- herpes simplex develop in immunocompromised pa-
neys causes obstruction of the tubular lumens in the tients. Urinary excretion of acyclovir occurs through
distal nephron from crystals admixed with cellular both glomerular filtration and tubular secre-
debris and proteinaceous material.75– 81 The admin- tion.82– 84 The drug reaches high concentrations in
istration of 4 to 6 g/day of sulfadiazine significantly the tubular lumen after the rapid clearance of acy-
increases the likelihood of sulfa-crystal precipitation clovir from the plasma. Renal excretion of un-
in the distal nephron.75– 81 Oliguric ARF, which de- changed drug accounts for approximately 62 to 91%
velops within approximately 1 week of therapy, her- of acyclovir elimination.82– 84 Acyclovir is relatively
alds the development of sulfa-crystal tubular and/or insoluble in the urine, with a maximum solubility of
calyceal deposition.75– 81 Patients are typically 2.5 mg/mL at physiologic pH.82– 84 Rapid intrave-
asymptomatic but may complain of back, flank, or nous bolus administration of acyclovir (500 mg/m2)
abdominal discomfort.75 Anywhere from less than contributes to intratubular precipitation of crys-
1% to as many as 29% of patients treated with tals.82,84,85 This combination of characteristics un-
sulfadiazine have been noted to develop ARF.75– 81 derlies the tendency for intravenous infusion of acy-
Examination of the urine sediment in these patients clovir to cause intratubular precipitation of crystals
typically reveals red blood cells mixed with a variety in the kidney. In contrast, low-dose intravenous and
of sulfadiazine crystals.75 Needle-like crystals, ro- oral acyclovir therapy are generally well tolerated;
settes, and crystals resembling “shocks of wheat” however, they can also cause ARF in the setting of
are often noted. Crystalluria has been documented severe volume depletion and excessive oral drug
to occur in up to 49% of patients infected with dosage.21,22,86,87 Animal experiments have demon-
HIV.75– 81 Sludge, calculous material, and small ra- strated acyclovir crystal deposition in collecting tu-
diolucent uroliths may also lodge in the renal paren- bules within 30 minutes of a single 50-mg intraperi-
chyma and/or calyces and appear as bilateral lay- toneal injection in mice.88 Deposition of crystals in
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 355
Drug-Induced Nephrotoxicity
tubular lumenal results in intrarenal nephron ob-
struction, whereas severe intraparenchymal precip-
itation of crystals can impinge on the renal venous
network and lead to impaired renal blood flow.83
These 2 events promote ARF.
Asymptomatic renal insufficiency is most com-
mon, but nausea/vomiting and flank or abdominal
pain will occasionally accompany renal failure.72– 84
Crystal nephropathy often develops within 24 to 48
hours of acyclovir administration. Three large series
observed a 12 to 48% incidence of acyclovir-associ-
ated renal failure.82– 84 Urinalysis usually reveals
both hematuria and pyuria, whereas birefringent
needle-shaped acyclovir crystals can also be seen in
the urine sediment with polarizing microscopy.82– 84
Although some patients require temporary dialysis,
most recover renal function with discontinuation of
acyclovir and volume resuscitation.89 Figure 2. Light microscopy reveals deposition of indinavir crys-
tals (arrows) admixed with protein in the tubular lumen of a
Prevention of acyclovir deposition in the kidneys patient treated with indinavir. The star highlights intersitial
can be accomplished by avoiding rapid bolus infu- fibrosis. [Reproduced from Reilly RF, Tray K, Perazella MA.
sion of acyclovir and infusing the drug slowly.82– 87 Indinavir nephropathy revisited: a pattern of insidious renal
Volume repletion and induction of high urinary flow failure with identifiable risk factors. Am J Kidney Dis 2001;38:
E23–E28. Copyright © 2001 WB Saunders. Used with
rates (100 to 150 mL/hour) before drug administra- permission.]
tion will also prevent crystal precipitation and sub-
sequent tubular obstruction [Table 1].82– 87 Therapy
with a loop diuretic may facilitate high urinary flow
rates, but caution to avoid volume depletion must be fected patients treated with indinavir.94 In 1 series,
employed. Importantly, a reduction in acyclovir dose urologic symptoms developed in 8% of patients
is critical in patients with underlying renal insuffi- treated with indinavir.94 In asymptomatic patients,
ciency. To this end, calculation of the proper acyclo- only abnormal serum (blood urea nitrogen, creati-
vir dose for prevailing GFR will significantly reduce nine) or urine (red and white blood cells, crystals)
acute renal impairment. Treatment of established tests provide evidence of renal injury from indinavir
renal failure includes induction of a diuresis with a crystals.94 Crystals of varying shapes including
loop diuretic to wash out obstructing crystals. Atten- platelike rectangles, fan-shaped crystals, and star-
tive supportive care, including adjustment of medi- burst forms are visualized upon examination of the
cation dosages, a restricted diet, and both metabolic urine using a lambda plate and/or polarizing light
and volume management, is required.82– 87 Hemodi- microscopy.94 Indinavir stones may be passed spon-
alysis, which removes significant amounts of acyclo- taneously or removed by urologic procedures to con-
vir, may be indicated when renal failure is severe.89 trol pain or relieve urinary obstruction.94,96 Chemi-
Indinavir. Indinavir is a protease inhibitor that cal analysis of stones reveals a composition
is employed to treat HIV infection.90 This drug has consisting of a mixture of indinavir and indinavir
recently been noted to cause crystal nephropathy, metabolites.93,94,96 Most cases of renal failure with
isolated crystalluria, and nephrolithiasis.28 –34,91–97 indinavir therapy have been mild and reversible;
Approximately 20% of the administered drug is however, more severe renal failure from obstructing
cleared by the kidneys, of which 11% is parent com- indinavir calculi and chronic kidney disease have
pound and the rest a variety of metabolites.94 Indi- also been reported.91–98
navir is very soluble at a urine pH of 3.5 (100 Indinavir therapy should be accompanied by the
mg/mL) but relatively insoluble at higher levels of daily intake of at least 2 to 3 liters of fluid by
urinary pH (0.035 mg/mL at pH 6.0; 0.02 mg/mL at patients to maintain high urinary flow rates and
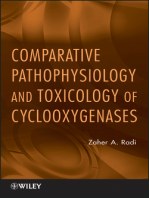
pH 7.0).92,93 Not unexpectedly, precipitation of indi- prevent crystal deposition in the kidneys.91–97 Be-
navir crystals occurs in tubular lumenae (Figure 2) cause indinavir is metabolized primarily in the liver
from the very low solubility of this drug in human through the P450III A pathway, the dose of drug
urine at a pH range of 5.5 to 7.0. Consequently, should be reduced in patients with severe hepatic
intrarenal tubular obstruction can cause acute or impairment. Acidification of the urine to a pH of 3.5
chronic renal failure.91–97 In addition, interstitial to 4.5 will improve indinavir solubility, but is ex-
fibrosis and obstructing indinavir calculi can also tremely difficult to achieve and is potentially harm-
promote impaired renal function.91,96 ful. Therefore, this form of therapy is not recom-
Classic renal colic, dysuria, back/flank pain, or mended. Discontinuation of indinavir generally
gross hematuria have been described in HIV-in- reverses nephrotoxicity; however, CKD from inter-
356 June 2003 Volume 325 Number 6
Perazella et al
stitial fibrosis has been noted with late recognition as well as the exclusion of other causes of ARF
of drug nephrotoxicity.98 Volume expansion allows supported the possibility of IVIG as the cause of
therapy with indinavir to continue safely in approx- renal insufficiency.
imately 75% of patients.94 It was observed that acute renal insufficiency af-
The deposition of crystalline material in the kid- ter this therapy developed in older patients and
neys of immunocompromised patients and those in- those with preexisting renal disease.105–124 Greater
fected with HIV is an important renal complication than 60% of patients who developed renal failure
of drug therapy. Often, patients requiring treatment were either older than 65 years of age or had renal
with culprit drugs are at highest risk to develop insufficiency (mean baseline serum creatinine was
crystal nephrotoxicity from pre-existing intravascu- 1.7 mg/dL). Unrecognized renal impairment in the
lar volume depletion, metabolic disturbances, con- elderly may have provided a predisposition to neph-
comitant nephrotoxic drug therapy, and underlying rotoxicity in this group. The daily dose of IVIG did
renal insufficiency. Recognition of at-risk physiology not seem to play a major role in the development of
in such patients can often prevent or reduce the ARF; however, a small number of patients benefited
development of crystal-induced acute renal insuffi- from either a lower dose or a longer dosing interval
ciency. Supportive care, adjustment of medication upon reintroduction of IVIG therapy after recovery
dose, and initiation of dialysis may be required in from renal failure.111,120,121
some patients. Fortunately, renal insufficiency is The clinical course of the cases of IVIG-associated
typically reversible over time. renal insufficiency seemed to follow a consistent pat-
tern. ARF developed after approximately 3 days of
Osmotic Nephrosis therapy, with a range of 1 to 10 days in the patients.
Oliguric renal failure occurred more commonly than
It has been debated whether hyperosmolar agents nonoliguric renal failure.105,107–109,111–113,116,121,123 The
can induce renal tubular injury. Induction of cell duration of renal insufficiency was approximately 2
swelling and vacuolization (causing disruption of weeks (range 3– 42 days), and renal replacement
cellular integrity) as well as tubular luminal occlu- therapy was required in one third of the pat-
sion from swollen tubular cells are the mechanisms ients.108 –111,113,119 –124 In 84% of cases, ARF was revers-
thought to underlie the development of renal failure ible, and renal function returned to baseline upon
with these agents. In the early 1940s, the demon- discontinuation of IVIG therapy. Of those patients
stration of severe swelling of proximal epithelial who did not recover renal function to baseline, 5 died,
cells was reported in patients who died of renal 2 had stable chronic renal failure, and 1 required
failure after administration of intravenous su- maintenance hemodialysis.
crose.99 This entity was given the name sucrose Several immunoglobulin preparations were used
nephropathy.99 Studies in experimental animals in the cases in which renal failure developed.105–124
performed at that time revealed that proximal tubu- However, the Sandoglobulin (Sandoz, East Hanover,
lar cell swelling could be reproducibly induced by NJ) brand of IVIG was employed in more than 80%
intravenous infusion of sucrose.100,101 Furthermore, of the cases. Notably, the stabilizing agent used in
alterations in renal function in these animals Sandoglobulin is sucrose. In contrast, most other
seemed to depend on the severity of cell swelling and immunoglobulin products employed maltose and
tubular obstruction.100,101 After these animal stud- other carbohydrates as the stabilizing agent. This
ies, this lesion was also observed with parenteral raised the suspicion that the stabilizing agent, su-
infusion of other filtered macromolecules such as crose, might play an important role in the develop-
mannitol, dextran, and radiocontrast.102,103 It was ment of acute renal insufficiency. However, the pre-
speculated that the mechanism underlying this le- dominance of cases of Sandoglobulin-associated
sion involved the uptake of nonmetabolizable mole- renal failure may be explained in part by the rela-
cules by pinocytosis into proximal cells, followed by tively frequent use of this brand of IVIG.
the accumulation of cellular water due to the oncotic Renal biopsy was performed in 10 of the cases,
gradient generated across the cell membrane.102,103 whereas a clinical diagnosis of IVIG-associated ARF
More recently, both intravenous immune globulin was made in the remaining patients. Eight of 10
(IVIG) and hydroxyethyl starch have been demon- biopsy specimens revealed a common pattern of
strated to cause an “osmotic nephrosis.” unique histopathologic lesions.107,112,113,121,125 The
IVIG. IVIG was initially introduced as a prophy- renal lesions were characterized by marked cellular
lactic therapy for infection in patients with deficien- swelling, cytoplasmic vacuolization, and degenera-
cies of immunoglobulins and a variety of immune- tion of proximal tubular epithelium. In addition,
mediated disorders.104 IVIG-associated ARF was some tubular lumina were narrowed or completely
first reported in 1987.105 Since the initial report, occluded by the swollen cells. The glomeruli were
more than 50 cases of IVIG-related acute renal in- usually spared, although 1 biopsy specimen demon-
sufficiency have been documented in the literature. strated mesangial proliferation.113 Except in 1 pa-
The temporal association of ARF with IVIG infusion tient who had an underlying IgA nephropathy,123
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 357
Drug-Induced Nephrotoxicity
immune deposits were consistently absent by both iting the dose of IVIG administered or lengthening
electron microscopy and immunofluorescent studies. the dosing interval may also benefit these patients.
Based on the available renal histopathological Hydroxyethyl Starch. Hydroxyethylstarch
studies, it seems likely that renal injury in the (HES) is an amylopectin substituted with hydroxy-
majority of patients treated with IVIG is caused by ethyl groups that is used to expand plasma volume
the uptake of sucrose into proximal tubular epithe- and improve hemodynamics in hypotensive pa-
lial cells.107,112,113,121 Cellular uptake of this filtered tients. It accomplishes this action through increas-
macromolecule results in swelling of proximal tubu- ing plasma refilling from the interstitial and intra-
lar cells, which can lead to narrowing and occlusion cellular space through its oncotic effects. An
of the tubular lumina. The evolution of structural association of nephrotoxicity with HES was noted
changes that follow an intravenous infusion of su- when renal transplant recipients who received kid-
crose has been described in experimental ani- neys from brain dead donors administered HES de-
mals.100,126 Swelling and vacuolization of tubular veloped ARF.128,129 Interestingly, the classic “osmot-
cells develop as early as 1 hour after sucrose infu- ic nephrosis” lesions described for sucrose, dextran,
sion in dogs and reach maximum severity at approx- mannitol, and IVIG were present in the biopsy spec-
imately 48 to 72 hours.100 By day 7 after infusion, imens obtained from these patients. Because of
resolution of these lesions commences and ap- these initial descriptions, however, controversy sur-
proaches completion by approximately 2 weeks. Su- rounding this association has existed based on re-
crose has been shown to enter proximal tubular cells ports refuting any connection of HES with renal
via pinocytosis, whereupon sucrose-containing pino- failure.130,131 Recently, several reports and studies
cytotic vesicles coalesce to form vacuoles that subse- provide data to support the contention that HES
quently fuse to cytoplasmic lysosomes and form therapy is associated with the development of renal
phagolysosomes.126 Because renal cells do not pos- dysfunction.
sess the enzymes necessary to digest sucrose, they Three cases of ARF ascribable only to therapy
are unable to metabolize this carbohydrate. As a with HES have been described in the postoperative
result, sucrose accumulates in the cell cytoplasm setting.132,133 Transient ARF developed after caesar-
ian section in 2 healthy female patients who re-
and leads to the progressive accumulation of cellular
ceived intravenous HES to expand intravascular
water and massive cell swelling.127
volume postoperatively.133 Another surgical patient
The mechanism that underlies IVIG-associated
who was administered HES (500 mL) for transient
ARF seems similar to the animal model of sucrose
intraoperative hypotension developed oliguric renal
nephropathy.112,113,121,122 The role of sucrose in the
failure in the postoperative period.132 Work up for
development of renal insufficiency after IVIG infu-
possible causes was negative; on day 4, the patient
sion is supported by several pieces of data. The underwent renal biopsy that demonstrated osmotic
majority of reported cases of IVIG-related ARF nephrosis-like lesions in the proximal tubules (Fig-
(83%) occur in association with Sandoglobulin ther- ure 3). A multicenter study evaluated the effects of
apy, which contains sucrose. Other IVIG prepara- HES (6%) and gelatin (3% fluid-modified) on renal
tions contain maltose and other carbohydrates and function in patients with severe sepsis.134 ARF, oli-
have rarely been associated with ARF. This occur- guria, and peak serum creatinine concentrations
rence probably relates to the fact that maltose is were significantly higher in the HES group than in
digested and metabolized by kidney cells, whereas the gelatin group. Multivariate analysis revealed
sucrose is not.122 Furthermore, patients who have that HES administration was a risk factor for ARF.
been treated with maltose-containing IVIG without Similarly, a well-matched case control study docu-
complication have subsequently developed ARF mented an increased risk for delayed graft function
when treated with sucrose-containing IVIG.107,113 in renal transplant recipients who received HES as
The clinical time course of renal failure associated a volume expander.135
with immunoglobulin therapy corresponds closely to As with IVIG, where sucrose is the osmotic agent
the rate of clearance of sucrose molecules from prox- associated with ARF and osmotic nephrosis, HES
imal tubular cells in animal studies.100,126 Finally, also seems to cause renal dysfunction through the
lesions identical to those described with sucrose development of proximal tubular swelling and vac-
nephropathy were found in 8 of 10 renal biopsy uolization (osmotic nephrosis). Like sucrose, HES in
specimens of patients treated with IVIG. taken up by proximal tubular cells, where it is not
Because sucrose seems to be the main culprit able to undergo degradation by the cell. Intracellu-
associated with the development of osmotic nephro- lar HES then generates an oncotic gradient across
sis with IVIG, a reduction in nephrotoxicity may be the cell membrane that causes intracellular accu-
achieved by avoiding IVIG which uses sucrose as a mulation of water and cellular swelling. Studies
stabilizer.122 Also, IVIG preparations containing su- where this plasma expander did not induce nephro-
crose should be used cautiously in patients with toxicity employed HES preparations with low molec-
pre-existing renal insufficiency and older age. Lim- ular weights and lower degrees of substitution
358 June 2003 Volume 325 Number 6
Perazella et al
4. Bombardier C, Laine L, Reicin A, et al. Comparison of
upper gastrointestinal toxicity of rofecoxib and naproxen in
patients with rheumatoid arthritis. N Engl J Med 2000;343:
1520 – 8.
5. Clive DM, Stoff JS. Renal syndromes associated with non-
steroidal antiinflammatory drugs. N Engl J Med 1984;310:
563–72.
6. Schlondorf D. Renal complications of nonsteroidal anti-
inflammatory drugs. Kidney Int 1993;44:643–53.
7. Smith WL, DeWitt DL. Biochemistry and prostaglandin
endoperoxide H synthase-1 and synthase-2 and their differ-
ential susceptibility to nonsteroidal anti-inflammatory
drugs. Semin Nephrol 1995;15:179 –94.
8. Komhoff M, Grone H-J, Klein T, et al. Localization of
cyclooxygenase-1 and -2 in adult and fetal human kidney:
implication for renal function. Am. J. Physiol. 1997;272:
F460 –F468.
9. Hao CM, Komhoff M, Guan Y, et al. Selective targeting of
Figure 3. Light microscopy of renal tissue obtained from patient
cyclooxygenase-2 reveals its role in renal medullary inter-
treated with hetastarch for intravascular volume resuscitation.
The straight arrows demonstrate swollen proximal tubular cells; stitial survival. Am J Physiol 1999;277:F352–F359.
the curved arrow demonstrates occlusion of the tubular lumen 10. Harris RC, McKanna JA, Akai Y, et al. Cyclooxygenase-2
from swollen cells. [Reproduced from LaBarthe AD, Jacobs F, is associated with the macula densa of rat kidney and
Blot F. Acute renal failure secondary to hydroxyethylstarch ad- increases with salt restriction. J Clin Invest 1994;94:2504 –
ministration in a surgical patient. Am J Med 2001;111:417– 8 10.
Copyright © 2001 Elsevier Science. Used with permission.] 11. Fitzpatrick FA, Soberman R. Regulated formation of
eicosanoids. J Clin Invest 2001;107:1347–51.
12. Smith WL, Lagenbach R. Why there are two cyclooxygen-
ase isozymes. J Clin Invest 2001;107:1491–5.
13. Palmer BF, Henrich WL. Clinical acute renal failure with
(number of hydroxyethylations at carbon positions nonsteroidal anti-inflammatory drugs. Semin Nephrol 1995;
C2, C3, or C6). A few practical points to reduce the 15:214 –27.
occurrence of osmotic nephrosis with HES therapy 14. Niwa T, Maeda K, Shibata M. Urinary prostaglandins
are worth noting. It seems reasonable to avoid ther- and thromboxane in patients with chronic glomerulonephri-
apy with HES in patients with pre-existing renal tis. Nephron 1987;46:281–7.
disease, to employ low-molecular-weight HES with 15. Smith WL. Prostanoid biosynthesis and mechanisms of
low degrees of substitution (HES 200/0.5) and to action. Am J Physiol 1982;263:F181–F187.
administer doses below the recommended upper 16. Breyer MD, Harris RC. Cyclooxygenase 2 and the kidney.
limit (33 mL/kg/day). Curr Opin Nephrol Hypertension 2001;10:89 –98.
17. Whelton A, Hamilton CW. Nonsteroidal anti-inflamma-
tory drugs: effects on kidney function. J Clin Pharmacol
Conclusion 1991;31:588 –98.
18. Guan Y, Chang M, Cho W, et al. Cloning, expression, and
Renal injury and clinical renal failure can occur regulation of rabbit cyclooxygenase-2 in renal medullary
through a variety of mechanisms after administra- interstitial cells. Am J Physiol 1997;273:F18 –F26.
tion of different therapeutic agents. Drug toxicity 19. Ohnaka K, Numaguchi K, Yamaka W, et al. Induction of
can develop from hemodynamic effects, direct tubu- cyclooxygenase-2 by angiotensin II in cultured rat vascular
lar injury from epithelial cell toxins, intratubular smooth muscle cells. Hypertension 1999;35:68 –75.
obstruction from insoluble crystals, and cellular 20. Yang T, Singh I, Pham H, et al. Regulation of cyclooxy-
swelling from osmotic agents. These adverse drug genase expression in the kidney by dietary salt intake. Am J
effects need to be kept in mind when evaluating the Physiol 1998;274:F481–F489.
patient who develops renal failure after therapy 21. Kester M, Coroneous E, Thomas P, et al. Endothelin
stimulates prostaglandin endoperoxide synthase-2 mRNA
with certain types of medications.
expression and protein synthesis through tyrosine kinase
signaling pathway in rat cells. J Biol Chem
References 1994;269:22574 –22580.
1. Cryer B, Feldman M. Cyclooxygenase-1 and cyclooxygen- 22. Ferreri NR, An SJ, McGiff JC. Cyclooxygenase-2 expres-
ase-2 selectivity of widely used nonsteroidal anti-inflamma- sion and function in the medullary thick ascending limb.
tory drugs. Am J Med 1998;104:413–21. Am J Physiol 1999;277:F360 –F368.
2. Crofford LJ. COX-1 and COX-2 Tissue expression: Impli- 23. Harris RC, Breyer MD. Physiological regulation of cyclo-
cations and predictions. J. Rheumatol 1997;24(Suppl 49): oxygenase-2 in the kidney. Am J Physiol Renal Physiol
15–9. 2001;281:F1–F11.
3. Siverstein FE, Faich G, Goldstein JL, et al. Gastroin- 24. Traynor TR, Smart A, Briggs JP, et al. Inhibition of
testinal toxicity with celecoxib vs. nonsteroidal anti-inflam- macula densa-stimulated renin secretion by pharmacologi-
matory drug for osteoarthritis and rheumatoid arthritis. cal blockade of cyclooxygenase-2. Am J Physiol 1999;277:
JAMA 2000;284:1247–55. F706 –F710.
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 359
Drug-Induced Nephrotoxicity
25. Yang T, Schnermann JB, Briggs JP. Regulation of cyclo- 45. Lalezari JP. Cidofovir: a new therapy for cytomegalovirus
oxygenase-2 expression in renal medulla by tonicity in vivo retinitis. J Acquir Immune Defic Syndr Hum Retrovirol
and in vitro. Am J Physiol 1999;277:F1–F9. 1997;14:S22–S26.
26. Hao CM, Yull F, Blackwell T, et al. Dehydration activates 46. Lalezari JP, Kuppermann BD. Clinical experience with
an NF-B-driven, COX2-dependent survival mechanism in cidofovir in the treatment of cytomegalovirus retinitis. J
renal medullary interstitial cells. J Clin Invest 2000;106: Acquir Immune Defic Syndr Hum Retrovirol 1997;14:S27–
973– 82. S31.
27. Abassi Z, Brodsky S, Gealekman O, et al. Intrarenal 47. Anonymous. Parenteral cidofovir for cytomegalovirus ret-
expression and distribution of cyclooxygenase isoforms in initis in patients with AIDS: the HPMPC peripheral cyto-
rats with experimental heart failure. Am J Physiol Renal megalovirus retinitis trial. A randomized, controlled trial.
Physiol 2001;280:F43–F53. Studies of Ocular complications of AIDS Research Group in
28. Llinas MT, Lopez R, Rodriguez F, et al. Role of COX-2- Collaboration with the AIDS Clinical Trials Group. Ann
derived metabolites in regulation of the renal hemodynamic Intern Med 1997;126:264 –74.
response to norepinephrine. Am J Physiol Renal Physiol 48. Lalezari JP, Holland GN, Kramer F, et al. Randomized,
2001;281:F975–F982. controlled study of the safety and efficacy of intravenous
29. Kammerl MC, Nusing RM, RichthammerW, et al. Inhi- cidofovir for the treatment of relapsing cytomegalovirus
bition of COX-2 counteracts the effects of diuretics in rats. retinitis in patients with AIDS. J Acquir Immune Defic
Kidney Int 2001;60:1684 –91. Syndr Hum Retrovirol 1998;17:339 – 44.
30. Muscara MN, Vergnolle N, Lovren F, et al. Selective 49. Meier P, Dautheville-Guibal S, Ronco PM, et al. Cido-
cyclo-oxygenase-2 inhibition with celecoxib elevates blood fovir-induced end-stage renal failure. Nephrol Dial Trans-
pressure and promotes leukocyte adherence. Br J Pharma- plant 2002;17:148 –9.
50. Cundy KC, Barditch-Crovo P, Walker RE, et al. Clinical
col 2000;129:1423–30.
31. Nantel F, Meadows E, Denis D, et al. Immunolocaliza- pharmacokinetics of adefovir in human immunodeficiency
tion of cyclooxygenase-2 in the macula densa of human virus type 1-infected patients. Antimicrob Agents Che-
elderly. FEBS Lett 1999;457:475–7. mother 1995;39:2401–5.
51. Fisher E, Brosgart C, Cohn D, et al. Safety of adefovir
32. Komhoff M, Jeck NDM, Seyberth HW, et al. Cyclooxy-
dipivoxil (ADV) and incidence of proximal tubular disorders
genase-2 expression is associated with the renal macula
(PRTD) in a placebo-controlled trial in patients with ad-
densa of patients with Bartter-like syndrome. Kidney Int
vanced HIV disease. Proceedings of the 6th Conference on
2000;58:2410 –24.
33. Rossat J, Maillard M, Nussberger J, et al. Renal effects Retroviruses and Opportunistic Infections; 1999 Jan 31–Feb
4; Chicago, Illinois. Alexandria (VA): Foundation for Retro-
of selective cyclooxygenase-2 inhibition in normotensive
virology and Human Health; 1999. [Abstract 678]
salt-depleted subjects. Clin Pharmacol Ther 1999;66:76 – 84.
52. Ho ES, Lin DC, Mendel DB, et al. Cytotoxicity of antiviral
34. Swan SK, Lasster KC, Ryan CF, et. al. Effect of cycloox-
nucleotides adefovir and cidofovir is induced by the expres-
ygenase inhibition on renal function in elderly persons re-
sion of human renal organic anion transporter 1. J Am Soc
ceiving a low-salt diet. A randomized, controlled trial Ann
Nephrol 2000;11:383–93.
Intern Med 2000;133:1–9. 53. Cihlar T, Lin DC, Pritchard JB, et al. The antiviral
35. Perazella MA, Eras J. Are selective COX-2 inhibitors
nucleotide analogs cidofovir and adefovir are novel sub-
nephrotoxic? Am J Kidney Dis 2000;35:937– 40.
strates for human and rat renal organic anion transporter 1.
36. Braden GL, O’Shea M, Mulhern J, et al. COX-2 inhibitor
Mol Pharmacol 1999;56:570 – 80.
acute renal failure: Association with hyperkalemia & type
54. Roch-Ramel F. Renal transport of organic anions. Curr
IV renal tubular acidosis [abstract]. J Am Soc Nephrol Opin Nephrol Hypertens 1998;7:517–24.
2000;11:126A. 55. Sweet D, Wolff N, Pritchard J. Expression cloning and
37. Stafford C, Bestoso JT. Celecoxib-induced acute renal characterization of ROAT1. J Biol Chem 1997;272:30088 –
failure [abstract]. J Am Soc Nephrol 2000;11:134A. 30095.
38. Perazella MA, Tray K. Selective COX-2 inhibitors: A pat- 56. Schooley RT, Ruane P, Myers RA, et al. Tenofovir DF in
tern of nephrotoxicity similar to traditional nonsteroidal antiretroviral-experienced patients: results from a 48-week,
anti-inflammatory drugs. Am J Med 2001;111:64 – 67. randomized, double-blind study. AIDS 2002;16:1257– 63.
39. Graham MG. Acute renal failure related to high-dose cele- 57. Barditch-Crovo P, Deeks SG, Collier A, et al. Phase I/II
coxib. Ann Intern Med 2001;135:69 –70. trial of the pharmacokinetics, safety, and antiretroviral ac-
40. Pfister AK, Crisalli RJ, Carter WH. Cyclooxygenase-2 tivity of tenofovir disoproxil fumarate in human immunode-
inhibition and renal function [letter]. Ann Intern Med 2001; ficiency virus-infected adults. Antimicrob Agents Che-
134:1077. mother 2001;45:2733–9.
41. Rocha JL, Fernandez-Alonso J. Acute tubulointerstitial 58. Coca S, Perazella MA. Acute Renal failure associated with
nephritis associated with the selective COX-2 enzyme inhib- tenofovir: evidence of drug-induced nephrotoxicity Am J
itor, rofecoxib. Lancet 2001;357:1946 –7. Med Sci 2002;324:342– 4.
42. Gadalean F, Barreto G, Epstein M. Acute renal failure 59. Verhelst D, Monge M, Meynard JL, et al. Fanconi syn-
induced by COX-2 specific inhibitors [abstract]. J Am Soc drome and renal failure induced by tenofovir: a first case
Nephrol 2001;12:779A. report. Am J Kidney Dis 2002;40:1331–3.
43. Navar LG, Harrison-Bernard LM, Imig JD, et al. Intra- 60. Berenson JR, Lichtenstein A, Porter L, et al. Efficacy of
renal angiotensin II generation and renal effects of AT1 pamidronate in reducing skeletal events in patients with
receptor blockade. J Am Soc Nephrol 1999;10:S266 –S272. advanced multiple myeloma. N Engl J Med 1996;334:488 –
44. Packer M, Lee WH, Medina N, et al. Functional renal 93.
insufficiency during long-term therapy with captopril and 61. Hortbagyi GN, Theriault RL, Lipton A, et al. Long-term
enalapril in severe congestive heart failure. Ann Intern Med prevention of skeletal complications of metastatic breast
1987;106:346 –55. cancer with pamidronate. J Clin Oncol 1998;16:2038 – 44.
360 June 2003 Volume 325 Number 6
Perazella et al
62. Physician’s desk reference. 54th ed. Montvale (NJ): Medical 82. Sawyer MH, Webb DE, Balow JE, et al. Acyclovir-in-
Economics Company; 2000. Pamidronate; p. 1998 –2002. duced renal failure. Clinical course and histology. Am J Med
63. Green JR, Seltenmeyer Y, Jaeggi KA, et al. Renal tol- 1988;84:1067–71.
erability profile of novel, potent bisphosphonates in two 83. Brigden D, Rosling AE, Woods NC. Renal function after
short-term rat models. Pharmacol Toxicol 1997;80:225–30. acyclovir intravenous injection. Am J Med 1982;73(Suppl
64. Markowitz GS, Appel GB, Fine PL, et al. Collapsing 1A):182–5.
focal segmental glomerulosclerosis following treatment with 84. Keeney RF, Kirk LE, Brigden D. Acyclovir tolerance in
high-dose pamidronate. J Am Soc Nephrol 2001;12:1164 – humans. Am J Med 1982;73(Suppl 1A):176 – 81.
72. 85. Bean B, Aeppli D. Adverse effects of high-dose intravenous
65. Lockridge L, Papac RJ, Perazella MA. Pamidronate- acyclovir in ambulatory patients with acute herpes zoster.
associated nephrotoxicity in a patient with Langerhan’s J Infect Dis 1985;151:362–5.
86. Giustina A, Romanelli G, Cimino A, et al. Low dose
histiocytosis. Am J Kidney Dis 2002;40:E2.
66. Rey J, Daumen-Legre V, Pham T, et al. Uveitis, an acyclovir and acute renal failure [letter]. Ann Intern Med
under-recognized adverse effect of pamidronate. Joint, 1988;108:312.
87. Eck P, Silver SM, Clark EC. Acute renal failure and coma
Bone, Spine 2000;67:337– 40.
after a high dose of oral acyclovir [letter]. N Engl J Med
67. Machado CE, Flombaum CD. Safety of pamidronate in
1991;325:1178.
patients with renal failure and hypercalcemia. Clin Nephrol
88. Dos Santos M, Dos Santos OF, Boim MA, et al. Nephro-
1996;45:175–9.
toxicity of acyclovir and ganciclovir in rats: Evaluation of
68. Ali SM, Esteva FJ, Hortobagyi G, et al. Safety and
glomerular hemodynamics. J Am Soc Nephrol 1997;8:361–7.
efficacy of bisphosphonates beyond 24 months in cancer 89. Krieble BF, Rudy DW, Glick MR, et al. Acyclovir neuro-
patients. J Clin Oncol 2001;19:3434 –7. toxicity and nephrotoxicity-the role for hemodialysis. Am J
69. Shankland SJ, Eitner F, Hudkins KL, et al. Differential
Med Sci 1993;305:36 –39.
expression of cyclin-dependent kinase inhibitors in human 90. Gulick R, Mellors J, Havlir D, et al. Treatment with
glomerular disease. Role in podocyte proliferation and mat- indinavir, zidovudine, and lamivudine in adults with Hu-
uration. Kidney Int 2000;58:674 – 83. man Immunodeficiency Virus infection and prior antiretro-
70. Berns JS, Cohen RM, Stumacher RJ, et al. Renal as- viral therapy. N Engl J Med 1997;337:734 –9.
pects of therapy for human immunodeficiency virus and 91. Tashima KT, Horowitz JD, Rosen S. Indinavir nephrop-
associated oppurtunistic infections. J Am Soc Nephrol 1991; athy (letter). N Engl J 8 Med 1997;336:138 –9.
1:1061– 80. 92. Perazella MA, Kashgarian M, Cooney E. Indinavir ne-
71. Fogazzi GB. Crystalluria: a neglected aspect of urinary phropathy in an HIV-infected patient with renal insuffi-
sediment analysis. Nephrol Dial Transplant 1996;11:379 – ciency and pyuria. Clin Nephrol 1998;50:194 – 6.
87. 93. Daudon M, Estepa L, Viard JP, et al. Urinary stones in
72. Conger JD. Acute uric acid nephropathy. Med Clin North HIV-1 positive patients treated with indinavir. Lancet 1997;
Am 1990;74:384 –92. 349:1294 –305.
73. Ogea Garcia JL, Villanueva Marcos JL, Jurado R. 94. Kopp JB, Miller KD, Mican JA, et al. Crystalluria and
Burkitt’s lymphoma and AIDS. Their presentation as tu- urinary tract abnormalities associated with indinavir. Ann
moral hepatomegaly and acute kidney failure due to tubular Intern Med 1997;127:119 –25.
deposit of urates. Ann Intern Med 1993;118:37–39. 95. Bach MC, Godofsky EW. Indinavir nephrolithiasis in
74. Perazella MA, Brown E. Electrolyte and acid-base disor- warm climates [letter]. J Acquir Immune Defic Syndr Hum
ders associated with AIDS: An etiologic review. J Gen Intern Retrovirol 1997;14:296 –7.
Med 1994;9:232– 6. 96. Berns JS, Cohen RM, Silverman M, et al. Acute renal
75. Simon DI, Brosius FC, Rothstein DM. Sulfadiazine-in- failure due to indinavir crystalluria and nephrolithiasis:
duced crystalluria revisted. The treatment of Toxoplasma report of two cases. Am J Kidney Dis 1997;30:558 – 60.
encephalitis in patients with acquired immune defiency 97. Grunke M, Valerius T, Manger B, et al. Renal dysfunc-
tion in a Human Immunodeficiency Virus-infected patient
syndrome Arch Intern Med 1990;150:2379 – 84.
76. Carbone LG, Bendixen B, Appel GB. Sulfadiazine-asso- who was treated with indinavir. Clin Infect Dis 1997;25:
ciated obstructive nephropathy occurring in a patient with 1270 –1.
98. Reilly RF, Tray K, Perazella MA. Indinavir nephropathy
acquired immune deficiency syndrome. Am J Kidney Dis
revisited: pattern of insidious renal failure with identifiable
1988;12:72–75.
risk factors. Am J Kidney Dis 2001;38:E23–E28.
77. Hein R, Brunkhorst R, Thon WF. Symptomatic sulfadi-
99. Anderson W, Bethea W. Renal lesions following adminis-
azine crystalluria in AIDS patients: A report of two cases.
tration of hypertonic solutions of sucrose. JAMA 1940;114:
Clin Nephrol 1993;39:254 – 6. 1983–7.
78. Sasson JP, Dratch PL, Shortsleeve MJ. Renal ultra- 100. Lindberg H, Wald M. Renal changes following the admin-
sound findings in sulfadiazine- induced crystalluria. Radiol- istration of hypertonic solutions. Arch Int Med 1939;63:907–
ogy 1992;185:739 – 40. 18.
79. Molina JM, Belenfant X, Doco-Lecompte T. Sulfadia- 101. Rigdon RH, Cardwell ES. Renal lesions following the
zine-induced crystalluria in AIDS patients with toxoplasma intravenous injection of hypertonic solution of sucrose: a
encephalitis. AIDS 1991;5:587–9. clinical and experimental study. Arch Int Med 1942;69:670 –
80. de Sequera P, Albalate M, Hernandez J, et al. Acute 90.
renal failure due to sulfadiazine crystalluria in AIDS pa- 102. DiScala V, Mautner W, Cohen J, et al. Tubular alter-
tients. Postgrad Med J 1996;72:557– 8. ations produced by osmotic diuresis with mannitol. Ann Int
81. Diaz F, Collazos J, Mayo J, et al. Sulfadiazine-induced Med 1965;63:767–75.
multiple urolithiasis and acute renal failure in a patient 103. Morgan T, Little J, Evans W. Acute renal failure associ-
with AIDS and Toxoplasma encephalitis. Ann Pharmacol ated with low-molecular weight dextran infusion. Brit Med
1996;30:41– 42. J 1966;2:737–9.
THE AMERICAN JOURNAL OF THE MEDICAL SCIENCES 361
Drug-Induced Nephrotoxicity
104. Anonymous. ASHP therapeutic guidelines for intravenous 122. Winward DB, Brophy MT. Acute renal failure after ad-
immune globulin. ASHP Commission on Therapeutics. Clin ministration of intravenous immunoglobulin: review of the
Pharm 1992;11:117–36. literature and case report. Pharmacotherapy 1995;15:765–
105. Barton J, Herrera G, Galla J, et al. Acute cryoglobuline- 72.
mic renal failure after intravenous infusion of gamma glob- 123. Hansen-Schmidt S, Silomon J, Keller F. Osmotic ne-
ulin. Am J Med 1987;82:624 –9. phrosis due to high dose immunoglobulin therapy contain-
106. Schifferli J, Leske M, Favre H, et al. High dose intrave- ing sucrose (but not with glycine) in a patient with immu-
nous IgG treatment and renal function. Lancet 991;337: noglobulin A nephritis. Am J Kidney Dis 1996;28:451–3.
457– 8. 124. Friedman KD, Saddler MC, Tarnover AC, et al. Tran-
107. Rault R, Piraino B, Johnston J, et al. Pulmonary and sient renal failure in a patient with idiopathic thrombocy-
renal toxicity of intravenous immunoglobulin. Clin Nephrol topenic purpura after treatment with concomitant protein-A
1991;36:83– 86. immunosorption and intravenous immune globulin. Blood
108. Ellie E, Combe C, Ferrer X. High-dose intravenous im- 1992;80(Suppl 1):483a.
mune globulin and acute renal failure. N Engl J Med 1992; 125. Tsinalis D, Dickenmann M, Brunner F, et al. Acute
327:1032–3. renal failure in a renal allograft recipient treated with
109. Stewart R, Winney R, Cash J. Renal toxicity of intrave- intravenous immunoglobulin. Am J Kidney Dis 2002;40:
nous immunoglobulin [letter]. Vox Sang 1993;65:244. 667–70.
110. Ruggeri M, Castaman G, de Narde G, et al. Acute renal
126. Schwartz SL, Johnson CB. Pinocytosis as cause of su-
failure after high-dose intravenous immune globulin in a
crose nephrosis. Nephron 1971;8:246 –54.
patient with Idiopathic Thrombocytopenic Purpura. Haema- 127. Cayco AV, Perazella MA, Hayslett JP. Renal insuffi-
tologica 1993;78:338 –9. ciency following intravenous immune globulin therapy: a
111. Pasatiempo A, Kroser J, Ruducek M, et al. Acute renal
report of two cases and analysis of the literature. J Am Soc
failure after intravenous immunoglobulin therapy. J Rheu-
Nephrol 1997;8:1788 –94.
matol 1994;21:347–9. 128. Legendre C, Thervet E, Page B, et al. Hydroxyethyl-
112. Ahsan N, Palmer B, Wheeler D, et al. Intravenous im-
starch and osmotic-nephrosis-like lesions in kidney trans-
munoglobulin-induced osmotic nephrosis. Arch Intern Med
plantation. Lancet 1993;342:248 –9.
1994;154:1985–7.
129. Cittanova ML, Lebanc I, Legendre C, et al. Effect of
113. Cantu T, Hoehn-Saric E, Burgess K, et al. Acute renal
hydroxyethylstarch in brain-dead kidney donors on renal
failure associated with immunoglobulin therapy. Am J Kid
function in kidney-transplant recipients. Lancet 1996;348:
Dis 1995;25:228 –34.
114. Poullin P, Moulen B, Ollier J, et al. Hyperoncotic renal 1620 –2.
130. Deman A, Peeters P, Sennesael J. Hydroxyethyl starch
failure after intravenous immunoglobulin therapy. Presse
does not impair immediate renal function in kidney trans-
Med 1995;24:441– 4.
115. Arunabh S, Kuman G, Avila V. Acute renal failure in- plant recipients: a retrospective, multicentre analysis.
duced by intravenous immune globulin. Am Fam Physician Nephrol Dial Transplant 1999;14:1517–20.
1996;53:862–3. 131. Bernard C, Alain M, Simone C, et al. Hydroxyethyl-
116. Corvetta A, Della Bitta R, Gabriella A, et al. Use of high starch and osmotic nephrosis-like lesions in kidney trans-
dose intravenous immunoglobulin in systemic lupus ery- plants. Lancet 1996;348:1595.
thematosus: report of three cases. Clin Exp Rheum 1989;7: 132. LaBarthe AD, Jacobs F, Blot F. Acute renal failure sec-
295–9. ondary to hydroxyethylstarch administration in a surgical
117. Rostoker G, Philippon C, Belghitti D, et al. Intravenous patient. Am J Med 2001;111:417– 8.
IgG for glomerulonephritis and renal function. Lancet 1991; 133. Dickenmann MJ, Filipovic M, Schneider MC, et al.
338:544 –55. Hydroxyethylstarch-associated transient acute renal failure
118. Kobosko J, Nicol P. Renal toxicity of intravenous immu- after epidural anaesthesia for labour analgesia and caesar-
noglobulin. Clin Nephrol 1992;37:216 –7. ean section. Nephrol Dial Transplant 1998;13:2706.
119. Phillips AO. Renal failure and intravenous immunoglobu- 134. Schortgen F, Lacherade JC, Brunner F, et al. Effects of
lin [letter]. Clin Nephrol 1992;37:217. hydroxyethylstarch and gelatin on renal function in severe
120. Donatini B. Transient renal dysfunction in diabetic pa- sepsis: a multicentre randomised study. Lancet 2001;357:
tients after IVIG therapy [letter]. J Int Med 1992;232:376. 911– 6.
121. Tan E, Hajinazarian M, Bay W, et al. Acute renal failure 135. Edwards CA, Knoll GA. Hydroxyethylstarch (HES) and
resulting from intravenous immmunoglobulin therapy. Arch the risk of delayed graft function (DGF) following renal
Neurol 1993;50:137–9. transplantation. J Am Soc Nephrol 2002;13:375–376A.
362 June 2003 Volume 325 Number 6
Вам также может понравиться
- Federal Trade Commission PBM Model OrderДокумент27 страницFederal Trade Commission PBM Model OrderHelen BennettОценок пока нет
- Case Study HIVДокумент46 страницCase Study HIVSHARNELLE FAITH C. ILAGANОценок пока нет
- NsaidДокумент29 страницNsaidAnonymous vMjb3lQOPoОценок пока нет
- Hetero Drugs ProjectДокумент74 страницыHetero Drugs ProjectJoshna IIAMОценок пока нет
- Administering Corticosteroids in Neurologic Diseases3724Документ12 страницAdministering Corticosteroids in Neurologic Diseases3724Carmen BritoОценок пока нет
- DOH Devolution Transition PlanДокумент32 страницыDOH Devolution Transition PlanMichi Go100% (1)
- Anti-Viral and Anti-Fungal AgentsДокумент212 страницAnti-Viral and Anti-Fungal Agentsmiguel cuevas100% (1)
- 2019 HIV Drug ChartДокумент5 страниц2019 HIV Drug ChartETОценок пока нет
- Art DrugsДокумент70 страницArt DrugsDr Daulat Ram DhakedОценок пока нет
- Hiv in PregnancyДокумент98 страницHiv in PregnancyAkrit DahalОценок пока нет
- Per A Zella 2003Документ14 страницPer A Zella 2003Fathanah Yanti MphОценок пока нет
- HNPДокумент10 страницHNPPattia1980Оценок пока нет
- Renal Effects of Selective Cyclo-Oxygenase-2 (COX-2) InhibitorsДокумент3 страницыRenal Effects of Selective Cyclo-Oxygenase-2 (COX-2) InhibitorsMohammedMukdadОценок пока нет
- KetorolacДокумент8 страницKetorolacwalit1101 mukrininОценок пока нет
- 01 HYP 0000115921 55353 E0-2Документ5 страниц01 HYP 0000115921 55353 E0-2marie gold sorilaОценок пока нет
- Efeitos Renais Dos Aines em CãesДокумент7 страницEfeitos Renais Dos Aines em CãesFabiana Faria LimaОценок пока нет
- Renal Effects of NSAIDДокумент8 страницRenal Effects of NSAIDtaner_soysurenОценок пока нет
- Update On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorДокумент21 страницаUpdate On The Clinical Pharmacology of Etoricoxib A Potent Cyclooxygenase2 InhibitorAnh Quoc LeОценок пока нет
- Selective COX-2 Inhibitors and Risk of Cardiovascular EventsДокумент6 страницSelective COX-2 Inhibitors and Risk of Cardiovascular EventsAditya Rahman RYОценок пока нет
- Analgesicos No Opiodes No Esteroideos y Cox SelectivosДокумент14 страницAnalgesicos No Opiodes No Esteroideos y Cox SelectivosXY PragmaОценок пока нет
- Electrolyte and Acid-Base Disturbances Associated With Non-Steroidal Anti-Inflammatory DrugsДокумент10 страницElectrolyte and Acid-Base Disturbances Associated With Non-Steroidal Anti-Inflammatory DrugsMelda Usman Al FatihОценок пока нет
- Cyclooxygenase-2 in Cardiovascular Biology: BackgroundДокумент6 страницCyclooxygenase-2 in Cardiovascular Biology: BackgroundDiego PicchioОценок пока нет
- The Cardiovascular Pharmacology of COX-2 Inhibition: Susanne Fries and Tilo GrosserДокумент7 страницThe Cardiovascular Pharmacology of COX-2 Inhibition: Susanne Fries and Tilo GrosserFernandiita de LopezОценок пока нет
- Batlouni Introduação PDFДокумент8 страницBatlouni Introduação PDFEryclisNunesОценок пока нет
- Review Article: Alleviating Promotion of Inflammation and Cancer Induced by Nonsteroidal Anti-Inflammatory DrugsДокумент18 страницReview Article: Alleviating Promotion of Inflammation and Cancer Induced by Nonsteroidal Anti-Inflammatory DrugsNadiaa MJОценок пока нет
- Walker 2017Документ18 страницWalker 2017ericdgОценок пока нет
- Lec 17Документ15 страницLec 17Abdullahayad farouqОценок пока нет
- COX-2 Inhibitors and Cardiovascular RiskДокумент3 страницыCOX-2 Inhibitors and Cardiovascular RiskelhierofanteОценок пока нет
- Cox 2 DocumentДокумент29 страницCox 2 DocumentLanggeng Perdhana Jangan MenyerahОценок пока нет
- Selective COX-2 Inhibitors: A Review of Their Structure-Activity RelationshipsДокумент30 страницSelective COX-2 Inhibitors: A Review of Their Structure-Activity RelationshipsMona SalihОценок пока нет
- kadlec et al 2016 role of pgc 1α in vascular regulationДокумент8 страницkadlec et al 2016 role of pgc 1α in vascular regulationKhairunnisa NsОценок пока нет
- Cox 2 InhibitorsДокумент9 страницCox 2 InhibitorsirlandagarandaОценок пока нет
- Risk PDFДокумент50 страницRisk PDFErick Antonio Castillo GurdianОценок пока нет
- Renal Medullary Interstitial COX-2 Is Essential in Preventing Saltsensitve Hypertension and Maintaining Renal Inner MedullaДокумент17 страницRenal Medullary Interstitial COX-2 Is Essential in Preventing Saltsensitve Hypertension and Maintaining Renal Inner MedullaMumtaz Maulana HidayatОценок пока нет
- Pharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Документ9 страницPharmacology - Anti-Inflammatory Drugs - Corticosteroid, NSAID, Leukotriene (Eicosanoids)Itharshan IndreswaranОценок пока нет
- Pharmacology of MeloxicamДокумент9 страницPharmacology of MeloxicamkwadwobrosОценок пока нет
- Ars 2016 6664Документ28 страницArs 2016 6664Irvin MarcelОценок пока нет
- COX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsДокумент4 страницыCOX-2 Selectivity Alone Does Not de Ne The Cardiovascularrisks Associated With Non-Steroidal Anti-In Ammatory DrugsruleshellzОценок пока нет
- AssignmentДокумент8 страницAssignmentAbdullah MahmoudОценок пока нет
- Update On The Use of Cyclooxygenase-2-Selective Nonsteroidal Anti-Inflammatory Drugs in Horses Review ArticleДокумент4 страницыUpdate On The Use of Cyclooxygenase-2-Selective Nonsteroidal Anti-Inflammatory Drugs in Horses Review ArticleSusanaОценок пока нет
- 1 SajaДокумент11 страниц1 SajaAbduh RijalОценок пока нет
- Anti-Inflammatory Drugs OPB AY1415Документ40 страницAnti-Inflammatory Drugs OPB AY1415Mohammad Hazamyn Hazrul HamzahОценок пока нет
- NSAID Nephropathy and COX-2 Inhibitors: Kellie A Goldsborough, MD Resident Grand Rounds November 2, 1999Документ49 страницNSAID Nephropathy and COX-2 Inhibitors: Kellie A Goldsborough, MD Resident Grand Rounds November 2, 1999Galon AirnyaОценок пока нет
- Farmakodinamika NSAID's TДокумент43 страницыFarmakodinamika NSAID's TDantiОценок пока нет
- Nsaids and Kidney: P Ejaz, K Bhojani, VR JoshiДокумент9 страницNsaids and Kidney: P Ejaz, K Bhojani, VR JoshiSatrio AjieОценок пока нет
- Nonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualДокумент12 страницNonsteroidal Anti-Inflammatory Drugs in Animals - Pharmacology - MSD Veterinary ManualFairuz Nanda MarhabanazОценок пока нет
- LipidsignalingaДокумент2 страницыLipidsignalingaMike GОценок пока нет
- Selective Cox-2 Inhibitor: Visha.M.GДокумент6 страницSelective Cox-2 Inhibitor: Visha.M.GinventionjournalsОценок пока нет
- Side Effects of NSAIDsДокумент8 страницSide Effects of NSAIDsAlmas PrawotoОценок пока нет
- Cyclo-Oxygenase 1 & 2 - A Brief Overview, and Their InhibitorsДокумент5 страницCyclo-Oxygenase 1 & 2 - A Brief Overview, and Their InhibitorsSandipan SahaОценок пока нет
- Using N, N, N',N'-tetramethyl-p-phenylenediamine (TMPD) To Assay Cyclooxygenase Activity in VitroДокумент13 страницUsing N, N, N',N'-tetramethyl-p-phenylenediamine (TMPD) To Assay Cyclooxygenase Activity in VitroTatianaAlejandraCárdenasSolanoОценок пока нет
- 7 31 34 Ijprbs 76.7Документ13 страниц7 31 34 Ijprbs 76.7hanifa lestariОценок пока нет
- Expression of Advanced Glycation End Products and TheirДокумент11 страницExpression of Advanced Glycation End Products and TheirTamam JauharОценок пока нет
- Clinical Pharmacology of Non Steroidal A20151118 17879 2qewjq WithДокумент14 страницClinical Pharmacology of Non Steroidal A20151118 17879 2qewjq WithAli KareemОценок пока нет
- Mechanisms Underlying The Cardiovascular Effects of COX-InhibitionДокумент14 страницMechanisms Underlying The Cardiovascular Effects of COX-InhibitionRangwani NesbitОценок пока нет
- (03241750 - Acta Medica Bulgarica) Renal Changes in Cocaine Abuse and AddictionДокумент5 страниц(03241750 - Acta Medica Bulgarica) Renal Changes in Cocaine Abuse and AddictionTeodorОценок пока нет
- Endothelial Dysfunction in Type 2 Diabetes MellitusДокумент7 страницEndothelial Dysfunction in Type 2 Diabetes MellitusKwame YeboahОценок пока нет
- Nsaid PDFДокумент38 страницNsaid PDFسامر الرفاعيОценок пока нет
- N A - D (Nsaid) : Onsteroidal NTI Inflammatory Rugs SДокумент43 страницыN A - D (Nsaid) : Onsteroidal NTI Inflammatory Rugs STes B FourieОценок пока нет
- Podocyte Injury and Its Consequences: Michio NagataДокумент10 страницPodocyte Injury and Its Consequences: Michio Nagatablume diaОценок пока нет
- Review Article: Ijprbs Chirag Modi, IJPRBS, 2012: Volume1 (3) : 120-132Документ13 страницReview Article: Ijprbs Chirag Modi, IJPRBS, 2012: Volume1 (3) : 120-132Uci Ramadhanty D3 2018Оценок пока нет
- Nonsteroidal Antiinflammatory DrugsДокумент12 страницNonsteroidal Antiinflammatory DrugsAlano S. LimgasОценок пока нет
- Study of Osteoarthritis Treatment With Anti-InflammatoryДокумент11 страницStudy of Osteoarthritis Treatment With Anti-InflammatoryDezha DetiroОценок пока нет
- NsaidsДокумент16 страницNsaidsraffia mahakОценок пока нет
- PainoxiaДокумент66 страницPainoxiaOmar WahbiОценок пока нет
- Cardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health IssueДокумент12 страницCardiovascular Risk of Nonsteroidal Anti-Inflammatory Drugs: An Under-Recognized Public Health IssueAri Dwi PrasetyoОценок пока нет
- Stress-Induced Ketoacidosis in Spinal Muscular Atrophy: An Under-Recognized ComplicationДокумент5 страницStress-Induced Ketoacidosis in Spinal Muscular Atrophy: An Under-Recognized ComplicationMabvan SarraОценок пока нет
- HIV/AIDS OverviewДокумент4 страницыHIV/AIDS OverviewAji Deonella Tangcangco CruzОценок пока нет
- Drug Name Mechanism of Action Indication Contraindications Side Effects/Adverse Effects Nursing ConsiderationДокумент5 страницDrug Name Mechanism of Action Indication Contraindications Side Effects/Adverse Effects Nursing ConsiderationWyeth Earl Padar EndrianoОценок пока нет
- Drug Induced Acute Kidney Injury.19 PDFДокумент14 страницDrug Induced Acute Kidney Injury.19 PDFJose santos MembreñoОценок пока нет
- 2013 Pipeline ReportДокумент295 страниц2013 Pipeline ReportLIONtescuОценок пока нет
- Agbaji, Oche O., Et Al. 2019Документ9 страницAgbaji, Oche O., Et Al. 2019priya panaleОценок пока нет
- Elias, Adikwu, Et Al. 2014Документ15 страницElias, Adikwu, Et Al. 2014priya panaleОценок пока нет
- Tacke2016 - Treatment For Hepatitis B in Patients With Drug ResistanceДокумент7 страницTacke2016 - Treatment For Hepatitis B in Patients With Drug ResistanceClarisa AnindyaОценок пока нет
- TENOFOVIR (Tenofovir Disoproxil, Tenofovir Disoproxil Fumarate)Документ1 страницаTENOFOVIR (Tenofovir Disoproxil, Tenofovir Disoproxil Fumarate)maeОценок пока нет
- Gilead and The Pharmasset Deal: A Case StudyДокумент27 страницGilead and The Pharmasset Deal: A Case StudyMarcus DeMasterОценок пока нет
- Treatment Considerations, and Nursing Implications: Cardiovascular Disease and HIV: PathophysiologyДокумент12 страницTreatment Considerations, and Nursing Implications: Cardiovascular Disease and HIV: PathophysiologyRicardo Costa da SilvaОценок пока нет
- Maternity Care Guidelines - 24 November 2023Документ266 страницMaternity Care Guidelines - 24 November 2023KhodaniОценок пока нет
- Product Monograph Atripla (Emtricitabine - Tenofovir D. F. - Efavirenz)Документ70 страницProduct Monograph Atripla (Emtricitabine - Tenofovir D. F. - Efavirenz)tartaruga_tartarugaОценок пока нет
- HBVGuidance Terrault Et Al-2018-Hepatology PDFДокумент40 страницHBVGuidance Terrault Et Al-2018-Hepatology PDFAnonymous wdmpgxОценок пока нет
- Hepatitis B: DR Tanmay Vyas (DM Hepatology)Документ37 страницHepatitis B: DR Tanmay Vyas (DM Hepatology)Sreekanth VattikondaОценок пока нет
- MedicinesДокумент32 страницыMedicinesValdez, Kaycee M.Оценок пока нет
- Baraclude: Generic Name: Entecavir 0.5 MG PO OD Antiviral AgentДокумент8 страницBaraclude: Generic Name: Entecavir 0.5 MG PO OD Antiviral AgentPatricia Jean FaeldoneaОценок пока нет
- FDA - HIV and AIDS Activities - Antiretroviral Drugs Used in The Treatment of HIV InfectionДокумент5 страницFDA - HIV and AIDS Activities - Antiretroviral Drugs Used in The Treatment of HIV InfectionMade YudanaОценок пока нет
- 89aced9f 1Документ60 страниц89aced9f 1Cao Minh TríОценок пока нет
- HIV - LancetДокумент13 страницHIV - LancetcristhianldsОценок пока нет
- HIV/AIDS Symptoms and SignsДокумент3 страницыHIV/AIDS Symptoms and SignsAmin MofrehОценок пока нет
- Wasting Away - Solomon2014Документ8 страницWasting Away - Solomon2014Владимир ДружининОценок пока нет
- HIV Infectious DiseasesДокумент50 страницHIV Infectious Diseasesabdul qayyumОценок пока нет