Академический Документы
Профессиональный Документы
Культура Документы
Blood Pharmacology PDF
Загружено:
Manikanta GupthaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Blood Pharmacology PDF
Загружено:
Manikanta GupthaАвторское право:
Доступные форматы
st
Pharmacology 3.2 1 Sem/A.Y. 2015-2016
Hematinics, Hemostatics and Coagulants
Glenn V. Guevara, MD September 11, 2015
OUTLINE B. Erythropoiesis
A. Introduction
B. Anemia
C. Iron Deficiency Anemia
D. Hypoproliferative Anemia
E. Megaloblastic Anemia
F. Myelopoiesis
G. Megakaryopoiesis
H. Hemostasis
I. Summary
HEMATINICS, HEMOSTATICS AND COAGULANTS
A. INTRODUCTION
A. Hematopoiesis Figure 2: Erythropoiesis
Erythropoietin: main regulator of erythropoiesis
o Stimulate hematopoietic stem cells from the bone
marrow to form RBCs
o Released by kidneys in response to low O2 tension
o Factors that decrease tissue oxygenation: low blood
pressure, anemia, low hemoglobin, poor blood flow,
pulmonary disease
o Increased number of RBCs results to an increased O2
carrying capacity, inducing a negative feedback on
EPO
Figure 3: Erythropoietin stimulation and inhibition
Iron: needed for maturation of red blood cells
Figure 1: Hematopoiesis o Each RBC contains several hundred hemoglobin
molecules which transport oxygen
o Iron is needed for the production of heme
Formation of blood components
Cobalamin
o Erythropoiesis: formation of RBCs
o Myelopoiesis: formation of granulocytes and Folic Acid
monocytes
o Megakaryopoiesis: formation of platelets B. ANEMIA
Derived from hematopoietic stem cells Decrease in the amount of RBCs or hemoglobin in the
blood
Leads to lowered ability of blood to carry oxygen
Causes:
o Blood loss (most common cause): trauma, GI
bleeding, abnormal menstrual bleeding
o Decreased RBC production
Nutrient deficiency (iron, cobalamin, folic acid);
most common cause among decreased RBC
production
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 1OF13
Pharmacology 3.02
Thalessemia
Bone marrow cancers Hematocrit (Hct)
Kidney disease
Chronic infections Male 45 %
Fluid overload- decrease in RBC production due to Female 40 %
volume expansion Hgb Count
Increased RBC breakdown- Sickle Cell Disease
Male 13.8 to 18.0 g/dl (8.56-11.17
Types of Anemia mmol/L)
o By size: normocytic, macrocytic, microcytic Female 12.1 to 15.1 g/dl (7.51-9.37 mmol/L)
o By color: normochromic, hypochromic, hyperchromic Children 11-16 g/dL (6.83-9.93 mmol/L)
Pregnant 11-14 g/dL (6.83-9.93 mmol/L)
RBC Count
Signs and Symptoms
Male 4.7-6.1 millions/uL
Female 4.2-5.4 millions/uL
MCV 80-100 fl (femtoliters)
MCH 27-31 pg/cell (picograms)
MCHC 32-36 g/dL or 19.9-22.3 mmol/L
Table 1: Normal values for CBC
C. IRON DEFICIENCY ANEMIA
Most common cause of anemia
Due to increased iron demand, iron loss or decreased
iron intake
More common in females (so take care and love your mom, sisters,
daughters and girlfriends, boys. There are a lot of illnesses associated
with women.)
Microcytic and hypochromic
Causes:
Increased demand
o Growth and development – children, adolescents
o Pregnancy
Figure 4: Shows a somewhat good looking man with a
creepy gaze. Also shown are the General Signs and Blood loss
Symptoms of Anemia. o Parasitic infections
o Menorrhagia
Diagnostic Tests o Peptic ulcers
o Hemoglobin Count – hemoglobin concentration o Patients on anticoagulants (aspirin, clopidogrel, etc)
o Hematocrit - proportion of blood volume occupied by
RBC; also called "packed cell volume" or "erythrocyte Decreased intake
volume fraction" (about 3x the Hgb concentration) o Low iron diet: vegetarians, vegans
o RBC Count – number of RBC o Malabsorption: intestinal resection, celiac disease,
o Mean Corpuscular Volume (MCV) inflammatory bowel disease, decreased acidity of
Average volume or size of RBC stomach (due to prolonged proton pump inhibitor use,
MCV = (Hct x 10) / RBC number in million e.g. omeprazole)
Normal MCV and decreased Hgb/Hct =
normocytic anemia; low MCV = microcytic and A. Diagnostic Tests
(Why do we need to know this? Kinda boring but just see yourself as House,
vice versa Shepherd, Yang or Grey diagnosing your anemia patient. Wee!)
o Mean Corpuscular Hemoglobin (MCH)
Average mass of hemoglobin per RBC in a CBC (see diagnostic tests of anemia)
sample of blood
Assess COLOR of the ANEMIA Serum iron
MCH = (Hgb x 10) / RBC number in million It is the amount of circulating iron bound to transferrin
o Mean Corpuscular Hemoglobin Concentration It can increase immediately on initiation of Fe
(MCHC) supplementation
Concentration of hemoglobin in a volume of packed
RBC – the HUE OF RBC Serum ferritin
MCHC = MCH/MCV x 100 Most SENSITIVE indicator but is not reliable if within
This is more sensitive for measuring the actual
normal limits
color because it considers both MCV and MCH
Remember that ferritin is the storage form of iron
o Blood Smear – morphology of RBCs
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 2OF13
Pharmacology 3.02
Total Iron Binding Capacity (TIBC)
Most SPECIFIC indicator (when levels are high)
It measures the blood capacity to bind iron with
transferrin. It is an indirect measure of transferrin
Transferrin is the transporter of iron in the blood. An
increase would point to an increased need for iron
(2017B)
It is usually elevated in IDA
Transferrin Saturation Index (Percent Saturation/ Iron
Saturation)
It is the percent saturation or iron saturation of
transferrin
How much iron is currently bound to transferrin
(2017B)
SI/TIBC x100
Table 2: Normal values
Serum Iron
Male 65-176 μg/dL
Female 50-170 μg/dL
Children 50-120 μg/dL
Figure 5: Increasing severity of iron imbalance up to Iron
Newborn 100-250 μg/dL
Deficiency Anemia. Note the boxes in green, which indicate
Serum Ferritin which stage would the first time the lab findings will appear
Male 18-270 ng/mL (2017B). As the disease progresses, the other parameters that
Female 18-160 ng/mL were normal become lower.
Children 7-140 ng/mL With a Negative Iron Balance, bone marrow iron stores,
Newborn 25-200 ng/mL serum ferritin decrease while TIBC increases.
Total Iron Binding Capacity 240-450 μg/dL With Iron Deficient Erythropoiesis, also SI, % saturation,
Transferrin Saturation Index marrow sideroblasts decrease while RBC
Male >15-50%
protoporphyrin increases.
Female >12-50%
With IDA (which is severe), there is also morphological
Still Possible 5-10%
change in the RBC
Definitely Abnormal <5%
Table 3: Differentiating microcytic anemia causes via lab
tests. These are the different diseases that can present with
microcytic anemia but focus your attention on IDA. There’s a
lower serum iron, % saturation, and serum ferritin but a higher
TIBC. If you order for a smear in IDA patients, you’d see a
microcytic & hypochromic morphology.
Tests Iron Inflammation Thalassemia Sideroblastic
Deficiency
Smear Micro/hypo N/micro/hypo Micro/hypo w/ Variable
targeting
Serum Iron <30 <50 (N) to high (N) to high
TIBC >360 <300 (N) (N)
%saturation <10 10-20 (N) 30-80 30-80
Ferritin <15 30-200 (N) 50-300 50-300
Hemoglobin (N) (N) Abnormal (N)
Figure 6: Hemoglobin Synthesis. Protoporphyrin IX is the
step before heme. When it binds to iron, then there is the
formation of heme. If there is an increase in protoporphyrin if
there is no iron available in circulation. Thus no heme is formed.
In severe forms of iron deficiency anemia, you see a lot of
immature RBC in the blood. Thus, you’ll need iron
supplementation to normal it out.
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 3OF13
Pharmacology 3.02
B. Iron Ferrous fumarate- usually combined with
In 1 mL of RBC, you will get 1 mg iron multivitamins like folic acid and Vit-B complex
Daily need: 15-20 mg/day (of elemental iron) due to 10- To reverse the anemia
15% absorption of dietary iron o You need to give iron supplementation for 3-
o M: 1 mg/day 12 months.
o F: 1.5 mg/day o In Harrisons, they suggested giving
o Higher requirement for: 300mg/day elemental iron but according to
Pregnant: 2-3x (5-6 mg) WHO, you can start with 60 mg/day elemental
Children/adolescents: 1.5x iron for patients with mild-moderate anemia.
Vegetarian diet has 50% less iron absorption o Eg. If a patient needs 60mg/day of elemental
High in Fe: iron, you can give ferrous sulphate hydrated
o red meat which has 65 mg. If you have a patient who
o egg yolk needs 300mg/day of elemental iron, then you
o dark leafy greens (spinach) need to give 5 tablets of ferrous sulphate
o dried fruit (raisins, prunes) hydrated.
o iron enriched foods (cereals, grains)
o mollusks (clams, oysters) Benefits of Effective Iron Supplementation Programs
o beans (soybeans) (Mentioned last year. From 2017 B)
Children/adolescents
Different forms of Iron: o improved behavioral and cognitive development
Heme iron o improve child survival
o Red meat (Eww. Eat white meat to be healthy.) Pregnant women and their infants:
o absorbed directly through the heme transporter o decreased incidence of low birth weight babies
FerrIc: IV supplement (e.g. Ferric Dextran) and perinatal mortality
o Why is it given parenterally? o decreased maternal mortality/obstetrical
This is because it must be first converted to complications
ferrous by duodenal cytochrome B (a All individuals
ferrireductase) to be absorbed in GIT. o improved fitness and work capacity
FerrOus: Oral preparations (e.g. Ferrous gluconate) o improved cognition
o Why oral? Because it can be directly absorbed by
the intestinal cell via DMT 1 Table 4: Common Oral Iron Preparations
Remember: Fair (Fer) ROD and RICky B
ROD: FerRous, Oral, Direct, DMT 1 Generic Name Percent Tablet Elixir Properties
RICky B: FerRiC, IV, duodenal cytochrome B Elemen (5 ml)
tal Iron
Storage and Transport (Mentioned last year. From 2017 B) Ferrous 20 % 325 300 Commonly
Inside the intestinal cell, iron is stored as ferritin. sulphate (65) (60) given due to
If iron is needed, it moves out as ferrous, becomes hydrated tolerability,
converted to ferric, and ferric binds to transferrin -> (dehydrate effectiveness
circulates in blood tetrahydrate) and low cost
Katzung: Ferritin is a B-globulin that can bind 2 molecules of More of the GI
ferric iron. irritation effect
195 90
C. Management (39) (18)
Packed RBC Transfusion – for SEVERE ACUTE ANEMIA
o Usually secondary to blood loss Ferrous 30-32%
o Supplementation can be started as adjunct but onset of sulphate
effects will be delayed dessicated
Oral iron (monohydrate)
Parenteral iron With incipients
Extended 20% 525 to prolong
D. Oral Iron Preparations (Refer to Table 4) Release (105) release
What you need to memorize in the table is the ferrous sulfate
elemental iron.
Ferrous 33 % 325 H% elemental
Remember that the supplement is often iron + a base
fumarate (107) iron; same
salt (sulfate, fumarate). Sometimes they don’t show the
elemental Fe in parenthesis and you have to compute effectiveness as
from the dosage. (2017B) sulfate
Elixirs are available for children and for patients who
cannot swallow. 195 100
Ferrous gluconate- given to children with iron (64) (33)
deficiency anemia. It is usually prepared as an elixir Ferrous 20% 75 (15) Iron amino acid
and combined with multivitamins. bisglycinate chelate; good
Extended release has excipients to prolong release absorption &
(2017B) high
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 4OF13
Pharmacology 3.02
bioavailability G. Response to Treatment
Reticulocyte count increases in 4-7 days after initiation of
Ferrous 12% 325 300 Similar efficacy therapy and peaks at 1 ½ weeks
gluconate (39) (35) and tolerability After 4 weeks of treatment, you need to see a Hemoglobin
as that of levels > 20g/dL. Thus first follow up is after 1 month.
sulfate
Absence of response may be due to poor absorption,
Polysaccharide 100% 150 100 Ferric complex
noncompliance to medication, or confounding diagnosis
iron (eg. (150) (100) with hydrolysed
Iron tolerance test –this is for adverse reactions and the
Maltose iron) starch; less GI
response of a patient
irritability;
o Give 2 iron tablets on an empty stomach
o Serum iron in 2 hours: If increase is at least 100 μg/dL,
E. WHO Guidelines of Iron Supplementation (from lecturer’s your treatment is adequate.
lecture slides)
The goal is to reverse anemia and provide 1g iron H. Parenteral Iron Therapy
stores for up to 3-12 months. Indicated for:
Patients under iron supplementation have to be Poor tolerance to oral iron
evaluated every month (2017) Acute condition (blood loss) AS ADJUNCT to packed RBC
Dosage: 60mg-300mg/day (300 is what Harrisons transfusion
recommends but for mild to moderate anemia, start at Most common use: Large demand for iron from patients
60 mg) being treated with erythropoietin (which cannot be
Adults: 60 mg satisfied by oral iron) especially hemodialysis patients or
Pregnant: 60 mg iron/400 μg folic acid for 6 months of patients with kidney problems
pregnancy but may extend 3-6 months postpartum
o Start supplementation at the SECOND Calculate the daily dose as follows:
trimester (2017) Body Weight (kg) x 2.3 x (15 – px Hgb in g/dL) + 500 or
st
o Higher toxicity in 1 trimester (2017) 1000 mg (depending on target iron stores)
o Metallic taste exacerbates vomiting in the
st
mother in 1 trimester (2017) Two ways to administer
Child 6-24 months: 12.5 mg iron/50 μg folic acid Administer total dose of iron required to correct deficit and
(N 6-12 months; LBW <2500g 2-24 months) provide at least 500 mg iron stores (can lead to more ADRs)
Child 2-5 yrs: 20-30mg iron Give repeated small doses for certain period of time (most
Child 6-11 yrs: 30-60 mg commonly used by doctors)
Adolescents and adults: 60 mg
Severe anemia Forms of parenteral iron
o Child <2 yrs: 25 mg iron + 100-400 μg folic Iron dextran
acid x 3 months o Contains 50 mg/mL elemental iron
o Child 2-12: 60 mg iron+ 400 μg folic acid x 3 o Not being used anymore high risk of anaphylaxis
months o Given <500mg IV/IM (half-life 6 hrs)
o Adolescents, adults, pregnant women: 120 Sodium Ferric Gluconate, Iron Sucrose, Ferumoxytol –
mg iron+ 400 μg folic acid x 3 months newer drugs
o Given in chronic renal failure (CRF)
F. Adverse Reactions & Precautions of Oral Iron o IV ONLY (Katzung)
Oral iron may cause GIT distress in 15-20% of patients o Ferritin levels between 500 and 1200 mg/mL and
o Most common complaint which can decrease compliance transferrin saturations of <25%
since treatment lasts for months o Lower risk of anaphylaxis
o Abdominal pain, nausea, vomiting, constipation
o You may switch to delayed release iron supplements Precautions (Katzung) (2017B)
because they have less GIT adverse reactions Monitor iron storage levels via SI or TIBC.
o This is often dose-related, another rationale to start low Be careful in giving parenteral iron because overdose and
(Katzung) toxicity can occur more easily as compared to the oral form.
o So, it is important to properly calculate the daily dose
Black stools are a side effect of oral iron. It has no needed by the patient.
significant clinical effect except possible masking of
gastrointestinal bleeding in fecalysis. (Katzung) I. Iron Toxicity
Taking the following with oral iron can DECREASE Acute
absorption: Exclusively in young children who swallow 10 tablets or
o milk, caffeine, antacids, calcium supplements more
Effects include necrotizing gastroenteritis, vomiting,
Vitamin C can INCREASE absorption. If you really need to abdominal pain, bloody diarrhea, shock, lethargy, dyspnea,
reverse anemia immediately, then you can give your iron coma and death
supplements with Vit C. Treatment includes:
o Whole bowel irrigation
o Deferoxamine (iron chelating compound)
o Supportive therapy
o According to Katzung, it is useless to give activated
charcoal because it does not bind iron.
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 5OF13
Pharmacology 3.02
Involved in erythropoiesis; stimulates progenitor
Chronic proliferation and maturation
Seen in patients given iron for a prolonged period of time at Involved in wound healing; it stimulates angiogenesis
maximum dose and smooth muscle fiber proliferation
Usually there is hemochromatosis aka iron overload results Involved in the brain’s response to neuronal injury
when there is excess iron deposition in heart, liver, pancreas Involved in vasocontriction-dependent hypertension
etc Increases iron absorption by suppressing hepicidin
May be inherited or acquired (mostly acquired)
o Inherited hemochromatosis C. Recombinant Human Erythropoietin
o B-thalassemia leading to repeated RBC transfusions
(Katzung) Epoietin alfa or Darbopoietin alfa
Treatment includes the ff: Increase Hct by 4 points and Hgb by 1g/dL in 2 weeks
o Intermittent phlebotomy (removes blood and therefore Darbopoietin alfa has a half-life 3-4x longer than that of
excess iron; 1 unit/week) epoietin alfa; it is a second generation erythropoiesis-
o Deferasirox: an oral iron chelator stimulating agent
According to Katzung, phlebotomy is what is usually done Adverse effects known include, but are not limited to,
because iron chelators are more complicated, expensive, allergic reactions, hypertension, migratory
and hazardous. thrombophlebitis, microvascular thrombosis, pulmonary
o It is only used as a last resort if a phlebotomy is not embolism, thrombosis of retinal artery, temporal veins,
enough. renal veins, headache, tachycardia, edema, shortness of
breath, GI upset (nausea, vomiting, diarrhea), stinging
D. HYPOPROLIFERATIVE ANEMIA sensation at injection site, flu-like symptoms
In light of this, iron supplementation and anticoagulants
At least 75% of all cases of anemia are hypoproliferative in may be needed
nature
Dosage for epoietin alfa (Guevarra, 2014):
A. Types and Diagnoses o CRF: 50-150U/kg 3x/week IV or 80-120U/kg 1-3x/week
IV /SQ (Hgb 10-12g/dL 4-6weeks; Hct 33-36% 2-4
Table 5: Diagnosis of Hypoproliferative Anemia months) ; maintained at 300U/kg
o AIDS: 100-300U/kg 3x/week IV/SQ
o Cancer: 150U/kg 3x/week; can reached 450-600U/kg
1x/week
o Surgery: 150-300U/kg OD for 10 days, day of surgery
and 4 days after surgery
Dosage for darbopoietin alfa (Guevarra, 2014):
o CRF: 45µg/kg 1x/wk IV/SQ
o Carries an increased risk of cancer recurrence.
E. MEGALOBLASTIC ANEMIA
Disorders characterized by presence of macrocytic red
cells in bone marrow
Causes:
O Cobalamin/folate deficiency
O Abnormality (genetic/acquired) in cobalamin/folate
Iron Deficiency anemia metabolism
Most common type O DNA synthesis defects
Anemia of chronic disease Cobalamin
Caused by chronic inflammation (rheumatoid arthritis), TB, A water soluble vitamin containing a cobalt molecule
tissue injury, and cancer Plays a role in regulating normal function of CNS, blood
formation, DNA synthesis, DNA regulation
Anemia of renal disease Synthesized by microorganisms mainly
Anemia results due to inadequacy of erythropoietin Coenzymes are methylcobalamin, a coenzyme involved
production secondary to impaired renal function in methionine, S-adenosylmethionine, and tetrahyrofolate
Examples are chronic renal failure (CRF), uremia, PCKD production, and adenosylcobalamin
Obtained via intake of fish, meat, dairy products
Anemia of metabolic disease We obtain 5-30 µg via diet, we lose 1-3 µg per day, a store
Hypothyroidism and starvation of 2-3 mg is good for 4 years
Passively absorbed in the buccal area, duodenum, and
*Usual observation is that red cells are normocytic and ileum; actively absorbed in the ileum in the presence of
normochromic gastric intrinsic factor
Normal range is 150-600 pmol or 200-900 pg/ml
B. Endogenous erythropoietin
Produced in the kidney by intestinal fibroblasts; hypoxia Cobalamin deficiency can be caused by (Guevarra, 2014):
stimulates its synthesis O Pernicious anemia due to IF loss secondary to
atrophic gastritis
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 6OF13
Pharmacology 3.02
O Inadequate amount of intake Therapy (Guevarra, 2014):
O Gastric and/or ileal resection O Given as folic acid, orally or parenterally or part of
O Decrease in gastric acid amount via proton pump MV prep
inhibitors and/or H2 blockers O Given as a prophylaxis in pregnant women, (dose
O Alcoholism of 400-500 µg per day); for hemolytic anemia it is
O Metformin intake given at a dose of 1 mg per day
O Malnutrition O Can be given as folinic acid (leucovorin calcium), a
derivative of tetrahydrofolate
Cobalamin deficiency results to (Guevarra, 2014): O Folinic acid circumvents DHF reductase inhibition (ex.
O Topic in question, megaloblastic anemia Resulting from methotrexate intake); it is an antidote
O Progressive swelling of myelinated neurons for folate antagonist toxicity (ex. Resulting from
O Demyelination trimethoprim and pyrimethamine intake)
O Neuronal cell death; these are seen in the spinal O Has no advantage over folic acid; it is actually more
column and cerebral cortex expensive
O Hand and foot paresthesia O Avoid multivitamin preparations; do multivitamin
O Decrease in vibration and position sense, with preparations only if there is evidence of vitamin
associated unsteadiness deficiency
O Decrease in deep tendon reflexes O Folic acid is well tolerated by the body, even at doses
O Confusion, moodiness, loss of memory as high as 15 mg per day
O Loss of central vision O Folic acid can decrease, even counteract effects of
drugs like phenobarbital, phenytoin, primidone
Vitamin B12 therapy (Guevarra, 2014)
O Given in cyanocobalamin and/or hydroxocobalamin, F. MYELOPOIESIS
as these are the active medicinal forms
O If there is inadequate intake, give orally; if there is IF
deficiency and/or gastric and ileal problems, give Myeloid growth factors are glycoproteins that stimulate the
parenterally proliferation and differentiation of one or more myeloid cell
O Cyanocobalamin is the first choice: give drug IM / lines
SQ (not IV as there is a risk of anaphylaxis; skin test Enhance the function of mature granulocytes and
needed), 1-1000µg 1-3x / week; supplementation is monocytes
80µg mixed w/ IF (not reliable; e.g. vegetarians) Produced naturally by a number of different cells, including
O An alternative is hydroxocobalamin, given 100 µg fibroblasts, endothelial cells, macrophages, and T cells
IM; this has a more sustained effect, lasting 3 months GM-CSF is capable of stimulating the proliferation,
O Treatment usually lasts for 6-12 months, as a long differentiation, and function of a number of the myeloid cell
term treatment; cyanocobalamin is given monthly in lineages
the form of 100 µg injections G-CSF is restricted to neutrophils and their progenitors,
O Also given for cases of neuropathies such as stimulating their proliferation, differentiation, and function
trigeminal neuralgia and multiple sclerosis, psychiatric
disorders, poor growth and/or nutrition, as a tonic for
patients suffering from tiredness and/or easy fatigue A. Conditions that affect Myelopoiesis
Folic acid Autologous bone marrow transplantation
Vitamin that is obtained from fresh green vegetables, fruits, Intensive myelosuppressive cancer chemotheraphy
liver, and yeast; 90% of vitamin is destroyed in the heat of
Zidovudine induced neutropenia in AIDS patients
cooking
Severe congenital neutropenia
Normally we obtain 50-500 µg of it per day; vegetarians
only obtain roughly 2 mg/day
B. Recombinant GM-CSF (Sargramostim)
We usually require 400 µg per day; pregnant women
require 500-600 µg per day; they must have an intake of at
least 400 µg per day to prevent defects in the neural tube Produced by yeast
Absorbed in duodenum and proximal jejunum (proximal
2
small intestine), transported while bound to a plasma- 125-500μg/m /d SQ (Half-life: 2-3hrs) [Katzung says: Serum
binding protein T1/2 of 2-7 hours after IV or SQ administration
Normal range is 9-45 nmol or 4-20 ng/mL
Slow infusion: 3-6 hours
Deficiency (Guevarra, 2014)
O Causes are alcoholism, diseases of the proximal small
intestine, inhibitors of dihydrofolate reductase such as Lower doses mainly affects neutrophils; larger doses
methotrexate and trimethoprim, drugs that interfere affect monocytes/eosinophils
in folate storage in tissues such as oral
contraceptives Adverse Effects: bone pain, malaise, flu-like symptoms,
O Deficiency of folic acid can result to higher incidences fever, diarrhea, dyspnea and rash, transient
of defects in the neural tube (anencephaly, supraventricular arrhythmia, elevation of serum creatinine,
encephaloceles, spina bifida), the topic in question bilirubin and hepatic enzymes
(megaloblastic anemia), coronary artery and
peripheral vascular diseases, venous thrombosis or
hyperhomocysteinemia
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 7OF13
Pharmacology 3.02
C. Recombinant G-CSF (Filgrastim/Pegfilgrastim) H. HEMOSTASIS
Filgrastim A. Elements of Hemostasis
o produced by Escherichia coli Primary Hemostasis
o Stimulates CFU-G to increase neutrophil o Affected by: aspirin and NSAIDs
production; stimulation of CFU-G to increase o Adequate vascular response, platelets, levels of Von
neutrophil production Willebrand factor
o 1-20μg/kg/d IV infusion for 30 mins
o Patient on cancer chemotherapy: 5μg/kg/d; daily Secondary Hemostasis
administration for 14-21 days o Affected by: warfarin and heparin
o Involve the extrinsic factors
Pelfigrastim o Adequate level of clotting factors, vitamin K
o gene through conjugation of a 20,000-Da
B. Bleeding Disorders
polyethylene glycol moiety to the G-CSF
glycoprotein produced by E. coli Causes
o Inherited coagulation disorders
o Longer half-life
clotting factor deficiency
o 6mg SQ
hemophilia
o Hemorrhagic diathesis of liver disease
G. MEGAKARYOPOIESIS o surgical procedures / multi-organ injuries
Thrombopoietin, a cytokine that predominantly stimulates o vitamin K deficiency
megakaryopoiesis. It is produced by the liver, marrow
stromal cells, and many other organs. It is the primary C. Diagnostic Tests
regulator of platelet production. platelet count: 150,000-400,000/m2
Interleukin-11 (IL-11) was cloned based on its activity to bleeding time (measure platelet function): 1-9 mins
promote proliferation of an IL-6-dependent myeloma cell line prothrombin time (measure extrinsic pathway; used for
Stimulates hematopoiesis, intestinal epithelial cell growth, warfarin): 11-13.5 sec
and osteoclasto-genesis and inhibits adipogenesis。 partial thromboplastin time (measure intrinsic pathway;
Enhances megakaryocyte maturation in-vitro; in-vivo used for heparin): 25-35sec
increases peripheral blood platelet counts
D. Vitamin K
Recombinant Interleukin-11 (Oprelvekin) cause of bleeding disorder
fat soluble
needed for complete synthesis of certain proteins that are
o Bacterially derived 19,000-Da polypeptide
required for blood coagulation (II, VII, IX, X) - 1972
also used to manipulate binding of calcium in bone and
o 25-50 μg/kg/d SQ; Half-life: 7 hours other tissues
o Administered daily; response in 5-9 days RDI
Infants: 10–20μg/day
o Used for chemotherapy induced thrombocytopenia Children & adolescents: 15–100μg/day
in non-myeloid malignancies (20,000/μL). Aim: Males: 120 μg/day
platelet count reaches 100,000/μL Females: 90 μg/day (lower than males)
o Adverse Effects: Fluid retention and associated Vitamin K Deficiency
cardiac symptoms, such as tachycardia palpitation, o Uncommon
edema, shortness of breath, blurred vision, injection o Causes:
site rash or erythema, and paresthesias. Resection of SI
Malabsorption syndrome
Recombinant Thrombopoietin Prolonged use of broad spectrum antibiotics
Diet low in vit. K
o Recombinant Human Megakaryocyte Growth and CKD
Development Factor (rHuMGDF) and Recombinant Alcoholics
Human Thrombopoietin (rHuTPO) – mixed results on Liver disease
efficacy Anticoagulants
o Mimics of recombinant thrombopoietin – used Salicylates
exclusively for ITP Barbiturates
Romiplostim – small peptide that binds with high Cefamandole
affiity to the thrombopoietin receptor o Usually occurs in newborns right after birth
Safe and efficacious in patients with ITP clotting factors are 30 to 60% of adult values
Platelet ct >50,000/μL in 8 weeks of study due to reduced synthesis of precursor proteins and
1-10 μg/kg/d SQ the sterility of their guts
Eltrombopag – 6 week course of 50-75mg/d st
Vit. K deficiency bleeding in 1 week of the infant's
orally life is 0.25 to 1.7%
o Well-tolerated given especially in premature babies
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 8OF13
Pharmacology 3.02
F. Tissue Plasminogen Activator (TPA) Inhibitors a day” dosing regimen for the patient. Which of the
Used to control bleeding in patients following drugs will be best suited for the patient?
Seen in the final stage of thrombin formation A. ferric-maltose complex 150 mg
Inhibitors of fibrinolysis B. ferrous sulfate dessicated 325 mg
Plasmin has a role in the lysis of clot made by secondary C. ferrous fumarate 200mg
hemostasis D. ferrous gluconate200 mg
4. Which of the following iron preparations is usually found
Aminocaproic acid in multivitamin medicated syrups because of its low
elemental iron content?
Competes for lysine binding sites on plasminogen and A. ferrous gluconate
B. ferrous sulfate dessicated
plasmin, blocking the interaction of plasmin with fibrin
C. ferrous fumarate
A very potent inhibitor of fibrinolysis (thrombi that formed
D. ferric-maltose complex
during treatment with the drug are not lysed)
Used to reduce bleeding after prostatic surgery or after 5. Which of the following conditions associated with
tooth extractions in haemophiliacs cobalamin deficiency will benefit most from oral
also used to prevent bleeding after surgical procedures cyanocobalamin?
(ability to treat a variety of bleeding disorders has been A. atrophic gastritis
unsuccessful) B. inflammatory bowel disease
st
Loading dose: 4-5g IV/PO during the 1 hour then 1-1.25g C. chronic alcoholism
PO q1Hour ; continuous IV infusion at 1g/Hr (continue for 8 D. ileal resection
hours or until bleeding is controlled, not to exceed 30g/day)
6. The conditions that will least likely benefit from epoeitin
Tranexamic acid alfa treatment
A. massive traumatic blood loss
Like aminocaproic acid, competes for lysine binding sites B. chronic renal failure
on plasminogen and plasmin, thus blocking their interaction C. cancer
with fibrin D. AIDS
Safer than aminocaproic acid 57. Which of the following will most likely happen when
Can be used for the same indications as aminocaproic correcting cobalamin deficiency with folic acid
acid and can be given IV or orally Usually given 1g 4x/day supplementation?
for 4 days (500mg 3x/day for 4-7days) A. lower incidence of homocysteinemia and venous thrombosis
B. lower incidence of megaloblastic anemia
*Adverse effects of both drugs: hypersensitivity reactions, C. decreased risk for nerve degeneration
nausea, vomiting, diarrhea, clotting problems (loss of vision, D. increased risk for neural tube defects
infarct, embolism) 8. In a patient with neutropenia, which of the following
agents will be least beneficial?
A. sargamostim
I. SUMMARY B. Romiplostim
Erythropoietin stimulates erythropoiesis. (without it there C. filgrastim
will be no erythropoiesis that will happen) D. perfilgrastim
Iron is needed for maturation of RBC. 9. Thrombocytopenia from immunosuppressive
Defective RBCs are formed in patients with Vit. B12 and B9 chemotherapy can be treated with the following
are deficient. medications EXCEPT:
GM-CSF, G-CSF, IL-11 and thrombopoietin are helpful in A. elthrombopag
certain conditions that produce neutropenia or B. romiplostim
thrombocytopenia C. sargramostim
Vit. K supplementation can be given to patients with certain D. Oprelvekin
bleeding disirders. 10. Which of the following available vitamin K preparations is
TPA inh. can be given to patients suffering bleeding from toxic for humans?
trauma, surgery, etc. A. phylloquinone
B. menaquinone
GUIDE QUESTIONS C. menatetrenone
1. All of the following substances delay absorption of
D. menadione
ingested iron EXCEPT:
Answers:
A. caffeine
B. milk 1)C 2)C 3)C 4)A 5)C 6)A 7)B 8)B 9)C 10)D
C. sodium ascorbate OBJECTIVES
D. calcium ascorbate None.
2. Which of the following parenteral iron preparations has a REFERENCES
higher incidence of anaphylactic reactions? 1. Dr. Guevarra’s Lecture
A. ferric gluconate 2. Katzung
B. ferric sucrose 3. 2017B trans
C. ferric dextran
D. ferric oxide
3.Lexi, a 32-year-old female, diagnosed with iron deficiency
anemia, needs 60mg a day of elemental iron. To minimize
the incidence of adverse reactions, you decided on a “once
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 9OF13
Pharmacology 3.02
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 10OF13
Pharmacology 3.02
APPENDIX
Table 6: Vitamin K1 vs. Vitamin K2
Vitamin K1 Vitamin K2
Form Phylloquinone, Menaquinones, Bacteria in SI can convert
Phytomenadione, vit .K1 to K2
Phytonadione,
Source Leafy green vegetables: Animal Meat:
dandelion greens, spinach, lettuce chicken, beef, their fat, livers, and organs
, cabbage, cauliflower, broccoli, Fermented or aged cheese, eggs
and brussels sprouts
Fruits: Bacteria in SI can convert K1 to K2
avocado, kiwifruit and grapes
Absorption Small intestine Small intestine
Signs and Symptoms of Anemia, bruising, bleeding gum or Deficiency Osteoporosis, Coronary heart
Deficiency nose, heavy menstrual bleeding disease, Severe aortic calcification
Therapy At birth: Menopausal women:
IV: 0.5 to 1.0 mg Orally (45 mg daily)
Newborns: To prevent osteoporosis
Human milk (1–4 μg/L) Rapid reversal from warfarin for pre-op:
Vit. K formula-derived milk Orally (1-2.5 mg)
(100 μg/L)
Figure 1: Events in Hemostasis
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 11OF13
Pharmacology 3.02
Figure 2: Factors that favor and inhibit thrombosis
Figure 3: Myelopoiesis
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 12OF13
Pharmacology 3.02
Figure 4: Megakaryopoiesis
2018-A DOMONDON, DUENAS, D UNGO, ENCARNACION, ENRIQUEZ 13OF13
Вам также может понравиться
- Haematinics & ErythropoietinДокумент30 страницHaematinics & ErythropoietinManikanta GupthaОценок пока нет
- Natal PlanetsДокумент290 страницNatal PlanetsAnonymous PErKNy9100% (1)
- SDG Business Reporting Analysis 2022Документ559 страницSDG Business Reporting Analysis 2022ComunicarSe-ArchivoОценок пока нет
- Crim 2 Assignment Title 8 of RPC Book 2Документ8 страницCrim 2 Assignment Title 8 of RPC Book 2Gio AvilaОценок пока нет
- Acid Base BalanceДокумент56 страницAcid Base BalanceVirendra Joshi100% (1)
- Intro-Generic vs. Brand Medicines-An OverviewДокумент8 страницIntro-Generic vs. Brand Medicines-An OverviewManikanta GupthaОценок пока нет
- Disorder of Respiratory SystemДокумент89 страницDisorder of Respiratory SystemDarine Nasr100% (1)
- Protein Binding of DrugДокумент22 страницыProtein Binding of DrugManikanta GupthaОценок пока нет
- TN Pharmacology in Tables PDFДокумент54 страницыTN Pharmacology in Tables PDFCean ObinaОценок пока нет
- Case-Studies - 018 - Presenting With Myocardial Infarction - NotesДокумент12 страницCase-Studies - 018 - Presenting With Myocardial Infarction - NotesInzemam Hashimi100% (1)
- Quiz With AnswersДокумент8 страницQuiz With Answersval284yОценок пока нет
- Pharma Rapid Review FOCUSДокумент85 страницPharma Rapid Review FOCUSKeelОценок пока нет
- Fact Sheet YaconДокумент2 страницыFact Sheet YaconTrilceОценок пока нет
- Cohort StudyДокумент46 страницCohort StudydrnareshchauhanОценок пока нет
- Complete DentureДокумент57 страницComplete Denturedr_ahmad_zuhdi100% (3)
- Drug DistributionДокумент49 страницDrug DistributionDrAmit VermaОценок пока нет
- 34 Drugs Used in Coagulation and Bleeding DisordersДокумент94 страницы34 Drugs Used in Coagulation and Bleeding DisordersJeanneОценок пока нет
- Drug InteractionsДокумент33 страницыDrug Interactions88AKK100% (1)
- AnswersДокумент91 страницаAnswersAndy Alvarez100% (1)
- Drugs Interaction1Документ13 страницDrugs Interaction1Akshay MandhotraОценок пока нет
- Final PharmacologyДокумент284 страницыFinal PharmacologytrialqwОценок пока нет
- Adrenergic Drugs 20.07.018 PDFДокумент59 страницAdrenergic Drugs 20.07.018 PDFHitesh karnОценок пока нет
- Blood Pressure Regulation-2Документ40 страницBlood Pressure Regulation-2Juliza FelicianoОценок пока нет
- Leaky Gut TreatmentДокумент5 страницLeaky Gut Treatmentfsilassie8012Оценок пока нет
- PharmacologyДокумент93 страницыPharmacologyPh SamerОценок пока нет
- MCQs 01-01 Introduction To Basic Principal of PharmacologyДокумент146 страницMCQs 01-01 Introduction To Basic Principal of PharmacologyNomi Waqas GulОценок пока нет
- DiureticsДокумент4 страницыDiureticsNazmul Islam AbirОценок пока нет
- Lab Diagnosis of NeoplasiaДокумент14 страницLab Diagnosis of Neoplasiasapphiresia100% (6)
- 4-Pharmacokinetics IДокумент88 страниц4-Pharmacokinetics IMarc Imhotep Cray, M.D.Оценок пока нет
- Pharmacology Trans ANS Drugs IДокумент20 страницPharmacology Trans ANS Drugs IPrincess Mara DuranОценок пока нет
- Quiz 3 Study QuestionsДокумент20 страницQuiz 3 Study QuestionsJessie AllisonОценок пока нет
- 6 Beta Adrenergic BlockersДокумент19 страниц6 Beta Adrenergic Blockersmatchees-gone rogue100% (1)
- Brain Edema XVI - Translate Basic Science Into Clinical Practice by Richard L Applegate, Gang Chen, Hua Feng, John H. ZhangДокумент376 страницBrain Edema XVI - Translate Basic Science Into Clinical Practice by Richard L Applegate, Gang Chen, Hua Feng, John H. ZhangAjie WitamaОценок пока нет
- Review Article Hijamah (Cupping Therapy) - A Comprehensive ReviewДокумент8 страницReview Article Hijamah (Cupping Therapy) - A Comprehensive ReviewMohamed ShiffaОценок пока нет
- GINA Assessment of Asthma ControlДокумент12 страницGINA Assessment of Asthma ControlaranspeterОценок пока нет
- Handbook ENGLISH FOR PHARMACY IIДокумент37 страницHandbook ENGLISH FOR PHARMACY IIAjeng Afriliana75% (4)
- CP RBC DisorderДокумент15 страницCP RBC DisorderDETECTIVE CONANОценок пока нет
- Affw0Glk0Slde - Fz@Eftracyainetb.G .Io#Fa9Diwtrdf0Doxycydine: ..Mwge P Mcnn5Документ2 страницыAffw0Glk0Slde - Fz@Eftracyainetb.G .Io#Fa9Diwtrdf0Doxycydine: ..Mwge P Mcnn5Raluca PăunaОценок пока нет
- Bio StatisticsДокумент101 страницаBio StatisticshferdjalОценок пока нет
- Ceftriaxone PDFДокумент1 страницаCeftriaxone PDFveniОценок пока нет
- ChemotherapyДокумент11 страницChemotherapyNedaAbdullahОценок пока нет
- Review Questions On Antiviral and AntibioticДокумент63 страницыReview Questions On Antiviral and AntibioticusedforfunplocОценок пока нет
- Spa PPT - FinalДокумент45 страницSpa PPT - FinalShivam DwivediОценок пока нет
- Emetics and Antiemetics DrugsДокумент15 страницEmetics and Antiemetics DrugsrajenderОценок пока нет
- Chapter 43 - Beta-LactamДокумент7 страницChapter 43 - Beta-LactamErika De JesusОценок пока нет
- Carbapenems PDFДокумент18 страницCarbapenems PDFElizabethHanganuОценок пока нет
- Antiemetic Drug Questions BankДокумент3 страницыAntiemetic Drug Questions Bankesraa elbassuonyОценок пока нет
- Differential Diagnosis in ChildrenДокумент1 страницаDifferential Diagnosis in ChildrendoctordilafrozaОценок пока нет
- Pedia All MCQs 1Документ578 страницPedia All MCQs 1Ahsan MumtazОценок пока нет
- Beta LactamДокумент18 страницBeta LactamCesar Saba0% (1)
- Pediatrics ImpДокумент233 страницыPediatrics Impملك عيسى100% (1)
- AnticoagulantsTypes, Mode of Action and Preparation of Anticoagulant Bottles.Документ40 страницAnticoagulantsTypes, Mode of Action and Preparation of Anticoagulant Bottles.Arslan Arshad100% (1)
- Caring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyДокумент34 страницыCaring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyRubinaОценок пока нет
- Pharmacology of Drugs For AnemiaДокумент49 страницPharmacology of Drugs For AnemiaAsticaPutriPurba100% (9)
- AutacoidsДокумент32 страницыAutacoidsRenellie TrimidalОценок пока нет
- Systemic Pathology - Dr. Priyanka SachdevДокумент792 страницыSystemic Pathology - Dr. Priyanka SachdevH GondaliyaОценок пока нет
- TUBERCULOSIS (Lec Community Medicine)Документ24 страницыTUBERCULOSIS (Lec Community Medicine)wanderer_1010Оценок пока нет
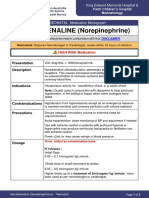
- NORADRENALINE (Norepinephrine) : Presentation DescriptionДокумент3 страницыNORADRENALINE (Norepinephrine) : Presentation DescriptionMutiaraОценок пока нет
- Gus TДокумент21 страницаGus THashemite MedicineОценок пока нет
- Iron PoisoningДокумент10 страницIron PoisoningOoi Ah Guan100% (1)
- Antiarrhythmic Drugs-Test-2-QuestionsДокумент7 страницAntiarrhythmic Drugs-Test-2-QuestionsDrishya BioplannetОценок пока нет
- General Pharmacology by Dr. BashirДокумент21 страницаGeneral Pharmacology by Dr. BashirrohishaakОценок пока нет
- Genpath 04 - RENAL LABORATORY TESTS - ppt.MEd 2016 (Ninaarajade's Conflicted Copy 2016-10-29) (ASUS's Conflicted Copy 2016-11-14)Документ67 страницGenpath 04 - RENAL LABORATORY TESTS - ppt.MEd 2016 (Ninaarajade's Conflicted Copy 2016-10-29) (ASUS's Conflicted Copy 2016-11-14)RjDОценок пока нет
- Pharma CNSДокумент20 страницPharma CNSIbrahem AlОценок пока нет
- PMLS 1 Topic 8.11 TransДокумент3 страницыPMLS 1 Topic 8.11 TransKae Abegail Garcia100% (1)
- Alata SaminaMCQsДокумент132 страницыAlata SaminaMCQsmintahmeshackbenjaminОценок пока нет
- Initial PE and Labs History Initial Impression: Location &Документ1 страницаInitial PE and Labs History Initial Impression: Location &kaydee.arОценок пока нет
- مصحح قروب زوم ++ 21 صفحة مهمДокумент12 страницمصحح قروب زوم ++ 21 صفحة مهمAlexandra RenneОценок пока нет
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingОт EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováОценок пока нет
- 112 Lecture MidtermsДокумент8 страниц112 Lecture MidtermsRose Ann CammagayОценок пока нет
- 112 Lecture MidtermsДокумент18 страниц112 Lecture MidtermsRose Ann CammagayОценок пока нет
- Hematology: FANER, Ned Denebe LACANILAO, Sunshine NUCUM, Billie Kim PAGADUAN, Maribec PUA, MonalisaДокумент31 страницаHematology: FANER, Ned Denebe LACANILAO, Sunshine NUCUM, Billie Kim PAGADUAN, Maribec PUA, MonalisatzuquinoОценок пока нет
- Menulis Daftar Pustaka VancouverДокумент11 страницMenulis Daftar Pustaka VancouverRatu Qurroh AinОценок пока нет
- Citation Styles & Bibliographic Format-UGC NETДокумент6 страницCitation Styles & Bibliographic Format-UGC NETManikanta GupthaОценок пока нет
- Referencing Style Guides - Library - University of QueenslandДокумент4 страницыReferencing Style Guides - Library - University of QueenslandManikanta GupthaОценок пока нет
- Citation Style Guides - APA, MLA, and HarvardДокумент5 страницCitation Style Guides - APA, MLA, and HarvardManikanta GupthaОценок пока нет
- Citation Management Softwares (Endnote, EndNote Web, RefWorks & Mendeley) - USCДокумент1 страницаCitation Management Softwares (Endnote, EndNote Web, RefWorks & Mendeley) - USCManikanta GupthaОценок пока нет
- Examples of References - Vancouver Style (From Uniform Requirements For Manuscripts,)Документ3 страницыExamples of References - Vancouver Style (From Uniform Requirements For Manuscripts,)Manikanta GupthaОценок пока нет
- FAQ Related To Databases, Journals, IndexingДокумент2 страницыFAQ Related To Databases, Journals, IndexingManikanta GupthaОценок пока нет
- Migraine Drugs - Sharma & SharmaДокумент2 страницыMigraine Drugs - Sharma & SharmaManikanta GupthaОценок пока нет
- PK-Factors Prolonging Drug Action-1Документ18 страницPK-Factors Prolonging Drug Action-1Manikanta GupthaОценок пока нет
- Predatory Journals-ReviewДокумент7 страницPredatory Journals-ReviewManikanta GupthaОценок пока нет
- ADRENERGIC RECEPTORS-Leraning Objectives & NotesДокумент10 страницADRENERGIC RECEPTORS-Leraning Objectives & NotesManikanta GupthaОценок пока нет
- Nsaids Mbbs PDFДокумент38 страницNsaids Mbbs PDFManikanta GupthaОценок пока нет
- Hepatoprotective Model Group (N 6) Drug & Dose: 8 OSE-mg/kg 9 Liqo E-Mg/kgДокумент4 страницыHepatoprotective Model Group (N 6) Drug & Dose: 8 OSE-mg/kg 9 Liqo E-Mg/kgManikanta GupthaОценок пока нет
- Non Judgemental CommunicationДокумент1 страницаNon Judgemental CommunicationManikanta GupthaОценок пока нет
- NSAID's QuestionsДокумент3 страницыNSAID's QuestionsManikanta Guptha100% (2)
- Migraine - Sharma & SharmaДокумент2 страницыMigraine - Sharma & SharmaManikanta GupthaОценок пока нет
- Pharmaco GeneticsДокумент52 страницыPharmaco GeneticsManikanta GupthaОценок пока нет
- Cardiovascular PharmacologyДокумент24 страницыCardiovascular PharmacologySuresh ShresthaОценок пока нет
- PD-Dose Response Curve & Drug Combined EffectsДокумент34 страницыPD-Dose Response Curve & Drug Combined EffectsManikanta GupthaОценок пока нет
- PK-factors Modifying Drug ResponseДокумент45 страницPK-factors Modifying Drug ResponseManikanta GupthaОценок пока нет
- Anti Anxiety DrugsДокумент29 страницAnti Anxiety DrugsManikanta GupthaОценок пока нет
- Potency and Selectivity of Agonist - Pharmacology in One SemesterДокумент6 страницPotency and Selectivity of Agonist - Pharmacology in One SemesterManikanta GupthaОценок пока нет
- PK - CYP3A4 and CYP2D6 Inhibitors and InducersДокумент5 страницPK - CYP3A4 and CYP2D6 Inhibitors and InducersManikanta GupthaОценок пока нет
- Drug Nomenclature: MR - Manikanta TMCДокумент5 страницDrug Nomenclature: MR - Manikanta TMCManikanta GupthaОценок пока нет
- P Glycoprotein Pharmacological RelevanceДокумент12 страницP Glycoprotein Pharmacological RelevanceManikanta GupthaОценок пока нет
- Intro-Glossary of Terms and Symbols Used in PharmacologyДокумент45 страницIntro-Glossary of Terms and Symbols Used in PharmacologyManikanta GupthaОценок пока нет
- Guide To: Raising DucksДокумент16 страницGuide To: Raising DucksNeil MenezesОценок пока нет
- Datasheet Reagent SansureДокумент3 страницыDatasheet Reagent Sansuredanang setiawanОценок пока нет
- 150 Years of PharmacovigilanceДокумент2 страницы150 Years of PharmacovigilanceCarlos José Lacava Fernández100% (1)
- VSR 421Документ2 страницыVSR 421AdarshBijapur0% (1)
- Bionic EyeДокумент6 страницBionic EyeAsfia_Samreen_29630% (1)
- Genetic Recombination in Bacteria Horizon of The BДокумент9 страницGenetic Recombination in Bacteria Horizon of The BAngelo HernandezОценок пока нет
- Fon by SatarДокумент40 страницFon by SatarAqib SatarОценок пока нет
- Orthopedic InstrumentsДокумент7 страницOrthopedic InstrumentsRonnie CanteroОценок пока нет
- EMOTIONS Are Metaphysical! - TriOriginДокумент1 страницаEMOTIONS Are Metaphysical! - TriOriginStellaEstel100% (2)
- S 0140525 X 00003368 AДокумент59 страницS 0140525 X 00003368 AEnver OruroОценок пока нет
- MenopauseДокумент21 страницаMenopauseDr K AmbareeshaОценок пока нет
- Suppositories Phardose LectureДокумент41 страницаSuppositories Phardose LecturePeter Paul RecaboОценок пока нет
- Vertical Farming-EENADU - My Simple Innovative and Cost Effective Method & OthersДокумент34 страницыVertical Farming-EENADU - My Simple Innovative and Cost Effective Method & OthersAnumakonda JagadeeshОценок пока нет
- (Ebook PDF) Equine Ophthalmology 3Rd Edition by Brian C. GilgerДокумент41 страница(Ebook PDF) Equine Ophthalmology 3Rd Edition by Brian C. Gilgerjessica.rohrbach136100% (47)
- 4 - Chapter - Respiratory SystemДокумент25 страниц4 - Chapter - Respiratory SystemleonОценок пока нет
- Name: DR Iqra RasoolДокумент65 страницName: DR Iqra RasoolFaryalBalochОценок пока нет
- Jurnal GerdДокумент6 страницJurnal GerddilaОценок пока нет
- 1st Internal Assessment Pharmacology 28.7.21 FinalДокумент2 страницы1st Internal Assessment Pharmacology 28.7.21 FinalSubhom MajumderОценок пока нет
- An Overview of Mechanical Ventilation in The Intensive Care UnitДокумент9 страницAn Overview of Mechanical Ventilation in The Intensive Care UnitJaime Javier VegaОценок пока нет
- Makabuhay IpДокумент7 страницMakabuhay IpButterflyCalmОценок пока нет
- The Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalДокумент4 страницыThe Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDIEGOОценок пока нет