Академический Документы
Профессиональный Документы
Культура Документы
Updates On An At-Risk Population Late-Preterm and Early-Term Infants
Загружено:
NoviaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Updates On An At-Risk Population Late-Preterm and Early-Term Infants
Загружено:
NoviaАвторское право:
Доступные форматы
CLINICAL REPORT Guidance for the Clinician in Rendering Pediatric Care
Updates on an At-Risk Population:
Late-Preterm and Early-Term Infants
Dan L. Stewart, MD, FAAP,a Wanda D. Barfield, MD, MPH, FAAP, RADM, USPHS,b COMMITTEE ON FETUS AND NEWBORN
The American Academy of Pediatrics published a clinical report on late- abstract
preterm (LPT) infants in 2007 that was largely based on a summary of a 2005
workshop convened by the Eunice Kennedy Shriver National Institute of a
School of Medicine, University of Louisville, Louisville, Kentucky; and
b
Child Health and Human Development, at which a change in terminology from Centers for Disease Control and Prevention, Atlanta, Georgia
“near term” to “late preterm” was proposed. This paradigm-shifting Clinical reports from the American Academy of Pediatrics benefit from
expertise and resources of liaisons and internal (AAP) and external
recommendation had a remarkable impact: federal agencies (the Centers for reviewers. However, clinical reports from the American Academy of
Disease Control and Prevention), professional societies (the American Pediatrics may not reflect the views of the liaisons or the
organizations or government agencies that they represent.
Academy of Pediatrics and American College of Obstetricians and
Dr Stewart and the members of the Committee on Fetus and Newborn
Gynecologists), and organizations (March of Dimes) initiated nationwide conceived the concept of updating the previous American Academy of
monitoring and educational plans that had a significant effect on decreasing Pediatrics publication on late-preterm infants, collaborated with Drs
Barfield and Raju, and reviewed the manuscript; Drs Barfield and Raju
the rates of iatrogenic LPT deliveries. However, there is now an evolving collaborated with Dr Stewart and members of the Committee on Fetus
concern. After nearly a decade of steady decreases in the LPT birth rate that and Newborn and reviewed the manuscript; and both authors
approved the final manuscript as submitted and agree to be
largely contributed to the decline in total US preterm birth rates, the birth accountable for all aspects of the work.
rate in LPT infants has been inching upward since 2015. In addition, evidence The guidance in this report does not indicate an exclusive course of
revealed by strong population health research demonstrates that being born treatment or serve as a standard of medical care. Variations, taking
into account individual circumstances, may be appropriate.
as an early-term infant poses a significant risk to an infant’s survival, growth,
All clinical reports from the American Academy of Pediatrics
and development. In this report, we summarize the initial progress and automatically expire 5 years after publication unless reaffirmed,
discuss the potential reasons for the current trends in LPT and early-term revised, or retired at or before that time.
birth rates and propose research recommendations. The findings and conclusions in this article are those of the authors
and do not necessarily represent the official position of the Centers for
Disease Control and Prevention.
This document is copyrighted and is property of the American
Academy of Pediatrics and its Board of Directors. All authors have filed
INTRODUCTION conflict of interest statements with the American Academy of
Pediatrics. Any conflicts have been resolved through a process
The American Academy of Pediatrics (AAP) published a clinical report on approved by the Board of Directors. The American Academy of
Pediatrics has neither solicited nor accepted any commercial
late-preterm (LPT) infants (born between 34 0/7 weeks’ gestation and involvement in the development of the content of this publication.
36 6/7 weeks’ gestation; Fig 1) in 20071 that was largely based on
DOI: https://doi.org/10.1542/peds.2019-2760
a summary of the 2005 workshop convened by the Eunice Kennedy Shriver
National Institute of Child Health and Human Development.2 At this Address correspondence to Dan L. Stewart, MD, FAAP. E-mail:
dan.stewart@louisville.edu
workshop, a change in terminology from “near term” to “late preterm” was
proposed. This shift in the paradigm recommendation led to a remarkable
impact: federal agencies (the Centers for Disease Control and Prevention), To cite: Stewart DL, Barfield WD, AAP COMMITTEE ON FETUS
AND NEWBORN. Updates on an At-Risk Population: Late-
professional societies (the AAP and American College of Obstetrics and
Preterm and Early-Term Infants. Pediatrics. 2019;144(5):
Gynecology), and organizations (March of Dimes) initiated nationwide e20192760
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
PEDIATRICS Volume 144, number 5, November 2019:e20192760 FROM THE AMERICAN ACADEMY OF PEDIATRICS
monitoring and educational plans
that had a significant effect on
decreasing the rates of iatrogenic LPT
deliveries, as noted in numerous
publications.
Evidence revealed by strong
population health research
demonstrated that LPT or early-term
(ET) births (between 37 0/7 weeks’
gestation and 38 6/7 weeks’
gestation; Fig 1) pose a significant
FIGURE 1
risk to an infant’s survival, growth, Definitions of gestational age periods from LPT to postterm. (Reprinted with permission from Engle
and development because of WA, Kominiarek M. Late preterm infants, early term infants, and timing of elective deliveries. Clin
increased morbidities and mortality Perinatol. 2008;35(2):325–341.)
in these at-risk groups (Fig 2). The
2007 AAP clinical report on LPT
births was an important milestone in After reaching a nadir of 9.57% in predominantly among non-Hispanic
helping health care providers 2014, the preterm birth rate black and Hispanic women.4,7 In
understand the magnitude of these increased to 9.97% in quarter 3 of 2018, the LPT birth rate rose to
untimely births and their relative 2018 (Fig 4).6 This report shows an 7.28% (Fig 5). These trends must be
contribution to overall preterm birth emerging concern. After nearly continually monitored with an
and disparities. Neonatologists and a decade of steady decreases, the exploration of causality.8 In this
pediatricians should be aware of the preterm birth rate is inching report, the initial progress is
current and ongoing challenges upward again. These trends are summarized, the potential reasons
infants face after being born LPT or largely attributable to increases for the current trends in LPT birth
ET. Understanding the current in the rate of LPT births, rates are discussed, and practice
terminology, factors contributing to
these early deliveries, and long-term
implications for growth and
development will help in prevention,
clinical management, and population-
based quality-improvement efforts.
Because LPT infants account for
approximately 70% of preterm births
in the United States, this is a costly
and important public health matter.3
LPTs represent 7% of all live births;
ET infants represent 26% of all live
births and 29% of all term infants4
(Fig 3). Recognition of these at-risk
subsets of preterm and term infants
has affected perinatal care and
launched a robust research endeavor
to decrease the number of
nonmedically indicated deliveries
of infants born LPT and ET5 while
seeking methods to optimize care
provided to these patients. There
have been more than 500
publications investigating the reasons FIGURE 2
for LPT and ET while recognizing that Neonatal and infant mortality by gestational age. Adapted from Reddy UM, Ko CW, Raju TN, Willinger
M. Delivery indications at late-preterm gestations and infant mortality rates in the United States.
there are a number of maternal, fetal, Pediatrics. 2009;124(1):234–240. (Reprinted with permission from Kardatzke MA, Rose RS, Engle WA.
and placental complications for which Late preterm and early term birth: at-risk populations and targets for reducing such early births.
either LPT or ET birth is warranted.5 NeoReviews. 2017;18(5):e265–e276.)
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
2 FROM THE AMERICAN ACADEMY OF PEDIATRICS
“Implicit in any definition or
subclassification of preterm or term
birth is the need for accurate dating,
which would likely lead to a lower
proportion of deliveries categorized
as postterm or early term.”8 The
ACOG considers first-trimester
ultrasonography to be the most
accurate method to establish or
confirm gestational age. Pregnancies
without an ultrasonographic
examination confirming or revising
the estimated due date before 22 0/7
weeks’ gestation should be
considered suboptimally dated. There
is no role for elective delivery in
a woman with a suboptimally dated
pregnancy. Although guidelines for
FIGURE 3
Percentage of births by gestational age at birth: United States 2017. (Adapted from Martin JA, indicated LPT and ET deliveries
Hamilton BE, Osterman MJ, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018; depend on an accurate determination
67:8.) of gestational age, women with
suboptimally dated pregnancies
and research recommendations are 38 weeks 6 days’ gestation be should be managed according to
proposed. designated as ET, those between these same guidelines because of the
39 weeks 0 days’ gestation and lack of a superior alternative.12
40 weeks 6 days’ gestation be After the 2005 Eunice Kennedy
CURRENT DEFINITIONS
designated as term, and those Shriver National Institute of Child
The national emphasis on reducing occurring at 41 weeks 0 days’ Health and Human Development
preterm births and the increase in gestation through 41 weeks 6 days’ workshop, there were concerns
scheduled deliveries has created gestation be designated as late about unintended consequences,
confusion around the definition of term.9,10 including an increase in stillbirths13
term gestation.9 The concept of and increasing the risks for the
“term” gestation provides guidance to According to the American College of mother and her fetus by the
clinicians and influences the public’s Obstetricians and Gynecologists avoidance of indicated LPT
perceptions about the optimal timing (ACOG), accurate dating of pregnancy deliveries. Current ACOG and Society
of delivery for a healthy pregnancy.9 is important to improve outcomes for Maternal-Fetal Medicine
This nomenclature acknowledged and is a research and public health recommendations state that there
that fetal maturation is a continuum, imperative. As soon as data from the are a number of maternal, fetal, and
yet the use of the label of term for last menstrual period, the first placental complications for which
pregnancies spanning 37 weeks’ accurate ultrasound examination, or either an LPT or ET delivery is
0 days gestation through 41 weeks 6 both are obtained, the gestational age warranted. The timing of delivery in
days’ gestation remained unchanged. and the estimated due date should be such cases must balance the
Recent data demonstrate that determined, discussed with the maternal and newborn risks of LPT
maternal and neonatal adverse patient, and documented clearly in and ET delivery with the risks
outcome rates are not the same the medical record. A pregnancy associated with further continuation
across the 5-week gestational age without an ultrasound examination of pregnancy. Deferring delivery to
range that constitutes term.9 Rather, that confirms or revises the estimated the 39th week is not recommended if
the frequency distribution of adverse due date before 22 0/7 weeks’ there is a medical or obstetric
outcomes is U shaped, with the nadir gestation should be considered indication for earlier delivery.
being between 39 weeks 0 days’ suboptimally dated. For the purposes
gestation and 40 weeks 6 days’ of research and surveillance, the best
gestation.9 The Defining “Term” obstetric estimate, rather than PATHOGENESIS OF PRETERM BIRTHS
Pregnancy workshop recommended estimates based on the last menstrual The pathogenesis of preterm birth is
that births occurring between period alone, should be used as the not completely understood. Two-
37 weeks 0 days’ gestation and measure for gestational age.11 thirds of preterm deliveries occur as
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
PEDIATRICS Volume 144, number 5, November 2019 3
FIGURE 4
Quarterly preterm birth rates 2017 to quarter 1 of 2019. (Adapted from Rossen LM, Osterman MJK, Hamilton BE, Martin JA. Quarterly Provisional
Estimates for Selected Birth Indicators, 2017–quarter 1, 2019. Hyattsville, MD: National Center for Health Statistics NVSS, Vital Statistics Rapid Release
Program; 2019.)
a result of spontaneous preterm labor states focused on policies and investigated in women anticipated to
and/or premature rupture of practices to reduce tobacco use in deliver between 34 and 37 weeks of
membranes.14 Risk factors that may pregnancy and reduce nonindicated pregnancy.24 Infants of women
contribute to these events include preterm delivery.18,19 State perinatal treated had significantly lower rates
a history of a previous preterm quality collaboratives, which of respiratory complications.
delivery (risk is 1.5–2.0 times consisted of teams of clinical and However, 35 women needed to be
higher)15; infection; inflammation; public health members, have also treated to improve outcomes in 1
maternal stress (acute and/or helped to reduce the rates of infant, and 24% of steroid-exposed
chronic); uterine, placental, and/or nonmedically indicated LPT and ET infants developed hypoglycemia
fetal anomalies; short cervix; as well births.20 Progress has been made in compared with 14.9% of those in the
as multifetal pregnancies.16 the rate for triplet and higher- placebo group. Thus, despite
Newnham et al17 recently reviewed order–multiple births, which has endorsements by the obstetric
current strategies for prevention of been on the decline since 1998 and professional societies,25–27 several
preterm birth, which include presently is the lowest in more than 2 experts have raised concerns about
decreasing smoking during decades.3,21–23 In part from the the routine use of antenatal steroids
pregnancy, cervical cerclage, judicious efforts from the March of Dimes in women during LPT gestations.27–29
use of fertility treatments, prevention program that no infant be delivered Pediatric providers, too, need to
of nonmedically indicated deliveries, electively before 39 weeks’ gestation, review a history of antenatal steroid
and the establishment of high-risk the cesarean delivery rate is down exposure while evaluating LPT
obstetric clinics. Public health efforts 3% from a peak of 32.9% in 2009.3 infants, including checking for
also contributed, using the neonatal hypoglycemia.
Collaboration on Innovation and In a large randomized controlled trial,
Improvement Network to reduce the benefits of a single course of Use of progesterone for women with
infant mortality. In these efforts, antenatal betamethasone was a previous history of spontaneous
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
4 FROM THE AMERICAN ACADEMY OF PEDIATRICS
FIGURE 5
Preterm birth rates: United States, overall and by race and ethnicity, 2014 and 2018. Source: National Center for Health Statistics, National Vital Statistics
System–Natality.
preterm birth decreases mortality advanced technologies to overcome contribution of ART to preterm
and the need for admission to the infertility has resulted in millions of births, the majority of which are also
NICU. Unfortunately, this pregnancies and subsequent live low birth weight, is a factor in the
improvement is limited to singleton births.37 Since 1995, the number of increases observed in the LPT and ET
pregnancies, not multiples.15,30,31 ART procedures performed in the population (Table 1).38,39
Likewise, 17-hydroxyprogesterone United States and the number of
has shown efficacy in women with infants born as a result of these SHORT- AND LONG-TERM MEDICAL AND
a short cervix documented by procedures have nearly tripled.22 NEURODEVELOPMENTAL SEQUELAE FOR
ultrasonography.32 Screening of Because many ART procedures LPT AND ET INFANTS
women with a previous preterm birth involve transferring multiple LPT infants are at increased risk for
at less than 34 weeks’ gestation may embryos, ART results in multiple- a number of adverse events, including
identify women with a cervical length gestation pregnancies and multiple respiratory distress, hypoglycemia,
,25 mm before 24 weeks’ gestation births. The percentage of infants born feeding difficulties, hypothermia,
who might potentially benefit from preterm and very preterm is higher hyperbilirubinemia, apnea, seizures,
a cervical cerclage.33,34 Variable among ART-conceived infants than and a higher rate of readmission after
access to 17-hydroxyprogesterone,
among infants in the total birth initial discharge.40,41 In addition, LPT
antenatal steroids, prenatal
population even with elective single- infants have higher rates of
ultrasonography, and early treatment
embryo transfers, which involves the pulmonary disorders during
and/or management of preterm
transfer of a single embryo. The childhood and adolescence, learning
prolonged rupture of membranes
and/or signs of infection may be
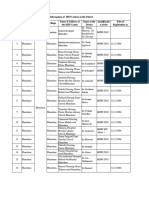
contributing to racial disparities in TABLE 1 The Percentage of Preterm Births by Gestational Age Groups Attributable to ART, 2015
preterm birth rates.35,36 In addition, Region Preterm (,37 wk) Very Preterm (,32 LPT Births (34 1 0/ ET Births (37 1 0/
lack of adequate prenatal care may Births Attributable wk) Births 7–36 1 6/7 wk) 7–38 1 6/7 wk)
delay appropriate management of to Attributable to Attributable to Attributable to
conditions that develop before and ART, % ART, % ART, % ART, %
during pregnancies, such as diabetes, United 5.3 5.4 5.0 2.1
hypertension, preeclampsia, and States
and
others.23
Puerto
Rico
Since the birth of the first US infant
Preterm: ,37 wk; very preterm: ,32 wk; LPT: 34 0/7–36 6/7 wk; ET: 37 0/7–38 6/7 wk. Source: Analyses of the National ART
conceived with assisted reproductive Surveillance System (NASS) data. Written communication with the Division of Reproductive Health, National Center for
technology (ART) in 1981, the use of Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, April 19, 2018.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
PEDIATRICS Volume 144, number 5, November 2019 5
difficulties, and subtle, minor deficits readmission rates are increased for infant.51,52 Chronic bilirubin
in cognitive function.42 As adults, LPT LPT (3.5%) versus term (2.0%) encephalopathy (kernicterus)
and ET infants have higher blood infants.49 Even among infants who secondary to high concentrations of
pressure and more often require were never in a NICU, the unconjugated bilirubin can result in
treatment of diabetes.43 In a Swedish readmission rate was threefold higher permanent neurologic damage. Even
cohort, former LPT infants at 18 to in LPT than in term infants.50 Many exposure to moderate concentrations
36 years of age showed an increased LPT infants are discharged early but of bilirubin may lead to more subtle
mortality rate compared with infants require readmission for jaundice, yet permanent neurodevelopmental
born at 37 to 42 weeks’ gestation feeding problems, respiratory impairment, which is labeled as
(hazard ratio, 1.31; 95% confidence distress, and proven or suspected bilirubin-induced neurologic
interval, 1.13–1.5).44 Several studies sepsis because of physiologic and dysfunction.51 Auditory neuropathy
have described an increased risk of metabolic immaturity. spectrum disorder is a common
neurologic, psychiatric, and manifestation of bilirubin-induced
Early discharge among LPT infants
developmental conditions in this neurologic dysfunction in the LPT
affected by discharge criteria
subset as they mature into adulthood infant.53
established for term infants show an
(Table 2).45 The United States does
increase in morbidities. In statewide Quinn et al54 recently published
not have registries tracking outcomes
data from Massachusetts, all state- a review of the literature concerning
of infants born at LPT gestations into
resident infants discharged after discharge criteria for the LPT infant.
adult age groups. However, on the
a hospital stay of less than 2 nights They found few differences in
basis of its national registry, the
were analyzed. In the LPT group discharge criteria between infants
Swedish National Cohort Study
(1004 infants), 4.3% were readmitted in the newborn nursery and those
reported a stepwise increase in
or required an observational stay in the NICU.55 Previously published
disability rates in young adulthood,
versus 2.7% of the term infants (n = discharge criteria from the AAP
which increased with the degree of
24 320). LPT infants were also evolved over time and include
preterm birth.46
1.5 times more likely to require physiologic stability and completed
hospital-related care. This study screenings for hearing loss,
LENGTH OF STAY AND DISCHARGE suggested that LPT infants discharged hyperbilirubinemia, car seat safety,
CRITERIA early experience significantly more hypoglycemia, critical congenital
neonatal morbidity than term infants; heart disease, and sepsis. Parental
The duration of birth hospitalization
however, this may be true only for education was also a major
correlates with gestational age at
breastfed infants. The authors component of discharge planning,
birth.47,48 Among 235 LPTs at 1 birth
concluded that evidence-based including umbilical cord care,
center, the length of the birth
recommendations for appropriate feeding, voiding and/or stooling,
hospitalization (mean 6 SD) was 12.6
discharge timing and postdischarge and weight gain. In addition, Quinn
6 10.6 days at 34 weeks’ gestation,
follow-up are needed.49 et al54 recommended maternal
6.1 6 5.8 days at 35 weeks’ gestation,
screening assessments for
and 3.8 6 3.6 days at 36 weeks’ Moderately preterm infants are also
depression, drug use, a safe home
gestation. The usual hospital stay for at increased risk for acute bilirubin
environment, and the existence of
a term infant is 2 days for a vaginal encephalopathy. Clinical
a support system.
delivery and 3 days for a cesarean manifestations may be more subtle in
delivery. In addition, hospital the LPT infant versus the term A major difference between newborn
discharge and discharge criteria for
TABLE 2 Neurologic, Psychiatric, and Developmental Disorders in LPT Infants as Adults the LPT infant is the transition to
safe sleep before discharge (supine
Neurologic and Psychiatric Conditions Relative Risk of LPT Versus Term (95%
CI) position). Given that LPT and ET
infants are at an increased risk of
Attention-deficit/hyperactivity disorder 1.7 (1.2–2.5)
Any psychiatric disorder 3.74 (1.59–8.78)
morbidity and mortality, greater
Any anxiety disorder 3.85 (1.52–9.52) efforts are needed to ensure safe and
Cerebral palsy 2.7 (2.2–3.3) healthy posthospitalization and
Cognitive disability 1.6 (1.4–1.8) home care practices for these
Schizophrenia 1.3 (1.0–1.7) vulnerable infants.56 Finally,
Any disorder of psychological development, behavior, and 1.4 (1.3–1.5)
emotion
standardized criteria for discharge
may improve outcomes and reduce
Adapted from Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med.
2008;359(3):262–273; and Kardatzke MA, Rose RS, Engle WA. Late preterm and early term birth: at-risk populations and maternal stress in these high-risk
targets for reducing such early births. NeoReviews. 2017;18(5):e265–2376. CI, confidence interval. groups.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
6 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Evaluating 161 804 infants in Florida a small but significant fraction of treating intrauterine infection,
between 34 and 41 weeks’ gestation infants born preterm are concerning. improving maternal nutrition, and
with a length of stay of #72 hours This population is at a slightly higher lifestyle modifications to decrease
revealed that LPT infants, compared risk for neuropsychological and stress.17
with term infants, had a 36% higher behavioral problems, hypertensive
risk for developmental delay or disorders and metabolic syndrome,
disability and a 19% higher risk of and developing at an earlier age when RECOMMENDATIONS
suspension in kindergarten after compared with term infants. Preterm
Accounting for approximately 32%
adjustment for 15 potential birth should be considered a chronic
of nearly 4 million live births
confounders. Disability in condition, and the primary care
annually, LPT and ET births remain
prekindergarten at 3 and 4 years of physician should glean this
a challenge, with a recent increase
age, exceptional student education, information; this would potentiate
seen in rates in the United States.
and retention in kindergarten all early diagnoses and timely
Pediatricians can continue to play an
carried a 10% to 13% increased risk intervention.59 Because of the
important role in the reduction of
among LPT infants. “Not ready to research gaps that exist, the US
these at-risk births.
start school” was borderline National Institutes of Health
significant. The authors concluded convened a multidisciplinary 1. LPT and ET infants have increased
that healthy LPT infants have conference with experts on adult risks of adverse medical,
a greater risk for developmental diseases in infants born preterm and neurodevelopmental, behavioral,
delay and school problems than term proposed a research agenda.60 and social sequelae into and
infants through the first 5 years of through adulthood. Neonatologists
life.57 and pediatricians can continue to
PRACTICAL CONSIDERATIONS
understand these risks and inform
School performance is also a concern Acceptance that early birth is not an parents, educators, and adult care
in LPT and ET infants. School inevitable and natural feature of clinicians.
performance in this group was human reproduction is the first step
2. Continued use of population data
evaluated in a cohort study at 7 years in ameliorating the societal burden of
within hospitals, states, regions,
of age in the population-based LPT and ET births.17 LPT and ET
and networks will help to monitor
prospective UK Millennium Cohort births are not caused by a single
rates of LPT and ET births for
Study with .6000 children. This entity but are the result of
trends, changes in practice, and
study used the statutory key stage 1 a heterogeneous group of conditions
need for intervention.
teacher assessment performed in the that affect the mother and/or fetus.61
third school year in England. The Potential interventions to reduce LPT 3. Promising interventions exist
primary outcome was not achieving births include the following: to prevent LPT and ET births,
the expected level ($2) in reading, but these interventions need to
1. prevention of exposure of be adopted and disseminated
writing, and mathematics. There was
pregnant women to cigarette equitably and financed by
a statistically significant increased
smoke,19 payers adequately to reduce
risk of poor performance in those
born LPT (adjusted relative risk, 1.36; 2. judicious use of non-ART fertility disparities.
95% confidence interval, 1.09–1.68). treatments and ART treatments 4. Multidisciplinary discussions and
ET infants performed statistically (eg, elective single-embryo planning with obstetric providers
significantly worse than the term transfer),39 will improve the understanding of
children in 4 of 5 individual subject 3. improvement of preconception the causes of and indications for
domains but not in the primary health to reduce chronic medical LPT and ET deliveries with the
outcome. This study concluded that conditions such as diabetes, intention of preventing iatrogenic
LPT, and to a lesser extent ET, birth obesity, and poor nutrition,15 and deliveries.18, 65
negatively affected academic 4. encouragement of longer 5. Health care providers for all age
outcomes at 7 years of age as interpregnancy interval because groups should consider obtaining
measured by key stage 1 a short interpregnancy interval of a patient’s birth history to include
assessments.58 ,6 months poses a higher risk of gestational age as
After review of 126 publications, Raju LPT delivery.62–64 a comprehensive means of
et al concluded that the Further success can be anticipated in evaluating and predicting current
overwhelming majority of adults born the future as other research and future health.48,49
at preterm gestation remain healthy discoveries are translated into clinical 6. Because these at-risk populations
and well, but adult outcomes in practice, including new approaches to of LPT and ET infants are at risk
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
PEDIATRICS Volume 144, number 5, November 2019 7
for adverse health outcomes, these Susan Wright Aucott, MD, FAAP Kasper S. Wang, MD, FACS, FAAP – Section on
groups should be added to Jay P. Goldsmith, MD, FAAP Surgery
Ivan L. Hand, MD, FAAP
payment models that better
Sandra E. Juul, MD, PhD, FAAP
finance practitioners who have to Brenda Bradley Poindexter, MD, MS, FAAP STAFF
increase their outreach, screening, Karen Marie Puopolo, MD, PhD, FAAP Jim Couto, MA
and treatment to provide Dan L. Stewart, MD, FAAP
appropriate care to these patients.
ABBREVIATIONS
LIAISONS
LEAD AUTHORS AAP: American Academy of
Wanda D. Barfield, MD, MPH, FAAP, RADM
Dan L. Stewart, MD, FAAP USPHS Pediatrics
Wanda D. Barfield, MD, MPH, FAAP, RADM Yasser El-Sayed, MD ACOG: American College of Obste-
USPHS
Erin L. Keels, DNP, APRN, NNP-BC – National tricians and Gynecologists
Association of Neonatal Nurses ART: assisted reproductive
Meredith Mowitz, MD, MS, FAAP
COMMITTEE ON FETUS AND NEWBORN, technology
Michael Ryan Narvey, MD, FAAP – Canadian
2018–2019 Paediatric Society ET: early-term
James J. Cummings, MD, FAAP, Chairperson Tonse N. K. Raju, MD, DCH, FAAP – National LPT: late-preterm
Ira S. Adams-Chapman, MD, FAAP Institutes of Health
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2019 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
1. Engle WA, Tomashek KM, Wallman C; 2017-Quarter 3, 2018. Hyattsville, MD: 13. MacDorman MF, Reddy UM, Silver RM.
Committee on Fetus and Newborn, National Center for Health Statistics Trends in stillbirth by gestational age in
American Academy of Pediatrics. “Late- NVSS, Vital Statistics Rapid Release the United States, 2006-2012. Obstet
preterm” infants: a population at risk. Program; 2019 Gynecol. 2015;126(6):1146–1150
Pediatrics. 2007;120(6):1390–1401 7. Shapiro-Mendoza CK, Lackritz EM. 14. Ananth CV, Joseph KS, Oyelese Y,
2. Raju TN, Higgins RD, Stark AR, Leveno Epidemiology of late and moderate Demissie K, Vintzileos AM. Trends in
KJ. Optimizing care and outcome for preterm birth. Semin Fetal Neonatal preterm birth and perinatal mortality
late-preterm (near-term) infants: Med. 2012;17(3):120–125 among singletons: United States, 1989
a summary of the workshop sponsored 8. Raju TNKR. The “late preterm” birth-ten through 2000. Obstet Gynecol. 2005;
by the National Institute of Child Health years later. Pediatrics. 2017;139(3): 105(5, pt 1):1084–1091
and Human Development. Pediatrics. e20163331 15. Shapiro-Mendoza CK, Barfield WD,
2006;118(3):1207–1214
9. Spong CY. Defining “term” pregnancy: Henderson Z, et al. CDC grand rounds:
3. Martin JA, Hamilton BE, Osterman MJK. recommendations from the defining public health strategies to prevent
Births in the United States, 2018. NCHS “term” pregnancy workgroup. JAMA. preterm birth. MMWR Morb Mortal
Data Brief. 2019;(346):1–8 2013;309(23):2445–2446 Wkly Rep. 2016;65(32):826–830
4. Martin JA, Hamilton BE, Osterman MJ. 10. ACOG committee opinion No 579: 16. Committee on Practice Bulletins—
Births: final data for 2017. Natl Vital definition of term pregnancy. Obstet Obstetrics, The American College of
Stat Rep. 2018;67(8):1–50 Gynecol. 2013;122(5):1139–1140 Obstetricians and Gynecologists.
Practice bulletin no. 130: prediction and
5. ACOG Committee Opinion No. ACOG 11. ACOG. Committee opinion No. 700
prevention of preterm birth. Obstet
committee opinion No. 764: medically summary: methods for estimating the
Gynecol. 2012;120(4):964–973
indicated late-preterm and early-term due date. Obstet Gynecol. 2017;129(5):
deliveries. Obstet Gynecol. 2019;133(2): 967–968 17. Newnham JP, Dickinson JE, Hart RJ,
e151–e155 et al. Strategies to prevent preterm
12. Committee opinion No. 688 summary:
birth. Front Immunol. 2014;5:584
6. Rossen LM, Osterman MJK, Hamilton BE, management of suboptimally dated
Martin JA. Quarterly Provisional pregnancies. Obstet Gynecol. 2017; 18. Hirai AH, Sappenfield WM, Ghandour
Estimates for Selected Birth Indicators, 129(3):591–592 RM, et al. The Collaborative
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
8 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Improvement and Innovation Network 29. Kaempf JW, Suresh G. Antenatal Prevention and Health Promotion,
(CoIIN) to reduce infant mortality: an corticosteroids for the late preterm Centers for Disease Control and
outcome evaluation from the US South, infant and agnotology. J Perinatol. 2017; Prevention. 2018
2011 to 2014. Am J Public Health. 2018; 37(12):1265–1267
39. Sunderam S, Kissin DM, Zhang Y, et al.
108(6):815–821
30. Dodd JM, Jones L, Flenady V, Cincotta R, Assisted reproductive technology
19. Dietz PM, England LJ, Shapiro-Mendoza Crowther CA. Prenatal administration of surveillance - United States, 2016. MMWR
CK, et al. Infant morbidity and mortality progesterone for preventing preterm Surveill Summ. 2019;68(4):1–23
attributable to prenatal smoking in the birth in women considered to be at risk 40. Institute of Medicine (US); Committee
U.S. Am J Prev Med. 2010;39(1):45–52 of preterm birth. Cochrane Database on Understanding Premature Birth and
20. ACOG. ACOG committee opinion no. 765: Syst Rev. 2013;(7):CD004947 Assuring Healthy Outcomes. The
avoidance of nonmedically indicated 31. Iams JD, Applegate MS, Marcotte MP, National Academies Collection: Reports
early-term deliveries and associated et al. A statewide progestogen Funded by National Institutes of Health.
neonatal morbidities. Obstet Gynecol. promotion program in Ohio. Obstet In: Behrman RE, Butler AS, eds. Preterm
2019;133(2):e156–e163 Gynecol. 2017;129(2):337–346 Birth: Causes, Consequences, and
21. Martin JA, Osterman MJ, Thoma ME. Prevention. Washington, DC: National
32. Romero R, Nicolaides K, Conde-Agudelo A,
Declines in triplet and higher-order Academies Press (US); 2007
et al. Vaginal progesterone in women
multiple births in the United States, with an asymptomatic sonographic short 41. Hibbard JU, Wilkins I, Sun L, et al;
1998-2014. NCHS Data Brief. 2016;(243): cervix in the midtrimester decreases Consortium on Safe Labor. Respiratory
1–8 preterm delivery and neonatal morbidity: morbidity in late preterm births. JAMA.
22. Sunderam S, Kissin DM, Crawford SB, a systematic review and metaanalysis of 2010;304(4):419–425
et al. Assisted reproductive technology individual patient data. Am J Obstet 42. Vohr B. Long-term outcomes of
surveillance - United States, 2015. Gynecol. 2012;206(2):124.e1–124.e19 moderately preterm, late preterm, and
MMWR Surveill Summ. 2018;67(3): 33. Owen J, Hankins G, Iams JD, et al. early term infants. Clin Perinatol. 2013;
1–28 Multicenter randomized trial of cerclage 40(4):739–751
23. Robbins C, Boulet SL, Morgan I, et al. for preterm birth prevention in high-risk 43. Gunay F, Alpay H, Gokce I, Bilgen H. Is
Disparities in preconception health women with shortened midtrimester late-preterm birth a risk factor for
indicators - behavioral risk factor cervical length. Am J Obstet Gynecol. hypertension in childhood? Eur
surveillance system, 2013-2015, and 2009;201(4):375.e1–375.e8 J Pediatr. 2014;173(6):751–756
pregnancy risk assessment monitoring 34. Berghella V, Rafael TJ, Szychowski JM, 44. Crump C, Sundquist K, Winkleby MA,
system, 2013-2014. MMWR Surveill Rust OA, Owen J. Cerclage for short Sundquist J. Preterm birth and risk of
Summ. 2018;67(1):1–16 cervix on ultrasonography in women epilepsy in Swedish adults. Neurology.
24. Gyamfi-Bannerman C, Thom EA. with singleton gestations and previous 2011;77(14):1376–1382
Antenatal betamethasone for women at preterm birth: a meta-analysis. Obstet
Gynecol. 2011;117(3):663–671 45. Moster D, Lie RT, Markestad T. Long-
risk for late preterm delivery. N Engl
term medical and social consequences
J Med. 2016;375(5):486–487 35. Braveman P, Heck K, Egerter S, et al. of preterm birth. N Engl J Med. 2008;
25. American College of Obstetricians and Worry about racial discrimination: 359(3):262–273
Gynecologists’ Committee on Obstetric a missing piece of the puzzle of Black-
White disparities in preterm birth? 46. Lindström K, Winbladh B, Haglund B,
Practice; Society for Maternal– Fetal
PLoS One. 2017;12(10):e0186151 Hjern A. Preterm infants as young
Medicine. Committee opinion No.677:
adults: a Swedish national cohort study.
antenatal corticosteroid therapy for 36. Profit J, Gould JB, Bennett M, et al. Pediatrics. 2007;120(1):70–77
fetal maturation. Obstet Gynecol. 2016; Racial/ethnic disparity in NICU quality
128(4):e187–e194 of care delivery. Pediatrics. 2017;140(3): 47. Laughon SK, Reddy UM, Sun L, Zhang J.
e20170918 Precursors for late preterm birth in
26. Committee on Obstetric Practice.
singleton gestations. Obstet Gynecol.
Committee opinion No. 713: antenatal 37. American College of Obstetricians and 2010;116(5):1047–1055
corticosteroid therapy for fetal Gynecologists’ Committee on Obstetric
maturation. Obstet Gynecol. 2017; Practice; Committee on Genetics; U.S. 48. Pulver LS, Denney JM, Silver RM, Young
130(2):e102–e109 Food and Drug Administration. PC. Morbidity and discharge timing of
Committee opinion No 671: perinatal late preterm newborns. Clin Pediatr
27. Kamath-Rayne BD, Rozance PJ,
risks associated with assisted (Phila). 2010;49(11):1061–1067
Goldenberg RL, Jobe AH. Antenatal
corticosteroids beyond 34 weeks reproductive technology. Obstet 49. Tomashek KM, Shapiro-Mendoza CK,
gestation: what do we do now? Am Gynecol. 2016;128(3):e61–e68 Weiss J, et al. Early discharge among
J Obstet Gynecol. 2016;215(4):423–430 38. Analyses of the National ART late preterm and term newborns and
28. Jobe AH, Goldenberg RL. Antenatal Surveillance System (NASS) data. risk of neonatal morbidity. Semin
Perinatol. 2006;30(2):61–68
corticosteroids: an assessment of Written communication with the
anticipated benefits and potential risks. Division of Reproductive Health, 50. Escobar GJ, Greene JD, Hulac P, et al.
Am J Obstet Gynecol. 2018;219(1):62–74 National Center for Chronic Disease Rehospitalisation after birth
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
PEDIATRICS Volume 144, number 5, November 2019 9
hospitalisation: patterns among infants and home care of late-preterm and birth: how often is it avoidable? Am
of all gestations. Arch Dis Child. 2005; early-term infants. Pediatrics. 2013; J Obstet Gynecol. 2009;201(4):
90(2):125–131 132(1):101–108 404.e1–404.e4
51. Wallenstein MB, Bhutani VK. Jaundice 57. Morse SB, Zheng H, Tang Y, Roth J. Early 62. Klebanoff MA. Interpregnancy interval
and kernicterus in the moderately school-age outcomes of late preterm and pregnancy outcomes: causal or
preterm infant. Clin Perinatol. 2013; infants. Pediatrics. 2009;123(4). not? Obstet Gynecol. 2017;129(3):
40(4):679–688 Available at: www.pediatrics.org/cgi/ 405–407
52. Bhutani VK, Johnson L. Kernicterus in content/full/123/4/e622
63. Ball SJ, Pereira G, Jacoby P, de Klerk N,
late preterm infants cared for as term 58. Chan E, Quigley MA. School Stanley FJ. Re-evaluation of link
healthy infants. Semin Perinatol. 2006; performance at age 7 years in late between interpregnancy interval and
30(2):89–97 preterm and early term birth: a cohort adverse birth outcomes: retrospective
53. Saluja S, Agarwal A, Kler N, Amin S. study. Arch Dis Child Fetal Neonatal Ed. cohort study matching two intervals
Auditory neuropathy spectrum disorder 2014;99(6):F451–F457 per mother. BMJ. 2014;349:g4333
in late preterm and term infants with 59. Raju TNK, Buist AS, Blaisdell CJ, Moxey- 64. Hanley GE, Hutcheon JA, Kinniburgh BA,
severe jaundice. Int J Pediatr Mims M, Saigal S. Adults born preterm: Lee L. Interpregnancy interval and
Otorhinolaryngol. 2010;74(11):1292–1297 a review of general health and system- adverse pregnancy outcomes: an
54. Quinn JM, Sparks M, Gephart SM. specific outcomes. Acta Paediatr. 2017; analysis of successive pregnancies.
Discharge criteria for the late preterm 106(9):1409–1437 Obstet Gynecol. 2017;129(3):408–415
infant: a review of the literature. Adv 60. Raju TNK, Pemberton VL, Saigal S, et al;
Neonatal Care. 2017;17(5):362–371 65. Donovan EF, Lannon C, Bailit J, et al;
Adults Born Preterm Conference
Ohio Perinatal Quality Collaborative
55. Benitz WE; Committee on Fetus and Speakers and Discussants. Long-term
Writing Committee. A statewide
Newborn, American Academy of healthcare outcomes of preterm birth: an
initiative to reduce inappropriate
Pediatrics. Hospital stay for healthy executive summary of a conference
scheduled births at 36(0/7)-38(6/7)
term newborn infants. Pediatrics. 2015; sponsored by the National Institutes of
weeks’ gestation [published correction
135(5):948–953 Health. J Pediatr. 2017;181:309–318.e1
appears in Am J Obstet Gynecol. 2010;
56. Hwang SS, Barfield WD, Smith RA, et al. 61. Holland MG, Refuerzo JS, Ramin SM, 202(6):603]. Am J Obstet Gynecol. 2010;
Discharge timing, outpatient follow-up, Saade GR, Blackwell SC. Late preterm 202(3):243.e1–243.e8
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
10 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Updates on an At-Risk Population: Late-Preterm and Early-Term Infants
Dan L. Stewart, Wanda D. Barfield and COMMITTEE ON FETUS AND
NEWBORN
Pediatrics 2019;144;
DOI: 10.1542/peds.2019-2760 originally published online October 21, 2019;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/144/5/e20192760
References This article cites 58 articles, 10 of which you can access for free at:
http://pediatrics.aappublications.org/content/144/5/e20192760#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Committee on Fetus & Newborn
http://www.aappublications.org/cgi/collection/committee_on_fetus_
_newborn
Fetus/Newborn Infant
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
Updates on an At-Risk Population: Late-Preterm and Early-Term Infants
Dan L. Stewart, Wanda D. Barfield and COMMITTEE ON FETUS AND
NEWBORN
Pediatrics 2019;144;
DOI: 10.1542/peds.2019-2760 originally published online October 21, 2019;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/144/5/e20192760
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,
60007. Copyright © 2019 by the American Academy of Pediatrics. All rights reserved. Print
ISSN: 1073-0397.
Downloaded from www.aappublications.org/news at Indonesia:AAP Sponsored on December 23, 2019
Вам также может понравиться
- Sclerema Neonatorum A Review of Nomenclature CliniДокумент9 страницSclerema Neonatorum A Review of Nomenclature CliniNoviaОценок пока нет
- Emergency Primary Assessment Skill Pediatric COVID 19 Toolkit 010120Документ8 страницEmergency Primary Assessment Skill Pediatric COVID 19 Toolkit 010120NoviaОценок пока нет
- A Comprehensive Review of Neurologic Manifestations of COVID-19 and Management of Pre-Existing Neurologic Disorders in ChildrenДокумент7 страницA Comprehensive Review of Neurologic Manifestations of COVID-19 and Management of Pre-Existing Neurologic Disorders in ChildrenNoviaОценок пока нет
- Fast, Cheap and Feasible: Implementation of Pediatric Telemedicine in A Public Hospital During The Covid-19 PandemicДокумент7 страницFast, Cheap and Feasible: Implementation of Pediatric Telemedicine in A Public Hospital During The Covid-19 PandemicNoviaОценок пока нет
- TRIANGLE Risk Assessment For Full September Opening - Covid 19Документ9 страницTRIANGLE Risk Assessment For Full September Opening - Covid 19NoviaОценок пока нет
- What Happens To Blood Glucose Concentrations After Oral Treatment For Neonatal Hypoglycemia?Документ6 страницWhat Happens To Blood Glucose Concentrations After Oral Treatment For Neonatal Hypoglycemia?NoviaОценок пока нет
- A Randomized Trial of Baby Triple P For Preterm Infants: Child Outcomes at 2 Years of Corrected AgeДокумент9 страницA Randomized Trial of Baby Triple P For Preterm Infants: Child Outcomes at 2 Years of Corrected AgeNoviaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Police BlotterДокумент4 страницыPolice BlotterArnold Cavalida Bucoy33% (3)
- Opening Doors (1) : Resources To Awaken Creative Learning - ContentsДокумент7 страницOpening Doors (1) : Resources To Awaken Creative Learning - ContentsAngie TitchenОценок пока нет
- Jurnal Tennis ElbowДокумент5 страницJurnal Tennis ElbowMuhamad Fahrizal RilahiОценок пока нет
- CIR Vs St. Luke'sДокумент32 страницыCIR Vs St. Luke'sSzia Darene MartinОценок пока нет
- Bhandara MTPДокумент2 страницыBhandara MTPAbhishek Motiram JagtapОценок пока нет
- A New Procedure For Treating A Sebaceous CystДокумент3 страницыA New Procedure For Treating A Sebaceous CystQuritaayun Zendikia LuckitaОценок пока нет
- Factors Contributing To Malnutrition Among HIV Positive Children Aged Between 6 and 60 MonthsДокумент10 страницFactors Contributing To Malnutrition Among HIV Positive Children Aged Between 6 and 60 MonthsInternational Organization of Scientific Research (IOSR)Оценок пока нет
- Care Bundles in Intensive CareДокумент4 страницыCare Bundles in Intensive CareYashoda PereraОценок пока нет
- Kel 5 Passive VoiceДокумент7 страницKel 5 Passive VoiceDesma LindaОценок пока нет
- Kartu SoalДокумент6 страницKartu SoalGetreda Oematan0% (1)
- 0824 Issue of The Daily JournalДокумент28 страниц0824 Issue of The Daily JournalSan Mateo Daily JournalОценок пока нет
- Fish & More: Seafood Retail OutletДокумент11 страницFish & More: Seafood Retail Outletranjeet vermaОценок пока нет
- MTI Act HospitilizationДокумент23 страницыMTI Act HospitilizationAli AsadОценок пока нет
- 1brisbane Final ReportДокумент49 страниц1brisbane Final ReportAustralian Human Rights100% (1)
- AUBMC Launches EpicДокумент2 страницыAUBMC Launches EpicghamОценок пока нет
- ArdsДокумент16 страницArdsCryptococcus NeoformansОценок пока нет
- ResumeДокумент2 страницыResumeapi-347141638Оценок пока нет
- FortisДокумент47 страницFortisKshitiz KadamОценок пока нет
- CDC Handbook On Birth Registration PDFДокумент61 страницаCDC Handbook On Birth Registration PDFCRGEMBACCSОценок пока нет
- Workshops, Seminars, Conferences and Symposia Attended During Assistant ProfessorДокумент4 страницыWorkshops, Seminars, Conferences and Symposia Attended During Assistant ProfessorAloah122346Оценок пока нет
- Internship Presentation ServalishsДокумент15 страницInternship Presentation Servalishsapi-334247133Оценок пока нет
- iCARE PAPER Revised..editedДокумент7 страницiCARE PAPER Revised..editedMoffat HarounОценок пока нет
- Skill Tree - Presentation HaryanaДокумент15 страницSkill Tree - Presentation Haryanas.sehgal845475Оценок пока нет
- ACOG 2009 Induction of LaborДокумент12 страницACOG 2009 Induction of LaborRiantiara PutrizaОценок пока нет
- Jaina Jose Mha 1 Year 2021-2023Документ35 страницJaina Jose Mha 1 Year 2021-2023Jaina JoseОценок пока нет
- Public Private HEM Status AsOn2May2019 4 09pmДокумент24 страницыPublic Private HEM Status AsOn2May2019 4 09pmVaibhav MahobiyaОценок пока нет
- Anaesthesia, Pharmacology, Intensive Care and Emergency A.P.I.C.E PDFДокумент253 страницыAnaesthesia, Pharmacology, Intensive Care and Emergency A.P.I.C.E PDFRatheesh KumarОценок пока нет
- JoelapplicattionДокумент4 страницыJoelapplicattionperrolobo73Оценок пока нет
- Job Description of Staff NursesДокумент3 страницыJob Description of Staff Nursesjerimiah_manzonОценок пока нет