Академический Документы
Профессиональный Документы
Культура Документы
Palliative Care Needs Assessment Guidance 01 FB
Загружено:
Diklatpimempat AngkatanlimabelasОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Palliative Care Needs Assessment Guidance 01 FB
Загружено:
Diklatpimempat AngkatanlimabelasАвторское право:
Доступные форматы
PALLIATIVE CARE NEEDS ASSESSMENT GUIDANCE
DOMAIN 1: PHYSICAL WELL-BEING DOMAIN 2: SOCIAL AND OCCUPATIONAL WELL-BEING
Patients with life limiting conditions frequently have multiple symptoms. Patient self report The family is the unit of care. When assessing patients with life-limiting illness it is
of symptoms varies from person to person. Some physical symptoms are readily reported important to explore their concerns in relation to their home, family and community,
by patients while others often require prompting. Some of the frequently encountered and to identify risk in relation to their autonomy and social functioning.
physical problems in the last year of life are outlined in table 1. Approach:
A social assessment seeks to gain some understanding of an individual’s life experience
Table 1 Frequently Encountered Physical Problems in the Last Year of Life with regard to their:
Frequently encountered physical problems in the last year of life • Background,
• Family support,
Somatic, visceral, neuropathic • Emotional and social support,
Pain Take a detailed pain history outlining • Practical concerns.
• Location, quality, intensity, duration, frequency Table 2 Suggested Prompts; Social and Occupational Well-being Assessment
• Associated/aggravating/relieving factors
• Treatment interventions to date Suggested Prompts
Fatigue Fatigue disproportionate to level of activity or not relieved by rest Invite discussion about family and relationships:
Family Support • Who lives with you?
Respiratory Dyspnoea, cough, oropharyngeal secretions
• Any children/adult dependents?
Gastrointestinal Anorexia, nausea, vomiting, constipation • any concerns/worries regarding family or personal relationships?
Neurological Insomnia, confusion, delirium, anxiety, depression Do you have any other support for example PHN, home help, private
carers, friends, neighbours?
Other Functional status, balance problems, oedema, wound problems Emotional and
• How often do you see them?
social support
• Do you need more support?
This is neither a prescriptive nor an exhaustive list- it serves to illustrate the variety of physical • What would help?
problems encountered and need for systematic assessment to identify physical problems
Discussion about practical issues:
Approach: • How are you managing?
• An introductory question to prompt the person to identify the physical needs of most • Any difficulties in: mobilising, managing the stairs, household
concern to them. Practical chores e.g. washing, cooking, etc?
• Thereafter a thorough and careful systems review will determine the presence and concerns and • Any concerns about future care needs, income, finances, sorting
severity of physical symptoms. advance care out your affairs?
After identification of symptoms: planning • What are the person’s wishes regarding:
• Elicit a history of symptoms including previous treatments received. – Goals of care?
• Ascertain the effect of the problem on the patient’s normal activities function. – Acceptable levels of intervention?
• Consider treatment options. – Preferred place of care (person and family)?
After identification of concerns:
Action: • Ascertain the effect of the problem on the patient’s normal activities function.
• Agree and implement a care plan with the patient and multidisciplinary team. • Consider treatment options.
• Establish whether these symptoms can be managed by the current treating team.
• If severe or intractable physical problems are identified or anticipated, consider referral Action:
to the specialist palliative care service. • Agree and implement a care plan with the patient and multidisciplinary team.
• Establish whether these symptoms can be managed by the current treating team.
• If severe or intractable physical problems are identified or anticipated, consider referral
to the specialist palliative care service.
DOMAIN 3: PSYCHOLOGICAL WELL-BEING DOMAIN 4: SPIRITUAL WELL-BEING
Patients with life limiting conditions frequently have psychological concerns. In order People have many different understandings to the word spiritual and how it impacts
to identify these concerns, it is important that the assessor is proactive in asking about on their lives. When completing spiritual assessment, assessors need to be aware of
emotional and psychological issues. alternative terms i.e. faith, belief, philosophy, religion, inner strength.
Approach: Approach:
Begin with an open exploratory question that invites the person to identify any An introductory question/s to alert individuals to a change in focus from clinical is
concerns. “Is there anything worrying you?” required e.g. How has this illness impacted on your life? The following is a suggested
Followed by consideration of the following: approach to assessment:
• Mood and interest
• Adjustment to illness
• Resources and strengths Table 4 Suggested Prompts: Spiritual Well-Being Assessment
• Uncontrolled multidimensional pain (total pain)
• Pre-existing mental illness
Suggested Prompts
Table 3 Suggested Prompts; Psychological Well-Being Sources of hope What gives you hope (strength, comfort peace) in the time
H
Suggested Prompts of illness?
• How is your mood?
• During the last month have you: O Organised religion Are you part or member of religious or spiritual community?
– been feeling down and/or hopeless? Does it help you?
– lost enjoyment in interests?
Mood and interest Personal
• Are you depressed? What aspect of your spiritual beliefs do you find most
• Do you feel tense or anxious? P spirituality & helpful and meaningful personally?
• Have you ever had a panic attack? practices
• Are there things you are looking forward to?
Adjustment to Effect on medical How do your beliefs affect the kind of care you would like
• What is your understanding of your illness? E
illness care and end of me to provide over the next few days/weeks/months?
Resources and • What is a source of support for you? life issues
strengths • Look for a range of possible supports: people, hobbies, faith, beliefs
After identification of concerns:
Uncontrolled multidimensional pain e.g. psychosocial, emotional, • Elicit history of concerns including previous supports/interventions received.
spiritual pain; consider if distress contributing to physical symptoms • Ascertain the effect of the problem on the patient’s normal activities/function.
Total pain
• Are there psychological, social, emotional, spiritual issues that • Consider treatment strategies/interventions.
may be contributing to symptoms?
Action
Pre-existing mental Persons with a history of current or past mental health problems
• Agree and implement a care plan with the patient and multidisciplinary team. This may
illness may be particularly at risk of psychological distress
include referral to pastoral care service.
After identification of concerns • Establish whether these needs can be managed by the current treating team.
• Elicit history of concerns including previous supports/interventions received. • If significant complex spiritual concerns are identified or anticipated, consider referral
• Ascertain the effect of the problem on the patient’s normal activities/function. to specialist palliative care service.
• Consider treatment options/interventions.
Action:
• Agree and implement a care plan with the patient and multidisciplinary team. See Palliative Care Needs Assessment Guidance accessible on
• Establish whether these needs can be managed by the current treating team. www.hse.ie/palliativecareprogramme
• If significant complex family and social concerns are identified or anticipated, consider NATIONAL CLINICAL PROGRAMME FOR PALLIATIVE CARE
referral to the Specialist Palliative Care Service.
Вам также может понравиться
- General Principles and Empirically Supported Techniques of Cognitive Behavior TherapyОт EverandGeneral Principles and Empirically Supported Techniques of Cognitive Behavior TherapyОценок пока нет
- Presentation 1 Deminsion ClassДокумент14 страницPresentation 1 Deminsion ClassMalikaJamesОценок пока нет
- Week 13Документ2 страницыWeek 13Juan Miguel TevesОценок пока нет
- Lesson Plan PP and CsДокумент36 страницLesson Plan PP and CsMamta SinghОценок пока нет
- Psych PDFДокумент11 страницPsych PDFBetina De Jesus0% (1)
- Clin MidtermДокумент9 страницClin MidtermAlexandraОценок пока нет
- Case Presentation InterviewДокумент10 страницCase Presentation Interviewapi-576594451Оценок пока нет
- Aug22 Mental HealthДокумент30 страницAug22 Mental HealthAmy Villa100% (1)
- Chapter 1Документ20 страницChapter 1Shiela BadiangОценок пока нет
- CaregiverfatigueДокумент1 страницаCaregiverfatigueapi-235628879Оценок пока нет
- Psych First AidДокумент42 страницыPsych First AidLady Love Cagas Andin-oОценок пока нет
- Reviewer For P1Документ4 страницыReviewer For P1Mindi May AguilarОценок пока нет
- Ncma111 Lecture & Laboratory - Final: Geriatic AdaptationДокумент29 страницNcma111 Lecture & Laboratory - Final: Geriatic AdaptationBb PrintsОценок пока нет
- Psychia NotesДокумент6 страницPsychia NotesMaria Theresa BuscasОценок пока нет
- 3 Use of Health Promotion Diagnoses at Every StageДокумент27 страниц3 Use of Health Promotion Diagnoses at Every Stagemedinna31100% (1)
- Moral Distress Moral Distress Moral Distress Moral Distress: - Fekadu Aga Fekadu AgaДокумент15 страницMoral Distress Moral Distress Moral Distress Moral Distress: - Fekadu Aga Fekadu AgaKimem EshetuОценок пока нет
- Tma 1 Prep & Block 1 Intro SlidesДокумент64 страницыTma 1 Prep & Block 1 Intro SlidesashleygvieiraОценок пока нет
- Protocolo AnsiedadДокумент6 страницProtocolo AnsiedadGabriela Espinosa ArreagaОценок пока нет
- P5. VIII - Mental Illnes - Siti Meilan SimbolonДокумент16 страницP5. VIII - Mental Illnes - Siti Meilan Simbolonsiti simbolonОценок пока нет
- Dep SlidesДокумент64 страницыDep SlidesYetnayet BekeleОценок пока нет
- Cancer Burden: Global Picture. Number of New Cancer Cases (In Millions)Документ5 страницCancer Burden: Global Picture. Number of New Cancer Cases (In Millions)Samantha BolanteОценок пока нет
- HERO-Ethiopia Module 1Документ52 страницыHERO-Ethiopia Module 1RahelAdmasuОценок пока нет
- Ocd 2022Документ30 страницOcd 2022jenОценок пока нет
- Lesson 6 STRESSДокумент37 страницLesson 6 STRESSjcaramat.dpnОценок пока нет
- Health, Illness, & NursingДокумент31 страницаHealth, Illness, & NursingLoo DrBradОценок пока нет
- Mental Health Last Minutes Notes-Week 1 To Week 5Документ17 страницMental Health Last Minutes Notes-Week 1 To Week 5Zxn SxhОценок пока нет
- Case Vignette Discussion Slides and Case ExamplesДокумент28 страницCase Vignette Discussion Slides and Case ExamplesSena UysakОценок пока нет
- Coping PPT - Class - StudentДокумент32 страницыCoping PPT - Class - StudentkatrinasdОценок пока нет
- Domains of Activities:: Roles and Functions of Psychiatric NursesДокумент3 страницыDomains of Activities:: Roles and Functions of Psychiatric NursesAfif Al BaalbakiОценок пока нет
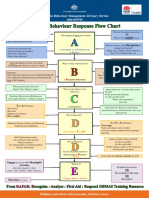
- Behaviour Response Flow Chart 5 Nov 2012Документ1 страницаBehaviour Response Flow Chart 5 Nov 2012jakilaОценок пока нет
- Biopsychosocial ModelДокумент12 страницBiopsychosocial Modelkatg121387Оценок пока нет
- Mental Health Awareness Presentation - Based On Maria and Ian's POTS TrainingДокумент37 страницMental Health Awareness Presentation - Based On Maria and Ian's POTS TrainingAbdull azizОценок пока нет
- DBTДокумент46 страницDBTDiana Davis100% (1)
- PFA Service Provider Self CareДокумент2 страницыPFA Service Provider Self CareHanna CostalesОценок пока нет
- HERO-Ethiopia Module 2Документ24 страницыHERO-Ethiopia Module 2RahelAdmasuОценок пока нет
- Treating PTSD During The COVID-19 Virus OutbreakДокумент50 страницTreating PTSD During The COVID-19 Virus OutbreakmniosoОценок пока нет
- PFA Appx CProviderCareДокумент6 страницPFA Appx CProviderCareAlicia NataОценок пока нет
- Outline of A Case Study ReportДокумент5 страницOutline of A Case Study ReportJedda Punzalan100% (1)
- Expectancies vs. Expectations: PH 303 Study Guide For Final Exam (Semi-Cumulative) Social Cognitive TheoryДокумент14 страницExpectancies vs. Expectations: PH 303 Study Guide For Final Exam (Semi-Cumulative) Social Cognitive TheoryMay CorpuzОценок пока нет
- Introduction To Evidence-Based Practice For Cpnes: Identify The Problem/OpportunityДокумент8 страницIntroduction To Evidence-Based Practice For Cpnes: Identify The Problem/OpportunityFranklyn ChamindaОценок пока нет
- Psychosocial Issues Associated With Acquired DisabilitiesДокумент71 страницаPsychosocial Issues Associated With Acquired DisabilitiesnesumaОценок пока нет
- Role of A Nurse in Palliative CareДокумент31 страницаRole of A Nurse in Palliative CareSophia Alexa Cassandra AlcantaraОценок пока нет
- CHN Quiz Coverage PDFДокумент4 страницыCHN Quiz Coverage PDFKatrina EstoconingОценок пока нет
- Teori Health BehaviorДокумент50 страницTeori Health BehaviorGilangОценок пока нет
- Self-Care: Good For You and Your Work: Ellen Newman Projects Coordinator Hunter Institute of Mental HealthДокумент36 страницSelf-Care: Good For You and Your Work: Ellen Newman Projects Coordinator Hunter Institute of Mental HealthErwin Y. CabaronОценок пока нет
- TCIS Study GuideДокумент2 страницыTCIS Study GuideAndrew100% (2)
- 306 Localpresentation 0Документ60 страниц306 Localpresentation 0mitesh20281Оценок пока нет
- Coping PPT Without Notes (1) - 3Документ35 страницCoping PPT Without Notes (1) - 3katrinasdОценок пока нет
- Psychosocial Assessment Questions Week 2 Class 3Документ10 страницPsychosocial Assessment Questions Week 2 Class 3parisa.ahmed97Оценок пока нет
- Day 02Документ36 страницDay 02Kazi NishatОценок пока нет
- Managing Challenging Behaviours SlidesДокумент110 страницManaging Challenging Behaviours SlidesPhttii phttiiОценок пока нет
- Evangelista Chapter 7Документ8 страницEvangelista Chapter 7Ellyza EvangelistaОценок пока нет
- Using Fam HLTH Model For FFC 2.2018Документ29 страницUsing Fam HLTH Model For FFC 2.2018Sharon DenhamОценок пока нет
- Abnormal Psychology AAДокумент94 страницыAbnormal Psychology AAIzabellaОценок пока нет
- Inpatient Drug Addiction Treatment Program at Las Vegas Recovery Center - Phase 1Документ6 страницInpatient Drug Addiction Treatment Program at Las Vegas Recovery Center - Phase 1Las Vegas Recovery CenterОценок пока нет
- Formulation and The Biopsychosocial Model Introduction For Psychiatry ResidentsДокумент10 страницFormulation and The Biopsychosocial Model Introduction For Psychiatry ResidentsLennard Ashley Salaysay100% (5)
- Orientation & Introduction To Mental Health 2017Документ27 страницOrientation & Introduction To Mental Health 2017James BrooksherОценок пока нет
- ICF SwallowingДокумент2 страницыICF SwallowingMarcela Sanhueza GarridoОценок пока нет
- Health 7 2nd QuarterДокумент13 страницHealth 7 2nd QuarterceanОценок пока нет
- Three Stage ProtocolДокумент1 страницаThree Stage ProtocolDiklatpimempat AngkatanlimabelasОценок пока нет
- Aphn Covid-19 PDFДокумент2 страницыAphn Covid-19 PDFDiklatpimempat AngkatanlimabelasОценок пока нет
- Clinical Frailty ScaleДокумент2 страницыClinical Frailty ScaleDiklatpimempat Angkatanlimabelas0% (1)
- Ethical Issues at The End of LifeДокумент7 страницEthical Issues at The End of LifeDiklatpimempat AngkatanlimabelasОценок пока нет
- SAS - Symptom Assessment ScaleДокумент1 страницаSAS - Symptom Assessment ScaleDiklatpimempat Angkatanlimabelas100% (1)
- SAS - Symptom Assessment ScaleДокумент1 страницаSAS - Symptom Assessment ScaleDiklatpimempat Angkatanlimabelas100% (1)
- Pceolc On AnonfileДокумент2 страницыPceolc On AnonfileDiklatpimempat AngkatanlimabelasОценок пока нет
- Core Competencies in Palliative Care - An EAPC White Paper On Palliative Care Education - Part 1 FBДокумент12 страницCore Competencies in Palliative Care - An EAPC White Paper On Palliative Care Education - Part 1 FBDiklatpimempat AngkatanlimabelasОценок пока нет
- Core Competencies in Palliative Care - An EAPC White Paper On Palliative Care Education - Part 2 FBДокумент6 страницCore Competencies in Palliative Care - An EAPC White Paper On Palliative Care Education - Part 2 FBDiklatpimempat AngkatanlimabelasОценок пока нет
- Jurnal ADHDДокумент9 страницJurnal ADHDjul yanОценок пока нет
- Understanding Personality DisorderДокумент58 страницUnderstanding Personality DisorderMaría Isabel Trujillo MayaОценок пока нет
- CBT - Case StudiesДокумент3 страницыCBT - Case StudiesArati KandolkarОценок пока нет
- PANSS Scoring CriteriaДокумент13 страницPANSS Scoring CriteriaSalzabila Bustam100% (2)
- Stress: A Concept Analysis: Patricia M. Goodnite, RN-BCДокумент4 страницыStress: A Concept Analysis: Patricia M. Goodnite, RN-BCJose Alonso Aguilar ValeraОценок пока нет
- Rimestad, T Al. (2016) - Short-And Long-Term Effects of Parent Training For Preschool Children With or at Risk of ADHD. Sistematic ReviewДокумент12 страницRimestad, T Al. (2016) - Short-And Long-Term Effects of Parent Training For Preschool Children With or at Risk of ADHD. Sistematic ReviewjuanОценок пока нет
- KuesionerДокумент121 страницаKuesionerAlpascaFirdaus100% (1)
- Wender Utah SpanishДокумент4 страницыWender Utah SpanishScribdTranslationsОценок пока нет
- 2018 Geriatric Psychiatry PDFДокумент738 страниц2018 Geriatric Psychiatry PDFNungki100% (10)
- Explorative Essay Rough DraftДокумент6 страницExplorative Essay Rough Draftapi-238508557Оценок пока нет
- Videbeck - Psychiatric Mental Health Nursing - NewДокумент27 страницVidebeck - Psychiatric Mental Health Nursing - NewJohnrey Tesoro0% (1)
- Fernandez Doctor - Goya's Mental Illness 1994Документ6 страницFernandez Doctor - Goya's Mental Illness 1994FranciscoОценок пока нет
- Discussion: Answer The Following QuestionsДокумент11 страницDiscussion: Answer The Following QuestionsAndrew Del RosarioОценок пока нет
- Health Promotion Seminar PlanДокумент4 страницыHealth Promotion Seminar Planapi-242399744Оценок пока нет
- Chapter 1 Lesson 1Документ8 страницChapter 1 Lesson 1Aizel ManiagoОценок пока нет
- Abnormal Psychology Case Studies 2-3Документ2 страницыAbnormal Psychology Case Studies 2-3AceОценок пока нет
- Adolescent HealthДокумент19 страницAdolescent Healthhou1212!67% (3)
- Workbook On Personal-Social Responsibility and WellnessДокумент9 страницWorkbook On Personal-Social Responsibility and WellnessJp Isles MagcawasОценок пока нет
- Solution Focused With AdolescentsДокумент28 страницSolution Focused With AdolescentsAlina Purdea100% (1)
- A Cognitive Interpersonal Therapy WorkbookДокумент256 страницA Cognitive Interpersonal Therapy WorkbookPedro IborraОценок пока нет
- The Beacon - May 3, 2012Документ20 страницThe Beacon - May 3, 2012schaffnerpubОценок пока нет
- Anna Higgins PDF ResumeДокумент2 страницыAnna Higgins PDF Resumeapi-271079545Оценок пока нет
- 04 Handout 1 PerdevДокумент2 страницы04 Handout 1 PerdevKing CjОценок пока нет
- The Bridge, November 3, 2016Документ24 страницыThe Bridge, November 3, 2016The BridgeОценок пока нет
- NIH Public Access: Author ManuscriptДокумент19 страницNIH Public Access: Author Manuscripta_l_y_nОценок пока нет
- Subjective Data: Short Term Goal: IndependentДокумент1 страницаSubjective Data: Short Term Goal: IndependentVanetОценок пока нет
- Code of EthicsДокумент1 страницаCode of EthicsJoshua R. CruzОценок пока нет
- Obsessive-Compulsive Disorder (OCDДокумент22 страницыObsessive-Compulsive Disorder (OCDaliОценок пока нет
- C C CC C C C C C C: Introducing Listening ParticipatingДокумент11 страницC C CC C C C C C C: Introducing Listening ParticipatingRENJULALОценок пока нет
- Bullying Argument EssayДокумент2 страницыBullying Argument EssayRaisa Pitas MalayОценок пока нет