Академический Документы
Профессиональный Документы
Культура Документы
Prevalence of Depressive and Anxious Disorders in An Area of The Family Health Strategy in The Southern Region of Tocantins
Загружено:
IJAERS JOURNALОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Prevalence of Depressive and Anxious Disorders in An Area of The Family Health Strategy in The Southern Region of Tocantins
Загружено:
IJAERS JOURNALАвторское право:
Доступные форматы
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
Prevalence of depressive and anxious disorders
in an area of the Family Health Strategy in the
Southern Region of Tocantins
Mariana Ferreira Bucar∗, Sávia Denise Silva Carlotto Herrera∗, Alice
Magalhães Faleiro, Elisa Palmeira Calil Fonseca, Caroline Rufoni, Vinicius
Lopes Marinho, Yuniel Martínez Hernández, Warly Neves de Araújo ∗,
Florence Germaine Tible Lainscek
*Corresponding Authors: marianafb28@gmail.com (M ariana Ferreira Bucar), saviadenise@hotmail.com (Sávia Denise Silva Carlotto
Herrera), warlynevesaraujo@gmail.com (Warly Neves de Araújo)
Emails: alicefaleiro@hotmail.com (Alice M agalhães Faleiro); elisapcf@hotmail.com (Elisa Palmeira Calil Fonseca);
danny.926rc@gmail.com (Daniela Rodrigues de Castro Silva); vinicius.marinho22@gmail.com (Vinicius Lopes M arinho);
dryuniel@gmail.com (Yuniel M artínez Hernández); fg.tl@hotmail.com (Florence Germaine Tible Lainscek)
Abstract—Introduction: Mental disorders are among the main causes of morbidity today and represent 22 to
25% of the care provided by the Family Health Strategy. Among them, depressive and anxious disorders are
emphasized. Objective: To verify the prevalence and clinical-epidemiological profile of patients with depressive
and anxious disorders and to analyze access to the mental health care network in an area of the Family Health
Strategy in the southern region of Tocantins. Methodology: This is an analytical, observational, cross-sectional
research of patients with anxious and depressive disorders of the Seville Basic Health Unit in Gurupi -TO, from
August to October 2018. Through a form completed by the physician during consultations, with variables:
epidemiological, chronic diseases, life habits, psychiatric disorder, non-pharmacological and pharmacological
treatments. Descriptive analysis of the data with the help of Microsoft Excel. Results and Discussion: 141 patients
participated in the study, with a prevalence of 5,59% o f depression and anxiety. Mostly with anxiety, women,
brown race, age group from 18 to 29 years and 50 to 59 years, occupation of the home, with incomplete second
degree, and with partner. Presenting systemic arterial hypertension and diabetes mellitus as comorbidities, they
did not adopt physical and pleasurable activities such as non-pharmacological treatment, on regular use of
antidepressants and/or anxiolytic, and follow-up only in the basic health unit. Conclusion: the prevalence of
patients with anxiety and depression was 5.59%, the study contributed to the characterization of these patients,
providing information that can be used to improve mental health care.
Keywords—Family Health Strategy. Primary Health Care. Research on Health Services. Mental Disorders.
I. INTRODUCTION According to the World Health Organizatio n
The perception of behavior went through several (WHO), one in four people in the world will be affected
classifications during history. Currently, the term "mental by a mental disturbance at a given stage of life [5] .
disorder" or "mental disorder" is used in order to reduce Studies show that there are millions of patients with
the stigma of psychological conditions [1]. mental illness in the world, there is also a progressive
Mental disorders are considered one of the main increase in [6] [7] [8].
causes of morbidity in current societies [2], represent Among mental disorders and behavior, depressive
four of the top ten causes of disability [3]. They reach and anxious disorders stand out, which in turn many
biological, cultural, social, economic and political people are diagnosed simultaneously with both
dimensions [4], contemplating the whole conditions [7]. The current criteria for the diagnosis of
mental disorders are characterized by the 5th edition of
biopsychosocial landscape, and still very neglected [5].
www.ijaers.com Page | 127
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
the Diagnostic and Statistical Manual of Mental of access of teams to patients [16].
Disorders [9]. Therefore, the Family Health Strategy (FHS) is
Depressed mood, loss of interest or pleasure, considered one of the gateways for patients with
feelings of guilt or low self-esteem, feelings of psychological complaints [12]. On average, 22 to 25%
uselessness, change in sleep pattern or appetite may be of the people assisted by the FHS present mental
present in those diagnosed with depressive disorders. disorders and require comprehend - sive and continuing
While anxious disorders refer to feelings of fear and
health care [15]. The greater proximity of the FHS, daily
anxiety, being classified into disorders: generalized
and continuous can determine more appropriate
anxiety, panic, phobias, posttraumatic stress and others
management of mental disorders in the long term and
[10].
also identify the relationship with environmental, family
In 2015, there were 322 million people in the
and community factors [17].
world living with depression, with a prevalence of
Given the various challenges of primary health
females and peak age group between 60 and 64 years, and
care, it is necessary to know the profile of depressive
of these, approximately 15% were in the Americas. In
mental disorders and anxious in primary care for the
Brazil, it reached 11.548.577 people, which
identification of the current reality. Since there is a
corresponded to 5,8% of the population [7]. By 2020, shortage of epidemiological studies of psychiatric
depression is estimated to reach second place in the disorders, making this research timely.
Disability Adjusted Life Years ranking after cardiac Thus, the present study describes the prevalence
ischemic diseases [6] [8]. and characterizes the clinical-epidemiolog ical profile of
Regarding anxiety disorders, while 264 million of patients with depressive and anxious disorders, as well
the world’s population had these disorders, 21% of them as analyzes their access to the mental health care network
belonged to the Americas and 18.657.943 were Brazilian in an area of health strategy of Family from the southern
in 2015 [7]. region of Tocantins in order to guide prevention projects,
Mental disorders are of paramount importance to contribute to the health promotion and quality of life of
public health, due to their chronic and disabling nature, these patients.
and because they are related to increased risk for
communicable and non-communicable diseases, and II. MATERIALS AND METHODS
also these patients are more likely not to adhere to The analytical, observational and cross-sectional
research was carried out at the Seville Basic Health Unit
treatment, which negatively affects their health [4] [11].
in Gurupi – Tocantins, from August to October 2018.
Borges [12] and collaborators point out that This study strictly obeyed Resolution number. 466/ 2012
"current public policies in mental health in Brazil of the National Health Council and approved by the
recommend that people with mental disorders be Ethics Committee on Research in Human Beings (CEP)
followed concomitantly in primary health care and in of Gurupi University (UNIRG) under opinion number.
specialized units". 2.820.700/ 2018.
The integration of the health network occurs Data collection occurred during the medical
through the reference and counter-reference process consultation based on the form containing epidemiological
between the different levels of complexity of the and clinical variables – gender, marital status, skin color,
services. However, it is emphasized that there is a failu re age group, occupation, schooling, residents of the house,
in this process among the s ervices of the network [13]. family income, housing, chronic diseases, life habits,
It is observed that treatment for these patients is psychiatric disorder, non-pharmacological treatment and
usually available for cases of greater severity or pharmacological treatment, and access to the health
requiring hospitalization and that comprehensiveness in network – use of health resources and need for referral to
meeting the needs of the population and the inequalities other health levels in the last 12 months. The collection
of the health and disease process, still need to be occurred from 8/27/2018 to 31/10/2018.
improved [6] [14]. The sample of this study consisted of 141 patients
So that mental health care will materialize through diagnosed with anxiety disorder and/or depressive
its strengthening and its articulation with primary care disorder confirmed during consultation and/or medical
[15]. Primary health care should allow the first access of records of both sexes, aged 18 years or older, and who
voluntarily signed the Free and Informed Consent Fo rm
people who demand mental health care, due to the ease
www.ijaers.com Page | 128
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
(FICF). noteworthy that the sample consisted of convenience
Patients with other mental disorders, and encompassing only patients diagnosed with mental
disabilities, physical or intellectual disorders were disorders who attended medical consultations in August
excluded to provide the information requested in data to October 2018.
collection, and those who were not in the unit area and The Mental Health Care Protocol states that the
who only attend for prescription renewal. overall prevalence of anxiety disorders in the adult
After data collection, the data was transferred to Brazilian population is 18% and that in all countries
the Google Forms platform form and transposed to a depression reaches up to 11% of the population at a
spreadsheet in Microsoft Excel®. The prevalence of certain time and throughout life, 20%. There is also a
anxious and depressive disorders was calculated, relationship of approximately 60% comorbidity between
considering the population universe of 2.520 patients. depression and generalized anxiety in primary care [18].
And the absolute and relative frequencies of each The prevalence rate in this study was lower than
variable analyzed were calculated considering the sample expected. The limitations of the results are recognized
of 141 patients. Presented the results descriptively, because it is a cross-sectional study, and the data are
mentioned in the text and in tables - Table 1 describes the measured only once and be delimited to a region of the
epidemiological profile of anxious and depressive urban area of a single city and by sampling being for
disorders, Table 2 refers to the housing conditions of convenience and not active search.
these patients and Table 3 characterizes the non- Tied to this, it is believed the short period of time
treatment pharmacological and pharmacological. of data collection; the great demand only for renewal of
prescriptions rather than new consultations for clinical
III. RESULTS AND DISCUSSION evaluation; refusal to participate in research for fear and
The Seville Basic Health Unit of Gurupi - prejudice; not every population in the studied area
Tocantins serves approximately 11,500 inhabitants. attends the basic health unit; and the stigma and
During the data collection period, 2,520 patients over 18 ignorance of mental disorders; all this influenced the
years of age were treated, where only 141 patients with results. Regarding the epidemiological profile of patients
anxious and depressive disorders signed the FICF with anxious and depressive disorders in this area of FHS
fulfilling the inclusion criteria of this study, there were in the southern region of Tocantins it was observed that
more patients diagnosed with AD and DD, however, the majority were: women, brown race, age group fro m
because they did not accept, they were excluded from the 18 to 29 years and 50 to 59 years, occupation of the
study. home, second degree marital status with partner (Table
The prevalence of anxiety and depression 1).
disorders was 5,59% in the population studied. It is
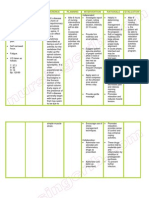
Table 1. Epidemiological profile of patients with anxious and depressive disorders in an area of Family Health Strategy in
the Southern Region of Tocantins, 2018.
Relative frequency
SEX n
(% )
Female 113 80,1
Male 28 19,9
AGE GROUP n %
18 the 29 years 35 24,82
30 the 39 years 18 12,77
40 the 49 years 24 17
50 the 59 years 35 24,82
60 the 69 years 15 10,64
70 years or more 14 9,93
SKIN COLOR n %
Yellow 5 3,55
White 21 14,9
Black 33 23,4
www.ijaers.com Page | 129
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
Brown 82 58,2
OCCUPATION n %
Student 25 17,0
Signed wallet 21 14,0
Standalone (a) 13 9,22
From home 50 35,0
Unemployed 13 9,22
Retired (a) / Pensioner 19 13,0
SCHOOLING n %
Illiterate (a) 5 3,55
Incomplete first degree 48 34
Full first grade 11 7,8
Incomplete second degree 11 7,8
Full second degree 33 23,4
Incomplete higher education 21 14,9
Complete higher education 12 8,51
MARITAL SITUATION n %
Single (a) 42 29,8
With companion (a) 67 47,5
Divorced/Separated (a) 15 10,6
Widower (a) 17 12,1
RESIDENTS IN THE HOUSE n %
1 person 16 11,35
2 or 3 people 80 56,74
4 people or more 45 31,91
FAMILY INCOME n %
≤ 1 minimum wage 57 40,4
1 to 2 minimum wages 2 1,42
2 to 3 minimum wages 61 43,3
4 to 6 minimum wages 14 9,93
≥ 7 minimum wages 7 4,96
HOUSING n %
Own 111 78,7
Rented 25 17,7
Borrowed/donated 5 3,55
Legend: n = number of patients.
In this study, most individuals with mental common among women, white race, adults with shorter
disorders belonged to females (80,1%), 51,1% (n = 72) school education time and people who do not have a
diagnosed with anxious disorders, 12% (n = 17) with stable marital relationship, causing a negative impact for
depressive disorders and 18% (n = 25) with both. Only their patients and family members [6] [11]. Regarding
14,9% (n = 21) males had anxious disorders and 4,3% (n age group, there was a predominance of anxiety and
= 6) depressive. depressive disorders between 18 and 29 years and 50
Females are considered a predictor factor of greater years; followed from 40 to 49 years (17%); 30 to 39 years
search for health care [19]. Studies show that in Brazil, but (12,77%); 60 to 69 years (10,64%); and 9,93% in those
women seek health services more than men [20] [21] . aged 70 years or older. Regarding race, there was a
Mental disorders are present in up to 20% of women and predominance of brown with 58,2%, followed by 23,4%
black patients, 14,9% of the white race and only 3,55%
mood and anxiety disorders are more common, [22]
yellow.
corroborating the findings of this study.
In a medium-sized municipality in the Midwest
As well as depression, which is also more
region of Brazil, the highest prevalence of commo n
www.ijaers.com Page | 130
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
mental disorder was in women, divorced or separated, she was married or living with someone as if married
yellow race, age group from 18 to 59 years, occupation (63,1%) [25].
of the home, with 4 to 7 years of study, monthly income For some authors, marital dissatisfaction is
of up to 1 salary of minimum and who lived in borrowed related to depression in women and dysthymia in men .
or donated housing [4]. Therefore, married women would have a higher risk of
In the evaluation of individuals with mental depression than single women, as well as divorced
disorders of a reference unit for family health program in women [24].
Santa Cruz do Sul, Rio Grande do Sul, it was found that In this study, it was verified how much family and
69,4% were female, with an average age of 37,96 years, housing conditions, that patients with mental disorders
and 62,9% attended the first degree incomplete, and lived with 1 or 2 more people, mostly with family income
94,6% had monthly income of up to three min imu m of 2 to 3 minimum wages (43,3%) and who lived in their
wages [23]. own home (78,7%).
A higher relationship between mental disorders in Patients with anxious and depressive disorders
this study was observed with the occupation of the home describe the number of residents in the house in 56,74%
35% (n = 50), followed by 17% (n = 25) of students, 14% as 2 or 3 people, followed by 31,91% as 4 people or more,
(n = 21) with signed portfolio, 13% (n = 19) retired (a) or and only 11,35% reside alone. Most patients in this study
pensioner, 9,22% (n = 13) of self-employed (a) and have their own home (78,7%), and the others live in
9,22% unemployed (a). rented homes (17,7%) and borrowed or donated (3,55%).
In another study conducted in primary care, the Family income corresponds to 2 to 3 min imu m
predominant categories among patients with Commo n wages in 43,3% of patients; followed by 40,4% living on
Mental Disorders were “from home” and self-employed . less or 1 minimum wage; 9,93% with 4 to 6 min imu m
The authors explain that this tendency to mental wages; 4,96% with 7 or more; and 1,42% between 1 and
disorders is related to the fact that women who perfo rm 2 minimum wages. It is believed that individuals with
domestic activities, isolate themselves at home and give incomes of up to one minimum wage were more likely to
up the consequent socialization of a professional develop Common Mental Disorder [4].
environment. While those so-called self-employed, that Among the 141 patients, the prevalence of patients
is, informal workers experience situations such as with anxious disorders was 66% (n = 93), depressive
uncertainty about the work situation [4]. disorders 16% (n =23) and 18% (n = 25) had both
The level of education found in this study was the diagnoses.
second incomplete grade corresponding to 34% of the It was found in this study that 39% (n = 55) of
total, followed by that with a complete second degree patients with depressive and anxious disorders practiced
(23,4%), incomplete higher education (14,9%), and physical activity, 16% (n = 22) used alcoholic beverages,
complete higher education (8,51%). Those with 13% (n = 18) smoked and 3% (n = 4) used illicit drugs.
complete first grade and incomplete second grade Authors state that smoking is directly related to anxiety
represented 7,8% each, and only 3,5% illiterate. disorders, especially in females, and also with depressive
In Lucchese study [4]and collaborators found that disorders, especially major depressive disorder [26].
respondents who were less likely to have common In a study with patients with depressive disorders,
mental disorders reported having four to seven years of 23% stated that they used tobacco and 2% of alcoholic
studies, and that the lower the number of years of study, beverages. Smoking interferes with neurotransmitter
the lower the number of years of study, the more than a metabolism and alters cytochrome P450 enzyme activity
factor related to the presence of no due to the difficulty of [24]. In another study, it was noted that 26,3% patients
insertion in the labor market. As Silva says [24]et al. that with anxiety or depressive disorders were smokers [25].
as the level of education decreases, the probability of Regarding the comorbidities of this study, 38% (n
presenting higher levels of depressive symptoms = 53) have systemic arterial hypertension (SAH), 12% (n
increases. = 17) diabetes mellitus (DM), 10% (n = 14)
Regarding marital status, it was observed that the hypothyroidism and none of the patients reported the
majority had a partner (a) representing 47,5% of the 141
diagnosis of dementias. While in Machado study [27]and
patients, 29,8% were single, 10,6% divorced/separated
collaborators, clinical data from elderly people with
(as), and 12,1% widowed (as). Like most patients with
anxious disorders showed that 31% reported presenting
anxious disorders in another psychiatric outpatient study,
SAH.
www.ijaers.com Page | 131
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
About anxious and depressive disorders activity. Among the classes most cited as
according to non-pharmacological and pharmacological pharmacological treatment are anxiolytics and
treatment (Table 2), it was noted that 14% (n = 20) of antidepressants and although most consider their
patients with anxious disorders practiced physical adherence to regular treatment, they stated only partial
activity; and 14,4% (n = 2) of those with depressive improvement.
disorders practiced physical activity and pleasurable
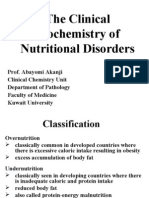
Table 2. Characterization of the treatment of patients with anxious and depressive disorders in an area of Family Health
Strategy in the Southern Region of Tocantins, 2018.
Anxious and
Depressive
Anxious disorders depressive
disorders
disorders
n % n % N %
NON-PHARMACOLOGICAL
TREATMENT
Physical activity 20 14 % 9 6,4 % 7 5%
Pleasurable activities 14 9,9 % 3 2,1 % 4 2,8 %
Physical and pleasurable activities 7 5% 2 14,4 % 1 0,7 %
No activity 51 36 % 9 6,4 % 13 9,2 %
They did not report 1 0,7 % 0 0% 0 0%
PHARMACOLOGICAL
TREATMENT
Anxiolytics 10 7,1 % 2 1,4 % 1 0,7 %
Antidepressants 25 18 % 9 6,4 % 12 8,5 %
Association and/or other classes of
9 6,4 % 9 6,4 % 7 5%
medications
No medication 49 35 % 3 2,1 % 5 3,5 %
They did not report 0 0% 0 0% 0 0%
ADHERENCE TO
PHARMACOLOGICAL
TREATMENT
Regular use 30 21 % 18 13 % 11 7,8 %
Irregular use 9 6,4 % 0 0% 4 2,8 %
Abandonment or suspension 14 9,9 % 1 1,7 % 5 3,5 %
You're not in treatment 40 28 % 4 2,8 % 5 3,5 %
They did not report 0 0% 0 0% 0 0%
RESPONSE TO
PHARMACOLOGICAL
TREATMENT
No improvement 2 1,4 % 0 0% 1 0,7 %
Partial improvement 23 16 % 7 5% 13 9,2 %
Total improvement 19 13 % 13 9,2 % 6 4,3 %
You're not in treatment 47 33 % 3 2,1 % 5 3,5 %
They did not report 2 1,4 % 0 0% 0 0%
Legend: n = number of patients. % = relative frequency.
Approximately 50% of patients with mental activities, as well as in an- other study in Itapuranga-GO
disorders do not perform physical and/or pleasurable that considered low the practice of physical exercises and
www.ijaers.com Page | 132
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
also suggests that physical activity helps in the mental health outpatient clinic, and only 2 patients were
rehabilitation of patients with psychological disorders, psychosocial care centers (CAPS).
acting as a "catalyst for interpersonal relationships and Since 11,34% (n = 16) claim to have achieved
stimulating the overcoming of small challenges" [24]. referral to other levels of care by the SUS, 8,51% (n =
Regarding pharmacological treatment, about 40% 12) did not achieve referral, and 68,8% (n = 97) did not
were not on use of any medication. Most patients with require access to other health levels.
anxious disorders used antidepressants (18%) and Regarding the time of referral for psychiatric
anxiolytics (7,1%). Furthermore, 6,4% cited other specialist, 0,7% (n = 1) was attended from 15 days to 1
pharmacological classes and/or drug associations, such month; 1,41% (n = 2) between 1 and 2 months; 3,54% (n
as antidepressant with anticonvulsant; anxiolytic, = 5) between 2 and 3 months; 4,96% (n = 7) had not yet
antidepressant and antipsychotic; anxiolytic and been attended. And 81,5% (n = 115) were not referred to
antidepressant; anxiolytic and anticonvulsant. the psychiatrist.
When asked about adherence to pharmacological While the referral time for care with a
treatment, 4,8% (n = 59) stated regular use of psychologist was for 0,7% (n = 1) up to 15 days; 1,41%
medications, 9,2% (n = 13) irregular use and 15,1% (n = (n = 2) between 15 days and 1 month; 0,7% (n = 2) fro m
20) abandoned or suspended treatment. Some of the 1 to 2 months; 0,7% (n = 1) from 4 to 5 months; 11,3%
justifications for the abandonment of treatment were: (n = 16) were not seen and 79,4% (n = 112) were not
fear of prejudice and influence of the family. forwarded.
Non-adherence to pharmacological treatment is a In a research in the Family Health Program in
complex and universal phenomenon, and when it comes Santa Cruz do Sul, Rio Grande do Sul, patients with
to psychiatric therapy, a worsening of diseases with mental disorders presented a higher number of
possible relapses and increased time for recovery is consultations with general practitioners and/or family
physicians, specialists and emergency in the last 12
noticed [28].
months, as well as schedules for some type of health
The improvement in pharmacological treatment
was considered total in about 26% (n = 38) of patients service [23]. The physician considered general
and partial by 34% (n = 43). In their minority, they practitioner is the most active in mental health in Brazil
reported not getting improvement. Corroborating the and other countries, such as England, USA, and Canada
interviewees from another study that the highest [24].
prevalence occurred among patients who improved Despite all impasse, it was observed that most
(74%) [24]. patients performed follow-up only in the basic health
Some researchers say that 3% of the Brazilian unit, demonstrating the resolution of primary care in the
population, that is, 5 million people, needed continuous southern region of Tocantins. However, it was observed
care for severe and persistent mental disorders, and that there is still difficulty in accessing other levels of
another 9% need eventual care related to less serious care that provided specialized care with psychologists
and psychiatrists with an average delay of 2 to 5 months.
disorders, totaling 20 million Brazilians [28].
Primary health care is the level of the health
IV. CONCLUSION
system responsible for providing the population with the
Knowledge of the profile of patients and the
necessary care for their most common health problems ,
environment in which they live becomes strategic for
including preventive, curative, rehabilitation and health
planning and improvements in mental health. In this
promotion measures [8]. study, there was a prevalence of anxiety and depressive
Data such as these demonstrate the need for a disorders of 5,59%. And the profile of patients with
well-structured mental health care network for better anxious and depressive disorders of a Family Health
monitoring and promotion of quality of life. Strategy area in the southern region of Tocantins was
Regarding the care network for mental health presented, which corresponded to women, of the brown
patients, in the last 12 months 14% (n = 27) required care race, aged 18 to 29 years and 50 to 59 years, of the home,
with psychiatric specialist and 2,83% (n = 4) emergency with incomplete second degree, and with companion.
care. Mostly diagnosed as anxious disorder, presenting
In the sample of this study 70,92% (n = 100) were systemic arterial hypertension and diabetes mellitus as
followed only in the basic health unit; 23,4% (n = 33) comorbidities, did not adopt physical and pleasurable
performed psychotherapy; 13,47% (n = 19) attended the activities such as non-pharmacological treatment, on
www.ijaers.com Page | 133
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
regular use of antidepressants and/or anxiolytic, with [7] WHO, WORLD HEALTH ORGANIZATION. Depression
clinical improvement considered partial and follow-u p and other Common M ental Disorders. Global Health
Estimates. 2017.
only in the basic health unit.
[8] Wenceslau LD, Ortega F. Mental health in primary care
Mental disorders in primary health care are
and Global Mental Health: international perspectives and
common, it is remarkable in this scenario the non-
Brazilian scenario. Interface (Botucatu). 2015; 19 (55):
adherence to treatment, difficulty in referral to 1121-1132.
specialized care (psychiatrist and psychotherapy) and [9] American Psychiatry Association. Diagnostic and
still family disarrangement due to difficulty in care of Statistical Manual of Mental disorders - DSM-5. 5th.ed.
these patients. Conferring a great impact on the lives of Washington: American Psychiatric Association, 2013.
patients with mental disorders. [10] Carvalho, A. Depression, and other common mental
The results demonstrated the importance of disorders: global and national framework and resource
epidemiological studies in mental health with the reference in emerging cases. General Health Directorate,
2017.
identification of risk groups in the studied region, which
[11] Forman-Hoffman VL, Batts KR, Hedden S, Spagnola K,
will allow discussion with the health team in search of Bose J. Comorbid M ental Disorders among Adults in the
strategies for prevention and health promotion. In M ental Health Surveillance Survey. Annals of
addition, they revealed the reality of access to Epidemiology. 2018.
specialized care. [12] Borges, T.L., Hegadoron, K.M ., M iasso, A.I. Common
The importance of primary care in the studied mental disorders and the use of psychotropic drugs in
area as a gateway to and offering health services to the women assisted in basic health units in a Brazilian urban
community is emphasized. However, there is a need for center. Panam. Mag. Salud Publish. 2015; 38 (3): 195-201.
articulation to facilitate access to specialized [13] Hilário, L.D. Inclusion of mental health actions in primary
care. 36 f. M onograph (Undergraduate Nursing) -
consultations promoting integrality in mental health
UNIVATES University Center, Lajeado, 2015.
care.
[14] Santos, T.V.C., Penna, C.M .M . Daily demands in primary
It is believed that the presence and valorization of care: the view of health professionals and users. Text and
professionals with their own training at this level of the Nursing Context. 2013; 22 (1):149-56.
health system is a differential in the quality of mental [15] Cabral, T.M .N., Albuquerque, P.C. M ental health from the
health services. As a suggestion for future research to be perspective of Community Health Agents: the perception
conducted, it is necessary to identify the general realit y of those who care. Health debate. 2015; 39 (104): 159-171.
of primary mental health care and also implemen t [16] BRASIL. M inistry of Health. Department of Health Care.
Department of Primary Care. M ental Health /M inistry of
instruments for screening mental disorders.
Health, Department of Health Care, Department of Primary
Care, Department of Strategic Programmatic Actions. –
REFERENCES
Brasilia: M inistry of Health, 2013.
[1] Assis, P. A brief manual of mental disorders: an
[17] Binotto, A.L. Epidemiological profile of patients with
introductory guide to psychopathology and diagnostic
mental disorders followed in primary health care. 76 f.
classification systems. 2010.
Dissertation (M aster's degree in Social M edicine) –
[2] Apostolo, J.L.A., Figueiredo, M .H., M endes, A.C.,
Ribeirão Preto School of M edicine, University of São
Rodrigues, M .A. Depression, anxiety and stress in primary
Paulo,2014.
health care users. Journal Latin American Nursing. 2011;
[18] FLORIANÓPOLIS, City Hall. Mental Health Care
19 (2): 6 Screens.
Protocol. M unicipal Health Secretary - M ental Health
[3] Carlotto M S. Common M ental Disorders in Workers of
Program, 2010.
Basic Health Units: Prevalence and Associated Factors.
[19] Levorato, C.D., M ello, L.M ., Silva, A.S., Nunes, A.A.
Psycho. Argum. 2016; 34 (85): 133-146.
Factors associated with the search for health services from
[4] Lucchese, R., Sousa, K., Bonfin, S.P., Vera, I., Santana,
a gender relational perspective. Science Collective Health,
F.R. Prevalence of common mental disorder in primary
2014; 19 (4).
care. Acta Paul. nursing. 2014; 27 (3): 200-7.
[20] Ribeiro, M .M . Use of Health Services in Brazil: an
[5] Cruz, D.P., Sena, E.L.S., M oreira, R.M ., Teixeira, J.R.B.,
investigation of the age standard by sex and coverage by
Lira, L.S.S.P., Anjos, K.F., Santos, V.C. Clinical-
health insurance [dissertation]. Belo Horizonte: Federal
epidemiological profile of patients treated in a psychiatric
University of M inas Gerais; 2005.
outpatient clinic. Cuban Magazine of Enfermería. 2014; 30
[21] Travassos, C., Viacava, F., Pinheiro, R., Brito, A Use of
(3).
health services in Brazil: gender, family characteristics,
[6] M olina, M .R.A.L., Wiener. C.D., Branco, J.C., Jansen, K.,
and social condition. Panam. Mag. Salud Publish, 2002; 11
Souza, L.D.M ., Tomasi, E., Silva, A.R.A., Pinheiro, R.T.
(5/6): 365-373.
Prevalence of depression in users of primary care units.
[22] Kassada, D.S., Waidman, M .A.P., M iasso, A.I., M arcon,
Clinical Psychiatry Journal. 2012; 39 (6): 194-7.
www.ijaers.com Page | 134
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol -7, Issue-1, Jan- 2020]
https://dx.doi.org/10.22161/ijaers.71.16 ISSN: 2349-6495(P) | 2456-1908(O)
S.S. Prevalence of mental disorders and associated factors
in pregnant women. Acta Paul. nursing. 2015; 28 (6): 495-
502.
[23] Gonçalves, D.M ., Kapczinski, F. Prevalence of mental
disorders in individuals from a reference unit for Family
Health Program in Santa Cruz do Sul, Rio Grande do Sul,
Brazil. Notebook. Public Health, 2008; 24 (9): 2043-2053.
[24] Silva, L.S., Sousa, T.F., M artins, W.L.L., Cunha, V.C.M .,
Cunha, C.R.M ., Fernandes, C.K.C. Epidemiological
profile of depressive disorder of patients treated at the basic
pharmacy of the municipality of Itapuranga-GO. Montes
Belos College Magazine (FM G) (FMB), 2014; 8 (1): 1-16.
[25] M unaretti, C.L., Terra, M .B. Anxiety disorders: a
prevalence and comorbidity study with smoking in a
psychiatric outpatient clinic. Brazilian Journal Psychiatry,
2007; 56 (2): 108-115.
[26] Vasconcelos, T.C., Dias, B.R.T., Andrade, L.R., M elo,
G.F., Barbosa, L., Souza, E. Prevalence of Anxiety and
Depression Symptoms in M edical Students. Brazilian
Journal of Medical Education, 2015; 39 (1): 135-142.
[27] M achado, M .B., Ignácio, Z.M ., Jornada, L.K., Réus, G.Z.,
Abelaira, H.M ., Arent, C.O., Schwalm, M .T, Ceretta, R.A.,
Ceretta, L.B., Quevedo, J. Prevalence of anxious disorders
and some comorbidities in the elderly: a population-based
study. Brazilian Journal Psychiatry, 2016; 65 (1): 28-35.
[28] Cardoso, L., Galera, S.A.F. M ental patients and their
profile of adherence to psychopharmacological treatment.
Nursing School Magazine USP, 2009; 43 (1): 161-167.
www.ijaers.com Page | 135
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Mental Health Class NotesДокумент3 страницыMental Health Class Notessuz100% (4)
- Nursing Care Plan Pott's DiseaseДокумент2 страницыNursing Care Plan Pott's Diseasederic95% (21)
- Accupressure EyeДокумент7 страницAccupressure Eyemayxanh1234100% (3)
- Ozone Unsung Hero by Navy Captain - Ajit VadakayilДокумент153 страницыOzone Unsung Hero by Navy Captain - Ajit Vadakayilsudhir shahОценок пока нет
- Tof Care PlanДокумент4 страницыTof Care Plankayal67% (12)
- Sanum Therapy Book Helios PDFДокумент314 страницSanum Therapy Book Helios PDFOscarОценок пока нет
- Timed Up and Go Test RalanДокумент1 страницаTimed Up and Go Test RalanBagus Andi PramonoОценок пока нет
- Facing Dengue and Malaria As A Public Health Challenge in BrazilДокумент6 страницFacing Dengue and Malaria As A Public Health Challenge in BrazilIJAERS JOURNALОценок пока нет
- Enhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionДокумент6 страницEnhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionIJAERS JOURNALОценок пока нет
- Business Logistics and The Relationship With Organizational SuccessДокумент4 страницыBusiness Logistics and The Relationship With Organizational SuccessIJAERS JOURNALОценок пока нет
- Climatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninДокумент8 страницClimatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninIJAERS JOURNALОценок пока нет
- Beef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaДокумент7 страницBeef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaIJAERS JOURNALОценок пока нет
- Impacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicДокумент7 страницImpacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicIJAERS JOURNALОценок пока нет
- Analysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingДокумент11 страницAnalysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingIJAERS JOURNALОценок пока нет
- Childhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationДокумент12 страницChildhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationIJAERS JOURNALОценок пока нет
- Associativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMДокумент9 страницAssociativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMIJAERS JOURNALОценок пока нет
- Study of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractДокумент8 страницStudy of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractIJAERS JOURNALОценок пока нет
- Humanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveДокумент12 страницHumanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveIJAERS JOURNALОценок пока нет
- The Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaДокумент4 страницыThe Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaIJAERS JOURNALОценок пока нет
- Breastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewДокумент16 страницBreastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewIJAERS JOURNALОценок пока нет
- Design and Building of Servo Motor Portable Coconut Peller MachineДокумент5 страницDesign and Building of Servo Motor Portable Coconut Peller MachineIJAERS JOURNALОценок пока нет
- Constructed Wetlands: Technology For Removing Drug Concentration From WaterДокумент12 страницConstructed Wetlands: Technology For Removing Drug Concentration From WaterIJAERS JOURNALОценок пока нет
- Multiprofessional Care For A Patient With Gestational DiabetesДокумент12 страницMultiprofessional Care For A Patient With Gestational DiabetesIJAERS JOURNALОценок пока нет
- Morphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaДокумент9 страницMorphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaIJAERS JOURNALОценок пока нет
- Water Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaДокумент11 страницWater Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaIJAERS JOURNALОценок пока нет
- VCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodДокумент6 страницVCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodIJAERS JOURNAL100% (1)
- Association of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixДокумент15 страницAssociation of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixIJAERS JOURNALОценок пока нет
- Process Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47Документ5 страницProcess Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47IJAERS JOURNALОценок пока нет
- Komla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)Документ9 страницKomla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)IJAERS JOURNALОценок пока нет
- The Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsДокумент8 страницThe Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsIJAERS JOURNALОценок пока нет
- Modeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilДокумент5 страницModeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilIJAERS JOURNALОценок пока нет
- Sociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilДокумент9 страницSociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilIJAERS JOURNALОценок пока нет
- Mining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaДокумент7 страницMining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaIJAERS JOURNALОценок пока нет
- Detection and Control of Bacterial BiofilmsДокумент15 страницDetection and Control of Bacterial BiofilmsIJAERS JOURNALОценок пока нет
- Assessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsДокумент13 страницAssessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsIJAERS JOURNALОценок пока нет
- Does Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyДокумент12 страницDoes Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyIJAERS JOURNALОценок пока нет
- Study Evaluating The Ability of Fe-BDC-PEG To Carry and Release Active Ingredient 5-FluorouracilДокумент5 страницStudy Evaluating The Ability of Fe-BDC-PEG To Carry and Release Active Ingredient 5-FluorouracilIJAERS JOURNALОценок пока нет
- DLP in Health 10 Global Health InitiativesДокумент10 страницDLP in Health 10 Global Health InitiativesJoshua MaravillasОценок пока нет
- Brain Biochemistry and DisordersДокумент191 страницаBrain Biochemistry and DisordersTrajce PasowskyОценок пока нет
- Lesson 10: Sexual Aspect of Self: Name: Ramil D Malapo Course: BEEDДокумент15 страницLesson 10: Sexual Aspect of Self: Name: Ramil D Malapo Course: BEEDJOANA MANAOGОценок пока нет
- Science 6 Endocrine SystemДокумент39 страницScience 6 Endocrine Systemcharmaine_olivia_1100% (1)
- Global Manual On Surveillance of AEFIДокумент128 страницGlobal Manual On Surveillance of AEFIHarold JeffersonОценок пока нет
- What Is Rheumatoid ArthritisДокумент16 страницWhat Is Rheumatoid ArthritisDurge Raj GhalanОценок пока нет
- Gold Awards: Organization Name Title of InnovationДокумент10 страницGold Awards: Organization Name Title of Innovationchek86351Оценок пока нет
- Plan Training Session: Trainers Methodology Level I Templates Document No. Issued By: Ntta Page I of VIIДокумент31 страницаPlan Training Session: Trainers Methodology Level I Templates Document No. Issued By: Ntta Page I of VIIBenevict L. IbañezОценок пока нет
- An Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsДокумент15 страницAn Analysis of Taiwan's Vaccination Services and Applications For Vaccine Injury CompensationsAnonymous FNZ3uR2AHsОценок пока нет
- Bite Force and Occlusion-Merete Bakke 2006Документ7 страницBite Force and Occlusion-Merete Bakke 2006Dan MPОценок пока нет
- Analytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajДокумент7 страницAnalytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajyusufОценок пока нет
- Daily RevisionДокумент13 страницDaily RevisionHanime hubОценок пока нет
- Assis 2017Документ19 страницAssis 2017widyadariОценок пока нет
- Lecture 32 - Nutritional DisordersДокумент43 страницыLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Chap 79Документ5 страницChap 79Ma.Nicole SubongОценок пока нет
- Mental Retardation Treatment and ManagementДокумент12 страницMental Retardation Treatment and ManagementMelchoniza CalagoОценок пока нет
- Dental Hygiene Bab 15Документ28 страницDental Hygiene Bab 15Cinta SalsabilaОценок пока нет
- FWD Medical Rider enДокумент12 страницFWD Medical Rider enKhairul HMSBОценок пока нет
- Requests For MED3 Fit Note': Covid-19 Guidance For PracticesДокумент2 страницыRequests For MED3 Fit Note': Covid-19 Guidance For Practicesplayjake18Оценок пока нет
- Liver Pathology EMQДокумент1 страницаLiver Pathology EMQhazirmm100% (2)
- Setting The Standard: Managing Food Allergies in SchoolДокумент50 страницSetting The Standard: Managing Food Allergies in SchooldadowildcatsОценок пока нет
- Febrele HemoragiceДокумент21 страницаFebrele HemoragiceRotaru MihaiОценок пока нет
- 109 513 1 PB PDFДокумент11 страниц109 513 1 PB PDFKolu koyОценок пока нет