Академический Документы
Профессиональный Документы
Культура Документы
Lancetpsychiatryarchitectureofchange
Загружено:
max viejaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Lancetpsychiatryarchitectureofchange
Загружено:
max viejaАвторское право:
Доступные форматы
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/319429422
Architecture of change: rethinking child and adolescent mental health
Article in The Lancet Psychiatry · September 2017
DOI: 10.1016/S2215-0366(17)30315-2
CITATIONS READS
13 308
3 authors:
Andrea Raballo Michele Poletti
Università degli Studi di Perugia Azienda Unità Sanitaria Locale Reggio Emilia
181 PUBLICATIONS 2,455 CITATIONS 140 PUBLICATIONS 1,602 CITATIONS
SEE PROFILE SEE PROFILE
Patrick D Mcgorry
Orygen The National Centre of Excellence in Youth Mental health
1,227 PUBLICATIONS 51,182 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Altered bodily experience and basic self-disturbance in multimodal hallucinations View project
Psychotic risk detection in children and adolescents View project
All content following this page was uploaded by Michele Poletti on 05 September 2017.
The user has requested enhancement of the downloaded file.
Comment
Now is an exciting time for scientists interested in the 1 Agrawal A, Nelson EC, Bucholz KK, et al. Major depressive disorder, suicidal
thoughts and behaviours, and cannabis involvement in discordant twins:
mental health effects of cannabis exposure. The study a retrospective cohort study. Lancet Psychiatry 2017; published online
by Agrawal and colleagues1 takes an important step July 24. http://dx.doi.org/10.1016/S2215-0366(17)30280-8.
2 Sherva R, Wang Q, Kranzler H, et al. Genome-wide association study of
in disentangling the relationships between cannabis cannabis dependence severity, novel risk variants, and shared genetic risks.
use, depression, and suicidal thoughts and behaviours, JAMA Psychiatry 2016; 73: 472–80.
3 Carey CE, Agrawal A, Bucholz KK, et al. Associations between polygenic risk
and I anticipate further research on this subject. The for psychiatric disorders and substance involvement. Front Genet 2016;
7: 149.
hypotheses presented in Agrawal and colleagues1 are
4 Silins E, Horwood LJ, Patton GC, et al, for the Cannabis Cohorts Research
not mutually exclusive, and should not be read as Consortium. Young adult sequelae of adolescent cannabis use:
an integrative analysis. Lancet Psychiatry 2014; 1: 286–93.
such. Cannabis use is probably related to depression 5 Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of
and suicidal behaviours through a constellation of marijuana use. N Engl J Med 2014; 370: 2219–27.
6 Schreiner AM, Dunn ME. Residual effects of cannabis use on neurocognitive
mechanisms, including shared genetic predispositions, performance after prolonged abstinence: a meta-analysis.
worsened societal outcomes, and environmental Exp Clin Psychopharmacol 2012; 20: 420–29.
7 ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC. Changes in
traumas resulting from cannabis use effecting mental cannabis potency over the last 2 decades (1995–2014): analysis of current
health outcomes, and also cannabis use directly data in the United States. Biol Psychiatry 2016; 79: 613–19.
8 Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit
mediating depression and suicidal behaviours through drug users. Drug Alcohol Depend 2007; 88: 188–96.
altered neurobiology. Successful social and medical 9 Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its
consequences: evidence from a longitudinal study of men with dual diagnoses
intervention strategies for suicide prevention and of mental illness and substance abuse. J Health Soc Behav 1997; 38: 177–90.
10 Mark Anderson D, Hansen B, Rees DI. Medical marijuana laws, traffic
reduction of cannabis use must consider and address fatalities, and alcohol consumption. J Law Econ 2013; 56: 333–69.
these hypotheses concurrently. 11 Morris RG, TenEyck M, Barnes JC, Kovandzic TV. The effect of medical
marijuana laws on crime: evidence from state panel data, 1990–2006.
PLoS One 2014; 9: e92816.
Laura M Huckins 12 Anderson DM, Rees DI, Sabia JJ. Medical marijuana laws and suicides by
gender and age. Am J Public Health 2014; 104: 2369–76.
Icahn School of Medicine, Psychiatric Genomics, New York, NY
10128, USA
laura.huckins@mssm.edu
I declare no competing interests.
Architecture of change: rethinking child and adolescent
mental health
The comprehensive, pan-European survey1 by the mental health services compared with all other age
MILESTONE Consortium on the architecture and groups.3–5 Thus, the division of mental health care along
functioning of childhood and adolescent mental health the paediatric or adult model, inspired by the traditional
Jim Reed Photography/Science Photo Library
services (CAMHS) clearly indicates that there are more organisation of somatic medicine, is unfortunate, as
differences than commonalities across European Union this division cuts across the age when risk for mental
countries. Besides the macroscopic heterogeneity, another disorders peaks, with obvious consequences in terms of
glaring problem is that “the organisation of services and undertreatment, discontinuity of care, and unmet needs.
the distribution of resources are often not based on users’ Furthermore, the developmental and cultural challenges
perspectives and needs, as they should be”.1 of transition to adulthood also now span a much longer
Such heterogeneity and distance from users’ needs— period, and extend at least into the mid-to-late twenties
which is plausibly also true on a global scale —is even in developed countries and increasingly within countries
more problematic as it fails to match the epidemiological with rapidly developing economies. Fast-paced economic,
burden of disease2 or the natural pattern of emerging cultural, technological, demographic, and social
mental disorders in young people. Indeed, young changes are responsible for this increase in challenge
people aged 12–25 years have the highest incidence and duration. Mental health care provision to immigrant and
prevalence of mental illness across the lifespan, while refugee youth is increasingly needed, and new morbid
also having the worst access to and engagement with phenomena are arising, such as social withdrawal with
656 www.thelancet.com/psychiatry Vol 4 September 2017
Downloaded for Anonymous User (n/a) at Azienda Unita Sanitaria Locale di Reggio Emilia from ClinicalKey.com by Elsevier on August 29, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Comment
internet addiction, cyberbullying, or hazardous social developmental psychopathology and follow the
games (eg, the so-called Blue Whale, a game played across multiple longitudinal fluctuations from subsyndromal
various social media platforms that allegedly encourages to syndromal states and back, with related changes in
some teenagers to attempt suicide).6,7 Hence, we cannot the intensity of the need of care.8,9
postpone a radical review of the structure and resourcing Moreover, such a model enables shifting of the
of health care for young people in transition from strategic focus from disease-specific interventions in
childhood to adulthood any longer. To be sustainable, this adulthood, to preventive low-threshold interventions
review should be guided by emerging research evidence in adolescence, which could be key to reducing disease
from the new youth mental health framework and burden and related costs in a global phase of increasing
transnational standards of care, and should ultimately demands and stable or deflating resources.10,11 Within
be reflected in the development and implementation of this perspective, enhancing resilience and targeting
international guidelines for novel service systems, such transdiagnostic modulators, such as emotion regulation
as are already being created and scaled up internationally. and social skills, could be a good compromise between
This approach would reorient and strengthen national timing and specificity of interventions.8–11 The substantial
health services and facilitate the integration of country- framework shift from existing CAMHS and adult mental
specific approaches and traditions within a broader and health services—which basically provide delayed and
future-oriented framework. Clearly, such creation of heavily restricted access to a small subgroup of people
youth-friendly primary care platforms, and structural with overt, severe, and complex disorders—is evident.
redevelopment and enhancement of contemporary The emphasis in youth-oriented interventions should
CAMHS, represents an excellent value proposition for move from symptom reduction and containment to
governments concerned with spiralling costs of health prevention, early intervention, and ultimately much
and social services, who are seeking a strong return on greater social and economic participation. The world
investment. This proposition is also a huge opportunity to has changed substantially in the past three decades, yet
bridge the serious gap between child–adolescent and adult service organisation has remained largely unchanged,
psychiatry. Bridging this gap might be achievable through embryonic, under-resourced, and mostly anchored
a framework shift that incorporates the full continuum to the post-asylum era mission. In this sense, the
of service response within a promotion and prevention transnational heterogeneity, poor access, and flawed
framework for youth mental health. Indeed, besides the transitions revealed by the MILESTONE survey1 suggest
quality and accessibility of youth mental health, a crucial that simple (although laudable) incremental change is
driving principle should be the stepwise gradient of unlikely to go anywhere close to meeting the unique
increasing intensity and specificity of treatment, inspired developmental and socio-cultural needs of adolescents.
by a developmentally informed clinical staging model.8,9 Rather, international mental health policies should be
Youth mental disorders affect motor, cognitive, much more ambitious and explore preventive strategies
language, learning, and behavioural development, with that are better suited to the developmental pattern of
lifelong consequences. Thus, timely identification in the mental vulnerabilities across the lifespan. A viable and
early phases is a major prerequisite for interventions overdue first step in this direction would be to reorient
that aim to positively modify the natural course of primary care and existing services towards youth-specific
these disorders, with potentially exponential cascading mental healthcare. 12
effects on long-term quality of life and socioemotional
functioning.8–10 Taking into account the developmental *Andrea Raballo, Michele Poletti, Patrick McGorry
stage of the person is essential in this sense, not only to Department of Psychology, Psychopathology and Development
Research, Norwegian University of Science and Technology
ensure a personalised or stratified treatment approach,
(NTNU), Trondheim N-7491, Norway (AR); Department of Mental
but also to promote smooth access pathways into Health and Pathological Addiction, Reggio Emilia Local Health
services and encourage participation and hope in families Trust, Reggio Emilia, Italy (MP); and Orygen (The National Centre
and carers.1 of Excellence in Youth Mental Health) and Centre for Youth Mental
Adoption of a transdiagnostic staging model Health, University of Melbourne, Parkville, VIC, Australia (PM)
andrea.raballo@ntnu.no
could provide a more suitable framework to capture
www.thelancet.com/psychiatry Vol 4 September 2017 657
Downloaded for Anonymous User (n/a) at Azienda Unita Sanitaria Locale di Reggio Emilia from ClinicalKey.com by Elsevier on August 29, 2017.
For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Comment
PM reports personal fees from Janssen Cilag and Lundbeck. PM has a patent 7 Inkster B, Stillwell D, Kosinski M, Jones P. A decade into Facebook: where is
PCT/AU2008/001337 pending to Orygen Youth Health Research Centre. All psychiatry in the digital age? Lancet Psychiatry 2016; 3: 1087–90.
other authors declare no competing interests. This work was supported by the 8 McGorry P, van Os J. Redeeming diagnosis in psychiatry: timing versus
Norwegian University of Science and Technology (NTNU) Onsager Fellowship specificity. Lancet 2013; 381: 343–45.
programme in Psychopathology and Development. 9 Raballo A, Larøi F. Clinical staging: a new scenario for the treatment of
psychosis. Lancet 2009; 374: 365–67.
1 Signorini G, Singh SP, Boricevic-Marsanic V, et al. Architecture and
functioning of child and adolescent mental health services: a 28-country 10 McGorry P, Nelson B. Why we need a transdiagnostic staging approach to
survey in Europe. Lancet Psychiatry 2017; 4: 715–24. emerging psychopathology, early diagnosis, and treatment.
JAMA Psychiatry 2016; 73: 191–92.
2 Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on
adolescent health and wellbeing. Lancet 2016; 387: 2423–78. 11 Singh SP, Tuomainen H. Transition from child to adult mental health
services: needs, barriers, experiences and new models of care.
3 Eyre O, Thapar A. Common adolescent mental disorders: transition to
World Psychiatry 2015; 14: 358–61.
adulthood. Lancet 2014; 383: 1366–68.
12 McGorry PD, Goldstone SD, Parker AG, Rickwood DJ, Hickie IB. Cultures for
4 Rice F, Eyre O, Riglin L, Potter R. Adolescent depression and the treatment
mental health care of young people: an Australian blueprint for
gap. Lancet Psychiatry 2017; 4: 86–87.
reform. Lancet Psychiatry 2014; 1: 559–68.
5 The Lancet Psychiatry. Hunting down an evidence base for adolescent
mental health. Lancet Psychiatry 2017; 4: 83.
6 Krausz RM, Choi F. Psychiatry’s response to mass traumatisation and the
global refugee crisis. Lancet Psychiatry 2017; 4: 18–20.
New policy and evidence on suicide prevention
Published Online Suicide prevention has rarely had such a high locality, and the growing concern over non-fatal self-
May 23, 2017
http://dx.doi.org/10.1016/
public profile in the UK as in the past 6 months, harm in young people. The strategy also emphasised
S2215-0366(17)30238-9 which have seen a series of publications covering the need to find ways to reduce male suicide, to
policy, practice, and research evidence. Perhaps treat depression in primary care, to strengthen acute
the key moment was in January, 2017, when UK mental health care, and to support families bereaved
Prime Minister Theresa May launched an updated by suicide. The original strategy,3 published in 2002,
national suicide prevention strategy in England,1 part had overseen a decrease in the national suicide rate,
of a suite of announcements on mental health with which reached a historically low figure in 2006–07.
young people and social justice as prominent themes. However, by 2012, when the strategy was relaunched,4
In her speech, May referred to the “shocking reality”2 of the suicide rate had increased following the worldwide
13 suicides per day in England. recession,5 when instability in the international
The updated national strategy emphasised two banking sector caused harm to the lives of vulnerable
things: the need for suicide prevention plans in every people. Figures for 2015 and 2016 suggest that the
increase has reversed, the main reduction being in
Panel: Key elements of safer care in mental health services men aged 40–60 years, the group in whom the post-
1 Safer wards recession rise also occurred, but in 2016 there were
• Removal of ligature points still 4540 suicides registered in England, with a male to
• Reduction in absconding female ratio of three to one.6,7
• Skilled inpatient observation The updated strategy drew on evidence from the
2 Care planning and early follow-up after discharge from
national confidential inquiry,8 whose 2016 report
hospital to community
3 No out of area admissions for acutely ill patients presented an analysis of suicides by mental health
4 24 h crisis resolution and home treatment teams patients over the preceding 20 years up to 2014.
5 Community outreach teams to support patients who This report noted an increasing number of suicides
might lose contact with conventional services by patients with mental disorders, but a decreasing
6 Specialised services for alcohol and drug misuse and dual
patient suicide rate. Crisis teams were highlighted as a
diagnosis
7 Multidisciplinary review of patient suicides, with input priority for suicide prevention: around 200 suicides per
from family year occur in patients under crisis teams, three times
8 Implementation of National Institute for Health and as many as in inpatient care. However, crisis teams
Clinical Excellence guidance on depression and self-harm are not inherently unsafe; the national confidential
9 Personalised risk management, without routine checklists
inquiry report also found improved patient safety
10 Low turnover of non-medical staff
where 24 h crisis teams were established. The risk of
658 www.thelancet.com/psychiatry Vol 4 September 2017
Downloaded for Anonymous User (n/a) at Azienda Unita Sanitaria Locale di Reggio Emilia from ClinicalKey.com by Elsevier on August 29, 2017.
View publication stats For personal use only. No other uses without permission. Copyright ©2017. Elsevier Inc. All rights reserved.
Вам также может понравиться
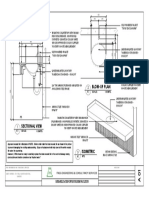
- RC Columns For Construction: Existing Culvert Location 900 MM Dia. CULVERTДокумент1 страницаRC Columns For Construction: Existing Culvert Location 900 MM Dia. CULVERTmax viejaОценок пока нет
- GRasdДокумент11 страницGRasdmax viejaОценок пока нет
- Perspective A (Front) Perspective B (Rear) : Epoxy Paint Finish (Gray)Документ2 страницыPerspective A (Front) Perspective B (Rear) : Epoxy Paint Finish (Gray)max viejaОценок пока нет
- PWD Ramp LayoutДокумент3 страницыPWD Ramp Layoutmax viejaОценок пока нет
- Lavatory Counter and Hanging CabinetДокумент3 страницыLavatory Counter and Hanging Cabinetmax viejaОценок пока нет
- Side View A 2: Second FloorДокумент3 страницыSide View A 2: Second Floormax viejaОценок пока нет
- Blow-Up Plan: FNGG Engineering and Consultancy Services RevisionsДокумент1 страницаBlow-Up Plan: FNGG Engineering and Consultancy Services Revisionsmax viejaОценок пока нет
- Blow-Up Plan: FNGG Engineering and Consultancy Services RevisionsДокумент1 страницаBlow-Up Plan: FNGG Engineering and Consultancy Services Revisionsmax viejaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Chiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFДокумент59 страницChiraghe Roshan Wa Amali Taweel - Nasir Khusrau PDFJuzer Songerwala100% (1)
- Awakening The Journalism Skills of High School StudentsДокумент3 страницыAwakening The Journalism Skills of High School StudentsMaricel BernalОценок пока нет
- Occ ST 1Документ3 страницыOcc ST 1Rona Marie BulaongОценок пока нет
- 08 Night 09 Days Ujjain & Omkareshwar Tour Package - Travel HuntДокумент5 страниц08 Night 09 Days Ujjain & Omkareshwar Tour Package - Travel HuntsalesОценок пока нет
- Michael Parenti - The Demonization of Slobodan MilosevicДокумент9 страницMichael Parenti - The Demonization of Slobodan MilosevicRicardo Castro Camba100% (1)
- HSE Matrix PlanДокумент5 страницHSE Matrix Planवात्सल्य कृतार्थ100% (1)
- Hanssen, Eirik.Документ17 страницHanssen, Eirik.crazijoeОценок пока нет
- Present Tenses ReviewДокумент6 страницPresent Tenses ReviewRamona DinuОценок пока нет
- Caisley, Robert - KissingДокумент53 страницыCaisley, Robert - KissingColleen BrutonОценок пока нет
- Thermal (TE-411,412,413,414,511)Документ25 страницThermal (TE-411,412,413,414,511)nved01Оценок пока нет
- Cloze Tests 2Документ8 страницCloze Tests 2Tatjana StijepovicОценок пока нет
- Elements of Visual Design in The Landscape - 26.11.22Документ15 страницElements of Visual Design in The Landscape - 26.11.22Delnard OnchwatiОценок пока нет
- LabДокумент11 страницLableonora KrasniqiОценок пока нет
- Using NetshДокумент2 страницыUsing NetshMohcin AllaouiОценок пока нет
- 20 Great American Short Stories: Favorite Short Story Collections The Short Story LibraryДокумент10 страниц20 Great American Short Stories: Favorite Short Story Collections The Short Story Librarywileyh100% (1)
- Feb 1 - ScottДокумент17 страницFeb 1 - ScottNyannnОценок пока нет
- Verbal Reasoning TestДокумент3 страницыVerbal Reasoning TesttagawoОценок пока нет
- They Cried MonsterДокумент13 страницThey Cried MonstermassuroОценок пока нет
- Read Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallДокумент1 страницаRead Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallKJRОценок пока нет
- Secant Method - Derivation: A. Bracketing MethodsДокумент5 страницSecant Method - Derivation: A. Bracketing MethodsStephen Dela CruzОценок пока нет
- Character Skills Snapshot Sample ItemsДокумент2 страницыCharacter Skills Snapshot Sample ItemsCharlie BolnickОценок пока нет
- Virtual Verde Release Plan Emails: Email 1Документ4 страницыVirtual Verde Release Plan Emails: Email 1Violet StarОценок пока нет
- The Newton-Leibniz Book Research - Gate - 06!12!2023Документ17 страницThe Newton-Leibniz Book Research - Gate - 06!12!2023Constantine KirichesОценок пока нет
- Mus Culo SkeletalДокумент447 страницMus Culo SkeletalKristine NicoleОценок пока нет
- Types of CostsДокумент9 страницTypes of CostsPrathna AminОценок пока нет
- ESC Cardiomyopathy ClassificationДокумент7 страницESC Cardiomyopathy Classificationvalerius83Оценок пока нет
- SKI Report2008 - 50 2Документ46 страницSKI Report2008 - 50 2nada safitriОценок пока нет
- Tutor InvoiceДокумент13 страницTutor InvoiceAbdullah NHОценок пока нет
- Presentation On HR Department of Mobilink.Документ18 страницPresentation On HR Department of Mobilink.Sadaf YaqoobОценок пока нет
- RH Control - SeracloneДокумент2 страницыRH Control - Seraclonewendys rodriguez, de los santosОценок пока нет