Академический Документы
Профессиональный Документы
Культура Документы
Breast Ca NCP
Загружено:
Thirdy AquinoИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Breast Ca NCP
Загружено:
Thirdy AquinoАвторское право:
Доступные форматы
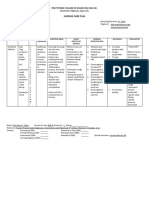
ASSESSMENT NURSING PLANNING INTERVENTION RATIONALE EVALUATION
DIAGNOSIS
Subjective: Altered Nutrition: Less After 1-2 hours of nursing Monitor daily food intake; Identifies nutritional After 1-2 hours of nursing
“Hindi ako makakain Than Body Requirements intervention Participate in have patient keep food strengths and intervention
ng maayos at related to Hypermetabolic specific interventions to diary as indicated. deficiencies. Patient demonstrate
nanghihina ako” state associated with stimulate increase in appetite and
cancer appetite/increase dietary Measure height, weight, If these measurements interest in treatment
Objective: intake. and tricep skinfold fall below minimum regimen
s/p chemotherapy thickness (or other standards, patient’s chief
s/p mastectomy anthropometric source of stored energy
weak looking measurements as (fat tissue) is depleted.
appropriate). Ascertain
vital signs amount of recent weight
BP 120/80 loss. Weigh daily or as
BT 36.8 indicated.
PR 84
RR 18 Assess skin and mucous Helps in identification of
membranes for pallor, protein-calorie
delayed wound healing, malnutrition, especially
enlarged parotid glands. when weight and
anthropometric
measurements are less
than normal.
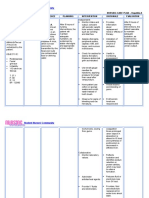
Encourage patient to eat Metabolic tissue needs
high-calorie, nutrient-rich are increased as well as
diet, with adequate fluid fluids (to eliminate waste
intake. Encourage use of products). Supplements
supplements and can play an important
frequent or smaller meals role in maintaining
spaced throughout the adequate caloric and
day. protein intake.
Create pleasant dining Makes mealtime more
atmosphere; encourage enjoyable, which may
patient to share meals enhance intake.
with family and friends.
Encourage open Often a source of
communication regarding emotional distress,
anorexia. especially for SO who
wants to feed patient
frequently. When patient
refuses, SO may feel
rejected or frustrated.
Adjust diet before and The effectiveness of diet
immediately after adjustment is very
treatment (clear, cool individualized in relief of
liquids, light or bland post therapy nausea.
foods, candied ginger, Patients must experiment
dry crackers, toast, to find best solution or
carbonated drinks). Give combination. Avoiding
liquids 1 hr before or 1 hr fluids during meals
after meals. minimizes becoming “full”
too quickly.
Control environmental Can trigger nausea and
factors (strong or noxious vomiting response.
odors or noise). Avoid
overly sweet, fatty, or
spicy foods.
Encourage use of May prevent onset or
relaxation techniques, reduce severity of
visualization, guided nausea, decrease
imagery, moderate anorexia, and enable
exercise before meals. patient to increase oral
intake.
Identify the patient who Psychogenic nausea and
experiences anticipatory vomiting occurring before
nausea and vomiting and chemotherapy generally
take appropriate does not respond to
measures. antiemetic drugs.
Change of treatment
environment or patient
routine on treatment day
may be effective.
Вам также может понравиться
- NCP PancreatitisДокумент2 страницыNCP PancreatitisJeanelle Generoso100% (1)
- Aaa Adolescent NCP FinalДокумент1 страницаAaa Adolescent NCP FinalJhaenelle Allyson TabiosОценок пока нет
- Nursing Care Plan: General: Goals Met GenreralДокумент3 страницыNursing Care Plan: General: Goals Met GenreralRomzy BasañesОценок пока нет
- CP Intestinal Obstruction Nursing Care PlanДокумент7 страницCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaОценок пока нет
- NCP PryllДокумент6 страницNCP PryllpjcolitaОценок пока нет
- NCP LaminectomyДокумент4 страницыNCP LaminectomyMark Zedrix MediarioОценок пока нет
- Nursing Care Plan For Breast Cancer NCP PDFДокумент2 страницыNursing Care Plan For Breast Cancer NCP PDFMaina BarmanОценок пока нет
- Chicken Pox N C P BY BHERU LALДокумент2 страницыChicken Pox N C P BY BHERU LALBheru Lal100% (1)
- Patient With Neutropenia Risk For Infection Related To Inadequate Secondary Defenses (Leukopenia, Neutropenia), Altered Response To MicrobialДокумент2 страницыPatient With Neutropenia Risk For Infection Related To Inadequate Secondary Defenses (Leukopenia, Neutropenia), Altered Response To MicrobialICa MarlinaОценок пока нет
- Nursingcrib Com NURSING CARE PLAN Hepatitis AДокумент2 страницыNursingcrib Com NURSING CARE PLAN Hepatitis APravesh Verma100% (1)
- NCP Proper - Obstructive JaundiceДокумент8 страницNCP Proper - Obstructive JaundiceWyen Cabatbat100% (2)
- Nursing Care PlanДокумент4 страницыNursing Care PlanKatrene Lequigan100% (1)
- NCP - Obstructive JaundiceДокумент8 страницNCP - Obstructive JaundiceWyen CabatbatОценок пока нет
- Nursing Care PlanДокумент6 страницNursing Care Plankreny1050% (2)
- Pediatric Ward Journal Binwag BSN 2aДокумент2 страницыPediatric Ward Journal Binwag BSN 2aVincentus BinОценок пока нет
- Assessment Diagnosis Planning Intervention Rationale EvaluationДокумент2 страницыAssessment Diagnosis Planning Intervention Rationale EvaluationVecky TolentinoОценок пока нет
- Fdar UTIДокумент2 страницыFdar UTINickaela CalalangОценок пока нет
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationДокумент3 страницыNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAbdallah AlasalОценок пока нет
- NCPДокумент4 страницыNCPAnn AquinoОценок пока нет
- N1007 Week Two - Nurse Care Plan - Diabetes - James ScalesДокумент1 страницаN1007 Week Two - Nurse Care Plan - Diabetes - James Scalesjumpshooter88100% (1)
- NCPДокумент5 страницNCPRose AnnОценок пока нет
- NCP For ConcussionДокумент3 страницыNCP For Concussiontamtam_antonio100% (1)
- NCPДокумент1 страницаNCPJ. ishtelleОценок пока нет
- NCP LymphomaДокумент3 страницыNCP Lymphomamahmoud fuqahaОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care PlanKath RubioОценок пока нет
- Word Ncp.......... TetanusДокумент6 страницWord Ncp.......... TetanusaianrОценок пока нет
- You Are Caring For A Patient With An NG Feeding TubeДокумент2 страницыYou Are Caring For A Patient With An NG Feeding TubeWen Silver100% (1)
- Total Abdominal Hysterectomy Actual NCPДокумент1 страницаTotal Abdominal Hysterectomy Actual NCPDoreen ClaireОценок пока нет
- NCP Pre EclampsiaДокумент2 страницыNCP Pre EclampsiaFarrah Grace Birowa0% (1)
- Nursingcrib Com NURSING CARE PLAN Hepatitis A PDFДокумент2 страницыNursingcrib Com NURSING CARE PLAN Hepatitis A PDFswapnilazarusОценок пока нет
- NCP Epidural HemДокумент32 страницыNCP Epidural HemKatrina PonceОценок пока нет
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermДокумент4 страницыNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoОценок пока нет
- NCP SviДокумент4 страницыNCP SviEjie Boy IsagaОценок пока нет
- NCPДокумент3 страницыNCPChrisTine M. MoralesОценок пока нет
- Nursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10Документ1 страницаNursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10YESSAMIN GUADIZ100% (2)
- Pleural EffusionДокумент5 страницPleural EffusionTerizla MobileОценок пока нет
- Nursing Care PlanДокумент3 страницыNursing Care PlanRaphael Reyes Enriquez100% (1)
- Rationale: This Will Assess Pain LevelДокумент7 страницRationale: This Will Assess Pain LevelCoreyОценок пока нет
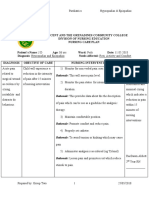
- Assessment Nursing Diagnosis Planning Implemantation Rationale EvaluationДокумент2 страницыAssessment Nursing Diagnosis Planning Implemantation Rationale EvaluationChloie Marie Rosalejos100% (1)
- Health Education HTPДокумент4 страницыHealth Education HTPizelelelsОценок пока нет
- NCP LocДокумент2 страницыNCP LocMel RodolfoОценок пока нет
- Anxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationДокумент2 страницыAnxiety Related To Hospitalization and Disease Condition As Manifested by Fiscal Expression and VerbalizationmonaОценок пока нет
- Body Weakness NCPДокумент1 страницаBody Weakness NCPtwicetrashОценок пока нет
- Nursing Care Plan HemorroidsДокумент2 страницыNursing Care Plan HemorroidsCaryl CagampangОценок пока нет
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationДокумент2 страницыNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationJamie Haravata0% (1)
- System Normal Abnormal Remarks Vital SignsДокумент3 страницыSystem Normal Abnormal Remarks Vital SignsJM RomiasОценок пока нет
- Nursing DiagnosisДокумент9 страницNursing DiagnosisSkyerexОценок пока нет
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanДокумент1 страницаIneffective Breathing Pattern Pneumonia Nursing Care Planjustin_saneОценок пока нет
- Deficient KnowledgeДокумент3 страницыDeficient KnowledgeCamilleAnneRoseRabinoОценок пока нет
- NCP pAlPITATIONSДокумент3 страницыNCP pAlPITATIONSHazel PalomaresОценок пока нет
- Care Plan ExampleДокумент2 страницыCare Plan Exampleincess27100% (1)
- NCP HypertensionДокумент1 страницаNCP HypertensionCharisse VillanuevaОценок пока нет
- Child - ImmunizationsДокумент1 страницаChild - ImmunizationsJOHN100% (1)
- NCP DMДокумент6 страницNCP DMstara123Оценок пока нет
- Mindanao State University: Nursing Care Plan For Cancer DiseasesДокумент11 страницMindanao State University: Nursing Care Plan For Cancer DiseasesAngelica Charisse BuliganОценок пока нет
- Nursing Care Plan Assessment Diagnosis Outcome Intervention Rationale EvaluationДокумент3 страницыNursing Care Plan Assessment Diagnosis Outcome Intervention Rationale EvaluationMarivic Yuson MalagarОценок пока нет
- Improved NutritionДокумент2 страницыImproved NutritionDaintyGarciaОценок пока нет
- Potential: Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationДокумент3 страницыPotential: Assessment Explanation of The Problem Objectives Nursing Interventions Rationale EvaluationBasema HashhashОценок пока нет
- Nursing Care Plan 1BSN 14 Group 1Документ8 страницNursing Care Plan 1BSN 14 Group 1Mikaella GacostaОценок пока нет
- COLON CANCER NCP-impaired nutrITIONДокумент3 страницыCOLON CANCER NCP-impaired nutrITIONNicole cuencosОценок пока нет
- Management Information System in HealthcareДокумент3 страницыManagement Information System in HealthcareThirdy AquinoОценок пока нет
- Health Teaching Plan DengueДокумент6 страницHealth Teaching Plan DengueThirdy Aquino100% (1)
- NURSING INFORMATICS Community Health ApplicationsДокумент6 страницNURSING INFORMATICS Community Health ApplicationsThirdy Aquino100% (2)
- Student Registration Form-V1012Документ2 страницыStudent Registration Form-V1012Thirdy AquinoОценок пока нет
- Personal Protective Equipment (PPE)Документ104 страницыPersonal Protective Equipment (PPE)Thirdy Aquino50% (2)
- Critical Care NursingДокумент90 страницCritical Care NursingThirdy Aquino100% (5)
- NCP LatestДокумент6 страницNCP LatestThirdy AquinoОценок пока нет
- Nursing Diagnosis and Nursing Interventions For Dengue Hemorrhagic FeverДокумент2 страницыNursing Diagnosis and Nursing Interventions For Dengue Hemorrhagic FeverThirdy Aquino82% (28)