Академический Документы
Профессиональный Документы
Культура Документы
Changes in The Degree of Bacterial Contamination of Different Areas of A Dental Unit Chair Used in The Clinical Practice of Dental
Загружено:
Alveolar 21Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Changes in The Degree of Bacterial Contamination of Different Areas of A Dental Unit Chair Used in The Clinical Practice of Dental
Загружено:
Alveolar 21Авторское право:
Доступные форматы
Biomedical Research 2018; 29 (20): 3692-3696 ISSN 0970-938X
www.biomedres.info
Changes in the degree of bacterial contamination of different areas of a
dental unit chair used in the clinical practice of dental hygiene after
disinfection.
Ga-Young Lee, Sol Lee, Seul Lee, Ho-Ju Lim, Su-Bin Bang, Seoul-Hee Nam*
Department of Dental Hygiene, College of Health Sciences, Kangwon National University, Samcheok-si, Republic of
Korea
Abstract
This study was conducted to determine the importance of infection prevention and to promote effective
disinfection through a comparison of the degrees of bacterial contamination before and after
disinfection in the clinical laboratory of a dental hygiene department. The subjects were five infection-
prone parts of a dental unit chair, including the back of the chair, the spitting bowl, the bracket button,
the light handle, and the bracket handle, of the clinical laboratory of the dental hygiene department of K
University in Gangwon Province. To compare the degree of bacterial contamination before disinfection
with that after disinfection, a sterilized cotton swab was used to swipe a 1x1cm area on the surface of a
dental unit chair before disinfection, after which the cotton swab was promptly put into a sterilized
saline solution. Safe Clean Spray (Associated Dental Products Ltd. Kemdent Works, Swindon, UK) was
then applied to the same 1 × 1 cm surface of the dental unit chair, and after 1 min, another sterilized
cotton swab was used to swipe the area, after which the cotton swab was promptly put into a sterilized
saline solution. The bacteria on the cotton swab were smeared onto a Lysogeny broth (LB) agar medium
and were cultured for 48 h at 37°C. The colony-forming unit (CFU) results showed less bacteria after
surface disinfection, and all the five areas of the dental unit chair showed significant results (p<0.05).
The bacterial identification results showed the highest rate of enterococcus in the pre-disinfected spitting
bowl, followed by the bracket handle, and the distribution of the gram-positive bacteria was high.
Although most of the bacteria were eliminated after surface disinfection, there were some remaining
bacteria. Therefore, the frequency of surface disinfection in clinical laboratories is increased to prevent
human cross-contamination from bacteria, using a more potent and biostable disinfectant.
Keywords: Cross-infection, Surface disinfection, Bacterial contamination, Dental unit chair.
Accepted on November 8, 2018
Introduction office staff during dental hygiene clinical practice through the
aerosols in the air or the contaminated materials in the clinic,
The dental hygiene department has been using an ultrasonic and plays the role of an infection pathway that can cause
scaler on patients in the dental hygiene department clinical horizontal and vertical infection in other patients and their
laboratory, for scaling practice. This creates an environment families [5]. The various microorganisms existing in the saliva
exposing both the patients and the dental practitioners to or blood of the patients can cause indoor pollution and can
various types of pathogenic microorganism, and may become become mediators for infection due to the various
an important cause of disease [1]. In particular, the use of an characteristics of dental practice. Therefore, infection
ultrasonic scaler releases fine-droplet-shaped aerosols with management is very crucial [6].
infectious factors and toxic particles into the air [2]. The
droplet-shaped aerosols float around in the air in the clinical Based on these characteristics of dental practice, the possibility
laboratory and contaminate the bodies of the dental practitioner of cross-infection from infectious microorganisms is very high
and patients as well as the surfaces of almost all the tools and in the dental staff and patients, and many endeavors have been
equipment used in the clinic [3]. made to prevent cross-infection. Exposure to patients with
various lifestyles can cause repeated aerosol infection and can
Cross-infection is the human-mediated infection of humans, increase the possibility of cross-infection as well as the
such as the patients or their guardians and the hospital staff infection risk. Therefore, a practitioner can be a mediator at the
members, or the infection of humans mediated by materials center of multiple disease occurrence, and as such, thorough
like the diagnostic tools or equipment in the clinic [4]. It is management is needed [7].
very important as it causes infection of the patients and dental
Biomed Res 2018 Volume 29 Issue 20 3692
Lee/Lee/Lee/Lim/Bang/Nam
To prevent cross-infection, safety glasses, gloves, masks, and before surface disinfection. Safe Clean Spray (Associated
scrubs must be worn so these can block infectious materials Dental Products Ltd. kemdent Works, Swindon UK) listed in
like the saliva, blood, and aerosols from the patient’s oral Table 1 was sprayed onto each of the same 1 × 1 cm areas of
cavity [8]. Furthermore, hand washing is a primary preventive the dental unit chair, and a sterilized cotton swab was used to
method for the cross-infection of practitioners from their swipe the area after 1 minute, after which the cotton swab was
patients as the hands are important factors in spreading promptly put into a 1.5 ml sterilized saline solution to
infectious diseases [5]. Therefore, the use of a primary determine the degree of surface bacterial contamination after
preventive method should be a priority in the prevention of disinfection. To identify the rate of bacterial growth, a 1 ml
cross-infection. smear preparation was made using Lysogeny broth (LB) agar,
and it was cultured for 48 h at a 37°C culture medium. The
Additionally, all the tools and equipment used in dental
colony-forming unit (CFU) of the LB agar plate was counted
procedures must be thoroughly sanitized and sterilized to
and recorded after the culture. Statistical analysis was then
prevent cross-infection and to minimize infection caused by
carried out using SPSS version 19.0 (SPSS Inc., Chicago, IL,
direct/indirect contact with the patient’s oral cavity [9].
USA). Student’s t-test was conducted to identify the change
Individual responsibility for infection prevention has not been
from before to after disinfection. A p-value<0.05 was
properly practiced, however, and great and small risks existing
considered statistically significant. From each of the isolated
widely in and around the clinical laboratories in schools can be
and incubated microorganisms, genomic deoxyribo nucleic
easily overlooked and neglected. Aerosols including infectious
acid (DNA) was extracted and subjected to polymerase chain
factors and toxic substances float around in a restricted space
reaction (PCR), and sequencing was performed to identify the
and are then dropped and cause infection. Therefore, the
strain.
surface of the dental unit chair must be frequently sanitized
[10]. Kim et al. [11] stated that the contaminated surface of a
dental unit chair can cause cross-infection of the patient, so it Results
must be sanitized after the treatment of every patient. In a
study investigating dental hygiene students’ awareness of the CFU changes before and after surface disinfection
risk of infection, a higher infection prevention practice rate was The degree of bacterial contamination of a dental unit chair in
shown when there were concerns about exposure to infectious the clinical laboratory of K University before surface
substances, blood, and saliva. The study emphasized the disinfection is shown in Figure 1. A large number of bacteria
importance of infection prevention practice even after a simple were shown at each of the five aforementioned parts of the
procedure where one did not directly contact a contaminated dental unit chair prior to disinfection, and most of the bacteria
substance, and the importance of the right recognition of were found to have been eliminated after surface disinfection.
infection prevention as well as the necessity of systemic Table 2 presents the before- and after-disinfection CFU results.
education requiring active practice [12]. The degree of bacterial contamination was high prior to surface
Therefore, this study investigated the degree of bacterial disinfection, and was highest in the spitting bowl (15.80 ± 4.16
contamination and the types of bacteria present on the surface CFU/ml), followed by the bracket handle (10.75 ± 7.02 CFU/
of a dental unit chair in the dental hygiene clinical laboratory ml), the light handle (7.17 ± 2.22 CFU/ml), the back of the
of K University by comparing the degrees of bacterial chair (6.38 ± 2.88 CFU/ml), and the bracket button (10.75 ±
contamination before and after disinfection. Furthermore, this 7.02 CFU/ml). All the five parts showed statistically significant
study can be used to raise the awareness of the importance of decreases in bacteria after surface disinfection (p<0.05).
infection prevention, and the study results can be used as
primary data to promote effective disinfection. Surface bacteria analysis
Table 3 shows the identification results of the bacteria that
Materials and Methods were purely separated from the surfaces of the five
Ten infection-prone unit chairs in the dental hygiene clinical aforementioned parts of the dental unit chair. The gram-
laboratory of K University in Gangwon Province were selected positive bacteria exceeded the gram-negative ones in quantity,
for contamination evaluation. The surface bacteria on the back and Enterococcus faecalis, Staphylococcus warneri,
of the chair, the spitting bowl, the bracket button, the light Micrococcus luteus, and Bacillus licheniformis were identified.
handle, and the bracket handle were collected to investigate the Among these, Staphlylococcus warneri were the most
degrees of bacterial contamination before and after frequently identified, followed by Enterococcus faeclis.
sterilization. A sterilized cotton swab was used to swipe a 1 ×1 Furthermore, different types of bacteria were identified after
cm area of each of the five aforementioned parts of the dental the surface disinfection of the four parts of the dental unit chair
unit chair before surface disinfection, after which the cotton other than the bracket handle, compared to before the surface
swab was promptly put into a 1.5 ml sterilized saline solution disinfection, while identical bacteria were found on the bracket
to determine the degree of surface bacterial contamination handle before and after surface disinfection.
3693 Biomed Res 2018 Volume 29 Issue 20
Changes in the degree of bacterial contamination of different areas of a dental unit chair used in the clinical practice
of dental hygiene after disinfection
Table 1. Product used for the surface disinfection of the dental unit chair.
Product Safe clean spray (Associated Dental Products Ltd. Kemdent Works, Swindon, UK)
Application time As per the manufacturer’s directions, it was applied for 1 min for surface disinfection.
Effective against Gram-positive: Enterococcus faecalis, Micrococcus luteus, Staphylococcus warneri, Bacillus licheniformis
Ingredients Ethanol, didecylidimethylammonium chloride
Table 2. Bacterial contamination levels of the surfaces of the five parts Bracket Button After 0.60 ± 0.54 0.000*
of the dental unit chair before and after surface disinfection.
Light handle Before 7.17 ± 2.22 0.015*
Group CFU (Mean ± SD) P-value Light handle After 0.67 ± 0.43 0.015*
Back of the chair Before 6.38 ± 2.88 0.020* Bracket handle Before 10.75 ± 7.02 0.046*
Back of a chair After 0.25 ± 0.71 0.020* Bracket handle After 0.38 ± 0.37 0.046*
Spitting bowl Before 15.80 ± 4.16 0.016* *Student’s t-test; p<0.05
Spitting Bowl After 1.00 ± 0.85 0.016*
Bracket button Before 4.71 ± 1.14 0.000*
Table 3. Identification of the bacteria collected from the dental unit chair.
Group Family Species Type Primer sequence (5‘-3‘)
Back of the chair Before Enterococcaeceae Enterococcus faecalis Gram-positive GGA TTA GAT ACC CTG GTA
Back of the chair After Microcoaccaceae Micrococcus luteus Gram-positive CCG TCA ATT CMT TTR AGT TT
Spitting bowl Before Enterococcaeceae Enterococcus faecalis Gram-positive GGA TTA GAT ACC CTG GTA
Spitting bowl After Staphylococcaceae Staphylococcus warneri Gram-positive GGA TTA GAT ACC CTG GTA
Bracket button Before Staphylococcaceae Staphylococcus warneri Gram-positive GGA TTA GAT ACC CTG GTA
Bracket Button After Bacillaceae Bacillus licheniformis Gram-positive GGA TTA GAT ACC CTG GTA
Light handle Before Enterococcaeceae Enterococcus faecalis Gram-positive GGA TTA GAT ACC CTG GTA
Light handle After Staphylococcaceae Staphylococcus warneri Gram-positive GGA TTA GAT ACC CTG GTA
Bracket handle Before Staphylococcaceae Staphylococcus warneri Gram-positive GGA TTA GAT ACC CTG GTA
Bracket handle After Staphylococcaceae Staphylococcus warneri Gram-positive GGA TTA GAT ACC CTG GTA
Discussion after every treatment, and Bae et al. [16] reported that 72.1%
do not do so. Moreover, both studies showed that surface
Risks of cross-infection and nosocomial infection lie in clinical disinfection is not being done properly. Furthermore, it has
laboratories due to the aerosols from the patients’ secretions been reported that the bacterial contamination is very high
(e.g., saliva, blood), the various pathogenic microorganisms, when the surfaces of the tools and equipment in the dental
and the various dusts generated during clinical practice [13]. In clinic are not disinfected, and that pathogenic sources of
addition, contacting various patients can increase the risk of infection can spread when a surface disinfectant is not used or
acquiring an infectious disease and cross-contamination. when surface disinfection is not properly done [17]. Therefore,
Therefore, infection prevention efforts are important, and it is all the equipment and tools used during dental procedures,
necessary to establish an infection prevention system [14]. including the dental unit chair, require sterilization or
Accordingly, dental hygiene students have an obligation to disinfection, and thorough management is necessary [18].
have an accurate knowledge of the situations that can cause
cross-infection in the clinical laboratory, and to make an effort To determine the extent to which the problem of the
to prevent cross-infection within the laboratory by preventing contamination of the equipment and tools in a dental clinic by
such situations from arising. microorganisms is addressed by surface disinfection, a
bacterial contamination test must be conducted. Practical
Many pathogenic microorganisms can remain and survive on studies on bacterial contamination to determine the risk of
the surfaces of the tools and equipment in the dental clinic, surface contamination in clinical laboratories, however, are
which can cause infection. Yoon et al. [15] reported, however, currently non-existent. Furthermore, as the risk of cross-
that 74.5% of dental practitioners do not disinfect such surfaces infection has increased and the importance of infection
Biomed Res 2018 Volume 29 Issue 20 3694
Lee/Lee/Lee/Lim/Bang/Nam
management has emerged, data to be used as bases for the with the results of the study conducted by Park et al. [19],
development of effective and practical infection management which showed the highest number of bacteria from the spitting
guidelines for dental hygiene students are necessary. Therefore, bowl among the five surfaces. It is thus considered that the
this study investigated the degree of bacterial contamination of spitting bowl has a higher number of bacteria compared to the
the surface of a dental unit chair before and after surface other parts of the dental unit chair due to the bacterial growth
disinfection by collecting bacteria from the dental unit chair of from secretions like the saliva and blood from the patient’s oral
a clinical laboratory, and analysed the effects of surface cavity after a dental procedure. Therefore, it must be
disinfection on the degree of bacterial contamination. thoroughly disinfected among all the parts of the dental unit
chair, and a more potent and biostable disinfectant must be
used for this purpose to remove the remaining bacteria after
surface disinfection. The result of the purely separated bacteria
from the surface of the dental unit chair in the clinical
laboratory in this study showed that gram-positive bacteria
were distributed overall. After surface disinfection,
Staphylococcus warneri was mostly detected from three parts:
the spitting bowl, light handle, and bracket handle.
Micrococcus luteus was detected from the back of the chair,
and Bacillus licheniformis was detected from the bracket
button. These results were consistent with those of a study on
contamination in a dental clinic, which reported that
Micrococcus uteus, Bacillus pumilus, and Staphylococcus
aureus were detected from the back of the dental unit chair, the
spitting bowl, and the light handle [20]. It has been reported
that pathogens like Staphylococci and Streptococci were
detected as indirect/direct infectious bacteria, causing serious
problems like cross-infection [21]. In particular,
Staphylococcus species was reported to have been detected in
the air of a dental clinic when a high-speed dental drill was
used with water spray, proving that the use of such drill with
water spray causes infection during dental procedures [22].
Although Staphylococcus warneri, which was detected from
the spitting bowl, light handle, and bracket handle in this study,
rarely causes diseases in healthy adults, it has been reported
that it can cause sepsis and osteomyelitis in immunosuppressed
patients [23]. Micrococcus luteus, which was detected from the
back of the chair in this study, exists in the nasal cavity, upper
respiratory tract, and oral mucosa, and is known to cause
meningitis and bacteremia when one is infected with it [24].
Bacillus is an aerobic gram-positive bacillus that forms spores.
It exists anywhere in the surrounding environment and is
frequently detected in dental clinics [25]. Severe infection from
Bacillus licheniformis, which was detected in the bracket
button in this study, is associated with immunosuppression and
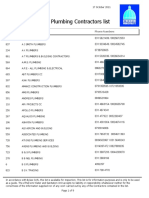
Figure 1. Changes in the number of surface microorganisms present trauma, and it is known that antibiotic use easily treats the
in the five parts of the dental unit chair in this study from before to infected regions [26]. The microorganisms that were detected
after disinfection. in this study suggest that the practice of thorough infection
management is necessary due to the maximized risk of
As a result, when the degree of bacterial contamination before
infection from these bacteria during various dental treatments.
the surface disinfection of the dental unit chair at the clinical
Based on these results, it is necessary to make dental hygiene
laboratory of the dental hygiene department of K University
students aware of the importance of surface disinfection in the
was compared to that after surface disinfection, the number of
clinical laboratory, and to increase the surface disinfection
bacteria collected from the surfaces of the five aforementioned
practice rate. In addition, review and application of the
parts of the dental unit chair after disinfection was significantly
infection management factors in clinical laboratories affecting
lower (p<0.05). The CFU level on the spitting bowl prior to
the numbers and types of bacteria, such as the disinfection
disinfection (15.80 ± 4.16 CFU/ml) was highest among the five
method and frequency, are recommended to decrease the
aforementioned parts of the dental unit chair, and was still
contamination rate by the surface bacteria. Therefore, it is
higher (1.00 ± 0.85 CFU/ml) than those of the four other parts
considered that education of future dental hygienist for
of the dental unit chair after disinfection. This was consistent
infection is necessary to encourage surface disinfection.
3695 Biomed Res 2018 Volume 29 Issue 20
Changes in the degree of bacterial contamination of different areas of a dental unit chair used in the clinical practice
of dental hygiene after disinfection
Conclusion 14. Moon SE, Lee DD, Kwon HK, Kim KJ. Analysis of
infection types on Stapylococcus aureus in dental office. J
Continuous measurement and analysis of the surface Korean Assoc Maxillofac Plast Reconsta Surg 2003; 25:
disinfection practice of clinical laboratories and the monitoring 25-32.
of effective infection management are considered necessary to
15. Yun KO. A study on the influence factor to the bacterial
minimize cross-infection and to protect dental hygiene
contamination in the dental office. (unpublished doctoral
students.
dissertation). Asan Univ Soonchunhyang 2014; 1-2.
16. Bae MR. Cognition and performance on infection control
Conflict of Interest of the clients and staffs in dental healthcare (Master’s
The authors report no conflict of interest related to this study, thesis). Kimhe University Inje 2011.
and do not have any financial interest in the companies whose 17. Jeong SY, Choi JH, Kim EK, Kim SM, Son HJ, Cho NH.
materials were included in this article. Actual disinfection and sterilization control in Korean
healthcare facilities. J Korean Acad Fundam Nurs 2014;
References 21: 392-400.
18. Choi JO, Lee YH, Nam SH. Factors affecting surface
1. Kim J, Woo HS, Jung MH. A study on the oral health management of dental unit chair. Biomed Res 2018; 29:
status, PHP Index and oral health behavior of patients in S 3129-3134.
college dental clinic. J Dent Hyg Sci 2009; 9: 145-151.
19. Park WY, Song CB, Lee SG, Lee KH. Relative light unit
2. Bentley CD, Burkhart NW, Crawford JJ. Evaluating (RLU) count at the dental environment by use of
spatter and aerosol contamination during dental FlugunTM and PCMX as a low temperature spray typed
procedures. J Am Dent Assoc 1994; 125: 579-584. sterilization agent. Int J Clin Prev Dent 2012; 8: 165-171.
3. Crawford JJ, Broderius C. Control of cross-infection risks 20. Yun KO, Kim HY. A study regarding bacterial
in the dental operatory: prevention of water retraction of contamination of surfaces in dental offices. Korean J Clin
bur cooling spray systems. J Am Dent Assoc 1988; 116: Lab Sci 2015; 47: 279-285.
685-687.
21. Kugel G, Perry RD, Ferrari M, Lalicata P. Disinfection
4. Shin SY, Yang YM, Kim MA, Kim JO, Baik BJ. The and communication practices: a survey of U.S. dental
effectiveness of clinical sterilization methods in dental air/ laboratories. J Am Dent Assoc 2000; 131: 786-792.
water syringes. J Korean Acad Pediatr Dent 2013; 40:
22. Mansour RA, Ali G, Mohammad RMN, Negar FN.
268-273.
Airborne microbial contamination of dental units.
5. Leggat PA, Kedjarune U, Smith DR. Occupational health Tanaffos 2008, 7: 54-57.
problems in modern dentistry: a review. Ind Health 2007;
23. Min JH, Park SN, Hwang HK, Min JB, Kim HS, Kook
45: 611-621.
JK. Detection of methicillin or vancomycin-resistant
6. Woo SH, Joo EJ. A study of personal protection Staphylococcus aureus from dental hospital. J Korean
equipment for infection control at dental offices. J Korean Acad Conserv Dent 2007; 32: 102-110.
Soc Dent Hyg 2010; 10: 459-464.
24. Miltiadous G, Elisaf M. Native valve endocarditis due to
7. Hardie J. Handpiece sterilization-the debate continues. J Micrococcus luteus: a case report and review of the
Can Dent Assoc 1993; 59: 355-362. literature. J Med Case Rep 2011; 5: 251.
8. Lee JY, Jeong MK. A study on recognition and practice of 25. Kedjarune U, Kukiattrakoon B, Yapong B, Chowanadisai
dental hygiene students for infection control dental S, Leggat P. Bacterial aerosols in the dental clinic: effect
hygiene major courses. J Korean Acad Dent Edu 2009; 9: of time, position and type of treatment. Int Dent J 2000;
73-88. 50: 103-107.
9. Ministry of Health and Welfare: Guideline on infection 26. Hong TW, Kim HY, Jee MG, Choi JW, Youg SJ, Shin KC,
control in dental treatments. Ministry of Health and Lee WY. A case of bacillus licheniformis bacteremia
Welfare, Sejong, 2006; 1-3. associated with bronchoscopy. Tuberc Respir Dis 2004;
10. Anuradha P. Shikha S. Aerosols and oral health. Uni J 57: 553-556.
Med Dent Sci 2015; 3: 11-13.
11. Kim KM, Hwang YS. A study on the state of infection *Correspondence to
control in dental clinic. J Korean Acad Dent Hyg Edu
2007; 7: 213-230. Seoul-Hee Nam
12. Han OS, Lee JR. Study on awareness and degree of Department of Dental Hygiene
practice about infection control by dental hygienics
students in some areas. J Dent Hyg Sci 2013; 13: 410-417. College of Health Sciences
13. Lee KH, Yang JE, Seon-Ho Mun SH, Kim JE. A study on Kangwon National University
the perception and needs about dental infection control of
the dental patients. J Korean Soc Dent Hyg 2017; 17: Republic of Korea
343-354.
Biomed Res 2018 Volume 29 Issue 20 3696
Вам также может понравиться
- 5 Manuscript 70 3 10 20200601Документ10 страниц5 Manuscript 70 3 10 20200601Alexandru Codrin-IonutОценок пока нет
- Protocolo de RXДокумент8 страницProtocolo de RXKaty Tarco RojasОценок пока нет
- 10.2478 - Cipms 2020 0019Документ4 страницы10.2478 - Cipms 2020 0019khamilatusyОценок пока нет
- Infection Control in Prosthodontics: A Literature ReviewДокумент3 страницыInfection Control in Prosthodontics: A Literature ReviewNamrata ModiОценок пока нет
- Pencegahan Dan Pengendalian Infeksi Silang Pada Tindakan Ekstraksi Gigi Di Poli Gigi Puskesmas Kakaskasen TomohonДокумент10 страницPencegahan Dan Pengendalian Infeksi Silang Pada Tindakan Ekstraksi Gigi Di Poli Gigi Puskesmas Kakaskasen TomohonEry IndraОценок пока нет
- Failure of Sterilization in A Dental Outpatient FaДокумент7 страницFailure of Sterilization in A Dental Outpatient FaNara PangestuОценок пока нет
- Evaluation of Infection Control Protocol in Dental RadiologyДокумент7 страницEvaluation of Infection Control Protocol in Dental RadiologyKaty Tarco RojasОценок пока нет
- 1Документ15 страниц1محمد ابوالمجدОценок пока нет
- 02 Antimicrobial AgentsДокумент10 страниц02 Antimicrobial AgentssandipladaniОценок пока нет
- Hong 2020 Clinical and Microbiological EfficaДокумент15 страницHong 2020 Clinical and Microbiological Efficabarrera2001Оценок пока нет
- بحث نور وتقى بعد اضافاتДокумент10 страницبحث نور وتقى بعد اضافاتtuqa abdul kareemОценок пока нет
- 86Документ5 страниц86Andrada IonescuОценок пока нет
- Streptococcus Mutans in Denture Stomatitis Patients Under Antifungal TherapyДокумент7 страницStreptococcus Mutans in Denture Stomatitis Patients Under Antifungal TherapyFebrian ArdwiantoОценок пока нет
- Airborne Microbial Contamination in Dental Practices in Iasi, RomaniaДокумент5 страницAirborne Microbial Contamination in Dental Practices in Iasi, RomaniaRahsunji Intan NurvitasariОценок пока нет
- Disinfection of Impression Materials II-1-4Документ4 страницыDisinfection of Impression Materials II-1-4ananthОценок пока нет
- Lactobacillus Salivarius NK02 A Potent Probiotic For ClinicalДокумент11 страницLactobacillus Salivarius NK02 A Potent Probiotic For ClinicalHossein ShahbaniОценок пока нет
- KJCLS 47 279Документ7 страницKJCLS 47 279ahmaad bakourОценок пока нет
- Orthodontic Instrument Sterilization With Microwave IrradiationДокумент6 страницOrthodontic Instrument Sterilization With Microwave Irradiationgreymon dmoОценок пока нет
- Candida Species in Children Undergoing Orthodontic Treatment With Removable Appliances. A Pilot StudyДокумент14 страницCandida Species in Children Undergoing Orthodontic Treatment With Removable Appliances. A Pilot StudyYasmin AfifahОценок пока нет
- Dental Radiographic Diagnosis - THUNTHYДокумент9 страницDental Radiographic Diagnosis - THUNTHYAnsh Veer ChouhanОценок пока нет
- Antibacterial Effect of Taurolidine (2%) On Established Dental Plaque BiofilmДокумент7 страницAntibacterial Effect of Taurolidine (2%) On Established Dental Plaque BiofilmDeepshriAgrawalОценок пока нет
- Microbiology and Management of Odontogenic InfectionsДокумент5 страницMicrobiology and Management of Odontogenic InfectionsJeninОценок пока нет
- Ipi376703 PDFДокумент8 страницIpi376703 PDFYunita PermataОценок пока нет
- The Effect of Removable Orthodontic Appliances On Oral Microbiota - A Systematic ReviewДокумент11 страницThe Effect of Removable Orthodontic Appliances On Oral Microbiota - A Systematic ReviewFauzan NurОценок пока нет
- Dental Laboratory Infection ControlДокумент6 страницDental Laboratory Infection ControlDrShweta SainiОценок пока нет
- Management of Deep Carious LesionsОт EverandManagement of Deep Carious LesionsFalk SchwendickeОценок пока нет
- Investigation of Organizational and Hygiene Features in Dentistry: A Pilot StudyДокумент6 страницInvestigation of Organizational and Hygiene Features in Dentistry: A Pilot Studyapi-239502672Оценок пока нет
- Role of disinfectants on alginate impression materialsДокумент13 страницRole of disinfectants on alginate impression materialsYasmine SalsabilaОценок пока нет
- Suppression of Streptococcus Mutans and Candida Albicans by Probioticsan in Vitro StudyДокумент8 страницSuppression of Streptococcus Mutans and Candida Albicans by Probioticsan in Vitro StudyTahir AliОценок пока нет
- MainДокумент5 страницMainRaji MurthyОценок пока нет
- MainДокумент5 страницMainRaji MurthyОценок пока нет
- Infection Control in the Dental Office: A Global PerspectiveОт EverandInfection Control in the Dental Office: A Global PerspectiveLouis G. DePaolaОценок пока нет
- Research Article: Factors Affecting Compliance of Infection Control Measures Among Dental RadiographersДокумент11 страницResearch Article: Factors Affecting Compliance of Infection Control Measures Among Dental RadiographersPRADNJA SURYA PARAMITHAОценок пока нет
- Microorganisms 10 00337 1Документ16 страницMicroorganisms 10 00337 1Maysaa mahdiОценок пока нет
- Applsci 11 02881 v2Документ11 страницApplsci 11 02881 v2kakanya donghyukОценок пока нет
- Archive of SID: The Antimicrobial Potential of Ten Often Used Mouthwashes Against Four Dental Caries PathogensДокумент13 страницArchive of SID: The Antimicrobial Potential of Ten Often Used Mouthwashes Against Four Dental Caries PathogensPranavОценок пока нет
- Topical and Systemic Antibiotics in The Management of Periodontal DiseasesДокумент12 страницTopical and Systemic Antibiotics in The Management of Periodontal DiseasesxdxdxdxdОценок пока нет
- Icmr-National Institute For Research in Tuberculosis-ChennaiДокумент27 страницIcmr-National Institute For Research in Tuberculosis-Chennaidhanya sriОценок пока нет
- Microbiological Analysis of In-Use Toothbrushes and Their Decontamination Using Disinfection: A Hospital Based Pilot StudyДокумент7 страницMicrobiological Analysis of In-Use Toothbrushes and Their Decontamination Using Disinfection: A Hospital Based Pilot StudyIJAR JOURNALОценок пока нет
- Prophylactic Antibiotic TRT in ImplantДокумент9 страницProphylactic Antibiotic TRT in ImplantEdu EduОценок пока нет
- CALIBR1Документ13 страницCALIBR1Codrin PanainteОценок пока нет
- Cariogram Outcome After 90 Days of Oral Treatment With Streptococcus Salivarius M18 in Children at High Risk For Dental Caries Results of AДокумент8 страницCariogram Outcome After 90 Days of Oral Treatment With Streptococcus Salivarius M18 in Children at High Risk For Dental Caries Results of AShameena KnОценок пока нет
- Propolis Chronic PeriodontitisДокумент11 страницPropolis Chronic PeriodontitisZoita MandilaОценок пока нет
- Management of Odontogenic Infection of Pulpal and Periodontal OriginДокумент6 страницManagement of Odontogenic Infection of Pulpal and Periodontal OriginNor Sakinah MОценок пока нет
- Jurnal 3 (Biofilm) Fixed PDFДокумент5 страницJurnal 3 (Biofilm) Fixed PDFNovia SillaОценок пока нет
- Antibiotics 10 00240Документ16 страницAntibiotics 10 00240Ayu SawitriОценок пока нет
- Rare Case of Odontogenic Infection Extending to Temporal SpaceДокумент5 страницRare Case of Odontogenic Infection Extending to Temporal SpaceAyu SawitriОценок пока нет
- 1 s2.0 S0882401015001527 MainДокумент8 страниц1 s2.0 S0882401015001527 MainAndrei AvîrvareiОценок пока нет
- Download Essential Microbiology For Dentistry 5Th Edition Edition Lakshman Samaranayake full chapterДокумент67 страницDownload Essential Microbiology For Dentistry 5Th Edition Edition Lakshman Samaranayake full chaptermargaret.jones429Оценок пока нет
- Antibiotics: Characterization and Antimicrobial Susceptibility of Pathogens Associated With Periodontal AbscessДокумент8 страницAntibiotics: Characterization and Antimicrobial Susceptibility of Pathogens Associated With Periodontal AbscessAhmed AlhadiОценок пока нет
- Document PDFДокумент11 страницDocument PDFputriika_27Оценок пока нет
- Effect of Morinda Citrifolia L. Fruit Juice On Gingivitis/periodontitisДокумент7 страницEffect of Morinda Citrifolia L. Fruit Juice On Gingivitis/periodontitisMuhamad Vicki SyahrialОценок пока нет
- Odontogenic Infections Etiologyand ManagementДокумент5 страницOdontogenic Infections Etiologyand ManagementYOSIОценок пока нет
- Download ebook Essential Microbiology For Dentistry Pdf full chapter pdfДокумент67 страницDownload ebook Essential Microbiology For Dentistry Pdf full chapter pdfmargarita.britt326100% (23)
- Antimicrobial Effectiveness of Cetylpyridinium Chloride and Zinc Chloride-Containing Mouthrinses On Bacteria of Halitosis and Peri-Implant DiseaseДокумент7 страницAntimicrobial Effectiveness of Cetylpyridinium Chloride and Zinc Chloride-Containing Mouthrinses On Bacteria of Halitosis and Peri-Implant DiseasePhuong ThaoОценок пока нет
- Journal of Biomedical and Pharmaceutical Research: ISSN (Online) : 2279-0594 ISSN (Print) : 2589-8752Документ4 страницыJournal of Biomedical and Pharmaceutical Research: ISSN (Online) : 2279-0594 ISSN (Print) : 2589-8752Alexandru Codrin-IonutОценок пока нет
- Interaction of Oral and Toothbrush Microbiota Affects Oral Cavity HealthДокумент9 страницInteraction of Oral and Toothbrush Microbiota Affects Oral Cavity HealthAlexandru Codrin-IonutОценок пока нет
- Diphtheria: Prepared By: Patricia Johanna A. Tan, BSN 3AДокумент18 страницDiphtheria: Prepared By: Patricia Johanna A. Tan, BSN 3ApatriciaОценок пока нет
- Workforce Development Model: A Comprehensive Strategy For Workforce Development For Environmental Public Health Professionals in South CarolinaДокумент15 страницWorkforce Development Model: A Comprehensive Strategy For Workforce Development For Environmental Public Health Professionals in South CarolinaPaul ByrneОценок пока нет
- Birao Sas 12 Microbiology and ParasitologyДокумент8 страницBirao Sas 12 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesОценок пока нет
- BMJGH 2019 January 4 Suppl 1 Inline Supplementary Material 2Документ5 страницBMJGH 2019 January 4 Suppl 1 Inline Supplementary Material 2teongОценок пока нет
- Personal HygieneДокумент15 страницPersonal HygieneIvan ToledoОценок пока нет
- AFPC Risk Assessment MatrixДокумент1 страницаAFPC Risk Assessment MatrixRiyadh SalehОценок пока нет
- Accuracy at Birth: Improving Birth Certificate Data: Beena Kamath, MD, MPHДокумент16 страницAccuracy at Birth: Improving Birth Certificate Data: Beena Kamath, MD, MPHkcochranОценок пока нет
- Monthly Monitoring Report (MMR) : Third Party Environmental Monitoring CCCC KKH-Phase II (Havelian-Thakot) ProjectДокумент84 страницыMonthly Monitoring Report (MMR) : Third Party Environmental Monitoring CCCC KKH-Phase II (Havelian-Thakot) ProjectDistinctive learningОценок пока нет
- Graphic Organizer ExampleДокумент1 страницаGraphic Organizer Exampleapi-398530613Оценок пока нет
- International Patient Safety Goals (Ipsg)Документ9 страницInternational Patient Safety Goals (Ipsg)Shibin100% (1)
- Guidelines For Perinatal CareДокумент19 страницGuidelines For Perinatal CareRiska KilkodaОценок пока нет
- DOH Annual Report 2017 0Документ49 страницDOH Annual Report 2017 0Jorem Paulo LabaoОценок пока нет
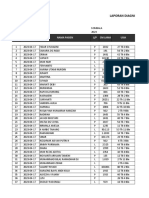
- Laporan Diagnosa Pasien Harian: Puskesmas: TanggalДокумент9 страницLaporan Diagnosa Pasien Harian: Puskesmas: TanggalRamlawatiОценок пока нет
- Guía Gold Epoc 2022 - Manual de BolsilloДокумент54 страницыGuía Gold Epoc 2022 - Manual de BolsilloAlejandro100% (1)
- Case Presentation: Typhoid FeverДокумент16 страницCase Presentation: Typhoid FeverCalingalan Hussin CaluangОценок пока нет
- Sterilitas, Asepsis Dan Antisepsis: Dr. Alex Kusanto Departemen Ilmu Bedah FKUAJДокумент40 страницSterilitas, Asepsis Dan Antisepsis: Dr. Alex Kusanto Departemen Ilmu Bedah FKUAJrinОценок пока нет
- Call For Applications For The Youth Pre Conference Compressed 1Документ10 страницCall For Applications For The Youth Pre Conference Compressed 1N'TCHAОценок пока нет
- MetronidazoleДокумент6 страницMetronidazolevenus healthklinik3Оценок пока нет
- Registered Plumbing ContractorsДокумент9 страницRegistered Plumbing ContractorsviveknayeeОценок пока нет
- Field Coordinator - GBVДокумент3 страницыField Coordinator - GBVHjha JhaОценок пока нет
- Folk Medicine in A North Indian Village - Khare 1963Документ5 страницFolk Medicine in A North Indian Village - Khare 1963frederic dugenouxОценок пока нет
- EXAMEN - 3EPPLI 30i+RFMHS 6 PDFДокумент13 страницEXAMEN - 3EPPLI 30i+RFMHS 6 PDFS Lucy PraGaОценок пока нет
- S.No. Nsg. Assessment Nsg. Diagnosis Expected Outcome Nursing Interventions Evaluation Planning ImplementationДокумент6 страницS.No. Nsg. Assessment Nsg. Diagnosis Expected Outcome Nursing Interventions Evaluation Planning ImplementationgopscharanОценок пока нет
- Antimicrobial Dressings Made Easy PDFДокумент6 страницAntimicrobial Dressings Made Easy PDFNinaОценок пока нет
- The Concepts of Community and Environment HealthДокумент12 страницThe Concepts of Community and Environment HealthRyan nani100% (1)
- DR Ward ClassДокумент36 страницDR Ward ClassChristy Mutia AlumbroОценок пока нет
- COVID-19 Vaccination Certificate QR CodeДокумент1 страницаCOVID-19 Vaccination Certificate QR CodeXyrene Del RosarioОценок пока нет
- Widal Test - Introduction, Principle and Procedure - Metropolis BlogsДокумент9 страницWidal Test - Introduction, Principle and Procedure - Metropolis BlogsinfoankitksОценок пока нет
- PP Hemorrhage: MCN Lec Semi-Quiz#1Документ4 страницыPP Hemorrhage: MCN Lec Semi-Quiz#1Faye TrishaОценок пока нет
- Detailed Speakers Listing 2-25-11Документ14 страницDetailed Speakers Listing 2-25-11magfound4mpОценок пока нет