Академический Документы
Профессиональный Документы
Культура Документы
Module 3 PDF
Загружено:
Rui ViegasОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Module 3 PDF
Загружено:
Rui ViegasАвторское право:
Доступные форматы
Foot & Ankle
Review Article
Pilon Fracture: Preventing
Complications
Abstract
Stephen A. Kottmeier, MD Fractures of the distal tibial plafond (ie, pilon) comprise a broad range
Randall Drew Madison, MD of injury mechanisms, patient demographics, and soft-tissue and
osseous lesions. Patients often present with considerably
Nicholas Divaris, MD
comminuted fracture patterns and notable soft-tissue compromise.
Surgical intervention must be performed with respect for the
exceedingly vulnerable soft-tissue envelope and with a properly
executed technique. Even with proper timing, favorable host factors,
and expert surgical technique, restoration of function and avoidance of
complications are not always achievable. Recently validated
techniques further diminish the risk of soft-tissue and osseous sepsis.
These techniques include early (ie, “immediate”) fixation, upgrading,
primary arthrodesis, staged sequential posterior and anterior fixation,
acute shortening, and transsyndesmotic fibular plating. Proper
application of these recently adopted techniques may be
instrumental in achieving aseptic union of pilon fractures.
T ibial pilon fractures represent a
wide array of osteoarticular,
metaphyseal, and soft-tissue com-
gical fixation. They advocated the
use of several treatment principles,
including lateral column restoration,
promise. The mechanism of injury medial column buttressing, and au-
is equally broad. The combinations togenous bone grafting in combina-
of articular comminution and meta- tion with articular reconstitution.
From the Department of Orthopedic diaphyseal osseous deficits may Their study consisted of a cohort
Trauma Service, State University of
prove therapeutically challenging. of lower-energy injuries for which
New York Health Sciences Center,
Stony Brook, NY. Circumferential soft-tissue compro- wound healing complication rates
mise is common, and it may predis- were deemed within acceptable pa-
Dr. Kottmeier or an immediate family
member serves as a board member, pose the patient to complications rameters. Adopting these principles,
owner, officer, or committee member such as infection and nonunion if other investigators witnessed con-
of the Orthopaedic Trauma proper timing and surgical approach cerning rates of infection.2,3 These
Association. Neither of the following
authors nor any immediate family are not carefully contemplated. Proper higher-energy lesions were, accord-
member has received anything of management of both the osseous and ingly, associated with more compli-
value from or has stock or stock soft-tissue element of the injury is re- cated pathoanatomic characteristics.
options held in a commercial company
quired to obtain favorable outcomes. Aseptic restoration of the articular
or institution related directly or
indirectly to the subject of this article: Restoration of function while avoiding surface and limb alignment should be
Dr. Madison and Dr. Divaris. catastrophic complications is the pri- predictive of both restored function
J Am Acad Orthop Surg 2018;26: mary treatment objective. and the avoidance of pain. The surgi-
640-651 In 1969, Rüedi and Allgower,1 who cal methods used to achieve articular
DOI: 10.5435/JAAOS-D-17-00160 were dissatisfied with nonsurgical reduction have, however, generated
management of intra-articular frac- conflicting results. Variables such as
Copyright 2018 by the American
Academy of Orthopaedic Surgeons. tures of the distal tibia, described mechanism of injury, host factors, and
favorable results achieved with sur- patient demographics may be more
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 1
Foot & Ankle Stephen A. Kottmeier, MD, et al
predictable determinants of out- emphasized meticulous soft-tissue ably and effectively managed with
comes. DeCoster et al4 investigated management in combination with ORIF. However, they acknowledged
the influence of injury severity and delayed definitive fixation to offer that early fixation may not yield
quality of reduction on the outcome. diminished additional compromise to acceptable results in patients with
They concluded that although the surrounding soft tissues. Short- and notable regional or systemic co-
quality of reduction offered a notable long-term outcomes demonstrated a morbidities (ie, alcohol abuse,
correlation with radiographic arthro- reduction in surgical complications. schizophrenia, diabetes, peripheral
sis, it did not independently correlate Despite adherence to contemporary neuropathy, hemorrhagic fracture
with the functional outcome. staged protocols, a relatively high blisters) and discouraged surgical
High infection rates and wound- complication rate may still exist. The intervention between 3 and 5 days
healing complications following evolution of biologically benign after injury. These investigators fur-
traditional surgical reduction have methods of reduction and plate fixa- ther advised that adopting this
prompted refinement of less-invasive tion has served to further diminish strategy demands the refined skills of
methods of osteoarticular recon- complication rates. This trend is most an orthopaedic traumatologist with
struction. Methods of minimizing the evident with regard to wound healing sufficient resources and access to the
risk of infection associated with tra- and subsequent development of operating room.10
ditional plating techniques have superficial or deep infection. In a retrospective comparative
evolved. Hybrid external fixation, study, Tang et al11 reported similar
which is characterized by early mini- results with early fixation of closed
mally invasive articular reconstruc- Early Primary Fixation pilon fractures. These authors stud-
tion neutralized by transarticular ied two groups of 23 patients, all
external fixation, initially appeared Optimal timing for surgical manage- with closed AO OTA type 43.C
to be an attractive alternative to tra- ment of pilon fractures remains con- pilon fractures. Group A was treated
ditional plating techniques. Although troversial. Early transarticular external with early fixation (ie, within 36
deep infection rates were diminished fixation followed by delayed internal hours) using minimally invasive
with external fixation, articular fixation is one management option; techniques, and group B was treated
malreduction and metadiaphyseal however, several authors have advo- with delayed fixation. They excluded
malalignment proved difficult to cated early primary open reduction all open fractures, injuries with AO
overcome and were associated with and internal fixation (ORIF) as a viable soft-tissue grades of $4, patients
less desirable outcomes.5-7 Studies strategy for managing both open and with compartment syndrome, and
seeking to compare this method of closed pilon fractures. patients with diabetes, cancer, or
treatment with traditional plating White et al10 studied a cohort of immunodeficiency. The overall in-
techniques had considerable design 95 patients with AO Orthopaedic fection rate was 17.4%, and
flaws. The compromised results of Trauma Association (OTA) type 43.C there was no significant difference
these hybrid constructs nurtured pilon fractures, most of whom had between the two groups. These au-
the tactic of staged treatment. This been treated with primary ORIF within thors, however, included superficial
approach emphasized soft-tissue 48 hours of injury. They reported that wound infections that did not require
recovery with initial application of deep infections requiring surgery surgical intervention in their analysis.
a spanning external fixator. Defini- occurred in 6% of patients. However, They reported no deep infections in
tive fixation was completed only patients with “local soft-tissue factors” the immediate fixation group and one
after the soft tissues were receptive such as gross contamination and the deep infection in the delayed fixation
(ie, resolution of swelling, regional presence of hemorrhagic fracture blis- group. Additionally, they reported
abrasions, and blisters). This fixation ters were excluded from the cohort. At statistically significant reduction in
was performed with the inclusion a minimum 1-year follow-up, the au- the surgical time and length of hos-
of strategically positioned surgical thors of the study assessed the quality pital stay for patients treated with
approaches and, where applicable, of fracture reduction and functional early fixation (P , 0.01 for both).11
minimally invasive methods of implant outcomes. Compared with the use of We have observed similar success
insertion. Several studies demonstrated delayed strategies, these authors (particularly with regard to ease of
efficacious management of high- observed enhanced anatomic fracture reduction) but have used this strategy
energy lesions using delayed surgi- reduction and similar functional out- with caution. Our experience has
cal intervention in this staged fashion comes with ORIF. They concluded been limited to closed fractures, usu-
and reported predictable and favor- that even high-energy pilon fractures ally in patients who have sustained
able outcomes.8,9 Adopted protocols within their cohort could be predict- isolated injuries. Typically, we
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 2
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 1 and metaphyseal insufficiency in
these open lesions. They remain
fraught with complications and the
potential for quiescent or obvious
infection, either of which may be
overwhelmingly refractory. Gardner
et al13 adopted a successful protocol
to manage open pilon fractures with
results yielding favorable outcomes
and an acceptable infection rate.
The first stage focused on imme-
diate débridement of devitalized
osseous and soft-tissue elements in
addition to the application of a
temporizing ankle-spanning external
fixator (Figure 1, A). Adequate
débridement with eradication of
all devitalized tissues, both soft
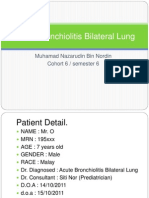
A, Intraoperative photograph showing an open tibial pilon fracture in a 22-year-
and osseous, was emphasized. These
old man who presented 36 hours after initial injury from an outside hospital with a
steel wire wound closure and a Penrose drain, and without a transarticular débridement efforts were performed
external fixator. The patient was treated with a temporizing spanning external through traumatic wound extensions
fixator and serial débridement. He subsequently underwent internal fixation, or anticipated subsequent surgical
antibiotic bead placement, and definitive wound coverage. Elective autologous
incisions. After recovery of soft tis-
bone grafting and bead extraction were performed several months later. B,
Postoperative AP radiograph obtained 12 weeks after initial injury showing early sues (usually within 1 to 3 weeks)
consolidation of callus. and in the absence of obvious signs
of infection, soft-tissue coverage
was next performed with inclusion
advocate the pursuit of early defini- such as social history, regional, and of antibiotic bead placement and
tive fixation only under the direction systemic comorbidities. contemporary plate fixation. Sev-
of an orthopaedic traumatologist and LeBus and Collinge12 assessed vas- eral months later, elective bone
in cases in which patient status and cular abnormalities in high-energy grafting was performed with bead
resources permit intervention within tibial plafond fractures with CT angi- extraction (Figure 1, B). This third
12 hours. ography. Their data analysis suggested stage was performed only in the
that open fractures were far more presence of resolved edema and in
likely than closed variants to be the absence of drainage or clinical
Open Pilon Fractures associated with arterial abnormalities. signs of infection.
High-energy pilon fractures, partic- They further concluded that no other Boraiah et al14 evaluated a staged
ularly those with associated open injury characteristics offered substan- protocol to address open fractures of
lesions, often present with defi- tial correlation with arterial injury. the pilon in an effort to minimize soft-
cient osteoarticular components and They did not, however, witness nota- tissue complications and subsequent
marginally salvageable metaphyseal ble postoperative wound-healing infection. They acknowledged that
components. Failure to recognize and abnormalities despite vascular com- restoration of limb alignment, rota-
address metadiaphyseal deficits, even promise (predominantly injury to the tion, and anatomic articular reconsti-
in the absence of infection, may pre- anterior neurovascular bundle). They tution when managing these lesions
dict failure. Threatened regional soft contended that their success was may minimize the evolution of post-
tissues and a considerably heightened likely due to the use of temporizing traumatic arthrosis. They further
risk of infection pose a therapeutic external fixation and minimally cautioned that surgical goals toward
dilemma. The outcome of high- invasive techniques with delayed articular reconstitution should not be
energy pilon fractures does not solely surgical intervention. Preserved col- pursued at a cost to regional soft tis-
depend on the integrity of regional lateral blood flow was suggested to sues, owing to the potential for
soft tissues and the osseous elements. compensate for arterial deficiency. disastrous outcomes. Sanders et al15
In addition, it is very much influenced Typically, multiple surgeries are similarly observed that, in severe
by individual patient characteristics required to address both articular open pilon fractures, the required
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 3
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 2
Intraoperative photographs showing the medial (A) and lateral (B) aspects of the lower leg in two different patients, with the
three angiosomes roughly delineated. Posteromedial (A) and anterolateral and posterolateral (B) approaches were
performed between the angiosomes, thereby limiting risk to the resultant skin bridge.
adequate débridement of soft and sought to ascertain the validity of a (Figure 2). The skin bridge and the
osseous tissues may result in con- commonly held conception that a source vessels in the overlying cuta-
siderable segmental bone loss and 7-cm skin bridge must be maintained neous blood supply appear tolerant of
articular deficits. The authors were between surgical incisions around this. This is in sharp contrast to the
able to achieve satisfactory out- the ankle joint. They suggested that risks posed by transverse incisions.
comes in a small cohort of patients adherence to this unconfirmed 7-cm The technique of deep surgical dis-
using immediate surgical arthrod- dogma was not required if proper section, perhaps more than the prox-
esis of the ankle joint. Their analysis soft-tissue management and appro- imity of the incisions to each other, has
confirmed the feasibility of limb priate timing of surgical intervention the greatest influence on wound
reconstruction in such scenarios. were maintained. They further sug- healing and evolution of infection.
Results, however, were of ques- gested that the pattern of injury, not
tionable value. They advised that skin bridge dimension, should dic-
patients be forewarned of the ex- tate surgical approach selection. In Minimally Invasive Fixation
pected multiple surgical procedures, most of their retrospectively re-
lengthy hospital admissions, and viewed cases, a skin bridge of ,7 cm Although the combination of multi-
substantial imposition on voca- was observed, and soft-tissue com- ple incisions and their proximity to
tional and personal relationships. plication and infection rates were each other was described earlier, the
Furthermore, they argued that pri- acceptable. The anterolateral (Böhler) attributes of minimally invasive
mary amputation in select cases may approach, in particular, has proven techniques have been explored and
prove to be the “conservative” resilient when combined with either adopted by some surgeons. Sub-
treatment of choice. medial or posterolateral approaches.17 muscular anterolateral (Böhler) ap-
Despite infrequent dehiscence, super- proaches cannot be used with purely
ficial infection, and eschar, it has percutaneous efforts because regional
Surgical Approach and proven to be receptive to and requiring neurovascular structures remain at
Infection of only local wound care and healing risk.19 Several studies have sought
Numerous surgical access strategies by secondary intention. to assess the efficacy of minimally
have been offered, each with unique Three vertically oriented angiosomes invasive subcutaneous instrumenta-
limitations, attributes, and charac- exist, supplying the overlying soft- tion methods to address pilon fractures
teristics. Various combinations of tissue envelope of the lower leg and and associated wound healing com-
approaches have been described, as ankle.18 Surgical incisions placed in plications.20,21 Such efforts are largely
have concerns regarding their prox- parallel between the angiosomes pose limited to medial column restoration
imity to one another. Howard et al16 no threat to the resultant skin bridge using percutaneous techniques. In a
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 4
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 3 mally (Figure 3, A). They suggested
that these lesions were challenging
from the standpoint of acceptable
reduction when managed in a de-
layed fashion. The authors main-
tained that delayed management of
these lesions required excessive
stripping, greatly impaired reduction
of these fragments, and compro-
mised anatomic restoration of the
articular surface. They proposed that
this fracture pattern could be more
expeditiously managed in the acute
setting during surgical débridement
and application of a transarticular
fixator. In accordance with this
technique, small fragment plates
were applied to the diaphyseal
component of the fracture, typically
in an antiglide fashion, through
small proximal incisions (Figure 3,
B). Avoidance of tenuous peripheral
soft tissues was required, and addi-
tional osteoarticular reconstruction
A, Three-dimensional CT scan demonstrating proximal apical extension (arrow) was deferred until soft-tissue status
of a pilon fracture pattern in continuity with a peripheral large articular implant. B,
Intraoperative AP fluoroscopic image showing fixation of the apical portion of a permitted. This served to reestablish
pilon fracture with an oblique extension encroaching proximally on the diaphysis length, rotation, and alignment of
using a proximal posteromedial approach remote from anticipated subsequent these regional fragments, which were
more peripheral approaches. commonly in continuity with either
the anterolateral (Chaput) or postero-
lateral (Volkmann) articular frag-
cadaver study, Borrelli et al22 healing complications.20,26 Most of ments. Early anatomic restoration of
described the extraosseous blood these were easily resolved without these fragments (through upgrad-
supply of the tibia and the effect notable negative effects on osseous ing) afforded a foundation for sub-
various forms of plate fixation have union or functional outcome. Al- sequent delayed definitive fixation.
on it. Percutaneously introduced though minimally invasive methods When applied to pilon fractures, the
plates seemed to cause less disruption of fixation demonstrated diminished technique of upgrading enables con-
to the extraosseous blood supply, rates of infection, obstacles remained. version of an AO/OTA type C (ie,
particularly in the medial aspect of Among these, nonunion, malre- complete articular involvement) pat-
the distal tibia. Subsequent studies duction, and angular deformities tern to an AO/OTA type B (ie, partial
have validated these findings from a were not uncommon. articular involvement) pattern.
clinical perspective.23,24 In contrast, Despite being performed in the acute
Lau et al25 observed a concerningly setting, it served to diminish subse-
high rate of late superficial infection, Upgrading quent soft-tissue compromise during
primarily with medial subcutaneous When managing soft-tissue concerns the course of definitive fixation.
plates. They maintained, however, in an effort to reduce the risk of This, in turn, diminished the risk of
that this had little effect on the out- infection, the concept of upgrading, infection and subsequent wound
come. These infections were success- in which a complex fracture pattern is compromise. The offered tech-
fully managed with a brief course of converted to a simpler one, may nique seems to be simple and safe,
antimicrobial therapy and, on occa- have a role. Dunbar et al27 identified and it is an adjunct to prevent
sion, implant extraction. Other a subset of pilon fractures presenting infection. It does, however, war-
studies have demonstrated similar with an oblique extension that en- rant further investigation and
findings with regard to medial wound croached on the diaphysis proxi- cautious application.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 5
Foot & Ankle Stephen A. Kottmeier, MD, et al
Sequential Fixation Figure 4
The limitations of traditional ante-
rior exposures with the patient su-
pine have proven challenging with
regard to the reduction of associ-
ated posterior malleolar patterns.
These important posterior compo-
nents, when accurately reduced, may
serve as a useful template for resto-
ration of the fracture length, angula-
tion, and articular reconstitution.
Soft-tissue detachment, in addition
to comminution and small fragment
dimensions, may make traditional
surgical exposures inadequate in
achieving required anatomic reduc-
tion (Figure 4, A). The resultant
malreduction may prohibit subse-
quent articular reconstitution. Ketz
and Sanders28 recognized potential
difficulties encountered during the
course of reduction of the posterior
malleolar fragment associated with
high-energy pilon fractures. In select
fracture patterns, the advantages of
direct posterior malleolar plating
performed with prone patient posi- A, Three-dimensional CT scan showing a posterior pilon variant with
tioning were readily apparent. These syndesmotic detachment (arrow). The syndesmotic detachment may complicate
investigators adopted a staged pro- reduction efforts when anterior approach strategies are used with the patient in
the supine position. B, Intraoperative lateral fluoroscopic image demonstrating a
tocol with initial application of an posterior antiglide plate (arrow) that was placed through a posterolateral incision
external fixator combined with a to restore an intact posterior column on which additional reduction and fixation
limited posterior open reduction may be executed. This foundation facilitates delayed, anteriorly based approach
through a posterolateral approach. and fixation.
This exposure was permitting of
concomitant fixation of the fibula. gical access (posteriorly) through dance with upgrading techniques
They acknowledged the limitations soft tissues, with subsequent fixation (despite early surgical intervention to
of articular scrutiny during the performed anteriorly. Surgical fixa- receptive soft tissues), hastened the
course of posterior fragment fixation tion through the more compromised recovery of peripheral soft tissues.
efforts, which were indirectly re- anterior soft tissues required con- This staged strategy of fixation may
duced. Caution was urged with re- siderable delay. Katz and Sanders28 reduce wound healing complication
gard to execution of fibula fixation reported improved articular re- rates and the risk of infection.
because any element of malrotation, ductions and better functional
shortening, or angular malalignment outcomes compared with previous
could prevent anatomic reduction of protocols of delayed single-stage Transsyndesmotic Fixation
the posterior fragment. After recov- definitive fixation. There were no On occasion, concerns regarding the
ery of soft tissues, a delayed second increased complications associated integrity of the soft tissues and host
staged surgical intervention was with wound healing. As described characteristics may exceed osseous
performed to reduce and fixate previously, this served to upgrade concerns. Low-energy fracture var-
the remaining anterior fragments to the lesion to a pattern of lesser iants with primarily medial com-
their now intact posterior fragment complexity with potentially more pounding wounds in patients with
counterparts (Figure 4, B). This predictable subsequent reduction considerable comorbidities are not
staged protocol permitted early sur- maneuvers. This protocol, in accor- uncommon. Sciadini et al29 reviewed
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 6
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 5 soft-tissue coverage. Most of these
patients have preexisting medical and
regional comorbidities. In addition, we
have found that this technique is
appropriate for deliberate, acute
shortening efforts (Figure 5). When
indicated in patients in whom complex
soft-tissue coverage is not appropriate,
shortening may facilitate wound clo-
sure. It is a potentially useful strategy
in the surgeon’s armamentarium to
avoid disastrous wound healing com-
plications and subsequent infection.
Primary Ankle Arthrodesis
Although the relationship between
the quality of reduction and func-
A, Intraoperative photograph demonstrating a high-energy open pilon fracture
in a 67-year-old man. The patient presented with concerning regional and tional outcome measures may offer
systemic comorbidities. He was deemed a poor candidate for medial soft- some correlation, an exception may
tissue reconstruction efforts. Conventional fixation efforts may have further be fracture patterns with extreme
complicated recovery of soft and osseous tissues. B, AP radiograph of the comminution and metadiaphyseal
ankle showing transsyndesmotic fixation of the pilon fracture. Deliberate
shortening was performed, further facilitating wound closure and uneventful impaction. Numerous studies have
wound healing medially. Bony union was achieved without adjuvant surgical or sought to ascertain the influence of the
grafting efforts. fracture pattern and surgical treatment
selection on the quality of reduction
and functional outcome of surgically
several cases of distal tibial fractures to minimally invasive plate fixation of managed pilon fractures. Anatomic
with minimal or no articular in- the medial column. Transsyndesmotic osteoarticular reconstruction in the
volvement but with notable medial fixation is perhaps most suitable setting of severe comminution is chal-
soft-tissue injury. These authors when conventional methods of fix- lenging, with no guarantee of favorable
described a novel approach of fixed ation may pose unacceptable risks outcomes. Furthermore, reconstruc-
angle transsyndesmotic fixation, to anterior or medial soft tissues. tion may result in a severe threat to soft
which offered minimal introduction Fixation is introduced through the tissues and infection; thus, a role for
of surgical insult, particularly to com- less traumatized and more resilient primary ankle arthrodesis may exist
promised medial soft tissues. Such lateral soft tissues. (Figure 6). Arthrodesis permits cau-
constructs have been previously Technical aspects of transsyndesmotic tious delayed treatment, which allows
described to enhance fixation in pa- fixation include the use of a fibular recovery of soft tissues.
tients with diabetes and osteoporotic plate with hybrid fixation techniques. Several studies have assessed the role
ankle fractures of low complexity Transsyndesmotic locking screws are of primary arthrodesis in the setting of
and energy. The greatest utility of the placed in the distal limit of the fibular severe articular comminution that pre-
technique is in the management of plate, engaging the distal tibia in cluded anatomic reconstitution. Bea-
valgus distal tibial fractures with a quadricortical fashion. Bicortical man and Gellman30 demonstrated
associated medial traction wounds. fibular or similar quadricortical reliably good outcomes with anterior
Sciadini et al29 proposed this tech- fibular-tibial screws are introduced plate fixation supplemented by a neu-
nique as a viable method of obtain- proximally. This construct serves to tralizing external fixator with primary
ing and maintaining reduction with bridge the tibial component of the arthrodesis of the ankle. These au-
or without the sustained application fracture pattern. Preferred con- thors, encouraged by expedited patient
of a transarticular external fixator. structs use a long precontoured dis- recovery, suggested the use of primary
Their cohort included patients with tal fibular plate. We have found that ankle arthrodesis to manage complex
high-energy injuries, including falls this construct is indicated for pa- patterns that are refractory to osteo-
from a height and vehicular injuries. tients with valgus patterns who are articular reconstitution. Acceptable
Medial soft tissues were not receptive deemed poor candidates for complex healing rates were reported, with good
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 7
Foot & Ankle Stephen A. Kottmeier, MD, et al
overall functional scores. Zelle et al31 Figure 6
reported satisfactory results with the
application of a posteriorly applied
blade plate. They described it as a
reliable method of addressing a small
subset of injury patterns that are
deemed nonreconstructable. Primary
arthrodesis is indicated for manage-
ment of fracture patterns with
extensive comminution and marked
impaction of the articular cartilage
(.50% of the tibial plafond delin-
eated on preoperative CT) within the
tibial metaphysis. The authors
reported good results, even in the
setting of metadiaphyseal deficits.
Zelle et al31 advocated the use of
primary arthrodesis in select patients
and highlighted the reduced rate of
infection compared with infection
rates associated with conventional
fixation techniques. The authors did
acknowledge the preferential goal of
articular reconstitution when possible,
in an effort to limit midfoot arthrosis,
which is a complication commonly associ-
ated with otherwise successful tibiotalar
arthrodesis.
Acute Shortening A, AP radiograph of the ankle of a 67-year-old woman who sustained a pilon
The combined presence of soft tissue fracture in a high-energy motor vehicle collision. The articular component was
deemed nonreconstructable, and the soft tissues were severely compromised. A
and osseous deficits complicates
temporizing transarticular external fixator was applied for 4 weeks, and then
management of severely comminuted primary ankle arthrodesis was performed. B, AP radiograph of the ankle after
pilon fractures, particularly those with primary arthrodesis with a lateral blade plate.
associated metadiaphyseal comminu-
tion. Soft-tissue reconstruction op-
tions include local rotation flaps, skin traumatic wound, necessitating soft- described by some as less prone to
grafts, and free flaps. In patients tissue coverage. We have successfully wound healing complications than
deemed poor candidates for such performed intentional shortening with other approaches.32,33 Others, how-
procedures, acute shortening of the the inclusion of posterior plating ever, have not found this to be the
distal fracture site facilitates closure of techniques in patients deemed poor case.34
the traumatic wound and may simul- candidates for soft-tissue transfer Alternatively, the use of ringed fix-
taneously address osseous deficits. (Figure 7). This management option ators may be considered. Monofocal
Unintended shortening upon appli- requires segmental osseous resection methods of management involve distal
cation of a temporary transarticular (ie, tibia and fibula), intraoperative shortening and the acceptance of lim-
external fixator is not uncommon vascular monitoring, and acceptance ited limb length inequality (Figure 8).
when managing open pilon fracture of limb shortening. The advantages of This step may be done acutely,
variants. The wound is often perceived acute shortening include shorter hos- gradually, or as a combination of
as easily coapted during débridement. pital stay and avoidance of compli- both if shortening of .3 cm is nec-
For simple fracture patterns, subse- cated soft-tissue reconstruction, both essary. The anticipated limb length
quent anatomic restoration may result of which reduce the cost of care. The inequality associated with acute
in a readily apparent diastasis of the posterolateral approach has been peripheral shortening may be
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 8
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 7
A, AP radiograph of the ankle demonstrating an open pilon fracture in a 72-year-old man. Restoration of the limb length resulted
in wound diastasis. He was deemed a poor candidate for soft-tissue coverage. B, Clinical photograph of the ankle after
deliberate limb shortening was performed, resulting in approximation of robust tissue margins. C, AP radiograph of the ankle
demonstrating fixation with a posterior plate. Clinical and radiographic union was achieved with restoration of aseptic function.
Figure 8
A, Preoperative AP radiograph of the ankle demonstrating a severe open tibial pilon fracture in a 58-year-old woman who
was injured in a motor vehicle collision. Débridement of devitalized tissues resulted in considerable osseous and soft-tissue
deficits requiring resection of the distal tibial osteoarticular segment. She was a poor candidate for both soft-tissue
reconstruction and osseous regeneration reconstruction maneuvers. B, Lateral radiograph of the ankle following monofocal
methods of limb shortening with the application of a circular tensioned wire external fixator. This resolved concerns for both
soft-tissue and osseous deficits. Acute shortening followed by subsequent gradual shortening was performed to ensure limb
perfusion. The arrows to the right indicate intentional acute shortening performed at the time of surgery. The arrows to the left
indicate subsequent gradual shortening/compression through the circular frame. C, AP radiograph of the ankle obtained
6 months after injury demonstrating successful fusion. (Reproduced with permission from Kottmeier S, Madison R, Divaris N, et
al: The infected pilon: Assessment and treatment strategies. Techniques in Foot & Ankle Surgery 2016;15:188–196.)
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 9
Foot & Ankle Stephen A. Kottmeier, MD, et al
Figure 9
A, AP radiograph of the ankle showing an open distal tibial pilon fracture with devitalized metadiaphyseal implants in a 42-
year-old patient. B, AP radiograph of the ankle after application of a circular fixator. A bifocal strategy (two levels of activity)
was used with distraction osteogenesis (proximal segment) and intercalary shortening (distal segment). The arrows indicate
distraction at the proximal osteotomy site and compression at the distal intercalary defect. C, Postoperative lateral
radiograph demonstrating satisfactory proximal bone regenerate and union of the distal region of intercalary bones loss.
(Reproduced with permission from Kottmeier S, Madison R, Divaris N, et al: The infected pilon: Assessment and treatment
strategies. Techniques in Foot & Ankle Surgery 2016;15:188–196.)
addressed by distraction osteo- Additionally, adjuvant bone grafting region of comminution has been
genesis techniques within the proximal techniques are unlikely to be required; described for defects ,3 cm. Caution
metaphyseal region of the tibia.35,36 these techniques are frequently re- has been advised when pursuing
These techniques can be performed quired to facilitate docking site union. shortening for defects .3 cm.40
simultaneously (ie, bifocal) or staged Several studies have demonstrated the Deliberate limb length reduction is
at a later date. Bifocal compression/ efficacy of described bifocal treatment limited by the circulatory status of
distraction osteogenesis addresses bone in the acute management of distal tibial the foot, which is monitored by
loss peripherally (through shortening) metaphyseal pilon fractures, particu- means of intraoperative Doppler
and resolves limb length discrepancy larly in the setting of open fractures ultrasonography of the posterior and
by proximal distraction osteogenesis and metaphyseal deficits.38,39 The anterior tibial arteries. Atbasi et al41
(Figure 9). Limb shortening peripher- ability to include primary wound clo- assessed the arterial configuration
ally, within the region of distal meta- sure is unique to acute shortening after acute tibial shortening with
physeal deficit, does not require protocols, thus eliminating the need for angiographic evaluation. In a clinical
adjuvant bone grafting techniques or complicated soft-tissue reconstruction study, 16 patients were monitored
the docking site preparation required efforts. This setting is particularly with intraoperative Doppler and
with bone transport techniques in important for patients who cannot pulse oximetry. The average amount
which the length of the limb is main- undergo complex soft-tissue coverage. of acute shortening was 5.5 cm
tained (ie, a form of monofocal treat- Additional gradual shortening of (maximum, 8 cm of shortening). Dig-
ment).37 In contrast to segmental 2 mm per day has been described for ital subtraction angiography was per-
bone transport, acute shortening ob- defects .3 cm.39 Shortening of the formed 1 week after the procedure,
viates docking site trajectory concerns. distal aspect of the tibia within the and CT angiography was performed
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 10
Foot & Ankle Stephen A. Kottmeier, MD, et al
2 years after the procedure. No stitution cannot be at the expense of 8. Patterson MJ, Cole JD: Two-staged delayed
open reduction and internal fixation of
discernible change in the arterial the soft tissues. Despite adherence to severe pilon fractures. J Orthop Trauma
configuration occurred with acute and proper execution of current fix- 1999;13:85-91.
shortening ,4 cm; however, increased ation techniques, infection of the 9. Sirkin M, Sanders R, DiPasquale T,
tortuosity of the vessels was noted. distal tibial pilon after surgical os- Herscovici D Jr: A staged protocol for soft
Arterial patency was maintained, and teosynthesis remains challenging. tissue management in the treatment of
complex pilon fractures. J Orthop Trauma
the newly acquired arterial configura- Patient characteristics, both regional 1999;13:78-84.
tion persisted for ,2 years with no and systemic, must be considered.
10. White TO, Guy P, Cooke CJ, et al: The
circulatory or limb perfusion compli- The limitations and difficulty of these results of early primary open reduction and
cations. Accordingly, a threshold for surgical reconstructions must be rec- internal fixation for treatment of OTA 43.
C-type tibial pilon fractures: A cohort
immediate acute shortening has yet to ognized and accepted by both the study. J Orthop Trauma 2010;24:757-763.
be convincingly demonstrated. treating surgeon and the patient.
11. Tang X, Liu L, Tu C, Li J, Li Q, Pei F:
Distally, both monofocal and bifo- Comparison of early and delayed open
cal techniques follow a similar pro- reduction and internal fixation for treating
tocol. Devitalized bone margins are References closed tibial pilon fractures. Foot Ankle Int
2014;35;657-664.
resected with aggressive débridement
of devitalized structures. Because of Evidence-based Medicine: Levels of 12. LeBus GF, Collinge C: Vascular
abnormalities as assessed with CT
the small dimension of the distal evidence are described in the table of angiography in high-energy tibial plafond
fragment and its proximity to the contents. In this article, references 6, fractures. J Orthop Trauma 2008;22:
7, 11, 28, and 40 are level III studies. 16-22.
ankle joint, inclusion of the foot
within the frame is typically re- References 1-5, 8-10, 12-17, 20, 21, 13. Gardner MJ, Mehta S, Barei DP, Nork SE:
23-27, 29-31, 33-35, 37-39, and 41 Treatment protocol for open AO/OTA type
quired. This configuration also C3 pilon fractures with segmental bone
serves to prevent equinus contrac- are level IV studies. References 18, loss. J Orthop Trauma 2008;22:451-457.
ture and offers enhanced stability to 19, 22, 32, and 36 are level V expert
14. Boraiah S, Kemp TJ, Erwteman A, Lucas
the ring construct. With bifocal efforts opinion. PA, Asprinio DE: Outcome following open
(acute or staged), a proximal tibial reduction and internal fixation of open
References printed in bold type are pilon fractures. J Bone Joint Surg Am 2010;
corticotomy is performed in a low- 92:346-352.
those published within the past 5
energy fashion by means of multiple
years. 15. Sanders R, Pappas J, Mast J, Helfet D: The
drill holes or a Gigli saw. Proximal salvage of open grade IIIB ankle and talus
distraction is initiated at a rate of 1. Rüedi T, Allgower M: Fractures of the fractures. J Orthop Trauma 1992;6:
1 mm per day, with a latency period of lower end of tibia into the ankle-joint. 201-208.
Injury 1969;1:92–99.
7 to 10 days. Both unifocal and bifocal 16. Howard JL, Agel J, Barei DP, Benirschke
treatment methods facilitate closure of 2. Dillin L, Slabaugh P: Delayed wound SK, Nork SE: A prospective study
healing, infection, and nonunion following evaluating incision placement and wound
the distal traumatic wound. With open reduction and internal fixation of healing for tibial plafond fractures. J
either method, segmental resection tibial plafond fractures. J Trauma 1986;26: Orthop Trauma 2008;22:299-305.
1116–1119.
of a portion of the fibula, corre- 17. Mehta S, Gardner MJ, Barei DP, Benirschke
sponding to the anticipated measured 3. McFerran MA, Smith SW, Boulas HJ, SK, Nork SE: Reduction strategies through
Schwartz HS: Complications encountered the anterolateral exposure for fixation of
shortening, is required. This allows in the treatment of pilon fractures. J Orthop type B and C pilon fractures. J Orthop
approximation of the peripheral Trauma 1992;6:195-200. Trauma 2011;25:116-122.
proximal and distal fragments. Inten- 4. DeCoster TA, Willis MC, Marsh JL, et al: 18. Attinger CE, Evans KK, Bulan E, Blume
tional shortening of the limb may Rank order analysis of tibial plafond P, Cooper P: Angiosomes of the foot and
favor primary wound healing and fractures: Does injury or reduction predict ankle and clinical implications for limb
outcome? Foot Ankle Int 1999;20:44-49. salvage: Reconstruction, incisions, and
make the soft tissues more resilient to revascularization. Plast Reconstr Surg
infection and osseous devitalization. 5. Barbieri R, Schenk R, Koval K, Aurori K, 2006;117(suppl 7):261S-293S.
Aurori B: Hybrid external fixation in the
treatment of tibial plafond fractures. Clin 19. Wolinsky P, Lee M: The distal approach for
Orthop Relat Res 1996:16-22. anterolateral plate fixation of the tibia: An
anatomic study. J Orthop Trauma 2008;
Summary 6. Pugh KJ, Wolinsky PR, McAndrew MP, 22:404–407.
Johnson KD: Tibial pilon fractures: A
Recent advances in osteosynthesis of comparison of treatment methods. J 20. Borg T, Larsson S, Lindsjö U: Percutaneous
Trauma 1999;47:937-941. plating of distal tibial fractures: Preliminary
the distal tibial plafond have been results in 21 patients. Injury 2004;35:
promising, offering improved out- 7. Watson JT, Moed BR, Karges DE, Cramer 608-614.
KE: Pilon fractures: Treatment protocol
comes and fewer complications. The based on severity of soft tissue injury. Clin 21. Collinge C, Sanders R, DiPasquale T:
pursuit of anatomic articular recon- Orthop Relat Res 2000:78-90. Treatment of complex tibial periarticular
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 11
Foot & Ankle Stephen A. Kottmeier, MD, et al
fractures using percutaneous techniques. Trauma Association 43C2 and 43C3 tibial fractures of the tibia. J Bone Joint Surg Br
Clin Orthop Relat Res 2000:69-77. pilon fractures. J Orthop Trauma 2012;26: 2007;89:80-88.
341-347.
22. Borrelli J Jr, Prickett W, Song E, Becker D, 36. Sales de Gauzy J, Vidal H, Cahuzac JP:
Ricci W: Extraosseous blood supply of the 29. Sciadini MF, Manson TT, Shah SB: Trans- Primary shortening followed by callus
tibia and the effects of different plating syndesmotic fibular plating for fractures of distraction for the treatment of a
techniques: A human cadaveric study. J the distal tibia and fibula with medial soft posttraumatic bone defect: Case report. J
Orthop Trauma 2002;16:691-695. tissue injury: Report of 6 cases and Trauma 1993;34:461-463.
description of surgical technique. J Orthop
23. Ronga M, Longo UG, Maffulli N: Trauma 2013;27:e65-e73. 37. Saleh M, Rees A: Bifocal surgery for
Minimally invasive locked plating of deformity and bone loss after lower-limb
distal tibia fractures is safe and effective. 30. Beaman DN, Gellman R: Fracture fractures: Comparison of bone-transport
Clin Orthop Relat Res 2010;468: reduction and primary ankle arthrodesis: A and compression-distraction methods. J
975-982. reliable approach for severely comminuted Bone Joint Surg Br 1995;77:429-434.
tibial pilon fracture. Clin Orthop Relat Res
24. Williams TH, Schenk W: Bridging- 2014;472:3823-3834. 38. Rozbruch SR, Weitzman AM, Watson JT,
minimally invasive locking plate Freudigman P, Katz HV, Ilizarov S:
osteosynthesis (Bridging-MILPO): 31. Zelle BA, Gruen GS, McMillen RL, Dahl Simultaneous treatment of tibial bone and
Technique description with prospective JD: Primary arthrodesis of the tibiotalar soft-tissue defects with the Ilizarov method.
series of 20 tibial fractures. Injury 2008;39: joint in severely comminuted high-energy J Orthop Trauma 2006;20:197-205.
1198-1203. pilon fractures. J Bone Joint Surg Am 2014;
96:e91. 39. Sen C, Kocaoglu M, Eralp L, Gulsen M,
25. Lau TW, Leung F, Chan CF, Chow SP:
Cinar M: Bifocal compression-distraction
Wound complication of minimally invasive 32. Konrath GA, Hopkins G II: Posterolateral
in the acute treatment of grade III open tibia
plate osteosynthesis in distal tibia fractures. approach for tibial pilon fractures: A report
fractures with bone and soft-tissue loss: A
Int Orthop 2008;32:697-703. of two cases. J Orthop Trauma 1999;13:
report of 24 cases. J Orthop Trauma 2004;
586-589.
26. Sitnik AA, Beletsky AV: Minimally invasive 18:150-157.
percutaneous plate fixation of tibia 33. Sheerin DV, Turen CH, Nascone JW:
40. Katsenis D, Triantafillis V, Chatzicristos M,
fractures: Results in 80 patients. Clin Reconstruction of distal tibia fractures
Dendrinos G: The reconstruction of tibial
Orthop Relat Res 2013;471:2783-2789. using a posterolateral approach and a blade
metaphyseal comminution using hybrid
plate. J Orthop Trauma 2006;20:247-252.
27. Dunbar RP, Barei DP, Kubiak EN, Nork frames in severe tibial plafond fractures. J
SE, Henley MB: Early limited internal 34. Bhattacharyya T, Crichlow R, Gobezie R, Kim Orthop Trauma 2013;27:153-157.
fixation of diaphyseal extensions in select E, Vrahas MS: Complications associated with
pilon fractures: Upgrading AO/OTA type C the posterolateral approach for pilon fractures. 41. Atbasi Z, Demiralp B, Kilic E, Kose O,
fractures to AO/OTA type B. J Orthop J Orthop Trauma 2006;20:104-107. Kurklu M, Basbozkurt M: Angiographic
Trauma 2008;22:426-429. evaluation of arterial configuration
35. El-Rosasy MA: Acute shortening and re- after acute tibial shortening. Eur J
28. Ketz J, Sanders R: Staged posterior tibial lengthening in the management of bone Orthop Surg Traumatol 2014;24:
plating for the treatment of Orthopaedic and soft-tissue loss in complicated 1587-1595.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 12
Review Article
Foot and Ankle Infections:
Diagnosis and Management
Abstract
Oke A. Anakwenze, MD Infections of the foot are a common source of morbidity, disability,
Andrew H. Milby, MD and potential limb loss. A large proportion of lower extremity
infections occurs in the setting of diabetic neuropathy, with or
Itai Gans
without circulatory compromise, and are potentially preventable
John J. Stern, MD with regular surveillance. Adequate diagnosis and treatment of foot
L. Scott Levin, MD, FACS infections can be challenging. Successful treatment is dependent
Keith L. Wapner, MD on factors such as etiology; vascular, neurologic, and immune
status; and the identity of the offending organism.
F oot infections are a common
source of morbidity, disability,
and potential limb loss. Trauma to
taining a history, including questions
regarding pain; ability to bear
weight; subjective fevers or chills; re-
and pathology of the lower leg, an- cent trauma; prior infections; and
kle, feet, and toes are risk factors for changes in activity, footwear, or hy-
subsequent infection and comprised giene. Systemic conditions such as di-
11.8% of injuries seen in emergency abetes, peripheral vascular disease,
departments in 2006.1 In the setting chronic liver or kidney disease, im-
of systemic conditions such as diabe- munosuppressive status, and gout
tes, infections pose an especially also must be noted.
challenging treatment dilemma be- Examination must take into ac-
cause patients often have compro- count vital signs and overall mental
mised vascular status, immune sta- status to assess for systemic infec-
tus, and wound healing capability. tion. The affected extremity should
Over 60% of nontraumatic lower- be compared with the unaffected ex-
limb amputations occur in patients tremity whenever possible, and vi-
with diabetes.2 Because many of sual inspection should note the pres-
these infections are preventable, their ence of deformity or other objective
identification has become a priority findings, including erythema, ecchy-
From the Department of
Orthopaedic Surgery
area in healthcare quality improve- mosis, or swelling. The integrity of
(Dr. Anakewnze, Dr. Milby, Dr. Levin, ment.3 Despite their impact on pa- the skin should be assessed for
and Dr. Wapner), the School of tient health and medical costs, treat- calluses or blisters and drainage.
Medicine (Mr. Gans), and the ment strategies for foot infections,
Department of Medicine, Division of Wound odor and any associated
Infectious Diseases (Dr. Stern), which may include prolonged antibi- drainage may aid in identification of
University of Pennsylvania, otic therapy with or without surgical an etiologic agent. Sites of tenderness
Philadelphia, PA. intervention, are poorly understood.
to palpation may be identified, and
J Am Acad Orthop Surg 2012;20: skin warmth may be noted in the af-
684-693
Diagnosis and fected extremity. Plantar foot sensa-
http://dx.doi.org/10.5435/ tion should be assessed, as well.
JAAOS-20-11-684 Classification
Saltzman et al4 found that the use of
Copyright 2012 by the American Evaluation of the patient with sus- a 4.5-g monofilament to test sensa-
Academy of Orthopaedic Surgeons.
pected foot infection begins by ob- tion at the plantar surface of the first
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 13
Foot & Ankle Oke A. Anakwenze, MD, et al
metatarsal head was highly sensitive other imaging techniques.
(up to 100%) but less specific (67%) Basic assessment of vascular supply
Skin and Nail Bed
in predicting the risk of ulcer devel- must be performed in all cases of
Disorders
opment in patients with diabetic neu- foot infection. In patients with sus-
Many superficial infections of the
ropathy. Dorsalis pedis and posterior pected vascular compromise, the
skin and nail bed (eg, felons, parony-
tibial pulses should be graded via ankle-brachial index (ABI), including
chia, onychomycosis) share much
palpation or Doppler ultrasound, dorsalis pedis and toe wave pressures
with their counterparts in the upper
and perfusion of the toes should be and wave forms, may be obtained to
extremity in terms of pathogenesis
assessed via capillary refill time. assess relative large-vessel perfusion
and management. Although well-
Particular attention should be paid to the extremity. Normal ABI is
>0.9, and an index of <0.45 is pre- characterized in the hand literature,
to hemoglobin and white blood cell
dictive of a poor healing response. felon of the toe has not been widely
(WBC) count as well as to inflam-
matory markers such as erythrocyte Toe wave pressures of 0.45 and 0.2 described as a distinct clinical entity.
sedimentation rate ([ESR], normal mm Hg are predictive of good and It is an infection that occurs within
range, 0 to 15 mm/h) and C-reactive poor healing responses, respectively. the tissue septae of the distal pulp of
protein (CRP) level (normal <1 mg/ Duplex ultrasonography is a nonin- the toe and is commonly the result of
dL). Other disease-specific markers, vasive method that can be used to direct inoculation with locally de-
such as hemoglobin A1C (normal screen for arterial stenoses and ve- structive organisms such as Staphy-
range, 4% to 6%), and nutritional nous outflow obstruction or insuffi- lococcus aureus. Typically, presenta-
markers, such as serum albumin ciency. Invasive imaging of the vas- tion consists of a severely painful,
(normal range, 3.4 to 5.4 g/dL), also culature with angiography may be tense, and erythematous distal toe.
may be useful for detecting infection. required depending on the site of Examination must assess for the ex-
Radiographic evaluation of the suspected vascular compromise or to tent of any local purulent collection.
lower extremity can be tailored assess for intraoperative changes in Surgical drainage with concomitant
based on the findings of the previ- perfusion; however, the use of this antibiotics is the treatment of choice
ously mentioned evaluation. Initial method should be carefully weighed and may be done at the bedside or in
imaging should include weight- against attendant risks of vascular the operating room, depending on
bearing plain radiographs to assess access and contrast administration. patient presentation (Table 1).
for fractures or dislocations, foreign Maintaining a working differential Approximately 1% of patients
bodies, subcutaneous emphysema, diagnosis that includes noninfectious who present to emergency depart-
and associated degenerative changes. etiologies is essential. Gout, deep ments with upper extremity infec-
CT can be used to further evaluate vein thrombosis, compartment syn- tions have paronychia.5 Presentation
the bony architecture. Suspicion of drome, Charcot neuroarthropathy, and treatment of paronychia in the
osteomyelitis may warrant addi- fracture, and malignancy may pre- upper and lower extremity is similar.
tional evaluation with MRI. With ei- sent with patterns of pain, swelling, It is often caused by direct or indirect
ther of these advanced imaging tech- or erythema that may arouse suspi- trauma to the cuticle or nail fold and
niques, consideration must be given cion for infection. Following diagno- may progress to subungual abscess if
to the patient’s renal function before sis, infection may be subclassified untreated. Primary causative organ-
administration of contrast material. into one or more of the following isms include S aureus, Streptococcus
Nuclear medicine studies, including general categories: (1) skin and nail pyogenes, Pseudomonas pyocyanea,
technetium Tc-99m– and indium-In- bed disorders, (2) soft-tissue infec- Proteus vulgaris, and Candida albi-
111–labeled leukocyte scans, can be tion, (3) diabetic foot infections, (4) cans.6 Diagnosis may be based on a
used in the setting of equivocal find- deep infections, and (5) septic arthri- history of minor trauma as well as
ings or relative contraindications to tis. erythema, edema, and/or tenderness
Dr. Stern or an immediate family member serves as a board member, owner, officer, or committee member of the American Board of
Internal Medicine. Dr. Levin or an immediate family member has received royalties from KLS Martin. Dr. Wapner or an immediate
family member has received royalties from Stryker; is a member of a speakers’ bureau or has made paid presentations on behalf of
and serves as a paid consultant to Small Bone Innovations, Wright Medical Technology, and Stryker; and has received research or
institutional support from Small Bone Innovations. None of the following authors or any immediate family member has received
anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the
subject of this article: Dr. Anakwenze, Dr. Milby, and Mr. Gans.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 14
Foot & Ankle Oke A. Anakwenze, MD, et al
Table 1
Surgical Intervention for Foot Infections
Indications Intervention Technical Considerations
Pedal onychomycosis Toenail débridement Early intervention beneficial (<6 mo symp-
tom duration)
Pedal onychocryptosis Toenail resection Multiple procedural variations described
Felon, fluid collection, or abscess Incision and drainage Wound must be probed to remove loculi
and is left open following packing to en-
sure continued drainage
Septic arthritis, infection following open Irrigation and débridement Repeat débridements may be necessary
fracture based on the clinical situation
Infected neuropathic ulcers, necrotizing Soft-tissue débridement Repeat débridements may be necessary
infection every 24 to 36 h to establish wound
margins free of infection
Infection with bony erosion and/or joint External fixation Ilizarov versus tubular frame fixation may
instability, progressive deformity be used based on site of pathology and
remaining bone stock
Osteomyelitis, infected implant, Charcot Staged irrigation and débridement followed Antibiotic-impregnated cement beads or
neuroarthropathy by stabilization or arthrodesis spacers may be used to increase local
drug concentrations
Soft-tissue defect overlying exposed ten- Local/regional soft-tissue transfer for wound Must optimize vascular and nutritional
don or bone coverage status
Infection in the setting of vascular insuffi- Minor/partial amputation Site of amputation must balance the need
ciency, gangrene to eradicate disease while optimizing
potential for rehabilitation
Overwhelming infection with deep tissue Major amputation Site of amputation must balance the need
involvement, systemic toxicity, low po- to eradicate disease while optimizing
tential for rehabilitation potential for rehabilitation
of proximal and lateral nail folds liptic wedge down to the bone. The tous toes with nail scaling and scal-
found on physical examination. If no margins are then undermined, and ing between the toes. Diagnosis
discrete abscess has formed, warm the wound is sutured.8 based on clinical appearance alone is
water compresses and soaking the af- In contrast to paronychia, onycho- common. Definitive diagnosis may
fected digit in Burow solution (ie, mycosis typically occurs in the lower be made by a positive microscopic
aluminum acetate) may be effective. extremity. It is present in 2% to 14% examination of toe nail clippings or
Oral antibiotic therapy with appro- of adults in Western populations, subungual debris with potassium hy-
priate coverage of causative organ- and its prevalence increases with age droxide preparation.9
isms also should be used for persis- and factors such as nail trauma, im- In individuals with intact immu-
tent lesions. munocompromised status, peripheral nity, onychomycosis is primarily a
Surgical intervention is typically re- vascular insufficiency, and Down cosmetic concern. Although a variety
served for cases in which an abscess syndrome.9 Onychomycosis is also a of oral and topical antifungal agents
is present.7 For refractory lesions, risk factor for ulcers in patients with is available to manage the infection,
deep incision under local anesthesia diabetes.10 Most common patho- the benefits of treatment must be
(eg, digital nerve block) may be re- gens include the dermatophytes weighed against the potential toxic-
quired. In our practice, we use the Trichophyton rubrum and T menta- ity of the long treatment course re-
Winograd procedure in cases that grophytes. Of the nondermato- quired to eradicate the infection.12
fail nonsurgical management. The phytes, candida species are most There is level I evidence that nail dé-
nail is split and a 0.25-inch–long common, and saprophytes (molds) bridement with topical antifungal
edge is removed. The matrix is then comprise the remaining causal lacquer may be more effective than
excised or curetted, with the strip of agents.11 débridement alone for management
nail fold removed to create a semiel- Presentation consists of erythema- of onychomycosis in these patients.13
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 15
Foot & Ankle Oke A. Anakwenze, MD, et al
fluctuant collection, surgical débride- ual evidence of infection. Early surgi-
Soft-tissue Infection ment typically is not indicated. cal intervention is of paramount im-
Although less common than celluli- portance; however, one study found
The foot and ankle are at particular
tis, necrotizing infections of the no difference in mortality rate in pa-
risk of soft-tissue infection because
lower extremity can result in limb tients treated with amputation com-
of their role in weight bearing and
loss or death, and a high level of pared with those treated with wide
potential exposure to trauma. More-
clinical suspicion must be main- débridement.16
over, they are frequently affected by tained to facilitate prompt diagnosis Similiarly, the role of hyperbaric
impaired perfusion or sensation as- and management. Two thirds of nec- oxygen (HBO) therapy, which theo-
sociated with systemic conditions. rotizing infections present in the retically increases tissue oxygen ten-
These factors must be taken into ac- lower extremity,15 and this must be sion, has not been fully elucidated in
count when treating patients with considered in the differential diagno- this patient cohort; most studies are
soft-tissue infections of the lower ex- sis in patients with unexplained limb anectodal or retrospective and dem-
tremity as opposed to similar infec- pain, especially in those with com- onstrate conflicting results. In a
tions in other anatomic locations. promised immune systems. Diabetes small retrospective study, Riseman
In a population-based, epidemio- is the most common comorbidity et al18 reported decreased mortality
logic study, cellulitis of the lower ex- identified, and a heightened level of in a group of patients with necrotiz-
tremity was found to be a common suspicion should be maintained ing fasciitis treated with débride-
clinical entity, with an incidence of when evaluating these patients.16,17 ment, antibiotics, and HBO therapy
199 per 100,000 person-years, in- Once a patient exhibits signs of sys- compared with those treated with
creasing incidence with age, and an temic toxicity such as hypotension débridement and antibiotics alone.
equal sex distribution.14 Approxi- and organ failure, mortality ap- Larger prospective studies are
mately 21.6% of the cases resulted in proaches 50% to 70%.15 needed to fully define the role of
hospitalization.14 Cellulitis is most Necrotizing infections may extend HBO therapy for management of
often the result of breaches in skin from an initial skin lesion and subse- necrotizing fasciitis. However, we be-
integrity combined with risk factors quently spread along fascial planes lieve that this therapy should be con-
such as obesity, venous insufficiency, and muscle compartments, or they sidered as an adjunctive option and
or lymphatic disruption from prior may occur insidiously in the absence should not be used in place of sur-
surgery.15 Physical manifestions in- of trauma. These infections are most gery.
clude rapidly spreading areas of often polymicrobial, but causative
edema, redness, and warmth, often agents frequently include Streptococ-
accompanied by lymphangitis and cus pyogenes, S aureus, and anaero- Diabetic Foot Infections
regional lymphadenopathy. Systemic bic streptococci.15 Necrotizing infec-
toxicity is typically absent, and ex- tion must be suspected in the setting More than 18 million Americans
tensive evaluation with blood culture of severe, constant pain dispropor- (6%) have diabetes, with nearly 30%
or skin biopsy is only necessary in tionate to examination, bullae, skin as yet undiagnosed.19 In patients
patients with unusual risk factors or necrosis, cutaneous anesthesia, or with diabetes aged >40 years, nearly
predisposing conditions. subcutaneous tissues with a wooden- 30% have impaired sensation in the
First-line therapy is medical, and hard feel. Infection may spread rap- feet.2 As a result, 10% to 15% of di-
initial antimicrobial agents should idly even after initiation of antibiotic abetic patients will develop a foot in-
include coverage of streptococci and therapy. Systemic toxicity is fre- fection during their lifetimes.20 Foot
staphylococci in the setting of quently observed, as manifested by ulceration in the diabetic population
trauma. Suitable agents include di- fever, leukocytosis, delirium, and re- is the most significant risk factor for
cloxacillin, cephalexin, or erythro- nal failure. Gas in the soft tissues subsequent amputation.21 Significant
mycin; local resistance patterns may be detected by crepitus, palpa- risk factors for ulceration include
should be taken into account when tion, or imaging; however, this is not neuropathy, ischemia, and micro-
selecting an agent. If methicillin- pathognomonic. Early surgical dé- trauma. The neuropathic foot is
resistant S aureus is suspected, then bridement of skin, subcutaneous fat, characterized by the lack of protec-
use of clindamycin, trimethoprim- and fascia is the mainstay of treat- tive sensation and autonomic dysreg-
sulfamethoxazole, vancomycin, dap- ment of necrotizing fasciitis. Repeat ulation, leading to dry skin. The foot
tomycin, or linezolid may be re- débridement may be required every acquires the characteristic “rocker
quired.15 In the absence of a discrete 24 to 36 hours until there is no resid- bottom” deformity caused by degen-
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 16
Foot & Ankle Oke A. Anakwenze, MD, et al
Table 2
Clinical Classification of Diabetic Foot Infections
Manifestation Infection Severitya PEDIS Grade28
Wound lacking purulence or any manifestations of inflammation (ery- Uninfected 1
thema, pain, tenderness, warmth, or induration)
Presence of ≥2 manifestations of inflammation, cellulitis/erythema ex- Mild 2
tending ≤2 cm around the ulcer, with infection limited to the skin or su-
perficial subcutaneous tissues. No other local complications or sys-
temic illness.
Infection (as above) in a patient who is systemically well and metaboli- Moderate 3
cally stable but which has ≥1 of the following characteristics: cellulitis
extending 2 cm, lymphangitic streaking, spread beneath the superficial
fascia, deep-tissue abscess, gangrene, and involvement of muscle,
tendon, joint, or bone
Infection in a patient with systemic toxicity or metabolic instability (eg, Severe 4
fever, chills, tachycardia, hypotension, confusion, vomiting, leukocyto-
sis, acidosis, severe hyperglycemia, or azotemia)
PEDIS = perfusion, extent/size, depth/tissue loss, infection, and sensation
a
Foot ischemia may increase the severity of any infection, and the presence of critical ischemia often makes the infection severe.
Adapted with permission from Lipsky BA, Berendt AR, Deery HG, et al: Diagnosis and treatment of diabetic foot infections. Clin Infect Dis
2004;39(7):885-910.
eration and collapse of the normal presence of an ulcer measuring >2 findings and the patient’s systemic
midfoot arch, resulting in limited cm2; positive probe to bone test in health status20,27 (Table 2). The Wag-
mobility. In addition, atrophy of the which a probe is used to check the ner classification can aid the physi-
intrinsic muscles of the foot allows depth of an ulcer (considered posi- cian in classifying patients into dif-
the stronger flexor muscles to draw tive when the ulcer is deep enough ferent treatment groups; diabetic
the toes up in a clawed position, cre- that the probe touches bone); ESR ulcers are graded based on depth and
ating new or increased points of >70 mm/h; and abnormal findings the presence of osteomyelitis or gan-
pressure at the tips of toes and meta- on radiography such as periosteal grene29 (Table 3).
tarsal heads. This atrophy, combined thickening or sclerosis, osteolysis, Therapeutic management of dia-
with ischemia that is commonly sec- cortical irregularity, or abnormal tra- betic foot ulcers and infections must
ondary to atherosclerosis of the tibial becular architecture.26 In addition, a thoroughly address all of the relevant
and peroneal arteries, is the main thorough and careful vascular exam- causative factors. Although ulcer-
causative factor that leads to ulcer ination must be performed. At mini- ation often precedes and coexists
development.22,23 Once an ulcer is mum, this should include documen- with infection, the two are by no
present, poor nutritional status (al- tation of dorsalis pedis and tibialis means inextricably linked. In the ab-
bumin level <3.5 g/dL) portends an artery pulses, with Doppler ultra- sence of the clinical stigmata of in-
unfavorable prognosis for wound sound and ABI assessment as needed. fection, there is no evidence to sup-
healing.24 Further imaging, including CT an- port routine antibiotic use as an
Infection is not necessarily present giography and magnetic resonance adjunct to ulcer healing.27 Whenever
or a prerequisite for development of angiography, may be of benefit in possible, clean biopsy and culture
these ulcers. Approximately 10% to terms of preoperative planning and should be obtained to determine the
20% of patients with diabetic foot does not have the risks inherent in appropriate organism-specific ther-
ulcers develop osteomyelitis.25 Estab- invasive angiography. apy. For ulcers with gross evidence
lishing the presence of concomitant The Infectious Diseases Society of of infection, the initial empiric regi-
infection is essential. In a meta- America and the International Work- men must take into account the se-
analysis of studies of diabetic pa- ing Group for the Diabetic Foot have verity of infection and likely etiologic
tients with osteomyelitis of the lower suggested and validated a classifica- agents. Empiric broad-spectrum anti-
extremity, the authors found that the tion and grading system whereby biotic therapy should be reserved for
following factors aided in diagnosis such infections may be labeled mild, severe infections and should be nar-
and were predictive of infection: moderate, or severe based on clinical rowed based on culture results and
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 17
Foot & Ankle Oke A. Anakwenze, MD, et al
Table 3
Wagner Classification of Diabetic Ulcers and the Authors’ Preferred Treatment
Grade Description Treatment
0 Skin intact but bony deformities lead Total contact casting
to “foot at risk”
1 Localized superficial ulcer Total contact casting ± irrigation and débridement
2 Ulcer deep to tendon, bone, ligament, Irrigation, débridement, and biopsy
or joint Correction of deforming plantar pressure-creating forces as needed (eg,
Achilles tendon lengthening, shoe modification)
Culture-specific antibiotic
Total contact casting
3 Deep abscess or osteomyelitis Irrigation, débridement, and biopsy as needed
Correction of deforming forces
Culture-specific antibiotic
Total contact casting
For significant skin defects: Free flap with plastic surgery consultation
when possible
Partial calcanectomy if heel defect is not salvageable
Amputation when all other options have failed
4 Gangrene of toes or forefoot Low-level, safe local amputation
5 Gangrene of entire foot Amputation
antibiotic susceptibility data. patients with extensive medical co- therapy. In a study of 10 diabetic pa-
For plantar ulcerations in direct morbidities or in those who lack tients with forefoot plantar ulcer-
weight-bearing areas, force patterns suitable vein graft or distal outflow ation treated with percutaneous
must be altered sufficiently to allow vessels, percutaneous transluminal Achilles tendon lengthening, Arm-
recovery of the soft-tissue envelope. angioplasty with or without stenting strong et al35 noted a significant re-
Total contact casting with continued can be employed.32 Rates of duction in forefoot dynamic pressure
intermittent débridements and cast amputation-free survival are similar along the plantar surface and signifi-
changes every 2 to 4 weeks is an ef- to those of open procedures, and cantly increased dorsiflexion on gait
fective initial approach.30 Reusable length and cost of hospitalization are analysis.
pneumatic orthoses may be used in both decreased in the short-term.33 Management of heel ulcers can be
cases that require more frequent However, these benefits must be challenging given the difficulty of at-
wound checks; however, this conve- weighed against the increased risk of taining adequate soft-tissue coverage
nience must be weighed against the restenosis and contrast nephrotoxic- even after eradication of infection.
increased risk of patient noncompli- ity. Therefore, many patients with heel
ance. Rocker-sole shoes can be used Surgical intervention is indicated ulcers undergo below-knee amputa-
to offload weight from the forefoot; for deep sequestered purulent collec- tion. Sural fasciomusculocutaneous
compared with other shoe therapeu- tions, extensive bone or joint in- free flaps have been used to provide
tic modifications, these shoes have volvement, or soft-tissue necrosis.27 wound coverage, and promising re-
been shown to significantly reduce Correction of deformities or bony sults have been reported in a small
forefoot pressure.31 prominences is essential to the long- case series.36 However, this approach
In patients with impaired vascular- term prevention of ulcer recurrence requires an adequate hospital facility,
ization, restoration of arterial blood caused by alterations in local pres- an experienced microvascular sur-
flow is essential to promote wound sure patterns.34 Achilles tendon geon, and patency of collateral ves-
healing and relieve pain. For occlu- lengthening is an effective way to re- sels for flap circulation and may lead
sive disease distal to the knee, the lieve pressure along the metatarsal to significant donor site morbidity.
historic standard of care has been heads, thereby preventing or effec- Alternatively, a partial calcanectomy
distal tibial or pedal grafting. In ap- tively treating ulcers in patients with can be used and may preclude the
propriate candidates, open revascu- significant pressure along the fore- need for below-knee amputation. In
larization leads to superior long-term foot secondary to deformity and in a study of 12 patients with calcaneal
patency and clinical durability.22 In those who have failed nonsurgical ulcers treated with partial calcanec-
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 18
Foot & Ankle Oke A. Anakwenze, MD, et al
tomy, Smith et al37 reported that ul- tis treated nonsurgically, Senneville guide treatment of ankle infection in
cers healed in 10 patients and that all et al39 found that bone culture–spe- patients with ipsilateral hip or knee
patients had reasonable healing po- cific antibiotic therapy (as opposed prosthesis. This cohort of patients re-
tential based on albumin (>3 g/dL), to soft-tissue swap culture) was the quires aggressive treatment aimed at
ABI (>0.45), lymphocyte count only factor predictive of successful eradicating infection before it
(>1,500), and transcutaneous oxygen treatment. spreads to the implant. In these pa-
pressure (>28 mm Hg). Our pre- Indications for surgical interven- tients, we recommend treatment sim-
ferred treatment for diabetic ulcers is tion in patients with osteomyelitis of ilar to that for other types of remote
based on the Wagner classification the lower extremity are largely de- infection, with the knowledge that
(Table 3). pendent on etiology. Early aggressive infections of the foot and ankle may
débridement is necessary for man- be more challenging to clear. Thor-
agement of penetrating traumatic in- ough examination of the joint with
Deep Infections juries or open wounds, whereas early the implant is necessary to assess for
débridement in the setting of chronic any change in appearance (eg, swell-
Osteomyelitis can occur in the pres- disease and systemic illness is contro- ing, drainage, warmth, erythema),
ence or absence of skin ulceration. versial because acceptable results range of motion, or pain with mo-
MRI has proved to be superior to have been reported with nonsurgical tion. The patient should be asked
other imaging modalities for detec- therapy alone.25,40 In patients with about any increased discomfort
tion of foot osteomyelitis.27 MRI compromised bone structure or sta- about the affected joint. If there is
may demonstrate signal changes bility and progressive deformity, ex- suspicion for a seeded joint based on
within the bone and deep or superfi- ternal fixation may be used to stabi- clinical examination findings, his-
cial tissue. In addition, purulent col- lize the foot while allowing ongoing tory, and elevated ESR and CRP
lections, soft-tissue edema, and syno- treatment of infection. Débridement level, we recommend joint aspiration
vial enhancement can also be with arthrodesis and external fixa- to assess cell count (normal, <1,100
appreciated by signal changes in af- tion following drainage of acute in- cell/mL, <64% neutrophils), Gram
fected areas. However, in the setting fection may provide an alternative to stain and culture, and crystal analy-
of Charcot arthropathy, MRI speci- amputation. In a series of 45 patients sis.43 Positive results are indicative of
ficity is approximately 80%. In the with Charcot arthropathy and osteo- a hematogenous infection, and treat-
setting of equivocal MRI findings, myelitis treated with débridement, ment is based on duration of symp-
an In-111–labeled leukocyte scan fusion, and external fixation, the au- toms. Specific management options
should be performed. A high- thors reported successful fusion in 39 are beyond the scope of this review.
intensity signal represents pooling of patients at a mean follow-up of 25.7 In patients with hematogenous
leukocytes in the affected region; weeks.41 In patients with large soft- periprosthetic infections associated
normal signal intensity represents the tissue defects, local or free tissue with foot or ankle infections, we rec-
absence of elevated leukocyte levels transfer (eg, vascularized soft tissue ommend treatment based on the
in both osteomyelitis and Charcot ar- flaps, autogenous bone grafts, vascu- American Academy of Orthopaedic
thropathy.38 larized bone grafts) may be used to Surgeons clinical practice guide-
Patients with osteomyelitis typi- restore the integrity of the soft-tissue lines.44
cally require a long course of tar- envelope.42 When infection is associ-
geted antibiotic therapy for complete ated with life-threatening systemic
eradication or suppression of infec- symptoms or occurs in a low- Septic Arthritis
tion. Due to the compounding of demand patient with little prospect
toxicity over the course of treatment, of rehabilitation, amputation may be The incidence of septic arthritis, or
tailoring the antibiotic regimen to the sole remaining surgical option. infection within the joint, ranges
the causative organism is essential Amputation must include as much of from approximately 2 to 10 per
(Table 4). Even when extensive surgi- the diseased tissue as possible while 100,000 persons.45 Approximately
cal intervention is not required, bone attempting to preserve enough resid- 3% to 7% of septic arthritis cases in-
biopsy may be indicated because ual limb for function recovery, ade- volve the foot and ankle.46,47 Septic
bone culture sensitivity is predictive quate wound healing, rehabilitation, arthritis may arise from local inocu-
of successful nonsurgical treatment. and accommodation of the prosthe- lation or hematogenous spread, with
In a retrospective multicenter study sis. the latter being more common in
of diabetic patients with osteomyeli- Adequate literature is lacking to children with open epiphyses than in
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 19
Foot & Ankle Oke A. Anakwenze, MD, et al
Table 4
Antibiotic Therapy for Management of Foot Infections
Antibiotic Route Suggested Dose Coverage Notes
Cephalexin Oral 500 mg every 6 h Staphylococcus, Strepto- Low serum levels
coccus, Gram-negative
bacteria
Amoxicillin-clavulanate Oral 500 mg every 6 h Staphylococcus, Strepto- Broad spectrum, potential
coccus, Gram-negative for diarrhea
bacteria, anaerobes
Clindamycin Oral 300 mg every 8 h Staphylococcus, Strepto- High osseous penetra-
coccus, anaerobes tion, potential for diar-
rhea
Ciprofloxacin Oral 750 mg every 12 h Gram-negative bacteria, Not effective for Gram-
Pseudomonas positive bacteria or an-
aerobes
Levofloxacin Oral 500 mg every 12 h Streptococcus, Gram- Not effective for anaer-
negative bacteria obes
Metronidazole Oral 500 mg every 8 h Gram-negative bacteria, High osseous penetra-
anaerobes tion, metallic taste
Trimethoprim- Oral 800/160 mg every 12 h Gram-negative bacteria Potential MRSA coverage
sulfamethoxazole dependent on local re-
sistance patterns
Cefazolin Intravenous 1 g every 8 h Staphylococcus, Strepto- Not effective for MRSA,
coccus, Gram-negative many Gram-negative
bacteria bacteria now resistant
Nafcillin Intravenous 2 g every 6 h Staphylococcus, Strepto- Not effective for MRSA
coccus
Ampicillin-sulbactam Intravenous 3 g every 8 h Staphylococcus, Strepto- Not effective for MRSA
coccus, Gram-negative
bacteria, anaerobes
Piperacillin-tazobactam Intravenous 3.375 g every 8 h Streptococcus, Gram- Effective for resistant
negative bacteria, Gram-negative bacteria
Pseudomonas
Vancomycin Intravenous 1 g every 12 h Staphylococcus, Strepto- MSRA coverage; nephro-
coccus toxic—must dose by
level
Levofloxacin Intravenous 500 mg every 12 h Streptococcus, Gram- Not effective for anaer-
negative bacteria obes, questionable ef-
fectiveness for Staphy-
lococcus species
Aztreonam Intravenous 1 g every 8 h Gram-negative bacteria Appropriate for patients
with penicillin and ceph-
alosporin allergies
MRSA = methicillin-resistant Staphylococcus aureus
adults. The tibiotalar and first meta- or intravenous drug abuse.48 Patients vated in all patients, with a mean
tarsophalangeal joints are most often commonly present with acutely swol- ESR of 82 mm/h and CRP level of
affected, presumably because of their len, warm, erythematous joints, in- 16.9 mg/dL reported. These findings
capacious size in comparison with ability to bear weight, and severe suggest that these nonspecific mark-
other joints of the foot and ankle. S pain with micromotion. Plain radi- ers can be used to rule out ankle in-
aureus is the most commonly iso- ography is typically nonspecific but fection. In contrast, the peripheral
lated causative organism.48 may reveal joint effusion. Holtom WBC count was found to be neither
Adjacent osteomyelitis is increas- et al48 reviewed 30 patients with sep- sensitive nor specific enough to be
ingly of concern in the setting of co- sis about the ankle joint and noted relied on for diagnosis of an acute
morbidities such as diabetes mellitus that the ESR and CRP level was ele- septic joint.48 MRI was found to be
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 20
Foot & Ankle Oke A. Anakwenze, MD, et al
Figure 1
References
Evidence-based Medicine: Levels of ev-
idence are described in the table of con-
tents. In this article, References 4, 13,
20, 31, 33-35, 45, 47, and 48 are level
II studies. References 17, 23, and 24
are level III studies. References 16, 21,
36-41, and 43 are level IV studies. Ref-
erences 5 and 8 are level V expert opin-
ion.
References printed in bold type are
those published within the past 5 years.
1. Pitts SR, Niska RW, Xu J, Burt CW; Di-
vision of Health Care Statistics: National
Algorithm for management of foot and ankle infections. Hospital Ambulatory Medical Care Sur-
vey: 2006 Emergency Department Sum-
mary. National Health Statistics Reports
2008;(7):1-40.
more effective than radiography for may be performed until he or she is 2. Centers for Disease Control and
diagnosis of sepsis with and without stable enough for surgery. If immedi- Prevention: National Diabetes Fact
Sheet: General Information and National
concomitant osteomyelitis. In cases ate surgical intervention is planned, Estimates on Diabetes in the United
with sufficient clinical suspicion for then initiation of antibiotic therapy States, 2007. Atlanta, GA, US
Department of Health and Human
septic arthritis, joint aspiration is the should be delayed until results of in- Services, 2008.
diagnostic tool of choice. WBC dif- traoperative cultures are obtained.
3. Adams K, Corrigan JM: Priority Areas
ferential counts between 50,000 and Determination of causative pathogen for National Action: Transforming
100,000 and a neutrophil shift and antibiotic sensitivities can obvi- Health Care Quality. Washington, DC,
National Academies Press, 2003.
>75% are commonly used as a cutoff ate the need for repeat surgical inter-
for infections as opposed to inflam- vention with its attendant morbidity. 4. Saltzman CL, Rashid R, Hayes A, et al:
4.5-gram monofilament sensation be-
matory conditions, which may pre- neath both first metatarsal heads indi-
sent with lower values; however, in cates protective foot sensation in diabetic
patients. J Bone Joint Surg Am 2004;
cases that are concerning for ankle Summary 86(4):717-723.
sepsis, one must be aware of inter-
5. Losanoff JE, Missavage AE, Linneman P,
laboratory variability in the assess- Infections of the foot and ankle are a Terry BE: Can paronychia cause a re-
ment of synovial fluid, whereby the common source of morbidity, dis- mote necrotizing soft tissue infection?
ability, and potential limb loss and J Emerg Med 2011;40(1):e11-e13.
same synovial fluid may yield differ-
ent values when assayed at different pose particular therapeutic chal- 6. Brook I: Paronychia: A mixed infection.
Microbiology and management. J Hand
laboratories.49 Gram stain and cul- lenges given their multifactorial etiol- Surg Br 1993;18(3):358-359.
ture can aid in narrowing the differ- ogy and frequent association with
7. Shaw J, Body R: Best evidence topic re-
ential count, with the culture being systemic illness. A systematic and port: Incision and drainage preferable to
more sensitive (75% to 95%) and multidisciplinary approach is essen- oral antibiotics in acute paronychial nail
infection? Emerg Med J 2005;22(11):
specific (>90%) for infection.50 tial for prevention and to guide ther- 813-814.
Surgical arthrotomy with irrigation apy (Figure 1). In patients with
8. Winograd AM: A modification of the
and débridement is the mainstay of peripheral neuropathy, a large pro- technic of operation for ingrown toenail.
treatment for acute bacterial septic portion of foot infections and associ- JAMA 1929;92(3):229-230.
arthritis to prevent articular damage ated morbidity can be prevented 9. de Berker D: Clinical practice: Fungal
and hematogenous spread. This pro- through careful surveillance. Addi- nail disease. N Engl J Med 2009;
360(20):2108-2116.
cedure can be performed with ar- tional evidence is necessary to deter-
mine standardized indications for 10. Mayser P, Freund V, Budihardja D: Toe-
throscopic or open techniques based
nail onychomycosis in diabetic patients:
on the clinical scenario and surgeon surgical intervention in patients with Issues and management. Am J Clin
preference. In the patient who is not neuropathic ulcers and lower ex- Dermatol 2009;10(4):211-220.
yet medically stable, serial aspiration tremity osteomyelitis. 11. Ghannoum MA, Hajjeh RA, Scher R,
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 21
Foot & Ankle Oke A. Anakwenze, MD, et al
et al: A large-scale North American Surg Br 1985;67(1):79-85. 38. Marcus CD, Ladam-Marcus VJ, Leone J,
study of fungal isolates from nails: The Malgrange D, Bonnet-Gausserand FM,
24. Pinzur M, Kaminsky M, Sage R, Cronin Menanteau BP: MR imaging of osteomy-
frequency of onychomycosis, fungal dis-
R, Osterman H: Amputations at the mid- elitis and neuropathic osteoarthropathy
tribution, and antifungal susceptibility
dle level of the foot: A retrospective and in the feet of diabetics. Radiographics
patterns. J Am Acad Dermatol 2000;
prospective review. J Bone Joint Surg Am 1996;16(6):1337-1348.
43(4):641-648.
1986;68(7):1061-1064.
12. Kumar S, Kimball AB: New antifungal 39. Senneville E, Lombart A, Beltrand E,
25. Game F: Management of osteomyelitis of et al: Outcome of diabetic foot osteomy-
therapies for the treatment of onychomy-
cosis. Expert Opin Investig Drugs 2009; the foot in diabetes mellitus. Nat Rev elitis treated nonsurgically: A retrospec-
18(6):727-734. Endocrinol 2010;6(1):43-47. tive cohort study. Diabetes Care 2008;
31(4):637-642.
13. Malay DS, Yi S, Borowsky P, Downey 26. Butalia S, Palda VA, Sargeant RJ, Detsky
MS, Mlodzienski AJ: Efficacy of debride- AS, Mourad O: Does this patient with 40. Berendt AR, Peters EJ, Bakker K, et al:
ment alone versus debridement com- diabetes have osteomyelitis of the lower Diabetic foot osteomyelitis: A progress
bined with topical antifungal nail lacquer extremity? JAMA 2008;299(7):806-813. report on diagnosis and a systematic re-
for the treatment of pedal onychomyco- view of treatment. Diabetes Metab Res
27. Lipsky BA, Berendt AR, Deery HG, et al: Rev 2008;24(suppl 1):S145-S161.
sis: A randomized, controlled trial.
Diagnosis and treatment of diabetic foot
J Foot Ankle Surg 2009;48(3):294-308.
infections. Clin Infect Dis 2004;39(7): 41. Dalla Paola L, Brocco E, Ceccacci T,
14. McNamara DR, Tleyjeh IM, Berbari EF, 885-910. et al: Limb salvage in Charcot foot and
et al: Incidence of lower-extremity cellu- ankle osteomyelitis: Combined use single
litis: A population-based study in Olm- 28. International Working Group on the stage/double stage of arthrodesis and
sted county, Minnesota. Mayo Clin Proc Diabetic Foot: International Consensus external fixation. Foot Ankle Int 2009;
2007;82(7):817-821. on the Diabetic Foot [CD-ROM]. 30(11):1065-1070.
Brussels, Belgium, International Diabetes
15. Stevens DL, Bisno AL, Chambers HF, Foundation, 2003. 42. Bishop AT, Wood MB, Sheetz KK: Ar-
et al: Practice guidelines for the diagnosis throdesis of the ankle with a free vascu-
and management of skin and soft-tissue 29. Wagner FW Jr: The dysvascular foot: A larized autogenous bone graft: Recon-
infections. Clin Infect Dis 2005;41(10): system for diagnosis and treatment. Foot struction of segmental loss of bone
1373-1406. Ankle 1981;2(2):64-122. secondary to osteomyelitis, tumor, or
30. Tyrrell W: Orthotic intervention in pa- trauma. J Bone Joint Surg Am 1995;
16. Ozalay M, Ozkoc G, Akpinar S, Hersekli
tients with diabetic foot ulceration. 77(12):1867-1875.
MA, Tandogan RN: Necrotizing soft-
tissue infection of a limb: Clinical pre- J Wound Care 1999;8(10):530-532.
43. Ghanem E, Parvizi J, Burnett RS, et al:
sentation and factors related to mortal- 31. Brown D, Wertsch JJ, Harris GF, Klein J, Cell count and differential of aspirated
ity. Foot Ankle Int 2006;27(8):598-605. Janisse D: Effect of rocker soles on plan- fluid in the diagnosis of infection at the
17. Bellapianta JM, Ljungquist K, Tobin E, tar pressures. Arch Phys Med Rehabil site of total knee arthroplasty. J Bone
Uhl R: Necrotizing fasciitis. J Am Acad 2004;85(1):81-86. Joint Surg Am 2008;90(8):1637-1643.
Orthop Surg 2009;17(3):174-182. 32. Commeau P: Endovascular procedures 44. Parvizi J, Della Valle CJ: AAOS Clinical
18. Riseman JA, Zamboni WA, Curtis A, for below the knee arteries in diabetics. Practice Guideline: Diagnosis and treat-
Graham DR, Konrad HR, Ross DS: Hy- Ann Cardiol Angeiol (Paris) 2008;57(6): ment of periprosthetic joint infections of
perbaric oxygen therapy for necrotizing 352-358. the hip and knee. J Am Acad Orthop
fasciitis reduces mortality and the need Surg 2010;18(12):771-772.
33. Adam DJ, Beard JD, Cleveland T, et al:
for debridements. Surgery 1990;108(5): Bypass versus angioplasty in severe 45. Kaandorp CJ, Van Schaardenburg D,
847-850. ischaemia of the leg (BASIL): Multi- Krijnen P, Habbema JD, van de Laar
19. Kruzikas DT, Jiang HJ, Remus D, Bar- centre, randomised controlled trial. MA: Risk factors for septic arthritis in
rett ML, Coffey RM, Andrews R: Pre- Lancet 2005;366(9501):1925-1934. patients with joint disease: A prospective
ventable Hospitalizations: A Window study. Arthritis Rheum 1995;38(12):
34. Mueller MJ, Hastings M, Commean PK,
Into Primary and Preventive Care, 2000. 1819-1825.
et al: Forefoot structural predictors of
Rockville, MD, Agency for Healthcare plantar pressures during walking in peo- 46. Vispo Seara JL, Barthel T, Schmitz H,
Research and Quality, 2000. ple with diabetes and peripheral neurop- Eulert J: Arthroscopic treatment of septic
20. Lavery LA, Armstrong DG, Murdoch athy. J Biomech 2003;36(7):1009-1017. joints: Prognostic factors. Arch Orthop
DP, Peters EJ, Lipsky BA: Validation of 35. Armstrong DG, Stacpoole-Shea S, Trauma Surg 2002;122(4):204-211.
the Infectious Diseases Society of Ameri- Nguyen H, Harkless LB: Lengthening of
ca’s diabetic foot infection classification 47. Stutz G, Kuster MS, Kleinstück F,
the Achilles tendon in diabetic patients Gächter A: Arthroscopic management of
system. Clin Infect Dis 2007;44(4):562- who are at high risk for ulceration of the
565. septic arthritis: Stages of infection and
foot. J Bone Joint Surg Am 1999;81(4): results. Knee Surg Sports Traumatol
21. Rosenbloom AL, Silverstein JH, Lezotte 535-538. Arthrosc 2000;8(5):270-274.
DC, Richardson K, McCallum M: Lim-
36. Chen SL, Chen TM, Chou TD, Chang 48. Holtom PD, Borges L, Zalavras CG: He-
ited joint mobility in childhood diabetes
SC, Wang HJ: Distally based sural fas- matogenous septic ankle arthritis. Clin
mellitus indicates increased risk for mi-
ciomusculocutaneous flap for chronic Orthop Relat Res 2008;466(6):1388-
crovascular disease. N Engl J Med 1981;
calcaneal osteomyelitis in diabetic pa- 1391.
305(4):191-194.
tients. Ann Plast Surg 2005;54(1):44-48.
22. Kalish J, Hamdan A: Management of 49. Hasselbacher P: Variation in synovial
37. Smith DG, Stuck RM, Ketner L, Sage fluid analysis by hospital laboratories.
diabetic foot problems. J Vasc Surg
RM, Pinzur MS: Partial calcanectomy Arthritis Rheum 1987;30(6):637-642.
2010;51(2):476-486.
for the treatment of large ulcerations of
23. Duckworth T, Boulton AJ, Betts RP, the heel and calcaneal osteomyelitis: An 50. Swan A, Amer H, Dieppe P: The value of
Franks CI, Ward JD: Plantar pressure amputation of the back of the foot. synovial fluid assays in the diagnosis of
measurements and the prevention of ul- J Bone Joint Surg Am 1992;74(4):571- joint disease: A literature survey. Ann
ceration in the diabetic foot. J Bone Joint 576. Rheum Dis 2002;61(6):493-498.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 22
Review Article
Foot Compartment Syndrome:
Diagnosis and Management
Abstract
Andrew Dodd, MD Although uncommon, foot compartment syndrome (FCS) is a
Ian Le, MD, FRCSC distinct clinical entity that typically results from high-energy
fractures and crush injuries. In the literature, the reported number
of anatomic compartments in the foot has ranged from 3 to 10, and
the clinical relevance of these compartments has recently been
investigated. Diagnosis of FCS can be challenging because the
signs and symptoms are less reliable indicators than those of
compartment syndrome in other areas of the body. This may lead
to a delay in diagnosis. The role of fasciotomy in management of
FCS has been debated, but no high-level evidence exists to guide
decision making. Nevertheless, emergent fasciotomy is commonly
recommended with the goal of preventing chronic pain and
deformity. Surgical intervention may also be necessary for the
correction of secondary deformity.
F oot compartment syndrome
(FCS) is relatively uncommon.1,2
Although isolated foot injuries result
patients with isolated calcaneal frac-
tures and suspected FCS underwent a
fasciotomy.
in FCS in only 2% of cases,3 ortho- Stiffness, chronic disability, defor-
paedic surgeons must remain aware mity, and pain are some of the com-
of this clinical entity because it can plications associated with untreated
result in negative sequelae. FCS ac- FCS2,4-8,10-13,15,16 (Table 1). Necrosis of
counts for <5% of limb compart- the intrinsic muscles of the foot can
ment syndrome cases.4 lead to ischemic contractures that
Typically, FCS is the result of high- may result in claw toe, hammer toe,
From the Section of Orthopaedic energy injuries to the foot such as and pes cavus. Neurovascular injury
Surgery, University of Calgary,
crush injuries, Lisfranc fracture- can also cause chronic pain and an
Calgary, Alberta, Canada.
dislocations, midfoot and forefoot insensate foot with secondary neuro-
Neither of the following authors nor
any immediate family member has
trauma, and calcaneal fractures.2,3,5-14 pathic pathology (eg, chronic ulcer-
received anything of value from or FCS can also develop after a tibial ation, joint destruction).2,5-8,10,12,13,15
has stock or stock options held in a fracture secondary to the communi-
commercial company or institution cation between the deep posterior
related directly or indirectly to the
subject of this article: Dr. Dodd and compartment of the leg and the cal- Pathophysiology
Dr. Le. caneal compartment of the foot.7
J Am Acad Orthop Surg 2013;21:
The most commonly cited etiology is Compartment syndrome is caused by
657-664 a high-energy fracture of the calca- increasing pressure secondary to
neus, which results in FCS in up to hemorrhage or edema within an ana-
http://dx.doi.org/10.5435/
JAAOS-21-11-657 10% of cases.3,10,12,15 However, data tomic compartment bound by inelas-
from a study by Thakur et al3 sug- tic fibrous tissue. Pressures rise until
Copyright 2013 by the American
Academy of Orthopaedic Surgeons. gest that this patient population may capillary perfusion pressure is ex-
be undertreated because only 1% of ceeded, resulting in ischemia, soft-
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 23
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
Table 1 ported high rates of sensory distur- the anatomic compartments of the
bance and pain at rest in patients foot using high-resolution MRI. The
Potential Complications
Associated With Untreated Foot treated for lower limb compartment authors found a 10th compartment
Compartment Syndrome syndrome. To our knowledge, no in addition to the 9 compartments
studies have examined the prevalence described by Manoli and Weber.26
Chronic pain
or natural history of neuropathic The 10th compartment is bounded
Insensate foot
pain in the setting of acute FCS. by the skin and contains the extensor
Foot and ankle stiffness
digitorum brevis and the extensor
Claw toe deformity
hallucis brevis in a newly described
Hammer toe deformity
Anatomy dorsal compartment.
Cavus foot deformity
In a cadaver study of the myofas-
Neuropathic pain
Understanding of the myofascial cial compartments of the foot, Ling
Neuropathic ulceration
compartments of the foot continues and Kumar8 dissected 13 feet and
to evolve. Early reports identified found three vertical fibrous septae in
four fascial compartments: medial, the hindfoot that, along with the
tissue compromise, and subsequent lateral, central, and interosseous.22-24 plantar aponeurosis, form the com-
necrosis followed by fibrosis and Myerson25 described methods for partments of the foot (Figure 1).
contracture of the compartment’s surgical decompression of these com- These results were substantially dif-
contents.2,4 partments. ferent from those of prior studies.
Claw toe is the most common se- Manoli and Weber26 performed in- The septae bound compartments
quela of FCS and develops when the fusion studies and reported that the identified as medial, intermediate,
extrinsic musculature overpowers foot could be divided into nine ana- and lateral. Skin and subcutaneous
the weak or scarred intrinsic foot tomic compartments, with the cen- tissue compose the medial border of
muscles, whereas cavus deformity is tral compartment divided into super- the medial compartment. As such,
the result of scarred and contracted ficial central and deep central (or only the intermediate and lateral
plantar structures.2 In the setting of calcaneal) compartments. They also compartments are rigidly bound by
intra-articular calcaneal fracture, increased the number of interosseous fascia on all sides. The authors found
claw toe develops after the fracture compartments from one to four, add- no evidence of a thick fascial layer
hematoma in the deep central com- ing a compartment for the adductor between the previously described su-
partment of the foot raises pressures hallucis muscle. New decompression perficial central and deep central
and compresses the medial and lat- techniques using multiple incisions (calcaneal) compartments, finding
eral plantar neurovascular bun- were recommended based on the in- only a thin and often incomplete
dles.12,15 This results in ischemic in- creased number of compartments.26 filmy layer of tissue instead. They
sult to the interosseous muscles and Guyton et al27 questioned the va- concluded that the intermediate and
quadratus plantae muscle, which de- lidity of previous gelatin infusion lateral compartments are the only
rive their blood supply from the me- studies in defining anatomic com- compartments that need surgical de-
dial and lateral plantar arteries. partments and accurately measuring compression and recommended a
Acute compartment syndrome can them without image guidance. The single plantar-based surgical ap-
also cause ischemic neuropathy and authors performed infusion studies proach to do so. These findings con-
chronic neuropathic pain.17 Periph- using CT guidance with simultane- flict with those of Stotts et al29 who
eral nerves may undergo irreversible ous compartment pressure monitor- reported on an isolated medial com-
damage after 4 to 6 hours of isch- ing, focusing on the distinction be- partment syndrome in the foot that
emia.17 Symptoms of neuropathic tween the superficial and deep required surgical decompression,
pain include numbness, spontaneous central compartments. They demon- which suggests that the medial com-
pain, allodynia, and hyperalgesia.18 strated active fluid communication partment is capable of developing
Neuropathic pain is associated with between the two compartments as pressures sufficient to warrant de-
poor general health and a decrease in pressures rose above 10 mm Hg. In compression.
many quality of life measurements.19 addition, they commented on the dif- Ling and Kumar8 attempted to
Management of neuropathic pain is ficulty of inserting an infusion needle qualify the clinical importance of the
difficult and the outcomes are gener- into the superficial central compart- foot compartments with regard to
ally poor. Multimodal drug therapy ment even with CT guidance. surgical decompression and con-
is often necessary.20 Frink et al21 re- Reach et al28 further investigated cluded that only two rigidly bound
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 24
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
Figure 1 tense swelling. Other authors agree
that although the presence of tense
swelling is not necessarily diagnostic,
it is suggestive of FCS.11-13,31 Substan-
tial pain with passive dorsiflexion of
the toes is a common physical find-
ing, but it may be present in the ab-
sence of compartment syn-
drome.1,2,11,13,30 Passive dorsiflexion
of the toes decreases the volume of
the interosseous compartments,
which exacerbates pain.2 Sensory
changes can be nonspecific, with the
most sensitive findings being de-
creased two-point discrimination
and decreased light touch on the
plantar aspect of the foot and toes.
Decreased pin-prick sensation is a
less sensitive finding.1,2,11,13,30,31 Motor
strength and the presence or absence
of palpable pulses are poor indica-
Illustration demonstrating the anatomic structures of the foot, including the tors of a developing compartment
three vertical septae (medial, intermediate, and lateral) that form the two syndrome.2 Serial examinations are
major compartments of the foot described by Ling and Kumar.8 (Reproduced helpful to observe changes in pain
with permission from Ling ZX, Kumar VP: The myofascial compartments of patterns and sensory findings.2
the foot: A cadaver study. J Bone Joint Surg Br 2008;90[8]:1114-1118.)
Compartment Pressure
compartments exist, which may sug- high-energy fractures and severe
Monitoring
gest that the clinical sequelae of FCS crush injuries to the foot are at risk
are a result of injury to the medial of developing FCS and should be FCS can be difficult to diagnose
and lateral plantar arteries and monitored serially.1,2 Open fractures based on physical findings; therefore,
nerves that traverse the newly termed and wounds do not result in reliable most authors agree that compart-
intermediate compartment. More re- decompression of myofascial com- ment pressure monitoring is the most
search is needed to confirm or refute partments and the presence or devel- reliable method for objective diagno-
these conclusions, including prospec- opment of compartment syndrome sis of FCS.1,2,4,5,11-13,30,32 Myerson1 rec-
tive studies comparing the new de- cannot be ruled out in the setting of ommends liberal use of pressure
compression technique described by these injuries.1 monitoring because increased pres-
the authors with more aggressive re- sures often precede clinical signs and
Pain associated with FCS has been
leases of all nine compartments of symptoms. Some authors advocate
described as a severe, relentless burn-
the foot. liberal pressure monitoring for any
ing that encompasses the entire
foot.12 Determining whether the pain foot trauma with significant swell-
Diagnosis and Physical is out of proportion to the injury is ing.1,30 Benefits of pressure monitor-
Examination difficult given the severe trauma typi- ing include the ability to monitor the
cally involved.1 Indications of a de- trend of the compartment pressures
Although diagnosis of FCS is estab- veloping FCS include progressive and to document adequate decom-
lished clinically and follows the same pain despite immobilization of the pression after fasciotomies.1,13
principles as those for diagnosis of foot and increasing analgesic re- In general, absolute compartment
compartment syndrome in other ar- quirement.1,2,13 pressures >30 mm Hg are an indica-
eas of the body, the signs and symp- In a series of 12 cases of FCS, Fak- tion for emergent decompres-
toms of FCS tend to be less reli- houri and Manoli30 reported that the sion.1,2,4,12,30,32 This indication is sup-
able.1,4 Patients who present with most consistent physical finding was ported by the findings of Mittlmeier
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 25
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
Figure 2
Photographs demonstrating the entry points for compartment pressure monitoring of the medial and calcaneal
compartments (A), superficial and deep central compartments (B), and lateral and interosseous compartments (C)
based on the specific needle placement landmarks of Reach et al.33 In panel A, for example, the needle entry point to
the calcaneal compartment is approximately 60 mm distal to the most prominent aspect of the medial malleolus.
et al16 in a study of 17 patients with measurement of pressures in particu- made to measure this compartment’s
calcaneal fractures, 12 of whom had lar compartments or the number of pressure.
central compartment pressures >30 compartments that should be mea- Several authors have described
mm Hg. Seven of the 12 patients sured.2,11,12 Myerson1 suggested mea- techniques for measuring the pres-
with pressures >30 mm Hg devel- suring the central and interosseous sure of the central compartment.
oped ischemic contractures, whereas compartments; however this recom- Myerson and Manoli12 describe a
5 with pressures <30 mm Hg did not mendation was based on the four- method that entails entering the skin
develop contractures. Serial measure- compartment model of the foot. perpendicular to the foot at a point
ments should be performed in pa- More recently, methods for measure- 3.8 cm distal to the tip of the medial
tients with compartment pressures ment of 9 or 10 compartments in the malleolus. No specific depth of pene-
between 20 and 30 mm Hg.5,32 Sys- foot have been described.2,4,33 Ling tration is given. In a second method,
temic hypotension decreases the tol- and Kumar8 suggest that only the in- the entry is made through the skin
erance for increased compartmental termediate and lateral compartments just below the base of the first meta-
pressures, and pressures within 10 to require pressure monitoring; these tarsal, passing above the abductor
30 mm Hg of the diastolic blood are the only compartments that the hallucis to a depth of 1.5 in.1 In a
pressure are an indication for decom- authors recommended decompress- high-resolution MRI study of the
pression.2,12 The calcaneal compart- ing. No evidence currently exists to compartments of the foot, Reach
ment of the foot consistently demon- substantiate a recommendation on et al33 describe specific needle place-
strates the highest pressures; how many compartments’ pressures ment landmarks (Figure 2). When
therefore, this compartment should should be measured because a firm entry to the calcaneal compartment
always be monitored.2,11,12 Commer- understanding of the number of clin- is required, they recommend a needle
cially available digital compartment ically important compartments in the entry point approximately 60 mm
pressure monitors have been used in foot is lacking. The calcaneal (ie, in- distal to the most prominent aspect
some studies.30,32 termediate) compartment has con- of the medial malleolus, inserted to a
Aside from the importance of mea- sistently demonstrated the highest depth of approximately 24 mm.33
suring the pressure of the compart- compartment pressure readings; The authors describe entry points
ment containing the quadratus plan- therefore, it is reasonable to suggest and depths for all 10 foot compart-
tae muscle, no consensus exists on that an attempt should always be ments.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 26
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
Nonspecific findings on physical treated with fasciotomy, Fakhouri
examination contribute to the diffi- Fasciotomy and Manoli30 reported good results.
culty in diagnosing FCS. Compart- Decompression was performed
When acute FCS is diagnosed, emergent
ment pressure monitoring should be through a single medial incision in
decompressive fasciotomy should be
considered standard for establishing six cases, medial and double dorsal
performed to prevent ischemic con-
a diagnosis of FCS. Increasing pain incisions in four, and medial plus
tracture.1,2,4,5,12,13,25,32 In the setting of
and sensory disturbances in a tense, dorsal and lateral incisions in two.
swollen foot should prompt mea- lower limb compartment syndrome, Split-thickness skin grafting was nec-
surement of compartment pressures. the best clinical results are achieved essary in four cases. At an average
when fasciotomy is performed early; follow-up of 21 months, no wound
the potential benefits of this proce- infections or wound complications
Acute Management dure decrease the longer the decom- were reported. No ischemic contrac-
pression is delayed from the time of tures developed; however, eight pa-
Initial management of suspected diagnosis.4 The high complication tients had some discomfort and stiff-
compartment syndrome entails the rate associated with delayed fasciot- ness in the foot.
removal of all restrictive dressings, omy has prompted the suggestion Currently, the three-incision ap-
elevation of the extremity to the level that compartment releases should proach is most commonly used for
of the heart, and prevention of sys- not be done if diagnosis is delayed decompressive fasciotomy in the
temic hypotension as well as serial >8 hours.10,34 However, it is not al- foot2,4,26 (Figure 3). This recommen-
examinations and compartment ways possible to know when the ini- dation is based on the nine-
pressure monitoring.1,13 If diagnosis tial signs and symptoms of compart- compartment model of the foot de-
of FCS is established, urgent decom- ment syndrome arose. scribed by Manoli and Weber.26 A
pressive fasciotomies should be con- In a study of 17 patients with medial incision is made starting 4 cm
sidered. Although most authors ad- intra-articular calcaneal fractures anterior to the posterior aspect of the
vocate the use of acute compartment and 12 with calcaneal compartment heel and 3 cm superior to the plantar
releases,1,2,4,5,12,13,25,32 we believe that pressures documented at >30 mm surface of the foot. This incision is
this management option remains Hg, Mittlmeier et al16 reported poor carried distally for approximately 6
controversial. To date, no studies outcomes in patients with FCS cm. Through this medial approach,
have compared early decompression treated without fasciotomy. Seven of the medial, superficial and deep cen-
versus delayed management of FCS, the 12 patients with pressures >30 tral, and lateral compartments are
and most recommendations in the mm Hg developed symptomatic released (Figure 3). Two dorsal inci-
literature are based on level IV and V plantar contractures, claw toe defor- sions are used, one just medial to the
evidence. Complication rates associ- mity, or both. second metatarsal and one just lat-
ated with each treatment pathway Myerson32 reviewed the results of eral to the fourth metatarsal to en-
are also poorly described in the liter- 14 cases of FCS treated with decom- sure an adequate skin bridge. The
ature, making it difficult to compare pressive fasciotomy. In nine cases, interosseous and adductor compart-
outcomes. the releases were performed through ments are released through these dor-
Early decompression and fasciot- two dorsal incisions; a single medial sal incisions.2,26
omy carries the risk of wound infec- incision was used in five. In three An alternative to the standard
tion and the potential need for soft- cases, wounds were closed acutely dorsal incisions was described by
tissue coverage. Delayed treatment with split-thickness skin excision Dunbar et al.35 They used a “pie-
presumably results in a higher rate of coverage, eight required delayed crusting” technique in which multi-
deformity and the sequelae listed in split-thickness skin grafting, and ple stab incisions are made over the
Table 1. Chronic pain is a common three (all medial) were closed with intermetatarsal spaces followed by
result of high-energy foot trauma delayed primary closure. Only one blunt dissection with a hemostat.
and may or may not be related to is- case required a free tissue transfer. At The goal is to reduce the need for
chemic insult to the peripheral nerves the latest follow-up, four patients skin grafts, which are often required
of the foot. Without high-quality were symptom free and six reported with longer incisions on the dorsum
prospective studies, it is difficult to only occasional discomfort in the of the foot.
determine whether one treatment foot. Only one patient developed a Ling and Kumar8 recommend a
pathway is superior to another; thus, claw toe deformity. plantar-based, single-incision fasciot-
further investigation is necessary. In a review of 12 cases of FCS omy. The incision begins 5 cm distal
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 27
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
Figure 3 son32 reported dorsal skin necrosis in
one patient, and one patient required
a free gracilis tissue flap for cover-
age. The medial-based fasciotomy in-
cision places the medial calcaneal
branch of the posterior tibial nerve
at risk of injury; however, the rate of
injury has not been documented.2
For management of acute FCS, we
recommend the use of the three-
incision approach (one medial inci-
sion, two dorsal incisions), with a
full decompression of all nine com-
partments performed. Currently, the
nine-compartment model of the foot
is the most accepted model described
in the literature.26 The “pie-crusting”
technique described by Dunbar
et al35 may provide similar decom-
pression of the dorsal foot compart-
ments with a decreased need for skin
grafting. Additional studies compar-
ing this approach and other ap-
proaches, such as that described by
Ling and Kumar,8 are needed.
Illustration of the feet demonstrating incision sites for a three-incision
fasciotomy. The blue panel indicates the level of the cross-section shown in Delayed Management
the inset image. Inset, Cross-section of the medial, superficial central, deep
central, and lateral compartments. The superior blue arrow indicates the
entrance into the deep central compartment. The inferior blue arrow indicates The natural history of nonsurgically
the entrance into the medial, superficial, central, and lateral compartments managed FCS includes potential de-
(from medial to lateral). (Courtesy of Herman Johal, MD, Calgary, Alberta, velopment of ischemic contractures,
Canada.)
neuropathy, deformity, and chronic
pain.7,36,37 The goal of management is
to the posterior aspect of the heel on split-thickness skin graft coverage 5 to achieve a functional, plantigrade,
the non–weight-bearing instep and to 7 days after the fasciotomy is per- and pain-free foot.7,10 Lesser toe de-
extends 5 cm distally. The authors formed. The medial incision can of- formities, cavus foot deformity, neu-
felt that this single incision could be ten be closed primarily or with de- ropathic pain, and ulceration sec-
used to decompress the intermediate layed primary closure.2,30,32 ondary to deformity and sensory
and lateral compartments, which Complication rates associated with disturbance are common problems
they believe is sufficient to decom- fasciotomy for FCS have been re- that must be addressed.7,10,36,37
press the foot. Data are lacking to ported to be lower than those for un- Claw toe, the most common defor-
support the use of this approach in a treated FCS.5 Nevertheless, a paucity mity associated with FCS, develops
clinical setting. of data exists in the current literature due to intrinsic muscle weakness and
Stabilization or repair of forefoot with regard to complication rates of extrinsic muscle overpull. Interosse-
and midfoot fractures at the time of both acute fasciotomy and untreated ous muscle injury, denervation, and
decompression is recommended to FCS. In their study of 12 cases of ischemic contracture of the quadra-
reduce further soft-tissue trauma. FCS treated with fasciotomy, Fak- tus plantae muscle, which inserts
Definitive management of calcaneal houri and Manoli30 documented no onto the flexor digitorum longus ten-
fractures should be delayed until infections and no wound complica- don, result in hyperextension of the
soft-tissue swelling has receded.2,12,30 tions. In his series of 14 feet with metatarsophalangeal (MTP) joints
Dorsal incisions commonly require FCS treated with fasciotomy, Myer- and flexion of the interphalangeal
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 28
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
joints. Less commonly, hammer toe locity studies can help distinguish be- Amputation can serve as a salvage
can develop in the setting of ischemic tween ongoing nerve compression option in cases of severe deformity,
contracture in the interosseous and and static ischemic nerve injury. In pain, and ulceration. Poor vascular
lumbrical muscles.36,37 Cavus defor- cases of nerve compression, neuroly- supply may also play a role in the
mity is also common, occurring as a sis of the tibial nerve and its distal choice of amputation over recon-
result of fibrosis and contracture of branches may be helpful.36,37 struction.10,36,37 We do not consider
the plantar intrinsic muscles and soft Management of claw toe deformity amputation a failure of treatment.
tissues.10,36,37 Additional sequelae in- is based on whether the deformity is For a functionless, insensate foot
clude neuropathic changes, neuro- flexible or rigid. Flexible deformities with the sequelae of ulceration and
pathic pain due to ischemic nerve in- are passively correctable at the inter- infection, amputation is an effective
jury, nerve compression symptoms phalangeal and MTP joints, whereas management option.
from fibrosis and contracture, and rigid deformities are not. Flexible de-
insensate areas of the foot with sub- formities can often be managed with
sequent ulcerations.7,36,37 flexor tenotomies and extensor ten- Summary
don lengthening. Flexor-to-extensor
tendon transfer (Girdlestone-Taylor FCS is an uncommon diagnosis, ac-
Management of Sequelae procedure) also can be used, al- counting for <5% of limb compart-
Associated With FCS though we infrequently perform this ment syndromes.4 A high index of sus-
procedure. In cases of rigid defor- picion for FCS must be maintained in
Nonsurgical mity, which are far more common the setting of a high-energy injury to
Nonsurgical management of complica- than flexible deformities, arthrodesis the foot (eg, severe crush injury). Phys-
tions associated with FCS is most likely is recommended.7,10,36-38 We recom- ical examination findings may be un-
to be successful in patients with mild, mend proximal interphalangeal ar- reliable for diagnosis; therefore, com-
flexible deformities with no neuropa- throdesis with MTP arthrotomy or partment pressure monitoring is
thy or static neuropathic symp- even a metatarsal shortening osteot- essential. Controversy exists regarding
toms.36,37 Toe deformities and cavus omy, if necessary. This is often sup- acute versus delayed management of
foot deformity may initially be man- plemented by extensor tendon FCS, and further research on the out-
aged with passive mobilization and lengthening and flexor tenotomies. comes of acute fasciotomy versus de-
stretching. Shoe wear modification (eg, Initially, cavus deformity associ- layed management is necessary. Acute
deep toe box) is also recommended. ated with FCS should be managed management, if chosen, typically con-
Custom orthotics may be beneficial for with soft-tissue procedures (eg, plan- sists of emergent decompressive fas-
management of cavus foot deformity. tar fascia release, long flexor tendon ciotomies using a three-incision tech-
In insensate areas of the foot, appropri- lengthening or release, scar tissue ex- nique. Reconstruction options include
ate skin care to avoid pressure ulcers is cision) followed by osteotomies or deformity correction, nerve decompres-
also important.7,36,37 selective arthrodesis, if necessary. In sion, and, in severe cases, amputation.
cases of cavus and concomitant claw Further research is also needed to de-
Surgical toe deformity, extensor digitorum termine the optimal decompression
longus tendon transfer to the meta- technique to avoid chronic FCS, which
In patients with more advanced de-
tarsal necks addresses both deformi- can result in deformity, dysfunction,
formity, progressive neuropathic
ties. If the correction is inadequate, a and chronic pain.
symptoms, or failed nonsurgical
treatment, surgical intervention may forefoot or midfoot dorsal closing
be indicated. Soft-tissue procedures, wedge osteotomy or arthrodesis may
Acknowledgments
osteotomies, arthrodesis, and ampu- be considered.36 At our institution,
tation are options that should be we proceed with soft-tissue balanc- The authors would like to thank
considered depending on clinical cir- ing before any bony procedures. If Herman Johal, MD, for the artwork
cumstances. Correction of deformity soft-tissue procedures do not provide he contributed to this publication.
and maintenance of the correction adequate correction, we perform
are the goals of surgical interven- dorsal closing wedge osteotomy
tion.36,37 Progressive neuropathic through the midfoot. In the setting of References
symptoms may indicate ongoing degenerative changes, deformity cor-
nerve compression in contracted fi- rection with midfoot or hindfoot ar- Evidence-based Medicine: Levels of
brotic tissues. Nerve conduction ve- throdesis is most effective. evidence are described in the table of
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 29
Foot & Ankle Andrew Dodd, MD, and Ian Le, MD, FRCSC
contents. In this article, references 3 13. Shereff MJ: Compartment syndromes of calcaneal compartment. Foot Ankle
the foot. Instr Course Lect 1990;39:127- 1990;10(5):267-275.
and 5 are level II studies. References 6, 132.
16, 21, 30, 32, and 34 are level IV 27. Guyton GP, Shearman CM, Saltzman
14. Chambers L, Hame SL, Levine B: Acute CL: The compartments of the foot
studies. References 1, 2, 4, 7, 9-14, exertional medial compartment revisited: Rethinking the validity of
17-20, 29, 31, and 35-38 are level V syndrome of the foot after playing cadaver infusion experiments. J Bone
basketball. Skeletal Radiol 2011;40(7): Joint Surg Br 2001;83(2):245-249.
expert opinion. 931-935.
References printed in bold type are 28. Reach JS Jr, Amrami KK, Felmlee JP,
15. Andermahr J, Helling HJ, Tsironis K,
et al: Anatomic compartments of the
those published within the past 5 Rehm KE, Koebke J: Compartment
foot: A 3-Tesla magnetic resonance
syndrome of the foot. Clin Anat 2001;
years. imaging study. Clin Anat 2007;20(2):
14(3):184-189.
201-208.
1. Myerson M: Diagnosis and treatment of 16. Mittlmeier T, Mächler G, Lob G,
compartment syndrome of the foot. Mutschler W, Bauer G, Vogl T: 29. Stotts AK, Carroll KL, Schafer PG,
Orthopedics 1990;13(7):711-717. Compartment syndrome of the foot after Santora SD, Branigan TD: Medial
intraarticular calcaneal fracture. Clin compartment syndrome of the foot: An
2. Fulkerson E, Razi A, Tejwani N: Review:
Orthop Relat Res 1991;269:241-248. unusual complication of spine surgery.
Acute compartment syndrome of the
Spine (Phila Pa 1976) 2003;28(6):E118-
foot. Foot Ankle Int 2003;24(2):180- 17. Ugalde V, Rosen BS: Ischemic peripheral
187. E120.
neuropathy. Phys Med Rehabil Clin N
3. Thakur NA, McDonnell M, Got CJ, Am 2001;12(2):365-380. 30. Fakhouri AJ, Manoli A II: Acute foot
Arcand N, Spratt KF, DiGiovanni CW: compartment syndromes. J Orthop
18. Gilron I, Watson CP, Cahill CM, Moulin
Injury patterns causing isolated foot Trauma 1992;6(2):223-228.
DE: Neuropathic pain: A practical guide
compartment syndrome. J Bone Joint for the clinician. CMAJ 2006;175(3): 31. Bibbo C, Lin SS, Cunningham FJ: Acute
Surg Am 2012;94(11):1030-1035. 265-275. traumatic compartment syndrome of the
4. Middleton S, Clasper J: Compartment 19. Smith BH, Torrance N: Epidemiology of foot in children. Pediatr Emerg Care
syndrome of the foot: Implications for neuropathic pain and its impact on 2000;16(4):244-248.
military surgeons. J R Army Med Corps quality of life. Curr Pain Headache Rep
2010;156(4):241-244. 32. Myerson MS: Management of
2012;16(3):191-198.
compartment syndromes of the foot.
5. Ojike NI, Roberts CS, Giannoudis PV: 20. Baron R, Binder A, Wasner G: Clin Orthop Relat Res 1991;271:239-
Foot compartment syndrome: A Neuropathic pain: Diagnosis, 248.
systematic review of the literature. Acta pathophysiological mechanisms, and
Orthop Belg 2009;75(5):573-580. treatment. Lancet Neurol 2010;9(8):807- 33. Reach JS Jr, Amrami KK, Felmlee JP,
819. Stanley DW, Alcorn JM, Turner NS: The
6. Lintz F, Colombier JA, Letenneur J, compartments of the foot: A 3-tesla
Gouin F: Management of long-term 21. Frink M, Klaus AK, Kuther G, et al: magnetic resonance imaging study with
sequelae of compartment syndrome Long term results of compartment clinical correlates for needle pressure
involving the foot and ankle. Foot Ankle syndrome of the lower limb in testing. Foot Ankle Int 2007;28(5):584-
Int 2009;30(9):847-853. polytraumatised patients. Injury 2007; 594.
7. Brey JM, Castro MD: Salvage of 38(5):607-613.
compartment syndrome of the leg and 34. Finkelstein JA, Hunter GA, Hu RW:
22. Grodinsky M: A study of the fascial Lower limb compartment syndrome:
foot. Foot Ankle Clin 2008;13(4):767- spaces of the foot and their bearing on
772. Course after delayed fasciotomy.
infection. Surg Gynecol Obstet 1929;49: J Trauma 1996;40(3):342-344.
8. Ling ZX, Kumar VP: The myofascial 739-751.
compartments of the foot: A cadaver 35. Dunbar RP, Taitsman LA, Sangeorzan
23. Wood Jones F: Structure and Function as BJ, Hansen ST Jr: Technique tip: Use of
study. J Bone Joint Surg Br 2008;90(8): Seen in the Foot. London, United
1114-1118. “pie crusting” of the dorsal skin in
Kingdom, Bailliere, Tindall, and Cox, severe foot injury. Foot Ankle Int 2007;
9. Maurel B, Brilhault J, Martinez R, 1946. 28(7):851-853.
Lermusiaux P: Compartment syndrome 24. Kamel R, Sakla FB: Anatomical
with foot ischemia after inversion injury 36. Santi MD, Botte MJ: Volkmann’s
compartments of the sole of the human ischemic contracture of the foot and
of the ankle. J Vasc Surg 2007;46(2): foot. Anat Rec 1961;140:57-60.
369-371. ankle: Evaluation and treatment of
25. Myerson MS: Experimental established deformity. Foot Ankle Int
10. Perry MD, Manoli A II: Reconstruction decompression of the fascial 1995;16(6):368-377.
of the foot after leg or foot compartment compartments of the foot: The basis for
syndrome. Foot Ankle Clin 2006;11(1): 37. Botte MJ, Santi MD, Prestianni CA,
fasciotomy in acute compartment Abrams RA: Ischemic contracture of the
191-201, x. syndromes. Foot Ankle 1988;8(6):308- foot and ankle: Principles of
11. Perry MD, Manoli A II: Foot 314. management and prevention.
compartment syndrome. Orthop Clin 26. Manoli A II, Weber TG: Fasciotomy of Orthopedics 1996;19(3):235-244.
North Am 2001;32(1):103-111. the foot: An anatomical study with 38. Mizel MS, Yodlowski ML: Disorders of
12. Myerson M, Manoli A: Compartment special reference to release of the the lesser metatarsophalangeal joints.
syndromes of the foot after calcaneal J Am Acad Orthop Surg 1995;3(3):166-
fractures. Clin Orthop Relat Res 1993; 173.
290:142-150.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 30
Research Article
Patient and Practice Trends in Total
Ankle Replacement and Tibiotalar
Arthrodesis in the United States
From 2007 to 2013
Abstract
Venus Vakhshori, MD Introduction: Both total ankle replacement (TAR) and tibiotalar
Andrew F. Sabour, BS arthrodesis (TTA) are used in the surgical management of ankle
arthritis. Over the past decade, TAR instrumentation, techniques, and
Ram K. Alluri, MD
implants have improved, making the procedure more reliable and
George F. Hatch III, MD reproducible, thus making TAR more common.
Eric W. Tan, MD Methods: The Nationwide Inpatient Sample database from 2007 to
2013 was used to obtain data on patients elder than 50 years who
underwent either TAR or TTA. Differences in temporal, demographic,
and diagnosis trends between TAR and TTA were analyzed.
Results: Between 2007 and 2013, 15,060 patients underwent TAR
and 35,096 underwent TTA. Patients undergoing TTA had
significantly more comorbidities (2.17 versus 1.55; P , 0.001). The
share of TAR performed increased significantly from 2007 (14%) to
2013 (45%) (P , 0.001). From 2007 to 2013, we found a 12-fold
increase in the odds of having a TAR for patients with posttraumatic
osteoarthritis (P , 0.001), a 4.9-fold increase for those with primary
osteoarthritis, and a 3.1-fold increase for patients with rheumatoid
arthritis (P , 0.001).
Conclusions: Over the past decade, the frequency of TAR has
increased, particularly in patients with posttraumatic arthritis and
osteoarthritis. Surgeons still perform TAR in healthier patients
compared with TTA; however, because surgeons become more
experienced with the technique, patients are undergoing TAR at a
markedly higher rate.
Level of Evidence: Level III: retrospective comparative study
From the Department of Orthopaedic
Surgery, Keck School of Medicine of
the University of Southern California,
Los Angeles, CA.
E nd-stage arthritis of the ankle
joint results in notable pain, dis-
ability, and resultant socioeconomic
the historic treatment of choice.1
However, TTA has a unique set of
complications, including adjacent
Correspondence to Dr. Vakhshori: and medical costs. These patients are joint degeneration with continued
venus.vakhshori@med.usc.edu often initially treated with conserva- pain, disability, activity limitation,
J Am Acad Orthop Surg 2019;27: tive therapies including nonsteroidal and persistent gait alterations.1-5
e77-e84 anti-inflammatory medications, joint In the 1970s, total ankle replace-
DOI: 10.5435/JAAOS-D-17-00526 injections, activity modification, ment (TAR) was introduced. Early
bracing treatment, and physical designs were complicated by severe
Copyright 2018 by the American
Academy of Orthopaedic Surgeons. therapy. When these methods fail, osteolysis, loosening, impingement,
tibiotalar arthrodesis (TTA) has been infection, and soft-tissue breakdown
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 31
Foot & Ankle Venus Vakhshori, MD, et al
and therefore were not readily im- in a number of recent database stud- accepted relative contraindication
plemented in management of ankle ies.12-15 However, these studies have for TAR, because younger, more
arthritis.2,6 More recent implants not specifically evaluated the trends active patients may place excessive
developed in the 1980s and 1990s in TAR compared with TTA with demand on the implants, which may
more closely replicate the ankle’s respect to indications and patient result in premature failure or need
natural anatomy and biomechanics and hospital specific factors. The for revision.2,6
and thereby provide improved func- purpose of this study was to eluci- Subjects were categorized based
tion with decreased wear and loos- date these trends in the use of TAR on the surgical procedure. Hospital
ening.2,6 Advances in technology, compared with TTA in a nationwide variables including bed number, gov-
surgical instrumentation, and implant database. ernment (public) or private (investor-
design, including the introduction of owned or not-for-profit) ownership,
mobile bearing articulations and and location were identified. Bed size
partially conforming surfaces, allow Methods categories are determined by
decreased constraint and prosthesis- Healthcare Cost and Utilization Pro-
bone interface stress, improving re- Data ject and vary based on region of the
sults and reproducibility.6 Using the Nationwide Inpatient country and teaching or nonteaching
Compared with TTA, TAR has Sample (NIS), Healthcare Cost and status. Rural versus urban status is
similar clinical outcomes and compli- Utilization Project, Agency for based on 2000 US Census data.16
cations with some reports describing Healthcare Research and Quality Demographic variables, comorbidities,
an increased risk of revision surgery discharge records, a retrospective patient location, length of stay, median
and others with lower complication review was performed from 2007 to household income, and primary pay-
rates; however, no randomized con- 2013 to identify patients who ment method were assessed for each
trolled trials comparing the two have underwent a TAR or TTA. The NIS group. Specific comorbidities such as
been performed and many studies includes about 20% of the approxi- hypertension, depression, diabetes,
report unequal baseline character- mately 37 million annual discharges diabetes with complications (diabetes
istics.7-11 A systematic review of in the United States and is the largest with ketoacidosis, hyperosmolarity,
intermediate and long-term out- inpatient database in the United coma, renal manifestations, ophthal-
comes by Haddad et al8 reported States.16,17 Using International mic manifestations, neurologic mani-
that 68.5% of patients with TAR Classification of Diseases, 9th edi- festations, or peripheral circulatory
have excellent or good American tion (ICD-9) codes, patients who disorders), obesity (body mass index .
Orthopaedic Foot and Ankle Society underwent a primary procedure of 30), peripheral vascular disorders,
ankle-hindfoot scores, compared TAR (81.56) or ankle arthrodesis and renal failure were also identified.
with 68.0% of patients with TTA. A (81.11) were identified. Revision The frequency of concomitant pro-
recently published meta-analysis by procedures (81.59) and patients who cedures as indicated by ICD-9 pro-
Kim et al9 reports no difference in had both arthroplasty on one cedure codes was determined for
the American Orthopaedic Foot and extremity and TTA on the contra- each group. These variables were
Ankle Society ankle-hindfoot score, lateral extremity were excluded. All compared by surgical procedure over
Short Form-36 physical and mental patients included in the study had a the entire study period.
component scores, visual analog concomitant diagnosis of tibiotalar To determine temporal changes,
scale for pain and patient satisfac- arthritis. Patients who died during the frequency of TAR and TTA was
tion; however, patients with TAR their hospitalization were excluded assessed for each year of the data-
were 81% more likely to have a from our analysis. Patients younger base. The frequency of TAR was
revision surgery. than 50 years were excluded to avoid determined for patients with post-
Nonetheless, the use of TAR is selection bias favoring TTA because traumatic osteoarthritis, primary
rapidly increasing as demonstrated age above 50 years is a commonly osteoarthritis, rheumatoid arthritis,
Dr. Alluri or an immediate family member has stock or stock options held in Axogen, Medtronic, Stryker, and Zimmer Biomet and has
received nonincome support (such as equipment or services), commercially derived honoraria, or other non-research-related funding (such
as paid travel) from Acumed, Arthrex, and Trimed. Dr. Hatch or an immediate family member is a member of a speakers’ bureau or has made
paid presentations on behalf of and serves as a paid consultant to Arthrex. Dr. Tan or an immediate family member is a member of a
speakers’ bureau or has made paid presentations on behalf of Arthrex and serves as a board member, owner, officer, or committee member
of the American Academy of Orthopaedic Surgeons and the American Foot Ankle Society. Neither of the following authors nor any
immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution
related directly or indirectly to the subject of this article: Dr. Vakhshori and Mr. Sabour.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 32
Foot & Ankle Venus Vakhshori, MD, et al
and comorbid diabetes, hyperten- Figure 1
sion, and coronary artery disease for
2007 compared with 2013. Incidence
per capita was calculated using 2010
US Census data for patients elder
than 50 years.
Statistical Analysis
Univariate analysis compared patient
demographics, preoperative co-
morbidities, inpatient variables, and
hospital variables between groups.
The Student t-test compared contin-
uous variables. The Fisher exact test
or chi-square analysis compared
Graph showing annual incidence of total ankle arthroplasty compared with
categorical variables. Preoperative tibiotalar arthrodesis.
comorbidities with P , 0.05 and
prevalence .0.5% were included
in a logistic regression for multivar- 5.68 days) than in those with TAR surgery in patients receiving TAR
iate analysis. A P value ,0.05 was (2.28 6 1.41 days) (P , 0.001). In were implant removal (9.8%), gas-
considered significant. addition, the proportion of patients trocnemius recession (7.7%), and
with Medicare and private insurance subtalar fusion (5.8%), whereas for
receiving TAR (94.5%) was signif- those receiving TTA, the most
Results icantly higher than those receiving common concomitant procedures
TTA (87.4%), whereas the oppo- were implant removal (21.7%), sub-
From 2007 to 2013, an initial cohort site was true for Medicaid patients talar fusion (9.6%), and application
of 50,156 patients elder than 50 years (1.4% for TAR compared with of a tibia and/or fibula external
who underwent either TTA or TAR 5.8% for TTA) (P , 0.001). Sim- fixation device (4.5%) (Table 4).
was identified. TTA was performed ilarly, patients with higher than Analysis of primary diagnosis
in 35,096 patients (69.9%), and TAR median household income were demonstrated that from 2007 to
was performed in 15,060 patients more likely to receive TAR (P , 2013, we noticed a 12.1-fold increase
(30.1%). From 2007 to 2013, the 0.001) (Table 1). Further demo- in the odds of having a TAR in pa-
yearly incidence of TAR per capita graphic and hospital information tients with posttraumatic osteo-
increased 421% from 0.86/100,000 is presented in Tables 1 and 2, arthritis (P , 0.001), a 4.9-fold
to 3.66/100,000, whereas the inci- respectively. increase for those with primary
dence of TTA per capita de- With regard to patient-specific vari- osteoarthritis (P , 0.001), and a
creased 18% from 5.37/100,000 to ables, TAR was performed in healthier 3.1-fold increase for patients with
4.40/100,000 (P , 0.001) (Figure 1). patients who had an average of rheumatoid arthritis (P , 0.001).
As a percentage of total procedures 1.55 comorbidities, compared with Furthermore, patients with combined
performed, TAR increased from patients who underwent TTA who comorbid diagnoses of diabetes,
14% in 2007 to 45% in 2013 had an average of 2.17 comorbidities hypertension, and coronary artery
(P , 0.001). The patients in the (P , 0.001). Patients with alcohol disease were 4.7 times more likely to
TAR group were older (mean age, abuse, anemia, depression, diabetes receive TAR in 2013 compared with
65.5 6 8.68 years) than those in the with or without chronic complica- 2007 (P , 0.001) (Table 5).
TTA group (mean age, 63.7 6 8.95 tions, obesity, peripheral vascular
years) (P , 0.001). No significant disease, psychoses, and renal failure
difference was found in sex between were all more likely to receive TTA Conclusions
the two groups (48.9% female un- compared with TAR in univariate
derwent TTA, 50.0% female under- and multivariate analysis (P , 0.01 Ankle arthritis is a debilitating con-
went TAR; P = 0.32). for each comorbidity) (Table 3). dition that results in pain and
The length of stay was significantly The most common concomitant pro- decreased function. For patients refrac-
longer in patients with TTA (3.43 6 cedures performed at the time of tory to conservative management,
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 33
Foot & Ankle Venus Vakhshori, MD, et al
Table 1
Demographic and Patient-specific Variables in Patients Receiving TTA and TAR
Arthrodesis (TTA), Arthroplasty (TAR),
Demographics N = 35,096 (%) N = 15,060 (%) P Value
Age (mean, yr) 63.7 6 8.95 65.5 6 8.68 ,0.001
Sex (female) 17,100 (48.9) 7,520 (50.0) 0.319
Race ,0.001
White 24,000 (84.6) 11,000 (88.4) —
Black 1,800 (6.3) 373 (3.0) —
Hispanic 1,480 (5.2) 441 (3.6) —
Asian or Pacific Islander 288 (1.0) 149 (1.2) —
Native American 118 (0.4) 63 (0.5) —
Other 699 (2.5) 414 (3.3) —
Primary payment method ,0.001
Medicare 17,500 (50.0) 8,140 (54.2) —
Medicaid 2,020 (5.8) 209 (1.4) —
Private 1,310 (37.4) 6,060 (40.3) —
Self-pay 383 (1.1) 89 (0.4) —
No charge or other 2,011 (5.7) 560 (3.7) —
Median household income ,0.001
0-25th percentile 7,910 (23.0) 2,570 (17.4) —
26-50th percentile 9,460 (27.5) 3,670 (24.9) —
51-75th percentile 8,880 (25.9) 4,010 (27.3) —
70-100th percentile 8,090 (23.6) 4,480 (30.4) —
TAR = total ankle replacement, TTA = tibiotalar arthrodesis
arthrodesis has long been an option Practice patterns have shifted in the The rise in TAR is multifactorial.
for this condition, but leads to last decade toward favoring arthro- Improved instrumentation and im-
noticeably altered gait mechanics plasty. From 1995 to 2004, arthro- plants resulting in improved clinical
and velocity, decreased range of desis was performed nearly 10 times outcomes and increased experience
motion, and resultant osteoarthritis more often than arthroplasty in Cal- with the procedure have contributed
of the adjacent joints. 1,3 Total ifornia.10 Our study demonstrates to this change in practice patterns. In
ankle arthroplasty aims to address a relative increase in the rate of the United States, the availability
the drawbacks of arthrodesis. After arthroplasty compared with arthro- of implant systems was extremely
arthroplasty, patients have im- desis, with arthroplasty accounting limited until just over a decade ago.
proved range of motion with less for 14% of the procedures for ankle Before 2005, the only Food and
load on surrounding joints and arthritis in 2007, to just under 50% Drug Administration-approved ankle
improved gait.2,4-6 Benefits of ar- by 2013. Terrell et al14 found an arthroplasty systems in the United
throplasty in the perioperative pe- increase in total ankle arthroplasty States were the Beuchel-Pappas TAR
riod have been reported and include from 0.63 per 10,000 in 2004 to (Endotec) introduced in the 1980s,
lower blood transfusion rates and 0.99 per 10,000 patients in 2009, a and the Agility Total Ankle System
lower rates of nonhome discharge.18 nearly 40% increase. This trend is (DePuy) prosthesis, approved in
However, arthroplasty is not with- also seen in the Medicare pop- 1992.2,20 The early outcomes of these
out its own limitations. Several ulation, in which the arthroplasty implants, especially the first-generation
studies have found similar patient volume increased over 12-fold from implants, were discouraging. Less
satisfaction and clinical outcomes 1991 to 2010, whereas arthrodesis comprehensive understanding of the
but increased risk of major surgical volume increased by only 36%, with ankle biomechanics, implant constraint
complications and revision surgery nearly 4 times as many US hospitals and bone-implant interface, and lim-
with arthroplasty.7-9,10,11,13,19 performing arthroplasty by 2010.12 ited surgeon experience led to high
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 34
Foot & Ankle Venus Vakhshori, MD, et al
Table 2
Hospital Variables and Length of Stay in Patients Receiving TTA and TAR
Arthrodesis (TTA), Arthroplasty (TAR),
Hospital Variables N = 35,096 (%) N = 15,060 (%) P Value
Length of stay (mean, d) 3.43 6 5.68 2.28 6 1.41 ,0.001
Bed size of the hospital ,0.001
Small 4,920 (14.2) 3,060 (20.4) —
Medium 8,510 (24.5) 3,660 (24.4) —
Large 21,300 (61.3) 8,270 (55.2) —
Ownership of hospital ,0.001
Government (public) 18,580 (72.4) 5,448 (65.9) —
Private (investor-owned or not-for-profit) 7,080 (27.6) 2,822 (34.1) —
Hospital setting ,0.001
Rural 1,760 (6.8) 286 (3.5) —
Urban 23,900 (93.2) 7,980 (96.5) —
TAR = total ankle replacement, TTA = tibiotalar arthrodesis
Table 3
Univariate and Multivariate Analysis of Preoperative Comorbidities in Patients Receiving TTA and TAR
Arthrodesis Arthroplasty Univariate Multivariate
Preoperative (TTA), N = 35,096 (TAR), N = 15,060 P OR (TAR/ P OR (TAR/ P
Comorbidities (%) (%) Value TTA) Value TTA) Value
Total comorbidities 2.17 6 1.69 1.55 6 1.31 ,0.001 — — — —
Alcohol abuse 578 (1.6) 122 (0.8) 0.001 0.49 ,0.001 0.48 ,0.001
Anemia 3,950 (11.3) 778 (5.2) ,0.001 0.43 ,0.001 0.63 ,0.001
Depression 4,760 (13.6) 1,730 (11.5) 0.004 0.83 ,0.001 0.88 ,0.001
Diabetes 6,560 (18.7) 1,810 (12.0) ,0.001 0.59 ,0.001 0.57 ,0.001
(uncomplicated)
Diabetes (with chronic 3,770 (10.7) 144 (1.0) ,0.001 0.08 ,0.001 0.10 ,0.001
complications)
Hypertension 22,600 (64.4) 8,830 (58.6) ,0.001 0.78 ,0.001 1.04 0.022
Hypothyroidism 4,270 (12.2) 2,050 (13.6) 0.043 1.14 ,0.001 1.24 ,0.001
Liver disease 637 (1.8) 197 (1.3) 0.089 0.72 ,0.001 0.91 0.265
Obesity 6,680 (19.0) 1,850 (12.3) ,0.001 0.59 ,0.001 0.71 ,0.001
Peripheral vascular 1,370 (3.9) 252 (1.7) ,0.001 0.42 ,0.001 0.66 ,0.001
disorders
Psychoses 1,040 (3.0) 284 (1.9) 0.001 0.63 ,0.001 0.69 ,0.001
Renal failure 3,110 (8.9) 424 (2.8) ,0.001 0.30 ,0.001 0.59 ,0.001
Rheumatoid arthritis/ 2,070 (5.9) 881 (5.9) 0.963 0.99 ,0.001 0.97 0.471
collagen vascular
disease
OR = odds ratio, TAR = total ankle replacement, TTA = tibiotalar arthrodesis
rates of complications and limited previous implant designs and in- Technology) in 2005, the Salto
functional benefits.21,22 Since 2005, strumentation, have been intro- Talaris Anatomic Ankle (Integra
current-generation ankle replace- duced including the INBONE Total LifeSciences) in 2006, the Scandina-
ments, which have improved on Ankle System (Wright Medical vian TAR (Stryker) in 2009, and the
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 35
Foot & Ankle Venus Vakhshori, MD, et al
Table 4
Number and Frequency of Concomitant Procedures in Patients Receiving TAR and TAA
Arthrodesis (TTA), Arthroplasty (TAR),
Concomitant Procedures N = 35,096 (%) N = 15,060 (%) P Value
Removal of implanted device from bone, tibia, 7,617 (21.7) 1,474 (9.8) ,0.0001
and fibula
Removal of implanted devices from bone, tarsals, 952 (2.7) 335 (2.2) 0.001
and metatarsals
Subtalar fusion 3,370 (9.6) 880 (5.8) ,0.0001
Tarsometatarsal fusion 398 (1.1) 102 (0.7) ,0.0001
Triple arthrodesis 194 (0.6) 129 (0.9) ,0.0001
Arthrodesis of other specified joints 349 (1.0) 220 (1.5) ,0.0001
Tendon transfer or transplantation 381 (1.1) 202 (1.3) 0.016
Gastrocnemius recession 635 (1.8) 1,165 (7.7) ,0.0001
Achilles tendon lengthening 409 (1.2) 166 (1.1) 0.583
Application of external fixator device, tibia, and 1,575 (4.5) 79 (0.5) ,0.0001
fibula
Application of external fixator device, ring system 1,165 (3.3) 21 (0.1) ,0.0001
TAR = total ankle replacement, TTA = tibiotalar arthrodesis
Table 5
Change in Incidence for Patients Receiving TAR From 2007 to 2013 Based on Primary Diagnosis
Diagnosis % TAR (2007) % TAR (2013) Odds Ratio (2013/2007) P Value
Posttraumatic osteoarthritis 9.3 55.5 12.1 ,0.001
Primary osteoarthritis 25.6 62.9 4.9 ,0.001
Rheumatoid arthritis 25.5 51.4 3.1 ,0.001
Comorbid DM 1 HTN 1 CAD 12.6 40.3 4.7 ,0.001
CAD = coronary artery disease, DM = diabetes, HTN = hypertension, TAR = total ankle replacement
Zimmer Trabecular Total Ankle phenomenon may be due to patients In our study, the increase in rate of
(Zimmer Biomet) in 2013.20,23 The with Medicaid living in rural areas arthroplasty is most notable for pa-
improvements in technology, in- with limited access to tertiary centers tients with posttraumatic arthritis
creased reproducibility, and wider that perform arthroplasty or reim- who had a 12-times increase in the
range of options for arthroplasty bursement patterns discouraging the odds of undergoing arthroplasty in
have likely contributed to the recent use of arthroplasty because of cost.24-26 2013 compared with 2007. More
increase in TARs. Interestingly, the proportion of pa- modest increases were seen for
Our data show that in this cohort tients receiving arthroplasty at a arthroplasty in primary osteoarthritis
of patients (age . 50 years), arthro- small hospital is larger than those (4.9-fold increase) and rheumatoid
plasty is more commonly performed receiving arthrodesis at a small hos- arthritis (3.1-fold increase). Patients
in older, white patients in private pital; the opposite is true for large with primary osteoarthritis, post-
hospitals in urban settings compared hospitals. This is potentially due to traumatic arthritis, and rheumatoid
with arthrodesis. This finding is patients receiving arthrodesis being arthritis have all been reported to
consistent with other database studies more medically complex and conse- have good outcomes after total ankle
reporting that patients with Medicare quently being treated at large referral arthroplasty.27-29 This likely reflects
or private insurance are three times centers. Further research is needed to both increasing surgeon experience
more likely to undergo arthroplasty elucidate the reasons behind hospital and comfort with arthroplasty in
than do those with Medicaid.24 This size and treatment choice. varying circumstances in addition to
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 36
Foot & Ankle Venus Vakhshori, MD, et al
improved surgical instrumentation, monly in the outpatient setting, many
techniques, and implants. patients have at least an overnight
References
The data from our cohort suggest hospital stay, with an average
Evidence-based Medicine: Levels of
that arthroplasty was generally reported length of stays of two to
evidence are described in the table of
limited to healthier patients. Patients four nights.18,30-33 The move to-
contents. In this article, references 4,
with medical comorbidities were ward outpatient arthroplasty and
7, 24, and 26 are level II studies.
more likely to undergo arthrodesis arthrodesis is recent, and it is possi-
References 1, 3, 9, 10-12, 15, 18, 27,
than arthroplasty, and patients who ble that by not capturing outpatient
and 29-33 are level III studies. Ref-
received an arthrodesis had a higher procedures, our data are most likely
erences 5, 8, 13, 14, 19, 21, 22, and
number of average comorbidities. In understating the growth of arthro-
28 are level IV studies. References 2,
both univariate and multivariate plasty from 2007 to 2013. In addi-
6, 17, 20, 23, and 25 are level V
analysis, patients with alcohol abuse, tion, outcome data are not provided
report or expert opinion.
anemia, depression, diabetes, obe- in the NIS database, and therefore,
sity, peripheral vascular disease, no follow-up data exist to determine References printed in bold type are
psychoses, or renal failure were all clinical results of either intervention. those published within the past 5
more likely to receive arthrodesis. With respect to concomitant proce- years.
These differences likely reflect sur- dures performed, these are listed
1. Coester LM, Saltzman CL, Leupold J,
geon preference to perform arthro- in the NIS by ICD-9 procedure Pontarelli W: Long-term results following
desis over arthroplasty in medically code, which is less descriptive than ankle arthrodesis for post-traumatic
arthritis. J Bone Joint Surg Am 2001;83-A:
complex patients to potentially de- Current Procedure Terminology 219-228.
crease surgical time and risk of revi- codes. Finally, this database study
2. Bonasia DE, Dettoni F, Femino JE, Phisitkul
sion surgery.7,9 The increased length allows us to draw only correlative P, Germano M, Amendola A: Total ankle
of stay and rate of nonhome discharge associations, and we cannot con- replacement: Why, when and how? Iowa
Orthop J 2010;30:119-130.
in patients with arthrodesis may be clude the reasons behind trends
related to medical comorbidities and in practice patterns. However, this 3. Thomas R, Daniels TR, Parker K: Gait
analysis and functional outcomes following
patient demographics rather than the study does provide valuable infor- ankle arthrodesis for isolated ankle
particular procedure being performed. mation regarding national trends arthritis. J Bone Joint Surg Am 2006;88:
Although patients with more co- regarding the use of arthroplasty 526-535.
morbidities are more likely to receive compared with arthrodesis for ankle 4. Singer S, Klejman S, Pinsker E, Houck J,
Daniels T: Ankle arthroplasty and ankle
an arthrodesis, arthroplasty volume arthritis.
arthrodesis: Gait analysis compared with
is expanding. Furthermore, patients In conclusion, this study demon- normal controls. J Bone Joint Surg Am
with comorbid hypertension, diabe- strates an increased national inci- 2013;95:e191(1-10).
tes, and coronary artery disease had dence of TAR compared with TTA 5. Pedowitz DI, Kane JM, Smith GM, Saffel
seen a 4.7-fold increase in the rate of from 2007 to 2013. Patients who HL, Comer C, Raikin SM: Total ankle
arthroplasty versus ankle arthrodesis: A
arthroplasty in 2013 compared with may have previously not been candi- comparative analysis of arc of movement
2007. This increase is likely the result dates for arthroplasty are now more and functional outcomes. Bone Joint J
2016;98-B:634-640.
of improvements in the implant design likely to undergo the procedure. The
and outcomes and increased surgeon largest changes were seen in patients 6. Easley ME, Vertullo CJ, Urban WC,
Nunley JA: Total ankle arthroplasty. J Am
experience with arthroplasty, allow- with posttraumatic osteoarthritis, Acad Orthop Surg 2002;10:157-167.
ing surgeons to perform arthroplasty primary osteoarthritis, and rheuma-
7. Daniels TR, Younger ASE, Penner M, et al:
on a wider range of patients. toid arthritis. Although arthroplasty Intermediate-term results of total ankle
It is important to recognize the is typically performed in healthier replacement and ankle arthrodesis: A
COFAS multicenter study. J Bone Joint
inherent limitations of this database patients, its use is growing among Surg Am 2014;96:135-142.
study. This is a retrospective obser- patients with increased medical co-
8. Haddad SL, Coetzee JC, Estok R, Fahrbach
vational review of a national data- morbidities. Arthroplasty is more K, Banel D, Nalysnyk L: Intermediate and
base searched by ICD-9 codes and common in patients who are white, long-term outcomes of total ankle
is subject to inaccuracies in coding. with Medicare or private insurance, arthroplasty and ankle arthrodesis: A
systematic review of the literature. J Bone
The NIS database includes only in- and those with higher incomes. Joint Surg Am 2007;89:1899-1905.
patients, so any arthrodesis or ar- Future prospective studies comparing
9. Kim HJ, Suh DH, Yang JH, et al:
throplasty performed in an outpatient TAR and TTA are necessary to Total ankle arthroplasty versus ankle
setting is not captured. Although determine the ideal surgical proce- arthrodesis for the treatment of end-stage
ankle arthritis: A meta-analysis of
ankle arthroplasty and arthrodesis are dure for patients with end-stage ankle comparative studies. Int Orthop 2017;41:
slowly being performed more com- arthritis. 101-109.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 37
Foot & Ankle Venus Vakhshori, MD, et al
10. SooHoo NF, Zingmond DS, Ko CY: complications and hospitalization 27. Pedersen E, Pinsker E, Younger ASE, et al:
Comparison of reoperation rates following outcomes after ankle arthrodesis versus Outcome of total ankle arthroplasty in
ankle arthrodesis and total ankle total ankle arthroplasty from 2002 to 2011. patients with rheumatoid arthritis and
arthroplasty. J Bone Joint Surg Am 2007; Foot Ankle Int 2015;36:360-368. noninflammatory arthritis: A multicenter
89:2143-2149. cohort study comparing clinical outcome
19. Gougoulias N, Khanna A, Maffulli N: How and safety. J Bone Joint Surg Am 2014;96:
11. Henricson A, Fredriksson M, Carlsson Å: successful are current ankle replacements?: 1768-1775.
Total ankle replacement and contralateral A systematic review of the literature. Clin
ankle arthrodesis in 16 patients from the Orthop 2010;468:199-208. 28. van Heiningen J, Vliet Vlieland TPM, van
Swedish Ankle Registry: Self-reported der Heide HJL: The mid-term outcome of
function and satisfaction. Foot Ankle Surg 20. Cracchiolo A, Deorio JK: Design features of total ankle arthroplasty and ankle fusion
2016;22:32-34. current total ankle replacements: Implants in rheumatoid arthritis: A systematic
and instrumentation. J Am Acad Orthop review. BMC Musculoskelet Disord 2013;
12. Pugely AJ, Lu X, Amendola A, Callaghan Surg 2008;16:530-540. 14:306.
JJ, Martin CT, Cram P: Trends in the use of
total ankle replacement and ankle 21. Stauffer RN, Segal NM: Total ankle
29. Bai L-B, Lee K-B, Song EK, Yoon TR, Seon
arthrodesis in the United States Medicare arthroplasty: Four years’ experience. Clin
JK: Total ankle arthroplasty outcome
population. Foot Ankle Int 2014;35: Orthop 1981;160:217-221.
comparison for post-traumatic and primary
207-215. 22. Kitaoka HB, Patzer GL: Clinical results of osteoarthritis. Foot Ankle Int 2010;31:
the Mayo total ankle arthroplasty. J Bone 1048-1056.
13. Seaworth CM, Do HT, Vulcano E, Mani
SB, Lyman SL, Ellis SJ: Epidemiology of Joint Surg Am 1996;78:1658-1664.
30. Mulligan RP, Parekh SG: Safety of
total ankle arthroplasty: Trends in New 23. Chou LB, Coughlin MT, Hansen S, et al: outpatient total ankle arthroplasty vs
York state. Orthopedics 2016;39:170-176. Osteoarthritis of the ankle: The role of traditional inpatient admission or overnight
arthroplasty. J Am Acad Orthop Surg observation. Foot Ankle Int 2017;38:
14. Terrell RD, Montgomery SR, Pannell WC,
2008;16:249-259. 825-831.
et al: Comparison of practice patterns in
total ankle replacement and ankle fusion in 24. Heckmann N, Bradley A, Sivasundaram L, 31. Basques BA, Bitterman A, Campbell KJ,
the United States. Foot Ankle Int 2013;34: Alluri RK, Tan EW: Effect of insurance on Haughom BD, Lin J, Lee S: Influence of
1486-1492. rates of total ankle arthroplasty versus surgeon volume on inpatient complications,
arthrodesis for tibiotalar osteoarthritis. cost, and length of stay following total
15. Stavrakis AI, SooHoo NF: Trends in
Foot Ankle Int 2017;38:133-139. ankle arthroplasty. Foot Ankle Int 2016;37:
complication rates following ankle
1046-1051.
arthrodesis and total ankle replacement. J 25. Patterson BM, Draeger RW, Olsson EC,
Bone Joint Surg Am 2016;98:1453-1458. Spang JT, Lin F-C, Kamath GV: A regional 32. Gonzalez T, Fisk E, Chiodo C, Smith J,
16. HCUP National Inpatient Sample (NIS): assessment of medicaid access to outpatient Bluman EM: Economic analysis and patient
Healthcare Cost and Utilization Project orthopaedic care: The influence of satisfaction associated with outpatient total
(HCUP). Rockville, MD, Agency for population density and proximity to ankle arthroplasty. Foot Ankle Int 2017;38:
Healthcare Research and Quality, 2012. academic medical centers on patient access. 507-513.
J Bone Joint Surg Am 2014;96:e156.
17. Alluri RK, Leland H, Heckmann N: 33. Best MJ, Buller LT, Miranda A: National
Surgical research using national databases. 26. Kim C-Y, Wiznia DH, Roth AS, Walls RJ, trends in foot and ankle arthrodesis: 17-
Ann Transl Med 2016;4:393. Pelker RR: Survey of patient insurance year analysis of the National Survey of
status on access to specialty foot and ankle Ambulatory Surgery and National Hospital
18. Jiang JJ, Schipper ON, Whyte N, Koh JL, care under the Affordable Care Act. Foot Discharge Survey. J Foot Ankle Surg 2015;
Toolan BC: Comparison of perioperative Ankle Int 2016;37:776-781. 54:1037-1041.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 38
Review Article
Ankle Distraction Arthroplasty:
Indications, Technique, and
Outcomes
Abstract
Mitchell Bernstein, MD, FRCSC Ankle distraction is an alternative to ankle arthrodesis or total ankle
Jay Reidler, MD, MPH arthroplasty in younger patients with arthritis. Ankle distraction
involves the use of external fixation to mechanically unload the ankle
Austin Fragomen, MD
joint, which allows for stable, congruent range of motion in the setting
S. Robert Rozbruch, MD of decreased mechanical loading, potentially promoting cartilage
repair. Adjunct surgical procedures are frequently done to address
lower-extremity malalignment, ankle equinus contractures, and
impinging tibiotalar osteophytes. Patients can bear full weight during
the treatment course. The distraction frame frequently uses a hinge,
and patients are encouraged to do daily range-of-motion exercises.
Although the initial goal of the procedure is to delay arthrodesis, many
patients achieve lasting clinical benefits, obviating the need for total
ankle arthroplasty or fusion. Complications associated with external
fixation are common, and patients should be counseled that clinical
improvements occur slowly and often are not achieved until at least 1
year after frame removal.
A nkle osteoarthritis is generally
a progressive condition, most
commonly the result of high-energy
ambulation do occur.5 Unlike fusion,
TAA does not affect range of motion
(ROM); however, its use in young
tibial plafond fractures, bimalleolar active patients may be contra-
ankle fractures, recurrent ankle insta- indicated because of wear, failure,
bility, and neuropathy.1-3 Lower- and subsequent revisions.6
extremity posttraumatic arthritis has In contrast to the aims of TAA and
an estimated cost of $12 billion ankle fusion, the aim of distraction
From the Department of Orthopaedic annually in the United States.4 It is arthroplasty is to optimize the body’s
Surgery, Loyola University Chicago
Stritch School of Medicine, Chicago,
often disabling, predominantly regenerative capacity and the func-
IL (Dr. Bernstein), the Department of affects young, active persons, and has tion of the diseased joint.7,8 An
Orthopaedics, Johns Hopkins a negative effect on quality-of-life external fixator is used to mechan-
University, Baltimore, MD measures that is comparable to that ically unload the ankle to relieve
(Dr. Reidler), and the Department of
Orthopaedic Surgery, Hospital for
of hip and knee arthritis.1 The pain, preserve ROM, and potentially
Special Surgery, Cornell University, mainstay of surgical treatment of delay or even partially reverse the
New York, NY (Dr. Fragomen and advanced ankle arthritis has tradi- effects of arthritis (Figure 1). The
Dr. Rozbruch). tionally included ankle arthrodesis or surgeon should be aware of this
J Am Acad Orthop Surg 2017;25: total ankle arthroplasty (TAA). treatment option, as well as its
89-99 Ankle arthrodesis reliably provides indications, outcomes, and potential
DOI: 10.5435/JAAOS-D-14-00077 pain relief. However, loss of ankle adverse effects for ankle arthritis.
motion, increased stress at adjacent Recent short- and intermediate-term
Copyright 2016 by the American
Academy of Orthopaedic Surgeons. joints that leads to degeneration, and evidence suggests that distraction
increased energy expenditure with arthroplasty may be a viable surgical
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 39
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
Figure 1 ability to withstand up to 5.5 times with a circular fixator.18,19 The
body weight during ambulation concept of the hinge is based on the
depends on a stable relationship theory that the talar dome is a frus-
among the bony and ligamentous tum of a cone with its apex medially
structures of the distal tibia, fibula, directed.
and talus.11 The tibial plafond has a Articular cartilage, or hyaline car-
central ridge oriented in the sagittal tilage, lacks blood supply, nerve
plane that is complementary to a innervation, and lymphatic drainage.
concavity on the talar dome. The It receives nutrition and expels waste
relationship between the distal fib- via diffusion and imbibition. Its high
ula, tibiotalar joint, and the medial tensile strength and elasticity func-
malleolus is maintained by the stout tion to withstand high loads, protect
ligaments that make up the ankle subchondral bone, and decrease
syndesmosis. friction between the two opposing
Ankle distraction frame mounted on One study demonstrated that even surfaces. Hyaline cartilage is primar-
an extremity model demonstrating our a 1-mm displacement of the talus in ily composed of type II collagen,
current assembly method. The red the ankle mortise generates a 42% water, and chondrocytes. Chon-
(circular) and blue (U-shaped) rings
are secured with 6-mm decrease in available joint contact drocytes, which produce enzymes,
hydroxyapatite-coated half pins and area.12 Consequently, the remaining proteins, and collagen, are responsi-
1.8-mm bayonet Kirschner wires to cartilage is exposed to compressive ble for the normal and pathologic
the tibia and foot, respectively. The forces over a smaller surface area, state of the articular surface.20,21
hinge (red arrow) is aligned with the
Inman axis. The acute and gradual potentially leading to degeneration Chondrocytes are metabolically
distraction is achieved with clockwise and arthritis. controlled via the surrounding
rotations of the square nuts (red The orientation of the ankle joint, mechanical environment and thus,
arrowhead), which are attached to the as described by a line perpendicular can upregulate the synthesis of deg-
tibial ring. Range-of-motion exercises
occur with unlocking the connection to the diaphysis of the tibia, is in slight radative cytokines, increasing cata-
between the two rings (yellow arrow). valgus. Named the lateral distal tibial bolic enzymes in the local milieu—a
Gradual dorsiflexion of the ankle, in angle, it measures on average 89° concept referred to as mechanoelec-
the setting of chronic ankle equinus, is (range, 86º to 92°). The axis of the trochemical events.22
achieved by gradually increasing the
distance between the square nut ankle joint is created through the Arthritis in the ankle is most often
(yellow arrow) and the proximal end of relationship between, and the geo- secondary, usually resulting from
the rod. (Copyright Mitchell Bernstein, metric constraints of, the talar dome, trauma.2,3 The energy dissipated
MD, FRCSC, Chicago, IL.) tibial plafond, and the lateral and through the articular surface and the
medial malleoli.13 The traditionally ensuing inflammatory response is
option with the use of appropriate accepted theory, proposed in the thought to be critical in post-
patient selection criteria.9,10 1950s, suggests that the ankle rotates traumatic arthritis.23,24 It has been
with one-degree of freedom about an demonstrated that the inflammation
axis (ie, the Inman axis) that lies resulting from the energy loss causes
Anatomy and between the tips of the medial and the production of dysfunctional
Biomechanics of the Ankle lateral malleoli.14-16 This axis is the cellular elements and chondrocyte
Joint basis for total ankle prosthesis apoptosis.25 In the subacute phase,
designs17 and forms the basis on articular cartilage changes its com-
The ankle is a highly constrained and which the hinge is built when dis- position, increasing its water con-
congruent weight-bearing joint. Its traction arthroplasty is performed tent and decreasing its proteoglycan
Dr. Bernstein or an immediate family member serves as a paid consultant to NuVasive, Smith & Nephew, and DuPuy Synthes and serves as
a board member, owner, officer, or committee member of the Limb Lengthening Reconstruction Society. Dr. Fragomen or an immediate
family member has received royalties from Small Bone Innovations; is a member of a speakers’ bureau, or has made paid presentations on
behalf of Smith & Nephew; and serves as a paid consultant to Smith & Nephew and DePuy Synthes. Dr. Rozbruch or an immediate family
member has received royalties from Small Bone Innovations and Smith & Nephew; is a member of a speakers’ bureau, or has made paid
presentations on behalf of Smith & Nephew; serves as a paid consultant to Small Bone Innovations and Smith & Nephew; and serves as a
board member, owner, officer, or committee member of the Limb Lengthening Reconstruction Society. Neither Dr. Reidler nor any
immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution
related directly or indirectly to the subject of this article.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 40
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
concentration. Furthermore, type II and has recalcitrant pain in the setting distraction, the etiology of ankle
collagen is weakened by a combina- of a congruent joint with preserved arthritis is critical. A history of injury
tion of decreased production by motion of .20°.33 Relative contra- or repetitive instability is therefore
chondrocytes and increased concen- indications include complex regional carefully elucidated.
tration of proinflammatory cytokines. pain syndrome, inflammatory ar- The physical examination begins
To restore normal homeostasis, thritides, previous infection, neuro- with an assessment to identify any
deeper layers containing “resting” pathic joint, and older age with low ipsilateral (or contralateral) extrem-
chondrocytes proliferate to increase functional demands. Patients with a ity malalignment, such as tibial mal-
anabolic activities. The exact cellu- painful stiff ankle (ie, ,20° of union, knee hyperextension, or tibia
lar mechanisms, signaling mole- motion) are less likely to do well with vara. The patient is screened for limb
cules, genetic factors, and the role of distraction because the procedure length inequality by comparing the
mechanical influences currently are does not reliably increase ROM, and heights of the iliac crests. Dynamic
not fully understood. thus, these patients may be better extremity instability, malalignment,
As the catabolic processes over- candidates for arthrodesis or TAA.10 and foot progression angle are
whelm resident chondrocytes, “full- Extra-articular deformity, located determined by observing the patient
thickness” chondral involvement in the hindfoot or distal tibia, is not a ambulate. A focused assessment of
ensues, exposing subchondral bone. contraindication if the deformity is the ankle and foot, including stability
Healing is possible, albeit unpre- addressed concurrently.34 Patients and ROM testing, completes the
dictably. This spontaneous healing with marked intra-articular defor- physical examination.
occurs in part because of the release mity or a flat-top talus, however, are No routine laboratory tests are
of growth factors from exposed felt to be poor candidates for ankle required. Infectious markers, such as
marrow spaces.26 The resultant local distraction. Asymmetric arthritis of white blood cell count and erythrocyte
inflammatory response recruits plu- the ankle is not a contraindication sedimentation rate and C-reactive
ripotent mesenchymal stem cells, for ankle distraction. For example, protein level, are ordered when active
which, depending on the local envi- patients with varus deformity at the infection is suspected or needs to be
ronment, can be manipulated to distal tibia and asymmetric joint ruled out.
develop fibrocartilage.27-30 This is wear on the medial side may benefit Radiographic evaluation includes
one potential pathway that distrac- from a supramalleolar osteotomy, AP, lateral, and mortise weight-
tion arthroplasty and adjunct pro- with correction of the varus defor- bearing views of the ankle (Figure 2).
cedures may use to exploit the mity and ankle distraction to offload Radiographs of the tibia and/or
formation of hyaline cartilage.31 the diseased segment. Finally, ante- a standing hindfoot alignment
For younger patients with rior joint space narrowing associated (Saltzman) view of the foot are ob-
posttraumatic lesions, a durable, with impinging anterior osteophytes tained in the case of pathology and/or
joint-sparing solution is desirable. should be identified. In these malalignment. CT scans of the ankle
Concurrently addressing all pathol- patients, arthroscopic or open de- are not routinely ordered. MRI is used
ogy, including equinus contracture, ti- compression, possibly in conjunction when osteochondral lesions need to be
biotalar osteophytes, supramalleolar with gastrocnemius recession, delineated or in the case of nonosseous
or hindfoot malalignment, and insta- should be considered. pathology (eg, lateral ankle ligament
bility, is central to treatment. Cartilage The success of ankle distraction is pathology, posterior tibial tendinosis).
regeneration is more reliable when it predicated on a thorough history, The ankle radiographs are also
occurs in the setting of a congruent, physical examination, and ancillary used to measure the weight-bearing
stable limb in anatomic alignment.19,32 tests. Our evaluation includes a review preoperative joint space in prepara-
of patients’ reasons for consultation tion for the required increase of 5 mm
and their perception of their disability during distraction to effectively
Distraction Arthroplasty in addition to the basic elements of a unload the ankle joint.10,35 The
thorough patient history: the location presence of subchondral sclerosis
The success of ankle distraction and quality of the pain, aggravating and subchondral cysts are noted. In
depends on proper patient selection and alleviating factors, subjective addition, the ankle joint should be
and appropriate management of description of instability, previous scrutinized for asymmetric wear.
expectations. The ideal candidate for nonsurgical and surgical treatments, This wear should be correlated to an
ankle distraction arthroplasty is a and other musculoskeletal com- associated deformity. For example, if
motivated patient who seeks an plaints. Because inflammatory arthri- the medial aspect of the ankle joint
alternative to ankle fusion or TAA tides are relative contraindications to demonstrates arthritis with relative
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 41
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
Figure 2
Preoperative AP (A) and lateral (B) standing radiographs of the ankle joint in a 53-year-old woman with posttraumatic arthritis.
Subchondral sclerosis and cysts, as well as decreased joint space are noted. Mild flattening of the talar dome is evident
anteriorly on the lateral radiograph. AP (C) and lateral (D) standing radiographs obtained immediately postoperatively after
distraction arthroplasty and osteophyte excision. Note the 1-inch calibration ball to measure the joint space E, Photograph of
the patient wearing the frame. AP (F) and lateral (G) standing radiographs of the ankle joint demonstrating joint space and
remodeling of the joint at an 18-month follow-up visit. (Copyright Mitchell Bernstein, MD, FRCSC, Chicago, IL.)
preservation of the lateral joint and Judet36 described a technique using those of normal hyaline cartilage.36
the patient has a posttraumatic varus external fixation to mechanically Aldegheri et al37 reported on the
deformity with an apex at the distal separate opposing joint surfaces to use of a hinged distractor for hip
tibial metaphysis, joint distraction in allow “for fibrous tissue between arthritis in 80 patients. Based on
addition to a supramalleolar osteot- the bone ends.” Their histologic good results achieved in 46 patients
omy may be indicated. analysis of regenerated tissue in at a minimum follow-up of 5 years,
dogs was done after the tibiotarsal the authors concluded that radio-
joints were devoid of articular graphic results do not always cor-
History of the Procedure cartilage and distracted for 30 days relate with clinical outcomes.
with a 4- to 8-mm gap. At 1 year, Patients aged .45 years with or
In 1978, seeking alternatives to they reported metaplastic changes without inflammatory arthritis had
TAA for joint arthritis, Judet and in the joint surface resembling uniformly poor results.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 42
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
increase in protoeglycan synthesis, were better (P , 0.004) than those
Mechanism of Action recruitment of mesenchymal stems obtained at 1-year follow-up.
cells, and optimization of the Although poorly understood, sev-
The exact mechanism of action for
mechanical environment.22,31,45 Fur- eral studies support the process of
distraction arthroplasty is unknown;
thermore, an improvement is seen in ankle joint remodeling after frame
however, it is based on the belief that
the density of the subchondral bone removal.10,40,46,47 The restoration
the biologic aspects of cartilage
with a decrease in sclerosis.40 This of preinjury ankle architecture and
regeneration are most likely to occur
subchondral change may improve the mechanics is thought to be instru-
in a mechanically unloaded, well-
biomechanical environment of the mental for prolonged benefit. The
aligned limb.38,39 The stiffness of
arthritic joint. In addition, resorption notion that improvements may
the circular ring fixator may allow
of subchondral cysts and improve- occur over 12 to 24 months sub-
for sufficient stress shielding at the
ment in edema may contribute to the sequent to frame removal should
ankle joint to allow subchondral
clinical improvement that we have be considered when counseling
bone remodeling, which has been
observed. patients in their recovery period.
shown to be of clinical benefit.40
In 2008, Paley et al48 published
However, this phenomenon, and its
their results on a modified distraction
clinical correlation to pain relief, is
Outcomes frame that was being used in Europe.
still controversial.
Motion during distraction was
In addition, weight bearing, sta-
In 1995, van Valburg et al44 pub- stressed, and an anatomically located
bility, and motion—crucial for pro- lished a preliminary retrospective hinge based on the Inman axis
moting durable articular cartilage— study on the use of ankle distraction became the foundation of the frame.
are possible for an extended period in 11 patients with severe post- Adjunctive procedures, such as os-
in the external fixator.41-43 traumatic arthritis scheduled for teophyte resection, gastrocnemius-
43
van Valburg et al measured intra- ankle arthrodesis. The patient soleus complex recession, and
articular hydrostatic pressure dur- cohort was relatively young (mean extremity realignment with osteot-
ing distraction by inserting a age, 35 years). An Ilizarov distrac- omy, were also done to maximize
pressure-sensitive catheter into the tion apparatus was used for a mean clinical outcomes.48 Nine males and
ankle. Recordings demonstrated of 15 weeks. Their technique, which 14 females were available for ret-
intra-articular pressure fluctuations, has since been slightly modified, rospective chart review after a mean
and the authors suggested that these consisted of ensuring a post- 17 weeks with external fixation.
fluctuations combined with the operative distraction gap of 5 mm Preoperative and postoperative
absence of mechanical stress were and the addition of hinges between ankle motion was 28° and 27°,
instrumental in articular cartilage 6 and 12 weeks postoperatively. At respectively. At a mean follow-up of
repair.43-45 They theorized that the a mean follow-up of 20 months 64 months (range, 24 to 157
intermittent fluid flow inside the (range, 10 to 60 months), all months), 77% patients reported
joint caused by pressure fluctuations patients reported a decrease in pain, ambulation for pleasure, and 33%
effectively mimics normal physio- and five patients (45%) reported a reported an ability to run. Radio-
logic processes in the absence of complete resolution of pain.44 Six graphic analysis revealed that the
load and shear and that this pro- patients (55%) had increased ROM, joint space after frame removal did
motes cartilage repair. In a study of and five (50%) had radiographic not remain distracted, although this
knee arthritis (induced by anterior evidence of increased tibiotalar joint did not affect clinical results. The
cruciate ligament resection) in a space. Encouraged by their results, authors claimed that the purpose
canine model, van Valburg et al31 the authors published a prospective of articular cartilage repair was
observed that, in addition to the study with a minimum 2-year to “seal cartilage cracks and
intermittent fluid flow caused by follow-up.46 The study included 17 defects,”48 which was supported by
an articulated knee hinge on the patients (mean age, 39.6 years) who an MRI study of three patients who
Ilizarov device, a change occurred in underwent annual evaluations for were treated with ankle distrac-
the proteoglycan metabolism that functional ability, mobility, and tion.49 Of note, 33% were not sat-
resembled the nonarthritic control pain scores. Ankle distraction failed isfied with the outcome of the
knee. in four patients, who ultimately procedure. Treatment failed in two
Factors that have been associated proceeded with arthrodesis. Of the patients (11%); one patient under-
with cartilage repair include a decrease remaining 13 patients, clinical out- went ankle fusion and another
in joint reactive forces (shear), an come scores at 2-year follow-up underwent TAA.48
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 43
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
Table 1
Summary of Outcomes and Adverse Events From Studies on Distraction Arthroplasty
No. of
Study Patients Follow-upa Agea (yr) Outcomes Adverse Events
Marijnissen 111 2 yr minimum 42.7 6 9.8 Pain and disability scores 48 patients (44%) had
et al9 decreased from 67% and subsequent arthrodesis
68% to 38% and 36%,
respectively, at 2 yr
Tellisi et al10 23 30.5 mo 43 (16–73) Decrease in pain in 91% of Pin-site infection in all patients; 2
(12–60 mo) patients of 23 patients (9%) went on to
arthrodesis
Saltzman 29 2 yr Fixed: 42.4 Better pain improvement in 19 of 29 patients (66%) had
et al32 (18–53) motion group at 2 yr; both recurrent pin-site infections; 2 of
Motion: 42.7 groups better at 2 yr than 29 patients (7%) had
(27–59) baseline osteomyelitis. 8 of 29 patients
(28%) had nerve injury of medial
calcaneal branch of the tibial
nerve and deep peroneal nerve;
1 of 29 patients (3%) had deep
vein thrombosis
Intema et al40 26 2 yr 41 6 9 Decrease in AOS pain and Not reported
disability scores; correlation
with subchondral bone
remodeling and clinical
improvement
Ploegmakers 22 10 yr 37 6 11 Decrease in pain scores from 6 of 22 patients (27%) had
et al47 (7–15 yr) 78% to 30%; increase in arthrodesis; 1 of 22 patients
function scores from 20% to (5%) had complex regional pain
73% syndrome
van Valburg 11 20 wk 35 (20–70) Pain decreased in all patients Not reported
et al44 (10–60 wk) 5 patients pain free
van Valburg 17 2 yr 40 (17–55) Decrease in physical, 4 of 17 patients (24%) had
et al46 functional, and pain disability arthrodesis; 4 of 17 patients (24%)
scores at 2 yrs (P , 0.003) had broken Kirschner wires
Paley et al48 23 64 mo (24– 45 (17–62) 71% of patients ambulating for 17 of 23 patients (74%) had pin-
157 mo) pleasure; 33% can run, 22% site infection; 1 of 23 patients
using assistive devices; 11% (4%) had arthrodesis; 1 of 23
with severe limitations patients (4%) had total ankle
arthroplasty; 10 of 23 patients
(43%) returned to operating
room for unplanned procedure
Nguyen 36 8.3 yr (6.1– Fixed: 42.4 AOS score ,43; age at time of 16 of 36 patients (45%) failed
et al50 10.5 yr) (18–53) distraction, and fixed versus treatment; 8 of 16 patients (50%)
Motion: 42.7 motion ankle distraction had ankle fusion, 5 of 16 patients
(27–59) predictive of failure at 2 yr (31%) had total ankle
postoperatively arthroplasty
Marijnissen 57 2.8 yr (2.5– 44 (18–65) Decrease in pain scores by 38% 16 of 57 patients (28%) had pin-
et al51 3.1 yr) (P , 0.0001); 69% increase in site infections; 8 of 57 patients
function (P , 0.0001); increase (14%) had broken Kirschner
in clinical condition by 120% wires
(P , 0.0001)
AOS = Ankle Osteoarthritis Scale
a
The values are given as the mean with the range in parentheses.
Copyright Mitchell Bernstein, MD, FRCSC, Chicago, IL.
A hinge allows for ROM during addition, while hinge distraction in ation, histologic proof of hyaline
rehabilitation, but ROM will not likely animals supports robust and dura- cartilage regeneration in humans
increase after frame removal.10,32 In ble articular-like cartilage regener- is lacking.8,31 In a prospective
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 44
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
randomized controlled trial, pain.46 Similar rates of failure were approach, respectively. An arthrot-
Saltzman et al32 compared 36 reported by Marijnissen et al51 and omy is used to remove impinging
patients who underwent distraction Ploegmakers et al47 (24% and 27%, anterior osteophytes. A supra-
arthroplasty with or without a respectively), who reported that malleolar osteotomy is added to
hinge. Two years after frame clinical recurrence of pain 1 year correct concomitant coronal or sag-
removal, clinical scores were better after frame removal was the reason ittal malalignment.19,34 This pro-
in the hinge group, although ankle for ankle arthrodesis.51 Marijnissen cedure requires placement of an
motion was similar in both groups. et al9 recently updated their clinical additional circular ring at the
However, in a subsequent report on results with data from a 12-year proximal tibia, with the distraction
the same cohort with longer follow- follow-up, noting a 44% rate of tibial ring closer to the ankle joint
up, the authors reported that conversion to ankle arthrodesis. In (Figure 3). The supramalleolar os-
patients without a hinge had the same study, Cox regression teotomy begins with the patient in a
improved outcomes.50 The authors analysis revealed that female sex was supine position on a radiolucent
could only speculate on the reason predictive of failure, whereas pre- table. A bump is placed under the
for the contradictory results, and operative ankle motion permitting ipsilateral buttock to ensure the limb
further research on the benefit of a distraction was protective.9 Nguyen is in neutral rotation (ie, patella
hinge is necessary. In a retrospec- et al50 reported on their cohort of 36 facing upward).
tive study of 23 patients with patients who underwent ankle dis- In addition to mechanical distrac-
hinged distraction arthroplasty, traction for end-stage osteoarthritis. tion, we prefer to inject bone marrow
Tellisi et al10 reported that all At a mean follow-up of 8.3 years, 29 autograft concentrate (BMAC) from
patients in the hinge group had patients (81%) were available for the ipsilateral iliac crest as described
severe posttraumatic arthritis and follow-up. Treatment failed in 13 by Hernigou et al.52 An aspirate of
were being considered for ankle patients (45%), requiring either 60 mL of marrow yields approxi-
arthrodesis. At a mean follow-up of ankle fusion or TAA. The authors mately 7 mL of BMAC. This aspirate
30.5 months (range, 12 to 60 months), reported that age, Ankle Osteoar- contains pluripotent stem cells,
no patient demonstrated a change in thritis Scale score, and the presence which are injected into the ankle
ankle motion. At the latest follow-up, of a hinge to allow ankle ROM were joint. We inject this percutaneously
21 of 23 patients (91%) reported predictors of failure at 2 years.50 at the end of the case, after the acute
improved pain, and 17 patients (74%) Finally, it is important to note distraction has been performed. We
had notable improvement in Ameri- that published results primarily routinely administer this aspirate as
can Foot and Ankle Society scores. analyze patients with severe ankle part of the ankle distraction pro-
The initial enthusiasm for ankle arthritis who otherwise would be cedure. Although clinical evidence is
distraction focused on the ability to considered candidates for arthrod- lacking, compelling basic science and
delay arthrodesis or TAA. Propo- esis (Table 1). Selection of patients animal studies support the use of
nents of distraction arthroplasty with moderate arthritis could lead BMAC to augment the cartilage
cite several advantages, including to improved long-term outcomes. regeneration.8,29,53-55
the minimally invasive nature of Further research is necessary. The application of the ankle dis-
the procedure, no required internal traction frame begins by choosing a
fixation, and no interference with tibial ring that allows for two finger-
future reconstructive efforts.10 How- Authors’ Preferred Surgical breadths of space circumferentially
ever, studies of ankle arthrodesis and Technique between the skin and the ring. The
TAA after distraction arthroplasty medial malleolus and the anterior
are lacking. The patient’s history and physical and posteromedial border of the
Nevertheless, clinical failures in the examination, as well as the results of distal tibia are marked. The prox-
form of ankle fusion or TAA do occur appropriate imaging studies will imal ring is secured with two 6-mm
following distraction.9,10,46,50 As dictate which, if any, adjunct surgi- hydroxyapatite-coated pins.56,57 The
noted, van Valburg et al46 reported cal treatments are required before first pin is placed approximately 6
on 17 patients with a mean age of the circular frame is mounted to the cm proximal to the medial malleolus
39.6 years who were treated with leg. Ankle equinus contracture with directly anterior in the tibial crest
fixed ankle joint distraction. Four a positive Silfverskiöld test is treated using a 4.8-mm drill bit. The pin is
patients (24%) required ankle fusion with a gastrocnemius Strayer or placed perpendicular to the shaft
within 1 year postoperatively Vulpius recession through a postero- of the tibia and secured to the
because of the recurrence of severe medial or direct posterior surgical ring with a three-hole cube. Before
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 45
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
Figure 3
Preoperative AP (A) and lateral (B) standing radiographs of the ankle joint in a 62-year-old woman who sustained a closed right
distal tibia fracture in a skiing accident. Note the decreased joint space, subchondral sclerosis, cysts, and anterior ankle
osteophytes. Lateral translation, recurvatum, and anterior subluxation of the talus also are evident. Supramalleolar osteotomy was
performed to correct extremity malalignment, and ankle distraction arthroplasty was done in conjunction with arthrotomy, excision
of tibiotalar osteophytes, microfracture of the talar dome and tibial plafond, and gastrocnemius-soleus complex recession. C,
Intraoperative fluoroscopic image demonstrating bone marrow aspirate injection into the ankle joint. D, Clinical photograph of the
lower extremity after frame application. Note the additional ring and struts used to correct supramalleolar malalignment. Lateral (E)
and AP (F) radiographs of the ankle joint at 6 months postoperatively. Reduction of the tibiotalar joint and restoration of coronal
and sagittal alignment have been achieved. Joint space is increased on weight-bearing radiographs. Clinical examination
demonstrated 10° of dorsiflexion and 25° of plantar flexion. (Copyright Mitchell Bernstein, MD, FRCSC, Chicago, IL.)
final tightening, intraoperative fluo- the axis of the tibial shaft. Universal of the lateral malleolus and exiting at
roscopy is used to confirm that the hinges are then applied in line with a the tip of the medial malleolus, in a
ring is positioned perpendicular to Kirschner wire, inserted from the tip posterolateral-to-anteromedial
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 46
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
direction18 (Figure 4). This approx- the use of the frame in distraction for Figure 4
imates the Inman axis. A footplate is at least 8 weeks, and no added
secured 1 inch proximal and parallel benefit has been seen beyond 12
to the plantar aspect of the foot. A weeks.8,31 We prefer to use the frame
locking rod connects the footplate to for 12 weeks.
the proximal adjustable ring, which In addition to distraction, the
allows for gradual dorsiflexion to senior authors (A.T.F., S.R.R.) cur-
correct equinus contractures. The rently inject autologous bone mar-
ring is unlocked four times daily row aspirate into the ankle joint and
for ROM exercises (15 repetitions/ routinely affect microfracture.
session). Typically, the ankle is Although the mechanism of action
acutely distracted 3 mm in the of hyaline cartilage regeneration
operating room by turning the remains elusive, and clinical data
square nuts on the proximal ring. are lacking, we feel that these
Acute distraction beyond that is adjunctive procedures may opti-
discouraged to avoid neurologic mize the local healing environment.
traction injury; acute correction of
equinus contracture is avoided for
the same reason. Once normal post- Complications
operative plantar sensation is con-
firmed, an additional 2 mm of The most common complication
distraction is usually done on post- associated with ankle distraction ar- AP fluoroscopic image of the ankle
operative day 1 and another 1 mm on throplasty is a superficial pin-site demonstrating insertion of a
postoperative day 2. At the 2-week infection, which typically resolves Kirschner wire to approximate the
clinic visit, another 1 to 2 mm of dis- with a course of oral antibiotics. The Inman axis during application of an
ankle distraction frame. The wire is
traction is done. Fluoroscopy is used to reported incidence ranges from 14% inserted from the tip of the lateral
confirm that a congruent distraction to 100%.10,32,48,50,51,58 Osteomyeli- malleolus aiming toward the distal
gap exists on the AP and lateral views. tis that requires hospital admission aspect of the medial malleolus in a
Postoperatively, the patient is al- and intravenous antibiotics is less posterolateral-to-anteromedial
direction. (Copyright Mitchell
lowed full weight bearing as toler- common, with a reported incidence Bernstein, MD, FRCSC, Chicago, IL.)
ated, with crutches. The neutral of 1.2% to 5.5%.32,48,51 Pin break-
position (ie, ankle dorsiflexion) is age does occur, usually in the mid-
marked on the hinge, and the physical foot because of the motion-induced are educated preoperatively and in
therapist teaches the patient how to cyclic fatigue of the Kirschner wire. the hospital before discharge regard-
unlock the hinge and do active- Likely underreported, the estimated ing the appropriate use of their
assisted ROM exercises with a foot incidence is 14% to 24% in two external fixation device. We recom-
strap. Once patients are comfortable, studies of 74 patients.51,58 Typically, mend daily pin-site care using a
they are encouraged to ambulate with this breakage occurs at the junction solution of 50% normal saline and
the frame’s hinge unlocked. Any of the wire connection onto the ring 50% hydrogen peroxide applied with
residual distraction beyond what and therefore is rectified by modi- sterile cotton-tipped swabs. To pro-
was done in the operating room is fying the connection of the wire- tect the soft tissues, each group of
undertaken by the physician in the fixation bolt closer to the skin. pins should be wrapped with 2-inch
hospital or 2 weeks later at the first Complications are best avoided cotton gauze.
clinical visit. We typically do not with stringent and consistent patient A thorough knowledge of cross-
distract .3 mm acutely. Based on a selection, meticulous surgical tech- sectional anatomy in the lower
recent biomechanical study, a rela- nique, and close clinical follow-up. extremity is required to avoid inad-
tive increase of 5 mm of joint space Patients should be screened at the vertent perforation or incarceration
should be obtained relative to the initial clinical visit for the inability to of neurovascular structures. Specifi-
preoperative standing radiograph to comply with postoperative regimens. cally, when placing the tibial ring,
ensure that the articular surfaces of Educational level, ability to take time the tibialis anterior tendon and
the tibial plafond and talar body do off work, living situation, and the anterior neurovascular bundle are at
not come in contact during weight availability of supportive family and/ risk of injury. The surgeon should
bearing.35 Animal models support or friends are determined. Patients have access to new, sharp 4.8-mm
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 47
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
bits to drill pilot holes for the 6-mm composition of the resultant gener- derived mesenchymal cell transplantation. J
Bone Joint Surg Br 2005;87(5):721-729.
half pins in each case. This pre- ated tissue is needed.
caution avoids thermal damage to 9. Marijnissen AC, Hoekstra MC, Pré BC,
et al: Patient characteristics as predictors of
bone, premature loosening, and pin- clinical outcome of distraction in treatment
site infection. The foot ring is applied References of severe ankle osteoarthritis. J Orthop Res
2014;32(1):96-101.
with care taken to avoid the medial
Evidence-based Medicine: Levels of
neurovascular structures. However, 10. Tellisi N, Fragomen AT, Kleinman D,
evidence are described in the table of O’Malley MJ, Rozbruch SR: Joint
in our experience, patients report preservation of the osteoarthritic ankle
contents. In this article, references 1,
heel numbness, which can be attrib- using distraction arthroplasty. Foot Ankle
9, 32, and 57 are level I studies. Int 2009;30(4):318-325.
uted to medial calcaneal branch
Reference 51 and 55 are level II
nerve irritation from the crossed 11. Stauffer RN, Chao EY, Brewster RC: Force
studies. References 5, 6, 11, and 33 and motion analysis of the normal,
hindfoot wires. These symptoms diseased, and prosthetic ankle joint. Clin
are level III studies. References 2-4,
should not be mistaken for plantar Orthop Relat Res 1977;127:189-196.
7, 10, 17, 18, 24, 34, 37, 39, 40, 44,
numbness at the forefoot consistent 12. Ringleb SI, Udupa JK, Siegler S, et al: The
46-50, and 53 are level IV studies.
with tibial nerve injury because the effect of ankle ligament damage and
References 15, 19, and 38 are level V surgical reconstructions on the mechanics
former should resolve, whereas the
expert opinion. of the ankle and subtalar joints revealed by
latter requires urgent release of dis- three-dimensional stress MRI. J Orthop Res
traction and possible tarsal tunnel References printed in bold type are 2005;23(4):743-749.
decompression. Posterior tibial those published within the past 5 13. Siegler S, Toy J, Seale D, Pedowitz D: The
nerve neurapraxia often occurs with years. Clinical Biomechanics Award 2013
presented by the International Society of
larger, acute distraction (.5 mm) in 1. Glazebrook M, Daniels T, Younger A, et al: Biomechanics: New observations on the
patients with contracted postero- Comparison of health-related quality of life morphology of the talar dome and its
medial soft tissues. between patients with end-stage ankle and relationship to ankle kinematics. Clin
hip arthrosis. J Bone Joint Surg Am 2008; Biomech (Bristol, Avon) 2014;29(1):1-6.
90(3):499-505.
14. Barnett CH, Napier JR: The axis of rotation
2. Saltzman CL, Salamon ML, Blanchard GM, at the ankle joint in man: Its influence upon
Summary et al: Epidemiology of ankle arthritis: Report the form of the talus and the mobility of the
of a consecutive series of 639 patients from a fibula. J Anat 1952;86(1):1-9.
tertiary orthopaedic center. Iowa Orthop J
Ankle distraction arthroplasty is a 2005;25:44-46. 15. Close JR: Some applications of the
surgical procedure whereby the functional anatomy of the ankle joint. J
3. Valderrabano V, Horisberger M, Russell I, Bone Joint Surg Am 1956;38(4):761-781.
ankle joint is temporarily mechan- Dougall H, Hintermann B: Etiology of
16. Inman VT: Inman’s Joints of the Ankle, ed
ically unloaded with an external ankle osteoarthritis. Clin Orthop Relat Res
2. Baltimore, MD, William and Wilkins,
2009;467(7):1800-1806.
fixator and is performed in con- 1991.
junction with osteophyte removal, 4. Brown TD, Johnston RC, Saltzman CL,
17. Hintermann B, Valderrabano V,
Marsh JL, Buckwalter JA: Posttraumatic
microfracture, soft-tissue release, osteoarthritis: A first estimate of incidence,
Dereymaeker G, Dick W: The HINTEGRA
and deformity correction, if neces- ankle: Rationale and short-term results of
prevalence, and burden of disease. J Orthop
122 consecutive ankles. Clin Orthop Relat
sary. Although robust clinical evi- Trauma 2006;20(10):739-744.
Res 2004;424:57-68.
dence is lacking, studies using 5. Thomas R, Daniels TR, Parker K: Gait
18. Inda DA, Blyakher A, O’Malley MJ,
animal models support the theory analysis and functional outcomes following
Rozbruch SR: Distraction arthroplasty for
ankle arthrodesis for isolated ankle
that the addition of mechanical un- the ankle using the Ilizarov frame. Tech
arthritis. J Bone Joint Surg Am 2006;88(3):
Foot Ankle Surg 2003;2(4)249-253.
loading and alignment correction 526-535.
improves the inherent ability of 19. Rozbruch SR: Posttraumatic reconstruction
6. Brunner S, Barg A, Knupp M, et al: The
of the ankle using the Ilizarov method. HSS
human cartilage repair to occur. Scandinavian total ankle replacement:
J 2005;1(1):68-88.
Long-term, eleven to fifteen-year,
The goals of the procedure are to survivorship analysis of the prosthesis in 20. Millward-Sadler SJ, Salter DM: Integrin-
provide pain relief, preserve seventy-two consecutive patients. J Bone dependent signal cascades in chondrocyte
motion, and to generate hyaline Joint Surg Am 2013;95(8):711-718. mechanotransduction. Ann Biomed Eng
2004;32(3):435-446.
cartilage or a durable hyaline-like 7. Wiegant K, van Roermund PM, Intema F,
cartilaginous substance. Although et al: Sustained clinical and structural 21. Pulai JI, Chen H, Im HJ, et al: NF-kappa B
benefit after joint distraction in the mediates the stimulation of cytokine and
clinical studies have demonstrated treatment of severe knee osteoarthritis. chemokine expression by human articular
good short- to intermediate-term Osteoarthritis Cartilage 2013;21(11): chondrocytes in response to fibronectin
1660-1667. fragments. J Immunol 2005;174(9):
clinical outcomes, the mechanisms 5781-5788.
for success and failure remain 8. Yanai T, Ishii T, Chang F, Ochiai N: Repair
of large full-thickness articular cartilage 22. Mow VC, Wang CC, Hung CT: The
unknown. Further clinical research defects in the rabbit: The effects of joint extracellular matrix, interstitial fluid and
on this procedure and the histologic distraction and autologous bone-marrow- ions as a mechanical signal transducer in
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 48
Foot & Ankle Mitchell Bernstein, MD, FRCSC, et al
articular cartilage. Osteoarthritis Cartilage 35. Fragomen AT, McCoy TH, Meyers KN, 47. Ploegmakers JJ, van Roermund PM, van
1999;7(1):41-58. Rozbruch SR: Minimum distraction gap: Melkebeek J, et al: Prolonged clinical benefit
How much ankle joint space is enough in from joint distraction in the treatment of
23. McKinley TO, Borrelli J Jr, D’Lima DD, ankle distraction arthroplasty? HSS J 2014; ankle osteoarthritis. Osteoarthritis Cartilage
Furman BD, Giannoudis PV: Basic science 10(1):6-12. 2005;13(7):582-588.
of intra-articular fractures and
posttraumatic osteoarthritis. J Orthop 36. Judet R, Judet T: The use of a hinge 48. Paley D, Lamm BM, Purohit RM, Specht SC:
Trauma 2010;24(9):567-570. distraction apparatus after arthrolysis and Distraction arthroplasty of the ankle: How
arthroplasty (author’s transl) [French]. Rev far can you stretch the indications? Foot
24. Haller JM, McFadden M, Kubiak EN, Chir Orthop Reparatrice Appar Mot 1978; Ankle Clin 2008;13(3):471-484, ix.
Higgins TF: Inflammatory cytokine 64(5):353-365.
response following acute tibial plateau 49. Lamm BM, Gourdine-Shaw M: MRI
fracture. J Bone Joint Surg Am 2015;97(6): 37. Aldegheri R, Trivella G, Saleh M: Articulated evaluation of ankle distraction: A
478-483. distraction of the hip: Conservative surgery preliminary report. Clin Podiatr Med Surg
for arthritis in young patients. Clin Orthop 2009;26(2):185-191.
25. D’Lima DD, Hashimoto S, Chen PC, Relat Res 1994;301:94-101.
Colwell CW Jr, Lotz MK: Human 50. Nguyen MP, Pedersen DR, Gao Y,
chondrocyte apoptosis in response to 38. Felson DT, Kim YJ: The futility of current Saltzman CL, Amendola A: Intermediate-
mechanical injury. Osteoarthritis Cartilage approaches to chondroprotection. Arthritis term follow-up after ankle distraction for
2001;9(8):712-719. Rheum 2007;56(5):1378-1383. treatment of end-stage osteoarthritis. J
Bone Joint Surg Am 2015;97(7):590-596.
26. Shapiro F, Koide S, Glimcher MJ: Cell 39. Kanamiya T, Naito M, Hara M,
origin and differentiation in the repair of Yoshimura I: The influences of 51. Marijnissen AC, Van Roermund PM, Van
full-thickness defects of articular cartilage. biomechanical factors on cartilage Melkebeek J, et al: Clinical benefit of joint
J Bone Joint Surg Am 1993;75(4): regeneration after high tibial osteotomy for distraction in the treatment of severe
532-553. knees with medial compartment osteoarthritis of the ankle: Proof of concept
osteoarthritis: Clinical and arthroscopic in an open prospective study and in a
27. Breinan HA, Martin SD, Hsu HP, Spector M: observations. Arthroscopy 2002;18(7): randomized controlled study. Arthritis
Healing of canine articular cartilage defects 725-729. Rheum 2002;46(11):2893-2902.
treated with microfracture, a type-II collagen
matrix, or cultured autologous chondrocytes. 40. Intema F, Thomas TP, Anderson DD, et al: 52. Hernigou P, Mathieu G, Poignard A,
J Orthop Res 2000;18(5):781-789. Subchondral bone remodeling is related to Manicom O, Beaujean F, Rouard H:
clinical improvement after joint distraction Percutaneous autologous bone-marrow
28. Furukawa T, Eyre DR, Koide S, Glimcher MJ: in the treatment of ankle osteoarthritis. grafting for nonunions: Surgical technique.
Biochemical studies on repair cartilage Osteoarthritis Cartilage 2011;19(6): J Bone Joint Surg Am 2006;88(suppl 1 pt
resurfacing experimental defects in the rabbit 668-675. 2):322-327.
knee. J Bone Joint Surg Am 1980;62(1):
79-89. 41. Hung SC, Nakamura K, Shiro R, Tanaka K, 53. Kim JD, Lee GW, Jung GH, et al: Clinical
Kawahara H, Kurokawa T: Effects of outcome of autologous bone marrow
29. Im GI, Kim DY, Shin JH, Hyun CW, continuous distraction on cartilage in a aspirates concentrate (BMAC) injection in
Cho WH: Repair of cartilage defect in the moving joint: An investigation on adult degenerative arthritis of the knee. Eur J
rabbit with cultured mesenchymal stem rabbits. J Orthop Res 1997;15(3): Orthop Surg Traumatol 2014;24(8):
cells from bone marrow. J Bone Joint 381-390. 1505-1511.
Surg Br 2001;83(2):289-294.
42. Nishino T, Chang F, Ishii T, Yanai T, 54. Betsch M, Thelen S, Santak L, et al: The
30. Kadiyala S, Young RG, Thiede MA, Bruder SP: Mishima H, Ochiai N: Joint distraction and role of erythropoietin and bone marrow
Culture expanded canine mesenchymal stem movement for repair of articular cartilage in concentrate in the treatment of
cells possess osteochondrogenic potential a rabbit model with subsequent weight- osteochondral defects in mini-pigs. PLoS
in vivo and in vitro. Cell Transplant 1997;6(2): bearing. J Bone Joint Surg Br 2010;92(7): One 2014;9(3):e92766.
125-134. 1033-1040.
55. Hegde V, Shonuga O, Ellis S, et al: A
31. van Valburg AA, van Roermund PM, 43. van Valburg AA, van Roy HL, Lafeber FP, prospective comparison of 3 approved
Marijnissen AC, et al: Joint distraction in Bijlsma JW: Beneficial effects of systems for autologous bone marrow
treatment of osteoarthritis (II): Effects on intermittent fluid pressure of low concentration demonstrated
cartilage in a canine model. Osteoarthritis physiological magnitude on cartilage and nonequivalency in progenitor cell number
Cartilage 2000;8(1):1-8. inflammation in osteoarthritis: An in vitro and concentration. J Orthop Trauma 2014;
study. J Rheumatol 1998;25(3):515-520. 28(10):591-598.
32. Saltzman CL, Hillis SL, Stolley MP,
Anderson DD, Amendola A: Motion 44. van Valburg AA, van Roermund PM, 56. Moroni A, Cadossi M, Romagnoli M,
versus fixed distraction of the joint in the Lammens J, et al: Can Ilizarov joint Faldini C, Giannini S: A biomechanical and
treatment of ankle osteoarthritis: A distraction delay the need for an arthrodesis histological analysis of standard versus
prospective randomized controlled trial. J of the ankle? A preliminary report. J Bone hydroxyapatite-coated pins for external
Bone Joint Surg Am 2012;94(11): Joint Surg Br 1995;77(5):720-725. fixation. J Biomed Mater Res B Appl
961-970. Biomater 2008;86(2):417-421.
45. Lafeber F, Veldhuijzen JP, Vanroy JL,
33. Smith NC, Beaman D, Rozbruch SR, Huber-Bruning O, Bijlsma JW: Intermittent 57. Pizà G, Caja VL, González-Viejo MA,
Glazebrook MA: Evidence-based hydrostatic compressive force stimulates Navarro A: Hydroxyapatite-coated
indications for distraction ankle exclusively the proteoglycan synthesis of external-fixation pins: The effect on pin
arthroplasty. Foot Ankle Int 2012;33(8): osteoarthritic human cartilage. Br J loosening and pin-track infection in leg
632-636. Rheumatol 1992;31(7):437-442. lengthening for short stature. J Bone Joint
Surg Br 2004;86(6):892-897.
34. Horn DM, Fragomen AT, Rozbruch SR: 46. van Valburg AA, van Roermund PM,
Supramalleolar osteotomy using circular Marijnissen AC, et al: Joint distraction in 58. van Roermund PM, Lafeber FP: Joint
external fixation with six-axis deformity treatment of osteoarthritis: A two-year distraction as treatment for ankle
correction of the distal tibia. Foot Ankle Int follow-up of the ankle. Osteoarthritis osteoarthritis. Instr Course Lect 1999;48:
2011;32(10):986-993. Cartilage 1999;7(5):474-479. 249-254.
© AMERICAN ACADEMY OF ORTHOPAEDIC SURGEONS 49
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- AyurvedA SYLUBUSДокумент110 страницAyurvedA SYLUBUSSri Sakthi Sumanan100% (1)
- Abdomen and Superficial Structures (Diagnostic Medical Sonography Series) Fourth EditionДокумент1 232 страницыAbdomen and Superficial Structures (Diagnostic Medical Sonography Series) Fourth EditionBenito Trevizo100% (2)
- Upper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedДокумент14 страницUpper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedJustyna PoznanskaОценок пока нет
- Head Massage TherapyДокумент169 страницHead Massage TherapyAnonymous vaQaeG15f100% (1)
- ARTNER, J. 2012. Atlas of Human Skeletal AnatomyДокумент68 страницARTNER, J. 2012. Atlas of Human Skeletal AnatomyDiana Rocio Carvajal ContrerasОценок пока нет
- Robyn Hondow - Origami For EveryoneДокумент22 страницыRobyn Hondow - Origami For EveryoneRui ViegasОценок пока нет
- 358 FullДокумент9 страниц358 FullRui ViegasОценок пока нет
- Projected Increase in Total Knee Arthroplasty in The United States Ean Alternative Projection ModelДокумент7 страницProjected Increase in Total Knee Arthroplasty in The United States Ean Alternative Projection ModelRui ViegasОценок пока нет
- Stephen 2015Документ9 страницStephen 2015Rui ViegasОценок пока нет
- Meniscal Repairs: A Review of Past, Current, and Future OptionsДокумент5 страницMeniscal Repairs: A Review of Past, Current, and Future OptionsRui ViegasОценок пока нет
- Pediatric Finger Fractures: Which Ones Turn Ugly?: Rauma UpplementДокумент7 страницPediatric Finger Fractures: Which Ones Turn Ugly?: Rauma UpplementRui ViegasОценок пока нет
- Module 2 PDFДокумент23 страницыModule 2 PDFRui ViegasОценок пока нет
- Management of Acute Hip Fracture - NEJM PDFДокумент10 страницManagement of Acute Hip Fracture - NEJM PDFRui ViegasОценок пока нет
- Anterior Cruciate Ligament Tear NEJMДокумент8 страницAnterior Cruciate Ligament Tear NEJMRui ViegasОценок пока нет
- Nick Robinson - World's Best OrigamiДокумент324 страницыNick Robinson - World's Best OrigamiRui Viegas86% (7)
- Bicontact: Aesculap OrthopaedicsДокумент52 страницыBicontact: Aesculap OrthopaedicsMohamed Swar Eldahab0% (1)
- TerminДокумент5 страницTerminAnonymous DA8iQzОценок пока нет
- Fibula Free Flap 2Документ5 страницFibula Free Flap 2Sanjay KumarОценок пока нет
- DCP and LC-DCP SystemsДокумент48 страницDCP and LC-DCP SystemsLA CbdingОценок пока нет
- Introduction To Health Care 4Th Edition Mitchell Solutions Manual Full Chapter PDFДокумент13 страницIntroduction To Health Care 4Th Edition Mitchell Solutions Manual Full Chapter PDFluyendonnasxs7100% (10)
- (Zoo301) Muscles OiaДокумент5 страниц(Zoo301) Muscles OiaRain HongОценок пока нет
- Twonewspeciesofthegenus Nemaspelailhavfromcavesin Georgia Opiliones NemastomatidaeДокумент19 страницTwonewspeciesofthegenus Nemaspelailhavfromcavesin Georgia Opiliones NemastomatidaeAneesh MathewОценок пока нет
- Nasopharyngeal Angiofibroma PDFДокумент10 страницNasopharyngeal Angiofibroma PDFAnonymous i4c2H2oPОценок пока нет
- 1.2.1 Positions Used in Nursing - SendДокумент45 страниц1.2.1 Positions Used in Nursing - Sendlumbasi150Оценок пока нет
- Anthropometry For Designers by John Croney 1Документ20 страницAnthropometry For Designers by John Croney 1Arturo EspitiaОценок пока нет
- Pacheco Et Al Phyllotis Pearsoni TH 2014Документ28 страницPacheco Et Al Phyllotis Pearsoni TH 2014Dennisse RuelasОценок пока нет
- Anfibios y Reptiles Del Ducto de PeruДокумент11 страницAnfibios y Reptiles Del Ducto de PeruJose Franco NaviaОценок пока нет
- Culture of The Cladoceran Moina MacrocopaДокумент6 страницCulture of The Cladoceran Moina MacrocoparoraysideblancoОценок пока нет
- Anatomy and Physiology of Speech Mechanism Study GuideДокумент33 страницыAnatomy and Physiology of Speech Mechanism Study GuidePhilip LuoОценок пока нет
- General AnatomyДокумент8 страницGeneral AnatomyKent SegubienseОценок пока нет
- TRATAMENTUL MEDICAL DE URGENTA Ro 346Документ19 страницTRATAMENTUL MEDICAL DE URGENTA Ro 346mihaela_bondocОценок пока нет
- Medical Terminology For Health Professions 7th Edition Ehrlich Test BankДокумент26 страницMedical Terminology For Health Professions 7th Edition Ehrlich Test BankGregorySimpsonmaos100% (46)
- Topography of Lower LimbДокумент10 страницTopography of Lower LimbMarina CretuОценок пока нет
- Intertrochanteric FractureДокумент2 страницыIntertrochanteric FractureDarwin Dux Lacson DimarucutОценок пока нет
- Fractures of The Distal Femur The And: Small AnirnДокумент11 страницFractures of The Distal Femur The And: Small AnirnVangelis PapachristosОценок пока нет
- Veterinary AnatomyДокумент4 страницыVeterinary AnatomysumОценок пока нет
- Sample Chapter of Wound Care Made Incredibly Easy! 1st UK EditionДокумент30 страницSample Chapter of Wound Care Made Incredibly Easy! 1st UK EditionLippincott Williams and Wilkins- Europe100% (2)
- (29final) 1125angl FinalДокумент133 страницы(29final) 1125angl FinalAlok KumarОценок пока нет
- Cucullanus Marajoara N. Sp.Документ10 страницCucullanus Marajoara N. Sp.Raul SousaОценок пока нет
- Acute Bronchiolitis Bilateral Lung Case Study PresentationДокумент36 страницAcute Bronchiolitis Bilateral Lung Case Study PresentationPyka Izzaty100% (1)