Академический Документы
Профессиональный Документы
Культура Документы
Nguyen Minh Tuan 2013
Загружено:
libremdОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Nguyen Minh Tuan 2013
Загружено:
libremdАвторское право:
Доступные форматы
Clinical Infectious Diseases
MAJOR ARTICLE
An Evidence-Based Algorithm for Early Prognosis of
Severe Dengue in the Outpatient Setting
Nguyen Minh Tuan,1 Ho Thi Nhan,2 Nguyen Van Vinh Chau,3 Nguyen Thanh Hung,1 Ha Manh Tuan,4 Ta Van Tram,5 Nguyen Le Da Ha,6 Phan Loi,7
Han Khoi Quang,8 Duong Thi Hue Kien,2 Tran Nguyen Bich Chau,2 Bridget Wills,2,9 Marcel Wolbers,2,9 and Cameron P. Simmons2,9,10
1
Children’s Hospital No. 1, 2Oxford University Clinical Research Unit, Hospital for Tropical Diseases, 3Hospital for Tropical Diseases, and 4Children’s Hospital No. 2, Ho Chi Minh City; 5Tien Giang
Provincial Hospital, My Tho; 6Dong Nai Children’s Hospital, Bien Hoa; 7Long An Provincial Hospital, Tan An; and 8Binh Duong Provincial Hospital, Thu Dau Mot, Vietnam; 9Centre for Tropical
Medicine, Nuffield Department of Medicine, University of Oxford, United Kingdom; and 10Department of Microbiology and Immunology, Peter Doherty Institute for Infection and Immunity, University
of Melbourne, Victoria, Australia
(See the Editorial Commentary by Low and Ooi on pages 664–5.)
Background. Early prediction of severe dengue could significantly assist patient triage and case management.
Methods. We prospectively investigated 7563 children with ≤3 days of fever recruited in the outpatient departments of 6 hospitals
in southern Vietnam between 2010 and 2013. The primary endpoint of interest was severe dengue (2009 World Health Organization
Guidelines), and predefined risk variables were collected at the time of enrollment to enable prognostic model development.
Results. The analysis population comprised 7544 patients, of whom 2060 (27.3%) had laboratory-confirmed dengue; nested
among these were 117 (1.5%) severe cases. In the multivariate logistic model, a history of vomiting, lower platelet count, elevated
aspartate aminotransferase (AST) level, positivity in the nonstructural protein 1 (NS1) rapid test, and viremia magnitude were all
independently associated with severe dengue. The final prognostic model (Early Severe Dengue Identifier [ESDI]) included history
of vomiting, platelet count, AST level. and NS1 rapid test status.
Conclusions. The ESDI had acceptable performance features (area under the curve = 0.95, sensitivity 87% (95% confidence
interval [CI], 80%–92%), specificity 88% (95% CI, 87%–89%), positive predictive value 10% (95% CI, 9%–12%), and negative pre-
dictive value of 99% (95% CI, 98%–100%) in the population of all 7563 enrolled children. A score chart, for routine clinical use, was
derived from the prognostic model and could improve triage and management of children presenting with fever in dengue-endemic
areas.
Keywords. dengue; diagnosis; tropical infectious diseases.
Dengue is the most common arboviral infection of humans The pathophysiological hallmarks of severe dengue are
and a public health burden in much of tropical Asia and Latin increased capillary permeability, coagulopathy, and a hemor-
America [1]. Seasonal epidemics, with children and young rhagic diathesis. For some patients this can lead to hypovolemic
adults most affected, place enormous stress on healthcare sys- shock, called dengue shock syndrome (DSS), with or without
tems in endemic countries. The burden of dengue in 10 endemic clinically severe bleeding. Other rare complications can include
countries was revealed with precision in phase 3 vaccine trials hepatic dysfunction, central nervous system involvement, and
of the now licensed Dengvaxia vaccine, in which approximately myocarditis [1, 3]. Progress in clinical management, particu-
10% of all febrile episodes in the control groups were confirmed larly fluid resuscitation and monitoring in intensive care, has
to be dengue cases [2]. Among these dengue cases, the percent- led to a decline in the dengue case fatality rate over the last 2
age requiring hospitalization was 19.1% in the Asian cohort and decades; it is now <1% of hospitalized cases in many settings
11.1% in the Latin American cohort [2]. [1], but can exceed 20% if treatment is inadequate [4]. There are
no specific antiviral or disease-modifying treatments for den-
Received 1 August 2016; editorial decision 8 November 2016; accepted 22 December 2016; gue despite recent efforts [5–8].
published online December 28, 2016.
Correspondence: C. Simmons, Department of Microbiology and Immunology, Peter Doherty DSS typically manifests between the fourth and sixth day of
Institute for Infection and Immunity, 792 Elizabeth St, University of Melbourne, VIC 3000, Aus- illness, during the so-called critical phase [1, 9, 10]. Features
tralia (csimmons@unimelb.edu.au).
such as abdominal pain, lethargy, rapidly rising hematocrit level,
Clinical Infectious Diseases® 2017;64(5):656–63
© The Author 2016. Published by Oxford University Press for the Infectious Diseases Society of and persistent vomiting have anecdotally been associated with
America. This is an Open Access article distributed under the terms of the Creative Commons progression to DSS or other clinically severe manifestations.
Attribution-NonCommercial-NoDerivs licence (http://creativecommons.org/licenses/by-nc-
nd/4.0/), which permits non-commercial reproduction and distribution of the work, in any
However, the prognostic value of these signs and symptoms,
medium, provided the original work is not altered or transformed in any way, and that the which usually occur near the time of shock, have not been for-
work is properly cited. For commercial re-use, please contact journals.permissions@oup.com.
mally evaluated. Thus emergency department physicians seeing
DOI: 10.1093/cid/ciw863
656 • CID 2017:64 (1 March) • Tuan et al
a patient with 3 days of fever in whom dengue is suspected are eligible for enrollment. Exclusion criteria were as follows: (1)
faced with a dilemma; to send the patient home with a request the attending physician believed they were unlikely to be able to
that they return for follow-up or to admit them for observa- attend follow-up or (2) the attending physician believed another
tion as they approach the critical phase. The hospitalization of a (nondengue) diagnosis was more likely.
large number of dengue cases for observation inevitably places
a burden on healthcare resources and has direct and indirect Data Collection at Enrollment
costs to patients and their families. Demographic details, clinical history and findings, and blood
Previous studies have explored early prognostic factors and samples for hematology, biochemistry, nonstructural protein
algorithms for predicting moderate or severe dengue. However, 1 (NS1) rapid test (NS1 Ag STRIP, Bio-Rad), and quantitative
heterogeneity in the case populations (adults vs children, hospi- reverse-transcription polymerase chain reaction (qRT-PCR)
talized vs outpatient) and clinical definitions of “severe” dengue were collected at the time of patient enrollment. The attending
[11–15] makes it difficult to make broad conclusions [1, 16–18]. physician was provided the routine hematology results only in
Additionally, most earlier prognostic studies did not report the order not to bias the decision on the patient’s management (eg,
positive and negative predictive values of the prognostic tool hospitalization vs ambulatory follow-up).
[11, 19, 20]. Against this backdrop, the aim of this current study
was to develop a practical, prognostic tool to enable the early Patient Follow-up and Case Definitions
prognosis of severe dengue in Vietnamese children. All ambulatory patients were followed up by daily phone call
to determine whether they were still at home or had been hos-
METHODS pitalized since the previous call. Daily phone calls were made
Human Research Ethics
until the fever had resolved and the patient had returned to
The scientific and ethical committees of all participating hos- daily activities. In 10% of all ambulatory patients, we collected
pitals and the Oxford University Tropical Research Ethical a convalescent blood sample (2 mL) on or after day 6 of illness
Committee (OXTREC 35-10) approved the study. Parents or for the purposes of diagnostic (immunoglobulin M [IgM])
guardians provided written informed consent for the child to serology. The selection of cases for follow-up and collection of a
participate. The study was conducted in compliance with good convalescent blood sample were by random assignment using a
clinical practice guidelines. computer-generated randomization list. For patients who were
hospitalized at any time during the 6 days after enrollment, a
Study Population second blood sample was collected at the time of discharge from
This was a prospective study of children with fever present- hospital and a case report form completed to capture data on
ing to the outpatient departments of collaborating hospi- whether the patient evolved to severe dengue according to the
tals in Vietnam including the Hospital for Tropical Diseases, World Health Organization (WHO) 2009 classification scheme.
Children’s Hospital No. 1, Children’s Hospital No. 2, Tien Giang Laboratory-confirmed dengue was defined as a positive
Provincial Hospital, Dong Nai Children’s Hospital, Binh Duong result with either one of the following tests: (1) validated qRT-
Provincial Hospital, and Long An Provincial Hospital. The pre- PCR assay [21]; (2) NS1 enzyme-linked immunosorbent assay
defined sample size was to enroll a sufficient number of patients (ELISA) (Platelia Dengue NS1 Ag ELISA, Bio-Rad); or (3) IgM
to detect 160 severe dengue cases (and thereby evaluate up to 16 seroconversion in paired blood samples (Panbio, Brisbane,
predefined variables for their association with severe dengue), Australia). IgM seroconversion was defined as a change in test
or 13 500 patients in total, whichever occurred first. For fund- result from negative to positive in paired plasma samples with the
ing reasons, the study stopped after enrollment of 7563 patients second sample collected ≥6 days after illness onset and >2 days
(and 117 severe dengue cases). The consequences of not recruit- after the first sample. A stepwise approach to diagnostic testing
ing the targeted number of severe cases was 2-fold. First, we was performed. First, all enrollment plasma samples were tested
downsized the number of predictor variables for testing so as to with a validated, qRT-PCR assay to detect dengue virus (DENV)
be compliant with the rule of thumb of having a minimum of 10 RNA. Next, any enrollment plasma samples that were negative in
outcome events per predictor variable in the regression proce- the qRT-PCR assay were tested using the Platelia Dengue NS1 Ag
dures. A relatively smaller sample size will also have generated ELISA assay and scored according to the manufacturer’s instruc-
a larger confidence interval for the estimation statistics than tions. Samples with equivalent results were repeated and, if still
would otherwise have been the case. Study enrollment com- equivocal, they were scored as negative. Next, IgM ELISA serol-
menced on 1 October 2010 and finished on 31 December 2013. ogy (Panbio) was performed according to the manufacturer’s
Children 1–15 years of age, accompanied by a parent/guardian instructions for patients who had paired plasma samples (100%
with a mobile phone, who presented to the designated outpa- of hospitalized cases and 10% of ambulatory cases) and who were
tient clinic with ≤72 hours of fever and in whom the attend- negative in both the DENV qRT-PCR assay and Platelia Dengue
ing physician believes dengue was a possible diagnosis were NS1 ELISA. Patients who had negative test results for DENV
Early Prognosis of Severe Dengue • CID 2017:64 (1 March) • 657
qRT-PCR and NS1 ELISA and no IgM seroconversion in paired complete hematological and biochemical data, of whom 2060
blood samples were classified as “not dengue.” Patients who had (27.3%) had laboratory-confirmed dengue and 1954 (25.9%)
negative test results for DENV qRT-PCR and NS1 ELISA at the were viremic as determined by qRT-PCR. Amongst the 2060
time of enrollment, but did not have paired samples available for laboratory confirmed dengue cases, there were 117 (5.6%) cases
serology, were classified as a “presumptive not dengue” case. For of severe dengue (WHO 2009 Guidelines) but no deaths. Table
analysis, data from “not dengue” and “presumptive not dengue” 1 describes the baseline characteristics of the study population.
cases were pooled and were categorized as “other febrile illness.”
Prognostic Models for Early Identification of Severe Dengue Cases Among
Statistical Methods Febrile Patients
To develop the prognostic models for severe dengue, we used For simplicity, all continuous variables were treated as linear
logistic regression procedures with predefined clinical, hema- terms in the multivariable model development of the prog-
tological, and biochemical variables and NS1 rapid test status. nostic algorithm (Supplementary Table 1 and Supplementary
Bayesian information criteria were used to downselect from the Statistical Appendix). Many of the predefined clinical and
original full models to the most parsimonious model for prac- laboratory variables that were collected at enrollment were
tical clinical application. Model validation was examined by 2 associated with progression to severe dengue in the univari-
approaches: (1) “leave-one-site-out cross-validation”—that is, ate analysis (Table 2). In the multivariate logistic model, a
repeatedly developing the algorithm on all but 1 study site and history of vomiting, lower platelet count, elevated aspartate
validation on the left-out study site; and (2) temporal validation aminotransferase (AST) level, and positivity in the NS1 rapid
with patients recruited before 15 June 2012 as the training set test were all independently associated with severe dengue
and patients recruited thereafter as the evaluation set [22]. The within the population of febrile patients. The most practical
final logistic regression model was converted to a nomogram and parsimonious prognostic model, herein called the Early
for ease of use in clinical practice. All analyses were performed Severe Dengue Identifier (ESDI), included history of vomiting,
with the statistical software R version 3.1.1 (R Foundation platelet count, AST (per 2-fold increase), and NS1 rapid test
for Statistical Computing, Vienna, Austria). Significance was status at the time of enrollment (Table 3). Figure 2A illustrates
assigned at P < .05 for all parameters and was 2-sided. the performance characteristics of the ESDI at various cutoffs
in the febrile population. At the cutoff of 0.02, the ESDI had
RESULTS a sensitivity of 87% (95% CI, 80%–92%), specificity of 88%
Baseline Characteristics of Study Participants (95% CI, 87%–89%), positive predictive value of 10% (95% CI,
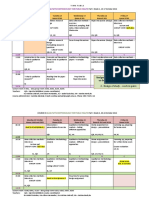
Between October 2010 and December 2013, we enrolled 7563 9%–12%), and negative predictive value of 99% (95% CI, 98%–
children with fever history of <72 hours at the outpatient depart- 100%) for correctly discriminating severe dengue from other
ments of 7 hospitals in southern Vietnam. A description of the cases within the febrile population. This cutoff was very close
study profile is shown in Figure 1. There were 7544 patients with to the point on the receiver operating characteristic (ROC)
Figure 1. Study profile with a description of the patient cohort and subgroups that were used to derive the prognostic models. Abbreviations: ELISA, enzyme-linked immu-
nosorbent assay; IgM, immunoglobulin G; NS1, nonstructural protein 1; RT-PCR, reverse-transcription polymerase chain reaction.
658 • CID 2017:64 (1 March) • Tuan et al
Table 1. Baseline Characteristics of Study Participants
Severe Dengue Nonsevere Dengue Other Febrile Illness
Characteristic (n = 117) (n = 1943) (n = 5484)
Age, y 9 (7–11) 9 (6–11) 5 (3–8)
BMI, kg/m2 16.9 (14.6–20.1) 16.5 (14.7–19.0) 15.6 (14.2–17.7)
Day of illness
1 15 (12.8) 426 (22.0) 1659 (30.3)
2 43 (36.8) 789 (40.8) 2372 (43.4)
3 59 (50.4) 718 (37.1) 1437 (26.3)
Vomiting 79 (67.5) 804 (41.6) 1902 (34.8)
Abdominal pain 34 (29.1) 385 (19.9) 930 (17.0)
Mucosal bleeding 9 (7.7) 112 (5.8) 134 (2.5)
WBC count, × 103 cells/µL 3.7 (2.5–5.8) 4.9 (3.6–6.9) 9.0 (6.4–12.5)
Platelet count, × 103 cells/µL 110 (86.5–147) 182 (144–227) 242 (201–291)
Hematocrit, % 40 (37.8–42.3) 38.6 (36.6–40.6) 37.4 (35.3–39.7)
Albumin, g/L 43.3 (40.5–45.1) 43.8 (41.8–45.8) 44.2 (42.2–46.2)
AST, U/L 101 (61.5–155) 50 (40–66) 42 (35–49)
NS1 rapid test positive 97 (82.9) 1360 (70.4) 37 (0.7)
Viremia concentration, log10 copies/mL 7.5 (6.4–8.3) (n = 115) 7.2 (6.0–8.2) (n = 1839) …
Serotype (n = 115) (n = 1839)
DENV-1 38 (32.5) 725 (37.5)
DENV-2 37 (31.6) 404 (20.9)
DENV-3 6 (5.1) 181 (9.4)
DENV-4 34 (29.1) 519 (26.8)
Unknown 2 (1.7) 104 (5.4)
Values are presented as median (interquartile range) for continuous variables or frequency (%) for categorical variables. All laboratory results were acquired on the day of enrollment.
Abbreviations: AST, aspartate aminotransferase; BMI, body mass index; DENV, dengue virus; NS1, nonstructural protein 1; WBC, white blood cell.
curve closest to the upper left corner (perfect model), which The calibration plot shows that the ESDI overestimates the risk
was 0.018 (Figure 2A). The area under the ROC curve (AUC) of severe dengue in the highest decile of predicted probability
of the ESDI in the analyzed population was 0.95 using the cut- (Figure 2C)—that is, patients scored as having the highest decile
off of 0.02 (Figure 2B). of risk actually have a lower true risk than the model suggests.
Table 2. Univariate Analysis of Candidate Predictors of Severe Dengue Among Laboratory-Confirmed Dengue and All Subjects
Severe Dengue vs Nonsevere Dengue Among
Laboratory-Confirmed Dengue Cases Severe Dengue vs All Other Study Participants
Predictor OR 95% CI P Value OR 95% CI P Value
Age (+ 1 y) 1.00 .95–1.06 .901 1.16 1.10–1.21 <.001
BMI (+ 1 kg/m2) 1.03 .98–1.09 .223 1.10 1.04–1.15 <.001
Day of illness (+ 1 d) 1.53 1.17–1.99 .002 1.97 1.52–2.56 <.001
Vomiting: Yes 2.92 1.96–4.33 <.001 3.60 2.45–5.36 <.001
Abdominal pain: Yes 1.65 1.09–2.49 .018 1.89 1.25–2.81 .003
Mucosal bleeding: Yes 1.35 .67–2.74 .405 2.40 1.12–4.54 .027
WBC (+ 1000 cells/µL) .85 .78–.93 <.001 .66 .60–.71 <.001
Platelet count (+ 10 000 cells/µL) .82 .79–.85 <.001 .77 .74–.79 <.001
Hematocrit (+ 1%) 1.14 1.08–1.20 <.001 1.20 1.14–1.26 <.001
Albumin (+ 1 g/L) .92 .87–.97 .003 .89 .85–.94 <.001
AST (per 2-fold increase) 3.74 3.00–4.68 <.001 5.07 4.18–6.16 <.001
NS1 rapid test positive: Yes 2.06 1.26–3.36 .004 20.82 13.12–34.77 <.001
Viremia (+ 1 log10 copies/mL) 1.22 1.07–1.39 .003 … … …
Serotypea
DENV-1 1.00 … … … … …
DENV-2 1.74 1.09–2.79 .020 … … …
DENV-3 .63 .26–1.52 .305 … … …
DENV-4 1.25 .78–2.02 .355 … … …
Abbreviations: AST, aspartate aminotransferase; BMI, body mass index; CI, confidence interval; DENV, dengue virus; NS1, nonstructural protein 1; OR, odds ratio; WBC, white blood cell.
a
Univariate effect of serotype on severe dengue estimated from univariate logistic regression, using DENV-1 as reference group.
Early Prognosis of Severe Dengue • CID 2017:64 (1 March) • 659
Table 3. Multivariate Analysis of Candidate Predictors for Severe Dengue in All Subjects
Full Model With Predefined Candidate Predictors Reduced Model by Stepwise BIC (ESDI)
Predictor OR 95% CI P Value OR 95% CI P Value
Age (+ 1 y) .97 .91–1.05 .481 … … …
BMI (+ 1 kg/m2) 1.03 .97–1.09 .369 … … …
Day of illness (+ 1 d) 1.69 .58–1.18 .295 … … …
Vomiting: Yes 2.13 1.36–3.32 <.001 2.14 1.4–3.3 <.001
Abdominal pain: Yes .98 .60–1.61 .933 … … …
Mucosal bleeding: Yes 1.74 .79–3.85 .192 … … …
WBC count (+ 1000 cells/µL) 1.04 .95–1.14 .41 … … …
Platelet count (+ 10 000 cells/µL) .83 .79–.88 <.001 .85 .81–.88 <.001
Hematocrit (+ 1 %) 1.06 1.00–1.14 .059 … … …
Albumin (+ 1 g/L) 1.00 .93–1.07 .937 … … …
AST (per 2-fold increase) 2.67 2.09–3.43 <.001 2.72 2.14–3.45 <.001
NS1 rapid test positive: Yes 9.91 5.58–17.59 <.001 8.61 5.12–14.48 <.001
Full model with predefined candidate predictors: clinical, hematological, and biochemical features and NS1 rapid test status.
Abbreviations: AST, aspartate aminotransferase; BIC, Bayesian information criteria; BMI, body mass index; CI, confidence interval; ESDI, Early Severe Dengue Identifier; NS1, nonstructural
protein 1; OR, odds ratio; WBC, white blood cell.
A summary of the performance characteristics of the ESDI by tem- looking for an evidence-based tool to improve triage and man-
poral and leave-one-site out validation is presented in Table 4. The agement. It could also deliver efficiencies to clinical trials (ie,
ESDI clearly showed good discriminative performance for both enable enrollment of patients at greater risk of severe dengue).
temporal and leave-one-site out validation with an AUC of at least The ability to make an early, evidence-based prognosis of
0.96. Leave-one-serotype-out validation results (Supplementary severe dengue could have practical rewards to clinical care,
Table 2) demonstrated the ESDI was robust to differences in the health systems, and clinical research. First, the ESDI could assist
serotypes that contributed to the dengue case population. clinical services in identifying at-risk patients for triage to more
regular observations than would occur under the current stand-
A Practical Tool for Physicians to Predict Severe Dengue ard of care; this could mean hospitalization or more regular
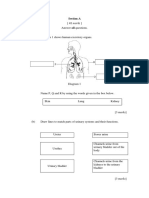
A nomogram was developed to predict severe dengue using the visits in an outpatient setting. Additionally, for outpatient care,
4 independent parameters in the ESDI (Figure 3). The nom- communication to the patient’s caregivers could be appropri-
ogram is used by totaling the points assigned on the scales ately calibrated and with attention to WHO-nominated clinical
for each independent parameter. For example, a patient with warning signs [1]. The benefits of early prognosis, with accom-
vomiting, a platelet count of 100 000 cells/µL, positive NS1 panying closer clinical management, could potentially include a
rapid test, and an AST level of 280 U/L (7-fold increase com- reduction in the frequency with which cases progress to severe
pared with the upper normal value of 40 U/L) has a score of disease and, hence, cost to the healthcare system and to families.
5 + 89 + 14 + 26 = 134, and the corresponding risk of severe However, the generally low positive predictive value of the ESDI
dengue is approximately 35%. (10% at a cutoff of 0.02) inevitably means that a large number of
cases identified as being at risk of severe disease will in fact have
DISCUSSION
uneventful disease evolutions. Nonetheless, the ESDI poten-
The great majority of clinically severe complications in pediat- tially offers a tool to clinicians in some circumstances because
ric dengue patients occur between the fourth and sixth day of they currently work in a vacuum of evidence with respect to
illness [1, 9, 10]. Thus there is a window of opportunity in the early prognosis of pediatric dengue cases.
first few days of illness to both make a diagnosis and try to iden- In the context of the multiparameter ESDI, the inclusion of
tify those patients at greatest risk of severe complications so that NS1 status (by rapid test) delivered a small but incremental
their management can be adapted accordingly. Yet the current improvement to prognostic model performance. Clinical tri-
standard of care in relation to diagnosis and prognosis in many als of candidate dengue therapeutics [5–7] have employed NS1
endemic countries relies mostly on subjective clinical skills that rapid tests to enable early diagnosis and enrollment. However,
are variable across different countries, across different levels of NS1 rapid tests have no utility as stand-alone prognostic tests.
the health system, and between individual physicians. Here we For example, a clinical trial of early prednisolone therapy in 225
demonstrate the feasibility of evidence-based early prognosis NS1 rapid test–positive Vietnamese children observed that only
(within 72 hours of illness onset) of severe dengue using simple 6.7% of cases (in the placebo arm) developed DSS. Treatment
clinical and laboratory investigations that are available in many trials in NS1 rapid test–positive adult dengue cases observe an
endemic settings. The ESDI model could be helpful to physicians even lower incidence of severe dengue [5, 7, 8]. Thus, currently,
660 • CID 2017:64 (1 March) • Tuan et al
meet their objectives. The ESDI could potentially enhance the
efficiency of some trials by enriching the study population with
cases at higher risk of developing severe dengue, compared with
the NS1 rapid test used alone.
Many of the parameters used in the ESDI are collectable in
primary care settings in Vietnam and other endemic coun-
tries. For example, the NS1 antigen rapid test is available in
many hospital emergency department/outpatient settings in
Vietnam. NS1 rapid tests are recommended by WHO as a rou-
tine screening test for patients with clinically suspected dengue
in the acute febrile phase [23]. The diagnostic performance, and
limitations, of this test have been extensively described in this
patient cohort [24] and elsewhere [25–32]. Previous studies also
demonstrated that viremia levels in the first 72 hours of illness
were positively correlated with NS1 rapid test positivity [31,
33–36]. Blood hematology (platelet count) and biochemistry
(AST level) were also important to the operation of the ESDI;
hence, only in settings where these services are routinely avail-
able could the ESDI be utilized. Potts et al previously observed
that elevated AST in the first 3 days of illness was a predictor for
severe dengue [20]. Presumably, early elevations in blood AST
concentrations are a signal of the severity of disseminated virus
infection and tissue damage.
Not all DENV serotypes were equally associated with severe
outcomes. DENV-2 in particular was overrepresented among
severe cases, consistent with previous studies [37, 38]. For rea-
sons of study design, we could not dissociate whether DENV-2
was acting as a proxy for secondary infection, itself a well-rec-
ognized risk factor for severe dengue, or was independently
associated with severe dengue.
Only one previous prospective study, of 1384 febrile Thai
children (including 37 with DSS), by Potts et al, is similar in
study design to that reported here. Potts et al used classification
and regression tree analysis to derive an algorithm from lab-
oratory variables collected at the time of enrollment (platelet
count, white blood cell count, monocyte percentage, and hema-
tocrit). The best algorithm had 97% sensitivity and 48% speci-
ficity for the identification of patients who progressed to DSS
[20]; however, positive and negative predictive values were not
reported. The study described here includes several important
points of difference including (1) a much larger sample size and
Figure 2. Performance of the Early Severe Dengue Identifier (ESDI) in reverse-tran-
scription polymerase chain reaction–positive dengue patients. A, Possible sensitiv-
inclusion of clinically severe cases who did not have DSS; (2)
ity/specificity trade-offs for different cutoff values of the ESDI and the distance acquisition of clinical and laboratory data; and (3) validation of
from the corresponding points on the receiver operating characteristic (ROC) curve model performance.
to the upper left corner (perfect model). B, ROC curve. C, Calibration plot displaying
Our study, and the resulting ESDI, has some inherent limita-
a scatterplot-smoother of predicted vs observed risks (dashed line), predicted vs
observed risks for 10 patient strata of equal size grouped according to predicted tions. First, the ESDI will not be suitable in all outpatient settings
risks (triangles), and the ideal identity line (solid line). The rugs at the bottom of because NS1 rapid tests and biochemistry are not always availa-
the graphs characterize the distribution of predicted risks in severe dengue and ble. The ESDI is only applicable to observations made in the first
nonsevere dengue cases, respectively. Abbreviation: AUC, area under the curve.
72 hours of illness; it is uncertain what the test performance will
be outside this window of presentation. The evolution of dengue
early-phase clinical trials endeavoring to use severe dengue as is probably impacted by clinical management, so the incidence
an endpoint would require very large patient sample sizes to rate of severe dengue described in this study could be context
Early Prognosis of Severe Dengue • CID 2017:64 (1 March) • 661
Table 4. Performance of the Early Severe Dengue Identifier in All Subjects
Parameter Apparent Performance Temporal Validation Leave-One-Site-Out Validation
Calibration intercept 0.09 0.11 0.13 (–.09 to .13)
Calibration slope 1.12 1.20 1.17 (.95–1.22)
AUC 0.95 (.92–.98) 0.96 (.93–.99) 0.96 (.91–.98)
Sensitivity (cutoff 0.02) 0.87 (.80–.92) 0.93 (.86–.97) 0.91 (.78–.95)
Specificity (cutoff 0.02) 0.88 (.87–.89) 0.85 (.84–.86) 0.86 (.82–.92)
PPV (cutoff 0.02) 0.10 (.09–.12) 0.10 (.09–.12) 0.10 (.09–.12)
NPV (cutoff 0.02) 0.99 (.98–1) 0.99 (.98–1) 0.99 (.97–1)
Data in parentheses are 95% confidence intervals. The prognostic model for severe dengue in all patients was the reduced model by stepwise Bayesian information criteria, derived from
the original full model that included all predefined clinical and hemobiochemical features and nonstructural protein 1 rapid test status.Abbreviations: AUC, area under the curve; NPV, negative
predictive value; PPV, positive predictive value.
dependent; for the same patient population, other settings ESDI has a good discriminative ability (AUC = 0.95), the low
might observe a lower or higher incidence of severe dengue and positive predictive value (common to many algorithms seeking
this could impact the prognostic classifier. Finally, although the to classify relatively rare events) means that the number of true
severe dengue cases will be overestimated. Application of the
ESDI may result in excessive hospitalizations, unnecessary fol-
low-up procedures, and the associated economic burden than
would occur under the current standard of care. Further “pilot
phase” research is needed to understand the benefits and disad-
vantages of the ESDI in routine practice and clinical research.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online.
Consisting of data provided by the author to benefit the reader, the posted
materials are not copyedited and are the sole responsibility of the author, so
questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors are grateful for the collaboration of the
patients and their families who participated in this research, and the many
healthcare workers who made this study possible.
Financial support. This work was supported by the Australian National
Health and Medical Research Council (GNT1006549) and the Wellcome
Trust (GNT084368/Z/07/Z).
Potential conflicts of interest. All authors: No reported conflicts.
The authors have submitted the ICMJE Form for Disclosure of Potential
Conflicts of Interest. Conflicts that the editors consider relevant to the con-
tent of the manuscript have been disclosed.
References
1. World Health Organization. Dengue: guideline for diagnosis, treatment, preven-
tion and control. Geneva, Switzerland: WHO, 2009.
2. L’Azou M, Moureau A, Sarti E, et al; CYD14 Primary Study Group; CYD15
Primary Study Group. Symptomatic dengue in children in 10 Asian and Latin
American countries. N Engl J Med 2016; 374:1155–66.
3. Martinez-Torres E, Polanco-Anaya AC, Pleites-Sandoval EB. Why and how chil-
dren with dengue die? Rev Cubana Med Trop 2008; 60:40–7.
4. Ranjit S, Kissoon N. Dengue hemorrhagic fever and shock syndromes. Pediatr
Crit Care Med 2011; 12:90–100.
5. Nguyen NM, Tran CN, Phung LK, et al. A randomized, double-blind placebo
controlled trial of balapiravir, a polymerase inhibitor, in adult dengue patients. J
Infect Dis 2013; 207:1442–50.
6. Tam DT, Ngoc TV, Tien NT, et al. Effects of short-course oral corticosteroid ther-
Figure 3. Nomogram of the prognostic model to predict the risk of severe den-
apy in early dengue infection in Vietnamese patients: a randomized, placebo-con-
gue. A vertical line from a predictor value to the “points” axis assigns points to the 4 trolled trial. Clin Infect Dis 2012; 55:1216–24.
required variables: vomiting, platelet count (PLT), nonstructural protein 1 (NS1) rapid 7. Low JG, Sung C, Wijaya L, et al. Efficacy and safety of celgosivir in patients with
test status, and aspartate aminotransferase (AST) level. The sum of these points (total dengue fever (CELADEN): a phase 1b, randomised, double-blind, placebo-con-
points) can then be translated to the corresponding predicted risk of severe dengue. trolled, proof-of-concept trial. Lancet Infect Dis 2014; 14:706–15.
662 • CID 2017:64 (1 March) • Tuan et al
8. Tricou V, Minh NN, Van TP, et al. A randomized controlled trial of chloroquine for 24. Tuan NM, Nhan HT, Chau NV, et al. Sensitivity and specificity of a novel classifier
the treatment of dengue in Vietnamese adults. PLoS Negl Trop Dis 2010; 4:e785. for the early diagnosis of dengue. PLoS Negl Trop Dis 2015; 9:e0003638.
9. Simmons CP, Farrar JJ, Nguyen vV, Wills B. Dengue. N Engl J Med 2012; 25. Hang VT, Nguyet NM, Trung DT, et al. Diagnostic accuracy of NS1 ELISA and
366:1423–32. lateral flow rapid tests for dengue sensitivity, specificity and relationship to virae-
10. Phung KL, Dong THT, Tran VD, et al. Clinical characteristics of dengue shock mia and antibody responses. PLoS Negl Trop Dis 2009; 3:e360.
syndrome in Vietnamese children; a 10-year prospective study in a single hospi- 26. Guzman MG, Jaenisch T, Gaczkowski R, et al. Multi-country evaluation of the
tal. Clin Infect Dis 2013; 57:1577–86. sensitivity and specificity of two commercially-available NS1 ELISA assays for
11. Tanner L, Schreiber M, Low JG, et al. Decision tree algorithms predict the diagno- dengue diagnosis. PLoS Negl Trop Dis 2010; 4.
sis and outcome of dengue fever in the early phase of illness. PLoS Negl Trop Dis 27. Duong V, Ly S, Lorn Try P, et al. Clinical and virological factors influencing the
2008; 2:e196. performance of a NS1 antigen-capture assay and potential use as a marker of den-
12. Khan MI, Anwar E, Agha A, et al. Factors predicting severe dengue in patients gue disease severity. PLoS Negl Trop Dis 2011; 5:e1244.
with dengue fever. Mediterr J Hematol Infect Dis 2013; 5:e2013014. 28. Dussart P, Petit L, Labeau B, et al. Evaluation of two new commercial tests for the
13. Fox A, Le NM, Simmons CP, et al. Immunological and viral determinants of den- diagnosis of acute dengue virus infection using NS1 antigen detection in human
gue severity in hospitalized adults in Ha Noi, Viet Nam. PLoS Negl Trop Dis 2011; serum. PLoS Negl Trop Dis 2008; 2:e280.
5:e967. 29. Kumarasamy V, Chua SK, Hassan Z, et al. Evaluating the sensitivity of a commer-
14. Chuansumrit A, Puripokai C, Butthep P, et al. Laboratory predictors of dengue cial dengue NS1 antigen-capture ELISA for early diagnosis of acute dengue virus
shock syndrome during the febrile stage. Southeast Asian J Trop Med Public infection. Singapore Med J 2007; 48:669–73.
Health 2010; 41:326–32. 30. Lapphra K, Sangcharaswichai A, Chokephaibulkit K, et al. Evaluation of an NS1
15. Carrasco LR, Leo YS, Cook AR, et al. Predictive tools for severe dengue con- antigen detection for diagnosis of acute dengue infection in patients with acute
forming to World Health Organization 2009 criteria. PLoS Negl Trop Dis 2014; febrile illness. Diagn Microbiol Infect Dis 2008; 60:387–91.
8:e2972. 31. Tricou V, Vu HT, Quynh NV, et al. Comparison of two dengue NS1 rapid tests for
16. Gregory CJ, Santiago LM, Arguello DF, Hunsperger E, Tomashek KM. Clinical sensitivity, specificity and relationship to viraemia and antibody responses. BMC
and laboratory features that differentiate dengue from other febrile illnesses Infect Dis 2010; 10:142.
in an endemic area—Puerto Rico, 2007–2008. Am J Trop Med Hyg 2010; 32. Zainah S, Wahab AH, Mariam M, et al. Performance of a commercial rapid den-
82:922–9. gue NS1 antigen immunochromatography test with reference to dengue NS1 anti-
17. Daumas RP, Passos SR, Oliveira RV, et al. Clinical and laboratory features that gen-capture ELISA. J Virol Methods 2009; 155:157–60.
discriminate dengue from other febrile illnesses: a diagnostic accuracy study in 33. Thomas L, Najioullah F, Verlaeten O, et al. Relationship between nonstructural
Rio de Janeiro, Brazil. BMC Infect Dis 2013; 13:77. protein 1 detection and plasma virus load in dengue patients. Am J Trop Med Hyg
18. Ho TS, Wang SM, Lin YS, Liu CC. Clinical and laboratory predictive markers for 2010; 83:696–9.
acute dengue infection. J Biomed Sci 2013; 20:75. 34. Chau TN, Anders KL, Lien le B, et al. Clinical and virological features of dengue
19. Falconar AK, Romero-Vivas CM. Simple prognostic criteria can definitively iden- in Vietnamese infants. PLoS Negl Trop Dis 2010; 4:e657.
tify patients who develop severe versus non-severe dengue disease, or have other 35. Duyen HT, Ngoc TV, Ha do T, et al. Kinetics of plasma viremia and soluble non-
febrile illnesses. J Clin Med Res 2012; 4:33–44. structural protein 1 concentrations in dengue: differential effects according to
20. Potts JA, Gibbons RV, Rothman AL, et al. Prediction of dengue disease severity serotype and immune status. J Infect Dis 2011; 203:1292–300.
among pediatric Thai patients using early clinical laboratory indicators. PLoS 36. Libraty DH, Young PR, Pickering D, et al. High circulating levels of the dengue
Negl Trop Dis 2010; 4:e769. virus nonstructural protein NS1 early in dengue illness correlate with the devel-
21. Hue KD, Tuan TV, Thi HT, et al. Validation of an internally controlled one-step opment of dengue hemorrhagic fever. J Infect Dis 2002; 186:1165–8.
real-time multiplex RT-PCR assay for the detection and quantitation of dengue 37. Vaughn DW, Green S, Kalayanarooj S, et al. Dengue viremia titer, antibody
virus RNA in plasma. J Virol Methods 2011; 177:168–73. response pattern, and virus serotype correlate with disease severity. J Infect Dis
22. Harrell F. Regression modeling strategies with applications to linear models, 2000; 181:2–9.
logistic regression, and survival analysis. New York: Springer, 2001. 38. Fried JR, Gibbons RV, Kalayanarooj S, et al. Serotype-specific differences in
23. World Health Organization. Handbook for clinical management of dengue. the risk of dengue hemorrhagic fever: an analysis of data collected in Bangkok,
Geneva, Switzerland: WHO, 2012. Thailand from 1994 to 2006. PLoS Negl Trop Dis 2010; 4: e617.
Early Prognosis of Severe Dengue • CID 2017:64 (1 March) • 663
Вам также может понравиться
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementОт EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouОценок пока нет
- Effects of Short-Course Oral Corticosteroid Therapy in Early Dengue Infection in Vietnamese Patients: A Randomized, Placebo-Controlled TrialДокумент10 страницEffects of Short-Course Oral Corticosteroid Therapy in Early Dengue Infection in Vietnamese Patients: A Randomized, Placebo-Controlled TrialJihadatul KholilahОценок пока нет
- Prediction of Dengue Disease Severity Among Pediatric Thai Patients Using Early Clinical Laboratory IndicatorsДокумент7 страницPrediction of Dengue Disease Severity Among Pediatric Thai Patients Using Early Clinical Laboratory Indicatorsnita_hasnitaОценок пока нет
- Nifurtimox 1Документ7 страницNifurtimox 1AYUSH DUBEYОценок пока нет
- Neutropenic Colitis in Children 2011Документ4 страницыNeutropenic Colitis in Children 2011IRINA SULEY TIRADO PEREZОценок пока нет
- Dengue Hemorrhagic Fever: The Sensitivity and Specificity of The World Health Organization Definition For Identification of Severe Cases of Dengue in Thailand, 1994-2005Документ10 страницDengue Hemorrhagic Fever: The Sensitivity and Specificity of The World Health Organization Definition For Identification of Severe Cases of Dengue in Thailand, 1994-2005Dessy AmaranthaОценок пока нет
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsДокумент9 страницResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998Оценок пока нет
- Journal PNTD 0001244Документ10 страницJournal PNTD 0001244Zulia Ahmad BurhaniОценок пока нет
- BJC 2017154Документ8 страницBJC 2017154Altair CamargoОценок пока нет
- Risk Factors For Mortality in Patients With DengueДокумент13 страницRisk Factors For Mortality in Patients With DengueTaufiqurrokhman RofiiОценок пока нет
- Journal of Pediatric HematologyДокумент10 страницJournal of Pediatric HematologyasepОценок пока нет
- Risk Factors For Herpes Zoster in Patients With Chronic Kidney Disease: A Case-Control StudyДокумент7 страницRisk Factors For Herpes Zoster in Patients With Chronic Kidney Disease: A Case-Control StudyPushpendra Singh ChouhanОценок пока нет
- Incidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorДокумент6 страницIncidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorTomasОценок пока нет
- Civ 028Документ9 страницCiv 028Deah RisbaОценок пока нет
- 2016 Article 1849 PDFДокумент8 страниц2016 Article 1849 PDFdydy_7193Оценок пока нет
- Dengue in Renal Transplant Patients A ReДокумент3 страницыDengue in Renal Transplant Patients A ReMaira EscobarОценок пока нет
- 2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)Документ6 страниц2 - Adult Meningitis in A Setting of High HIV and TB Prevalence - Findings From 4961 Suspected Cases 2010 (Modelo para o Trabalho)SERGIO LOBATO FRANÇAОценок пока нет
- Chakra - Factors Associated With Complications of C DiffДокумент8 страницChakra - Factors Associated With Complications of C DiffCherry SmileОценок пока нет
- Jorgensen 2017Документ6 страницJorgensen 2017jessicapxeОценок пока нет
- Chronic Kidney Disease Is Associated With A Higher 90-Day Mortality Than Other Chronic Medical Conditions in Patients With SepsisДокумент8 страницChronic Kidney Disease Is Associated With A Higher 90-Day Mortality Than Other Chronic Medical Conditions in Patients With Sepsisida ayu agung WijayantiОценок пока нет
- Measures of Disease Frequency: Prevalence and IncidenceДокумент4 страницыMeasures of Disease Frequency: Prevalence and IncidenceVenia MursalimОценок пока нет
- Clinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalДокумент4 страницыClinical and Laboratory Characteristics of Pediatric Dengue Fever Patients in A Tertiary Care HospitalPratiwi UmbohОценок пока нет
- The Clinical Spectrum of Henoch - Schönlein Purpura in Children: A Single-Center StudyДокумент8 страницThe Clinical Spectrum of Henoch - Schönlein Purpura in Children: A Single-Center StudyDaniela PetricanОценок пока нет
- Community-Acquired Pneumonia Requiring Hospitalization Among U.S. AdultsДокумент13 страницCommunity-Acquired Pneumonia Requiring Hospitalization Among U.S. AdultsCindy De PataОценок пока нет
- The Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioДокумент7 страницThe Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioMaharaniОценок пока нет
- 10 1016@j Jaad 2019 05 096Документ8 страниц10 1016@j Jaad 2019 05 096JohnОценок пока нет
- Diabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyДокумент12 страницDiabetes With Hypertension As Risk Factors For Adult Dengue Hemorrhagic Fever in A Predominantly Dengue Serotype 2 Epidemic: A Case Control StudyDwitari Novalia HaraziОценок пока нет
- Immunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary ReportДокумент9 страницImmunogenicity of Fractional-Dose Vaccine During A Yellow Fever Outbreak - Preliminary Reportrizki agusmaiОценок пока нет
- A Novel Clinical Grading Scale To Guide The Management of Crusted ScabiesДокумент6 страницA Novel Clinical Grading Scale To Guide The Management of Crusted ScabiesFelisiana KasmanОценок пока нет
- Lepto SpirosДокумент8 страницLepto SpirosNisa UcilОценок пока нет
- Idsa GuidelinesДокумент34 страницыIdsa GuidelinesROSEN NОценок пока нет
- Mathur 2015Документ7 страницMathur 2015Maximiliano OliveraОценок пока нет
- Complicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023Документ4 страницыComplicaciones Neurológicas de Las Infecciones Por Rotavirus en Niños Ped Inf Dis 07 2023ANNIX FERRERОценок пока нет
- mdw557 2Документ7 страницmdw557 2mfaddhilОценок пока нет
- Tourniquet TestingДокумент6 страницTourniquet TestingPatrick RamosОценок пока нет
- Predictive Value of Proteinuria in Adult Dengue SeverityДокумент6 страницPredictive Value of Proteinuria in Adult Dengue SeverityWindy SuryaОценок пока нет
- Efficacy of Clinacanthus Nutans Extracts in PatientsДокумент7 страницEfficacy of Clinacanthus Nutans Extracts in Patientsconrad9richterОценок пока нет
- IDSA Nec FascДокумент34 страницыIDSA Nec FascShameen KhanОценок пока нет
- Diarrea en QuimioterapiaДокумент6 страницDiarrea en QuimioterapiaPaola DiazОценок пока нет
- 10.1007@s12098 020 03454 1Документ6 страниц10.1007@s12098 020 03454 1rayhantaswinОценок пока нет
- Management of Patients Suspected of Having Dengue FeverДокумент6 страницManagement of Patients Suspected of Having Dengue FeverRam Kripal MishraОценок пока нет
- Point-Of-Care Diagnostic Tests For Influenza in The Emergency DepartmentДокумент15 страницPoint-Of-Care Diagnostic Tests For Influenza in The Emergency DepartmentCristiano NogueiraОценок пока нет
- Menstrual Toxic Shock SyndromeДокумент9 страницMenstrual Toxic Shock SyndromeKristine MonicaОценок пока нет
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesДокумент11 страницEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidОценок пока нет
- Nej Mo A 0807381Документ12 страницNej Mo A 0807381Mildred MontОценок пока нет
- Maternal, Fetal, and Neonatal Outcomes in Pregnant Dengue Patients in MexicoДокумент8 страницMaternal, Fetal, and Neonatal Outcomes in Pregnant Dengue Patients in MexicoLola del carmen RojasОценок пока нет
- EA Davis,: E Coli, G Vaginalis) Salmo-Nella, Campylobacter) Streptococcus)Документ1 страницаEA Davis,: E Coli, G Vaginalis) Salmo-Nella, Campylobacter) Streptococcus)Khupe KafundaОценок пока нет
- Pi Is 1201971213002142Документ5 страницPi Is 1201971213002142melisaberlianОценок пока нет
- Community-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenДокумент11 страницCommunity-Acquired Pneumonia Requiring Hospitalization Among U.S. ChildrenHanida Rahmah TaminОценок пока нет
- Age-Related Differences in Hospitalization Rates, Clinical Presentation, and Outcomes Among Older Adults Hospitalized With Influenza-U.S. Influenza Hospitalization Surveillance NetworkДокумент8 страницAge-Related Differences in Hospitalization Rates, Clinical Presentation, and Outcomes Among Older Adults Hospitalized With Influenza-U.S. Influenza Hospitalization Surveillance NetworkTony RobertsОценок пока нет
- Lovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialДокумент9 страницLovastatin For The Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled TrialBpmStfbОценок пока нет
- Hospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionДокумент7 страницHospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionadhitiaОценок пока нет
- Mortality & Recurrent Seizure Risk After New-Onset Seizure in HIV-positive Zambian AdultsДокумент10 страницMortality & Recurrent Seizure Risk After New-Onset Seizure in HIV-positive Zambian AdultsAdam PrabataОценок пока нет
- Microbiological Evaluation of Nosocomial Infections by Using National Nosocomial Infection Surveillance (NNIS) SystemДокумент13 страницMicrobiological Evaluation of Nosocomial Infections by Using National Nosocomial Infection Surveillance (NNIS) SystemJanatinAzaОценок пока нет
- Effect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyДокумент4 страницыEffect of Prednisolone During Defervescence in Dengue Haemorrhagic Fever: An Open Label Controlled StudyFabiola StellaОценок пока нет
- Current Trends in The Epidemiologyof Nosocomial Bloodstream Infectionsin Patients With Hematological Malignanciesand Solid Neoplasms in Hospitalsin The United StatesДокумент8 страницCurrent Trends in The Epidemiologyof Nosocomial Bloodstream Infectionsin Patients With Hematological Malignanciesand Solid Neoplasms in Hospitalsin The United StatespaulaveronicaОценок пока нет
- Christensen 2020Документ11 страницChristensen 2020Francisco ChourioОценок пока нет
- Kumar 2006Документ8 страницKumar 2006aiturraldeОценок пока нет
- Jose Research v2Документ10 страницJose Research v2Jose Emmanuel FranciaОценок пока нет
- 6 - Iype2014Документ7 страниц6 - Iype2014Muhammad SyaifullahОценок пока нет
- Zhang 2019 Plos NTDДокумент20 страницZhang 2019 Plos NTDlibremdОценок пока нет
- Questions To Integrate A Gender Perspective Into Research CooperationДокумент3 страницыQuestions To Integrate A Gender Perspective Into Research CooperationlibremdОценок пока нет
- Cloete 2018 Scielo South AfricaДокумент10 страницCloete 2018 Scielo South AfricalibremdОценок пока нет
- Curriculum Vitae Ladson Hinton Personal Information: Lwhinton@ucdavis - EduДокумент34 страницыCurriculum Vitae Ladson Hinton Personal Information: Lwhinton@ucdavis - EdulibremdОценок пока нет
- Boukary 2012 Plos OneДокумент12 страницBoukary 2012 Plos OnelibremdОценок пока нет
- Tesis AlirezaДокумент98 страницTesis AlirezalibremdОценок пока нет
- Arnault 2008 Is There An Asian Idiom of Distress Somatic Symptoms in FemaleДокумент15 страницArnault 2008 Is There An Asian Idiom of Distress Somatic Symptoms in FemalelibremdОценок пока нет
- Multinomial Logistic Regression Basic RelationshipsДокумент73 страницыMultinomial Logistic Regression Basic RelationshipslibremdОценок пока нет
- No Woman Should Die Giving LifeДокумент112 страницNo Woman Should Die Giving LifelibremdОценок пока нет
- Nutrition Transition in 2 Lowland Bolivian Subsistence PopulationsДокумент13 страницNutrition Transition in 2 Lowland Bolivian Subsistence PopulationslibremdОценок пока нет
- Call For Abstracts Social Inequity in Health SymposiumДокумент1 страницаCall For Abstracts Social Inequity in Health SymposiumlibremdОценок пока нет
- QM 1 Schedule 2014-15 Final 0930 CambroДокумент2 страницыQM 1 Schedule 2014-15 Final 0930 CambrolibremdОценок пока нет
- Cineforum 2017: Director: Davis GuggenheimДокумент1 страницаCineforum 2017: Director: Davis GuggenheimlibremdОценок пока нет
- Clinical Dementia Rating Worksheet: Memory Questions For InformantДокумент10 страницClinical Dementia Rating Worksheet: Memory Questions For InformantlibremdОценок пока нет
- Welcomeletter Research Method and Philosophy November 2014Документ1 страницаWelcomeletter Research Method and Philosophy November 2014libremdОценок пока нет
- Fahetal2010 PDFДокумент10 страницFahetal2010 PDFlibremdОценок пока нет
- Abstract Book Leish World Congress 5Документ1 116 страницAbstract Book Leish World Congress 5libremdОценок пока нет
- Borang IshipДокумент9 страницBorang IshipUlfa RahayuОценок пока нет
- 5000L Series CatalogueДокумент24 страницы5000L Series CataloguekahlaouiОценок пока нет
- Assessing Health Impacts of Air Pollution From Electricity Generation The Case of ThailandДокумент22 страницыAssessing Health Impacts of Air Pollution From Electricity Generation The Case of Thailandcamilo_ortiz_6100% (1)
- Alumec 89 DatabladДокумент12 страницAlumec 89 DatabladMedoBoudyОценок пока нет
- 10 Suresh Nair - Journey ManagementДокумент25 страниц10 Suresh Nair - Journey ManagementMuhammad Zulkifli HarahapОценок пока нет
- Starbucks Managing High Growth BrandДокумент15 страницStarbucks Managing High Growth BrandSumit BansalОценок пока нет
- Week 5 UltrasoundДокумент26 страницWeek 5 UltrasoundNoor FarhanОценок пока нет
- Roth Conversion Strategies To ConsiderДокумент5 страницRoth Conversion Strategies To Considerkj4892Оценок пока нет
- Upstream Marine Standard IBU ChevronДокумент52 страницыUpstream Marine Standard IBU ChevronAndrew Hendy Indrakusuma50% (2)
- CUP 04 BOIN USA 02 WebДокумент2 страницыCUP 04 BOIN USA 02 WebMajid abdulОценок пока нет
- Brammer Standard Company, Inc.: Bs Su LAS-14Документ3 страницыBrammer Standard Company, Inc.: Bs Su LAS-14Ali MohsinОценок пока нет
- Unit 1 - 2Документ3 страницыUnit 1 - 2BahrouniОценок пока нет
- LabreportДокумент4 страницыLabreportDarwinys SamijonОценок пока нет
- Transcritical Co2 Refrigeration - PDFДокумент11 страницTranscritical Co2 Refrigeration - PDFHector Fabian Hernandez Algarra100% (1)
- Toyota/Lexus U140E/F, U240E, U241E: Click On Part Numbers For Product Details or VisitДокумент1 страницаToyota/Lexus U140E/F, U240E, U241E: Click On Part Numbers For Product Details or Visitvipper king2012Оценок пока нет
- Formatof Indenity BondДокумент2 страницыFormatof Indenity BondSudhir SinhaОценок пока нет
- Zuckerindustrie 139 (2) - 2014Документ9 страницZuckerindustrie 139 (2) - 2014Mateus RochaОценок пока нет
- People. Passion. Possibilities.: .30 .11 Thread Relief As RequiredДокумент40 страницPeople. Passion. Possibilities.: .30 .11 Thread Relief As RequiredFranciscoОценок пока нет
- United States Patent: (45) Date of Patent: Sep - 8, 2020Документ14 страницUnited States Patent: (45) Date of Patent: Sep - 8, 2020M FОценок пока нет
- LOTO-100 CompactoДокумент3 страницыLOTO-100 CompactoRyan KaneОценок пока нет
- Final - Urban and Transportation Engineering - PPT Group 1Документ19 страницFinal - Urban and Transportation Engineering - PPT Group 1JayChristian QuimsonОценок пока нет
- Section A: Jawab Semua SoalanДокумент3 страницыSection A: Jawab Semua SoalanAzreen IzetОценок пока нет
- RFOC Learner's Guide Page 1-212Документ240 страницRFOC Learner's Guide Page 1-212Travel GnrOneОценок пока нет
- Recent Advances in Natural Polymer-Based Drug Delivery SystemsДокумент18 страницRecent Advances in Natural Polymer-Based Drug Delivery SystemsTelmoОценок пока нет
- Metrel D.D. - Class A Power Quality AnalysersДокумент7 страницMetrel D.D. - Class A Power Quality AnalysersMonster LifeОценок пока нет
- Hydraulics A320Документ101 страницаHydraulics A320KamalVirk100% (6)
- More Evidence Confirms Diet's Link To Mental Health: Could An Apple A Day Really Keep Depression and Anxiety Away?Документ5 страницMore Evidence Confirms Diet's Link To Mental Health: Could An Apple A Day Really Keep Depression and Anxiety Away?psychologyconceptsОценок пока нет
- Sigma MP 102 (US) EN SdsДокумент9 страницSigma MP 102 (US) EN SdsEduardo GarzaОценок пока нет
- ScimagojrДокумент1 653 страницыScimagojrKomariah ErvitaОценок пока нет
- Sentence PatternДокумент2 страницыSentence PatternBrito RajОценок пока нет