Академический Документы
Профессиональный Документы
Культура Документы
The Properties of Chlorhexidine and Undesired Effects of Its Use in Endodontics
Загружено:
SoleyliLizbhetОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Properties of Chlorhexidine and Undesired Effects of Its Use in Endodontics
Загружено:
SoleyliLizbhetАвторское право:
Доступные форматы
Q U I N T E S S E N C E I N T E R N AT I O N A L
ENDODONTICS
Anarela Bernardi Cleonice Silveira
Teixeira
The properties of chlorhexidine and undesired effects
of its use in endodontics
Anarela Bernardi, DDS, MSc 1/Cleonice Silveira Teixeira, DDS, MSc, PhD 2
Objective: The purpose of this article was to review the litera- and genotoxicity that depend on the dose and exposed area.
ture on the properties of chlorhexidine (CHX) and the adverse There is scientific evidence showing the possibility of tooth
effects that may occur from its use in endodontics. In addition, staining and formation of brown precipitate when its use is
adverse effects that may result from its use, such as dark stain- associated with sodium hypochlorite. On the other hand, it is
ing of teeth, chemical interaction with sodium hypochlorite and not well established that its use interferes with the quality of
formed flocculate, biologic hazards, and interactions with the endodontic fillings. With respect to the biologic risks, the degra-
filling material were evaluated. Data Sources: Relevant publi- dation of CHX may generate para-chloroaniline and free radi-
cations on the use CHX in endodontics were thoroughly cals, which are harmful to the vital tissues. There is no
reviewed from the literature published between the years 2007 established consensus on the potential risk of CHX.
and 2014. Method and Materials: The authors conducted an Conclusion: The final considerations of this review will encour-
electronic search using the English language databases Medline age researchers to seek scientific evidence demonstrating the
and PubMed. Results: According to the reviewed studies, it safety of the use and applicability of CHX in endodontic therapy.
was concluded that CHX has proven antimicrobial activity, (Quintessence Int 2015;46:575–582; doi: 10.3290/j.qi.a33934)
excellent substantivity, low surface tension, and low cytotoxicity
Key words: chlorhexidine, endodontics, properties, root canal therapy
The chemomechanical preparation of root canals is a pulp and periapical tissues, have the ability to dissolve
crucial step for endodontic treatment, and it is impor- organic matter, and be able to lubricate the root
tant to use irrigating solutions that are associated with canals.2,3 Sodium hypochlorite (NaOCl) solution is most
endodontic instruments for cleaning, disinfecting, and commonly used during mechanical preparation, and its
shaping the root canal system, preparing them for the main advantages are its antimicrobial action, whitening
root filling treatment.1 effect, and power of dissolving organic tissue.4,5
The solution used as an irrigant during endodontic However, in teeth with pulp necrosis and chronic
treatment should be antimicrobial, biocompatible with periapical lesions, it is difficult to eliminate microorgan-
isms that remain in the root canal system, dentinal
tubules, apical external root surface, and apical peri-
1 Master, Postgraduate Program in Dentistry, Federal University of Santa Catarina,
Center for Health Sciences, Florianópolis, Santa Catarina, Brazil. odontium, even after the biomechanical preparation,
2 Professor, Department of Dentistry, Federal University of Santa Catarina, Center demonstrating the need to complement endodontic
for Health Sciences, Florianópolis, Santa Catarina, Brazil.
therapy with a root canal dressing.6
Correspondence: Dr Anarela Bernardi Vassen, Avenida Nossa Senhora Calcium hydroxide has commonly been used as a
da Conceição, 1725, sl 02, Bairro: Vila Betariz, Maracajá – SC, CEP 88915-
000, Brazil. Email: anarela.bernardi@hotmail.com root canal dressing. Though the use of this dressing is
VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015 575
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
widespread and accepted in endodontic practice, some CHX has interesting properties, among which the
microorganisms are resistant to its action.7,8 following can be highlighted.
Therefore, many drugs have been studied and
tested to supplement and/or potentiate its antimicro- Substantivity
bial effect. One of the various alternative irrigating solu- CHX digluconate is a broad spectrum antibacterial
tions and intracanal medications on the dental market agent with substantivity (Table 1), ie, it binds to the
is chlorhexidine (CHX). This drug is an effective antimi- hydroxyapatite of the enamel and dentin or anionic
crobial agent in the root canal that has potential for use groups of glycoproteins, is slowly released, and its con-
as an irrigant or intracanal medication. centration decreases in the middle, prolonging its anti-
Based on the above considerations, the purpose of bacterial effects for a long period of time.8,11-15 It has
this article was to review the literature on the properties been recommend that the substantivity property of
of CHX and its possible adverse effects during endodon- CHX should be harnessed in endodontics through its
tic use. In addition, some adverse effects that may result use as a final irrigant16 because its residual effect can
from its use are discussed, such as dark tooth staining, remain for up to 12 weeks.17 In another study, Souza et
chemical interaction with NaOCl and formed flocculate, al18 investigated the substantivity of CHX solution and
biologic hazards, and interaction with the filling material. gel within a system of canals for 24 hours, 30 days, and
90 days. The CHX solution showed a higher substantiv-
ity than CHX gel, except for groups incubated for 90
METHOD AND MATERIALS days. The results indicate that solution and gel chlor-
Relevant publications on the use CHX in endodontics hexidine are retained in the root dentin for 90 days.
were thoroughly reviewed from the literature pub-
lished between the years 2007 and 2014, using the
English language databases Medline and PubMed.
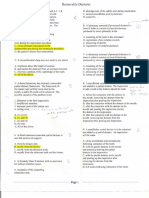
Table 1 Studies related to chlorhexidine regarding
substantivity and antimicrobial activity
PROPERTIES
Antimicrobial
Study Substantivity activity
CHX has been used as a therapeutic agent in several
Gomes et al8 X X
areas of dentistry, including periodontics, surgery, and
11
Rölla et al X
more recently endodontics. The mechanism of action
Komorowski et al12 X
of CHX can be explained by the chemical interaction
Basrani et al13 X
between this substance and bacterial cell membranes. 14
Soares et al X X
For a high dose (2%), the electrostatic binding between
Mohammadi and Abbott15 X X
their cationic molecules and negatively charged bac- Cook et al 16 X
terial cell wall causes CHX to exert a bactericidal action, Rosenthal et al17 X
resulting in precipitation and coagulation of cytoplas- Souza et al18 X
mic proteins, and, consequently, cell death. At lower Vaghela et al 19 X
doses (0.2%), the cell membrane integrity is altered, Mohammadi et al20 X
resulting in a bacteriostatic effect due to leakage of low Atila-Pektas et al 21 X
molecular weight bacterial components.9,10 Krithikadatta et al22 X
Because of its higher solubility, the salt of CHX diglu- Souza-Filho et al 23 X
conate is most commonly used in endodontic treatment, Delgado et al24 X
including as an irrigant during chemomechanical prepar- Lee et al25 X
30
Signoretti et al X
ation or as intracanal medication in cases of pulp necrosis.
576 VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
Antimicrobial activity not as efficient in removing or dissolving the bio-
Studies have shown that CHX has efficient antimicro- film,15,35,36 and it does not remove the smear layer.37
bial activity in endodontics,8,15,19 and that this effect can
be observed with both the use of CHX as irrigating Permeability interference in dentinal tubules
solution20 and as an intracanal medicament.21 The and root canal filling
action against resistant organisms, especially Enterococ- The use of CHX does not seem to hinder the sealing of
cus faecalis and Candida albicans, has been studied in the root canal filling in the apical region,38 and it does
detail.8,14,22,23 Some studies show better antimicrobial not affect the sealing ability in the root canal length as
activity of CHX alone compared to calcium hydroxide a whole.39 Another study found decreased apical seal-
[Ca(OH)2], especially against E faecalis.22-24 The use of a ing ability using AH Plus, Epiphany SE, and MM-Seal
polymeric device for the controlled release of CHX has when CHX was used as an irrigating solution.40 Homay-
also been shown to be more effective against E faecalis ouni et al41 reported that the presence of the precipi-
compared to the use of Ca(OH)2 paste.25 Other studies tate that is formed from the interaction between NaOCl
report that there is no difference in the reduction of and CHX has a negative effect on the sealing ability of
bacterial counts using an intracanal dressing of CHX gutta-percha and AH26 sealers.
because this reduction is already achieved in the first
session of biomechanical treatment using 2.5% NaOCl26 Cytotoxic effect
and 1.3% NaOCl.27 Interestingly, another study showed Several studies have shown that CHX may have cyto-
that the use of CHX as an irrigant during root canal toxic effects that increase with the concentration of the
preparation also appears to be sufficient for reducing solution.42,43 Moreover, because of its low toxicity, it has
the bacterial count, but there is no further significant been indicated for treating teeth with incomplete root
reduction from using a dressing of Ca(OH)2 mixed with formation or hypersensitivity to NaOCl.44 Another study
2% CHX.28,29 Several studies claim that CHX enhances reported that CHX does not alter cell viability or immu-
the antibacterial activity of residual Ca(OH)2.14,15,30 Sil- nostimulatory and anti-inflammatory properties.45 Pre-
veira et al31 reported that medications consisting of viously, Silva et al46 concluded that the addition of 0.4%
Ca(OH)2 and other drugs (camphorated paramonochlo- CHX to Calen paste allows for an adequate tissue
rophenol [CMCP], propylene glycol) perform better response, whereas Ca(OH)2 with 2% CHX has unsatisfac-
than when added to CHX, eliminating, in a short period tory results.
of time, Staphylococcus aureus and E faecalis.
Genotoxicity
Surface tension Studies have shown that the genotoxicity of CHX may
22,32
CHX has a low surface tension, providing faster be irrelevant.47,48 However, Yeung et al49 found that CHX,
propagation on the tooth surface, and allowing greater when associated with NaOCl or with Ca(OH)2, exhibits
flow of the drug into the root canal with a high pene- antioxidant and pro-oxidant reactions. Furthermore,
tration coefficient. This drug is an interesting option as Arabaci et al50 showed the dose-dependent genotoxic
a vehicle for Ca(OH)2.33 and cytotoxic effects of CHX on human lymphocytes in
vitro. In this way, when the chlorhexidine is extruded, in
Dissolution of organic tissue, biofilm, and high concentrations, to the periapical tissues, the poten-
smear layer tial genotoxic and tissue damage should be considered.
The literature has shown that the action of CHX depends Based on the results of the cytotoxicity and genotoxicity
on pH (it is most stable at a pH between 5 and 8) and its studies, it is worth noting that the use of CHX should be
activity is greatly reduced in the presence of organic restricted to the root canal space and care must be
matter.28 CHX does not dissolve organic tissues,15,34 it is taken with the choice of the concentrations used.
VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015 577
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
Figs 1a to 1c Endodontic
access cavities containing: CHX
(a), CHX and EDTA (b), and CHX
and NaOCl (c). The interaction
between EDTA and CHX causes
a white precipitate (b). The
interaction between CHX and
NaOCl results in the formation
of a precipitate with a dark
a b c amber color (c).
Table 2 Studies related to chlorhexidine regarding chemical interactions, degradation, and resulting metabolites
Study Chemical interactions of EDTA Chemical interactions of NaOCl CHX: Degradation pathway (PCA)
Mohammadi and Abbott15 X
González-López et al51 X
Rasimick et al29 X
52
Prado et al X X
Basrani et al53 X X
Bui et al54 X
Vianna and Gomes55 X
56
Marchesan et al X
Akisue et al57 X
Basrani et al58 X
Krishnamurthy and Sudhakaran59 X
60
Thomas and Sem X
Cintra et al61 X
Zong and Kirsch62 X
Barbin et al65 X
66
Barbin et al X
Havlíková et al67 X
WHO68 X
EC69 X
70
Alexander and Lustigman X
Kohlbecker71 X
EDTA, ethlyenediaminetetraacetic acid; PCA, para-chloroanaline.
Chemical interactions The mixing of 1% CHX with 17% ethylenediamine-
The use of chlorhexidine with other chemicals in end- tetraacetic acid (EDTA) instantly generates a highly
odontics may result in the formation of precipitates (Fig 1 insoluble solid precipitate, staining pink.51 However,
and Table 2). The formed precipitate is of clinical rele- Rasimick et al29 reported that this interaction between
vance with respect to the impairment of dental staining, EDTA and CHX causes a white precipitate and over 90%
interference with dentin permeability, effect on the diffu- of the precipitate mass is either EDTA or CHX, although
sion of intracanal dressing, and damage to the sealing of para-chloroaniline (PCA) is not detected. It was sug-
the root canal filling. Furthermore, some of the products gested that the precipitate is most likely a salt formed
formed from the interaction of chlorhexidine with other by the neutralization of the cationic ions of CHX. In
chemical substances may be harmful to host tissues. another study, Prado et al52 observed a milky white
578 VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
precipitate that formed after the association between DEGRADATION AND RESULTING
EDTA and CHX, and when combined with saline solu- METABOLITES
tion and ethanol, it produced a precipitated salt.
The interaction between CHX and NaOCl results in Zong and Kirsh62 studied the degradation pathway of
the formation of a precipitate with a dark amber color. CHX and concluded that under acidic conditions, CHX
Some studies have reported that higher levels of leads to the direct formation of PCA. Under alkaline
chloride in the NaOCl solution result in higher levels of conditions, CHX indirectly leads to the formation of
precipitate.53-61 Prado et al52 studied the byproducts PCA by forming p-chlorophenylurea.
formed by the associations between the irrigators that For dentistry, CHX degradation can occur through
are most commonly used in endodontic practice. CHX the action of NaOCl53,58,63,64 and Ca(OH)2 as well by the
produced an orange-brown precipitate when associ- temperature and storage time, which generate byprod-
ated with 1% to 5.25% NaOCl and an orange-white ucts (Table 2).65,66 It has been observed that CHX diglu-
precipitate when combined with 0.16% NaOCl. The conate alone decomposes into different products,
minimum concentration of NaOCl required for the for- including PCA.53,62,65,67 Due to their molecular structure
mation of the precipitate is 0.19%, and 0.023% for a and the high pH level of Ca(OH)2, when CHX is associ-
color change.54 The precipitate is flocculated and has ated with this drug, it can produce reactive oxygen
dimensions of approximately 250 nm, reducing the species and oxidative DNA. In this way, the use of CHX,
dentin permeability in the apical third.58 This precipi- mainly at higher concentrations, could result in a
tate generates an undesirable chromatic effect on the potential genotoxicity and tissue damage when it
dental crown.15,57 Furthermore, the precipitate forma- extrudes into the periradicular tissue during endodon-
tion has been related to tooth staining.55-58 Bui et al54 tic and periodontal procedures.49,65
also observed changes in the permeability of dentinal
tubules, which become more plugged in the cervical Para-chloroaniline (PCA)
and middle thirds of the canal. Several authors have PCA, CAS (registry number) no. 106-47-8, is a colorless
also observed higher precipitation levels in these loca- to slightly amber-colored crystalline solid with a mild
tions and suggest that this could affect the sealing of aromatic odor. The chemical is soluble in water and
the root canal filling.15,59 Cintra et al61 demonstrated, in common organic solvents.68
an in vivo study, that the precipitate has greater toxicity The general public may be exposed to PCA from the
than NaOCl or CHX alone. use of PCA-based dyed/printed textiles, papers, cosmet-
In order to prevent or remove the precipitate ics, and pharmaceutical products. Exposure can result
formed by the interaction of chlorhexidine with hypo- from residual PCA in the commercial product or from
chlorite, studies have been performed in the search for degradation of this product to PCA during use. It can be
a possible solvent.56,59 The use of acetic acid (vinegar) dermal (from wearing clothes and using soaps or
seemed to have a proven action on the dissolution of mouthwashes), oral (small children sucking on clothes
flocculate. However, this solvent did not remove the and other materials and the use of mouthwashes), or
brown color already established.56 Another option to from direct entry into the bloodstream (eg, through the
avoid or minimize the formation of the precipitate is breakdown products of CHX in spray antiseptics).
the use of irrigation in larger volumes of saline and From the use of CHX-containing mouthwashes, the
distilled water for dilution of NaOCl, and to irrigate with following oral and dermal (via mucous membrane)
absolute alcohol before using CHX as final irrigant.59 exposure concentrations can be estimated. In the Euro-
pean Union (EU), the maximum permitted level of CHX
in cosmetic products is 0.3%.69 According to a German
manufacturer, CHX contains < 500 mg PCA/kg,70 result-
VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015 579
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
ing in a maximum of approximately 1.5 mg PCA/L com- CONCLUSION
mercial CHX solution. PCA concentrations between 0.5
and 2.4 mg/L were detected in CHX preparations (CHX According to the studies reviewed, it can be concluded
content 0.2%). Assuming two mouthwashes per day that CHX:
with 10 mL of the CHX solution in each, the mucous • has antimicrobial activity, excellent substantivity,
membrane is exposed to between 10 and 48 μg of and low surface tension
PCA.71 Approximately 30% of CHX is retained in the oral • has cytotoxicity and genotoxicity that are dose-
cavity and approximately 4% is swallowed.72 Therefore, dependent and depend on the exposed contact area
uptake of PCA from mouthwash is from 50 to 255 ng/kg • does not dissolve organic tissue, biofilm, and smear
body weight (average body weight 64 kg).73 layers
According to the World Health Organization,74 there • could cause dental staining and the formation of a
are reports of severe methemoglobinemia in neonates brown precipitate when its use is associated with
from neonatal intensive care units in two countries in NaOCl
which premature babies were exposed to PCA as a • used in combination with hypochlorite, with a sol-
breakdown product of CHX; CHX, which had been inad- vent applied before or afterwards, may have
vertently used in the humidifying fluid, broke down to decreased formation of precipitate
PCA upon heating in a new type of incubator. Three • use during endodontic treatment is not well estab-
neonates in one report (14.5% to 43.5% methemoglobin) lished to interfere with the quality of the root canal
and 33 of 415 neonates in another report (6.5% to 45.5% filling
methemoglobin during the 8-month screening period) • use can cause degradation into CHX byproducts,
were found to be methemoglobin-positive. A prospec- such as PCA and free radicals, that are harmful to
tive clinical study showed that immaturity, severe illness, host tissues
time exposed to PCA, and low concentrations of NADH • use has unknown potential therapeutic risk in end-
reductase probably contributed to the condition. odontics.
CLINICAL RELEVANCE REFERENCES
1. Siqueira JF Jr, Guimarães-Pinto T, Roças IN. Effects of chemomechanical prep-
Any drug may simultaneously have positive and nega- aration with 2.5% sodium hypochlorite and intracanal medication with calci-
tive effects. Medicines from small, chemically produced um hydroxide on cultivable bacteria in infected root canals. J Endod
2007;33:800–805.
molecules may generate many residues when they 2. Zehnder M. Root canal irrigants. J Endod 2006;32:389–398.
degrade. In endodontics, the use of CHX has little scien- 3. Young GR, Parashos P, Messer HH. The principles of techniques for cleaning
root canals. Aust Dent J 2007;52:S52–S63.
tific evidence originated from in vivo studies, and a
4. Zehnder M, Kosicki D, Luder H, Sener B, Waltimo T. Tissue dissolving capacity
variety of in vitro studies provide conflicting results. and antibacterial effect of buffered and unbuffered hypochlorite solutions.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:756–762.
The substantivity characteristics and residual effect
5. Mohammadi Z. Sodium hypochlorite in endodontics: an update review. Int
(considered virtues) may even be a cause for concern Dent J 2008;58:329–341.
because they could keep CHX or its degradative 6. Nair, PN. On the causes of persistent apical periodontitis: a review. Int Endod
J 2006;39:249–281.
byproducts in the host tissues for a long period of time. 7. Evans M, Davies JK, Sundqvist G, Figdor D. Mechanisms involved in the resis-
The formation of PCA and free radicals has sparked tance of Enterococcus faecalis to calcium hydroxide. Int Endod J
2002;35:221–228.
many discussions in the literature. Consensus on the 8. Gomes BP, Vianna ME, Sena NT, Zaia AA, Ferraz CC, de Souza Filho FJ. In vitro
potential therapeutic risk has not been established. The evaluation of the antimicrobial activity of calcium hydroxide combined with
chlorhexidine gel used as intracanal medicament. Oral Surg Oral Med Oral
final considerations of this review encourage research- Pathol Oral Radiol Endod 2006;102:544–550.
ers to seek scientific evidence to prove the safety of 9. Davies A. The mode of action of chlorhexidine. J Periodontal Res 1993;12(Suppl
1):S68–S75.
their use and applicability in endodontic therapy.
580 VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
10. Athanassiadis B, Abbott PV, Walsh LJ. The use of calcium hydroxide, antibiot- 32. Taşman F, Cehreli ZC, Oğan C, Etikan I. Surface tension of root canal irrigants.
ics and biocides as antimicrobial medicaments in endodontics. Aust Dent J J Endod 2000;26:586–587.
2007;52:S64–S82. 33. Basrani B, Ghanem A, Tjäderhane L. Physical and chemical properties of chlor-
11. Rölla G, Löe H, Schiott CR. The affinity of chlorhexidine for hydroxyapatite and hexidine and calcium hydroxide-containing medications. J Endod
salivary mucins. J Periodontal Res 1970;5:90–95. 2004;30:413–417.
12. Komorowski R, Grad H, Wu XY, Friedman S. Antimicrobial substantivity of 34. Okino LA, Siqueira EL, Santos M, Bombana AC, Figueiredo JA. Dissolution of
chlorexidine treated bovine root dentin. J Endod 2000;26:315–317. pulp tissue by aqueous solution of chlorhexidine digluconate and chlorhexi-
13. Basrani B, Santos JM, Tjäderhane L, et al. Substantive antimicrobial activity in dine digluconate gel. Int Endod J 2004;37:38–41.
chlorhexidine-treated human root dentin. Oral Surg Oral Med Oral Pathol Oral 35. Chávez de Paz LE, Bergenholtz G, Svensäter G. The effects of antimicrobials on
Radiol Endod 2002;94:240–245. endodontic biofilm bacteria. J Endod 2010;36:70–77.
14. Soares JA, Leonardo MR, Tanomaru Filho M, Silva LA, Ito IY. Residual antibac- 36. Del Carpio-Perochena AE, Bramante CM, Duarte MA, et al. Biofilm dissolution
terial activity of chlorhexidine digluconate and camphorated p-monochloro- and cleaning ability of different irrigant solutions on intraorally infected den-
phenol in calcium hydroxide-based root canal dressings. Br Dent J tin. J Endod 2011;37:1134–1138.
2007;18:8–15. 37. Menezes AC, Zanet CG, Valera MC. Smear layer removal capacity of disinfec-
15. Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine tant solutions and without EDTA for the irrigation of canals: a SEM study.
in endodontics. Int Endod J 2009;42:288–302. Pesqui Odontol Br 2003;17:349–355.
16. Cook J, Nandakumar R, Fouad AF. Molecular- and culture-based comparison 38. Wuerch RM, Apicella MJ, Mines P, Yancich PJ, Pashley DH. Effect of 2% chlor-
of the effects of antimicrobial agents on bacterial survival in infected dentinal hexidine gel as an intracanal medication on the apical seal of the root-canal
tubules. J Endod 2007;33:690–692. system. J Endod 2004;30:788–791.
17. Rosenthal S, Spångberg L, Safavi K. Chlorhexidine substantivity in root canal 39. Kontakiotis EG, Tsatsoulis IN, Papanakou SI, Tzanetakis GN. Effect of 2% chlor-
dentin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:488–492. hexidine gel mixed with calcium hydroxide as an intracanal medication on
18. Souza M, Cecchin D, Farina AP, et al. Evaluation of chlorhexidine substantivity sealing ability of permanent root canal filling: a 6-month follow-up. J Endod
on human dentin: a chemical analysis. J Endod 2012;38:1249–1252. 2008;34:866–870.
19. Vaghela DJ, Kandaswamy D, Venkateshbabu N, Jamini N, Ganesh A. Disinfec- 40. Bodrumlu E, Parlak E, Bodrumlu EH. The effect of irrigation solutions on the
tion of dentinal tubules with two different formulations of calcium hydroxide apical sealing ability in different root canal sealers. Br Oral Res 2010;24:165–169.
as compared to 2% chlorhexidine: as intracanal medicaments against Entero- 41. Homayouni H, Majd NM, Zohrehei H, et al. The effect of root canal irrigation
coccus faecalis and Candida albicans: an in vitro study. J Conserv Dent with combination of sodium hypochlorite and chlorhexidine gluconate on
2011;14:182–186. the sealing ability of obturation materials. Open Dent J 2014 8:184–187.
20. Mohammadi Z, Giardino L, Palazzi F. Evaluation of the antifungal activity of 42. Souza LB, de Aquino SG, de Souza PP, Hebling J, Costa CA. Cytotoxic effects of
four solutions used as a final rinse in vitro. Aust Endod J 2013;39:31–34. different concentrations of chlorhexidine. Am J Dent 2007;20:400–404.
21. Atila-Pektaş B, Yurdakul P, Gülmez D, Görduysus O. Antimicrobial effects of 43. Lessa FC, Aranha AM, Nogueira I, Giro EM, Hebling J, Costa CA. Toxicity of
root canal medicaments against Enterococcus faecalis and Streptococcus chlorhexidine on odontoblast-like cells. J Appl Oral Sci 2010;18:50–58.
mutans. Int Endod J 2013;46:413–418. 44. Jeansonne MJ, White RR. Comparison of 2% chlorhexidine gluconate and
22. Krithikadatta J, Indira R, Dorothykalyani AL. Disinfection of dentinal tubules 5.25% sodium hypochlorite as antimicrobial endodontic irrigants. J Endod
with 2% chlorhexidine, 2% metronidazol, bioactive glass when compared with 1994;20:276–278.
calcium hydroxide as intracanal medicaments. J Endod 2007;33:1473–1476. 45. Silva RA, Leonardo MR, da Silva LA, Faccioli LH, de Medeiros AI. Effect of a
23. Souza-Filho FJ, Soares Ade J, Vianna ME, Zaia AA, Ferraz CC, Gomes BP. Anti- calcium hydroxide–based paste associated to chlorhexidine on RAW 264.7
microbial effect and pH of chlorhexidine gel and calcium hydroxide alone and macrophage cell line culture. Oral Surg Oral Med Oral Pathol Oral Radiol
associated with other materials. Br Dent J 2008;19:28–33. Endod 2008;106:e44–e51.
24. Delgado RJ, Gasparoto TH, Sipert CR, et al. Antimicrobial effects of calcium 46. Silva RA, Assed S, Nelson-Filho P, Silva LA, Consolaro A. Subcutaneous tissue
hydroxide and chlorhexidine on Enterococcus faecalis. J Endod response of isogenic mice to calcium hydroxide-based pastes with chlorhexi-
2010;36:1389–1393. dine. Braz Dent J 2009;20:99–106.
25. Lee Y, Han SH, Hong SH, Lee JK, Ji H, Kum KY. Antimicrobial efficacy of a 47. Hikiba H, Watanabe E, Barrett JC, Tsutsui T. Ability of fourteen chemical agents
polymeric chlorhexidine release device using in vitro model of Enterococcus used in dental practice to induce chromosome aberrations in Syrian hamster
faecalis dentinal tubule infection. J Endod 2008;34:855–858. embryo cells. J Pharmacol Sci 2005;97:146–152.
26. Paquette L, Legner M, Fillery ED, Friedman S. Antibacterial efficacy of chlor- 48. Ribeiro DA, Scolastici C, De Lima PL, Marques ME, Salvadori DM. Genotoxicity
hexidine gluconate intracanal medication in vivo. J Endod 2007;33:788–795. of antimicrobial endodontic compounds by single cell gel (comet) assay in
27. Malkhassian G, Manzur AJ, Legner M, et al. Antibacterial efficacy of MTAD final Chinese hamster ovary (CHO) cells. Oral Surg Oral Med Oral Pathol Oral Radiol
rinse and two percent chlorhexidine gel medication in teeth with apical Endod 2005;99:637–640.
periodontitis: a randomized double-blinded clinical trial. J Endod 49. Yeung SY, Huang CS, Chan CP, et al. Antioxidant and pro-oxidant properties
2009;35:1483–1490. of chlorhexidine and its interaction with calcium hydroxide solutions. Int
28. Wang CS, Arnold RR, Trope M, Teixeira FB. Clinical efficiency of 2% chlorhexi- Endod J 2007;40:837–844.
dine gel in reducing intracanal bacteria. J Endod 2007;33:1283–1289. 50. Arabaci T, Türkez H, Canakçi CF, Ozgöz M. Assessment of cytogenetic and
29. Rasimick BJ, Nekich M, Hladek MM, Musikant BL, Deutsch AS. Interaction cytotoxic effects of chlorhexidine digluconate on cultured human lympho-
between chlorhexidine digluconate and EDTA. J Endod 2008;34:1521–1523. cytes. Acta Odontol Scand 2013;71:1255–1260.
30. Signoretti FG, Gomes BP, Montagner F, Barrichello Tosello F, Jacinto RC. Influ- 51. González-López S, Camejo-Aguilar D, Sanchez-Sanchez P, Bolaños-Carmona
ence of 2% chlorhexidine gel on calcium hydroxide ionic dissociation and its V. Effect of CHX on the decalcifying effect of 10% citric acid, 20% citric acid, or
ability of reducing endotoxin. Oral Surg Oral Med Oral Pathol Oral Radiol 17% EDTA. J Endod 2006:32:781–784.
Endod 2011;111:653–658. 52. Prado M, Santos Júnior HM, Rezende CM, et al. Interactions between irrigants
31. Silveira CF, Cunha RS, Fontana CE, et al. Assessment of the antibacterial activ- commonly used in endodontic practice: a chemical analysis. J Endod
ity of calcium hydroxide combined with chlorhexidine paste and other intra- 2013;239:505-510.
canal medications against bacterial pathogens. Eur J Dent 2011;5:1–7. 53. Basrani BR, Manek S, Sodhi RN, Fillery E, Manzur A. Interaction between sodi-
um hypochlorite and chlorhexidine gluconate. J Endod 2007;33:966–969.
VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015 581
Q U I N T E S S E N C E I N T E R N AT I O N A L
Bernardi/Teixeira
54. Bui TB, Baumgartner JC, Mitchell JC. Evaluation of the interaction between 65. Barbin LE, Saquy PC, Guedes DF, Sousa-Neto MD, Estrela C, Pécora JD. Determi-
sodium hypochlorite and chlorhexidine gluconate and its effect on root nation of para-chloroaniline and reactive oxygen species in chlorhexidine and
dentin. J Endod 2008;34:181–185. chlorhexidine associated with calcium hydroxide. J Endod 2008;34:1508–1514.
55. Vianna ME, Gomes BP. Efficacy of sodium hypochlorite combined with chlor- 66. Barbin LE, Estrela C, Guedes DF, Spanó JC, Sousa-Neto MD, Pécora JD. Detec-
hexidine against Enterococcus faecalis in vitro. Oral Surg Oral Med Oral tion of para-chloroaniline, reactive oxygen species, and 1-chloro-4-itroben-
Pathol Oral Radiol Endod 2009;10:585–589. zene in high concentrations of chlorhexidine and in a mixture of chlorhexidine
56. Marchesan MA, Pasternak Júnior B, Afonso MM, Sousa-Neto MD, Paschoalato and calcium hydroxide. J Endod 2013;39:664–668.
C. Chemical analysis of the flocculate formed by the association of sodium 67. Havlíková L, Matysová L, Nováková L, Hájková R, Solich P. HPLC determination
hypochlorite and chlorhexidine. Oral Surg Oral Med Oral Pathol Oral Radiol of chlorhexidine gluconate and p-chloroaniline in topical ointment .J Pharm
Endod 2007;103:e103–e105. Biomed Anal 2007;43:1169–1173.
57. Akisue E, Tomita VS, Gavini G, Poli de Figueiredo JA. Effect of the combination 68. World Health Organization. International Agency for Research on Cancer:
of sodium hypochlorite and chlorhexidine on dentinal permeability and scan- Monographs on the Evaluation of Carcinogenic Risks to Humans—Occupa-
ning electron microscopy precipitate observation. J Endod 2010;36:847–850. tional Exposures of Hairdressers and Barbers and Personal Use of Hair Colou-
58. Basrani BR, Manek S, Mathers D, Fillery E, Sodhi RN. Determination of 4-chlo- rants; Some Hair Dyes, Cosmetic Colourants, Industrial Dyestuffs and
roaniline and its derivatives formed in the interaction of sodium hypochlorite Aromatic Amines. Lyon: International Agency for Research on Cancer,
and chlorhexidine by using gas chromatography. J Endod 2010;36:312–314. 1993:1–436.
59. Krishnamurthy S, Sudhakaran S. Evaluation and prevention of the precipitate 69. EC. Cosmetics legislation. Cosmetic products. Brussels: European Commis-
formed on interaction between sodium hypochlorite and chlorhexidine. J sion, DG III Enterprise, 2003.
Endod 2010;36:1154–1157. 70. Alexander M, Lustigman BK. Effect of chemical structure on microbial degra-
60. Thomas JE, Sem DS. An in vitro spectroscopic analysis to determine whether dation of substituted benzenes. J Agric Food Chem 1966;14:410–413.
para-chloroaniline is produced from mixing sodium hypochlorite and chlor- 71. Kohlbecker G. Toxic impurities in chlorhexidine digluconate. Deutsch Zahnar-
hexidine. J Endod 2010;36:315–317. ztl Z 1989;44:273–276.
61. Cintra LT, Watanabe S, Samuel RO, et al. The use of NaOCl in combination 72. Bonesvoll P, Lökken P, Rölla G, Paus PN. Retention of chlorhexidine in the
with CHX produces cytotoxic product. Clin Oral Investig 2014;18:935–940. human oral cavity after mouth rinses. Arch Oral Biol 1974;19:209–212.
62. Zong Z, Kirsch LE. Studies on the instability of chlorhexidine, part I: kinetics 73. IPCS. Assessing human health risks of chemicals. Derivation of guidance val-
and mechanisms. J Pharm Sci 2012;101:2417–2427. ues for health-based exposure limits. Geneva: World Health Organization,
63. Basrani BR, Manek S, Fillery E. Using diazotization to characterize the effect of International Programme on Chemical Safety (Environmental Health Criteria
heat or sodium hypochlorite on 2.0% chlorhexidine. J Endod 2009;35:1296– 170), 1994.
1299. 74. World Health Organization. Concise international chemical assessment docu-
64. Kim HS, Zhu Q, Baek SH, et al. Chemical interaction of alexidine and sodium ment (No 48): 4-Chloroaniline (2003). Geneva: WHO, 2003:1–56.
hypochlorite. J Endod 2012;38:112–116.
582 VOLUME 46 • NUMBER 7 • JULY/AUGUST 2015
Copyright of Quintessence International is the property of Quintessence Publishing Company
Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv
without the copyright holder's express written permission. However, users may print,
download, or email articles for individual use.
Вам также может понравиться
- Ot Equator Prosthetic: Fixed and Removable DentistryДокумент36 страницOt Equator Prosthetic: Fixed and Removable Dentistryvaleriu vatamanОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Endodontic MishapsДокумент199 страницEndodontic Mishapsrasagna reddy100% (4)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- الملف الذهبي ٢ Cerrected by Yes We Can 2021Документ41 страницаالملف الذهبي ٢ Cerrected by Yes We Can 2021linahouhouОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Phonological Analysis Between Swedish and EnglishДокумент11 страницPhonological Analysis Between Swedish and EnglishJeedu AlotaibiОценок пока нет
- Mouth Breathing I. Etiology and EffectsДокумент16 страницMouth Breathing I. Etiology and EffectsRommy MelgarejoОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Unioeste 2012 2. Mackenzie 2003Документ3 страницыUnioeste 2012 2. Mackenzie 2003Vítor S. SilvaОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Chapter 3Документ7 страницChapter 3Thanh TúОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- H BIRN + WINTHER - Oral Minor Surgery (Compressed)Документ131 страницаH BIRN + WINTHER - Oral Minor Surgery (Compressed)Dr. Mahmoud Tawfik ElSorady100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Assessment of Facial Landmarks For Bone Asymmetry in Geometric Morphometric Studies: A Systematic ReviewДокумент20 страницAssessment of Facial Landmarks For Bone Asymmetry in Geometric Morphometric Studies: A Systematic ReviewIvan GalicОценок пока нет
- Dental Caries - SravanДокумент18 страницDental Caries - Sravan12C29 SRAVAN VSОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- 4 RemovableДокумент17 страниц4 Removableay daОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Manual ItДокумент28 страницManual ItJesús Torres YauriОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Saudi Licence Exam For General DentistДокумент159 страницSaudi Licence Exam For General DentistYounus Shaik91% (124)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Hajara Farzeen - Apex Locator (F)Документ3 страницыHajara Farzeen - Apex Locator (F)A ZainОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Lip Enhancement: Physical Assessment, Injection Techniques, and Potential Adverse EventsДокумент10 страницLip Enhancement: Physical Assessment, Injection Techniques, and Potential Adverse EventsFaragau TeodoraОценок пока нет
- MODUL PRAKTEK Dental MaterialДокумент11 страницMODUL PRAKTEK Dental MaterialPutri Amalia MahsunОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Clinician's Guide To The Diagnosis Tooth Sensitivity (Taha 2014) HD DRG - PituДокумент112 страницClinician's Guide To The Diagnosis Tooth Sensitivity (Taha 2014) HD DRG - PituJesicaОценок пока нет
- Post-Operative Complications of Periodontal SurgeryДокумент2 страницыPost-Operative Complications of Periodontal SurgeryReshmaa RajendranОценок пока нет
- Gic PPTДокумент75 страницGic PPT71. Karan SatykiОценок пока нет
- The Bathroom Personal Hygiene VerbsДокумент1 страницаThe Bathroom Personal Hygiene Verbsmargarita100% (2)
- Post Insertion Problem and Its ManagmentДокумент108 страницPost Insertion Problem and Its Managmentranjeet kumar chaudharyОценок пока нет
- Treatment Planning of The Edentulous Maxilla PDFДокумент17 страницTreatment Planning of The Edentulous Maxilla PDFAmy CuadraОценок пока нет
- Smiles 3 Mod Test 3BДокумент5 страницSmiles 3 Mod Test 3BBiljana Nestorovska0% (1)
- Oral Lec 8Документ9 страницOral Lec 8Adam AliraqiОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- MIS V3 CatalogДокумент28 страницMIS V3 CatalogJorge SaenzОценок пока нет
- SOP Management of Periodontal Conditions in Primary Settings Final Approved PK (KP)Документ15 страницSOP Management of Periodontal Conditions in Primary Settings Final Approved PK (KP)Afiqah Binti Muhamed FaizalОценок пока нет
- Class V Cavity PreparationДокумент1 страницаClass V Cavity PreparationALI abd-alamamОценок пока нет
- Retention of Removable Complete Dentures Made With Different Posterior Palatal Seal Techniques and Oral Health Quality of Life: A Clinical StudyДокумент5 страницRetention of Removable Complete Dentures Made With Different Posterior Palatal Seal Techniques and Oral Health Quality of Life: A Clinical StudyZachary DuongОценок пока нет
- SDCEP Oral Health Management of Patients at Risk of MRONJ Guidance in BriefДокумент6 страницSDCEP Oral Health Management of Patients at Risk of MRONJ Guidance in BriefLupu AndreeaОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Mod 1.2 Musculoskeletal System UpdatedДокумент26 страницMod 1.2 Musculoskeletal System UpdatedNandhkishoreОценок пока нет