Академический Документы
Профессиональный Документы
Культура Документы
Anti-Malerials Materials
Загружено:
raj royelАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Anti-Malerials Materials
Загружено:
raj royelАвторское право:
Доступные форматы
BASICS OF MALARIA
• Malaria: ‘Mal’ + ‘Aria’ = Bad or Poisonous air.
• Malaria is a mosquito-borne infectious disease affecting humans and other animals
caused by parasitic protozoans (a group of single-celled microorganisms) belonging to
the Plasmodium type.
• Main four species of plasmodia infect humans:
o Plasmodium vivex
o Plasmodium falciparum
o Plasmodium ovale
o Plasmodium malariae
• P.falciparum infection can lead to capillary obstruction and death if treatment is not
instituted promptly. P.vivex causes milder form of the disease. P.malariae is common to
many tropical regions, but P.ovale is rarely encountered.
• Malaria causes symptoms that typically include fever, tiredness, vomiting,
and headaches. In severe cases it can cause yellow skin, seizures, coma, or death.
Symptoms usually begin ten to fifteen days after being bitten.
• The insect vectors are the female anopheles female mosquito which breeds in stagnant
water.
• According to World Health Organization (WHO), Malaria is a significant public health
problem in more than 90 countries inhabited by some 2400 million people (about 40%
of the world’s population).
• The disease causes an estimated 300 million acute illness acute illness each year and at
least 1 million deaths.
• More than 90% of these occur in sub-Saharan Africa, and it is estimated that the disease
kills an African child every 30 seconds. Even those who survive may suffer lasting mental
impairment.
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 1
LIFE CYCLE OF MALARIAL PARASITE
Figure-1: Life cycle of malarial parasite with different stages
• The mosquito, not the human, is the definitive host for plasmodia, and it has been said
that the only function of human is to enable the parasite to infect more mosquitoes so
that further sexual recombination occur.
• The life cycle of the parasite consist of a sexual cycle, which take place in female
anopheles mosquito, and an asexual cycle, which occurs in humans.
• When an infected mosquito bites, it injects plasmodium sporozoites into the blood
stream. The sporozoites migrate through the blood to the liver, where they form cyst-like
structures contains thousands of merozoites.
• Schizonts (the pre-erythrocytic stage), which liberate merozoites: these infect red blood
cells, forming motile trophozoites, using haemoglobin as a nutrient, which after
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 2
development, release another batch of erythrocyte-infecting merozoites , causing fever,
this constitutes the erythrocyte cycle.
• Dormant hypnozoites, which may liberate merozoites later (the exoerythrocytic stage)
• Eventually, the infected cell ruptures, releasing heam and merozoites that can enter other
erythrocyte.
• Alternatively, released merozoites can become gametocytes, which are picked up by
mosquitoes from the blood they ingest, the cycle thus begins again. The gametocyte
becomes sporozoites in the insect
Figure-2: The life cycle of malarial parasite (P.falsiparum) showing the sites of action
of anti malarial drugs
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 3
ADVANCED THERAPY FOR MALARIA:
• The best way to deal with Malaria is to avoid the disease in the first place by mosquito
bites.
• Some drugs can be used prophylactically to prevent malaria, while others are directed
towards treating acute attacks.
• In general, Malarial drugs are classified in terms of the action against the different stages
of life cycle of the parasite.
1) Blood Schizonticidal agents
• Blood schizonticidal agents are used to treat acute attacks, they are also known as drugs
that produce a ‘suppressive’ or ‘clinical’ cure.
• They act on the erythrocytic forms of the plasmodium
• Drugs :
o Quinoline-methanols: (Quinine, Mefloquine)
o 4-aminoquinolones: (Chloroquine)
o Phenanthrene: (Halofantrine)
o Interfere with folate synthasis: (Pyrimethamine, Proguanil)
o Hydroxy naphthoquinone compound: (Atovaquone)
o Compounds derived from quinghaosu: (Artemether, Artesunate, Arteflene)
2) Chemoprophylaxis
• Drugs used for chemoprophylaxis block the link between exoerythrocytic stage and
erythrocytic stage, Thus, prevent the development of malarial attacks
• Prevention of infection by killing of sporozoites on entry into the host.
• Drugs :
o Chloroquine, Mefloquine Proguanil, pyrimethamine, Dapsone and Doxycycline
3) Curative-suppressive therapy
• Useful after observing malarial symptomes
• Drugs :
o Chloroquine, Quinine, Artether, Atovaquone, Lumifantrine
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 4
4) Radical cure therapy
• These agents affect a ‘radical’ (striking root of infection) cure by acting on the parasites
in the liver. They destroy gametocytes, thus reduce the spread of infection.
• Only 8-aminoquinolones have this action.
• Drugs :
o Primaquine, tafenoquine
5) Folate antagonists
• They inhibit Dihydrofolate reductase.
• Drugs :
o Pyrimethamine, Proguanil, Sulfadoxine, Dapsone
6) Gameticidals
• These drugs destroy the sexual forms of the parasite in the blood and thereby prevent
transmission of the infection to the mosquito.
• Chloroquine and quinine have gametocytocidal activity against P. vivax and P. malariae,
but not against P. falciparum. Primaquine has gametocytocidal activity against all
plasmodia, including P. falciparum.
• Drugs :
o Artemisinin, Primaquine, Trimethoprim, Chloroquine
7) Sporonticidals
• These drug prevent development of oocysts in the mosquito and thus ablate the
transmission
• Drugs :
o Dihydrofolate reductase Primaquine, Chloroguanide,
8) Curcumin-Artemisinin Combination Therapy
• Artemisinin and curcumin show an additive interaction in killing Plasmodium falciparum
in culture.
• curcumin isolated from the roots of Curcuma longa (turmeric) has antimalarial activity
preventing recrudescence due to artemisinin
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 5
• In vivo, 3 oral doses of curcumin following a single injection of ALPHA AND BETA
arteether
• Artemisinin and curcumin (98% curcuminoid content)
9) Aminoacyl-tRNA Synthetase Inhibitors
• Drug : Mupirocin, Borrelidin
• Mechanism of mupirocin inhibition. Mupirocin is a natural product of Pseudomonas
fluorescens and is the only commercially available antibiotic that inhibits bacterial AaRS
Borrelidin which is lethal to P. yoelii murine malaria.
10)Proline‑tRNA synthetase Inibitors
• Drug : Febrifugin, Halofiginone
• It is Chinese herb derived molecule, which is highly efficient inhibitors of malarial
parasite growth
• It targets both asymptomatic liver stage and blood stages of plasmodium parasite.
• THE cytoplasmic copy of ProRS gene from malarial parasite was identified as the specific
target for these molecules.
11)Malarial vaccines
• P.falciparum genome vaccine
• Blood stage vaccines: MSP1, AMA1, MSP3, GLURP
• Pf RH5
• RTS,S/AS01
• Whole organism vaccine(Full length recombinant Plasmodium falciparum protein)
• Transmission blocking vaccines
12) Combination Therapy
• Sulpha drugs: (Sulphadoxine + pyrimethamine)
• Artemisinin + Lumifantrine (Chloroquine resistant Malaria)
• Artemisinin + Chloroquine (To increase the effectiveness of therapy)
• Biguanide derivatives: (Proguanil + Atovaquone mixture)
13) Drugs obtained from natural sources and terpenoids
o Artemisinin, Artemether, Arteether, Artesunate
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 6
14) Cytokine based therapy
• The relationship between host and parasite is determined largely by host cytokines
and as more understanding of the role of cytokines is gained, the possibility of utilizing
this for therapy is being studied.
• Agents being considered include peptide antagonists at cytokine receptors, soluble
cytokine receptors, anti-cytokine antibodies and mutant cytokines.
• IL-2 has been shown to protect monkeys against malaria
2.4 DETAILED NOTE ON SOME IMPORTANT ANTI-MALARIAL DRUGS:
(1) CHLOROQUINE
• Blood schizonticidal agent that is used to treat acute
attacks, they are also known as drugs that produce a
‘suppressive’ or ‘clinical’ cure.
• They act on the erythrocytic forms of the plasmodium.
Mechanism:1 (Assumption):
Figure-3: Famous formulation of
chloroquine (Lariago-DS)
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 7
Mechanism: 2 (Actual Mechanism):
Resistance Mechanism:
• Plasmodium falciparum is now resistance to chloroquine is most parts of the world.
• Resistance appears to result from Effulx pump development and it efflux out the drug
from the paracitic vesicle as a result of mutations in plasmodia transporter genes.
Pharmacokinetic aspects:
• Absorbed: After oral administration
• Distribution: Concentrate in Erythrocyte, spleen, Kidney, Lungs also, penetrate CNS and
travels through placenta.
• Metabolism: Dealkylated by hepatic oxidase system.
• Excretion: in urine (70% unchanged, 30% Metabolite)
• Half life: 50 hours
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 8
Therapeutic uses:
• Anti-Malarial (Safest during pregnancy)
• Rheumatoid arthritis
• Amoebicidal agent
• Quinine like effect: useful in arrythmia
Adverse effect:
• Nausea, Vomiting, Headache
• Dizziness
• Blurring vision
• Fatal dysrhythmia (High dose)
(2) QUININE
• Quinine and its isomer Quinidine are blood Schizonticidal agent, useful for malarial strain
that is resistant to Chloroquine.
• Obtained from cinchona bark.
Mechanism: 1 (Just like chloroquine)
Also,
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 9
Mechanism: 2
Also,
Mechanism: 3
Also,
Mechanism: 4
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 10
Therapeutic uses:
• Cerebral Malaria
• Ecbolic agent
Adverse effect:
• Black water urine
• Cinchonism (Ringing of Ear, Blurred vision, Headache)
• Vertigo
• Ototoxicity
• Contraindicated in pregnancy (Ecbolic action, Premature baby birth/Abortion)
(3) 8-AMINOQUINOLINES
• The only 8-aminoquinoline licensed for current use Primaquine.
• Etaquine and Tafenoquine are more active and slowly metabolised analogues of
primaquine.
• This class of drug is extended against liver hypnozoites and they can effect a radical cure
of those form of malaria in which the parasites have a dormant stage in liver-P.vivex and
P.ovale
• It has a gametocidal action and it is most effective anti-Malarial drug for preventing
transmission of the disease.
Mechanism:
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 11
Pharmacokinetic aspects:
• Given orally and is well absorbed.
• Its metabolism is rapid and very little drug is present in the body after 10-12 hours.
• Half life is 3-6 hours,
Adverse effect:
• It causes haemolysis in individual with and X chromosome-linked genetic metabolic
condition: G6PD deficiency (Glucose-6-phosphate dehydrogenase deficiency) in Red
cells.
• So, Red cells are not able to regenerate NADPH, Its concentration being reduced by
oxidant metabolic derivative of primaquine.
• As a result, Function of red cells are impaired and haemolysis occurred.
(4) QINGHAOSU (ARTEMESININ) AND RELATED COMPOUNDS
• The qinghaosu based compounds are derived from the herb qing hao, a tradition Chinese
remedy for malaria.
• Artemisinin, a poorly soluble chemical extract from Artemisia a fast acting blood
Schizonticide effective in treating acute attack of malaria.
• Artesunate, a water soluble derivative and synthetic analogues artemether and
artether have higher activity and better absorbtion.
• Artemisinin and derivative compounds are effective against multi drug resistant
P.falciparum
Mechanism:
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 12
Adverse effect:
• Transient Heart block
• Decreasing in Neutrophil count
• Episodes of fever
• According to animal study, artemisinin shows cause unusual injury to brain stem.
Combinations
• Artemisinin + Lumifantrine (Chloroquine resistant malaria)
• Artemisinin + Chloroquine (increase effectiveness of the therapy)
• Never give combination of artemisinin with sulpha drug due to antagonistic action
(5) FOLATE ANTAGONISTS
• Folate antagonists inhibit Dihydrofolate reductase.
• Pyrimethamine is having similar structure to trimethoprim
• Abnormal folic acid formed. due to that Protein synthesis in parasite stop.
• Drugs: Sulphamethoxazole, Sulfadoxime, proguanil, pyrimethamine, Dapsone
Mechanism:
ANTI-MALARIAL AGENTS – JINAL ADHIYA – M.PHARM (PHARMACOLOGY) 13
Вам также может понравиться
- Anti Malarial AgentsДокумент98 страницAnti Malarial AgentswasimaОценок пока нет
- Pha 402 AntimalarialДокумент22 страницыPha 402 AntimalarialTemitopeОценок пока нет
- Malaria Cycle and Antimalarials PDFДокумент22 страницыMalaria Cycle and Antimalarials PDFPreeti YadavОценок пока нет
- Unit 2 (C) Anti-Malarials, Educational PlatformДокумент50 страницUnit 2 (C) Anti-Malarials, Educational PlatformIzazОценок пока нет
- Anti-Parasitic: Anti-Inflammatory and Anti-Infective Agents: Mechanism of Drug ActionДокумент12 страницAnti-Parasitic: Anti-Inflammatory and Anti-Infective Agents: Mechanism of Drug ActionMIKAELA DAVIDОценок пока нет
- Antimalarial DrugsДокумент45 страницAntimalarial DrugsDeribe BekeleОценок пока нет
- Antimalarial Drug CologyДокумент15 страницAntimalarial Drug CologyManthan ChauhanОценок пока нет
- Chapter - Iii Antimalarial, Antiprotozoal and Anthelmintic DrugsДокумент28 страницChapter - Iii Antimalarial, Antiprotozoal and Anthelmintic DrugsNEHA DIXITОценок пока нет
- Antiprotozoa MedicineДокумент10 страницAntiprotozoa MedicineWaldian IsmailОценок пока нет
- Anti Malarial Drugs 1Документ87 страницAnti Malarial Drugs 1F ParikhОценок пока нет
- MalariaДокумент61 страницаMalariaEscitalopram 5mgОценок пока нет
- Pharmacology-Unit-III (F) AntimalarialdrugsДокумент59 страницPharmacology-Unit-III (F) Antimalarialdrugswebpixel services100% (1)
- Anti Malaria¡Документ107 страницAnti Malaria¡makioedesemiОценок пока нет
- Afb5 - 1. Antimalarials MedicalДокумент63 страницыAfb5 - 1. Antimalarials MedicalAx D98Оценок пока нет
- Health Care Assistant PharmacologyДокумент16 страницHealth Care Assistant PharmacologyImmelda Stella Medessoh DohoОценок пока нет
- Anti Malarial DrugsДокумент107 страницAnti Malarial DrugsSindile MchunuОценок пока нет
- Farmakologi 4 (Antimalaria)Документ7 страницFarmakologi 4 (Antimalaria)Gifanichan MvpshawolandromedaОценок пока нет
- Antimalarial DrugsДокумент33 страницыAntimalarial DrugsPinakin Dhirajlal Jadav100% (1)
- Antiparasitic Drugs (Antiprotozoal: DR John EgbagbaДокумент37 страницAntiparasitic Drugs (Antiprotozoal: DR John EgbagbaPrincewill SeiyefaОценок пока нет
- Anti Protozoal P1Документ5 страницAnti Protozoal P1N Gv FcОценок пока нет
- Antimalarial Drugs 1AДокумент49 страницAntimalarial Drugs 1Apallavi DiwareОценок пока нет
- Farmakologi AntiprotozoaДокумент32 страницыFarmakologi AntiprotozoatriyantiОценок пока нет
- Anti MalariaДокумент28 страницAnti MalariaselviaОценок пока нет
- Drug TransplantationДокумент36 страницDrug Transplantationsajad abasewОценок пока нет
- Antiprotozoal DrugsДокумент37 страницAntiprotozoal DrugsMoneto CasaganОценок пока нет
- Antiprotozoal Drugs NotesДокумент22 страницыAntiprotozoal Drugs NotesMae Lislie Canonigo - FloresОценок пока нет
- Anti-Malarials and Drug Treatment of MalariaДокумент38 страницAnti-Malarials and Drug Treatment of MalariaIgbashioОценок пока нет
- Antiprotozoal Drugs: Blood and Tissue ProtozoaДокумент12 страницAntiprotozoal Drugs: Blood and Tissue ProtozoaStefan HutsonОценок пока нет
- Antimalarial DrugsДокумент56 страницAntimalarial DrugsKasturiRangan SrivatsaОценок пока нет
- Unit 1b. AntihelminthicsДокумент71 страницаUnit 1b. AntihelminthicsDerrick SHEMAОценок пока нет
- Anti Malarial AgentsДокумент23 страницыAnti Malarial AgentsJia YingОценок пока нет
- Anti Malarial Drugs by Salaria AnamikaДокумент10 страницAnti Malarial Drugs by Salaria AnamikaSalaria Anamika100% (1)
- ANTIMALARIAL DrugsДокумент25 страницANTIMALARIAL DrugsMANAS ChhapoliyaОценок пока нет
- 12 MalariaДокумент61 страница12 MalariaMewael TesfamichaelОценок пока нет
- Antimalarial DrugsДокумент28 страницAntimalarial DrugsJane Pearson100% (1)
- 19-Antiprotozoal Drugs IIДокумент37 страниц19-Antiprotozoal Drugs IIShashidharan MenonОценок пока нет
- Antimalarial DrugsДокумент19 страницAntimalarial Drugspallavi DiwareОценок пока нет
- Antiparasitic DrugsДокумент60 страницAntiparasitic DrugsMaxamed Faarax XaashiОценок пока нет
- Antimalarial, Antiprotozoal, and Antihelmintic AgentsДокумент37 страницAntimalarial, Antiprotozoal, and Antihelmintic AgentsQuolette ConstanteОценок пока нет
- Anti-Malarial DrugsДокумент58 страницAnti-Malarial Drugs88AKKОценок пока нет
- Antimalarials DrugsДокумент27 страницAntimalarials DrugsAlishba MushtaqОценок пока нет
- SESSION 8 - Anti-Malaria DrugsДокумент48 страницSESSION 8 - Anti-Malaria DrugsYassboy MsdОценок пока нет
- Antiprotozoal Drugs: Blood and Tissue ProtozoaДокумент12 страницAntiprotozoal Drugs: Blood and Tissue ProtozoaLuciano Rodrigues SimoesОценок пока нет
- Anti ProtozoaДокумент29 страницAnti ProtozoaIsheanesu MugwisiОценок пока нет
- GROUP A1 (A) Topic 5Документ37 страницGROUP A1 (A) Topic 5KhaiОценок пока нет
- Antibiotics/Anti-infective: Classes of Drugs That Act As Anti-InfectivesДокумент6 страницAntibiotics/Anti-infective: Classes of Drugs That Act As Anti-InfectivesJL D. BusiaОценок пока нет
- Antimalarial DrugsДокумент49 страницAntimalarial DrugsMalueth Angui0% (1)
- Malaria + Treatment + PreventionДокумент9 страницMalaria + Treatment + PreventionAmedeus FelixОценок пока нет
- Malaria: Michael Aguilar, RMTДокумент27 страницMalaria: Michael Aguilar, RMTFrankenstein MelancholyОценок пока нет
- Antiprotozoal DrugsДокумент46 страницAntiprotozoal DrugsKrupasagar Pn PalegarОценок пока нет
- Antiprotozoals Part IДокумент46 страницAntiprotozoals Part IAYO NELSONОценок пока нет
- Pharmacology of AntimalarialsДокумент39 страницPharmacology of AntimalarialsAntonyОценок пока нет
- Plasmodium. It Is AДокумент21 страницаPlasmodium. It Is AAgam MittalОценок пока нет
- Anti Malaria LsДокумент39 страницAnti Malaria LsSolaОценок пока нет
- .Trashed 1651316704 SporozoaДокумент30 страниц.Trashed 1651316704 SporozoaLeo ShibalataniОценок пока нет
- 40 Antimalaria 2015 Mandell Douglas and Bennett S Principles and PracticДокумент21 страница40 Antimalaria 2015 Mandell Douglas and Bennett S Principles and PracticHelen DyОценок пока нет
- Module 8B - Antimicrobials-3Документ39 страницModule 8B - Antimicrobials-3weissОценок пока нет
- DISEASE: - Malaria - : CAUSATIVE AGENTДокумент3 страницыDISEASE: - Malaria - : CAUSATIVE AGENTDiamante MhayaleneОценок пока нет
- Antiprotozoal Drugs Notes PDFДокумент26 страницAntiprotozoal Drugs Notes PDFMae Lislie Canonigo - FloresОценок пока нет
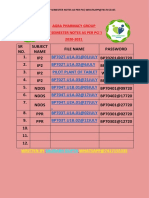
- BP702T.U1A.01@01JULY BP702T.U1A.02@6JULY Pilot Plant of Tablet BP702T.U1A.03@21JULY BP704T.U1B.01@09JULY BP704T.U1A.02@17JULYДокумент3 страницыBP702T.U1A.01@01JULY BP702T.U1A.02@6JULY Pilot Plant of Tablet BP702T.U1A.03@21JULY BP704T.U1B.01@09JULY BP704T.U1A.02@17JULYraj royelОценок пока нет
- BP502TPДокумент2 страницыBP502TPraj royel100% (2)
- Upsc Di Syllabus 2019Документ1 страницаUpsc Di Syllabus 2019raj royelОценок пока нет
- Paper AllДокумент2 страницыPaper Allraj royelОценок пока нет
- Gujarat Technological University: A. Physical Properties: Physical Form (Crystal & Amorphous), Particle SizeДокумент2 страницыGujarat Technological University: A. Physical Properties: Physical Form (Crystal & Amorphous), Particle Sizeraj royelОценок пока нет
- Gujarat Technological UniversityДокумент1 страницаGujarat Technological Universityraj royelОценок пока нет
- Pharmacognosy: Gpat Test Paper 1Документ10 страницPharmacognosy: Gpat Test Paper 1raj royel100% (1)
- Gujarat Technological University: A. Physical Properties: Physical Form (Crystal & Amorphous), Particle SizeДокумент2 страницыGujarat Technological University: A. Physical Properties: Physical Form (Crystal & Amorphous), Particle Sizeraj royelОценок пока нет
- Gujarat Technological University: W.E.F. AY 2017-18Документ3 страницыGujarat Technological University: W.E.F. AY 2017-18raj royelОценок пока нет
- Gujarat Technological University: Subject Name: Practice SchoolДокумент1 страницаGujarat Technological University: Subject Name: Practice Schoolraj royelОценок пока нет
- Gujarat Technological University: W.E.F. AY 2017-18Документ2 страницыGujarat Technological University: W.E.F. AY 2017-18raj royel100% (1)
- Gujarat Technological University: W.E.F. AY 2017-18Документ2 страницыGujarat Technological University: W.E.F. AY 2017-18raj royelОценок пока нет
- Question Bank PP Sem 2Документ4 страницыQuestion Bank PP Sem 2raj royel100% (1)
- Gujarat Technological University: W.E.F. AY 2017-18Документ2 страницыGujarat Technological University: W.E.F. AY 2017-18raj royel100% (1)
- Bioassay 5th SemДокумент66 страницBioassay 5th Semraj royel100% (10)
- Drugs Inspector-For Medial DevicesДокумент3 страницыDrugs Inspector-For Medial Devicesraj royelОценок пока нет
- Gujarat Technological University: W.E.F. AY 2017-18Документ2 страницыGujarat Technological University: W.E.F. AY 2017-18raj royelОценок пока нет
- Extrinsic Factorsanimated-My Ppt-Factor-Kns - Copy-1Документ58 страницExtrinsic Factorsanimated-My Ppt-Factor-Kns - Copy-1raj royelОценок пока нет
- Prepared By: Ms. Hetal B.GavitДокумент39 страницPrepared By: Ms. Hetal B.Gavitraj royel100% (1)
- DelhousiДокумент6 страницDelhousivatsalОценок пока нет
- BP501TTДокумент2 страницыBP501TTraj royelОценок пока нет
- Py Gpat 2016Документ15 страницPy Gpat 2016raj royelОценок пока нет
- BP502TPДокумент2 страницыBP502TPraj royel100% (2)
- Acids, Bases & Buffers - Copy-1Документ95 страницAcids, Bases & Buffers - Copy-1raj royel100% (1)
- 1 BenzeneДокумент41 страница1 Benzeneraj royelОценок пока нет
- Crude Drug ClassificationДокумент22 страницыCrude Drug Classificationraj royel100% (1)
- Gujarat Technological UniversityДокумент1 страницаGujarat Technological Universityraj royelОценок пока нет
- Daftar ObatДокумент27 страницDaftar Obathanny nuguОценок пока нет
- HFS PHILIPPINES, INC., G.R. No. 168716 Ruben T. Del Rosario and Ium Shipmanagement As, Petitioners, Ronaldo R. Pilar, Respondent. PromulgatedДокумент8 страницHFS PHILIPPINES, INC., G.R. No. 168716 Ruben T. Del Rosario and Ium Shipmanagement As, Petitioners, Ronaldo R. Pilar, Respondent. PromulgateddanexrainierОценок пока нет
- +bashkir State Medical UniversityДокумент2 страницы+bashkir State Medical UniversityCB SharmaОценок пока нет
- Maquet Meera BrochureДокумент16 страницMaquet Meera BrochureFeridun MADRANОценок пока нет
- Biopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Документ22 страницыBiopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Md. Abu Bakar Siddique TayefОценок пока нет
- Medical Surgical Nursing ReviewДокумент97 страницMedical Surgical Nursing ReviewBernadeth Josefa BorelaОценок пока нет
- Checklist Konseling Gizi Penderita Hipertensi Dan HiperlipidemiaДокумент3 страницыChecklist Konseling Gizi Penderita Hipertensi Dan HiperlipidemiaAtika WulandariОценок пока нет
- AlprazolamДокумент10 страницAlprazolamWen SilverОценок пока нет
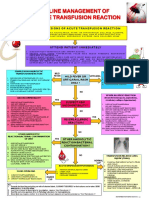
- Transfusion Reaction PDFДокумент1 страницаTransfusion Reaction PDFKah Man GohОценок пока нет
- Leaflet Glycophos 1 (Spesifikasi Produk)Документ2 страницыLeaflet Glycophos 1 (Spesifikasi Produk)Irhamna FauziahОценок пока нет
- Paket 2 OkДокумент5 страницPaket 2 OkBerna TodingОценок пока нет
- A Regenerative Interventional Approach To The Management of Degenerative Low Back PainДокумент16 страницA Regenerative Interventional Approach To The Management of Degenerative Low Back PainAthenaeum Scientific PublishersОценок пока нет
- Raja Sir CampДокумент6 страницRaja Sir CampNivedan KothekarОценок пока нет
- EndometriosisДокумент153 страницыEndometriosisoannny8661Оценок пока нет
- Diana Sanchez V City & County of DenverДокумент48 страницDiana Sanchez V City & County of DenverEllyn SantiagoОценок пока нет
- Parkinsons Presentation Case StudyДокумент33 страницыParkinsons Presentation Case Studyapi-287759747Оценок пока нет
- Compare Prokaryotes and Eukaryotes: Gram +ve Gram - Ve Peptidoglycan Layer Teichoic Acid Surface AntigenДокумент12 страницCompare Prokaryotes and Eukaryotes: Gram +ve Gram - Ve Peptidoglycan Layer Teichoic Acid Surface AntigenAamir BugtiОценок пока нет
- Medical Surgical Nursing Nclex Questions Integu2Документ12 страницMedical Surgical Nursing Nclex Questions Integu2dee_day_8100% (2)
- Emqs ObsДокумент33 страницыEmqs Obsbakkiaha100% (1)
- Herk Iames Pressley RidgeДокумент3 страницыHerk Iames Pressley Ridgeapi-350759206Оценок пока нет
- Khalil High Yeild Step 2 Cs Mnemonic 2nd EdДокумент24 страницыKhalil High Yeild Step 2 Cs Mnemonic 2nd EdCarolina Lopez100% (1)
- 6 Metronidazole Drug StudyДокумент4 страницы6 Metronidazole Drug Studyshadow gonzalezОценок пока нет
- The Letter of Intent To Enter PracticeДокумент4 страницыThe Letter of Intent To Enter Practicekazniels100% (1)
- Burnout: From Popular Culture To Psychiatric Diagnosis in SwedenДокумент21 страницаBurnout: From Popular Culture To Psychiatric Diagnosis in SwedenRajan PandaОценок пока нет
- Anesthesia For TurpДокумент5 страницAnesthesia For Turptnim.dsОценок пока нет
- D. Santhi Krupa, Et Al IJAPRДокумент6 страницD. Santhi Krupa, Et Al IJAPRAtraoОценок пока нет
- Pga CetДокумент31 страницаPga CetDrHassan Ahmed ShaikhОценок пока нет
- Process RecordingДокумент12 страницProcess RecordingIanna J. L. PedrosaОценок пока нет
- Immediate Care of The NewbornДокумент4 страницыImmediate Care of The NewbornMichelle GambolОценок пока нет
- Post-Operative Abdominal Infections: Epidemiology, Operational Definitions, and OutcomesДокумент10 страницPost-Operative Abdominal Infections: Epidemiology, Operational Definitions, and OutcomesJared CossioОценок пока нет