Академический Документы
Профессиональный Документы
Культура Документы
Medical Students Experiences of Moral Distress .33
Загружено:
AlloiBialbaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Medical Students Experiences of Moral Distress .33
Загружено:
AlloiBialbaАвторское право:
Доступные форматы
Well-Being of Students
Medical Students’ Experiences of Moral
Distress: Development of a Web-Based Survey
Catherine Wiggleton, MD, Emil Petrusa, PhD, Kim Loomis, MD, John Tarpley, MD,
Margaret Tarpley, Mary Lou O’Gorman, MDiv, and Bonnie Miller, MD
Abstract
Purpose situations and the intensity of distress than did men (P ⫽ .04), men tended to
To develop an instrument for measuring that they caused. The survey was become more distressed by each event
moral distress in medical students, administered to 106 fourth-year medical witnessed (P ⫽ .057).
measuring the prevalence of moral students during a three-week period in
distress in a cohort of students, and 2007; the response rate was 60%.
identifying the situations most likely to
Results Conclusions
Downloaded from https://journals.lww.com/academicmedicine by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3c9CHBlrWfCrg06gMQVuM9muOUUuFIDSST/mXsH/7Ndw= on 08/26/2020
cause it. Moral distress, defined as the
Each of the situations was experienced Medical students frequently experience
negative feelings that arise when one
knows the morally correct thing to do by at least some of the 64 respondents, moral distress. Our survey can
but cannot act because of constraints or and each created some degree of moral be used to measure aspects of the
hierarchies, has been documented in distress. On average, students witnessed learning environment as well as
nurses but has not been measured in almost one-half of the situations at least individual responses to the environment.
medical students. once, and more than one-third of the The variation found among student
situations caused mild-to-moderate responses warrants further investigation
Method distress. The survey measured individual to determine whether students at either
The authors constructed a survey distress (Cronbach alpha ⫽ 0.95), which extreme of moral distress are at risk of
consisting of 55 items describing varied among the students. Whereas burnout or erosion of professionalism.
potentially distressing situations. women witnessed potentially distressing
Responders rated the frequency of these situations significantly more frequently Acad Med. 2010; 85:111–117.
T he practice of medicine is in a position of vulnerability and need. students struggle with moral issues on a
fundamentally a moral endeavor. As This unbalanced relationship creates a regular basis. Specifically, students
argued by Pellegrino,1 knowledge and moral imperative: Physicians must reported that they had a strong desire to
expertise place the physician in a position uphold the promise to use their skills in do what they thought was in patients’
of authority, and illness places the patient service to their patients, and they must be best interests, but they were frustrated by
mindful and principled in negotiating the a variety of obstacles, including systems
conflicts of interest that arise on a daily of care, the hierarchy of medical
Dr. Wiggleton is resident, Department of basis.2 The moral development of medical education, and conflicts with patients’
Pediatrics, Vanderbilt University School of Medicine,
Nashville, Tennessee. students should thus be considered a own values and wishes. These stories
matter of high priority for medical were recounted with a sense of distress
Dr. Petrusa is director, Office for Teaching and
Learning in Medicine, Center for Outcomes and
educators. Using validated instruments that and sometimes anguish. One might
Research in Education, Vanderbilt University School measure stages of moral reasoning, expect that the students’ position at the
of Medicine, Nashville, Tennessee. investigators have found, however, that bottom of the medical hierarchy would
Dr. Lomis is assistant professor, Department of medical students do not show the progress absolve them of a sense of responsibility
Surgery, Vanderbilt University School of Medicine, that would be expected in others of for the situations they encountered, but,
Nashville, Tennessee. similar age and educational level. Some paradoxically, it seemed to heighten that
Dr. Tarpley is professor, Department of Surgery, students may, in fact, regress.3,4 The sense, because they often felt that they
Vanderbilt University School of Medicine, Nashville, question then arises as to whether the were the only ones who cared. If they
Tennessee.
process of medical education impedes didn’t act, then who would?
Ms. Tarpley is associate in surgery, Department of rather than promotes moral growth.5
Surgery, Vanderbilt University School of Medicine, In 1984, Jameton6 described the concept
Nashville, Tennessee. For seven years, we sponsored monthly of moral distress, defining it as the
Ms. O’Gorman is director of pastoral care, St. meetings of medical students and faculty, negative feelings that arise when one
Thomas Hospital, Nashville, Tennessee. in which students described experiences knows the morally correct response to a
Dr. Miller is senior associate dean for health on their clinical rotations that raised situation but cannot act because of
sciences education, Vanderbilt University School of ethical or moral questions. Participation institutional or hierarchal constraints. He
Medicine, Nashville, Tennessee. in these sessions was voluntary, and the also said that episodes of moral distress
Correspondence should be addressed to Dr. Miller, students were assured that these meetings are distinct from moral dilemmas, which
201 Light Hall, Vanderbilt University School of provided a safe haven for frank involve decisions between two potentially
Medicine, Nashville, TN 37232-0685; telephone:
(615) 343-7536; e-mail: bonnie.m.miller@ discussion. The accumulated body of correct courses of action and which are
vanderbilt.edu. stories supported the notion that not always accompanied by negative
Academic Medicine, Vol. 85, No. 1 / January 2010 111
Well-Being of Students
emotional responses.7 Nurses are felt to its items were applicable to students, and departments, who were known to have
be particularly prone to moral distress we obtained permission to adapt these expertise in biomedical ethics and/or
because of their direct responsibility for items for use in our survey. We generated survey design. On the basis of this
patient care combined with their lack of additional items from a review of the feedback, we revised the initial item set
ultimate decision-making authority. stories told by our students during the to produce a survey version with 55
Using instruments constructed to measure voluntary meetings of the past seven discrete situations.
moral distress, investigators have shown years. Finally, we conducted a review of
that it can ultimately affect a nurse’s the literature using the PubMed database. Study design
capacity for caring and that it is linked to We used the search terms “moral distress,” We offered the Web-based survey to the
withdrawal from patient contact, burnout, “moral dilemma,” and “ethical dilemma,” entire fourth-year class during a three-
and attrition from the profession.8 –11 and we limited results to those that week period in March 2007. This sample
focused on medical education.15–18 This of 106 students did not include the eight
The physician literature contains much process resulted in a total of 50
less about moral distress. Using focus focus group participants. An e-mail
potentially distressing situations. provided an explanation of the study as
group methodology, Kalvemark et al12
showed that moral distress occurs in well as a link to the survey. We included
For each situation, respondents rated the an informed consent document at the
physicians, nurses, and pharmacists in frequency of its occurrence and the
the context of ethical dilemmas and beginning of the survey, and we assured
degree of resulting distress. Frequency students that their responses would
resource constraints, and that it might ratings used a five-point scale: 0 ⫽ never, remain anonymous. Written consent was
occur even when one acted on conscience 1 ⫽ infrequently, 2 ⫽ occasionally, 3 ⫽ not required, because subsequent
but violated policies or regulations. frequently, and 4 ⫽ very frequently. completion of the survey implied that
Hamric and Blackhall13 recently devised a Distress ratings used a four-point scale: consent was given. Nonresponders were
scale by which to measure moral distress 0 ⫽ no distress, 1 ⫽ mild distress, 2 ⫽ sent periodic reminders. As an incentive
in physicians and nurses who deliver end- moderate distress, and 3 ⫽ severe to participate, respondents were included
of-life care in intensive care units. They distress. The distress scale also had the
found that both nurses and physicians in a raffle for a variety of prizes, ranging
option of “no distress because it never in value from movie tickets to iPod
experience moral distress, especially in happened.” For both scales, response
cases of prolonged and futile care. Higher nanos. The study received exempt status
options were labeled. The instrument from Vanderbilt University School of
moral distress scores correlated with less included a definition of moral distress,
job satisfaction in nurses and subsequent Medicine’s institutional review board.
and respondents were asked to limit their
risk of attrition, but the numbers were responses to clinical experiences during
too small to show the same relationships Statistical analysis
the past year.
in physicians.13 It seems logical that We used SPSS software (version 15.0;
moral distress would occur in medical In considering causes for student inaction SPSS Inc., Chicago, Illinois) to analyze
students, who simultaneously witness when, in theory, some action could be the data, including the frequency of and
and participate in the moral quandaries taken, we focused on the students’ distress ratings for each individual
that arise in patient care. They feel a position in the hierarchy of medical situation. To evaluate individual
laudable sense of responsibility for their education. The literature and our own students, we summed each student’s
patients, but they are constrained from experience suggested that fear for grades, frequency ratings and distress ratings and
action by their position in the hierarchy concern for one’s relationship with team created a scatterplot. We calculated
and their valid concern for subsequent members, and insecurity regarding Cronbach alpha to determine the
evaluations. In this study, we aimed to personal knowledge and skills block a suitability of the scale for assessment of
construct an instrument that measures student’s impulse to act.17,19 At the end of individual situations. We reviewed men’s
moral distress in physicians-in-training, the survey, we included six items regarding and women’s total frequency scores, total
to determine the extent of this these reasons, and we asked the students to distress scores, mean distress scores per
phenomenon in a cohort of students, and rate them according to the five-point situation, and mean frequency scores per
to determine the types of situations most frequency scale described above. situation to ascertain whether there were
likely to elicit this response. differences according to gender.
After initial construction of the
instrument, we convened a focus group
Method Results
of eight fourth-year medical students
Survey development who volunteered in response to an e-mail Sixty-four of the 106 medical students
For moral distress to occur, two elements request sent to the entire class. They completed the survey, for a 60%
must be present: a situation or episode completed the survey and immediately response rate. Sixty (83%) of the
that is perceived as morally incorrect, and discussed their reactions; they also responding students were between 25
a context that constrains one from taking provided feedback on the clarity and and 29 years old. Thirty-three (52%)
corrective action. In developing our organization of the survey and suggested were female, and 31 (48%) were male.
survey, we considered both elements. additional situations that, in their Relative to the whole class of 51 women
experience, had created moral distress. and 55 men, women were more likely
Corley14 developed a moral distress scale We also obtained input from selected to respond than were men, with
for the nursing profession that has been faculty members, both within the medical response rates of 65% and 56%,
shown to be reliable and valid. A few of school and from other university respectively. There was no correlation
112 Academic Medicine, Vol. 85, No. 1 / January 2010
Well-Being of Students
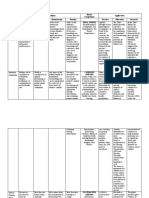
between the age of the respondent and scale). Table 1 shows the frequency of items that appear in both tables are
frequency or distress. Gender occurrence of and the distress ratings for footnoted in each table.
differences are reported below. these situations in the order of frequency
(mean frequency for all items ⫽ 1.0). Individual students’ moral distress
Analysis of individual situations Nineteen (35%) of the 55 situations in We also examined the differences
Nearly half (n ⫽ 26) of the situations the survey caused at least mild-to- between the responses of individual
included in the survey had a mean moderate distress. Table 2 shows the students, calculating an overall distress
frequency greater than 1.0, which meant frequency of occurrence of and the score as well as the relationship between
that, on average, students witnessed these distress ratings for these 19 situations, in frequency of a situation and the resulting
situations at least once (referred to as order of the degree of distress (mean distress. We computed distress scores (d)
“infrequently” in the five-point rating distress for all items ⫽ 1.5). The eight by adding the distress ratings (from the
Table 1
Frequency of Situations That Occurred at Least Once, Ranked From Most Often
to Least Often, and Corresponding Mean Distress Scores From a Cohort of 64
Fourth-Year Medical Students, Vanderbilt University School of Medicine, 2007*
Frequency: Distress:
Situation mean (SD) mean (SD)
Members of my team “bad-mouthed” other services. 2.70 (0.97) 0.95 (0.66)
...................................................................................................................................................................................................................................................................................................................
A member of my team made disparaging or demeaning comments about a patient who was overweight or obese. 2.20 (1.04) 1.16 (0.87)
...................................................................................................................................................................................................................................................................................................................
A patient presented with very advanced disease because he or she faced barriers to accessing care.† 2.14 (0.89) 1.90 (0.76)
...................................................................................................................................................................................................................................................................................................................
Multiple providers were involved in the care of one of my patients, and, because their roles were not fully 2.14 (1.11) 1.34 (0.82)
explained, there was confusion on the part of the patient and/or family.
...................................................................................................................................................................................................................................................................................................................
Over the course of a patient’s hospitalization, he or she was cared for by multiple doctors and services, which led to 1.95 (1.20) 1.50 (0.76)
fragmented, discontinuous care.†
...................................................................................................................................................................................................................................................................................................................
A member of my team made disparaging or demeaning remarks about one of our patients. 1.83 (0.94) 1.18 (0.76)
...................................................................................................................................................................................................................................................................................................................
A member of my team was disrespectful to someone below himself or herself on the team ranking.† 1.70 (1.11) 1.86 (0.81)
...................................................................................................................................................................................................................................................................................................................
The attending physician or resident answered a patient’s questions inadequately or simply ignored them.† 1.66 (1.04) 1.50 (0.73)
...................................................................................................................................................................................................................................................................................................................
A member of my team made disparaging or demeaning comments about a patient who was a smoker. 1.64 (1.04) 0.72 (0.74)
...................................................................................................................................................................................................................................................................................................................
I withheld information from a patient who requested it, because I felt it was not my responsibility or place to 1.61 (1.15) 1.37 (0.77)
provide it.
...................................................................................................................................................................................................................................................................................................................
Poor communication between multiple teams that were collaborating in the care of one my patients negatively 1.53 (0.91) 1.67 (0.79)
affected his or her care.†
...................................................................................................................................................................................................................................................................................................................
I promised one of my patients that someone would come back to talk to him or her, even though I was not sure it 1.45 (1.14) 1.35 (0.69)
would actually happen.
...................................................................................................................................................................................................................................................................................................................
Optimal care was not provided to one of my patients because of language barriers.† 1.42 (0.85) 1.53 (0.76)
...................................................................................................................................................................................................................................................................................................................
I participated in “bad-mouthing” another service. 1.42 (1.00) 0.83 (0.69)
...................................................................................................................................................................................................................................................................................................................
Delays occurred in the performance of tests or procedures because of scheduling problems or lost requests, and 1.41 (1.00) 1.47 (0.72)
this resulted in suboptimal patient care.
...................................................................................................................................................................................................................................................................................................................
Suboptimal care was provided to a patient because our team was too tired and overworked. 1.41 (1.11) 1.47 (0.74)
...................................................................................................................................................................................................................................................................................................................
The team went along with a treatment that we did not believe was indicated, because an attending insisted on it. 1.38 (0.98) 1.14 (0.75)
...................................................................................................................................................................................................................................................................................................................
A member of the team gave incorrect or uncertain information on rounds, but I said nothing. 1.38 (0.97) 0.96 (0.70)
...................................................................................................................................................................................................................................................................................................................
A member of my team was disrespectful to the nursing and/or ancillary staff. 1.31 (0.96) 1.37 (0.87)
...................................................................................................................................................................................................................................................................................................................
Delays in the return of laboratory data or radiology reports negatively affected the patient. 1.30 (1.02) 1.44 (0.81)
...................................................................................................................................................................................................................................................................................................................
Optimal care was not provided to a patient because of insurance status.† 1.20 (1.22) 1.67 (0.93)
...................................................................................................................................................................................................................................................................................................................
Optimal care was not provided to a patient as a result of stigmatizing social circumstances or conditions (e.g., 1.16 (1.06) 1.42 (0.79)
alcoholism, drug abuse, homelessness, or obesity).
...................................................................................................................................................................................................................................................................................................................
Our team continued to provide therapy at the patient’s or family’s request, even though I thought it only prolonged 1.14 (1.08) 1.85 (0.79)
the patient’s suffering.†
...................................................................................................................................................................................................................................................................................................................
A patient was discharged before I thought it was safe, because there was no one at home to care for the patient. 1.11 (0.97) 1.39 (0.87)
...................................................................................................................................................................................................................................................................................................................
I made disparaging or demeaning remarks about one of my patients. 1.03 (0.85) 1.14 (0.90)
...................................................................................................................................................................................................................................................................................................................
An attending and/or resident misrepresented the degree of my experience in performing a procedure. 1.03 (0.98) 1.12 (0.81)
* The wording “at least once” equals the ranking term “infrequently.” Respondents completed a survey
composed of 55 situations; they were asked to specify the frequency with which each situation occurred, by
using a five-point scale (0 ⫽ never, 1 ⫽ infrequently, 2 ⫽ occasionally, 3 ⫽ frequently, and 4 ⫽ very frequently),
and the degree of moral distress the situation caused, by using a four-point scale (0 ⫽ none, 1 ⫽ mild distress,
2 ⫽ moderate distress, and 3 ⫽ severe distress). Definitions for each degree of distress were provided at the
beginning of the survey. A score of “at least once” corresponds to a mean frequency of ⱖ1.0.
†
This item is also listed in Table 2.
Academic Medicine, Vol. 85, No. 1 / January 2010 113
Well-Being of Students
Table 2
Situations That Occurred at Least Once, Presented in Order From High to Low
Reported Distress Rankings, and Corresponding Mean Frequency Scores From a
Cohort of 64 Fourth-Year Medical Students, Vanderbilt University School of
Medicine, 2007*
Distress: Frequency:
Situation mean (SD) mean (SD)
A patient presented with very advanced disease because he or she faced barriers to accessing care.† 1.90 (0.76) 2.14 (0.89)
...................................................................................................................................................................................................................................................................................................................
One of my superiors behaved inappropriately, but I did not report it because I was afraid it would affect 1.89 (0.98) 0.98 (0.96)
my evaluation.
...................................................................................................................................................................................................................................................................................................................
A member of my team was disrespectful to someone below himself or herself on the team ranking.† 1.86 (0.81) 1.70 (1.11)
...................................................................................................................................................................................................................................................................................................................
Our team continued to provide therapy at the patient’s or family’s request, even though I thought it only 1.85 (0.79) 1.14 (1.08)
prolonged the patient’s suffering.†
...................................................................................................................................................................................................................................................................................................................
I felt that a patient was discriminated against by a member of my team on the basis of gender, race, 1.82 (0.88) 0.34 (0.62)
sexual orientation, or religion.
...................................................................................................................................................................................................................................................................................................................
An error was made in the care of one of my patients that was not fully or truthfully disclosed. 1.74 (0.64) 0.83 (0.81)
...................................................................................................................................................................................................................................................................................................................
One of my superiors behaved inappropriately, but I did not report it because I did not believe it was my 1.70 (0.88) 0.94 (0.94)
place to do so.
...................................................................................................................................................................................................................................................................................................................
I performed a procedure that I did not feel qualified to do, because I was afraid of being perceived as 1.68 (0.85) 0.47 (0.67)
incompetent.
...................................................................................................................................................................................................................................................................................................................
Optimal care was not provided to a patient because of insurance status.† 1.67 (0.93) 1.20 (1.22)
...................................................................................................................................................................................................................................................................................................................
Our team withdrew life support at the patient’s or family’s request, even though I thought the patient 1.67 (1.12) 0.19 (0.50)
could have survived with continued treatment.
...................................................................................................................................................................................................................................................................................................................
Poor communication between multiple teams that were collaborating in the care of one my patients 1.67 (0.79) 1.53 (0.91)
negatively affected his or her care.†
...................................................................................................................................................................................................................................................................................................................
A member of my team was rude and disrespectful to a patient or family member. 1.64 (0.88) 0.98 (0.81)
...................................................................................................................................................................................................................................................................................................................
I believe that a patient did not receive the standard of care for his or her condition. 1.64 (0.67) 0.78 (0.77)
...................................................................................................................................................................................................................................................................................................................
I performed a procedure that I did not feel qualified to do, because I felt pressured by a resident or 1.60 (0.88) 0.44 (0.73)
attending.
...................................................................................................................................................................................................................................................................................................................
Our team continued life support, even though I thought it was not what the patient would have 1.56 (0.85) 0.67 (0.94)
wanted.
...................................................................................................................................................................................................................................................................................................................
A patient was discharged before I thought it was medically safe. 1.54 (0.78) 0.52 (0.76)
...................................................................................................................................................................................................................................................................................................................
Optimal care was not provided to one of my patients because of language barriers.† 1.53 (0.76) 1.42 (0.85)
...................................................................................................................................................................................................................................................................................................................
Over the course of a patient’s hospitalization, he or she was cared for by multiple doctors and services, 1.50 (0.76) 1.95 (1.20)
and this led to fragmented, discontinuous care.†
...................................................................................................................................................................................................................................................................................................................
The attending physician or resident answered a patient’s questions inadequately or simply ignored 1.50 (0.73) 1.66 (1.04)
them.†
* The wording “at least once” equals the ranking term “infrequently.” Respondents completed a survey
composed of 55 situations and were asked, for each situation, to report the frequency with which it occurred,
by using a five-point scale (0 ⫽ never, 1 ⫽ infrequently, 2 ⫽ occasionally, 3 ⫽ frequently, and 4 ⫽ very
frequently), and the degree of moral distress it caused, by using a four-point scale (0 ⫽ no distress, 1 ⫽ mild
distress, 2 ⫽ moderate distress, 3 ⫽ severe distress). Definitions for each degree of distress were provided at the
beginning of the survey. Mild-to-moderate distress corresponds to a mean distress rating of ⱖ1.5 (where 1 ⫽
mild distress, and 2 ⫽ moderate distress).
†
This item is also listed in Table 1.
four-point scale) given to all items by an is 0.95, which indicates very high internal frequency rating per situation than did
individual student. With 55 items and a consistency. men (1.19 [SD: 0.52] and 0.95 [SD: 0.40],
maximum distress rating of 3, the respectively; P ⫽ .04). We found no
maximum d is 165. These scores ranged Gender analysis significant difference between the sum of
from 1 to 97 (mean: 46.9 [SD: 21.7]), Whereas the sample sizes were small, we distress ratings for men and for women,
with an approximately normal did find differences between the sexes in but men experienced distress per
distribution. Each student’s frequency measures of frequency and distress. Both situation at a level almost significantly
and distress sums were plotted against male and female students witnessed higher than that experienced by women
each other so that we could examine the nearly every situation included in the (1.46 [SD: 0.42] and 1.23 [SD: 0.51],
relationship between frequency and survey. The mean (SD) sum of frequency respectively; P ⫽ .057).
distress. Figure 1 shows a wide ratings was significantly higher for
distribution of these data, although there women than for men (65.19 [SD: 28.73] Reasons for not taking action
is a generally linear trend (R ⫽ 0.67). and 52.94 [SD: 22.12], respectively; P ⫽ .04). Table 3 shows the reasons that students
Cronbach alpha, in which each “item” is In addition, we found that women chose not to take action in the face of
the product of its frequency and distress, had a significantly higher mean (SD) distressing situations. The most
114 Academic Medicine, Vol. 85, No. 1 / January 2010
Well-Being of Students
medical students experience moral
distress on a regular basis. The survey we
created for this evaluation allows the
quantifying of both the frequency and the
intensity of episodes of moral distress. By
elucidating the types of situations that
cause distress, the results provided a
description of the clinical learning
environment, which allows us to gauge
how well that environment reflects the
professional values the medical
profession espouses. Although it was not
specifically designed for this purpose, the
survey also provides a tool for measuring
the burden of distress experienced by
individual students.
We set out to assess the frequency at
which medical students encounter
morally questionable situations and the
degree of distress they felt as a result.
Collectively, fourth-year medical students
recalled every one of the situations on the
survey, and, collectively, each situation
induced some degree of distress. On
Figure 1 Relationship between frequency and distress sums depicted as a scatterplot with
corresponding correlation coefficient (R) for a cohort of fourth-year medical students (N ⫽ 64) at
average, nearly half of the situations
Vanderbilt University School of Medicine, March 2007. occurred at least infrequently, and more
than one-third caused mild-to-moderate
distress. Only eight situations did both.
frequently cited reasons were the opportunity for these students to discuss These higher-frequency/high-distress
student’s subordinate role on the medical experiences they found ethically or items seem to be situations in which
team and his or her lack of confidence morally troubling. Their accounts students (1) perceive a direct, negative
regarding a full understanding of the provided strong anecdotal evidence that impact on patient care or (2) witness
situation. students experience what Jameton6 behavior that is directly disrespectful to
described as “moral distress,” the others. In general, it seems that situations
negative emotions that arise when one that pose more immediate potential harm
Discussion knows the morally correct response to a to others, whether by insult or by injury,
The monthly gatherings of third- and situation but cannot take action because cause a greater amount of distress.
fourth-year medical students that we of systemic constraints. The current study
sponsored for seven years provided an provided quantitative evidence that Several of the items that appeared on the
higher-frequency list did not cause even a
mild amount of distress. Most of these
higher-frequency/low-distress situations
Table 3 involved disrespectful remarks about
Reasons (and Their Mean [SD] Frequency) for Not Taking Action in the Face of other care teams or about patients. The
Distressing Situations in 64 Fourth-Year Medical Students, Vanderbilt University
Vanderbilt University School of Medicine’s
School of Medicine, 2007*
Compact for Teachers and Learners of
Frequency: Medicine clearly declares that such
Reason mean (SD) disparaging comments are unacceptable,20
Because I wanted to be perceived as a “team player.” 1.43 (1.03) and our students recognize them as
.........................................................................................................................................................................................................
Because I wanted to preserve my relationship with an attending and/or 1.64 (1.16) unprofessional, but perhaps this behavior
a resident. is so embedded in the culture that it no
.........................................................................................................................................................................................................
Because taking action might have negatively affected my evaluation. 1.67 (1.22) longer induces the negative emotional
.........................................................................................................................................................................................................
Because I did not want to be disrespectful of my attending and/or 1.83 (0.93) response that characterizes moral
resident. distress. It is also possible that the link
.........................................................................................................................................................................................................
Because I felt that my concerns or questions were due to incomplete 2.09 (1.08) between this behavior and its ultimate
knowledge and judgment. negative impact on team morale and
.........................................................................................................................................................................................................
Because I played a subordinate role on the team. 2.16 (1.04) patient care is so indirect that our
students fail to perceive it.
* Respondents used a five-point scale (0 ⫽ never, 1 ⫽ infrequently, 2 ⫽ occasionally, 3 ⫽ frequently, and 4 ⫽
very frequently) to rate the frequency with which each reason accounted for their not taking action in a
distressing situation. The value in the first cell is significantly different from all other values (P ⬍ .05), and the In February 2007, the Liaison Committee
values in the next three cells are significantly different from those in the last two cells (P ⬍ .05). on Medical Education21 adopted a new
Academic Medicine, Vol. 85, No. 1 / January 2010 115
Well-Being of Students
standard stating, “Medical schools must for assessing individuals and suggests that hidden curricula of local environments,
ensure that the learning environment responses from students are consistently without the need for or an attempt at
for medical students promotes the different. Our data demonstrated great generalization.
development of explicit and appropriate variability in the frequency and intensity
professional attributes (attitudes, of distress episodes reported by Future directions
behaviors, and identity).” In addition, it individual students. This variability is We are currently administering this
stated that schools should “regularly illustrated by the scatterplot, which survey to third-year medical students and
assess the learning environment and suggests that students who more the residents who work with them during
develop appropriate strategies to enhance frequently experience distress episodes their clerkships. We hope this effort will
the positive and mitigate the negative also are more intensely distressed by what determine whether the response to
influences.”21 We feel that a survey such they observe, notwithstanding gender potentially distressing situations changes
as the one reported here can aid both in variability. This finding raises a number as learners progress through training. In
the assessment process and in the crafting of questions that call for further addition, we plan to include burnout
of educational strategies. For example, investigation: (1) What is the meaning of scales to determine whether high levels of
five of the eight items that appeared on these differences? (2) Do they reflect distress place physicians-in-training at
both Table 1 and Table 2 describe inherent differences in moral sensitivity? risk, as was found for nurses.6 –11 The
inadequacies in our macrosystems or (3) Are students who experience greater gender differences we found suggest that
microsystems of care, including poor degrees of moral distress at risk of women perceive a greater number of
access, inadequate insurance coverage, burnout and cynicism, as has been situations to be distressing but that men
language barriers, and fragmentation. As suggested by the nursing literature? are more distressed per situation
part of recent curricular revisions in our (4) If so, what interventions can be witnessed. We are curious as to whether
medical school, the students now fully implemented to address this risk? (5) Are these differences will persist with a larger
explore the structure of the U.S. health students with a lower degree of moral sample size.
care system and the impact of the sensitivity callous, insensitive, or jaded,
inequities of that system on the lives of and, if so, what are the implications for Measurement is a first and necessary step
those at its fringes. Our data suggest their capacity for compassionate care? (6) in creating change, and we are now using
that students still experience distress, Do students in the midrange of moral our data toward that end. Our efforts
however, when they encounter these sensitivity represent a healthy norm, and, thus far have primarily been aimed at
inequities in the bitter circumstances of if so, what are the coping skills they have raising the awareness of institutional
real patients who could have fared better, employed to help them deal with distress? leadership groups. We have presented
if not for their lack of access. We in the (7) Does moral distress relate in any way these data to the department chairs
medical profession do discuss our moral to the erosion of professional ideals that and course directors who sit on our
obligation to promote the health of all is so often cited as a consequence of Undergraduate Medical Education
members of society, but, as Sautz22 medical education? Executive Committee; the initial response
suggests, perhaps we need to move has been one of concern and support. In
beyond discussion and equip students Limitations addition, we have been asked to present
with the skills to become forceful change The current study was limited by its these findings to our Clinical Enterprise
agents, thereby encouraging them to retrospective design that relied on Group, a committee of department chairs
mobilize their distress into action. Our recalled estimates of both frequency and and administrators that oversees all
findings also point to the need to supply intensity. Despite the inaccuracies of clinical operations at our medical center.
medical students with a greater memory, we must assume that the Although cross-institutional awareness is
understanding of the microsystems that reported events and the emotions that critically important, interventions may be
exist within our hospitals and clinics, accompanied them were real. In addition, more successful at the departmental level,
so that they might help to solve the whereas the survey design provided because accountability is more direct
problems caused by fragmentation and quantitative evidence that confirmed the there, and microcultures may change
inefficiencies. Finally, the Vanderbilt reality of moral distress, it lacked the more rapidly than larger institutional
Compact for Teachers and Learners of richness and nuance of narrative. We cultures. Data from more recent
Medicine clearly outlines professional suggest that future explorations of moral administrations of the survey will allow
expectations,20 but the data from the distress employ both qualitative and us to present department-specific
current study confirm that infractions quantitative methods. With a response information, and we hope that this
are common. We still have work to do if rate of 60%, we cannot exclude the information will provide an incentive for
we hope to achieve an educational possibility of selection bias, although the change as well as an accurate baseline
environment that fully embodies these widespread distribution of student from which to measure the impact of
professional expectations and allows our responses would argue against this. targeted interventions. In the meantime,
students to speak up (diplomatically) Finally, our data were limited to one our Department of Surgery has devoted a
when they witness lapses. We must also cohort in one institution, and thus our grand rounds session to the topic, and
counteract these infractions by providing findings may not be generalizable. our Department of Emergency Medicine
steadfast examples of superb role Although we strongly suspect that our recently initiated its own study of moral
models.23 institution is not unique in this regard, distress.
we acknowledge that each institution has
The high calculated Cronbach alpha that its idiosyncrasies. A survey of this nature When we revised our third-year
we found supports the use of that scale might be most valuable in elucidating the curriculum in 2006, we replaced the
116 Academic Medicine, Vol. 85, No. 1 / January 2010
Well-Being of Students
voluntary monthly meetings with four input from these sessions, we plan to 11 Meltzer LS, Huckabay LM. Critical care nurses’
required small-group sessions that occur create standardized scenarios that perceptions of futile care and its effect on
burnout. Am J Crit Care. 2004;13:202–208.
during quarterly intersession weeks. illustrate the most common of the
12 Kalvemark S, Hoglund AT, Hansson MG,
These meetings are led by “master clinical distressing situations, so that our Westerholm P, Bengst A. Living with
teachers” (MCTs), skilled clinician– students have the chance to practice conflicts—Ethical dilemmas and moral
educators selected and funded by responses that are both effective and distress in the health care system. Soc Sci
Vanderbilt University School of Medicine morally sound. Med. 2004;58:1075–1084.
13 Hamric AB, Blackhall LJ. Nurse–physician
to serve as the core teaching faculty for Funding/Support: The Vanderbilt University Cal perspectives on the care of dying patients in
the third and fourth years of medical Turner Program for Moral Leadership in the intensive care units: Collaboration, moral
school. The MCTs have undergone Professions provided support for this study, and distress, and ethical climate. Crit Care Med.
faculty development to better understand C.W. received support from the Vanderbilt 2007;35:422– 429.
the concepts and potential causes of University School of Medicine Medical Scholars 14 Corley MC. Development and evaluation of a
Program. moral distress scale. J Adv Nurs.
moral distress. To provide continuity,
2001;33:250 –256.
each MCT follows the same group of Other disclosures: The authors had no conflict of 15 Christakis DA, Feudtner C. Ethics in a short
eight students throughout the year. interest. white coat: The ethical dilemmas that medical
Before each session, students must record Ethical approval: The study received exempt students confront. Acad Med. 1993;68:249 –254.
short reflections in an electronic learning status from the institutional review board of the 16 Hicks LK, Lin Y, Robertson DW, Robinson
portfolio; these reflections are then Vanderbilt University School of Medicine. DL, Woodrow SI. Understanding the ethical
dilemmas that shape medical students’ ethical
reviewed by the MCTs. Students are development: Questionnaire survey and focus
given the option of discussing their group study. BMJ. 2001;322:709 –710.
References
reflections during the small-group 17 Caldicott C, Faber-Langendoen K. Deception,
session, and most take advantage of this 1 Pellegrino E. Toward a reconstruction of discrimination, and fear of reprisal: Lessons
medical morality. J Med Humanit. 1987;8:7–18. in ethics from third-year medical students.
opportunity. Although students are asked 2 Pellegrino E. Humanism and the Physician. Acad Med. 2005;80:866 – 873.
to write about any memorable or Knoxville, Tenn: The University of Tennessee 18 Bisonette R, O’Shea RM, Horwitz M, Route
instructive event—not only those events Press; 1979:117–129. C. A data-generated basis for medical ethics
that cause distress—MCTs report that a 3 Patenaude J, Niyonsenga T, Fafard D. education: Categorizing issues experienced by
Changes in students’ moral development students during clinical training. Acad Med.
preponderance of the stories deal with a during medical school: A cohort study.
few themes: inadequate systems, difficult 1995;70:1035–1037.
CMAJ. 2003;168:840 – 844. 19 Ginsberg S, Regehr G, Lingard L. The
communications, and breaches of 4 Self DJ, Schrader DE, Baldwin DC, Wolinski disavowed curriculum: Understanding
professionalism. One of us (K.D.L.) FD. The moral development of medical students’ reasoning in professionally
recently analyzed close to 200 of these students: A pilot study of the possible challenging situations. J Gen Intern Med.
influence of medical education. J Med Educ. 2003;18:1015–1022.
reflections and identified themes that are 1993;27:26 –34.
very consistent with the items on our 20 Camac B, Boehm F, Miller B. Vanderbilt
5 Hafferty FW, Franks R. The hidden
University School of Medicine Compact
survey.24 Students and MCTs alike curriculum, ethics teaching and the structure
Between Teachers and Learners. Available at:
reacted very positively to these sessions of medical education. Acad Med. 1994;69:
https://www.mc.vanderbilt.edu/medschool/
861– 871.
and complained only that the one-hour 6 Jameton A. Nursing Practice: The Ethical Issues.
pdf/compact4teachers_learners05.pdf.
sessions did not provide enough time to New York, NY: Prentice Hall; 1984:5– 6. Accessed March 1, 2009.
address and fully discuss all of the student 7 Jameton A. Dilemmas of moral distress: 21 Liaison Committee on Medical Education.
Moral responsibility and nursing practice. Functions and Structure of a Medical School.
concerns. As a result, four more sessions Available at: http://www.lcme.org/functions
AWHONNS Clin Issues Perinat Womens
have been added, so that they now occur Health Nurs. 1993;4:542–551. 2007jun.pdf. Accessed March 1, 2009.
eight times a year, at six-week intervals. 8 Corley MC. Nurse moral distress: A proposed 22 Sautz JW. Are we serious about teaching
Data have not yet documented the theory and research agenda. Nurs Ethics. professionalism in medicine? Acad Med.
effectiveness of these sessions, but this 2002;9:636 – 650. 2007;82:574 –577.
9 Nathaniel A. Moral distress among nurses. 23 Huddle TS. Teaching professionalism: Is
strategy has been championed by others medical morality a competency? Acad Med.
Am Nurses Assoc Ethics Human Rights
as a possible means of supporting the Issues Update. 2002;2(1). Available at: 2005;80:885– 891.
moral growth of learners.25 Finally, our http://www.nursingworld.org/MainMenu 24 Lomis KD, Carpenter RO, Miller BM. Moral
MCTs value their roles in affirming the Categories/EthicsStandards/IssuesUpdate/ distress in the third year of medical school: A
moral instincts of our students and also UpdateArchive/IssuesUpdateSpring2002/ descriptive review of student case reflections.
MoralDistress.aspx. Accessed March 1, 2009. Am J Surg. 2009:197:107–112.
recognize a need to help students develop 10 Sundin-Huard D, Fahy K. Moral distress, 25 Branch WT. Supporting the moral
the skills required to handle morally advocacy and burnout: Theorizing the development of medical students. J Gen
distressing situations. On the basis of the relationships. Int J Nurs Pract. 1999;5:8 –13. Intern Med. 2000;15:503–508.
Academic Medicine, Vol. 85, No. 1 / January 2010 117
Вам также может понравиться
- Medical Students' Endeavor To Make Use of Their Mental CapabilitiesДокумент6 страницMedical Students' Endeavor To Make Use of Their Mental CapabilitiesGauri ShahОценок пока нет
- Traditional and Western Medicine: Voices from Jamaican Psychiatric PatientsОт EverandTraditional and Western Medicine: Voices from Jamaican Psychiatric PatientsОценок пока нет
- Nolen-Hoeksema (2004)Документ6 страницNolen-Hoeksema (2004)briancrowder12Оценок пока нет
- Treating Adult Survivors Childhood Emotional Abuse Neglect G0003 PDFДокумент8 страницTreating Adult Survivors Childhood Emotional Abuse Neglect G0003 PDFColten KollenbornОценок пока нет
- How Can Students Diagnostic Competence Benefit.32Документ7 страницHow Can Students Diagnostic Competence Benefit.32Carlos Roberto Pires de Oliveira LimaОценок пока нет
- Dabon, Keyle Ann F. Quiambao, Rosel E. Santos, Jewel Anne DДокумент9 страницDabon, Keyle Ann F. Quiambao, Rosel E. Santos, Jewel Anne DJewel Anne SantosОценок пока нет
- An Interdisciplinary Community Diagnosis Experience in An Undergraduate Medical Curriculum: Development at Ghent UniversityДокумент9 страницAn Interdisciplinary Community Diagnosis Experience in An Undergraduate Medical Curriculum: Development at Ghent UniversityEgi NabilaОценок пока нет
- Potential Predictors of Psychological DistressДокумент11 страницPotential Predictors of Psychological DistressJose Angel LopezОценок пока нет
- The Stigma ScaleДокумент8 страницThe Stigma ScaleIka JuitaОценок пока нет
- E-Hidden in Plain Sight The Formal Informal and Hidden Curricula of A Psychiatry ClerkshipДокумент8 страницE-Hidden in Plain Sight The Formal Informal and Hidden Curricula of A Psychiatry Clerkshipusman sajidОценок пока нет
- Engel 1980 The Clinical Application of of The Biopsychosocial Model PDFДокумент10 страницEngel 1980 The Clinical Application of of The Biopsychosocial Model PDFDiego Almanza HolguinОценок пока нет
- Wakefiled (1992)Документ16 страницWakefiled (1992)Danusia JОценок пока нет
- Navarro, General Trias City, Cavite: Senior High School DepartmentДокумент5 страницNavarro, General Trias City, Cavite: Senior High School DepartmentVan TracilynОценок пока нет
- Understanding Families' Experiences Non-SyndromicДокумент8 страницUnderstanding Families' Experiences Non-Syndromiccristobal.mezaОценок пока нет
- Demographic, Personality, and Social Cognition Correlates of Coronavirus Guideline Adherence in A U.S. SampleДокумент11 страницDemographic, Personality, and Social Cognition Correlates of Coronavirus Guideline Adherence in A U.S. Samplesayyid cbrОценок пока нет
- TANAKA Et Al-2005-Psychiatry and Clinical NeurosciencesДокумент6 страницTANAKA Et Al-2005-Psychiatry and Clinical NeurosciencesBakrОценок пока нет
- Evidence For A Mental Health Crisis in Graduate EducationДокумент3 страницыEvidence For A Mental Health Crisis in Graduate EducationJeferson BarbosaОценок пока нет
- 10 1038@nbt 4089 PDFДокумент3 страницы10 1038@nbt 4089 PDFAnonymous DSATBjОценок пока нет
- (1930) BOHANNAN - Mental Hygiene From The Standpoint of College Administration 1930Документ16 страниц(1930) BOHANNAN - Mental Hygiene From The Standpoint of College Administration 1930Thiago Marques LeãoОценок пока нет
- 27716335Документ3 страницы27716335Mark BenОценок пока нет
- Med Research Imposter Syndrome Proposal CsuДокумент38 страницMed Research Imposter Syndrome Proposal CsuRuth Anne Sharmaine SantosОценок пока нет
- Psychology 2Документ10 страницPsychology 2PandaОценок пока нет
- Stress, Anxiety and Depression in Students of A Private Medical School in Karachi, PakistanДокумент6 страницStress, Anxiety and Depression in Students of A Private Medical School in Karachi, PakistanRika RatnasariОценок пока нет
- Systematic Review of Depression, Anxiety, and Other Indicators of Psychological Distress Among U.S. and Canadian Medical StudentsДокумент20 страницSystematic Review of Depression, Anxiety, and Other Indicators of Psychological Distress Among U.S. and Canadian Medical StudentsSteven FongОценок пока нет
- Argument SupportationДокумент6 страницArgument SupportationJULIA KooОценок пока нет
- Theorists Phil BarkerДокумент12 страницTheorists Phil BarkerAlleah Mendoza100% (1)
- Social Support and Mental Health Among College StudentsДокумент9 страницSocial Support and Mental Health Among College StudentsIra LampayanОценок пока нет
- Explore The Knowledge and Impact On Dysmenorrhea Among Nursing Students of Selected CollegeДокумент5 страницExplore The Knowledge and Impact On Dysmenorrhea Among Nursing Students of Selected CollegeEditor IJTSRDОценок пока нет
- ResearchДокумент134 страницыResearchMie LОценок пока нет
- Methodology of PCДокумент0 страницMethodology of PCShibu MundayatОценок пока нет
- Re-Defining Moral Distress: A Systematic Review and Critical Re-Appraisal of The Argument-Based Bioethics LiteratureДокумент16 страницRe-Defining Moral Distress: A Systematic Review and Critical Re-Appraisal of The Argument-Based Bioethics Literatureadhafauzihendrawan2004Оценок пока нет
- Trauma-Informed SchoolsДокумент17 страницTrauma-Informed SchoolsCamille RichouxОценок пока нет
- Sentinel Emotional Events: The Nature, Triggers, and Effects of Shame Experiences in Medical ResidentsДокумент9 страницSentinel Emotional Events: The Nature, Triggers, and Effects of Shame Experiences in Medical ResidentsYoliset RomeroОценок пока нет
- Georgina ParkerДокумент10 страницGeorgina Parkermsoto20052576Оценок пока нет
- Trauma Informed Aplications of ABAДокумент22 страницыTrauma Informed Aplications of ABACarregan AlvarezОценок пока нет
- NURES Group4 (CU2)Документ8 страницNURES Group4 (CU2)AriaОценок пока нет
- A Qualitative Study of Mental Health Experiences and College StudДокумент109 страницA Qualitative Study of Mental Health Experiences and College Studcatherine oroОценок пока нет
- Reflection In/and Writing: Pedagogy and Practice in Medical EducationДокумент7 страницReflection In/and Writing: Pedagogy and Practice in Medical Educationulices quintanaОценок пока нет
- Effectiveness of Jacobson'S Progressive Muscle Relaxation (JPMR) Technique On Social Anxiety Among High School Adolescents in A Selected School of Udupi District, Karnataka StateДокумент5 страницEffectiveness of Jacobson'S Progressive Muscle Relaxation (JPMR) Technique On Social Anxiety Among High School Adolescents in A Selected School of Udupi District, Karnataka StateSidharth PraveenОценок пока нет
- An Assessment of Suicide-Related Knowledge and Skills Among Health ProfessionalsДокумент10 страницAn Assessment of Suicide-Related Knowledge and Skills Among Health ProfessionalsIshban Wang'ombeОценок пока нет
- Integenerational Transmission of DepressionДокумент26 страницIntegenerational Transmission of DepressionHector LegrekОценок пока нет
- Patient-Centred Attitudes Among Medical Students in Mali, West Africa: A Cross-Sectional StudyДокумент10 страницPatient-Centred Attitudes Among Medical Students in Mali, West Africa: A Cross-Sectional Studyhamayal xОценок пока нет
- Selected College Students Perceptions Knowledge and Awareness oДокумент88 страницSelected College Students Perceptions Knowledge and Awareness oDiksha chaudharyОценок пока нет
- The Construction of Fear Americans PrefeДокумент19 страницThe Construction of Fear Americans Prefeega meilindraОценок пока нет
- Effects of A Risk and Resilience Course On Stress, Coping Skills, and Cognitive Strategies in College StudentsДокумент7 страницEffects of A Risk and Resilience Course On Stress, Coping Skills, and Cognitive Strategies in College StudentscrazyappleОценок пока нет
- E144 Vol. 52 No. 6 December 2016 Selected AbstractsДокумент2 страницыE144 Vol. 52 No. 6 December 2016 Selected AbstractsJos CanalesОценок пока нет
- OutДокумент127 страницOutMai MimiОценок пока нет
- (Bradford Books) Prinz, Wolfgang - Sebanz, Natalie - Disorders of Volition-The MIT Press (2006)Документ502 страницы(Bradford Books) Prinz, Wolfgang - Sebanz, Natalie - Disorders of Volition-The MIT Press (2006)Víctor FuentesОценок пока нет
- LGBT 2020 0494Документ9 страницLGBT 2020 0494Belén DobrichОценок пока нет
- 2016-The - Clinical - Teacher (Clinical Teaching Lesson Plan)Документ2 страницы2016-The - Clinical - Teacher (Clinical Teaching Lesson Plan)Justin VergaraОценок пока нет
- ABowman Dissertatio FinalДокумент133 страницыABowman Dissertatio FinalManu JimenezОценок пока нет
- The Associations Between University Adjustment AduДокумент13 страницThe Associations Between University Adjustment AduAna Maria NОценок пока нет
- Anxiety in Children With Autism Spectrum Disorders - An ExaminatioДокумент138 страницAnxiety in Children With Autism Spectrum Disorders - An ExaminatioFakher KhaliliОценок пока нет
- The Role of Psychological Flexibility in Graduate Student StressДокумент144 страницыThe Role of Psychological Flexibility in Graduate Student StressYuva RaniОценок пока нет
- Current Concepts in Feminizing Gender Surgery.46Документ11 страницCurrent Concepts in Feminizing Gender Surgery.46Razaria DailyneОценок пока нет
- TeachingДокумент6 страницTeachingmelanieОценок пока нет
- 3-Characteristics of The Informal CurriculumДокумент10 страниц3-Characteristics of The Informal CurriculumKОценок пока нет
- Bmjopen-2020-046654 Kohort (M7)Документ8 страницBmjopen-2020-046654 Kohort (M7)rsandal1997Оценок пока нет
- Dorothy Johnson Theory PDFДокумент7 страницDorothy Johnson Theory PDFJenny SorianoОценок пока нет
- OB Journal AppraisalДокумент2 страницыOB Journal AppraisalAlloiBialbaОценок пока нет
- Reflection 6Документ2 страницыReflection 6AlloiBialbaОценок пока нет
- Health Care For PublishДокумент99 страницHealth Care For PublishAlloiBialbaОценок пока нет
- (Template) PediaДокумент7 страниц(Template) PediaAlloiBialbaОценок пока нет
- Alloi: Li, X., Et Al. (2020)Документ2 страницыAlloi: Li, X., Et Al. (2020)AlloiBialbaОценок пока нет
- Bialba TB PharmaДокумент2 страницыBialba TB PharmaAlloiBialbaОценок пока нет
- (Surg2) 5.2 Urology Part 1 - Dr. YusiДокумент18 страниц(Surg2) 5.2 Urology Part 1 - Dr. YusiAlloiBialbaОценок пока нет
- Case LegMedДокумент1 страницаCase LegMedAlloiBialbaОценок пока нет
- CAP Nelsons DR - Atienza 2020-2021Документ15 страницCAP Nelsons DR - Atienza 2020-2021AlloiBialbaОценок пока нет
- (Surg2) 5.1a Introduction To Anesthesia Part 1Документ21 страница(Surg2) 5.1a Introduction To Anesthesia Part 1AlloiBialbaОценок пока нет
- (Surg2) 5.4 Urology Part 3Документ23 страницы(Surg2) 5.4 Urology Part 3AlloiBialbaОценок пока нет
- Wooten Review ArticleДокумент9 страницWooten Review ArticleAlloiBialbaОценок пока нет
- Pharmacotherapeutic (Medpharma30) AY 2020-2021 Treatment Drug SelectionДокумент2 страницыPharmacotherapeutic (Medpharma30) AY 2020-2021 Treatment Drug SelectionAlloiBialbaОценок пока нет
- (Surg2) 5.1c Anesthesia Video TranscriptionДокумент5 страниц(Surg2) 5.1c Anesthesia Video TranscriptionAlloiBialbaОценок пока нет
- Over-the-Counter Medications in PregnancyДокумент8 страницOver-the-Counter Medications in PregnancyAlloiBialbaОценок пока нет
- (Surg2) 5.1b Introduction To Anesthesia-Part 2Документ16 страниц(Surg2) 5.1b Introduction To Anesthesia-Part 2AlloiBialbaОценок пока нет
- (Surg2) 5.3 Urology Part 2 - Dr. YusiДокумент19 страниц(Surg2) 5.3 Urology Part 2 - Dr. YusiAlloiBialbaОценок пока нет
- Paediatric Pharmacokinetics: Key Considerations: Hannah Katharine Batchelor & John Francis MarriottДокумент10 страницPaediatric Pharmacokinetics: Key Considerations: Hannah Katharine Batchelor & John Francis MarriottAlloiBialbaОценок пока нет
- Pharmacotherapy During Pregnancy, Childbirth and LactationДокумент6 страницPharmacotherapy During Pregnancy, Childbirth and Lactationfiras frsОценок пока нет
- Surger YII Clinic AL Case: Group 4B Bernabe, Bernardo, Bialba, BigorniaДокумент39 страницSurger YII Clinic AL Case: Group 4B Bernabe, Bernardo, Bialba, BigorniaAlloiBialbaОценок пока нет
- Paediatric Pharmacokinetics: Key Considerations: Hannah Katharine Batchelor & John Francis MarriottДокумент10 страницPaediatric Pharmacokinetics: Key Considerations: Hannah Katharine Batchelor & John Francis MarriottAlloiBialbaОценок пока нет
- Good Prescribing GuideДокумент142 страницыGood Prescribing GuideTheresa ValleriОценок пока нет
- Pharmacology: Outline PharmacodynamicsДокумент11 страницPharmacology: Outline PharmacodynamicsAlloiBialbaОценок пока нет
- (Surg2) 5.1d Anesthesia PointersДокумент12 страниц(Surg2) 5.1d Anesthesia PointersAlloiBialbaОценок пока нет
- Don't Use AbbreviationДокумент3 страницыDon't Use AbbreviationSara tarekОценок пока нет
- Rational Prescribing: The Principles of Drug Selection: Author: Simon RJ MaxwellДокумент6 страницRational Prescribing: The Principles of Drug Selection: Author: Simon RJ MaxwellAlloiBialbaОценок пока нет
- Tratamiento - Integral.de - Las.quemaduras EspañolДокумент21 страницаTratamiento - Integral.de - Las.quemaduras EspañolPablo HenríquezОценок пока нет
- Neuropreceptorial ChecklistДокумент33 страницыNeuropreceptorial ChecklistAlloiBialba0% (1)
- Neuropreceptorial ChecklistДокумент33 страницыNeuropreceptorial ChecklistAlloiBialba0% (1)
- Standard Operating ProceduresДокумент89 страницStandard Operating ProceduresAsfa JaVed100% (11)
- Cultivating Empathy For The Mentally Ill Using Simulated Auditory HallucinationsДокумент4 страницыCultivating Empathy For The Mentally Ill Using Simulated Auditory HallucinationsGloria Carbajal ZegarraОценок пока нет
- MSPE Noteworthy Characteristics Worksheet: Complete This Worksheet and Bring It To Your Mandatory Career Advising SessionДокумент2 страницыMSPE Noteworthy Characteristics Worksheet: Complete This Worksheet and Bring It To Your Mandatory Career Advising SessionHải Dương NguyễnОценок пока нет
- Clinical Sports MedicineДокумент729 страницClinical Sports MedicineRugiada222100% (2)
- Henry Ford Macomb Hospital ProgramДокумент26 страницHenry Ford Macomb Hospital ProgramRamanpreet Kaur MaanОценок пока нет
- Islamic Perspective Written ReportДокумент8 страницIslamic Perspective Written ReportAbegail JutbaОценок пока нет
- XJXNDДокумент56 страницXJXNDGautam NatrajОценок пока нет
- John FlynnsДокумент10 страницJohn Flynnssamwong87Оценок пока нет
- Medical Ethics: Indian Journal ofДокумент76 страницMedical Ethics: Indian Journal ofkaarkkiОценок пока нет
- Insan Anatomisi Atlasi Mcminn 1515167549Документ18 страницInsan Anatomisi Atlasi Mcminn 1515167549Müslüm ŞahinОценок пока нет
- Allied Health Sciences: The Tamilnadu Dr. M.G.R. Medical UniversityДокумент4 страницыAllied Health Sciences: The Tamilnadu Dr. M.G.R. Medical Universitysasenthil241464Оценок пока нет
- Cover Letter For Medical OfficerДокумент8 страницCover Letter For Medical Officerbcqvdfyg100% (2)
- Rockefeller Foundation RapportДокумент477 страницRockefeller Foundation RapportundermattanОценок пока нет
- Choosing A Medical School & MD-PHD Program: A Black Student's GuideДокумент16 страницChoosing A Medical School & MD-PHD Program: A Black Student's GuideAyomide OjebuobohОценок пока нет
- Who MC Topic-6Документ14 страницWho MC Topic-6Kartika Radianti WardhaniОценок пока нет
- Research 1st Year Med StudentsДокумент26 страницResearch 1st Year Med StudentsMutasimОценок пока нет
- Becoming A DoctorДокумент5 страницBecoming A DoctorInzi AsadОценок пока нет
- Journal of Health Global 2018Документ344 страницыJournal of Health Global 2018Rizki Agung PrasetyoОценок пока нет
- A New Leadership Curriculum: The Multiplication of IntelligenceДокумент4 страницыA New Leadership Curriculum: The Multiplication of IntelligenceGisele PhaloОценок пока нет
- SWU Orientation Surgery 2Документ17 страницSWU Orientation Surgery 2Jabagat, Benedict Christian P.Оценок пока нет
- Hong Kong's First Professor of Pathology and The Laboratory of The Royal College of Physicians of EdinburghДокумент6 страницHong Kong's First Professor of Pathology and The Laboratory of The Royal College of Physicians of EdinburghJhonalValdimirQuispeMamaniОценок пока нет
- Communication Skills Education For Doctors: An UpdateДокумент50 страницCommunication Skills Education For Doctors: An UpdateDaniel PendickОценок пока нет
- 2024-2025 Fulltime Application FormДокумент9 страниц2024-2025 Fulltime Application Formmbewerahab6Оценок пока нет
- KHYBER PAKHTUNKHWA PUBLIC SERVICE COMMISSION AdvertisementДокумент16 страницKHYBER PAKHTUNKHWA PUBLIC SERVICE COMMISSION Advertisementzahoor aliОценок пока нет
- Ebook Goldman Cecil Medicine PDF Full Chapter PDFДокумент67 страницEbook Goldman Cecil Medicine PDF Full Chapter PDFjames.farnan170100% (25)
- Wilson Newsletter September 2020Документ2 страницыWilson Newsletter September 2020Valerie PadillaОценок пока нет
- Problem-Based Learning in Clinical Education The Next Generation by Cindy E. Hmelo-SilverДокумент261 страницаProblem-Based Learning in Clinical Education The Next Generation by Cindy E. Hmelo-Silverjuanc1112Оценок пока нет
- Teresa M Rust Curriculum VitaeДокумент5 страницTeresa M Rust Curriculum Vitaeapi-309387276Оценок пока нет
- Wissenswertes Für Die USA-FamulaturДокумент2 страницыWissenswertes Für Die USA-FamulaturCoskun SuermeliОценок пока нет
- Child and Adolescent Psychiatry - Blackwell's Neurology and Psychiatry Access SeriesДокумент416 страницChild and Adolescent Psychiatry - Blackwell's Neurology and Psychiatry Access SeriesErickson Arthur Siahaan0% (1)
- From Paycheck to Purpose: The Clear Path to Doing Work You LoveОт EverandFrom Paycheck to Purpose: The Clear Path to Doing Work You LoveРейтинг: 4.5 из 5 звезд4.5/5 (39)
- The 7 Habits of Highly Effective People: The Infographics EditionОт EverandThe 7 Habits of Highly Effective People: The Infographics EditionРейтинг: 4 из 5 звезд4/5 (2475)
- Summary: 12 Months to $1 Million: How to Pick a Winning Product, Build a Real Business, and Become a Seven-Figure Entrepreneur by Ryan Daniel Moran: Key Takeaways, Summary & AnalysisОт EverandSummary: 12 Months to $1 Million: How to Pick a Winning Product, Build a Real Business, and Become a Seven-Figure Entrepreneur by Ryan Daniel Moran: Key Takeaways, Summary & AnalysisРейтинг: 5 из 5 звезд5/5 (2)
- The 30 Day MBA: Your Fast Track Guide to Business SuccessОт EverandThe 30 Day MBA: Your Fast Track Guide to Business SuccessРейтинг: 4.5 из 5 звезд4.5/5 (19)
- Designing Your Life by Bill Burnett, Dave Evans - Book Summary: How to Build a Well-Lived, Joyful LifeОт EverandDesigning Your Life by Bill Burnett, Dave Evans - Book Summary: How to Build a Well-Lived, Joyful LifeРейтинг: 4.5 из 5 звезд4.5/5 (62)
- The Proximity Principle: The Proven Strategy That Will Lead to the Career You LoveОт EverandThe Proximity Principle: The Proven Strategy That Will Lead to the Career You LoveРейтинг: 4.5 из 5 звезд4.5/5 (93)
- Start.: Punch Fear in the Face, Escape Average, and Do Work That MattersОт EverandStart.: Punch Fear in the Face, Escape Average, and Do Work That MattersРейтинг: 4.5 из 5 звезд4.5/5 (56)
- Steal the Show: From Speeches to Job Interviews to Deal-Closing Pitches, How to Guarantee a Standing Ovation for All the Performances in Your LifeОт EverandSteal the Show: From Speeches to Job Interviews to Deal-Closing Pitches, How to Guarantee a Standing Ovation for All the Performances in Your LifeРейтинг: 4.5 из 5 звезд4.5/5 (39)
- Work Stronger: Habits for More Energy, Less Stress, and Higher Performance at WorkОт EverandWork Stronger: Habits for More Energy, Less Stress, and Higher Performance at WorkРейтинг: 4.5 из 5 звезд4.5/5 (12)
- The First 90 Days: Proven Strategies for Getting Up to Speed Faster and SmarterОт EverandThe First 90 Days: Proven Strategies for Getting Up to Speed Faster and SmarterРейтинг: 4.5 из 5 звезд4.5/5 (122)
- The Business of Beauty: Your Guide To Happiness And Success In The Salon IndustryОт EverandThe Business of Beauty: Your Guide To Happiness And Success In The Salon IndustryРейтинг: 3.5 из 5 звезд3.5/5 (2)
- The 2-Hour Job Search: Using Technology to Get the Right Job FasterОт EverandThe 2-Hour Job Search: Using Technology to Get the Right Job FasterРейтинг: 4 из 5 звезд4/5 (23)
- The 12 Week Year: Get More Done in 12 Weeks than Others Do in 12 MonthsОт EverandThe 12 Week Year: Get More Done in 12 Weeks than Others Do in 12 MonthsРейтинг: 4.5 из 5 звезд4.5/5 (90)
- 12 Habits Of Valuable Employees: Your Roadmap to an Amazing CareerОт Everand12 Habits Of Valuable Employees: Your Roadmap to an Amazing CareerОценок пока нет
- The Ultimate Sales Letter, 4th Edition: Attract New Customers, Boost Your SalesОт EverandThe Ultimate Sales Letter, 4th Edition: Attract New Customers, Boost Your SalesРейтинг: 4.5 из 5 звезд4.5/5 (98)
- The Power of Body Language: An Ex-FBI Agent's System for Speed-Reading PeopleОт EverandThe Power of Body Language: An Ex-FBI Agent's System for Speed-Reading PeopleРейтинг: 5 из 5 звезд5/5 (9)
- The Everything Guide To Being A Paralegal: Winning Secrets to a Successful Career!От EverandThe Everything Guide To Being A Paralegal: Winning Secrets to a Successful Career!Рейтинг: 5 из 5 звезд5/5 (1)
- What Every BODY is Saying: An Ex-FBI Agent’s Guide to Speed-Reading PeopleОт EverandWhat Every BODY is Saying: An Ex-FBI Agent’s Guide to Speed-Reading PeopleРейтинг: 4.5 из 5 звезд4.5/5 (354)
- Company Of One: Why Staying Small Is the Next Big Thing for BusinessОт EverandCompany Of One: Why Staying Small Is the Next Big Thing for BusinessРейтинг: 3.5 из 5 звезд3.5/5 (14)
- Happy at Work: How to Create a Happy, Engaging Workplace for Today's (and Tomorrow's!) WorkforceОт EverandHappy at Work: How to Create a Happy, Engaging Workplace for Today's (and Tomorrow's!) WorkforceОценок пока нет
- Real Artists Don't Starve: Timeless Strategies for Thriving in the New Creative AgeОт EverandReal Artists Don't Starve: Timeless Strategies for Thriving in the New Creative AgeРейтинг: 4.5 из 5 звезд4.5/5 (197)
- Ultralearning: Master Hard Skills, Outsmart the Competition, and Accelerate Your CareerОт EverandUltralearning: Master Hard Skills, Outsmart the Competition, and Accelerate Your CareerРейтинг: 4.5 из 5 звезд4.5/5 (360)
- Got Your Attention?: How to Create Intrigue and Connect with AnyoneОт EverandGot Your Attention?: How to Create Intrigue and Connect with AnyoneРейтинг: 4.5 из 5 звезд4.5/5 (4)