Академический Документы
Профессиональный Документы
Культура Документы
35 PDF
Загружено:
Daniela HernandezОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
35 PDF
Загружено:
Daniela HernandezАвторское право:
Доступные форматы
THE IMPACT OF THE DOCENT CLINICAL PHARMACIST
ON TREATMENT OF STREPTOCOCCAL PNEUMONIA
by Joel O. Covinsky, Stephen C. Hamburger, Kim L. Kelly, Bonnie Pastewski,
Nancy Robertson, Roger Eskridge, Glen Park, and Edward J. Twin
IN THE EARLY 1970s, the first doctoral level clinical phar- medication cost per day, and outpatient costs, including
macist was hired by the Kansas City General Hospital outpatient medical cost, were among the kinds of in-
(now called Truman Medical Center-West) to assist the formation collected for these monthly reports. In an ef-
medical staff in developing sound therapeutic programs fort to identify the docent clinical pharmacist's specific
for the management of disease. Dr. Edward J. Twin was contribution to these cost figures in the inpatient area,
the executive medical director for the Kansas City the following study was designed, using an infectious
General Hospital and for the affiliate Jackson County disease model.
Hospital (now called Truman Medical Center-East). Ac- The purpose of this two-phase, retrospective study
cording to Twin, these doctors of pharmacy were as- was to determine the influence of the clinical phar-
signed to various medical teams (called docent teams) macists on the management of streptococcal
and were responsible for drug therapy on their respec- (pneumococcal) pneumonia. Streptococcal pneumonia
tive units.' They were called docent clinical pharmacists was chosen as the model disease state for several
and were accountable for the selection of therapy ac- reasons: it has a 5-10 percent per year incidence of mor-
cording to considerations of efficacy, safety, and cost. tality in the U.S.; there is a recognized problem with
Numerous programs were developed to evaluate the inappropriate antibiotic utilization;' use of antibiotics
quality of care provided by these multidisciplinary do- is associated with tremendous expense (often consum-
cent teams. For example, under the direction of the ing from Y4 to Y3 or more of the hospital pharmacy's
Department of Medicine, a multidisciplinary commit- budget); and well-documented standards for ap-
tee was charged with the responsibility of developing propriate drug therapy for this disease have been
audit criteria for the common diseases seen at the two published in the medical literature. 3 Additionally, the
institutions. These audits provided the objective indices emergence of antibiotic-resistant bacteria has been
for evaluating the quality of patient care on the in- reported at numerous institutions.':" Finally, the Joint
dividual units. Additionally, data were collected on a Commission on Accreditation of Hospitals has required
monthly basis to evaluate the activities of the various the development of formal programs to review antibiotic
units by examining the efficiency with which hospital usage in hospitalized patients. For these reasons, the
personnel, facilities, and resources were utilized in review of an infectious disease provided an optimal
providing patient care. Inpatient costs, including model for evaluating the contribution of the docent
clinical pharmacist to an area of patient care that re-
JOEL O. COVINSKY, Pharm.D., is Associate Professor and quired further study.
Director of Clinical Pharmacology Program, Schools
of Medicine and Pharmacy, University of Missouri-
Kansas City, and Docent Clinical Pharmacist, Clinical Methods
Pharmacology Section, Truman Medical Center;
STEPHEN C. HAMBURGER, M.D., is Associate Professor Truman Medical Center consists of two hospitals,
and Vice-Chairman, Department of Medicine, School Truman Medical Center-West (TMC-W) and Truman
of Medicine; KIM L. KELLY, Pharm.D., atthetimeofthis Medical Center-East (TMC-E). Since 1971, there have
study, was Associate Professor, Schools of Medicine been full-time docent clinical pharmacists at TMC-W.
and Pharmacy, University of Missouri-Kansas City, and TMC-E did not have a clinical pharmacist until 1974.
Docent Clinical Pharmacist, Clinical Pharmacology Sec- Thus, this study was divided into two parts: a two-year
tion, Truman Medical Center; he is now Director of
Professional Education for Syva Company, and Clinical study of the treatment of streptococcal pneumonia at
Professor of Medicine at the University of Missouri TMC-W and TMC-E prior to 1974, and a two-year
School of Medicine. BONNIE PASTEWSKI, Pharm.D., is study of the treatment of streptococcal pneumonia at
Assistant Professor of Clinical Pharmacy, Philadelphia TMC-E after a clinical pharmacist was hired.
College of Pharmacy and Science; NANCY ROBERTSON, The Medical Records Department retrieved the
Pharm.D., is Assistant Professor of Clinical Pharmacy, records of all patients admitted at either TMC-W or
College of Pharmacy, Medical University of South TMC-E between June 1972 and June 1974 who had a
Carolina; ROGER ESKRIDGE, Pharm.D., is Assistant primary diagnosis of streptococcal pneumonia. In ad-
Director of Pharmacy Services, Trinity Lutheran dition, the Medical Records Department at TMC-E
Hospital, Kansas City; GLEN PARK, Pharm.D., at the retrieved the charts of all patients admitted with a
time of this study, was Clinical Pharmacist, Department
of Pharmacy Services, University Hospitals of primary diagnosis of streptococcal pneumonia between
Cleveland; he is now a faculty member at the Universi- June 1975 and June 1977. To be included in this study,
ty of Iowa; EDWARD J. TWIN, M.D., is Professor and all patients had to meet the Department of Medicine
Senior Docent, School of Medicine, University of audit criteria for the diagnosis of streptococcal
Missouri-Kansas City, Kansas City, MO. pneumonia. They could not have (1) postoperative
Drug Intelligence and Clinical Pharmacy VOL 16 JULY/AUG 82 587
Downloaded from aop.sagepub.com at Purdue University on June 5, 2016
pneumonias, (2) pneumonia diagnosed after hospital formed on an IBM (360-60) computer with the assistance
day 3, (3) allergic pneumonitis, (4) other occurrences of the statistical analysis system package. An estimated
that superceded the treatment of pneumonia and became hospital stay was derived from the patient's total
the primary diagnosis (e.g., acute myocardial infarc- number of hospital days.
tion), (5) white blood cell counts < 1500, (6) antibiotic The chi-square test was done to compare, statistical-
therapy less than one week before hospitalization, nor ly, the drug regimens utilized for streptococcal
(7) pneumonia with concurrent infection elsewhere. Pa- pneumonia at TMC-W and TMC-E with the standard
tients younger than 16 years were also excluded from recommended regimen.
the study.
Information gathered from each medical record Results
included:
Tables 1-5 contain comparative information on the
1. the diagnostic criteria-vital signs, chest X-ray, length of stay, raw cost of antibiotics, raw cost of in-
complete blood count with white blood cell dif- travenous additives, total raw costs of antibiotic ad-
ferential, Gram stain of the sputum or trans- ministration, raw cost of antibiotics on a daily basis,
tracheal aspiration, or culture and sensitivity total raw cost of antibiotic per day including intravenous
tests of the sputum or transtracheal aspirate; additives when appropriate, and finally, the patient
2. drug utilization (choice of antibiotic, dosage, charge based on the procedure utilized at these hospitals
number of total doses, and route of adminis- today.
tration); Table 1 shows a cross-group comparison of the out-
3. duration of hospital stay (total days of hos- come data obtained at TMC-W and TMC-E, with and
pitalization); and without the docent clinical pharmacist. The first column
4. readmission rate. shows the results obtained at TMC-W with the docent
clinical pharmacist. The second column shows the
No attempt was made to match the patient populations
results obtained in the group of patients at TMC-E
of the two institutions, although it is believed that they
treated by physicians with no previous exposure to the
are similar in many respects. Both hospitals, for exam-
ple, provide care to patients in the lower socioeconomic docent clinical pharmacist. Column 3 shows the results
class; however, TMC-W cares for more black patients obtained in a small group of patients who were treated
than does TMC-E. by physicians who had previous exposure to the docent
clinical pharmacist, and column 4 shows the results ob-
The standard accepted treatment for streptococcal
tained in a group of patients at TMC-E after the addi-
pneumonia was obtained from The Medical Letter
"Antimicrobial Therapy."> The drug regimen of choice tion of the clinical pharmacist. Statistically significant
is a 10- to 14-day course of penicillin: procaine penicillin differences in cost of raw antibiotics, total cost for an-
600000 U im q12h for 1-4 days followed by penicillin tibiotic administration, daily raw cost for antibiotics,
VK 250 mg po q6h to complete the 10- to 14-day course. total raw cost for antibiotic administration, and patient
charges were apparent.
In patients allergic to penicillin, the drug regimen of
choice for streptococcal pneumonia is a 10- to 14-day Table 2 compares TMC-W with the total population
course of erythromycin ethylsuccinate 500 mg po q6h. of patients treated at TMC-E prior to the hiring of the
clinical pharmacists. In combining the populations
Each chart was examined by clinical pharmacy
previously listed separately in columns 2 and 3 in Table
students, a resident or faculty member, and one of the
physician coinvestigators. (The two coinvestigators 1, the contamination of the study population by
previous exposure to the docent clinical pharmacist is
were, at the time of the study, medical directors for the
respective institutions and practicing internists.)
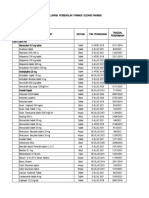
The cost for all pharmaceutical products was ob- Table 1. Comparison of TMC-W and TMC-E
tained from the 1974 TMC hospital bid prices. Daily with and without the Docent Clinical Pharmacist
inpatient costs for antibiotics and intravenous solutions,
with or without piggy-back infusion sets, were TMC-E No Pharm 0
calculated. At the beginning of the study, the pharmacy Pharm 0 Pharm 0 C Pharm 0 Education
TMC-W TMC-E Education TMC-E
had no centralized intravenous additive service; all in-
n 12 7 4 8
travenous solutions were prepared by the nurse direct-
length of Stay 8.33 5.86 3.25 12.25
lyon the unit. Subsequently, the pharmacy initiated an S.D. 4.54 5.0.2.12 S.D. 1.84 S.D. 9.96
intravenous additive program, charging a fee of $15 for Raw Dru9 Cost 9.23 7.29 4.91 116.43
all intravenous solutions, $2 for all intramuscular in- S.D. 9.60 5.0.3.27 S.D. 5.95 S.D. 149.53 •
jections or medications administered by intravenous Raw Cost of 7.83 6.80 2.13 28.26
Additive S.D. 9.39 5.0.5.29 S.D. 4.25 S.D. 36.12
push, and $0.60 for all oral medications. The results of
this study reflect the system currently used to determine Total Raw Cost 17.0 14.11 37.41 408.69
S.D. 17.71 5.0.7.73 5.0.65.80 S.D. 592.94 •
patient medication charges. Raw Cost of 1.24 1.46 1.06 8.11
Statistical comparisons were made between TMC- Drug Per Day S.D. 1.03 5.0.0.99 S.D. 0.87 S.D. 7.51 •
E, both with and without physician exposure to a clinical
pharmacist, and TMC-W.
Total Raw Cost
Per Day S.D.
2.38
2.11
280
5.0.2.13
6.47
5.0.11.64 5.0
32.63
3961
.
Patient 149.60 112.69 41.50 520.35
The Mann-Whitney U test and the Kruskal- Wallis Charge S.D. 159.81 5.0.94.36 5.0.72.70 S.D. 600.13 •
test were utilized to compare, statistically, the costs
calculated in this study. The calculations were per- • Statistically significant with P < 0.05 (Kruskal Wallis test)
588
Downloaded from aop.sagepub.com at Purdue University on June 5, 2016
DOCENT CLINICAL PHARMACIST
Table 2. Comparison of TMC-W with TMC-E Table 3. Comparison of TMC-W with Subgroup
before Hiring a Clinical Pharmacist at TMC-E with No Exposure to the
Docent Clinical Pharmacist
TMC-W TMC-East
Pharm.D No Pharm 0 TMC-E with
TMC-W No Pharm D
Pharm 0 Education
n 12 12
12 8
length of Stay 8.33 9.25
5.0.4.54 5.0.9.16 length of Stay 8.33 12.25
S.D. 4.54 S.D. 9.96
Raw Drug Cost 9.23 79.26
5.0.9.60 S.D. 131.55
Raw Drug Cost 9.23 116.43
Raw Cost for 7.83 19.55 S.D. 9.60 5.0.149.53*
Additive 5.0.9.39 5.0.31.63
Raw Cost for 7.83 28.26
Additive S.D. 9.39 S.D. 36.12
Total Raw Cost 17.02 284.10
S.D. 17.71 5.0.505.84
Total Raw Cost 17.02 408.69
Raw Cost of 1.24 5.76 5.0.17.71 S.D. 592.94 *
Drug Per Day S.D. 1.03 S.D. 6.94 *
Raw Cost of 1.24 8.11
Drug Per Day S.D. 1.03 S.D. 7.51 *
Total Raw Cost 2.38 23.91
Per Day 5.0 2.11 S.D. 34.66
Total Raw Cost 2.38 32.63
Per Day S.D. 2.11 S.D. 39.61 *
Patient Charge 149.60 361.57
S.D. 159.81 5.0.577.84
Patient Charge 149.60 520.35
5.0.159.81 5.0.600.13 *
• Statistically significant with Pe 0.05 (Mann Whitney U test)
..
• StatIstIcally SIgnifIcant wIth peO.05 (Mann WhItney U test)
evident. Table 2 shows a consistent pattern with the
previous comparison; however, only the raw cost of
drug per day was significantly different, statistically. Table 4. Apparent Sustained Influence of Teaching
Table 3 compares TMC-W with the subgroup of pa- Program by the Docent Clinical Pharmacist
tients at TMC-E treated by physicians not previously
exposed to the docent clinical pharmacist. Thus, Table TMC-E TMC-E
3 clarifies the source of significant differences shown No Prior
in the cross-group comparison. There was a statistical- Pharm 0 Pharm 0
ly significant difference in the raw cost of antibiotics, Education Education
the total raw cost for administering the antibiotics, the Number of Patients 8 4
raw cost for the antibiotics given daily, the total raw
length of Stay 12.25 3.25
cost per day for antibiotic administration, and the pa- S.D. 9.96 S.D. 1.84
tient charge.
Table 4 shows the apparent sustained influence of a Raw Drug Cost 116.43 4.91 *
teaching program, provided by the docent clinical phar- 5.0.149.79 S.D. 5.95
macist, in a small population sample. At TMC-E, when
Raw Cost for 28.26 2.13
comparisons were made between data for patients Additive S.D. 36.12 S.D. 4.25
treated by physicians with previous exposure to the do-
cent clinical pharmacist and patients treated by physi- 37.41
Total Raw Cost 408.69 *
cians with no prior exposure, the difference in the raw 5.0.592.94 S.D. 70.80
cost of antibiotics, the total raw cost for administering
the antibiotics, the raw cost for the antibiotics on a daily Raw Cost of Drug 8.11 1.06 *
basis, the total raw cost per day for antibiotic ad- Per Day S.D. 7.51 S.D. 0.87
ministration, and the patient charge was statistically
significant. Total Raw Cost 32.63 6.47 *
Table 5 shows a comparison of TMC-E, prior to hir- Per Day S.D. 39.61 S.D. 11.64
ing the docent clinical pharmacist, with TMC-E after
Patient Charge 520.35 41.50 *
the clinical pharmacist was added to the Department of 5.0.600.13 S.D. 72.35
Medicine staff. There was a statistically significant dif-
ference in the raw cost of antibiotics, the total raw cost • Statistically significant with P eO.05 (Mann Whitney U test)
Drug Intelligence and Clinical Pharmacy VOL 16 JULY/AUG 82 589
Downloaded from aop.sagepub.com at Purdue University on June 5, 2016
Table 5. Comparison of TMC-E before and after penicillin therapy is considerably cheaper than in-
Hiring a Docent Clinical Pharmacist travenous infusion, the clinical pharmacist recommend-
ed oral penicillin as soon as the patient was able to take
Prior to Pharm 0 Post Pharm 0 medications by mouth. This one factor dramatically in-
TMC-E TMC-E fluenced the cost of antibiotic therapy.
n 72 7 Drug-drug, drug-disease, and drug-laboratory in-
length of Stay 9.25 5.86 teractions can significantly influence patient manage-
S.D. 9.16 S.D. 2.12
ment and hospital stay. In this study, the only signifi-
Raw Drug Cost 79.26 7.29 * cant drug-drug and drug-disease interactions were found
S.D. 131.55 S.D. 3.27
at TMC-E prior to the hiring of the clinical pharmacist.
Raw Cost for 19.55 6.80 For example, one patient was placed initially on am-
Additive S.D. 31.63 S.D. 5.29 picillin for the treatment of streptococcal pneumonia
Total Raw Cost 284.10 14.11 * and developed a rash. The patient was hyperuricemic
5.0.505.84 S.D. 7.73 at the time of admission, which may have contributed
Raw Cost of 5.76 1.46 * to what was interpreted as an allergic reaction to
Drug Per Day S.D. 6.94 S.D. 0.99 penicillin. Consequently, a more expensive antibiotic
was substituted. None of the patients admitted to this
Total Raw Cost 23.91 2.80 *
Per Day S.D. 34.66 S.D. 2.13 study was noted to have a penicillin allergy; however,
second-line antibiotics were frequently employed in the
Patient 361.57 112.69 * initial phase of this study at TMC-E, where there was
Charge 5.0.577.84 S.D. 94.36
no clinical pharmacist. In one case, combination therapy
• Statistically significant with peO.OS (Mann Whitney U test) with a cephalosporin and aminoglycoside was initiated.
This combination may have been responsible for the pa-
for antibiotic administration, the raw cost for antibiotics tient's subsequent development of renal problems.v'
on a daily basis, the total raw cost per day for antibiotic although the significance of this interaction is
administration, and the patient charge. questionable.v" If one compares the length of hospital-
Table 6 compares drug selection for the treatment of ization at TMC-W with TMC-E prior to and after the
streptococcal pneumonia at: TMC-W with the docent hiring of the docent clinical pharmacist, a trend toward
clinical pharmacist, TMC-E with physicians previously .a shorter hospital stay is noted for those patients in the
exposed to the docent clinical pharmacist, TMC-E with institution at which a clinical pharmacist was present.
physicians not previously exposed to the docent clinical While it is impossible to substantiate a cause and effect
pharmacist, and TMC-E after the addition of the do- relationship between the hospital stay and the contribu-
cent clinical pharmacist. It is important to realize that tion of the clinical pharmacist, drug-related complica-
none of the patients reviewed in this study had a history tions may have influenced the length of stay of those
of penicillin allergy. There was a statistically significant patients treated at TMC-E prior to the hiring of the
difference in drug choice between physicians without clinical pharmacist.
prior exposure to the docent clinical pharmacist and The docent clinical pharmacist does have significant
physicians practicing with or previously exposed to the educational responsibilities for the basic and clinical
docent clinical pharmacist. pharmacology instruction provided at TMC-W. This has
been described elsewhere.10 Despite the small sample size
Discussion for this four-year study, the data in Table 1 indicate that
those physicians who received a portion of their educa-
After all the criteria were met, the final sample size tion or training with the docent clinical pharmacist
of this study was relatively small. Additionally, in com- tended to prescribe drugs in a more cost-effective man-
paring two institutions with affiliation agreements, one
might anticipate cross-over contamination to influence Table 6. Comparison of Drug Selection for Treatment
the outcome. This contamination may have been a fac- of Streptococcal Pneumonia in TMC-W and TMC-E
tor in the antibiotic selection process at the two institu-
tions. For some, it may be difficult to perceive a cause
Number Non
and effect relationship between the presence of the do- o( Penicillin Penicillin
cent clinical pharmacist and the prescribing practices Patients
utilized in these two institutions without first recogniz-
TMC-W
ing that the docent clinical pharmacists in these institu- with Pharm 0 12 12 0
tions function as part of the attending staff. Examina-
tion of the various data subsets consistently indicates TMC-E
No Pharm 0 8 0 8
significant differences between the prescribing practices
of those physicians exposed to the clinical pharmacist TMC-E
and those who are not. Antibiotic costs are influenced trained with 4 4 0
Pharm 0
not only by the selection of the specific antibiotic but
also by the method of administration. In this institu- TMC-E 7 7 0
tion, the method by which the antibiotics were ad- with Pharm 0
ministered contributed significantly to the overall pa- Note: None of the patients had history of penicillin allergy
tient charge. Inasmuch as oral or intramuscular Statistically significant PeO.OOl (Ch. Square test X'= 38.83)
590
Downloaded from aop.sagepub.com at Purdue University on June 5, 2016
ner. However, it obviously would be inappropriate to Revised & Updated, July 1981
overstate the significance of this finding, based on such
a small sample.
Although it is impossible to control all the indepen- PSYCHOTROPIC
dent variables that may have contributed to the dif-
ferences in this study (e.g., the immunocompetence of DRUG HANDBOOK
the patient or the patient's condition on admission to Third Edition
the hospital), one significant variable needs to be con-
sidered: the attending physician staff. During the initial Paul J. Perry, Ph.D. Bruce Alexander, Pharm.D.
phase of study at TMC-E, the attending staff included Associate Professor Clinical Assistant Professor
physicians who currently hold academic appointments The University of Iowa The University of Iowa
College of Pharmacy College of Pharmacy
at this medical center. and and
During these two study periods, no patient was re- Clinical Pharmacist Clinical Pharmacist
admitted to either institution for pneumonia during the Psychiatric Hospital Psychiatry Service
Iowa City. Iowa Iowa City VA Medical Center
six months following the study period. Thus, the more Iowa City, Iowa
economical approach to the treatment of pneumonia ap-
peared to be successful. Barry I. Liskow, M.D.
Chief. Alcohol Dependency Treatment Unit
This study is one of many internal reviews that have Kansas City VA Medical Center
been conducted over the past ten years to evaluate the Kansas City, Missouri
impact of the docent clinical pharmacist on patient care and
Associate Professor
in this institution. Results to date have been encourag- Department of Psychiatry
ing. Plans for the future include comparison of the University of Kansas
results of this study with studies at other similar institu- Kansas City, Kansas
tions in this region of the country. ~ A quick reference gUide on drugs used for treating psychiatric
patients. Includes cost comparisons. drug Interaction tables.
patient Instruction section. rational prescribing principles. and
KEY WORDS: docent clinical pharmacists.
other practical Information and clinical data.
TABLE OF CONTENTS
ABSTRACT I. General Principles - Therapeutic Use
This two-phase retrospective study was designed to evaluate 2. General Principles - Adverse Effects
the impact of the clinical pharmacist on prescribing practice 3. Antipsychotics
of physicians in an internal medicine service. Streptococcal 4. Antidepressants
(pneumococcal) pneumonia was chosen as the model disease 5. lithium
state. The drug of choice was used more frequently and 6. Antianxiety Agents
there was a statistically significant difference in raw cost 7. Hypnotics
of antibiotic, total cost for antibiotic administration, daily 8. Analgesics
raw cost for antibiotics; total raw cost for antibiotic adminis- 9. Agents for Treating Extrapyramidal Side Effects
tration, and patient charges when physicians were exposed to 10. Disulfiram
the clinical pharmacists' influence. I I. Drug Interactions
j 2. Management and Treatment of Drug Overdosage
13. Management of Withdrawal
References 14. Amy tal interview
15. Electroconvulsive Therapy
I. Dimond EG. The academic plan for the school of medicine.
16. Patient Instructions
Kansas City: University of Missouri-Kansas City, 1977.
2. Counts GW. Review and control of antimicrobial usage in 204 pages, soft cover, 41f2 x 6 3k inches.
hospitalized patients. A recommended collaborative approach. JAMA Send check, money order or credit card number
1977;238:2170-4. (MasterCard or Visa) to:
3. Simmons HE, Stolly PD. This is medical progress? Trends and
consequences of antibiotic use in the United States. JAMA HARVEY WHITNEY BOOKS PRICE $9.50
1974;227: 1023-8. . (plushandling and postage
P.O. BOX 42442 If not prepaid)
4. Sherris JC, The epidemiologyof drug resistance. In: Brachman Prepayment IS required
PS, Eickhoff TC, eds. Proceedings of the International Conference CINCINNATI, OH 45242 for individual orders.
of Nosocomial Infections. Baltimore: WaverlyPress, Inc., 1971: 50-60.
5. The medical letter on drugs and therapeutics. Handbook on
antimicrobial therapy. New Rochelle,NY: MedicalLetter, Inc. Revised Send _ _ copies at $9.S0 each of PSYCHOTROPIC DRUG
edition, 1976. HANDBOOK to:
6. Borrows SN. Anuria and acute tubular necrosis associated with Name
gentamicin and cephalothin. JAMA 1972;222:1546-7.
7. Fillastre lP, Laumonier R, et al. Acute renal failure associated Address _
with combined gentamicin and cephalothin therapy. Br Med J
1973;2:396.
8. Fanning WL, Gump 0, lick H. Gentamicin and cephalothin
associated rises in blood urea nitrogen. Antimicrob Agents Chemother City
1976;10:80-3. State/Country Z,p _
9. Luft FC, Patel V, Yum MN, Kleit SA. Nephrotoxicity of
cephalosporin-gentamicin combinations in rats. Antimicrob Agents o payment enclosed: 0 please bill 0 VISA D MasterCard
Chemother 1976;9:831-9. Exp. date Signature
10. Covinsky 10. The role of the clinical pharmacist in medical Acct.
education. J Clin Pharmacol 1981;21:198-200. No.
Drug Intelligence and Clinical Pharmacy VOL 16 /ULY/AUG82 591
Downloaded from aop.sagepub.com at Purdue University on June 5, 2016
Вам также может понравиться
- Management of Medical Technology: A Primer for Clinical EngineersОт EverandManagement of Medical Technology: A Primer for Clinical EngineersРейтинг: 5 из 5 звезд5/5 (1)
- Common AbbreviationsДокумент15 страницCommon AbbreviationsKronii OuroОценок пока нет
- Management of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)От EverandManagement of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)Оценок пока нет
- Daftar Obat Aman Dan Bahaya Ibu HamilДокумент8 страницDaftar Obat Aman Dan Bahaya Ibu HamilAnnida Nurul Haq80% (5)
- Improving Outcomes in Chronic Obstructive Pulmonary Disease: Optimizing Maintenance Therapy Across Health Care SettingsОт EverandImproving Outcomes in Chronic Obstructive Pulmonary Disease: Optimizing Maintenance Therapy Across Health Care SettingsОценок пока нет
- UPenn Foreign Donations For Fiscal Year 2021Документ9 страницUPenn Foreign Donations For Fiscal Year 2021JoeSchoffstallОценок пока нет
- Therapeutic Guidelines in Systemic Fungal Infection. 3rd Ed.Документ127 страницTherapeutic Guidelines in Systemic Fungal Infection. 3rd Ed.PrisОценок пока нет
- Pharmaceutical QBD (Final)Документ41 страницаPharmaceutical QBD (Final)Tahsin AhmedОценок пока нет
- Cleaning Validation (CV) Procedure and Protocol - Guideline SOPsДокумент30 страницCleaning Validation (CV) Procedure and Protocol - Guideline SOPsDeepakОценок пока нет
- Report Analysis Lentin Commission Report On The Glycerol Tragedy at The J.J. Hospital, Bombay (Lentin Commission Report)Документ4 страницыReport Analysis Lentin Commission Report On The Glycerol Tragedy at The J.J. Hospital, Bombay (Lentin Commission Report)sohel alamОценок пока нет
- Clinical Trial PhasesДокумент11 страницClinical Trial Phasesheyyo ggОценок пока нет
- First Name Last Name Title Email AddressДокумент111 страницFirst Name Last Name Title Email AddressDebjani DuttaОценок пока нет
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareОт EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareОценок пока нет
- Articulo NeumoniaДокумент7 страницArticulo NeumoniaEd BarajasОценок пока нет
- CMA AntibioticsДокумент11 страницCMA AntibioticsNovita Oktavianti DehiОценок пока нет
- Determinants of Vancomycin Use in Adult Intensive Care Units in 41 United States HospitalsДокумент7 страницDeterminants of Vancomycin Use in Adult Intensive Care Units in 41 United States HospitalsGayan KarunanandaОценок пока нет
- WSC Abstracts - 2011Документ667 страницWSC Abstracts - 2011cyber_zac52Оценок пока нет
- Using Antibiograms To Improve Antibiotic PrescribingДокумент7 страницUsing Antibiograms To Improve Antibiotic PrescribingfaradillasuciОценок пока нет
- Jamda: Original StudyДокумент6 страницJamda: Original StudyNami NakanoОценок пока нет
- See Also Page 1013: ESS S OREДокумент3 страницыSee Also Page 1013: ESS S ORESundas EjazОценок пока нет
- British Journal of Clinical PharmacologyДокумент6 страницBritish Journal of Clinical PharmacologyJunerey Hume Torres RodriguezОценок пока нет
- Preventing Ventilator-Associated ICHEДокумент8 страницPreventing Ventilator-Associated ICHEFelix Brian FelixОценок пока нет
- Medicine American Journal of Hospice and PalliativeДокумент6 страницMedicine American Journal of Hospice and Palliativem1k0eОценок пока нет
- Apakah Pemberian Antibiotic Berpengaruh Terhadap Batuk Orang DewasaДокумент14 страницApakah Pemberian Antibiotic Berpengaruh Terhadap Batuk Orang DewasaIzza Aliya KennedyОценок пока нет
- National Trends in The Use of S by Primary Care Physicians For Adult Patients WithДокумент12 страницNational Trends in The Use of S by Primary Care Physicians For Adult Patients WithIzza Aliya KennedyОценок пока нет
- Neumonia Asosiada A VentiladorДокумент11 страницNeumonia Asosiada A VentiladorYnomata RusamellОценок пока нет
- Steinberg 2009Документ7 страницSteinberg 2009majedОценок пока нет
- Clinical Microbiology and InfectionДокумент6 страницClinical Microbiology and InfectionAccel XtremeОценок пока нет
- Clinical Practice Guideline Safe Medication Use.32Документ39 страницClinical Practice Guideline Safe Medication Use.32Edward ZiyachechaОценок пока нет
- Jurnal Interna UTIДокумент8 страницJurnal Interna UTIErdika Satria WahyuonoОценок пока нет
- National Ambulatory Antibiotic Prescribing Patterns For Pediatric Urinary Tract Infection, 1998 - 2007Документ9 страницNational Ambulatory Antibiotic Prescribing Patterns For Pediatric Urinary Tract Infection, 1998 - 2007Rodolfo Rodriguez CamposОценок пока нет
- Prescribing Patterns and Pharmacoeconomic Analysis of Drugs Used in Pediatric Asthma Patients at Tertiary Care HospitalДокумент18 страницPrescribing Patterns and Pharmacoeconomic Analysis of Drugs Used in Pediatric Asthma Patients at Tertiary Care Hospitalrajesh sumanОценок пока нет
- Makro LidДокумент7 страницMakro Liddoc_aswarОценок пока нет
- Antibiotic Prescribing During Pediatric Ambulatory Care Visits For AsthmaДокумент8 страницAntibiotic Prescribing During Pediatric Ambulatory Care Visits For AsthmameriatmajaОценок пока нет
- Risk Factors For Ventilator-Associated Events - Liu 2019Документ6 страницRisk Factors For Ventilator-Associated Events - Liu 2019Maxi BoniniОценок пока нет
- Alok A. Khorana - Incidence and Predictors of Venous Thromboembolism (VTE) Among Ambulatory High-RiskДокумент8 страницAlok A. Khorana - Incidence and Predictors of Venous Thromboembolism (VTE) Among Ambulatory High-RiskFarid RakhmanОценок пока нет
- Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired PneumoniaДокумент5 страницAtients Hospitalized After Initial Outpatient Treatment For Community-Acquired PneumoniaMazKha BudОценок пока нет
- AnnalsATS 201605-398OCДокумент8 страницAnnalsATS 201605-398OCRodrigoSachiFreitasОценок пока нет
- Vail Et Al 2016 Epidemiology of Vasopressin Use For Adults With Septic ShockДокумент8 страницVail Et Al 2016 Epidemiology of Vasopressin Use For Adults With Septic ShockWend Panga CongoОценок пока нет
- Procalcitonin and AB DecisionsДокумент10 страницProcalcitonin and AB DecisionsDennysson CorreiaОценок пока нет
- Peters 2017Документ5 страницPeters 2017Friska Permatasari NababanОценок пока нет
- Ad Hoc Data SourcesДокумент11 страницAd Hoc Data SourcesVINAY KUMARОценок пока нет
- Cancer Immunotherapy Trials Leading A Paradigm Shift in Drug DevelopmentДокумент8 страницCancer Immunotherapy Trials Leading A Paradigm Shift in Drug Development49qmzqdpndОценок пока нет
- Walk 2020Документ19 страницWalk 2020Marcus ShawОценок пока нет
- Effect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyДокумент8 страницEffect of A Centralized Clinical Pharmacy Anticoagulation Service On The Outcomes of Anticoagulation TherapyDyla FaradhylaОценок пока нет
- Clin Infect Dis.-2007-Dellit-159-77Документ19 страницClin Infect Dis.-2007-Dellit-159-77Melo PerezОценок пока нет
- FN 2011 IdsaДокумент38 страницFN 2011 IdsaNuttawath UngwichanpunyaОценок пока нет
- Clinical Practice Guideline For The Use of Antimicrobial Agents in Nutropenic Patients CID 11Документ38 страницClinical Practice Guideline For The Use of Antimicrobial Agents in Nutropenic Patients CID 11Mariela ColomboОценок пока нет
- MДокумент6 страницMMathilda UllyОценок пока нет
- Amira PresuurevulcerДокумент59 страницAmira PresuurevulcerrantiОценок пока нет
- Art 09Документ9 страницArt 09Francisca DonosoОценок пока нет
- Ab Round StewardshipДокумент7 страницAb Round StewardshipbpinsaniОценок пока нет
- Resistensi AntibiotikДокумент21 страницаResistensi AntibiotikMaruliTuaОценок пока нет
- Rota Vietnam EE FisherДокумент7 страницRota Vietnam EE FisherKartavya TiwariОценок пока нет
- Prevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsДокумент10 страницPrevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsAkshayОценок пока нет
- Vandergarde Thorax2006Документ5 страницVandergarde Thorax2006Oneng IfayaniОценок пока нет
- 55-Article Text-103-1-10-20200408Документ7 страниц55-Article Text-103-1-10-20200408Kshitiz112Оценок пока нет
- 2013 Surgical Prophylaxis ASHP, IDSA, SHEA, SISДокумент8 страниц2013 Surgical Prophylaxis ASHP, IDSA, SHEA, SISMara Medina - BorleoОценок пока нет
- Analisis Minimalisasi Biaya (CMA)Документ7 страницAnalisis Minimalisasi Biaya (CMA)diahsaharaОценок пока нет
- Medication Error Patients Admitted To Medical Ward in Primary Hospital, Ethiopia: Prospective Obserbetional StudyДокумент18 страницMedication Error Patients Admitted To Medical Ward in Primary Hospital, Ethiopia: Prospective Obserbetional StudybezieОценок пока нет
- Moxifloxaxin For CAPДокумент9 страницMoxifloxaxin For CAPmateri posОценок пока нет
- HOSPITAl PHARMACOEPIDEMIOLOGYДокумент6 страницHOSPITAl PHARMACOEPIDEMIOLOGYDhruvi PatelОценок пока нет
- Kumar 2006Документ8 страницKumar 2006aiturraldeОценок пока нет
- Efficacy of Clinacanthus Nutans Extracts in PatientsДокумент7 страницEfficacy of Clinacanthus Nutans Extracts in Patientsconrad9richterОценок пока нет
- The Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioДокумент7 страницThe Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioMaharaniОценок пока нет
- Drug Utilisation Study of UTIДокумент4 страницыDrug Utilisation Study of UTIviva.anu24Оценок пока нет
- Pittsburgh Lung Conference: PneumoniaДокумент4 страницыPittsburgh Lung Conference: PneumoniaYudha Rental'sОценок пока нет
- Drug Interactions in Infectious Diseases: Mechanisms and Models of Drug InteractionsОт EverandDrug Interactions in Infectious Diseases: Mechanisms and Models of Drug InteractionsManjunath P. PaiОценок пока нет
- Negative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsДокумент8 страницNegative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDaniela HernandezОценок пока нет
- Editorial: Academic Pharmacy Practice and ResearchДокумент3 страницыEditorial: Academic Pharmacy Practice and ResearchDaniela HernandezОценок пока нет
- BMC Health Services Research: Describing The Impact of Health Research: A Research Impact FrameworkДокумент18 страницBMC Health Services Research: Describing The Impact of Health Research: A Research Impact FrameworkDaniela HernandezОценок пока нет
- Special Features: Opportunities and Responsibilities in Pharmaceutical CareДокумент11 страницSpecial Features: Opportunities and Responsibilities in Pharmaceutical CareDaniela HernandezОценок пока нет
- 38 PDFДокумент9 страниц38 PDFDaniela HernandezОценок пока нет
- 42 PDFДокумент5 страниц42 PDFDaniela HernandezОценок пока нет
- Individualized Pharmacokinetic Monitoring Results in Less Aminoglycoside-Associated Nephrotoxicity and Fewer Associated CostsДокумент9 страницIndividualized Pharmacokinetic Monitoring Results in Less Aminoglycoside-Associated Nephrotoxicity and Fewer Associated CostsDaniela HernandezОценок пока нет
- Ractice Nsights: The Critical Care Pharmacist: An Essential Intensive Care PractitionerДокумент5 страницRactice Nsights: The Critical Care Pharmacist: An Essential Intensive Care PractitionerDaniela HernandezОценок пока нет
- Research/Practice ReportsДокумент4 страницыResearch/Practice ReportsDaniela HernandezОценок пока нет
- 集中治療室における薬剤師による MRSA 感染症治療への介入効果: a ,c a b b c a ,cДокумент8 страниц集中治療室における薬剤師による MRSA 感染症治療への介入効果: a ,c a b b c a ,cDaniela HernandezОценок пока нет
- Pharmacy Practice InsightsДокумент11 страницPharmacy Practice InsightsDaniela HernandezОценок пока нет
- Evidence of The Economic Benefit of Clinical Pharmacy Services: 1996-2000Документ20 страницEvidence of The Economic Benefit of Clinical Pharmacy Services: 1996-2000Daniela HernandezОценок пока нет
- Dissolution - A Quality Parameter For Testing of Pharmaceutical Dosage FormДокумент10 страницDissolution - A Quality Parameter For Testing of Pharmaceutical Dosage FormFaisal AbbasОценок пока нет
- Rudan Systems 230117Документ21 страницаRudan Systems 230117Marco ManzoОценок пока нет
- Chemistry Homework #2Документ2 страницыChemistry Homework #2Own AbbadiОценок пока нет
- 905 Uniformity of Dosage UnitsДокумент10 страниц905 Uniformity of Dosage UnitsIcee SinlapasertОценок пока нет
- Buffer Stock Maret1Документ22 страницыBuffer Stock Maret1Selvi RatnasariОценок пока нет
- Drug Registration Guidance Document DRGD - Second Edition Revised - July 2019Документ710 страницDrug Registration Guidance Document DRGD - Second Edition Revised - July 2019Revathy ThandapaniОценок пока нет
- 2-3 Assessing Specs - FPPДокумент41 страница2-3 Assessing Specs - FPPyolandatyasОценок пока нет
- Sar Loop DiureticsДокумент2 страницыSar Loop DiureticsTikendraОценок пока нет
- Saturation Kinetics: Prepared and Presented by Mohammed Muzammil 1 Year Mpharm Department of PharmacologyДокумент28 страницSaturation Kinetics: Prepared and Presented by Mohammed Muzammil 1 Year Mpharm Department of PharmacologyMaaz Uddin SiddiquiОценок пока нет
- Pcog Notes (Alkaloids II)Документ4 страницыPcog Notes (Alkaloids II)sadburgerОценок пока нет
- Warehouse Split 4Документ95 страницWarehouse Split 4reliefdailymailОценок пока нет
- Dossier Preparation Requirements For Generic Drugs of Us Europe IndiaДокумент13 страницDossier Preparation Requirements For Generic Drugs of Us Europe IndiaTuyến Đặng ThịОценок пока нет
- IMPORTACIONESДокумент11 страницIMPORTACIONESCinthia Chavez MaldonadoОценок пока нет
- Dispensadores Bigfarma1Документ5 страницDispensadores Bigfarma1Milagros AliffОценок пока нет
- In Vitro Studies On Release and Human Skin Permeation of Australian Tea Tree Oil (TTO) From Topical FormulationsДокумент7 страницIn Vitro Studies On Release and Human Skin Permeation of Australian Tea Tree Oil (TTO) From Topical FormulationsEng.Químico SCОценок пока нет
- DR Hemanth S NaikДокумент48 страницDR Hemanth S NaikElfiaNeswitaОценок пока нет
- ATC/DDD Classification (Temporary) : New ATC 5th Level CodesДокумент7 страницATC/DDD Classification (Temporary) : New ATC 5th Level CodesLola AgustianaОценок пока нет
- Genotoxicity of Drugs Mechanisms, Testing Guidelines and Methods For EvaluationДокумент8 страницGenotoxicity of Drugs Mechanisms, Testing Guidelines and Methods For Evaluationyogesh ushirОценок пока нет
- A. Gudang Farmasi 2023 (Feni Dwi) UpdateДокумент882 страницыA. Gudang Farmasi 2023 (Feni Dwi) UpdatehefikurniasariОценок пока нет
- Civic Drive, Filinvest City, Alabang 1781 Muntinlupa, PhilippinesДокумент2 страницыCivic Drive, Filinvest City, Alabang 1781 Muntinlupa, PhilippinesRegulatory CPGОценок пока нет
- SUPAC Guidelines PPT - 2Документ19 страницSUPAC Guidelines PPT - 2Sparsh SharmaОценок пока нет
- Nirav Industrial Training Ppt-1.NewДокумент15 страницNirav Industrial Training Ppt-1.NewMehul ThakkarОценок пока нет