Академический Документы
Профессиональный Документы
Культура Документы
175086-Article Text-448016-1-10-20180724 PDF
Загружено:
Tanya PinedaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
175086-Article Text-448016-1-10-20180724 PDF
Загружено:
Tanya PinedaАвторское право:
Доступные форматы
Bain and Kongnyuy Legal and ethical aspects of MDSR
COMMENTARY
Legal and Ethical Considerations during Maternal Death
Surveillance and Response
DOI: 10.29063/ajrh2018/v22i2.2
Luchuo Engelbert Bain1,2* and Eugene Justine Kongnyuy3
Vrije Universiteit, Faculty of Science, Athena Institute for Research on Innovation and Communication in Health
and Life Sciences, Amsterdam, The Netherlands1; Centre for Population Studies and Health Promotion, Yaounde,
Cameroon2; United Nations Population Fund (UNFPA), Abuja, Nigeria3
*For Correspondence: Email: lebaiins@gmail.com; Phone: +31(0)205989170
Abstract
Maternal death surveillance and response (MDSR) is a promising strategy, to identify record and track key drivers of maternal
deaths. Despite its potential in reducing maternal mortality, ethical and legal challenges need to be properly ascertained and acted
upon, to guarantee its acceptability, sustainability, and effectiveness. This paper proposes a legal and ethical framework to guide
practitioners and researchers through the MDSR process. Three (03) categories of both legal and ethical issues are discussed:
namely the issues related to data, people and use of findings. Most challenges of the MDSR strategy have ethical and legal
underappraisal origins, the most outstanding being the low maternal death notification rates. Efforts should be made for
respondents to properly understand the rationale for the process, and how the data obtained will be put into use. Dispelling fears
of possible litigation remains fundamental in obtaining quality data. Health care providers involved in the process need to
understand their ethical and legal responsibilities, as well as privileges (legal protection). It is hoped that this framework will
offer a structure to guide professionals in improving MDSR implementation and research. (Afr J Reprod Health 2018; 22[2]: 17-
25).
Keywords maternal death surveillance, mortality, legal, ethical
Résumé
La surveillance et l‘intervention en cas des décès maternels (SIDM) constituent une stratégie prometteuse pour identifier et
enregistrer les principaux facteurs de mortalité maternelle. En dépit de son potentiel de réduction de la mortalité maternelle, les
défis éthiques et juridiques doivent être correctement établis et mis en pratique, afin de garantir leur acceptabilité, leur durabilité
et leur efficacité. Cet article propose un cadre juridique et éthique pour guider les praticiens et les chercheurs dans le processus de
la SIDM. Trois (03) catégories de questions juridiques et éthiques sont discutées: à savoir les questions liées aux données, aux
personnes et à l'utilisation des résultats. La plupart des défis de la stratégie SIDM ont des origines éthiques et juridiques sous-
évaluées, les plus remarquables étant les faibles taux de notification des décès maternels. Des efforts devraient être faits pour que
les répondants comprennent correctement la raison d'être du processus et comment les données obtenues seront utilisées. Dissiper
les craintes d'éventuels litiges reste fondamental pour obtenir des données de qualité. Les fournisseurs de soins de santé impliqués
dans le processus doivent comprendre leurs responsabilités éthiques et légales, ainsi que leurs privilèges (protection juridique).
On espère que ce cadre offrira une structure pour guider les professionnels dans l'amélioration de la mise en œuvre et de la
recherche en matière de la SIDM. (Afr J Reprod Health 2018; 22[2]: 17-25).
Mots-clés: surveillance de la mortalité maternelle, mortalité, juridique, éthique
African Journal of Reproductive Health June 2018; 22 (2):17
Bain and Kongnyuy Legal and ethical aspects of MDSR
Introduction manner to guarantee its acceptability,
sustainability, and effectiveness.
Maternal mortality remains unacceptably high, While the right of parents to determine freely and
with about 830 women dying from preventable responsibly the number and spacing of their
pregnancy- or childbirth-related complications children was first articulated in the 1968 UN
every day. Maternal death is the death of a woman International Conference on Human Rights, the
while pregnant or within 42 days of termination of right of women to go through pregnancy and
pregnancy, irrespective of the duration and site of childbirth safely was first made explicit only in
the pregnancy, from any cause related to or 1994 as part of the Programme of Action of the UN
aggravated by the pregnancy or its management International Conference on Population and
but not from accidental or incidental causes1. Over Development, ICPD4. Preventable maternal deaths
99% of these deaths occur in low and middle- seem to be concentrated among marginalized
income countries (LMICs) 1. One target under groups of women and they are marked by a lack of
Sustainable Development Goal 3 is to reduce the accountability5. Nationally and internationally,
global maternal mortality ratio to less than 70 per human rights approach incorporated into the
100 000 births, with no country having a maternal strategic package of reducing maternal deaths can
mortality rate of more than twice the global enhance accountability and responsibility5,6,13.
average by 20301. Properly assessing the progress Human rights constitute a bridge between ethics
with regards to reduction in maternal mortality and law. From a justice point of view, it is a
remains a very difficult challenge due to paucity, serious moral – ethical concern that the estimated
non – inclusive, and incorrectness of data, lifetime risk of maternal mortality in high-income
especially from developing countries where most countries is 1 in 3300 in comparison with 1 in 41 in
of these deaths do occur. Maternal death low-income countries7. Amzat has argued that a
surveillance response (MDSR) presents a unique rights-based approach, with special focus on
opportunity to appropriately identify, record and respect of women‘s autonomy, would contribute in
track key drivers of maternal deaths. Routine data alleviating maternal mortality in Africa6. A human
collection at local and national levels is a core rights approach in current efforts to reduce
ingredient of this approach that will permit timely maternal mortality appears plausible, because this
policy changes to properly and specifically curb problem has serious connections with country legal
preventable causes of maternal deaths. Not only systems and health policy frameworks5.
does the MDSR provide a quality control tool for Proper recognition and acting upon the ―no
current policy measures directed at reducing blame, no shame‖ practice during MDSR has the
maternal deaths, MDSR promotes routine potential of curbing under reporting of maternal
identification and timely notification of maternal deaths14-16. This issue has both ethical and legal
deaths and is a form of continuous surveillance components that need to be clearly elucidated and
linking health information system from local to acted upon for the paradigm to achieve its intended
national level2. MDSR will enhance accountability goals. Actors within the MDSR cycle will feel
mechanisms by providing information on whether safer and motivated in ―faithfully‖ reporting and
policies and actions meant to reduce maternal investigating circumstances surrounding maternal
mortality are effective3. Despite the promising deaths without fear of litigation or stigma.
nature of the MDSR approach in reducing maternal Recognizing the legal implications of this endeavor
mortality, ethical and legal challenges need to be warrant schooling of MDSR teams on the legal
properly ascertained and acted upon in a timely guarantees they have as they get the job done, as
African Journal of Reproductive Health June 2018; 22 (2):18
Bain and Kongnyuy Legal and ethical aspects of MDSR
well as making them act more responsibly when it be of interest to future actors in MDSR,
comes to proper handling of privacy and researchers, and policy makers in better dealing
confidentiality issues. Upholding the virtues of with such challenges.
respect, guaranteeing privacy, and confidentiality, In August 2011, the Committee on the
stops the activity from being a mere moral - Elimination of Discrimination against Women
professional responsibility, but also to be an ethical (CEDAW), became the first UN human rights body
mandate in respecting engagements taken before to issue a decision on maternal mortality. They
respondents especially during the verbal - social recognized ensuring availability and proper
autopsies. Failure to properly act on this will not functioning of services that guarantee a safe
only lead to distrust in the health system but pregnancy and childbirth as a fundamental human
endangers future interventions or research right21. The United Nations (UN) Human Rights
activities. In Kenya, it has been highlighted that not Council has highlighted maternal mortality as an
having legislation that clearly articulates the issue bearing not just on development, but also on
―blame free‖ principle hinders attainment of human rights22. Maternal deaths are consequently
MDSR goals, especially when it comes to maternal gross violations of human rights, with shared
death notification8,14-16. The confidential enquiry responsibilities at different strata of society. We
into maternal deaths (CEMD) in the Republic of engage into this debate from a premise that
South Africa could be an example to follow, where challenges encountered during MDSR can be better
review related material (forms, reports etc.) cannot understood and overcome if examined through
be used for litigation or disciplinary processes17. ethical and legal lenses. For instance, maternal
These legal considerations are so important, death notification remains a key obstacle in the
especially when it comes to the terminology that is MDSR cycle8,15. Fear of blame, lack of guarantee
used during the MDSR process. Policy documents of respondent privacy and confidentiality, absence
should be careful regarding avoiding words that of legislation to guarantee that findings will not be
could indirectly have blame implications. In used for litigation purposes could account for low
Malaysia for instance, sub – standard care as a notification rates. The ethical and legal framework
cause of death has been replaced with ―remediable proposed is drawn from the literature, personal and
factors‖. This makes the health care more field experiences of the authors. It is hoped that
comfortable and ready for change, rather than fall this legal and ethical framework will provide a
under weight of blame. The law however needs to structure to guide professionals in improving
draw the line between being accountable and MDSR practice and research.
meeting up to one‘s professional responsibilities15-
17
. The law for instance in the Republic of South Discussion
Africa (1997) and Kenya (2004) makes maternal
death notification mandatory15-8. This can go a long Legal issues during MDSR
way in improving upon the maternal death
notification rates15. The line between responsibility Laws may affect access to information (hospital
and accountability of health care and MDSR staff records), protection of people involved (providers,
can only be clearly drawn with a legal framework, investigators, and family members) in MDSR and
specific to MDSR19. With many countries being at the use of the results. Provisions of the law with
different stages in the MDSR experience, regards to ownership, access and use of medical
highlighting the possible ethical and legal concerns records, protection of health staff involved in the
that could probably arise during the process could MDSR process and potential use of its findings
African Journal of Reproductive Health June 2018; 22 (2):19
Bain and Kongnyuy Legal and ethical aspects of MDSR
need to be clearly defined. Country specific should be kept hidden as much as possible. Legal
guidelines based on existing laws will help reduce backing should be used to prevent the use of
potential tensions that might occur during the information for litigation and members of MDSR
implementation process. committee should decline from giving testimony in
court if they were part of the review. The same
Access to data person should NOT participate in maternal death
reviews and take administrative or legal action
Legal access is generally needed to review hospital against persons involved in clinical care or MDSR
records. Whether all MDSR committee members process. The two processes should be separate and
all have legal access to hospital records should be parallel.
carefully assessed and defined. If all members do,
the potential of sensitive information revealed ―on Litigation
the streets‖ could have serious implications. It
should be the responsibility of the committee It is important for laws to be passed that clearly
members to keep the information secret, and spell out the roles and responsibilities of the
sanctioning those potentially found guilty of MDSR teams, as well as protecting them from
revealing such information should be clearly spelt litigation (immunity). For instance, in sensitive
out, based on the country specific laws. maternal death cases like those arising from
clandestine abortions, without clear laws protecting
Protection of people involved in MDSR both the informants and the data collection team,
there exists a grey zone where without legal
Laws are needed to guarantee the immunity of protection, potential shortcomings of the health
those reviewing maternal deaths and other people care system (staff) and informants might be subject
involved from civil and professional liability. Data to litigation. The law must specify the role of the
gathered during maternal death review needs MDSR team as being not for ―policing‖ and must
protection by law as purely confidential and need protect the informants. Privacy and confidentiality
not be disclosed or used in subsequent lawsuits. must be upheld as legal obligations within the
Safeguards to protect medical records through MDSR package. Without these standards put into
encryption and masking of patient identifiers could law and made known to both the MDSR team and
be used. Working in locked doors and cabinets or the informants, fear might disrupt the optimal
destruction of sensitive physical files (after MDSR functioning of this approach. A clear legal
committee consent) can be carefully evaluated and framework to protect workers is important, but this
used. Conducting periodic data security audits does not in no away disengage them from their
could be a valuable way to ensure safety of responsibilities.
collected data.
Oath taking
Use of findings of MDSR (results)
It might be of interest in some cases for MDSR
The aim of MDSR (and Maternal Death Reviews) committee members to legally go through an oath
is to understand why women die so that preventive taking ritual in court to guarantee that information
strategies can be developed. Results should not be from informants shall remain anonymous and
used to discipline providers or family members of private. This could foster public trust and dispel
the deceased. Patients and provider identifiers fear, offering a unique opportunity for more
African Journal of Reproductive Health June 2018; 22 (2):20
Bain and Kongnyuy Legal and ethical aspects of MDSR
complete information with regards to causes of anonymous: ‗no name, no blame‘ However,
death to be obtained. Verbal autopsies especially complete anonymity is easier for Confidential
narratives from the community could be very Enquiry into Maternal Deaths, but difficult to
informative to improve quality of care. Legal achieve especially in facility-based Maternal Death
experts in developing legislation specific to the Reviews and verbal autopsy. In the absence of
MDSR and countries should look for ways to make complete anonymity, the signing of a
MDSR practitioners, understand the legal confidentiality agreement by those who have
imperative and obligations of upholding participant access to identifiable information should be
privacy and confidentiality. considered.
Ethical Issues Confidentiality
The following are common ethical issues Confidentiality applies to data. It is the obligation
encountered during MDSR: to keep identifiable personal information private.
Permission should be obtained to speak to family
Privacy members and healthcare providers. A clearly
signed interview consent form or obtaining
Privacy applies to the person. Privacy refers to the permission ―on tape‖ could be potential gateways
individual desire to control who has access to to guarantee confidentiality. Identities of the
him/herself. Privacy applies to the person as deceased, relatives and providers should be kept
opposed to confidentiality which applies to data. confidential and known only to those collecting the
Privacy is a person‘s desire of having control over data. Data collection forms, case summaries,
the extent, timing, and circumstances of sharing review meetings and all reports should not contain
oneself (physically, behaviorally, or intellectually) personal identifiers. Documents containing
with others. Individuals have the right to limit personal identity should:
access by others to aspects of their person _ that can
include thoughts and personal information. Taking Not be shared by email,
informed consent from all patients, health care Should be kept in locked office/cabinets
staff, family and community members before (hard copy)
conducting interviews should not only constitute a Password protected files (electronic data).
legal but must be upheld as a key ethical All notes with identifying information
imperative. collected for MDSR should be destroyed,
once MDSR reports are produced.
Anonymity
Confidentiality of the data obtained during the
It involves removal of personal identifiers from MDSR enquiry is a key legal – ethical imperative
documents. It is important to ensure confidentiality of MDSR. Confidentiality refers to the obligation
during MDSR. Anonymity entails that personal of professionals who have access to patient records
identity remains completely unknown. The names or communication to hold that information
of the deceased should NOT appear in MDSR undisclosed. Privacy, as distinct from
forms & database. Patient & staff identifiers in confidentiality, is viewed as the right of the
patient‘s folders, records and case summaries individual client or patient to be let alone and to
should be masked. Discussions should be make decisions about how personal information is
African Journal of Reproductive Health June 2018; 22 (2):21
Bain and Kongnyuy Legal and ethical aspects of MDSR
shared. Confidentiality therefore falls within the 1. Fully informed about the review process
main responsibilities of the MDSR committee. 2. Informed that their participation is
Studies from Malawi have identified lack of voluntary
privacy as a key hindrance to the implementation 3. Informed that the interview can be
of this approach8. In China, confidentiality and interrupted at their request
anonymity were key challenges identified to ensure 4. Given consent forms should ideally be
the success of the MDSR9. Trusting relationships administered before family members are
between the community and health care teams interviewed.
constitute the corner stone of this approach, for
adequate and appropriate maternal death indicators Consenting parties who participate in the MDSR
should adequately understand what it entails, its
to be obtained10. Upholding the ideals of privacy
relevance, and understand their right to freedom of
and confidentiality must remain key initial starting
choice (accepting or declining participation). The
points for implementation of the MDSR. Proper
informed consent process could face some
training and education of the MDSR teams and the
challenges: insufficient or inappropriate quantity
community with regards to the intentions of this
and quality of information provided with regards to
approach remain imperative to curb abuses and
the MDSR, indirect coercion from health care staff
fear to disclose useful information. Without
(where patients think that what comes from them
guaranteeing respect of these ideals, underreporting
should be for the patient‘s good as a rule) and fear
and wrong information might distort the intended
of being indexed in case they refuse to participate.
goals of the MDSR.
For informed consent to make sense in this case, it
should be a process and not an on the spot or one-
Beneficence
time decision-making activity. A poor informed
The benefits from findings from MDSR are consent process in case of realized breach of
enormous if properly acted upon. It has a big confidence might disrupt trusting relationships
potential of reducing maternal mortality and between partners in the MDSR process. Proper
morbidity. Data should be collected in a way that education of the MDSR committee members with
they can be analysed and used at different levels regards to the quantity and quality of information
for the purpose for which they are collected. Data to be provided to respondents is a priority. When
should have collected in a way that maximises participants realize that they are respected and are
analysis and response at different levels. aware this as an autonomous choice either to
Maximizing the use of data collected is a core accept or refute participation, they feel respected
justification of MDSR. Not using correctly, the and trust is consequently enhanced13. Reported fear
collected data is unethical. of litigation, privacy and anonymity concerns
probably arise from a poor informed consent
Autonomy or self-determination process. Participants should be made to properly
understand the rationale of the information
Individuals are independent and can make rational obtained, and that it is not meant for potential
decisions for themselves. It is the right of punishment and that they are protected (in
competent adults to make informed decisions for countries where laws are already in force with
themselves, about their own medical care and regards to MDSR) by law. Community
participation in any review process or research. involvement from the very planning stages of the
Family and community members should be: process can foster trust, acceptability, ownership
African Journal of Reproductive Health June 2018; 22 (2):22
Bain and Kongnyuy Legal and ethical aspects of MDSR
and sustainability of such endeavors. A pilot study MDSR committee members and should be read at
in Malawi using a community-linked maternal the beginning of every review meeting. Its purpose
death review (CLMDR) approach to measure and is to uphold ethical practices among MDSR
prevent maternal mortality showed increased committee members including confidentiality. It
maternal death identification thanks to community outlines the code of conduct for participants:
involvement, increased quantity of available
Purpose of Maternal Death Review
information for subsequent analysis and improved
Arriving on time
stakeholder involvement11. Aborigo et al in Ghana
have highlighted the importance of carefully Respecting each other‘s ideas and
considering sociocultural sensitivities during verbal opinions
autopsies. Some death types need to be approached Maintaining confidentiality: No name, no
with heightened caution during verbal autopsies12. blame
The MDSR team must carefully consider the Active participation without violence
consent process based on the circumstance and No attempts to falsify records
community in question. In certain communities Accepting criticisms to improve clinical
with strong cultural bonds between the traditional care
chiefs and the people, one might feel compelled to Committment to implement
consent to the MDSR activity once the chief says recommendations from Maternal Death
ok, for fear of social exclusion. Combs Thorsen et Review
al have suggested that in such circumstances, the Legal and ethical framework for MDSR
individuals should always be told in the presence
of the chiefs that participation in the activity is Using evidence from the literature and field
voluntary20. experience on MDSR, the following legal and
ethical framework for MDSR has been proposed
Charter for MDSR? (Table 1). Three categories of both legal and
ethical issues involved in MDSR have been
The MDSR committee should consider having a identified: the issues with data, people, and use of
Charter for MDSR. This Charter is signed by findings from MDSR.
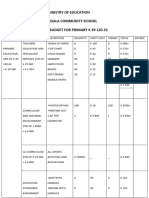
Table 1: Legal and Ethical Framework for MDSR.
Legal Ethical
Data Legal access to data Confidentiality – MDSR Charter can improve
Data protection confidentiality
Anonymity
People Immunity – protection of people involved Privacy – ensuring informed consent can
Oath taking by MDSR committee resolve privacy issues
Autonomy (self-determination)
Benefits Use of findings of MDSR only for the Beneficence
authorized purposes Improved quality of care and reduction of
Reduced risk of litigation maternal mortality
African Journal of Reproductive Health June 2018; 22 (2):23
Bain and Kongnyuy Legal and ethical aspects of MDSR
Conclusion Funding
With most maternal deaths being preventable, None
failure to eliminate these deaths translates to a
failure in guaranteeing the right of the woman to Authors' Contributions
life. This should more than ever before constitute
an ethical – moral priority for global health actors. EJK conceived the initial idea. EJK and LEB did
MDSR is a promising data collection and public the literature searchers and contributed
health intervention tool when it comes to intellectually. Both authors agree on the current
identifying key drivers of maternal mortality and version of the manuscript.
acting upon them in an effective and timely
manner. Legal and ethical barriers if not properly References
ascertained might render this approach 1. WHO | Maternal mortality [Internet]. [cited 2016 Jul 16].
unproductive. Access to data, protection of parties Available from:
involved in the MDSR process, use of MDSR http://www.who.int/mediacentre/factsheets/fs348/e
findings and litigation issues are key legal concerns 2. WHO | Maternal Death Surveillance and Response:
Technical Guidance. Information for Action to
that must be carefully ascertained. Ethical Prevent Maternal Death. WHO. Accessed July 16,
imperatives like ensuring privacy, anonymity, 2016.
respect of autonomy, beneficence, and http://www.who.int/maternal_child_adolescent/docu
confidentiality can enhance trusting relationships ments/maternal_death_surveillance/en/.
3. Hounton S, De Bernis L, Hussein J, Graham WJ, Danel I,
between MDSR teams and the community. Byass P and Mason EM. Towards elimination of
Monitoring and evaluation of the legal and ethical maternal deaths: maternal deaths surveillance and
ideals proposed could go a long way to guarantee response. Reprod Health. 2013 Jan 2;10:1.
the sustainability of the MDSR process and 4. Programme of action of the International Conference on
achievement of its intended goals. Authors have Population and Development. paragraph 7.3. New
York: United Nations; 1994.
proposed a legal and ethical framework for MDSR 5. Gruskin S, Cottingham J, Hilber AM, Kismodi E, Lincetto
and hope that it will provide a structure to guide O and Roseman MJ. Using human rights to improve
practitioners and researchers in improving MDSR maternal and neonatal health: history, connections
practice and research in view to reducing maternal and a proposed practical approach. Bull World
Health Organ. 2008 Aug;86(8):589–93.
mortality. 6. Amzat J. The question of autonomy in maternal health in
Africa: a rights-based consideration. J Bioeth Inq.
Consent for Publications 2015 Jun;12(2):283–93.
7. WHO | Trends in Maternal Mortality: 1990 to 2015.
The authors have read and approve the publication WHO. Accessed July 16, 2016.
http://www.who.int/reproductivehealth/publications/
of the manuscript in its current form. This monitoring/maternal-mortality-2015/en/.
manuscript has not been submitted for publication 8. Kongnyuy EJ and van den Broek N. The difficulties of
elsewhere and has not been previously published. conducting maternal death reviews in Malawi. BMC
Pregnancy Childbirth. 2008;8:42.
9. Gao Y, Kildea S, Barclay L, Hao M and Zeng W. Maternal
Competing Interests mortality surveillance in an inland Chinese province.
Int J Gynaecol Obstet. 2009 Feb;104(2):128–31.
The authors declare they have no conflict of 10. Eyal N. Using informed consent to save trust. J Med
interest Ethics. 2014 Jul;40(7):437–44.
African Journal of Reproductive Health June 2018; 22 (2):24
Bain and Kongnyuy Legal and ethical aspects of MDSR
11. Bayley O, Chapota H, Kainja E, Phiri T, Gondwe C, King Shweni P and National Committee on Confidential
C, Nambiar B, Mwansambo C, Kazembe P, Costello Enquiries into Maternal Deaths in South Africa . The
A, Rosato M and Colbourn T. Community-linked confidential enquiry into maternal deaths in South
maternal death review (CLMDR) to measure and Africa: a case study. BJOG: Int J Obstet Gy. 2014
prevent maternal mortality: a pilot study in rural Sep 1;121:53–60.
Malawi. BMJ Open. 2015 Apr 20;5(4):e007753. 18. Ameh CA, Smith H and van den Broek N. Maternal Death
12. Aborigo RA, Allotey P, Tindana P, Azongo D and Surveillance and Response in Kenya. Geneva:
Debpuur C. Cultural imperatives and the ethics of World Health Organization; 2015.
verbal autopsies in rural Ghana. Glob Health Action. http://www.who.int/maternal_child_adolescent/epid
2013;6:18570. emiology/maternal-death-surveillance/case-
13. Bueno de Mesquita J and Kismödi E. Maternal mortality studies/kenya/en/ Accessed: 10th of November, 2017
and human rights: landmark decision by United 19. Bandali S, Thomas C, Hukin E, Matthews Z, Mathai M,
Nations human rights body. Bull World Health Ramachandran Dilip T, Roos N, Lawley R, Igado O
Organ. 2012 Feb 1;90(2):79A. and Hulton L. Maternal Death Surveillance and
14. Smith H, Ameh C, Godia P, Maua J, Bartilol K, Amoth P Response Systems in driving accountability and
Mathai M and van den Broek N. Implementing influencing change. Int J Gynaecol Obstet. 2016 Dec
Maternal Death Surveillance and Response in 1;135(3):365–71.
Kenya: Incremental Progress and Lessons Learned. 20. Combs Thorsen V, Sundby J, Meguid T and Malata A.
Glob Health Sci Pract. 2017 Sep 27;5(3):345–54. Easier said than done!: methodological challenges
15. Smith H, Ameh C, Roos N, Mathai M and Broek NVD. with conducting maternal death review research in
Implementing maternal death surveillance and Malawi. BMC Med Res Methodol. 2014 Feb
response: a review of lessons from country case 21;14:29.
studies. BMC Pregnancy and Childbirth. 2017 Jul 21. CEDAW-C-KEN-CO-7.pdf [Internet]. [cited 2018 May
17;17:233. 22]. Available from:
16. WHO | Beyond the numbers [Internet]. WHO. Available http://www2.ohchr.org/english/bodies/cedaw/docs/c
from: o/CEDAW-C-KEN-CO-7.pdf
http://www.who.int/maternal_child_adolescent/docu 22. Bueno de Mesquita J and Kismödi E. Maternal mortality
ments/9241591838/en/ and human rights: landmark decision by United
17. Moodley J, Pattinson R, Fawcus S, Schoon M, Moran N, Nations human rights body. Bull World Health
Organ. 2012 Feb 1;90(2):79-79A.
African Journal of Reproductive Health June 2018; 22 (2):25
Вам также может понравиться
- Powerpoint Presentation R.A 7877 - Anti Sexual Harassment ActДокумент14 страницPowerpoint Presentation R.A 7877 - Anti Sexual Harassment ActApple100% (1)
- Conflict WaiverДокумент2 страницыConflict WaiverjlurosОценок пока нет
- Maternal Death ReviewsДокумент4 страницыMaternal Death ReviewsJosephine AikpitanyiОценок пока нет
- Practitioners Guide For Business Development Planning in FPOsДокумент70 страницPractitioners Guide For Business Development Planning in FPOsMythreyi ChichulaОценок пока нет
- Chapter Two Complexity AnalysisДокумент40 страницChapter Two Complexity AnalysisSoressa HassenОценок пока нет
- Mercury 150HPДокумент5 страницMercury 150HP이영석0% (1)
- MEMORANDUMДокумент8 страницMEMORANDUMAdee JocsonОценок пока нет
- Home Guaranty Corp. v. Manlapaz - PunzalanДокумент3 страницыHome Guaranty Corp. v. Manlapaz - PunzalanPrincess Aliyah Punzalan100% (1)
- Data-Driven Healthcare: Revolutionizing Patient Care with Data ScienceОт EverandData-Driven Healthcare: Revolutionizing Patient Care with Data ScienceОценок пока нет
- Delta PresentationДокумент36 страницDelta Presentationarch_ianОценок пока нет
- To Err Is Human 1999 Report Brief PDFДокумент8 страницTo Err Is Human 1999 Report Brief PDFAjib A. Azis100% (3)
- Managerial Accounting-Fundamental Concepts and Costing Systems For Cost Analysis Module 1Документ40 страницManagerial Accounting-Fundamental Concepts and Costing Systems For Cost Analysis Module 1Uzma Khan100% (1)
- Rehabilitation and Retrofitting of Structurs Question PapersДокумент4 страницыRehabilitation and Retrofitting of Structurs Question PapersYaswanthGorantlaОценок пока нет
- Nursing Ethical Dilemma With Using Informatics Technology: March 2019Документ10 страницNursing Ethical Dilemma With Using Informatics Technology: March 2019Ahmed MasoudОценок пока нет
- Respectful Maternity Care: An Overview PowerpointДокумент15 страницRespectful Maternity Care: An Overview PowerpointJhpiego100% (1)
- Perceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesДокумент14 страницPerceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesRhod Bernaldez EstaОценок пока нет
- Research Papers On Access To HealthcareДокумент7 страницResearch Papers On Access To Healthcaregw1w9reg100% (1)
- A Global Database of Abortion Laws, Policies, Health Standards and GuidelinesДокумент6 страницA Global Database of Abortion Laws, Policies, Health Standards and GuidelinesRahmadani NabilaОценок пока нет
- Optimising Caesarean Section Use 3: Interventions To Reduce Unnecessary Caesarean Sections in Healthy Women and BabiesДокумент11 страницOptimising Caesarean Section Use 3: Interventions To Reduce Unnecessary Caesarean Sections in Healthy Women and Babiesforensik24mei koasdaringОценок пока нет
- Ethical Concerns Relating To Taking Birth Control PillsДокумент8 страницEthical Concerns Relating To Taking Birth Control PillsMichael MbithiОценок пока нет
- Abortion ResearchДокумент56 страницAbortion Researchcodmluna3Оценок пока нет
- The Applications of Mobile Health Technology (Mhealth) in Reducing Maternal Mortality and Improving Maternal Health - Sarah KimДокумент16 страницThe Applications of Mobile Health Technology (Mhealth) in Reducing Maternal Mortality and Improving Maternal Health - Sarah KimnurjОценок пока нет
- Workshop MigHealthCare StrengtheningДокумент1 страницаWorkshop MigHealthCare StrengtheningYang GuoОценок пока нет
- Criteria Possible Points Points EarnedДокумент6 страницCriteria Possible Points Points Earnedapi-350882100Оценок пока нет
- Ethical Aspects of Digital Health From A Justice Point of ViewДокумент5 страницEthical Aspects of Digital Health From A Justice Point of ViewAlejo DavidОценок пока нет
- Framework For Ensuring Human Rights in The Provision of Contraceptive Information and ServicesДокумент24 страницыFramework For Ensuring Human Rights in The Provision of Contraceptive Information and ServicesSara Fernandez RiveraОценок пока нет
- Articulo Publicado Frontiers Public HealthДокумент17 страницArticulo Publicado Frontiers Public HealthKathia Cancino RojasОценок пока нет
- 1-Teen Pregnancy As A Public Health Problem.....Документ6 страниц1-Teen Pregnancy As A Public Health Problem.....catholic HymnsОценок пока нет
- 5139 BC 262Документ7 страниц5139 BC 262wowlwowlskeowОценок пока нет
- Disease Control Priority-3Документ23 страницыDisease Control Priority-3Abubakar Abdhoo100% (1)
- Nurses and Health Professionals Facing Female GeniДокумент12 страницNurses and Health Professionals Facing Female GeniBiaОценок пока нет
- Mapeh 10Документ17 страницMapeh 10mary triskayeОценок пока нет
- WYA Reproductive Health White PaperДокумент20 страницWYA Reproductive Health White PaperWorld Youth AllianceОценок пока нет
- Global Abortion Policies DatabaseДокумент5 страницGlobal Abortion Policies DatabaseHumberto Herrera GutierrezОценок пока нет
- Ethics, Privacy, and SecurityДокумент10 страницEthics, Privacy, and SecuritySittie Aina Munder100% (1)
- Ryzza BaldiviesoДокумент31 страницаRyzza BaldiviesoRobert DemagneОценок пока нет
- Moving Beyond Disrespect and Abuse Addressing The Structural Dimensions of Obstetric VioleДокумент10 страницMoving Beyond Disrespect and Abuse Addressing The Structural Dimensions of Obstetric VioleMaryОценок пока нет
- A Review of Women's Intellectual Contribution Under The Bureaucracy in PakistanДокумент36 страницA Review of Women's Intellectual Contribution Under The Bureaucracy in PakistansalmankhataniОценок пока нет
- Research PartialДокумент8 страницResearch PartialAmie VОценок пока нет
- GP ScaffoldДокумент7 страницGP ScaffoldMinh HoangОценок пока нет
- Torts Research Paper 1Документ8 страницTorts Research Paper 1Cristelle Estrada-Romuar JurolanОценок пока нет
- What Is Health Informatics?Документ4 страницыWhat Is Health Informatics?Yna HerraduraОценок пока нет
- Main Content JuryДокумент15 страницMain Content Juryarushi.singhОценок пока нет
- WHO Recommendations On Antenatal Care For A Positive Pregnancy Experience in KenyaДокумент10 страницWHO Recommendations On Antenatal Care For A Positive Pregnancy Experience in KenyaMartin Otundo RichardОценок пока нет
- The Safe Motherhood InitiativeДокумент3 страницыThe Safe Motherhood InitiativeAnonymous g6L7jJWОценок пока нет
- ResearchProposal FinalDraft MirandaDuckworthДокумент13 страницResearchProposal FinalDraft MirandaDuckworthMiranda DuckworthОценок пока нет
- Jurnal 1Документ10 страницJurnal 1dinidinayОценок пока нет
- Association of Rule of Law and Health Outcomes: An Ecological StudyДокумент9 страницAssociation of Rule of Law and Health Outcomes: An Ecological StudybogdanОценок пока нет
- Uu200 EthicsДокумент6 страницUu200 EthicsFiza AliОценок пока нет
- World Health Organization: by Wendy BraunДокумент8 страницWorld Health Organization: by Wendy BraunAnonymous AvbmJ5JTОценок пока нет
- Debating Medicalization of Female Genital Mutilation/Cutting (FGM/C) : Learning From (Policy) Experiences Across CountriesДокумент10 страницDebating Medicalization of Female Genital Mutilation/Cutting (FGM/C) : Learning From (Policy) Experiences Across CountriesPutu AdiОценок пока нет
- Child Sexual Abuse: Current Evidence, Clinical Practice, and Policy DirectionsОт EverandChild Sexual Abuse: Current Evidence, Clinical Practice, and Policy DirectionsОценок пока нет
- Evaluation of The Effect of Birth and Death Registration On Health Service Delivery (A Case of Tolon District of Ghana)Документ10 страницEvaluation of The Effect of Birth and Death Registration On Health Service Delivery (A Case of Tolon District of Ghana)Igbani VictoryОценок пока нет
- Kesehatan Anak (Child Health)Документ15 страницKesehatan Anak (Child Health)AndiniОценок пока нет
- WHO Coșbuc MUN 2023 Study GuideДокумент17 страницWHO Coșbuc MUN 2023 Study Guideluca mscОценок пока нет
- Ryzza - Baldivieso 2Документ34 страницыRyzza - Baldivieso 2Robert DemagneОценок пока нет
- Ensuring The Accessibility of Standard Health Care System and Reproductive Rights For Pregnant Women and Children Amid Covid-19 Pandemic. OverviewДокумент9 страницEnsuring The Accessibility of Standard Health Care System and Reproductive Rights For Pregnant Women and Children Amid Covid-19 Pandemic. Overviewaxium 2014Оценок пока нет
- Lecture 1intro RHДокумент32 страницыLecture 1intro RHAd Nan AbduselamОценок пока нет
- JournalДокумент2 страницыJournalRenalyn MangadchilОценок пока нет
- Jurnal Jaminan KesДокумент25 страницJurnal Jaminan KesMeisya MonicaОценок пока нет
- Maternal Mortality PDFДокумент101 страницаMaternal Mortality PDFCamille Joy BaliliОценок пока нет
- JHJHJJHДокумент14 страницJHJHJJHnur arifahОценок пока нет
- PR1 RRLДокумент4 страницыPR1 RRLalayanjoshua26Оценок пока нет
- Reproductive and Child Health ProgrammeДокумент2 страницыReproductive and Child Health ProgrammeAnnapurna DangetiОценок пока нет
- Public Health Delivery in The Information Age - The Role of Informatics and TechnologyДокумент22 страницыPublic Health Delivery in The Information Age - The Role of Informatics and Technologysbaracaldo2Оценок пока нет
- Disaster Nursing Final ModuleДокумент7 страницDisaster Nursing Final ModuleJerome Reyes is PogiОценок пока нет
- Aismun 2020 - Un Women Committee GuideДокумент29 страницAismun 2020 - Un Women Committee GuideLauraОценок пока нет
- Incident Reporting SystemsДокумент5 страницIncident Reporting SystemsPaulo'RodriguesОценок пока нет
- Pharm Info Lab PrefiДокумент1 страницаPharm Info Lab PreficalopemichelleОценок пока нет
- Literature Review On Neonatal DeathДокумент6 страницLiterature Review On Neonatal Deathafdtovmhb100% (1)
- FNCP GroupДокумент13 страницFNCP GroupTanya PinedaОценок пока нет
- Public Health Laws Affecting The Practice of Nursing PDFДокумент118 страницPublic Health Laws Affecting The Practice of Nursing PDFTanya PinedaОценок пока нет
- NutriiiДокумент1 страницаNutriiiTanya PinedaОценок пока нет
- Table Synthesis ContextДокумент2 страницыTable Synthesis ContextTanya PinedaОценок пока нет
- Literatur Matrix NCM RleДокумент3 страницыLiteratur Matrix NCM RleTanya PinedaОценок пока нет
- Defeating An Old Adversary Cement Kiln BallsДокумент5 страницDefeating An Old Adversary Cement Kiln BallsManish KumarОценок пока нет
- STM Series Solar ControllerДокумент2 страницыSTM Series Solar ControllerFaris KedirОценок пока нет
- Terms and Conditions 27 06 PDFДокумент4 страницыTerms and Conditions 27 06 PDFShreyash NaikwadiОценок пока нет
- Bank of AmericaДокумент1 страницаBank of AmericaBethany MangahasОценок пока нет
- Sign Language To Speech ConversionДокумент6 страницSign Language To Speech ConversionGokul RajaОценок пока нет
- 7Документ101 страница7Navindra JaggernauthОценок пока нет
- Creative Thinking (2) : Dr. Sarah Elsayed ElshazlyДокумент38 страницCreative Thinking (2) : Dr. Sarah Elsayed ElshazlyNehal AbdellatifОценок пока нет
- Salem Telephone CompanyДокумент4 страницыSalem Telephone Company202211021 imtnagОценок пока нет
- Health, Safety & Environment: Refer NumberДокумент2 страницыHealth, Safety & Environment: Refer NumbergilОценок пока нет
- Circuitos Digitales III: #IncludeДокумент2 страницыCircuitos Digitales III: #IncludeCristiamОценок пока нет
- Pthread TutorialДокумент26 страницPthread Tutorialapi-3754827Оценок пока нет
- Income Tax Calculator 2023Документ50 страницIncome Tax Calculator 2023TARUN PRASADОценок пока нет
- Practical GAD (1-32) Roll No.20IF227Документ97 страницPractical GAD (1-32) Roll No.20IF22720IF135 Anant PatilОценок пока нет
- Is.14785.2000 - Coast Down Test PDFДокумент12 страницIs.14785.2000 - Coast Down Test PDFVenkata NarayanaОценок пока нет
- Simavi - Project Officer PROPOPIДокумент4 страницыSimavi - Project Officer PROPOPIAgus NugrahaОценок пока нет
- Kompetensi Sumber Daya Manusia SDM Dalam Meningkatkan Kinerja Tenaga Kependidika PDFДокумент13 страницKompetensi Sumber Daya Manusia SDM Dalam Meningkatkan Kinerja Tenaga Kependidika PDFEka IdrisОценок пока нет
- Question Bank For Vlsi LabДокумент4 страницыQuestion Bank For Vlsi LabSav ThaОценок пока нет
- Tate Modern London, Pay Congestion ChargeДокумент6 страницTate Modern London, Pay Congestion ChargeCongestionChargeОценок пока нет
- Ministry of Education Musala SCHДокумент5 страницMinistry of Education Musala SCHlaonimosesОценок пока нет