Академический Документы
Профессиональный Документы
Культура Документы
Systemic and Inflammatory Response To Injury: Dr. Michael Martin Baccay
Загружено:
Ramil Salmorin0 оценок0% нашли этот документ полезным (0 голосов)
28 просмотров9 страницОригинальное название
ACFrOgDg8X-N0mL8vwYQIwHH3Z74KS7OMk3c8uOTOkQ_vo7gbrbOUKq8GWVIo6y09DZ5AjhNLR73DVr2a2R-lLAFwyi299gHeN78B5GtpGTVZGW_6RLnPSgzwNwWiIUb2Z8EPFfATbsNu48UbTUT
Авторское право
© © All Rights Reserved
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
28 просмотров9 страницSystemic and Inflammatory Response To Injury: Dr. Michael Martin Baccay
Загружено:
Ramil SalmorinАвторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 9
SYSTEMIC AND INFLAMMATORY RESPONSE TO INJURY
Dr. Michael Martin Baccay
September 7, 2020
SEM 1 MIDTERMS – TRANS 3
OUTLINE The body responds to both injury and infection with:
o Brain & hormones (neural and hormonal response)
I. Detection of Cellular Injury o Cellular level (cell-mediated response)
A. Systemic Response Types:
B. DAMPs Innate – acute inflammation; first responders
C. PAMPs Adaptive – figure out what exactly do they need to
II. Neuroendocrine response to injury respondproduction of antibody; they have sense of
A. HPA Axis (until ghrelin, aldosterone, insulin) preparedness
B. Sympathetic nervous system (catecholamines) A. Damage Associated Molecular Patterns (DAMPS)
III. Sepsis, severe sepsis, septic shock
Aka alarmins
IV. Signal Transduction
V. Cell signaling pathways Produced following tissue and cellular injury.
A. JAK-STAT signaling Interact with immune and nonimmune receptors to initiate a
B. Suppressors of Cytokine Signaling sterile systemic inflammatory response following severe
C. G-protein coupled receptor family traumatic injury.
D. Tumor necrosis factor family Released either passively from necrotic/damaged cells or
E. Transforming growth factor actively from physiologically stressed cells.
VI. Endothelial-mediated injury Once they are outside the cell, DAMPs promote the activation
A. Neutrophil-endothelium interaction of innate immune cells, as well as the recruitment and
B. Chemokines activation of antigen-presenting cells, which are engaged in
C. Nitric Oxide host defense.
D. Prostacyclin A. Damps that Mediate Detection of Injury
E. Endothelin
F. Platelet-activating factor 1. High Mobility Group Protein B1 (HMGB1)
G. Natriuretic peptides The best characterized DAMP
H. Leukocyte endothelium interaction Rapidly released into the circulation within 30 minutes
VII. Cell-mediated immune response following trauma
VIII. Cells of the immune system The diverse proinflammatory biologic responses that result
IX. Leukocyte-Endothelium Interaction from HMGB1 signaling include:
o Release of cytokines and chemokines from
Legends macrophages/monocytes and dendritic cells; o Neutrophil
from the book activation and chemotaxis;
take note/ boards/good to know o Alteration in epithelial barrier function, including increased
permeability; and
General info (from 2022 trans, Doc’s ppt, and additional
o Increased procoagulant activity on platelet surfaces
references other than the book)
HMGB1 binding to TLR4 triggers the proinflammatory cytokine
I. DETECTION OF CELLULAR INJURY
release that mediates “sickness behavior”
A. Systemic Response
2. Mitochondrial DNA (mtDNA)
Act as DAMPs by triggering an inflammatory response to
necrosis and cellular stress
The release of mtDNA and formyl peptides from damaged or
dysfunctional mitochondria has been implicated in activation
of the macrophage inflammasome (a cytosolic signalling
complex that responds to cellular stress)
With stress and tissue injury mtDNA and peptides are released
from damaged mitochondria where they can contribute to a
sterile inflammatory response
B. DAMPS as Ligands for Pattern Recognition Receptors
1. Soluble Pattern Recognition Molecules (PRM):
The Pentraxins
PRMs are a molecularly diverse group of molecules that share
Figure 1. Key players of systemic response
a conserved mode of action that is defined by complement
Two most important provoking factors in surgery:
activation, agglutination and neutralization and opsonization
o Infection/ Sepsis
The best describe of the PRMs are the pentraxins.
o Injury/ Trauma
Synthesized at sites of injury and inflammation by
Maintenance – hardest and most important part; body tries to
macrophages and dendritic cells, while neutrophils can store
return everything to normal (homeostasis)
PRMs and release them rapidly following activation.
Apoptosis – cell death; normal occurrence because everything
dies eventually but it has to follow the natural course.
TRANSCRIBERS Batinga, Pajinag, Salmorin EDITOR Salmorin 1
2. C – Reactive Protein (CRP) brain (nucleus tractus solitarius).
The first PRM to be identified
Synthesized in the liver in response to IL-6 A. ACTH
Part of the acute-phase protein response Acts on the zona fasciculata of the adrenal glands
Marker of the proinflammatory response in many clinical Synthesizes and secretes glucocorticoids
setting, including appendicitis, vasculitis, and ulcerative colitis. B. Cortisol
F-actin is an evolutionarily conserved DAMPs recognized by Major glucocorticoid which is essential for survival during
DNGR-1 (receptor for dead cells). The identification of F-actin significant physiologic stress
as a DNGR-1 ligand suggests that cytoskeletal exposure is a Trauma increase cortisol anti-inflammatory actions
universal sign of cell damage that can be targeted by the Elicits action thru a cytosolic receptor (glucocorticoid
innate immune system to initiate immunity. receptor).
C. Pathogen Associated Molecular Patterns Lipid soluble - can diffuse through the plasma membrane to
Along with DAMPs, interact with specific cell receptors that interact with its receptor sequestered in the cytoplasm in a
are located both on the cell surface and intracellularly. complex with heat shock proteins
o Endotoxin Ligand binding activation of GR modulate
A toxin produced by certain bacteria and released upon proinflammatory gene transcription and signaling
destruction of bacterial cell. events“net” anti-inflammatory effect.
o Flagellin Glucocorticoids can negatively affect the access of the
A potent activator of a broad range of cell types involved transcription factor, NF-κB, to the promoter regions of its
in innate and adaptive immunity. target genes via a mechanism that involves histone
o dsRNA deacetylase 2.
o Peptidoglycan Glucocorticoids can inhibit a major mechanism by which TLR
II. NEUROENDOCRINE RESPPONSE TO INJURY ligation induces proinflammatory gene expression.
Traumatic injury results in complex neuroendocrine signaling Glucocorticoid receptor (GR) complex bind to specific
Enhance immune defense and rapidly mobilize substrates nucleotide sequences (glucocorticoid response
necessary to meet essential energy and structural needs elements)promote the transcription of genes (IL-10 and IL-1
Two principle neuroendocrine pathways: receptor Antagonist) anti-inflammatory functions
o Hypothalamic-pituitary-adrenal (HPA) axis - Results in the GR complex activation can indirectly influence TLR activity via
release of glucocorticoid hormones. an interaction with signaling pathways such as the mitogen-
o Sympathetic nervous system - Results in release of the activated protein kinase and transforming growth factor–
catecholamines (epinephrine and norepinephrine) activated kinase-1 (TAK1) pathways
A. Hypothalamic-Pituitary-Adrenal (HPA) Axis GR complex can target both suppressor of cytokine signaling 1
Respond to injury-associated stress (SOCS1) and type 1 IFNs to regulate TLR- induced STAT1
activation
After injury, corticotropin releasing hormone (CRH) is secreted
from the paraventricular nucleus (PVN) of the hypothalamus C. Adrenal Insufficiency
o Mediated by TNF-α, IL-1β, IL-6, and the type I IFNs (IFN-α/β) Due to inadequate amounts of circulating cortisol and
as a result of innate immune response to injury. aldosterone.
Cortisol release Caused by exogenous steroid administration who undergo a
o Mediated by IL-2 and IFN-γ as a result of adaptive immune stressor such as surgery (in patients with atrophic adrenal
response glands).
Direct neural input via afferent vagal fibers that interconnect S/sx: tachycardia, hypotension, weakness, nausea, vomiting,
with neurons projecting to the hypothalamus and fever.
o Trigger CRH release stimulate secretion of ACTH by the Relative adrenal insufficiency
APG o Adrenal gland cannot mount an effective cortisol response
Cytokines that act on the hypothalamus are also capable of to match the degree of injury
stimulating ACTH release from the anterior pituitary so that Critical illness-associated cortisol insufficiency in trauma
marked elevations in ACTH and in cortisol can occur that are patients occurs more frequently.
proportional in magnitude to the injury severity Bimodal presentation: patient is at increased risk both early
following the injury associated inflammatoryresponse and in a
delayed fashion, with sepsis being the initiating event.
Laboratory findings in adrenal insufficiency
o Hypoglycemia from decreased gluconeogenesis
o Hyponatremia from impaired renal tubular sodium
resorption
o Hyperkalemia from diminished kaliuresis
Diagnosis: monitoring of basal and ACTH-stimulated cortisol
levels = lower than normal
Treatment: low-dose steroid supplementation.
B. Macrophage Inhibitory Factor
Modulates cortisol function
Proinflammatory cytokine expressed by anterior pituitary,
macrophages, and T lymphocytes
Figure 2. Neural circuit relaying messages of localized injury to the
SURG – [03] Systemic and Inflammatory Respose to Injury 2
Counteracts the anti-inflammatory activity of glucocorticoids o Seen in critically ill patients
causes exacerbation of inflammation associated with acute o Positive predictor of intensive care unit survival in septic
lung injury. patients
Upregulate the expression of TLR4 in macrophages F. Catecholamines in Post-Injury Inflammation
Early increase in plasma MIF has been detected in severely Injury induced activation of SNS secretion of Ach from
injured patients and was found to correlate with NF-κB preganglionic sympathetic fibers innervating the adrenal
translocation and respiratory burst in polymorphonuclear medulla
lymphocytes (PMNs) derived from severely injured patients. Adrenal medulla = considered a modified postganglionic
MIF after injury may be beneficial in preventing early PMN neuron
activation and subsequent organ failure in severely injured Ach signaling to resident chromaffin cells surge of
patients. epinephrine (EPI) and norepinephrine (NE) release into the
C. Growth Hormone circulation (regulated by central and peripheral mechanisms)
Neurohormone expressed primarily by the pituitary gland that release of EPI
has both metabolic and immunomodulatory effects o Modulated by transcriptional regulation of
Promotes protein synthesis and insulin resistance and phenylethanolamine N-methyltransferase (PNMT)
enhances the mobilization of fat stores o PNMT - catalyzed the last step of catecholamine
Upregulation: by hypothalamic GH-releasing hormone biosynthesis pathway methylating NE to form EPI
Downregulation: by somatostatin o PNMT transcription - key step in regulating EPI production
Exerts its downstream effects through direct interaction with and is activated in response to stress and tissue hypoxia by
GH receptors and through the enhanced hepatic synthesis of hypoxia- inducible factor 1α (HIF1A)
insulin-like growth factor (IGF)-1 Catecholamine release:
Enhances phagocytic activity of immunocytes – inc. lysosomal o Causes increased heart rate, myocardial contractility,
superoxide production conduction velocity, and blood pressure; redirection of
inc. proliferation of T-cell populations blood flow to skeletal muscle; increased cellular
inc. severe injury suppression of the GHIGF-IGFBP dec. metabolism throughout the body; and mobilization of
axis IGF levels glucose from the liver via glycogenolysis, gluconeogenesis,
Administration of exogenous recombinant human GH (rhGH) - lipolysis, and ketogenesis (“fight or flight” response).
associated with increased mortality, prolonged ventilator o Insulin release is decreased mainly through the stimulation
dependence, and increased susceptibility to infection of α-adrenergic pancreatic receptors hyperglycemia
proinflammatory response mitochondrial dysfunction.
GH level = independent predictor of mortality, along with the
o Goal: re-establish and maintain the system’s homeostasis,
APACHE II/SAPS II scores
including the innate immune system
Severely burned children
o It directly influence inflammatory cytokine production
o rhGH administration is beneficial
EPI levels condition the activity and responsiveness of
Improved growth and lean body mass hypermetabolism
cytokine-secreting cells
was significantly attenuated.
Epinephrine infusion (higher doses) - inhibit production
Significant in serum GH, IGF-1, and IGFBP-3.
of TNF-α in vivo and to enhance the production of the
D. Insulin-Like Growth Factor (IGF) - 1 anti-inflammatory cytokine IL-10
Anabolic growth factor improve the metabolic rate, gut Stress levels of glucocorticoids and EPI
mucosal function, and protein loss after traumatic injury. Inhibit production of IL-12 (potent stimulator of Th1
< 5% = circulates free in the plasma responses)
Remainder = bound principally to one of six IGF-binding Decrease Th1 cytokine production and increase Th2
proteins (IGFBPs), the majority to IGFBP-3. cytokine production
Liver – IGF inc. CHON synthesis and glycogenesis o Adrenal gland: catecholamine (part. EPI) – causes innate
Adipose tissue - inc. glucose uptake and lipid utilization proinflammatory cytokine regulation and adaptive Th
Skeletal muscle – inc. glucose uptake and CHON synthesis. responses; may act in concert with cortisol to modulate
E. Ghrelin cytokine activity during injuries
Natural ligand for the GH-secretagogue receptor 1a (GHS-R1a) Human immune cells (e.g., mononuclear cells, macrophages,
GHS-R1a – expressed in immune cells, B and T cells, and granulocytes) express adrenergic receptors that are members
neutrophils of the family of G-protein–coupled receptors that act through
Appetite stimulant secreted by the stomach promotes GH the activation of intracellular second messengers such as cyclic
secretion and in glucose homeostasis, lipid metabolism, and adenosine monophosphate (cAMP) and calcium ion influx
immune function. Second messengers regulate the release of inflammatory
In rodent gut ischemia/reperfusion model, ghrelin cytokine and chemokines and other immune cell functions
administration caused the ff: SNS has direct immune modulatory properties via its
o Inhibited proinflammatory cytokine release innervation of lymphoid tissues containing resting and
o Reduced neutrophil infiltration activated immune cells
o Ameliorated intestinal barrier dysfunction Stimulation of postganglionic nerves NE release NE
o Attenuated organ injury interacts with β2-adrenergic receptors expressed by CD4+ T
o Improved survival and B lymphocytes
Effect of ghrelin is dependent on an intact vagus nerve Human peripheral blood mononuclear cells contain inducible
Effect is mediated via the CNS (“cholinergic anti- inflammatory mRNA for the catecholamine-generating enzymes, tyrosine-
pathway) hydroxylase and dopamine-β- hydroxylase, and data suggest
High ghrelin levels that cells can regulate their own catecholamine synthesis in
response to extracellular cues
SURG – [03] Systemic and Inflammatory Respose to Injury 3
Exposure of peripheral blood mononuclear cells to NE Bacteremia – the presence of viable bacteria in circulating
triggers a distinct genetic profile that indicates a modulation blood.
of Th cell function Systemic Inflammatory Response Syndrome (SIRS) – the
G. Aldosterone systemic inflammatory response to a wide variety of severe
A mineralocorticoid released by the zona glomerulosa of the clinical insults, manifested by two or more of the following
adrenal cortex. conditions:
Binds to the mineralocorticoid receptor of principal cells in the o Temp above101F (38.3C) or below 96.8F (36C)
collecting duct of the kidney o HR >90bpm
It can stimulate expression of genes involved in sodium o RR >20bpm or PaCO2 <32mmHg
reabsorption and potassium excretion to regulate extracellular o WBC count >12,000/mm3, <4,000/mm3, or >10% immature
volume and blood pressure. (band) forms
A. Mononuclear Cells (Monocytes & Lymphocytes) Sepsis – the systemic inflammatory response to infection and
is defined as the presence of SIRS in addition to documented
Has mineralocorticoid receptor (MR) that binds aldosterone
or presumed infection. The clinical manifestations would
with high specificity, regulating sodium and potassium flux, as
include two or more of the following conditions* as a result of
well as plasminogen activator inhibitor-1 and p22 phox
documented infection.
expression
Severe Sepsis/SIRS – Sepsis (SIRS) associated with organ
Aldosterone also inhibits cytokine-mediated NF-κB activation
dysfunction, hypoperfusion, or hypotension. Hypoperfusion
in neutrophils, which also possess a functional MR.
and perfusion abnormalities may include, but are not limited
H. Insulin to, lactic acidosis, oliguria, or an acute alteration in mental
Hyperglycemia and insulin resistance – hallmarks of injury and status. Sepsis is usually considered severe when the patient
critical illness. exhibits at least one of the following signs and symptoms
o Due to the catabolic effects of circulating mediators, (which indicate an organ may be failing):
including catecholamines, cortisol, glucagon, and GH. o Significantly decreased urine output
Proglycemic factors, particularly EPI, induces: o Abrupt change in mental status
o Glycogenolysis o Decrease in platelet count
o Lipolysis o Difficulty breathing
Aerobic glycolysis – increased lactate production independent o Abnormal heart pumping function
of available oxygen in a process o Abdominal pain
Severe stress – associated with insulin resistance, leading to Multiple Organ Dysfunction Syndrome (MODS) – presence of
decreased glucose uptake in the liver and the periphery altered organ function in an acutely ill patient such that
contributing to acute hyperglycemia. homeostasis cannot be maintained without intervention.
It is a hormone secreted by the pancreas IV. SIGNAL TRANSDUCTION
Mediates an overall host anabolic state through: Signal Transduction – the process of transferring a signal
o Hepatic glycogenesis and glycolysis throughout an organism, especially across or through a cell.
o Peripheral glucose uptake Receptors – it waits for a chemical, physical or electrical signal.
o Lipogenesis Chemical signals are ligands, and can be produced by
o Protein synthesis. organisms to control their body or received by the
Insulin Receptor (IR) environment.
o Widely expressed and consists of two isoforms, which can Receptor Proteins – specialized by the type of cell they are
form homo- or heterodimers with insulin binding. attached to. Each type of cell receives different signals from
o Dimerization leads to receptor autophosphorylation and the body and environment, so that the body can produce a
activation of intrinsic tyrosine kinase activity. specific and coordinated response.
o Downstream signaling events are dependent on the Second Messenger – carry the message to the nucleus or
recruitment of the adaptor proteins, insulin receptor other organelles
substrate (IRS-1), and Shc to the IR.
Systemic insulin resistance likely results from proinflammatory
signals, which modulate the phosphorylation of IRS-1 to affect
its function.
III. SEPSIS, SEVERE SEPSIS, & SEPTIC SHOCK
Figure 3. Criteria for SIRS, sepsis, severe sepsis and septic shock.
Infection – a host response to the presence of microorganisms Figure 4. Sigal transduction pathway
or tissue invasion by microorganisms.
SURG – [03] Systemic and Inflammatory Respose to Injury 4
V. CELL SIGNALING PATHWAYS The JAK/STAT pathway is inhibited by the action of
Act on their target cells by binding to specific membrane phosphatase, the export of STATs from the nucleus, and the
receptors interaction of antagonistic proteins
These receptor families have been organized by structural B. Suppressors of Cytokine Signaling
motifs and include: A. Suppressors of Cytokine Signaling Molecules (SOCS)
o Type I cytokine receptors Family of proteins that function as a negative feedback loop
o Type II cytokine receptors for type I and II cytokine receptors by terminating JAK- STAT
o Chemokine receptors signaling
o TNF receptors(TNFRs) Eight family members
o Transforming growth factor receptors(TGFRs) o SOCS1-3: associated with cytokine receptor signaling
There are cytokine receptors that belong to the o SOCS4-8: associated with growth factor receptor signaling.
immunoglobulin receptor superfamilies. PRRs, including both TLR and C-type lectin receptors: activate
Several of these receptors have characteristic signaling SOCS by:
pathways that are associated with them. o Induction of SOCS proteins is achieved through activators
A. JAK-STAT SIGNALING (Receptor Kinase) of JAK-STAT signaling, creating an inhibitory feedback loop
through which cytokines can effectively self-regulate by
extinguishing their own signal.
o SOCS molecules can positively and negatively influence the
activation of macrophages and dendritic cells and are
crucial for T-cell development and differentiation.
o All SOCS proteins are able to regulate receptor signaling
through the recruitment of proteasomal degradation
components to their target proteins, whether the target is
a specific receptor or an associated adaptor molecule.
Once associated with the SOCS complex, target proteins are
readily ubiquinated and targeted to the proteasome for
degradation
SOCS1 and SOCS3: also exert an inhibitory effect on JAK- STAT
signaling via their N-terminal kinase inhibitory region (KIR)
domain.
Figure 5. JAK-STAT signaling pathway o N-terminal kinase inhibitory region (KIR) domain
A major subgroup of cytokines, comprising roughly 60 factors, Acts as a pseudo-substrate for JAK
bind to receptors termed type I/II cytokine receptors Binds with high affinity to the JAK kinase domain to
Cytokines that bind these receptors include: inhibit its activity.
o Type I IFNs SOC3: positive regulator of TLR4 responses in macrophages
o IFN-γ via inhibition of IL-6 receptor–mediated STAT3 activation.
o ILs (e.g., IL-6, IL-10, IL-12, and IL-13 Deficiency of SOCS activity → cell hypersensitive to certain
o Hematopoietic growth factors stimuli, such as inflammatory cytokines and GHs
These cytokines play essential roles in the initiation, C. G Protein Receptor Family
maintenance, and modulation of innate and adaptive Chemokine Receptors that respond to ligands such as
immunity for host defense. adrenaline and serotonin
All type I/II cytokine receptors selectively associate with the On ligand binding to the receptor (R), the G protein (G)
Janus kinases (JAKs). undergoes a conformational change through guanosine
o Represent a family of tyrosine kinases that mediate the triphosphate–guanosine diphosphate conversion and in turn
signal transduction for these receptors. activates the effector (E) component.
JAKs are constitutively bound to the cytokine receptors, and The E component subsequently activates second messengers.
on ligand binding and receptor dimerization, activated JAKs Three subunits of Heterotrimeric G proteins:
phosphorylate the receptor to recruit signal transducer and o Gα, Gβ, and Gγ
activator of transcription (STAT) molecules. G proteins perform functionally as dimers because the signal is
Activated STAT proteins further dimerize and translocate into communicated either by the Gα subunit or the Gβγ complex.
the nucleus where they modulate the transcription of target
genes
Individual cytokines activate more than one STAT
STAT-DNA binding can be observed within minutes of cytokine
binding
STATs: modulate gene transcription via epigenetic
mechanisms
JAKs and STATs: central players in the regulation of key
immune cell function, by providing a signaling platform for
Proinflammatory cytokines (IL-6 via JAK1 and STAT3) and anti-
inflammatory cytokines (IL-10 via STAT3) and integrating
signals required for helper and regulatory T-cell development
and differentiation
Figure 6. G-protein coupled receptor activation pathway
SURG – [03] Systemic and Inflammatory Respose to Injury 5
Includes the receptors for catecholamines, bradykinins, and Type I receptors: distinguished by the presence of a
leukotrienes, in addition to a variety of other ligands important glycine/serine-rich membrane domain found
to the inflammatory response. Type II receptors
Classification according to their pharmacologic properties (4 Each TGF-β ligand binds a characteristic combination of type I
Main Families): and type II receptors, both of which are required for signaling
o Class A Rhodopsin-Like o Whether the type I or the type II receptor binds first is
o Class B Secretin-like, ligand-dependent, and the second type I or type II receptor
o Class C Metabotropic Glutamate/Pheromone → recruited to form a heteromeric signaling complex.
o Class D Frizzled Receptors TGF-β binds to the TGF-β receptor → heterodimerization →
Ligand binding → GPCR activation → extracellular domain activates the receptor, which then directly recruits and
shift: transmitted to cytoplasmic portion of the receptor → activates a receptor-associated Smad (Smad2 or Smad3)
facilitate coupling to its principle effector molecules, the through phosphorylation → additional “common” Smad is
heterotrimeric G proteins. then recruited
A. G o Activated Smad complex translocate into the nucleus and,
There are more than 20 known Gα subunits, they have been with other nuclear cofactors, regulates the transcription of
divided into 4 families based on sequence similarity, which has target genes.
served to define both receptor and effector coupling. Also induce the rapid activation of the Ras-extracellular signal-
Gαs: signal through the activation (Gαs) of adenylate cyclase regulated kinase (ERK) signaling pathway in addition to other
MAPK pathways (JNK, p38MAPK)
to ↑ cAMP levels → activate gene transcription through the
Inhibits immune responses by:
activity of intracellular signal transducers such as protein
o Suppression of IL-2 production by T cells (one of the most
kinase A.
important effects)
Gαi: inhibition (Gαi) of adenylate cyclase to ↓ cAMP levels
o Inhibits T-cell proliferation
Gq pathway: stimulates phospholipase C-β to produce the
o Can regulate the maturation of differentiated dendritic
intracellular messengers inositol trisphosphate and
cells and dendritic cell–mediated T-cell responses.
diacylglycerol.
o Induce “alternative activation” macrophages, designated
o Inositol triphosphate: triggers the release of calcium from
M2 macrophages, which express a wide array of anti-
intracellular stores from the ER
inflammatory molecules, including IL-10 and arginase-1.
o Diacylglycerol: recruits protein kinase C to the plasma
membrane for activation.
Gα12/13: act through Rho- and Ras-mediated signaling.
D. Tumor Necrosis Factor Superfamily
The signaling pathway for TNFR1 (55 kDa) and TNFR2 (75 kDa)
occurs by the recruitment of several adapter proteins to the
intracellular receptor complex.
Optimal signaling activity requires receptor trimerization
TNFR1: initially recruits TNFR- associated death domain
(TRADD) → induces apoptosis through the actions of
proteolytic enzymes known as caspases.
CD95 and TNFR1: possess similar intracellular sequences
known as death domains (DDs).
Figure 7. Ligand-gated ion channels vs G-coupled receptors
o Both recruit the same adapter proteins: Fas- associated
death domains (FADDs) before activating caspase 8.
VI. ENDOTHELIAL MEDIATED INJURY
o TNFR1: induces apoptosis by activating caspase 2 through
the recruitment of receptor-interacting protein (RIP). A. Vascular Endothelium
RIP - has a functional component that can initiate NF-κB Normal: VE has overall anticoagulant properties mediated via
and c-Jun activation, both favoring cell survival and the production and cell surface expression of heparin sulfate,
proinflammatory functions dermatan sulfate, tissue factor pathway inhibitor, protein S,
TNFR2: lacks a DD component but recruits adapter proteins thrombomodulin, plasminogen, and tissue plasminogen
known as TNFR-associated factors 1 and 2 (TRAF1, TRAF2) that activator
interact with RIP to mediate NF-κB and c-Jun activation that Sepsis Injury: VE has overall procoagulant shift via decreased
recruits additional proteins that are antiapoptotic, known as production of anticoagulant factors, which may lead to
inhibitor of apoptosis proteins (IAPs). microthrombosis and organ injury
B. Neutrophil-Endothelium Interaction
E. Transforming Growth Factor-B Family of Receptors
Neutrophil facilitation and immunocyte migration: Brought
B. TGF-1 about by increased vascular permeability, chemoattractants,
Pleiotropic cytokine expressed by immune cells that has and increased endothelial adhesion factors (selectins on cell
potent immunoregulatory activities surfaces.).
Essential for T-cell homeostasis In response to inflammatory stimuli released from sentinel
Receptors for TGF-β ligands: TGF-β superfamily of receptors leukocytes in the tissues, including chemokines, thrombin,
o Type I transmembrane proteins that contain intrinsic leukotrienes, histamine, and TNF → activation of vascular
serine/threonine kinase activity endothelium and alteration of surface protein expression.
o Comprise two subfamilies: Within 10 to 20 minutes: P-selectins are mobilized to the cell
surface where it can mediate neutrophil recruitment.
SURG – [03] Systemic and Inflammatory Respose to Injury 6
After 2 hours: Provision of additional surface expression of E- o CX3C
selectin. D. Nitric Oxide
E-selectin and P-selectin bind P-selectin glycoprotein ligand-1 Maintains normal vascular smooth muscle cell relaxation
(PSGL-1) on the neutrophils to orchestrate the capture and Reduces platelet adhesion and aggregation and interferes
rolling of these leukocytes and allow targeted immunocyte with leukocyte adhesion to the endothelium
extravasation. Easily traverses cell membranes, has a short half-life of a few
Immobilized chemokines on the endothelial surface create a seconds, and is oxidized into nitrate and nitrite
chemotactic gradient to further enhance immune cell Endogenous NO formation is largely derived from the action
recruitment. of NO synthase (NOS).
Table 1. Molecules that mediate Leukocyte-endothelial interaction NOS
Adhesion Action Origin Inducers Target Cells
o Constitutively expressed in endothelial cells (NOS3)
Molecule of o Generates NO by catalyzing the degradation of L-arginine
Expression to L-citrulline and NO, in the presence of oxygen and
Selectins NADPH
L-selectin Fast rolling Leukocytes Native Endothelium, o 2 additional isoforms of NOS: neuronal NOS (NOS1) and
platelets,
inducible NOS (iNOS/ NOS2).
eosinophils
P-selectin Slow rolling Platelets and Thrombin, Neutrophils, Guanylyl cyclase (GC) mediates the vasodilatory effect of NO
endothelium histamine monocytes o When NO is formed by endothelium, it rapidly diffuses into
adjacent cells where it binds to and activates guanylyl
E-selectin Very slow Endothelium Cytokines Neutrophils,
rolling monocytes, cyclase.
lymphocytes o GC catalyzes the dephosphorylation of guanosine
Immunoglobulins triphosphate (GTP) to cyclic guanosine monophosphate
ICAM-1 Firm adhesion/ Endothelium, Cytokines Leukocytes (cGMP), which serves as a second messenger for signaling
transmigration leukocytes, smooth muscle relaxation.
fibroblasts, Due to the upregulation of iNOS expression, NO synthesis is
epithelium
ICAM-2 Firm adhesion Endothelium, Native Leukocytes
increased in response to TNF-α and IL-1β, as well as microbial
platelets products.
VCAM-1 Firm adhesion/ Endothelium Cytokines Monocytes, o Severe systemic injury and associated hemorrhage
transmigration lymphocytes produce an early upregulation of iNOS in the liver, lung,
PECAM-1 Adhesion/ Endothelium, Native Endothelium, spleen, and vascular system in which NO acts as an
transmigration platelets, platelets, immunoregulator which modulates cytokine production
leukocytes leukocytes
and immune cell development.
β2-(CD18) Integrins
CD18/11a Firm adhesion/ Leukocytes Leukocyte Endothelium
o Because of greater iNOS activity and expression, NO is
transmigration activation increased in septic shock, where it is associated with low
CD18/11b Firm adhesion/ Neutrophils, Leukocyte Endothelium peripheral vascular resistance and hypotension as well as
(Mac-1) transmigration monocytes, activation with changes in vascular permeability and inhibition of
natural killer noradrenergic nerve transmission.
cells
o Cytokines modulate NO release by increasing arginine
CD18/11c Adhesion Neutrophils, Leukocyte Endothelium
monocytes, activation availability through the expression of the cationic amino
natural killer acid transporter (CAT) or by increasing
cells tetrahydrobiopterin levels, a key cofactor in NO synthesis.
β1-(CD29) Integrins o Protein and membrane phospholipid alterations by
VLA-4 Firm adhesion/ Lymphocytes Leukocyte Monocytes, nitrosylation and the inhibition of mitochondrial
transmigration monocytes activation endothelium,
epthelium
respiration, also happen when NO is increased
E. Prostacyclin (PGI2)
C. Chemokines Best described effects: Cardiovascular system
First identified through their chemotactic and activating A potent vasodilator that also inhibits platelet aggregation
effects on inflammatory cells Pulmonary system: It reduces pulmonary blood pressure and
Produced at high levels following nearly all forms of injury in bronchial hyper-responsiveness.
all tissues, where they are key attractants for immune cell Kidneys: It modulates renal blood flow and glomerular
extravasation. filtration rate.
Soluble proteins, which when secreted, bind to Acts through its receptor (a G-protein–coupled receptor of the
glycosaminoglycans on the cell surface or in the ECM. In this rhodopsin family) to → stimulation of adenylate cyclase →
way, the chemokines can form a fixed chemical gradient that synthesis of cAMP from adenosine triphosphate (ATP) →
promotes immune cell exit to target areas. cAMP-mediated decrease in intracellular calcium and
Chemokines are distinguished (in general) from cytokines by subsequent smooth muscle relaxation
virtue of their receptors, which are members of the G-protein- During systemic inflammation: endothelial prostacyclin
coupled receptor superfamily. expression is impaired → more pro-coagulant profile of
4 Major Groups: endothelium
o C-X-C: important for neutrophil (PMN) proinflammatory Both intravenous and inhaled exogenous prostacyclin
function analogues have been used to improve oxygenation in patients
o C-C: Generally, attract monocytes, eosinophils, basophils with acute lung injury.
and lymphocytes Infusion of prostacyclin improved cardiac index, splanchnic
o C: Specific for lymphocytes blood flow as measured by intestinal tonometry, and oxygen
SURG – [03] Systemic and Inflammatory Respose to Injury 7
delivery in patients with sepsis and there was no significant o Natriuretic
decrease in mean arterial pressure. o Vasorelaxant
F. Endothelin o Cardiac remodeling properties that are effected by
Potent mediators of vasoconstriction signaling through a common receptor: the guanylyl
Release is upregulated in response to hypotension, injury, cyclase-A (GC-A) receptor
thrombin, TGFβ, IL-1, angiotensin II, vasopressin, Both are increased in the setting of cardiac disorders.
catecholamines, and anoxia. VII. CELL MEDIATED IMMUNE RESPONSE
Primarily released to the abluminal side of endothelial cells, An immune response that does not involve antibodies
and very little is stored in cells. Regulation: at the Involves the activation of phagocytes, antigen-specific
transcriptional level. cytotoxic T-lymphocytes, and release of cytokines in response
3 members to an antigen
o ET-1 Role: Detect and eliminate cells that harbor intracellular
Most potent endogenous vasoconstricton. pathogens
Estimated to be 10 times more potent than angiotensin II. Antigen-specific cells
Synthesized primarily by endothelial cells. o CD8+ cytotoxic T lymphocytes (CTLs)
Infusion of it is associated with increased pulmonary o Cytokine-secreting CD4+ TH (T helper cells)
vascular resistance and pulmonary edema and may I. Steps
contribute to pulmonary abnormalities during sepsis. I. Na ve T lymphocytes recognize MHC-associated peptide
o ET-2 antigens displayed on dendritic cells.
o ET-3 II. The T cells are activated to proliferate and to differentiate into
3 ET receptors: associated with increased NO and prostacyclin effector and memory cells, which migrate to the site of
production, which may serve as a feedback mechanism infection.
o ETA: associated with increased inotropy and chronotropy III. CD4+ effector T cells of the TH1 subset recognize the antigens
o ETB of microbes ingested by phagocytes, and activate the
o ETC phagocytes to kill the microbes. Other subsets of effector cells
At low levels, in conjunction with NO, ETs regulate vascular enhance leukocyte recruitment and stimulate different
tone. immune responses.
At increased concentrations, ETs can disrupt the normal blood CD8+ cytotoxic T lymphocytes (CTLs) kill infected cells harboring
flow and distribution and may compromise oxygen delivery to microbes in the cytoplasm. Some T cells remain in the lymphoid
the tissues. organs and help B cells to produce antibodies and some will
G. Platelet Activating Factor differentiate into memory cells
Phosphatidylcholine: major lipid constituent of the plasma
membrane. Enzymatic processing by: VIII. CELL OF THE IMMUNE SYSTEM
o Cytosolic phospholipase A2 (cPLA2) 2 Specialized Types of Stem Cells
o Calcium-independent phospholipase A2 (iPLA2) o Lymphoid progenitor: gives rise to the T and B
Precursor molecule for eicosanoids lymphocytes.
o Arachidonic acid T lymphocytes (T for thymus, where they mature)
o Platelet-activating factor (PAF) B lymphocytes (B for bone marrow, where they originate)
Acute inflammation: PAF is released by immune cells following Natural killer (NK) cells
the activation of PLA2. o Myeloid progenitor: gives rise to different types of
o Receptor for PAF (PAFR): constitutively expressed by leukocytes, erythrocytes and megakaryocytes.
platelets, leukocytes, and endothelial cells
o Ligand binding to the PAFR → activation and aggregation
of platelets and leukocytes, leukocyte adherence, motility,
chemotaxis, and invasion, as well as ROS generation
o PAFR ligation results in the:
Upregulation of numerous proinflammatory genes
including COX-2, iNOS, and IL-6.
Generation of lipid intermediates such as arachidonic
acid and lysophospholipids through the activation of
PLA2.
H. Natriuretic Peptides
2 kinds
o Atrial natriuretic factor (ANF)
o Brain natriuretic peptide (BNP) Figure 8. Cells of the immune system
Released primarily by atrial tissue but are also synthesized by
A. Platelets
the gut, kidney, brain, adrenal glands, and endothelium.
Functionally active forms Play a role in both local and systemic inflammatory responses,
o C-terminal fragments of a larger prohormone particularly following ischemia reperfusion.
o Both N- and C-terminal fragments are detectable in the Express functional scavenger and TLRs that are important
blood (referred to a N- terminal pro-BNP and pro-ANF, detectors of both pathogens and “damage”- associated
respectively) molecules.
Biologic Properties At the site of tissue injury, complex interactions between
o Diuretic platelets, endothelial cells, and circulating leukocytes facilitate
SURG – [03] Systemic and Inflammatory Respose to Injury 8
cellular activation by the numerous local alarmins and immune arginase-1 and IL-10, in addition to a variety of PRRs
mediators. (e.g., scavenging molecules).
B. Dendritic Cells F. Neutrophils
Activated in response to damage signals, to stimulate both First responders to sites of infection and injury
the innate and the adaptive immune responses. Potent mediators of acute inflammation
Specialized antigen-presenting cells (APCs). Chemotactic mediators from a site of injury induce neutrophil
“Professional APCs”: Principal function of capturing, adherence to the vascular endothelium and promote eventual
processing, and presenting both endogenous and exogenous cell migration into the injured tissue.
antigens, which, along with their co- stimulatory molecules, Once primed and activated by inflammatory stimuli, including
are capable of inducing a primary immune response in resting TNF, IL-1, and microbial pathogens, neutrophils are able to
na ve T lymphocytes. enlist a variety of killing mechanisms to manage invading
Have the capacity to further regulate the immune response, pathogens.
both positively and negatively, through the upregulation and Phagocytosed bacteria are killed using NADPH oxygenase-
release of immunomodulatory molecules such as the dependent generation of ROS or by releasing lytic enzymes
chemokine CCL5 and the CXC chemokine CXCL5. and antibacterial proteins into the phagosome.
Have been implicated both in the induction and maintenance When highly activated, neutrophils can also extrude a
of immune tolerance as well as in the acquisition of immune meshwork of chromatin fibers, composed of DNA and
memory. histones that are decorated with granule contents.
C. Eosinophils Neutrophil extracellular traps (NETs): Effective mechanism
Immunocytes whose primary functions are antihelminthic whereby neutrophils can immobilize bacteria to facilitate their
Found mostly in tissues such as the lung and gastrointestinal killing; may also serve to prime T cells, making their threshold
tract, which may suggest a role in immune surveillance for activation lower.
Can be activated by IL-3, IL-5, GM-CSF, chemoattractants, and Neutrophils facilitate the recruitment of monocytes into
platelet-activating factor inflamed tissues. These recruited cells are capable of
Activation can lead to subsequent release of toxic mediators, phagocytosing apoptotic neutrophils to contribute to
including ROSs, histamine, and peroxidase resolution of the inflammatory response.
D. Mast Cells IX. LEUKOCYTE-ENDOTHELIUM INTERACTION
Important in the primary response to injury because they are Process: Leukocytes first roll → become activated and adhere
located in tissues. to the endothelium → transmigrate across the endothelium
TNF release from mast cells has been found to be crucial for and pierce the basement membrane → migrate toward chemo
neutrophil recruitment and pathogen clearance. attractants emanating from the source of injury
With a role in the anaphylactic response to allergens. Molecules used in the process
On activation from stimuli including allergen binding, infection, o Selectins: Rolling
and trauma, mast cells produce histamine, cytokines, o Chemokines: Activation of neutrophils to increase avidity
eicosanoids, proteases, and chemokines, which leads to: of integrins
o Vasodilation o Integrins: Firm adhesion
o Capillary Leakage o CD31 (PECAM-1): Transmigration/Diapedesis
o Immunocyte Recruitment
Important co-signaling effector cells of the immune system via
the release of IL-3, IL-4, IL-5, IL-6, IL-10, IL-13, and IL-14, as well
as macrophage migration– inhibiting factor
E. Monocytes/ Macrophages
Mononuclear phagocytes that circulate in the bloodstream
and can differentiate into macrophages, osteoclasts, and DCs
on migrating into tissues.
Macrophages: main effector cells of the immune response to
infection and injury, primarily through mechanisms that
include phagocytosis of microbial pathogens, release of
inflammatory mediators, and clearance of apoptotic cells.
Figure 8. Leukocyte Edothelium Interaction
Fulfill homeostatic roles beyond host defense
o Remodeling of tissues, both during development and in X. REFERENCES
the adult animal
In response to various signals, macrophages may undergo: Naregta 2022 Trans
o Classical M1 activation (stimulated by TLR ligands and IFN-γ). Brunicardi, F.C. (2019). Schwartz’ Principles of Surgery (11th ed).
M1 phenotype: Characterized by the expression of high USA: McGraw-Hill.
levels of proinflammatory cytokines, like TNF-α, IL-1,
and IL-6, in addition to the synthesis of ROS and RNS;
promote a strong Th1 response
o Alternative M2 activation (stimulated by type II cytokines IL-
4/IL-13).
M2 phenotype: Considered to be involved in the
promotion of wound repair and the restoration of
immune homeostasis through their expression of
SURG – [03] Systemic and Inflammatory Respose to Injury 9
Вам также может понравиться
- Surgery Systemic Response to InjuryДокумент11 страницSurgery Systemic Response to InjuryMATTHEW EARL MALUMAYОценок пока нет
- Biologic Therapies: What and When?: ReviewДокумент10 страницBiologic Therapies: What and When?: ReviewRameshKrishnanОценок пока нет
- Humoral Immune System ExplainedДокумент11 страницHumoral Immune System ExplainedMariel AsisОценок пока нет
- Inflammation TASK 1. Briefly Discuss The Three Divisions of Immunity and Its Relationship To One AnotherДокумент5 страницInflammation TASK 1. Briefly Discuss The Three Divisions of Immunity and Its Relationship To One Anotherkristine keen buanОценок пока нет
- Understanding the Physiology of the Immune SystemДокумент66 страницUnderstanding the Physiology of the Immune SystemSriwiji SetianiОценок пока нет
- SURGERY A: SYSTEMIC INFLAMMATORY RESPONSEДокумент4 страницыSURGERY A: SYSTEMIC INFLAMMATORY RESPONSEAisha Al JenaibiОценок пока нет
- L2 IS Nature of Antigens and The MajorДокумент4 страницыL2 IS Nature of Antigens and The MajorErickson MoragaОценок пока нет
- Cellular ComponentДокумент10 страницCellular ComponentHeran TeferiОценок пока нет
- Reviews: Polymeric Particle-Based Therapies For Acute Inflammatory DiseasesДокумент18 страницReviews: Polymeric Particle-Based Therapies For Acute Inflammatory DiseasesJ. Antonio Ram. M.Оценок пока нет
- Patofisiologi GBSДокумент9 страницPatofisiologi GBSIrma SavitriОценок пока нет
- NCM 112: Medical Surgery CareДокумент8 страницNCM 112: Medical Surgery CareDANAH MARGARET VILLAGONZALOОценок пока нет
- Pertaining To Extracellular Fluid Such As Plasma and Lymph. The Term Humoral Immunity Is Used To Denote Antibody Mediated Immune ResponsesДокумент4 страницыPertaining To Extracellular Fluid Such As Plasma and Lymph. The Term Humoral Immunity Is Used To Denote Antibody Mediated Immune ResponsesZhon CabitacОценок пока нет
- The Immunology of Infection 2017Документ10 страницThe Immunology of Infection 2017Natalia HernandezОценок пока нет
- Immunology & Serology Section Chapter 1: Immunology: Initial Immune ResponseДокумент43 страницыImmunology & Serology Section Chapter 1: Immunology: Initial Immune ResponseCharmaine Dela CruzОценок пока нет
- Chapter 4 Innate ImmunityДокумент74 страницыChapter 4 Innate Immunity13701319477Оценок пока нет
- Inflammasomes in The CNSДокумент14 страницInflammasomes in The CNSMathieu VigneauОценок пока нет
- Management of Head and Neck Infections in The PDFДокумент8 страницManagement of Head and Neck Infections in The PDFVijay TiwariОценок пока нет
- MHC Antigen Processing and PresentationДокумент4 страницыMHC Antigen Processing and PresentationTreyton Sekani LopezОценок пока нет
- Immunity System Health and Defense CH 57 & 58Документ19 страницImmunity System Health and Defense CH 57 & 58NaОценок пока нет
- The Essentials of ImmunologyДокумент29 страницThe Essentials of ImmunologyBrunoОценок пока нет
- DAMPs, PAMPs and Alarmins. All We Need To Know About DangerДокумент5 страницDAMPs, PAMPs and Alarmins. All We Need To Know About DangerjesusОценок пока нет
- The Lymphatic System and Non-Immune ResponseДокумент11 страницThe Lymphatic System and Non-Immune ResponseSheena PasionОценок пока нет
- Immunity of Parasitic InfectionsДокумент4 страницыImmunity of Parasitic InfectionsCoy NuñezОценок пока нет
- Signaling Comunication of Recognizing AntigenДокумент17 страницSignaling Comunication of Recognizing AntigenyulisaninasaraОценок пока нет
- In Ammation, Immunity and Allergy: Learning ObjectivesДокумент6 страницIn Ammation, Immunity and Allergy: Learning ObjectivesJavier VeraОценок пока нет
- Acute Disseminated Encephalomyelitis ADEM AtfДокумент4 страницыAcute Disseminated Encephalomyelitis ADEM AtfAfrah AbdulОценок пока нет
- Immuno and InfectiousДокумент17 страницImmuno and Infectiousgreen_archerОценок пока нет
- Chapter 21 - The Immune System: Innate and Adaptive Body DefensesДокумент2 страницыChapter 21 - The Immune System: Innate and Adaptive Body DefensesChryza Faith QuicoyОценок пока нет
- Points of Control in Inflammation: InsightДокумент7 страницPoints of Control in Inflammation: InsightAsish GeiorgeОценок пока нет
- OVERVIEW OF THE IMMUNE SYSTEM IN SECTION 1Документ18 страницOVERVIEW OF THE IMMUNE SYSTEM IN SECTION 1musatiiОценок пока нет
- Nursing Care of a Child with Immune DisordersДокумент4 страницыNursing Care of a Child with Immune DisordersChin T. OndongОценок пока нет
- Sistem Imun Non Spesifik-2Документ28 страницSistem Imun Non Spesifik-2Asrun PutraОценок пока нет
- 9. Immune GM eng 2022Документ23 страницы9. Immune GM eng 2022kabulkabulovich5Оценок пока нет
- Homeostasis 2Документ15 страницHomeostasis 2Luis MangelОценок пока нет
- Antigens, MHC, and CytokinesДокумент44 страницыAntigens, MHC, and CytokinesVia Gail CanlasОценок пока нет
- InflamaciónДокумент12 страницInflamaciónDaniОценок пока нет
- Innate Immunity: - Properties of Innate Immunity - Components of Innate ImmunityДокумент39 страницInnate Immunity: - Properties of Innate Immunity - Components of Innate Immunityrima melliaОценок пока нет
- 2 Antiviral ImmunityДокумент23 страницы2 Antiviral ImmunityVlad SmithОценок пока нет
- Dendritic Cells: A Link Between Innate and Adaptive ImmunityДокумент14 страницDendritic Cells: A Link Between Innate and Adaptive ImmunityPilar SNОценок пока нет
- Definitions and Outline Structure of The Immune SystemДокумент5 страницDefinitions and Outline Structure of The Immune SystemanonymousОценок пока нет
- The Immune System:: Innate and Acquired ImmunityДокумент47 страницThe Immune System:: Innate and Acquired ImmunityBad BunnyОценок пока нет
- 2 MICRO1 - Host vs. Microbes 2015BДокумент5 страниц2 MICRO1 - Host vs. Microbes 2015BCAMO SAMANTHA LOUISEОценок пока нет
- 4 Immunopathology (Page 131-168) .Kelik-2022Документ38 страниц4 Immunopathology (Page 131-168) .Kelik-2022Pola PhotographyОценок пока нет
- Wang 2022Документ15 страницWang 2022Statistics LearningОценок пока нет
- The Immune System: Innate and Adaptive Defenses Against InfectionДокумент54 страницыThe Immune System: Innate and Adaptive Defenses Against InfectionKristian Dwi Cahya100% (1)
- Immunology Chapter 1Документ4 страницыImmunology Chapter 1Milad MovahediОценок пока нет
- Basic Concepts of Immune Response and Defense DevelopmentДокумент11 страницBasic Concepts of Immune Response and Defense DevelopmentRosydina Robi'aqolbiОценок пока нет
- Immunometabolism IДокумент29 страницImmunometabolism IMatheus TavaresОценок пока нет
- Major Histocompatibility Complex and Antigen PresentationДокумент5 страницMajor Histocompatibility Complex and Antigen PresentationTreyton Sekani LopezОценок пока нет
- Immunology NotesДокумент27 страницImmunology Notescomputerlois88% (8)
- 2022 PSL301Hblood2-1Документ30 страниц2022 PSL301Hblood2-1Jo JacquesОценок пока нет
- 10 Pharmacology - ImmunopharmacologyДокумент17 страниц10 Pharmacology - ImmunopharmacologyArnoldBorromeoОценок пока нет
- IMMUNOLOGYДокумент21 страницаIMMUNOLOGYNicole AguilarОценок пока нет
- The Immune System: Back To The BasicsДокумент37 страницThe Immune System: Back To The BasicsHani GowaiОценок пока нет
- Prelim - Adaptive Immune ResponseДокумент12 страницPrelim - Adaptive Immune ResponseJustin BellosaОценок пока нет
- Humoral Innate Immunity and Acute-PhaseДокумент14 страницHumoral Innate Immunity and Acute-PhaseEdgar JoseОценок пока нет
- Immunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityОт EverandImmunology Unveiled: A Comprehensive Journey through the Human Immune System: Guardians of the Body: The Unseen Heroes of ImmunityОценок пока нет
- Essentials of Mucosal ImmunologyОт EverandEssentials of Mucosal ImmunologyMartin F. KagnoffОценок пока нет
- Cell of Immunoglobulin SynthesisОт EverandCell of Immunoglobulin SynthesisBenvenuto PernisОценок пока нет
- Certificate of CompletionДокумент1 страницаCertificate of CompletionRamil SalmorinОценок пока нет
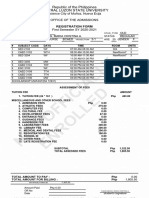
- Science City of Muñoz, Nueva Ecija Office of The Admissions First Semester SY 2020-2021Документ1 страницаScience City of Muñoz, Nueva Ecija Office of The Admissions First Semester SY 2020-2021Ramil SalmorinОценок пока нет
- Inflammation and Repair: Dr. Sheryl Q. RacelisДокумент23 страницыInflammation and Repair: Dr. Sheryl Q. RacelisRamil SalmorinОценок пока нет
- Inflammation and Repair: Dr. Sheryl Q. RacelisДокумент23 страницыInflammation and Repair: Dr. Sheryl Q. RacelisRamil SalmorinОценок пока нет
- 30 Minute Choir Book, Vol5 Preview PDFДокумент260 страниц30 Minute Choir Book, Vol5 Preview PDFRamil SalmorinОценок пока нет
- Prime BadgesДокумент1 страницаPrime BadgesRamil SalmorinОценок пока нет
- Refresher Environmental Compliance CertificateДокумент1 страницаRefresher Environmental Compliance CertificateRamil SalmorinОценок пока нет
- Prime BadgesДокумент1 страницаPrime BadgesRamil SalmorinОценок пока нет
- Pulse Steroid TherapyДокумент10 страницPulse Steroid Therapyselvie87Оценок пока нет
- CortisolДокумент27 страницCortisolCao YunОценок пока нет
- Decalcifiying Pineal GlandДокумент8 страницDecalcifiying Pineal Glandsonden_291% (11)
- Topical Corticosteroids in Plaque PsoriasisДокумент5 страницTopical Corticosteroids in Plaque PsoriasisAnggie Pradetya MaharaniОценок пока нет
- Signal Molecule TrackerДокумент4 страницыSignal Molecule Trackerarman_azad_2Оценок пока нет
- Side Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWДокумент1 122 страницыSide Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWAndrei E. HawayОценок пока нет
- Treatment of Adrenal Insufficiency in Adults - UpToDateДокумент19 страницTreatment of Adrenal Insufficiency in Adults - UpToDatewawa chenОценок пока нет
- FAR 381 Adrenocorticosteroids: Shamiso MlamboДокумент22 страницыFAR 381 Adrenocorticosteroids: Shamiso MlamboHuzaifa KhanОценок пока нет
- HydrocortisoneДокумент2 страницыHydrocortisoneMaggieОценок пока нет
- DexamethasoneДокумент4 страницыDexamethasoneMits Valencia Karlsson0% (2)
- Pharmacology ChemotherapyДокумент28 страницPharmacology ChemotherapyDartiguesОценок пока нет
- Farmakologi Obat Pada Reaksi HipersensitivitasДокумент59 страницFarmakologi Obat Pada Reaksi HipersensitivitasTitip Elia GustamiОценок пока нет
- Assignment For Endocrine SystemДокумент5 страницAssignment For Endocrine SystemMoheeddin KababОценок пока нет
- CT findings and complications of subdural and epidural haematomasДокумент3 страницыCT findings and complications of subdural and epidural haematomasKay BristolОценок пока нет
- Hydrocortisone Generic/Brand Name, Classification, Dosing, and Nursing ResponsibilitiesДокумент5 страницHydrocortisone Generic/Brand Name, Classification, Dosing, and Nursing ResponsibilitiesryanОценок пока нет
- Chapter 6 - Endocrine System 2Документ12 страницChapter 6 - Endocrine System 2AyeshaОценок пока нет
- Sex-Based Differences in Physiology: What Should We Teach in The Medical Curriculum?Документ3 страницыSex-Based Differences in Physiology: What Should We Teach in The Medical Curriculum?Khaled Abdel-saterОценок пока нет
- Drug Study BAIAEДокумент5 страницDrug Study BAIAEDAOman09Оценок пока нет
- Biochemical Pharmacology: Naina Monga, Gurupreet S. Sethi, Kanthi Kiran Kondepudi, Amarjit S. NauraДокумент12 страницBiochemical Pharmacology: Naina Monga, Gurupreet S. Sethi, Kanthi Kiran Kondepudi, Amarjit S. NauraRONALD. D VIERA .MОценок пока нет
- EndocrineДокумент94 страницыEndocrineSuzana VoiculescuОценок пока нет
- Chapter 5 Endocrinology 1Документ53 страницыChapter 5 Endocrinology 1Abubakar JallohОценок пока нет
- Semper Fit Advance Fitness CourseДокумент255 страницSemper Fit Advance Fitness CourseUnited States Militia73% (11)
- Clinical Relevance of Steroid Use in Neuro-Oncology. 2017Документ10 страницClinical Relevance of Steroid Use in Neuro-Oncology. 2017Nicolas RodriguezОценок пока нет
- Therapeutic Strategies in CopdДокумент378 страницTherapeutic Strategies in Copdgermany23Оценок пока нет
- Glucocorticoid DeflazacortДокумент25 страницGlucocorticoid DeflazacortChintan ChavdaОценок пока нет
- Deflazacort Training Manual OverviewДокумент10 страницDeflazacort Training Manual Overviewanupdr_cОценок пока нет
- Cushing Syndrome Addisons 1Документ6 страницCushing Syndrome Addisons 1Czarena Ysabelle PayotОценок пока нет
- Standardised nomenclature for glucocorticoid dosages and treatment regimensДокумент6 страницStandardised nomenclature for glucocorticoid dosages and treatment regimensTurboОценок пока нет
- Endocrine Pharmacology OverviewДокумент52 страницыEndocrine Pharmacology OverviewNicole Opao100% (4)
- Prescribing Information for Kenalog-10 InjectionДокумент8 страницPrescribing Information for Kenalog-10 InjectionArlette DerizkaОценок пока нет