Академический Документы
Профессиональный Документы
Культура Документы
Multi Source Tomography
Загружено:
Fanof EcdОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Multi Source Tomography
Загружено:
Fanof EcdАвторское право:
Доступные форматы
Increased microcalcification visibility in lumpectomy specimens
using a stationary digital breast tomosynthesis system
Andrew W Tucker*, Yueh Z Lee, Cherie M Kuzmiak, Jabari Calliste, Jianping Lu, and Otto
Zhou
University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
ABSTRACT
Current digital breast tomosynthesis (DBT) systems have been shown to have diminished microcalcification (MC)
visibility compared to 2D mammography systems. Rotating gantry DBT systems require mechanical motion of the
X-ray source which causes motion blurring of the focal spot, thus reducing spatial resolution. We have developed a
stationary DBT (s-DBT) technology that uses a carbon nanotube (CNT) based X-ray source array in order to acquire
all the projections images without any mechanical motion. It is capable of producing full tomosynthesis datasets
with zero motion blur. It has been shown to have significantly higher spatial resolution than continuous motion
DBT systems. An s-DBT system also allows for a wider angular span without increasing the acquisition time. A
larger angular span covers a larger portion of the Fourier domain, thus decreasing the tissue overlap. In this study,
we compare tomosynthesis imaging of MCs, in lumpectomy specimens, between an s-DBT system and a rotating
gantry DBT system. Results show that s-DBT produces better MC sharpness and reduced tissue overlap compared
to continuous motion DBT systems.
Key Words: Mammography, Digital breast tomosynthesis, CNT X-ray, Specimen imaging, High resolution
1. INTRODUCTION
Microcalcifications (MCs) are helpful in breast cancer diagnosis for malignancy determination. Characteristics such
as size, distribution, morphology, and variability of the MCs help in the assessment 1, 2. Some MCs can be less than
100 µm in diameter, so high spatial resolution is needed in mammography for their visualization. Full-field digital
mammography (FFDM) systems, the current gold standard for screening mammography, have no z-axis information
which results in tissue overlap in the images. This leads to high false positive and false negative rates3, 4. Digital
breast tomosynthesis (DBT) is capable of reducing tissue overlap by using a small number of angular projection
images.
Current DBT systems have been shown to have better sensitivity and specificity for breast masses compared to
FFDM5, 6. However, current DBT systems acquire projection images by moving a single X-ray source over the
angular span. This motion blurs the focal spot thus reducing the spatial resolution of the system which leads to
reduced MC visibility compared to FFDM6. The Selenia Dimensions DBT system (Hologic Inc., Bedford, MA)
acquires DBT datasets in a continuous motion mode. Since FDA approval of the Selenia Dimensions in early 2011
for combination (combo) mode (DBT plus FFDM) screening examinations, a large number of single site studies
have been reported on the Selenia Dimensions showing the improved sensitivity and specificity of the system over a
2D imaging modality5-7. The sensitivity and specificity improvement was shown for cases with breast masses.
However, for cases with MCs, the use of the combo mode has shown no improvement in the area under the curve
when compared with FFDM imaging alone6. The added FFDM image in combo mode allows for visualization of
MCs but still lacks z-axis resolution and doubles the dose to the patient.
*awtucker@ncsu.edu; phone 1-704-614-2640; http://research.physics.unc.edu/project/zhou/
Medical Imaging 2014: Physics of Medical Imaging, edited by Bruce R. Whiting, Christoph Hoeschen, Despina Kontos,
Proc. of SPIE Vol. 9033, 903316 · © 2014 SPIE · CCC code: 1605-7422/14/$18 · doi: 10.1117/12.2043522
Proc. of SPIE Vol. 9033 903316-1
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
A stationary digital breast tomosynthesis (s-DBT) system uses a carbon nanotube (CNT) based X-ray source array
in order to acquire a full DBT acquisition with zero source motion blur8, 9. The spatial resolution of s-DBT has been
shown to be significantly higher than continuous motion DBT systems10. Higher spatial resolution should allow for
better visualization of MCs. In s-DBT, a larger angular span can be acquired without an increase in acquisition
time. Larger angular spans cover a larger portion of the Fourier domain, thus decreasing the tissue overlap present
in the reconstruction images. In this study, we demonstrate improved visibility of MCs, in human tissue, using an s-
DBT system compared to the Selenia Dimensions DBT system.
2. METHODS
2.1 s-DBT system
The CNT X-ray source array (XinRay Systems LLC, Research Triangle Park, NC) is mounted on a Hologic Selenia
Dimensions DBT system (Hologic Inc., Bedford, MA). The system consists of 31 individual focal spots distributed
in a linear array over a 30 degree span that can be operated at up to 45 kVp10. The system uses a tungsten anode
with a 1.0 mm thick aluminum filter and a 700 mm source-to-imager distance (SID). Breast surgical specimen
images were collected using 15 projection images over a 28 degree span and a detector pixel size of 0.07 mm. A 26
kVp tube potential was used with 100 mAs tube exposure for each specimen. Figure 1 (Left) shows the s-DBT
system after integration with the CNT X-ray source.
The measured system modulation transfer function (MTF) of the s-DBT system is 5.15 cycles/mm at 10% (using the
full resolution of the detector), which is significantly higher than the value measured on a continuous motion DBT
system (2.8 cycles/mm)9, 10.
Figure 1: Left - Image of the s-DBT system with integrated CNT based X-ray source array. The arrow points to the source
array. Right - Image of the Selenia Dimensions DBT system in our lab.
Proc. of SPIE Vol. 9033 903316-2
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
2.2 Continuous motion DBT system
A Hologic Selenia Dimensions DBT system (Hologic Inc., Bedford, MA) was used as the continuous motion DBT
system11. Figure 1 (Right) shows an image of the Selenia Dimensions in our lab. The system uses a tungsten anode
with a 0.7 mm thick aluminum filter and a 700 mm SID. The s-DBT system was modeled after the Selenia
Dimensions but uses a 1 mm thick aluminum filter instead. Lumpectomy images on the Selenia Dimensions were
collected using 15 projection images over an angular span of 15 degrees and a detector pixel size of 0.14 mm. The
same tube potential and exposure were used for the Selenia Dimensions as the s-DBT system (26 kVp, 100 mAs).
2.3 Specimen retrieval and imaging
Under an institutional review board approved protocol, 23 patients with known breast lesions (BIRADS 4 or 5) and
who were scheduled for a pre-operative needle localization for open surgical biopsy were recruited. Once the
procedure was completed the specimen was picked up from the operating room and transported it to the Department
of Radiology for imaging. Hospital protocol requires a magnified 2D FFDM image for each specimen in order to
assess removal of the localized lesion and surgical margins. After imaging was completed, the specimen was
transported to our imaging facility where it was imaged on an s-DBT system and a Selenia Dimensions system. The
specimen was then returned to the Department of Pathology for histologic evaluation. A one hour time frame was
adhered to from excision time in the operating room to specimen return in Pathology.
All surgical specimens were imaged in a quasi-radiolucent specimen container. Figure 2 (Left) shows an image of
the specimen container on the s-DBT system. Once the breast specimen was place in a container by the surgeon it
was gently compressed with a perforated labeled grid. A 2D FFDM of the grid can be seen in Figure 2 (Right).
6
The grid is used for localization of lesions in the specimen for the Department of Pathology.
el Ía II o la "Y. IJ 000
000
+9.,60
040,11,,,,
001:014041taea
Ei 0 it::.^$1g!
ü? 40
06V(-:)01)410001111101111111
I,-*6
40:F;i40/00
60.00000111
:?s3$***V6
4010ie
í
Figure 2: (Left) - Image of a specimen container on the s-DBT system. The arrow points to the container. (Right) - A 2D
FFDM of one of the specimen containers showing the perforated grid.
2.4 Reconstructions
Image reconstruction for both systems was completed with a dynamic 3D image reconstruction software package
developed by Real Time Tomography, LLC (Villanova, PA). This software uses a back projection filtering method
to reconstruct the pseudo-3D volume from the projection images12. Images were reconstructed with a pixel size
Proc. of SPIE Vol. 9033 903316-3
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
equivalent to a 1.8x magnification (a 1.8x radiographic magnification is used in specimen radiography). Figure 3
shows an s-DBT reconstruction slice of a lumpectomy specimen.
Figure 3: An s-DBT reconstruction slice of a lumpectomy specimen. Guide wires and surgical clips were present in most
specimen images.
2.5 MC selection
All breast surgical specimen image datasets were analyzed for isolated MCs that were visible in both imaging
modalities and that were not in the vicinity of other objects (other MCs or guide wires). Twelve isolated MCs were
selected in five different specimens for further analysis. Visually, the in-focus plane was determined. The
sharpness of each MC was analyzed in both the x-y plane and the z-axis. An MC area estimate was used for x-y
plane, and the artifact spread function (ASF) was used for the z-axis.
2.6 X-Y plane sharpness
A small region of interest (ROI) was selected around each MC that was analyzed. A threshold value of 50%
between the maximum and minimum pixel intensity value, for the ROI, was set. Pixels above this threshold value
were segmented and determined to be contained in the MC. Area estimates were made by multiplying the
reconstruction pixel size by the number of pixels contained in the MC. The area estimate of the MC was used as the
figure of merit for x-y plane sharpness.
2.7 Z-axis sharpness
Using the same ROI and segmented area as above (Section 2.6), the ASF was calculated for each MC. The ASF is a
figure of merit which evaluates the out of plane blurring effect in tomosynthesis reconstructions 4. The equation for
ASF in reconstruction plane "z" can be found below:
(1)
Proc. of SPIE Vol. 9033 903316-4
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
where "SA" is the average pixel intensity in the segmented region, "SB" is the average pixel intensity in the
background region, and "zo" is the plane of reconstruction where the MC is in focus. The full width at half
maximum (FWHM) of the ASF was used as the figure of merit for z-axis sharpness.
3. RESULTS
3.1 Image Comparison
Figure 4 shows reconstruction slices of a breast specimen using the s-DBT system and the continuous motion DBT
system. Zoomed in regions of interest (Figure 4-Below) clearly show the increased image sharpness in the s-DBT
system. In the s-DBT image, MCs are not "blurred" together as in the continuous motion DBT image. The
increased angular coverage in the s-DBT system removes artifacts from out-of-plane MCs making delineation more
accurate.
Figure 4: Reconstruction slice of a specimen with a large cluster of MCs using the s-DBT system (Top-Left) and the continuous
motion DBT system (Top-Right). MC sharpness is superior in the zoomed in s-DBT reconstruction (Bottom-Left) compared to
the continuous motion DBT system (Bottom-Right).
Proc. of SPIE Vol. 9033 903316-5
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
3.2 X-Y plane sharpness
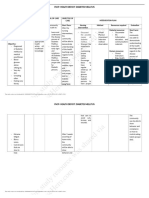
Results for each MC size can be found in Table 1. A smaller area was found for every MC using the s-DBT
system. The average decrease in area for s-DBT was 28.92 ±12.60%. This can be attributed to the higher spatial
resolution of s-DBT compared to continuous motion DBT systems. Figure 5 shows visual comparison between the
two systems for six of the MCs. Based on the MC area calculation and the visual comparison in this study, it can be
determined that s-DBT has improved x-y plane sharpness than continuous motion DBT.
Table 1: Results of the MC area calculation and the FWHM of the ASF. Results show that for every MC analyzed, s-DBT
outperformed the continuous motion DBT system in localization of the MCs in the x, y, and z directions.
Percent FWHM FWHM
MC s-DBT DBT
Area of ASF of ASF -
case Area Area
Decrease - s-DBT DBT
Number (mm2) (mm2)
for s-DBT (mm) (mm)
1 3.6 4.09 11.98 3.5 5
2 2.33 3.66 36.34 2.5 4.5
3 2.79 3.05 8.52 2 4
4 1.69 2.79 39.43 1.5 5
5 1.74 3.08 43.51 1.5 4
6 2.96 3.59 17.55 2.5 4
7 1.7 2.74 37.96 1.5 3.5
8 2.21 3.69 40.11 1.5 4
9 2.1 3.69 43.09 2.5 4
10 2.43 3.21 24.30 3.5 4.5
11 2.5 3.1 19.35 3.5 5
12 2.82 3.76 25.00 2.5 5
MC 1 MC 2 MC 3 MC 4 MC 5 MC 6
Figure 5: Zoomed in ROIs of the first 6 MCs. The row above contains the s-DBT reconstruction images, while the row below
contains the continuous motion DBT system reconstruction images.
Proc. of SPIE Vol. 9033 903316-6
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
3.3 Z-axis sharpness
Figure 6 shows the ASF of s-DBT and continuous motion DBT for MC number 6. For this MC, the FWHM was
found to be 2.5 mm for s-DBT and 4 mm for DBT. Table 1 shows all results for the 12 MCs. The s-DBT system
reduced the ASF width by an average of 2.00±0.67 mm. From the data it can be seen that s-DBT has better z-axis
sharpness than continuous motion DBT.
ASF: s-DBT vs. Continuous Motion DBT
Normalized Average Intensity
1
s-DBT
Continous Motion DBT
0.8
0.6
0.4
0.2
0
-3 -2 -1 0 1 2 3
Distance from Plane of Focus (mm)
Figure 6: Plot of the ASF for s-DBT and continuous motion DBT for MC number 6. The larger angular coverage of the s-DBT
system reduces out-of-plane reconstruction artifacts.
4. DISCUSSION AND CONCLUSION
This work demonstrates that an s-DBT system can produce increased microcalcification sharpness in human breast
tissue compared to a Selenia Dimensions DBT system. Increased MC sharpness leads to increased MC visibility,
which is apparent in Figure 4 and Figure 5. Increased MC sharpness was shown for every MC that was analyzed.
Increased sharpness in the x-y plane of an s-DBT reconstruction slice comes from the decreased size of the effective
focal spot. In a continuous motion DBT system, such as the Selenia Dimensions, the focal spot is blurred during
image acquisition. The blurring of the focal spot increases the effective focal spot size of the system. Consequently,
increasing the exposure of an image acquisition further increases the effective focal spot size by increasing the
amount of X-ray tube travel time. An s-DBT system has no focal spot blur. Therefore, the effective focal spot size
is equal to the focal spot size times the focal spot enlargement factor (as with all X-ray imaging systems).
Increasing the exposure of an image acquisition does not change the effective focal spot size, only the acquisition
time. This is consistent with previous phantom studies that show an increase in the value of the MTF for s-DBT9, 10.
As the angular span of a single source DBT system increases so does the z-axis sharpness and the total acquisition
time. Long acquisition times in mammography leads to patient motion which can decrease image sharpness. The
effect of patient motion on image sharpness can be more dramatic than the focal spot blurring of continuous motion
DBT systems13. An s-DBT system is capable of using larger angular spans with zero increase in image acquisition
time. The increased z-axis sharpness in s-DBT not only increases MC visibility but also further decreases tissue
overlap. A large angular span gives better coverage of the Fourier domain, which is the underlying reason behind
the increased MC visibility and decreased tissue overlap.
Proc. of SPIE Vol. 9033 903316-7
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
We reported the first comparison of an s-DBT system with a continuous motion DBT system using human breast
tissue. It has been shown that s-DBT is capable of producing higher MC sharpness in the x, y, and z directions.
MCs ranging in measured in-plane area from 1.69 to 3.6 mm2 had an average decrease in area of 28.92±12.60% and
an average decrease in ASF width of 2.00±0.67 mm when imaged on the s-DBT system compared to the Selenia
Dimensions. The higher sharpness of s-DBT reconstructions could produce higher area under the curve values for
screening patients with MCs. This study was conducted without the focusing voltage of the s-DBT system on. A
further increase in sharpness is expected with the focusing electrodes engaged.
5. ACKNOWLEDGEMENT
The project is supported by the National Cancer Institute under grant number U54CA119343. We would like to
thank Hologic for providing the Selenia Dimension tomosynthesis system and for technical support. Thanks to
Emily Gidcumb, Christy Inscoe, Jing Shan, and Marci Potuzko for support in acquiring image datasets.
6. REFERENCES
[1] Itani, M., Griffin, A. T., and Whitman, G. J., “Mammography of breast calcifications,” Imaging,
5(1), 63-74 (2013).
[2] Sickles, E. A., “Breast calcifications: mammographic evaluation,” Radiology, 160(2), 289-293
(1986).
[3] Elmore, J. G., Barton, M. B., Moceri, V. M. et al., “Ten-year risk of false positive screening
mammograms and clinical breast examinations,” New England Journal of Medicine, 338(16),
1089-1096 (1998).
[4] Wu, T., Moore, R. H., Rafferty, E. A. et al., “A comparison of reconstruction algorithms for breast
tomosynthesis,” Medical Physics, 31(9), 2636 (2004).
[5] Rafferty, E. A., Park, J. M., Philpotts, L. E. et al., “Assessing radiologist performance using
combined digital mammography and breast tomosynthesis compared with digital
mammography alone: results of a multicenter, multireader trial,” Radiology, 266(1), 104-113
(2013).
[6] Michell, M., Iqbal, A., Wasan, R. et al., “A comparison of the accuracy of film-screen
mammography, full-field digital mammography, and digital breast tomosynthesis,” Clinical
radiology, 67(10), 976-981 (2012).
[7] Bernardi, D., Ciatto, S., Pellegrini, M. et al., “Prospective study of breast tomosynthesis as a
triage to assessment in screening,” Breast Cancer Res Treat, 133(1), 267-71 (2012).
[8] Qian, X., Rajaram, R., Calderon-Colon, X. et al., “Design and characterization of a spatially
distributed multibeam field emission x-ray source for stationary digital breast tomosynthesis,”
Medical Physics, 36(10), 4389-4399 (2009).
[9] Qian, X., Tucker, A., Gidcumb, E. et al., “High resolution stationary digital breast tomosynthesis
using distributed carbon nanotube x-ray source array,” Medical Physics, 39(4), 2090 (2012).
[10] Tucker, A. W., Lu, J., and Zhou, O., “Dependency of image quality on system configuration
parameters in a stationary digital breast tomosynthesis system,” Medical Physics, 40(3), 031917-
10 (2013).
[11] Ren, B., Ruth, C., Wu, T. et al., "A new generation FFDM/tomosynthesis fusion system with
selenium detector," Proc. SPIE. 7622, 76220B (2010).
[12] Kuo, J., Ringer, P. A., Fallows, S. G. et al., "Dynamic reconstruction and rendering of 3D
tomosynthesis images," Proc. SPIE. 7961, 796116 (2011).
Proc. of SPIE Vol. 9033 903316-8
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
[13] Acciavatti, R. J., and Maidment, A. D., "Optimization of continuous tube motion and step-and-
shoot motion in digital breast tomosynthesis systems with patient motion," Proc. SPIE. 8313,
831306-1-831306-12 (2012).
Proc. of SPIE Vol. 9033 903316-9
Downloaded From: http://proceedings.spiedigitallibrary.org/ on 06/27/2016 Terms of Use: http://spiedigitallibrary.org/ss/TermsOfUse.aspx
Вам также может понравиться
- Kidney and Tumor Segmentation Using Combined Deep Learning MethodДокумент11 страницKidney and Tumor Segmentation Using Combined Deep Learning MethodegamrОценок пока нет
- The Basics of Maxillofacial Cone Beam Computed Tomography: Allan G. Farman and William C. ScarfeДокумент12 страницThe Basics of Maxillofacial Cone Beam Computed Tomography: Allan G. Farman and William C. ScarfeMANUELA GUTIERREZ MESAОценок пока нет
- Clinical: Clinical Applications of Cone-Beam Computed Tomography in Dental PracticeДокумент6 страницClinical: Clinical Applications of Cone-Beam Computed Tomography in Dental PracticeNaro HassanОценок пока нет
- Chapter 22 - Computed Tomography Simulation ProceduresДокумент30 страницChapter 22 - Computed Tomography Simulation ProceduresCarlo Gangcuangco ValdezОценок пока нет
- 3D Cone-Beam CT With A Twin Robotic X-Ray System in Elbow Imaging Comparison of Image Quality To High-Resolution Multidetector CTДокумент9 страниц3D Cone-Beam CT With A Twin Robotic X-Ray System in Elbow Imaging Comparison of Image Quality To High-Resolution Multidetector CTfadi.hadbh28Оценок пока нет
- Breast Tomosynthesis:: Special ReviewДокумент13 страницBreast Tomosynthesis:: Special ReviewMelanie DascăluОценок пока нет
- Comparison of Cone-Beam Imaging With Orthopantomography and Computerized Tomography For Assessment in Presurgical Implant DentistryДокумент10 страницComparison of Cone-Beam Imaging With Orthopantomography and Computerized Tomography For Assessment in Presurgical Implant DentistryMihai DascalescuОценок пока нет
- Automatic Segmentation of Liver Tumor in CT ImagesДокумент6 страницAutomatic Segmentation of Liver Tumor in CT Imagesmanju.dsatmОценок пока нет
- NahidaДокумент7 страницNahidaانجاز مشاريعОценок пока нет
- Contrast-Enhanced MammographyОт EverandContrast-Enhanced MammographyMarc LobbesОценок пока нет
- Currently Available Maxillofacial CBCT EquipmentДокумент4 страницыCurrently Available Maxillofacial CBCT EquipmentzilniОценок пока нет
- 3D Cone-Beam CT of The Ankle Using A Novel Twin Robotic X-Ray SystemДокумент7 страниц3D Cone-Beam CT of The Ankle Using A Novel Twin Robotic X-Ray Systemanderson.mancianoОценок пока нет
- Effect of Voxel Size On The Accuracy of 3D Reconstructions With - DMFR - 81804525Документ7 страницEffect of Voxel Size On The Accuracy of 3D Reconstructions With - DMFR - 81804525doutormarcoОценок пока нет
- X-Ray Guided Robotic Radiosurgery For Solid Tumors: Industrial Robot February 2001Документ12 страницX-Ray Guided Robotic Radiosurgery For Solid Tumors: Industrial Robot February 2001Alex SheldonОценок пока нет
- Development of 3D Patient-Based Super-Resolution Digital Breast Phantoms Using MLДокумент13 страницDevelopment of 3D Patient-Based Super-Resolution Digital Breast Phantoms Using MLbirdie namnamОценок пока нет
- Evaluation of RT Imaging DevicesДокумент7 страницEvaluation of RT Imaging DevicesKurt Van DelinderОценок пока нет
- Digital Breast TomosynthesisДокумент24 страницыDigital Breast Tomosynthesisمهدي الزيودОценок пока нет
- Recent Advances in Mammography: DR - Suhas B Resident (MD Radio-DiagnosisДокумент69 страницRecent Advances in Mammography: DR - Suhas B Resident (MD Radio-DiagnosisMassimo RiserboОценок пока нет
- Temporal Bone Imaging: Comparison of Flat Panel Volume CT and Multisection CTДокумент6 страницTemporal Bone Imaging: Comparison of Flat Panel Volume CT and Multisection CTNovi DwiyantiОценок пока нет
- A Deep Learning Approach For Radiological Detection and Classification ofДокумент8 страницA Deep Learning Approach For Radiological Detection and Classification ofroomaarlopezsalgadoОценок пока нет
- Truncation Artifact and Boundary Artifact Reduction in Breast Tomosynthesis ReconstructionДокумент9 страницTruncation Artifact and Boundary Artifact Reduction in Breast Tomosynthesis ReconstructionLaudani GómezОценок пока нет
- Microwave Imaging ThesisДокумент4 страницыMicrowave Imaging ThesisSteven Wallach100% (2)
- Computed TomographyДокумент4 страницыComputed TomographyemilyОценок пока нет
- Scatter Correction Method For Cone-Beam CT Based On Interlacing-Slit ScanДокумент8 страницScatter Correction Method For Cone-Beam CT Based On Interlacing-Slit ScanСергій СенчуровОценок пока нет
- Shouldconebeam Computedtomographybe Routinelyobtainedinimplant Planning?Документ17 страницShouldconebeam Computedtomographybe Routinelyobtainedinimplant Planning?javiers45Оценок пока нет
- Lung Paper - ModifiedДокумент12 страницLung Paper - ModifiedMaheswari VutukuriОценок пока нет
- Computerized Detection of Lung Nodules by Means of "Virtual Dual-Energy" RadiographyДокумент10 страницComputerized Detection of Lung Nodules by Means of "Virtual Dual-Energy" RadiographyAntony RatheeshОценок пока нет
- BGRT 4Документ7 страницBGRT 4Nelson Appiah-AgyeiОценок пока нет
- Radio Digital 1Документ6 страницRadio Digital 1Lucy Esther Calvo PerniaОценок пока нет
- Helianthus DBT EngДокумент16 страницHelianthus DBT EngDavid Enrique Camacho PinedaОценок пока нет
- Jurnal 3 - Imaging Anatomy of The Jaw and Dentition With Cone Beam Computed Tomography - Febby Sitti NurДокумент11 страницJurnal 3 - Imaging Anatomy of The Jaw and Dentition With Cone Beam Computed Tomography - Febby Sitti NurFEBBY SITTIОценок пока нет
- Original ContributionДокумент13 страницOriginal ContributionBarron ManОценок пока нет
- A BERT Encoding With Recurrent Neural Network and Long-Short Term Memory For Breast Cancer Image Classification - 1-s2.0-S2772662223000176-MainДокумент15 страницA BERT Encoding With Recurrent Neural Network and Long-Short Term Memory For Breast Cancer Image Classification - 1-s2.0-S2772662223000176-MainSrinitish SrinivasanОценок пока нет
- 2019 20 Bio Medical Titles With AbstractsДокумент16 страниц2019 20 Bio Medical Titles With AbstractsWekesa RobinsonОценок пока нет
- An Overview of Volumetric Imaging Technologies and Their Quality Assurance For IGRTДокумент9 страницAn Overview of Volumetric Imaging Technologies and Their Quality Assurance For IGRTBounegta AhmedОценок пока нет
- X GuideNavigationModelAccuracyJOI10.16Документ7 страницX GuideNavigationModelAccuracyJOI10.16Mrinmayee ThakurОценок пока нет
- A Visual 3d-Tracking and Positioning Technique For Stereotaxy With CT ScannersДокумент11 страницA Visual 3d-Tracking and Positioning Technique For Stereotaxy With CT Scannershectorkevin2008Оценок пока нет
- Radiation Oncology: Investigation of The Usability of Conebeam CT Data Sets For Dose CalculationДокумент13 страницRadiation Oncology: Investigation of The Usability of Conebeam CT Data Sets For Dose CalculationCarolina CorreiaОценок пока нет
- Sanders - Samei - 2016 - Patient-Specific Quantification of Image Quality - Method For Measuring Resolution in Clinical CT Images - Medical - PhysicsДокумент10 страницSanders - Samei - 2016 - Patient-Specific Quantification of Image Quality - Method For Measuring Resolution in Clinical CT Images - Medical - PhysicsmartuflashОценок пока нет
- Resume C-ArmДокумент4 страницыResume C-Armp27838121011Оценок пока нет
- Plagiarism Scan Report Plagiarism Scan Report: Content Checked For Plagiarism Content Checked For PlagiarismДокумент2 страницыPlagiarism Scan Report Plagiarism Scan Report: Content Checked For Plagiarism Content Checked For PlagiarismBlack Hack HakerОценок пока нет
- Three-Dimensional Computerized Orthognathic Surgical Treatment PlanningДокумент10 страницThree-Dimensional Computerized Orthognathic Surgical Treatment PlanningRajan KarmakarОценок пока нет
- TAC PeñascoДокумент10 страницTAC PeñascoJose ManuelОценок пока нет
- EBCD (Early Breast Cancer Detector)Документ3 страницыEBCD (Early Breast Cancer Detector)Vivi KoОценок пока нет
- Quality Assurance For Image-Guided Radiation Therapy Utilizing CT-basedДокумент18 страницQuality Assurance For Image-Guided Radiation Therapy Utilizing CT-based2016508吳翊晨Оценок пока нет
- 20 09 25 Pristina Dose White Paper - JB73643XXДокумент10 страниц20 09 25 Pristina Dose White Paper - JB73643XXMerab KvintradzeОценок пока нет
- ImplantesДокумент5 страницImplantesTania CGОценок пока нет
- Cohen2019 Atualização Sobre Os Aspectos Atuais Da Imagem Orbital .Tomografia Computadorizada, Ressonância Magnética e UltrassonografiaДокумент11 страницCohen2019 Atualização Sobre Os Aspectos Atuais Da Imagem Orbital .Tomografia Computadorizada, Ressonância Magnética e Ultrassonografiaana clara scopelОценок пока нет
- KamasutraДокумент20 страницKamasutraBlach MentholОценок пока нет
- Deep Learning-Based Segmentation of Epithelial Ovarian Cancer On T2-Weighted Magnetic Resonance ImagesДокумент14 страницDeep Learning-Based Segmentation of Epithelial Ovarian Cancer On T2-Weighted Magnetic Resonance Imagessukeshini jadhavОценок пока нет
- Classification of Whole Mammogram and Tomosynthesis Images Using Deep Convolutional Neural NetworksДокумент6 страницClassification of Whole Mammogram and Tomosynthesis Images Using Deep Convolutional Neural NetworksPriya HankareОценок пока нет
- Deep Learning-Based Cell Identification and Disease Diagnosis Using Spatio-Temporal Cellular Dynamics in Compact Digita PDFДокумент18 страницDeep Learning-Based Cell Identification and Disease Diagnosis Using Spatio-Temporal Cellular Dynamics in Compact Digita PDFJeffreyОценок пока нет
- Computer VisionДокумент12 страницComputer VisionMoriwamОценок пока нет
- 1 s2.0 S2212440312000442 MainДокумент6 страниц1 s2.0 S2212440312000442 MainMarinaОценок пока нет
- Digital Mammography RCNAДокумент14 страницDigital Mammography RCNADr PiyushОценок пока нет
- Textbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationОт EverandTextbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationОценок пока нет
- Computed Tomography MachineДокумент24 страницыComputed Tomography MachineGaurav Molankar100% (1)
- 1.principles of ContrastДокумент8 страниц1.principles of Contrastvidi87Оценок пока нет
- PravallikaДокумент28 страницPravallikaVegesana SumythriОценок пока нет
- An Image Based Vibration Sensor For Soft Tissue Modal Analysis in A Digital Image Elasto Tomography (DIET) SystemДокумент4 страницыAn Image Based Vibration Sensor For Soft Tissue Modal Analysis in A Digital Image Elasto Tomography (DIET) Systemjuliogomez008Оценок пока нет
- Amx4 Series DiagnosticsДокумент216 страницAmx4 Series DiagnosticsLuis Lizama93% (15)
- Field Emission Displays: A Critical Review: A.A. Talin, K.A. Dean, J.E. JaskieДокумент14 страницField Emission Displays: A Critical Review: A.A. Talin, K.A. Dean, J.E. JaskieFanof EcdОценок пока нет
- GE AMX 4 Plus Portable X-Ray System BrochureДокумент5 страницGE AMX 4 Plus Portable X-Ray System BrochureFanof Ecd0% (1)
- 510 (K) of Safety and Effectiveness: GE Medical P.O. B 0 4 1 4, WIДокумент4 страницы510 (K) of Safety and Effectiveness: GE Medical P.O. B 0 4 1 4, WIFanof EcdОценок пока нет
- Field Emission Cathodes To Form An Electron Beam Prepared From Carbon Nanotube SuspensionsДокумент32 страницыField Emission Cathodes To Form An Electron Beam Prepared From Carbon Nanotube SuspensionsFanof EcdОценок пока нет
- NIH Public Access: Author ManuscriptДокумент16 страницNIH Public Access: Author ManuscriptFanof EcdОценок пока нет
- Microelectronic Engineering: Masayoshi Nagao, Tomoya YoshidaДокумент7 страницMicroelectronic Engineering: Masayoshi Nagao, Tomoya YoshidaFanof EcdОценок пока нет
- Behling 2017Документ25 страницBehling 2017Fanof EcdОценок пока нет
- Piranha: Reference Manual - English - Version 5.5DДокумент104 страницыPiranha: Reference Manual - English - Version 5.5DFanof EcdОценок пока нет
- Ahernandez Tasmics Published PDFДокумент17 страницAhernandez Tasmics Published PDFFanof EcdОценок пока нет
- Ahernandez Tasmics Published PDFДокумент17 страницAhernandez Tasmics Published PDFFanof EcdОценок пока нет
- X-Ray Production: Online TextbookДокумент14 страницX-Ray Production: Online TextbookFanof EcdОценок пока нет
- L3 Comparison ZimekДокумент105 страницL3 Comparison ZimekFanof EcdОценок пока нет
- 2015 JMEMS X Rays VelasquezДокумент11 страниц2015 JMEMS X Rays VelasquezFanof EcdОценок пока нет
- CS 7 Universal Controller Sell Sheet M1086 317 RevAДокумент1 страницаCS 7 Universal Controller Sell Sheet M1086 317 RevAFanof EcdОценок пока нет
- Calle de La Lectura 2011Документ25 страницCalle de La Lectura 2011Fanof EcdОценок пока нет
- KDR DDR Sell Sheet M1583 0120 RevAДокумент1 страницаKDR DDR Sell Sheet M1583 0120 RevAFanof EcdОценок пока нет
- CS7 Operations Manual 1.30 PDFДокумент424 страницыCS7 Operations Manual 1.30 PDFHoàng Dương NguyễnОценок пока нет
- See Radiology Like Never Before.: KDR AU-DDR SystemДокумент6 страницSee Radiology Like Never Before.: KDR AU-DDR SystemFanof EcdОценок пока нет
- RadComp4.2 User ManualДокумент21 страницаRadComp4.2 User ManualFanof EcdОценок пока нет
- P2110 DatasheetДокумент12 страницP2110 DatasheetR Bonifacio DaitanОценок пока нет
- Bigfoot The MonsterДокумент9 страницBigfoot The MonsterFanof EcdОценок пока нет
- Patterned Transparent Conducting Films For Touch Sensor ApplicationsДокумент1 страницаPatterned Transparent Conducting Films For Touch Sensor ApplicationsFanof EcdОценок пока нет
- Icnirp PDFДокумент20 страницIcnirp PDFJorge AguirreОценок пока нет
- Ortel - Letter AgreementДокумент2 страницыOrtel - Letter AgreementFanof EcdОценок пока нет
- Motion To Vacate Brief and Supporting DeclarationsДокумент65 страницMotion To Vacate Brief and Supporting DeclarationsAlyssaBereznakОценок пока нет
- Stephen Rizzone BioДокумент2 страницыStephen Rizzone BioFanof EcdОценок пока нет
- Software Access PointДокумент5 страницSoftware Access PointFanof EcdОценок пока нет
- Ossia Q & A: General Company Questions What Is Ossia?Документ7 страницOssia Q & A: General Company Questions What Is Ossia?Fanof EcdОценок пока нет
- Mathis Et. Al. Intraoperative MV & PPCДокумент17 страницMathis Et. Al. Intraoperative MV & PPCJun HungОценок пока нет
- Backpacking First Aid KitДокумент2 страницыBackpacking First Aid KitAndrewОценок пока нет
- Beyond Wedge: Clinical Physiology and The Swan-Ganz CatheterДокумент12 страницBeyond Wedge: Clinical Physiology and The Swan-Ganz Catheterkromatin9462Оценок пока нет
- Toxicology Manual PDFДокумент250 страницToxicology Manual PDFJuliane Sunga100% (2)
- POPS PretestДокумент6 страницPOPS Pretestkingjameson1Оценок пока нет
- Implementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardДокумент9 страницImplementasi Program Antenatal Terpadu Di Puskesmas Tanjung Agung Kabupaten Ogan Komering Ulu Dengan Pendekatan Balance ScorecardRosinta Dwi OktaviaОценок пока нет
- This Study Resource Was Shared Via: Fncp-Health Deficit: Diabetes MellitusДокумент3 страницыThis Study Resource Was Shared Via: Fncp-Health Deficit: Diabetes MellitusAlhadzra AlihОценок пока нет
- Modern Concepts in Aesthetic Dentistry AДокумент247 страницModern Concepts in Aesthetic Dentistry AHamad KayaniОценок пока нет
- Family Planning in The Hospital Operational Guide For Recording and Reporting PDFДокумент69 страницFamily Planning in The Hospital Operational Guide For Recording and Reporting PDFViolet CherryОценок пока нет
- Basic Principles of Periodontal SurgeryДокумент100 страницBasic Principles of Periodontal SurgerySandip Ladani100% (2)
- Thrombolytic Therapy in Acute Myocardial InfarctionДокумент7 страницThrombolytic Therapy in Acute Myocardial InfarctionRumela Ganguly ChakrabortyОценок пока нет
- 01CLOSTRIDIUMДокумент15 страниц01CLOSTRIDIUMaldea_844577109Оценок пока нет
- NT Biology Answers Chapter 11Документ4 страницыNT Biology Answers Chapter 11ASADОценок пока нет
- Ok Urologi Maret 2021 Minggu IДокумент25 страницOk Urologi Maret 2021 Minggu ILittle DevОценок пока нет
- Cannabis and Cannabinoids in The Perioperative PeriodДокумент15 страницCannabis and Cannabinoids in The Perioperative PeriodyenuginОценок пока нет
- 2015catalog PDFДокумент52 страницы2015catalog PDFNegoi Mihai0% (1)
- Jurnal SinusitisДокумент4 страницыJurnal SinusitisAndriyani YaniОценок пока нет
- Chylothorax OriginalДокумент4 страницыChylothorax OriginalMaria CostandachiОценок пока нет
- Carcinoma of PancreasДокумент15 страницCarcinoma of Pancreasعمار عارفОценок пока нет
- The Well-Being of The EMT: Emergency Medical Technician - BasicДокумент30 страницThe Well-Being of The EMT: Emergency Medical Technician - Basicalsyahrin putraОценок пока нет
- Anaphy ReviewerДокумент19 страницAnaphy ReviewerGian Paolo P. CHAVEZОценок пока нет
- Chapter 43 - Thrombocytopenia and ThrombocytosisДокумент6 страницChapter 43 - Thrombocytopenia and ThrombocytosisNathaniel SimОценок пока нет
- HR Policy ManualДокумент34 страницыHR Policy Manualshamna AbdullaОценок пока нет
- Fynadine 20mgДокумент2 страницыFynadine 20mgNgo Van TruongОценок пока нет
- Journal of Chronic PainДокумент8 страницJournal of Chronic PainRirin TriyaniОценок пока нет
- Fracture of The Upper HumerusДокумент22 страницыFracture of The Upper HumerusOlasinde AnthonyОценок пока нет
- Jurnal 4Документ5 страницJurnal 4Nindita RahmaОценок пока нет
- Cardiovascular Examination: Preparation of The PatientДокумент4 страницыCardiovascular Examination: Preparation of The PatientLolla SinwarОценок пока нет
- Perspektif Keperawatan PaliatifДокумент11 страницPerspektif Keperawatan PaliatifAyudina FebrianiОценок пока нет
- Mci Ayn Muswil PtbmmkiДокумент49 страницMci Ayn Muswil PtbmmkiLucya WulandariОценок пока нет