Академический Документы
Профессиональный Документы
Культура Документы
Nursing Care Plan: Artery Blockage May Be
Загружено:
Dienizs Labini Tadena0 оценок0% нашли этот документ полезным (0 голосов)
34 просмотров5 страниц1. The patient presented with an altered level of consciousness possibly due to coagulopathy from a stroke.
2. Over the next 24 hours, the nursing care plan aims to maintain or improve the patient's level of consciousness, cognition, motor function and vital signs while monitoring for increased intracranial pressure.
3. Interventions include frequent assessments of vital signs, neurological function, factors contributing to decreased cerebral perfusion and signs of neurological deterioration which could require transferring the patient to critical care.
Исходное описание:
Оригинальное название
D123 NCP
Авторское право
© © All Rights Reserved
Доступные форматы
DOCX, PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документ1. The patient presented with an altered level of consciousness possibly due to coagulopathy from a stroke.
2. Over the next 24 hours, the nursing care plan aims to maintain or improve the patient's level of consciousness, cognition, motor function and vital signs while monitoring for increased intracranial pressure.
3. Interventions include frequent assessments of vital signs, neurological function, factors contributing to decreased cerebral perfusion and signs of neurological deterioration which could require transferring the patient to critical care.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
34 просмотров5 страницNursing Care Plan: Artery Blockage May Be
Загружено:
Dienizs Labini Tadena1. The patient presented with an altered level of consciousness possibly due to coagulopathy from a stroke.
2. Over the next 24 hours, the nursing care plan aims to maintain or improve the patient's level of consciousness, cognition, motor function and vital signs while monitoring for increased intracranial pressure.
3. Interventions include frequent assessments of vital signs, neurological function, factors contributing to decreased cerebral perfusion and signs of neurological deterioration which could require transferring the patient to critical care.
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате DOCX, PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 5
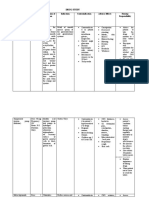
NURSING CARE PLAN
ASSESSMENT DIAGNOSIS PLANNING INTERVENTIONS RATIONALE EVALUATION
OBJECTIVE: Ineffective Cerebral After 24 hours, the patient 1. Assess factors 1. Assessment will determine After 24 hours, the patient
Loss of Perfusion maybe r/t will maintain; related to individual and influence the choice of will maintain;
consciousness coagulopathy as 1. Maintain usual situation for interventions. Deterioration in 1. Maintain usual
VS taken: evidenced by altered or improved decreased cerebral neurological signs or failure to or improved
BT: 36 LOC. LOC, cognition, perfusion and improve after initial insult LOC, cognition,
BP: 180/120 and motor and potential for may reflect decreased and motor and
PR: 78 sensory function. increased ICP. intracranial adaptive capacity sensory function.
RR: 18 2. Demonstrate 2. Changes in blood requiring patient to be 2. Demonstrate
stable vital signs pressure, compare transferred to critical area for stable vital signs
and absence of BP readings in both monitoring of ICP, other and absence of
increased ICP. arms. therapies. If the stroke is increased ICP.
3. Display no evolving, patient can 3. Display no
further 3. Heart rate and deteriorate quickly and require further
deterioration or rhythm, assess for repeated assessment and deterioration or
recurrence of murmurs. progressive treatment. If the recurrence of
deficits. 4. Respirations, noting stroke is “completed,” the deficits.
patterns and neurological deficit is GOAL WAS NOT MET
rhythm (periods nonprogressive, and treatment
of apnea after is geared toward rehabilitation
hyperventilation), and preventing recurrence.
Cheyne-Stokes 2. Fluctuations in pressure may
respiration. occur because of cerebral
injury in vasomotor area of
5. Evaluate pupils, the brain. Hypertension or
noting size, shape, postural hypotension may
equality, light have been a precipitating
reactivity. factor. Hypotension may
occur because of shock
6. Document changes (circulatory
in vision: reports of collapse). Increased ICP may
blurred vision, occur because of tissue edema
alterations in visual or clot formation. Subclavian
field, depth artery blockage may be
perception. revealed by difference in
7. Assess higher pressure readings between
functions, including arms.
speech, if patient is 3. Changes in rate, especially
alert. bradycardia, can occur
because of the brain damage.
8. Position with head Dysrhythmias and murmurs
slightly elevated may reflect cardiac disease,
and in neutral which may have precipitated
position. CVA (stroke after MI or from
9. Maintain bedrest, valve dysfunction).
provide quiet and 4. Irregularities can suggest
relaxing location of cerebral
environment, insult or increasing ICP and
restrict visitors and need for further intervention,
activities. Cluster including possible respiratory
nursing support.
interventions and 5. Pupil size and equality is
provide rest periods determined by balance
between care between parasympathetic and
activities. Limit sympathetic innervation.
duration of Response to light reflects
procedures. combined function of the
optic (II) and oculomotor (III)
cranial nerves.
6. Specific visual alterations
reflect area of brain involved,
indicate safety concerns, and
influence choice of
interventions.
7. Changes in cognition and
speech content are an
indicator of location and
degree of cerebral
involvement and may indicate
deterioration or increased ICP.
8. Reduces arterial pressure by
promoting venous drainage
and may improve cerebral
perfusion.
9. Continuous stimulation or
activity can increase
intracranial pressure
(ICP). Absolute rest and quiet
may be needed to prevent
rebleeding in the case of
hemorrhage.
ASSESSMENT DIAGNOSIS PLANNING INTERVENTIONS RATIONALE EVALUATION
OBJECTIVE: Impaired verbal After 24 hours, the 1. Listen for 1. Feedback helps patient After 24 hours, the
errors in realize why caregivers
CVD patient communication r/t patient will; conversation are not understanding patient will;
and provide or responding
Difficulty of to alteration in feedback. appropriately and
1. Indicate an 2. Point to provides opportunity 1. Indicate an
speech perception as objects and ask to clarify meaning.
understanding understanding
patient to 2. Tests for expressive
of the of the
Restlessness name them. aphasia. Patient may
evidenced by communication communication
3. Ask patient to recognize item but not
problems. write his name be able to name it. problems.
NGT Feed difficulty of
2. Establish and a short 3. Tests for writing 2. Establish
method of sentence. If disability (agraphia) method of
Unable to comprehending or unable to and deficits in reading
communication communication
write, have comprehension
communicate in which needs in which needs
maintaining patient read a (alexia), which are
can be can be
short sentence. also part of receptive
VS taken: communication. expressed. 4. Write a notice and expressive expressed.
3. Use resources at the nurses’ aphasia. 3. Use resources
BT: 36 station and 4. Allays anxiety related
appropriately. appropriately.
patient’s room to inability to
BP: 180/120 about speech communicate GOAL WAS NOT MET
impairment. and fear that needs
PR: 78 Provide a will not be met
special call promptly.
RR: 18 bell that can be 5. Helpful in decreasing
activated by frustration when
minimal dependent on others
pressure if and unable to
necessary. communication
5. Anticipate and desires.
provide for 6. Reduces confusion and
patient’s allays anxiety at
needs. having to process and
6. Talk directly respond to large
to patient, amount of information
speaking at one time. As
slowly and retraining progresses,
distinctly. advancing complexity
Phrase of communication
questions to be stimulates memory
answered and further enhances
simply by yes word and idea
or no. Progress association.
in complexity 7. Assesses individual
as patient verbal capabilities and
responds. sensory, motor, and
7. Respect cognitive functioning
patient’s to identify
preinjury deficits/therapy needs.
capabilities;
avoid
“speaking
down” to
patient or
making
patronizing
remarks.
8. Consult and
refer patient to
speech
therapist.
Вам также может понравиться
- NCP For Subarachnoid HemorrhageДокумент4 страницыNCP For Subarachnoid HemorrhageJoan Rose Rendon-Hung78% (18)
- NCP - Decreased Intracranial Adaptive Capacity R/T Space - Occupying Lesion.Документ1 страницаNCP - Decreased Intracranial Adaptive Capacity R/T Space - Occupying Lesion.Carl Elexer Cuyugan Ano100% (6)
- Neurology Multiple Choice Questions With Explanations: Volume IОт EverandNeurology Multiple Choice Questions With Explanations: Volume IРейтинг: 4 из 5 звезд4/5 (7)
- Nursing Care PlanДокумент4 страницыNursing Care Planmanu_gutierrez0891% (11)
- Nursing Care Plan For HypertensionДокумент4 страницыNursing Care Plan For HypertensionKathleen Dimacali100% (2)
- NCP #1 Ineffective Cerebral Tissue PerfusionДокумент4 страницыNCP #1 Ineffective Cerebral Tissue PerfusionsteffiОценок пока нет
- NCP Ineffective Cerebral Tissue Perfusion STROKEДокумент3 страницыNCP Ineffective Cerebral Tissue Perfusion STROKEMa. Elaine Carla TatingОценок пока нет
- Hypertension Nursing Care PlanДокумент3 страницыHypertension Nursing Care Plangeng gengОценок пока нет
- HALOPERIDOL Drug StudyДокумент2 страницыHALOPERIDOL Drug Studyanreilegarde89% (9)
- Nursing Care Plan For HypertensionДокумент5 страницNursing Care Plan For HypertensionJessy MalloОценок пока нет
- Decreased Cardiac Output EclampsiaДокумент6 страницDecreased Cardiac Output EclampsiaNursesLabs.com100% (7)
- Nursing Care Plan For Palliative Care Nursing NotesДокумент2 страницыNursing Care Plan For Palliative Care Nursing NotesblaireОценок пока нет
- Urinary Tract Infection Nursing-Care-PlanДокумент3 страницыUrinary Tract Infection Nursing-Care-PlanRnspeakcomОценок пока нет
- (Adolescence and Education) Tim Urdan, Frank Pajares - Academic Motivation of Adolescents-IAP - Information Age Publishing (2004) PDFДокумент384 страницы(Adolescence and Education) Tim Urdan, Frank Pajares - Academic Motivation of Adolescents-IAP - Information Age Publishing (2004) PDFAllenОценок пока нет
- The Permission Wheel Hawkes L PDFДокумент8 страницThe Permission Wheel Hawkes L PDFNandita Asthana SankerОценок пока нет
- Case Study 1 NCPДокумент3 страницыCase Study 1 NCPJayson SamonteОценок пока нет
- Assessment Nursing Diagnosis Goals/ Objectives Nursing Interventions Rationale EvaluationДокумент4 страницыAssessment Nursing Diagnosis Goals/ Objectives Nursing Interventions Rationale EvaluationGene Chavez AppleОценок пока нет
- Nanda NCP BasedДокумент14 страницNanda NCP Baseddeliejoyce100% (1)
- Nursing Care Plan: Group 4-Open Wound Head Injury After Debris FallДокумент3 страницыNursing Care Plan: Group 4-Open Wound Head Injury After Debris FallNicole Villanueva, BSN - Level 3AОценок пока нет
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Objective: Short Term: Independent: Short TermДокумент3 страницыAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Objective: Short Term: Independent: Short TermMicaela CrisostomoОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care PlanMel Izhra N. MargateОценок пока нет
- NS3 Ncp-FdarДокумент5 страницNS3 Ncp-FdarArdiene Shallouvette GamosoОценок пока нет
- Actual Nursing Care Plan #1: Deficient Fluid VolumeДокумент7 страницActual Nursing Care Plan #1: Deficient Fluid VolumeAubrey SungaОценок пока нет
- Risk For Peripheral Neurodysfunction NCPДокумент3 страницыRisk For Peripheral Neurodysfunction NCPLeonardo Martin FrivaldoОценок пока нет
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveДокумент2 страницыNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanОценок пока нет
- CCU NCP Week 2Документ4 страницыCCU NCP Week 2April Kate BanagodosОценок пока нет
- NCPДокумент6 страницNCPJane CasiquinОценок пока нет
- Hypertension Nursing Care PlanДокумент3 страницыHypertension Nursing Care PlanAsylla PajijiОценок пока нет
- Kami Kagina, Gulpiyada Lang Siya Nadulaan Kusog Kag Gapukol Iya Hambalanon, Kag Nagakiwi Iya Nga Itsura." As VerbalizedДокумент4 страницыKami Kagina, Gulpiyada Lang Siya Nadulaan Kusog Kag Gapukol Iya Hambalanon, Kag Nagakiwi Iya Nga Itsura." As VerbalizedKoleen Lhyte T. UYОценок пока нет
- Data Nursing Diagnos IS Scientific Backgrou ND Goal/Objective Nursing Interventions Rationale EvaluationДокумент4 страницыData Nursing Diagnos IS Scientific Backgrou ND Goal/Objective Nursing Interventions Rationale EvaluationDienizs LabiniОценок пока нет
- Ineffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7Документ2 страницыIneffective Cerebral Tissue Perfusion Related To Interruption of Blood Flow Secondary To Hemorrhage As Evidenced by GCS of 7dana100% (4)
- Postop Actual &potential NCPДокумент12 страницPostop Actual &potential NCPJohn Paul Delos SantosОценок пока нет
- Baldo NCP R.A Case ObДокумент2 страницыBaldo NCP R.A Case ObRoxanne BaldoОценок пока нет
- Group 1 - VITALS SIGNS and INTERVENTIONSДокумент19 страницGroup 1 - VITALS SIGNS and INTERVENTIONSTrishОценок пока нет
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermДокумент5 страницAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term: Short TermJA BerzabalОценок пока нет
- Subdural HematomaДокумент4 страницыSubdural Hematomarodamel gundanОценок пока нет
- Ineffective Cerebral Tissue PerfusionДокумент4 страницыIneffective Cerebral Tissue PerfusionLeticia ElricОценок пока нет
- Risk For IneffectiveДокумент6 страницRisk For IneffectiveAce FabrigasОценок пока нет
- Jade R. Dinolan BSN-4: Diagnosi SДокумент5 страницJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- NCP BeeaДокумент3 страницыNCP BeeaKiko BernardinoОценок пока нет
- Date/Time Cues N E E D Nursing Diagnosis Objectives of Care Nursing Interventions EvaluationДокумент4 страницыDate/Time Cues N E E D Nursing Diagnosis Objectives of Care Nursing Interventions EvaluationRczhОценок пока нет
- Nursing Care Plan 1Документ4 страницыNursing Care Plan 1Kiko BernardinoОценок пока нет
- NCP - Tissue Perfusion (Cerebral)Документ2 страницыNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Decreased Cardiac OutputДокумент5 страницDecreased Cardiac Outputshuang81Оценок пока нет
- Nursing Care PlanДокумент3 страницыNursing Care PlanAmal Bacaraman MauteОценок пока нет
- annotated-COURSE TASK 2 INCREASED ICPДокумент8 страницannotated-COURSE TASK 2 INCREASED ICPJake AllegoОценок пока нет
- Hemorrhagic StrokeДокумент2 страницыHemorrhagic StrokeMuhammad Anwar AnsoriОценок пока нет
- Nursing Care PlanДокумент7 страницNursing Care PlanGem Ma100% (7)
- Nic IctpДокумент2 страницыNic IctpRobby BanjarОценок пока нет
- Concept Map, Neil Floyd Ventura PDFДокумент1 страницаConcept Map, Neil Floyd Ventura PDFNeil Floyd VenturaОценок пока нет
- Revised NCP 1-3Документ6 страницRevised NCP 1-3MarcieОценок пока нет
- NCP - Activity IntoleranceДокумент4 страницыNCP - Activity IntoleranceRoyce Vincent TizonОценок пока нет
- Patients Nursing PlanДокумент3 страницыPatients Nursing Planmharjoe pulmanoОценок пока нет
- Final NCP (Jannel)Документ6 страницFinal NCP (Jannel)Zed P. EstalillaОценок пока нет
- Med Ward NCP Week 3Документ4 страницыMed Ward NCP Week 3Ghianx Carlox PioquintoxОценок пока нет
- NCP (Stroke)Документ9 страницNCP (Stroke)Claire M. AuditorОценок пока нет
- Assessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGДокумент11 страницAssessment Explanation Planning Interventions Rationale Evaluation Subjective: Objective: STG: STGGrape JuiceОценок пока нет
- Log Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaДокумент4 страницыLog Book Case Debriefing With The Preceptor Name of The Trainee: SCFHS Reference No: Year: D D Case Category: Date: AreaS DОценок пока нет
- The Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareОт EverandThe Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareОценок пока нет
- The Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaОт EverandThe Psychology of Hysteria - A Selection of Classic Articles on the Analysis and Symptoms of HysteriaОценок пока нет
- A Simple Guide to Parkinson's Disease and Related Brain ConditionsОт EverandA Simple Guide to Parkinson's Disease and Related Brain ConditionsОценок пока нет
- Republic of The PhilippinesДокумент12 страницRepublic of The PhilippinesDienizs Labini TadenaОценок пока нет
- Case Scenario Rotation 2Документ3 страницыCase Scenario Rotation 2Dienizs Labini TadenaОценок пока нет
- Poor Water Supply and SanitationДокумент1 страницаPoor Water Supply and SanitationDienizs Labini TadenaОценок пока нет
- Labini, Dienizs Act.1 CHNДокумент4 страницыLabini, Dienizs Act.1 CHNDienizs Labini TadenaОценок пока нет
- Labini, Dienizs Bsn-3E: Incomplete Immunization Criteria Score Computation Answer JustificationДокумент6 страницLabini, Dienizs Bsn-3E: Incomplete Immunization Criteria Score Computation Answer JustificationDienizs Labini TadenaОценок пока нет
- Discharge Planning: MedicationsДокумент3 страницыDischarge Planning: MedicationsDienizs Labini TadenaОценок пока нет
- DS 4 To 6Документ8 страницDS 4 To 6Dienizs Labini TadenaОценок пока нет
- Kardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Документ11 страницKardex: GCS: 12-13/15 (M:5, V:4-5, E:3)Dienizs Labini TadenaОценок пока нет
- Drug Study: Labini, Dienizs Bsn-3EДокумент10 страницDrug Study: Labini, Dienizs Bsn-3EDienizs Labini TadenaОценок пока нет
- Nursing Care PlanДокумент4 страницыNursing Care PlanDienizs Labini Tadena100% (1)
- MVH Ward Case ScenarioДокумент3 страницыMVH Ward Case ScenarioDienizs Labini TadenaОценок пока нет
- Rhu Act. 2Документ2 страницыRhu Act. 2Dienizs Labini TadenaОценок пока нет
- Labini, Dienizs Bsn-3e Module 4 ActivtyДокумент3 страницыLabini, Dienizs Bsn-3e Module 4 ActivtyDienizs Labini TadenaОценок пока нет
- Dienizs Labini - NCM 117 Skills Activity #1Документ3 страницыDienizs Labini - NCM 117 Skills Activity #1Dienizs Labini TadenaОценок пока нет
- Dienizs Labini BSN-3E Brain Cancer Activities: B. Glioblastoma MultiformeДокумент11 страницDienizs Labini BSN-3E Brain Cancer Activities: B. Glioblastoma MultiformeDienizs Labini TadenaОценок пока нет
- Dienizs Labini BSN-3E Brain Cancer Activities: B. Glioblastoma MultiformeДокумент11 страницDienizs Labini BSN-3E Brain Cancer Activities: B. Glioblastoma MultiformeDienizs Labini TadenaОценок пока нет
- Do You Love MeДокумент3 страницыDo You Love MeDienizs Labini TadenaОценок пока нет
- Case Scenario For ADHDДокумент2 страницыCase Scenario For ADHDDienizs Labini TadenaОценок пока нет
- University of Northern PhilippinesДокумент15 страницUniversity of Northern PhilippinesDienizs Labini TadenaОценок пока нет
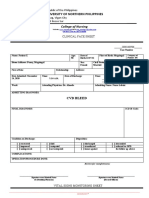
- Clinical Face Sheet: Diabetes Millitus T2Документ3 страницыClinical Face Sheet: Diabetes Millitus T2Dienizs Labini TadenaОценок пока нет
- D123 DRQДокумент1 страницаD123 DRQDienizs Labini TadenaОценок пока нет
- Stress Corrosion Cracking Behavior of X80 PipelineДокумент13 страницStress Corrosion Cracking Behavior of X80 Pipelineaashima sharmaОценок пока нет
- Educ 3 Prelim Act.1 AlidonДокумент2 страницыEduc 3 Prelim Act.1 AlidonJonash AlidonОценок пока нет
- Damodaram Sanjivayya National Law University VisakhapatnamДокумент6 страницDamodaram Sanjivayya National Law University VisakhapatnamSuvedhya ReddyОценок пока нет
- 059 Night of The Werewolf PDFДокумент172 страницы059 Night of The Werewolf PDFomar omar100% (1)
- Spitzer 1981Документ13 страницSpitzer 1981Chima2 SantosОценок пока нет
- HDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Документ40 страницHDFC Bank-Centurion Bank of Punjab: Presented By: Sachi Bani Perhar Mba-Ib 2010-2012Sumit MalikОценок пока нет
- German Lesson 1Документ7 страницGerman Lesson 1itsme_ayuuОценок пока нет
- Diva Arbitrage Fund PresentationДокумент65 страницDiva Arbitrage Fund Presentationchuff6675Оценок пока нет
- Sabbir 47MДокумент25 страницSabbir 47MMd.sabbir Hossen875Оценок пока нет
- Feng Shui GeneralДокумент36 страницFeng Shui GeneralPia SalvadorОценок пока нет
- Lecture 4 PDFДокумент9 страницLecture 4 PDFVarun SinghalОценок пока нет
- Delegated Legislation in India: Submitted ToДокумент15 страницDelegated Legislation in India: Submitted ToRuqaiyaОценок пока нет
- English HL P1 Nov 2019Документ12 страницEnglish HL P1 Nov 2019Khathutshelo KharivheОценок пока нет
- Chemistry InvestigatoryДокумент16 страницChemistry InvestigatoryVedant LadheОценок пока нет
- DH 0507Документ12 страницDH 0507The Delphos HeraldОценок пока нет
- Assignment File - Group PresentationДокумент13 страницAssignment File - Group PresentationSAI NARASIMHULUОценок пока нет
- Game Theory Presentation: Big BrotherДокумент11 страницGame Theory Presentation: Big BrotherNitinОценок пока нет
- PsychometricsДокумент4 страницыPsychometricsCor Villanueva33% (3)
- Fort - Fts - The Teacher and ¿Mommy Zarry AdaptaciónДокумент90 страницFort - Fts - The Teacher and ¿Mommy Zarry AdaptaciónEvelin PalenciaОценок пока нет
- Emma The Easter BunnyДокумент9 страницEmma The Easter BunnymagdaОценок пока нет
- Grope Assignment 1Документ5 страницGrope Assignment 1SELAM AОценок пока нет
- Ra 7877Документ16 страницRa 7877Anonymous FExJPnCОценок пока нет
- Consortium of National Law Universities: Provisional 3rd List - CLAT 2020 - PGДокумент3 страницыConsortium of National Law Universities: Provisional 3rd List - CLAT 2020 - PGSom Dutt VyasОценок пока нет
- Queen of Hearts Rules - FinalДокумент3 страницыQueen of Hearts Rules - FinalAudrey ErwinОценок пока нет
- Group 2 Lesson 2 DramaДокумент38 страницGroup 2 Lesson 2 DramaMar ClarkОценок пока нет
- MELC5 - First ObservationДокумент4 страницыMELC5 - First ObservationMayca Solomon GatdulaОценок пока нет
- Qafqaz UniversityДокумент3 страницыQafqaz UniversityQafqazlife QUОценок пока нет
- Landslide Hazard Manual: Trainer S HandbookДокумент32 страницыLandslide Hazard Manual: Trainer S HandbookMouhammed AbdallahОценок пока нет