Академический Документы
Профессиональный Документы
Культура Документы
Sonographic Appearance of The Epididymis in Pediatric Testicular Torsion
Загружено:
Lilik FitrianaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Sonographic Appearance of The Epididymis in Pediatric Testicular Torsion
Загружено:
Lilik FitrianaАвторское право:
Доступные форматы
Nussbaum Blask and Pe d i a t r i c I m a g i n g • O r i g i n a l R e s e a r c h
Rushton
Sonography of Testicular
Torsion in Pediatric Patients
A C E N T U
R Y O F Sonographic Appearance
of the Epididymis in
MEDICAL IMAGING
Pediatric Testicular Torsion
Anna R. Nussbaum Blask1 OBJECTIVE. The purpose of this study was to determine the frequency of an enlarged epi-
H. Gil Rushton2 didymis in pediatric patients with testicular torsion and to determine whether an altered epi-
didymis might be a helpful ancillary sonographic sign of testicular torsion.
Nussbaum Blask AR, Rushton HG MATERIALS AND METHODS. The sonograms of 50 pediatric patients (age range, ne-
onate–17 years) with testicular torsion were retrospectively reviewed for the size, appearance,
and blood flow of the epididymis. Medical records were reviewed for surgical and pathologic
findings and to determine whether testicular salvage had been possible.
American Journal of Roentgenology 2006.187:1627-1635.
RESULTS. The epididymis was enlarged (maximum dimension, 5.5 cm) in 47 of the 50 pa-
tients with acute or late phase torsion and after manual or spontaneous detorsion. The average dif-
ference in volume between the ipsilateral epididymis and the contralateral epididymis was 30
cm3, highly significant (p < 0.0001). The shape of the epididymis was altered in 92% of the cases
(globular, bilobular, or multilobular). Seventy-three percent showed increased echogenicity and
27% appeared isoechoic. Of those with active torsion, 93% of the epididymides were avascular;
2%, hypovascular; and 5%, hypervascular. After detorsion, 100% of the epididymides (10/10)
had blood flow. In patients with testicular loss due to infarction, pathology showed engorgement
and enlargement of the epididymis with hemorrhagic infarction. In one patient with a hypervas-
cular epididymis, surgery showed inflammation and erythema of the epididymis. Testicular loss
occurred in each type of epididymal flow pattern.
CONCLUSION. A markedly enlarged, echogenic, and avascular or hypovascular epididymis
is an ancillary sonographic sign in pediatric patients with testicular torsion. A hypervascular en-
larged epididymis infrequently occurs (5% of cases) and should not be mistaken for epididymitis.
In addition, the return of epididymal blood flow is an ancillary sign of successful testicular detorsion.
he acutely painful scrotum is a Radiologic imaging studies are performed
Keywords: color Doppler sonography, emergency
T common clinical occurrence in pe-
diatric patients and is treated as a
clinical emergency because of the
frequently in the acutely symptomatic patient
to avoid unnecessary surgical exploration.
Over the past several years, testicular color
radiology, epididymis, genitourinary tract imaging, possibility of testicular torsion. Testicular tor- Doppler sonography has become the initial im-
pediatric radiology, testicular torsion sion, which requires immediate surgical inter- aging study of choice because of its reported
vention or manual detorsion, must be distin- high sensitivity (78.6–89%) and specificity
DOI:10.2214/AJR.05.0461 guished from the nonsurgical conditions of (77–100%), coupled with its lack of radiation
Received April 14, 2005; accepted after revision
torsion of the appendix testis, epididymitis, and and rapidity of performance, replacing testicu-
November 10, 2005. epididymoorchitis. If clinical suspicion of tes- lar scintigraphy in most cases [3–6]. In our in-
ticular torsion is high, surgery is performed stitution, scintigraphy recently has served as an
1Department of Radiology, Children’s National Medical without additional imaging studies. However, ancillary second study reserved for cases that
Center, 111 Michigan Ave., NW, Washington, DC 20010. in most cases in the pediatric population, the were indeterminate for torsion on sonography
Address correspondence to A. R. Nussbaum Blask
(ablask@cnmc.org).
absolute differentiation of testicular torsion or showed decreased—but still present—flow
from the nonsurgical conditions based on only compared with the asymptomatic side.
2Department of Urology, Children’s National Medical physical signs and symptoms is difficult. In ad- The role of power Doppler sonography in
Center, Washington, DC 20010. dition, up to 70% of patients with an acute scro- the examination of the testes has been inves-
AJR 2006; 187:1627–1635
tum have nonsurgical conditions [1, 2]. The age tigated. Whether it provides an additional
of the patient is not helpful in the differential di- advantage over color Doppler sonography
0361–803X/06/1876–1627
agnosis because testicular torsion can occur in or might, in fact, increase the false-negative
© American Roentgen Ray Society patients of any age, including neonates [3, 4]. rate because of its increased sensitivity to
AJR:187, December 2006 1627
Nussbaum Blask and Rushton
decreased but still present arterial blood sides was determined. Sonographic studies had volume between the symptomatic side and the
flow is not yet known [7–11]. In several re- been performed using a standardized method to asymptomatic side was a value other than zero. The
ports, researchers have described false-neg- obtain longitudinal images parallel to the long portion of the epididymis that was enlarged was
ative color Doppler sonography findings in axis of the testis and transverse images perpen- documented as the head, head and body, body and
patients with testicular torsion despite its dicular to the long axis of the testis. The length tail, head and tail, or entire epididymis.
high reported sensitivities [12–15]. In addi- and depth of the entire visualized portion of the The gray-scale appearance of the epididymis
tion, seeing flow in the normal prepubertal epididymis were measured with calipers on a was evaluated. The shape was further analyzed to
testis may be difficult or impossible, making single longitudinal image in the plane of maxi- determine if it maintained a triangular configura-
the diagnosis of torsion on the contralateral mal enlargement. The transverse measurement tion or if it was distorted into a globular, bilobular,
symptomatic side more difficult [3, 4, 10, was obtained from a single transverse image in or multilobular shape. The echotexture of the epi-
11, 16]. In fact, some authors have sug- the plane of maximal enlargement. didymis on the side of testicular torsion was evalu-
gested that radionuclide scintigraphy re- On the symptomatic side, if only the head was en- ated and characterized as isoechoic or hyperechoic
main the imaging technique of choice in larged and the head was the only portion of the epi- and as homogeneous or heterogeneous in texture.
prepubertal children [10]. didymis visualized, it was used for the measure- The number of epididymides containing multiple
In our previous study of 46 pediatric pa- ments of epididymal size. A range of sizes was prominent cystic spaces was tabulated.
tients with an acute scrotum, we observed obtained for the symptomatic side and for the The vascularity of the ipsilateral epididymis
that a markedly enlarged avascular epidid- asymptomatic side. The epididymal size in the and the symptomatic testis was evaluated in all 50
ymis was present in children with torsion of asymptomatic hemiscrotum served as the control subjects with color flow Doppler imaging using
the testis; it was a source of confusion in sample in 41 of the 50 patients because there were no low-flow settings (HDL 3000 or 5000, ATL). Each
several cases because of its masslike ap- cases of bilateral synchronous testicular torsion. In sonographic examination was performed by one
pearance [3]. In this study, we retrospec- the remaining nine patients, the epididymis in the of three experienced pediatric sonographers. The
American Journal of Roentgenology 2006.187:1627-1635.
tively reviewed a series of pediatric patients asymptomatic hemiscrotum could not be measured epididymis was characterized as vascular if color
with the known diagnosis of testicular tor- retrospectively because images were insufficient or flow was seen, avascular if no color flow was de-
sion, including 13 patients with torsion from the epididymis was not seen or because of prior re- tected, and hypovascular if only minimal flow was
our previous study, to determine the fre- moval or atrophy of the contralateral testis and epi- seen. If the epididymal flow was greater than the
quency of this finding on testicular sonogra- didymis (two patients). In eight of these nine flow seen in the asymptomatic side, it was consid-
phy. Also, we wanted to determine whether patients, the epididymis in the symptomatic hemis- ered hypervascular. Pulsed Doppler tracings of the
an abnormal appearance of the epididymis crotum was matched to that of an age-matched con- epididymis were not obtained except in two pa-
might be a useful ancillary gray-scale and trol subject. In one of the nine patients, no quantita- tients. The Doppler findings in the symptomatic
color Doppler sign of testicular torsion. In tive analysis was performed because of the lack of testis were correlated with the findings in the ipsi-
addition, we wanted to see whether there hard-copy images. Evaluation was qualitative only lateral epididymis. The number of cases with
were any differences in the appearance of and based on the written report. manual detorsion or spontaneous detorsion was
the epididymis during acute phase torsion, The shape of each epididymis in the sympto- tabulated, and color Doppler examinations were
during late phase torsion, or after spontane- matic hemiscrotum was categorized as triangular, assessed both before and after detorsion, if avail-
ous or manual detorsion, and we wanted to round, or ovoid, and an estimated volume was ob- able, or only after detorsion if sonography had not
correlate the appearance of the epididymis tained using the formula for a pyramid, sphere, or been performed before detorsion.
with pathologic and surgical findings. Our prolate ellipsoid, respectively, in 49 of the 50 pa- The patients’ medical records were reviewed for
final aim was to determine whether the tients. The estimated volume of the normal epidid- surgical and pathologic findings and to determine
sonographic appearance of the epididymis ymis was calculated using the formula for a pyra- whether testicular salvage had been possible.
could be of any assistance in predicting tes- mid because review of the images in our series The diagnosis of testicular torsion was estab-
ticular salvage. indicated the shape of the normal epididymis was lished by surgery in 48 of the 50 patients; by late
best approximated by the triangular shape; none testicular atrophy in one patient; and by nuclear
Materials and Methods was globular, bilobular, or multilobular. scintigraphy performed 24 hours after the initial
All patients with a hospital discharge diagnosis Other authors have previously described the sonography in one patient, whose parents declined
of testicular torsion between January 1992 and shape of the normal epididymis as pyramidal [17, giving consent for surgical intervention. Scans
2002 were identified by performing a computerized 18]. Leung et al. [18] in their sonographic analysis were divided into those showing acute phase ver-
search of medical records. Patients who had under- of 40 asymptomatic men suggested that the epi- sus late phase torsion on the basis of the duration
gone color Doppler sonography of the testis and didymis has a triangle, crescent, or teardrop shape. of each patient’s symptoms, as described by Chen
epididymis as part of their diagnostic evaluation The volume of the epididymis on the symptomatic et al. [19]: Acute phase torsion was defined
formed the study group, which was composed of 50 side was compared with that of the contralateral as < 24 hours of pain and late phase torsion as ≥ 24
patients who ranged in age from neonate to 17 normal epididymis using a Student’s t test of the hours of pain.
years. Institutional review board consent for the difference between the means. Before statistical
study was obtained. Each sonogram was retrospec- tests were applied, the data were checked for nor- Results
tively reviewed by one of the authors for all of the mality and homogeneity of variance. Normalizing Of the 50 cases, 34% were acute phase tor-
parameters being evaluated. The reviewer was not variance-stabilizing data transformations were ap- sion and 66% were late phase torsion. Of the
blinded to clinical information. plied to satisfy the criteria for parametric analysis 17 patients with acute phase torsion, 10
The size of the epididymis on both the symp- before testing. Thereafter, a Student’s t test was ap- (59%) underwent manual detorsion and spon-
tomatic and the contralateral asymptomatic plied to test whether the difference in epididymal taneous detorsion occurred in one (6%).
1628 AJR:187, December 2006
Sonography of Testicular Torsion in Pediatric Patients
A B C
Fig. 1—Longitudinal images of epididymis in three patients with testicular torsion.
A, Sonogram of 16-year-old boy shows diffuse enlargement of head, body, and tail of epididymis (E) with bilobular shape. Note diffusely increased echogenicity.
American Journal of Roentgenology 2006.187:1627-1635.
B, Sonogram of 15-year-old boy shows heterogeneously increased echogenicity of epididymis (E) with globular shape.
C, Sonogram of 15-year-old boy shows head of epididymis (E) is enlarged, has isoechoic texture, and is slightly triangular. T = testis.
The average difference in volume between measurements. By contrast, epididymal en- tients with testicular torsion and hyperemic
the epididymis ipsilateral to testicular torsion largement was less pronounced in infants and epididymides, and most of the areas of sonolu-
and the contralateral epididymis was 30 cm3 in three boys with acute phase torsion. There cency were confirmed to be vascular channels
with a 95% CI of 18.8–47.9 cm3. This differ- were five patterns of enlargement of the epi- on the available color Doppler images. Be-
ence is highly statistically significant (p < didymis: head only (39.1%); head and body cause of the retrospective nature of our study,
0.0001). Enlargement was evident in 47 of the (13%); body and tail (4.3%); head and tail we could not determine if the other spaces
50 patients with acute phase or late phase tor- (2.2%); and diffuse (41.3%) involving the without color fill-in were vascular channels as
sion and after manual and spontaneous detor- head, body, and tail with increased tissue well or if they were areas of necrosis, hemor-
sion. The size of the epididymis was normal in cephalad, lateral, and caudad, respectively, to rhage, or thrombus within vessels. In the five
the remaining three patients, one with acute the testis (Figs. 1A–1C). other cases examined after manual or sponta-
phase torsion and two with late phase torsion. The shape of the epididymis was altered in neous detorsion, most, but again not all, of the
Of the latter two cases, one was in a neonate. acute phase or late phase torsion and after man- cystic and tubular spaces were confirmed to be
The epididymal size on the symptomatic ual or spontaneous detorsion. The epididymis vascular. In two of the latter patients examined
side ranged from maintained a triangular configuration in the re- both before and after detorsion, the cystic
maining 8% of cases. In the cases in which the spaces were seen to be primarily vascular
0.9 L × 0.5 D × 1 T cm normal triangular configuration was lost, the channels that filled in with color on Doppler
shape was globular (87%), bilobular (9%), or imaging after detorsion (Figs. 2A–2C).
to multilobular (4%) (Figs. 1A–1C). Before undergoing surgery because of tes-
The echotexture of the epididymis was al- ticular torsion, 39 patients received no treat-
5.5 L × 4.5 D × 4.5 T cm. tered in patients with acute phase or late phase ment, 10 patients underwent manual detorsion,
torsion and in those examined after manual or and spontaneous detorsion occurred in one pa-
The measurements on the asymptomatic side spontaneous detorsion. The most common tient. Of the 10 patients with manual detorsion,
ranged from pattern was markedly increased echogenicity seven were sonographically examined only af-
(36/49 [73%]), either heterogeneous with in- ter detorsion, one only before detorsion, and
0.3 L × 0.3 D × 0. 3 T cm creased foci (n = 29 cases) or homogeneous two were examined before and after detorsion.
with a diffuse increase in echogenicity (n = 7) The patient with spontaneous detorsion was
to (Figs. 1A–1C). Less commonly, the epidid- examined before and after detorsion. Epidid-
ymis was isoechoic (13/49 [27%]). ymal blood flow was evaluated.
0.9 L × 1.7 D × 1.1 T cm, Multiple cystic spaces were seen in 13 Of the 43 patients with active torsion at the
cases. Six of these cases showed no flow in the time of sonography, the epididymis was avas-
where L is length, D is depth, and T is trans- epididymis or cystic spaces because they were cular in 40 patients, hypovascular in one pa-
verse. In most cases, epididymal enlargement evaluated after testicular detorsion only. Two tient, and hypervascular in two patients
was visually obvious, even without obtaining of the cases with cystic spaces were in the pa- (Figs. 3A–3C). Of the 10 patients who were ex-
AJR:187, December 2006 1629
Nussbaum Blask and Rushton
A B
American Journal of Roentgenology 2006.187:1627-1635.
C D
Fig. 2—15-year-old boy with acute phase torsion that resolved after spontaneous detorsion.
A, Epididymis contains multiple cystic spaces and no flow on sonogram obtained during acute phase torsion.
B, Testis is avascular on sonogram obtained during acute phase torsion.
C, Sonogram obtained after spontaneous detorsion shows that epididymis has regained flow. Cystic spaces in epididymis are vascular channels.
D, Sonogram obtained after spontaneous detorsion shows that testis also has regained flow.
amined after detorsion, either manual or spon- ymis and acute phase torsion. In the two pa- showed congestion of the distal spermatic
taneous, all epididymides were vascular and six tients with unexpected epididymal hyperemia, cord. No other surgical or pathologic report in-
of the 10 were hypervascular. Of the three cases the testis was avascular in one and hypovascu- cluded an evaluation of the size of the sper-
examined before and after detorsion, the transi- lar in the second. In the former, scintigraphy matic cord. Information about the degree of
tion from no epididymal flow to epididymal also showed increased flow to the epididymis torsion of the spermatic cord was available in
flow was observed, similar to the observation of and a photon-deficient testis. 11 cases. Seven patients with late phase torsion
flow in the corresponding testis (Fig. 2). The Surgery and pathologic examination of 30 had from 540° to 720° or more of cord torsion
testis was also avascular in 34 of the 40 patients, patients with testicular loss and avascular epi- with both an avascular epididymis and avascu-
whereas it was hypovascular in the remaining didymis, as shown by the Doppler flow pattern, lar testis at sonography; testicular salvage was
six patients with an associated avascular epi- showed engorgement and enlargement of not possible. In one patient with acute phase
didymis. The testis also showed decreased flow the epididymis with hemorrhagic infarction torsion with a twist of 540–720° who had both
in the one patient with a hypovascular epidid- (Fig. 4). Two surgical cases after detorsion avascular epididymis and avascular testis, tes-
1630 AJR:187, December 2006
Sonography of Testicular Torsion in Pediatric Patients
American Journal of Roentgenology 2006.187:1627-1635.
A B
Fig. 3—Acute phase torsion with hyperemic epididymis.
A and B,15-year-old boy who underwent imaging after 20 hours of pain. Sonograms
show hyperemic epididymis (E) (A) and decreased flow in testis (T) (B). Testis was not
salvaged.
C, 5-year-old boy who underwent imaging after 12 hours of pain. Sonogram shows
hyperemic epididymis (E) with no flow in testis (T). Testis was salvaged.
ticular salvage was successful. In three pa- (Fig. 3C). In the second case of hyperemic epi- possible viability. These three testes subse-
tients, a 360° twist of the spermatic cord was didymis, surgery revealed hemorrhagic infarc- quently atrophied, and testicular salvage was
seen. One of the three patients had late phase tion of the epididymis, and testis salvage was not possible in any of the remaining cases of
torsion and an avascular epididymis and avas- not possible; that patient had a 20-hour history late phase torsion. Testicular loss occurred in
cular testis; testicular salvage was not possible. of pain and minimal flow in the testis at Dop- each type of epididymal flow pattern.
The second case was also in a patient with late pler imaging (Figs. 3A and 3B).
phase torsion with an avascular epididymis, The success rates of immediate testicular Discussion
minimal flow in the testis, and no testicular sal- salvage were assessed. Of the 17 patients with Color Doppler sonography is the imaging
vage. The third was a patient with acute phase acute phase torsion, two experienced testicular technique that is most frequently used to differ-
torsion and a hyperemic epididymis, avascular loss: One had a delay in treatment and the other entiate between surgical (testicular torsion)
testis, and testicular salvage. had testicular infarction with a history of 20 versus nonsurgical (epididymitis, torsion of the
Surgery revealed an inflamed erythematous hours of pain. Of the remaining 15 patients appendix testis, or epididymoorchitis) condi-
epididymis in one of the two patients with a hy- with acute torsion, the testis was salvaged. In tions in pediatric patients with an acutely pain-
peremic epididymis. The testis, which ap- 14 of 15, pain was present for 7 hours or less, ful scrotum. In some cases, differentiation be-
peared avascular at Doppler imaging, was is- and in the remaining patient, pain was present tween surgical versus nonsurgical disease may
chemic with 360° of torsion but was salvaged; for 12 hours. Three of the 33 testes in late be difficult because of low flow in the prepu-
the patient had a 12-hour history of pain phase torsion were not removed because of bertal testis and because arterial flow, albeit di-
AJR:187, December 2006 1631
Nussbaum Blask and Rushton
Fig. 4—Pathologic tional evidence of a successful manual detor-
specimen of infarcted sion. Epididymal hyperemia was the pre-
testis (T) and epididymis
(E) from 17-year-old boy dominant finding after testicular detorsion.
with late phase torsion Spontaneous detorsion should be a strong
shows diffusely consideration in a patient whose pain has
swollen epididymis.
C = spermatic cord.
abated suddenly or who reports episodes of
intermittent pain because epididymitis can
have the same sonographic appearance.
Marked enlargement of the epididymis
when the studies were initially performed was
a confusing finding in several of our cases, and
the possibility of an extratesticular mass or he-
matoma was considered. Enlargement of the
epididymis in patients with testicular torsion
has not been previously emphasized. However,
our observations confirmed findings described
previously by a few investigators. In one study,
epididymal enlargement with hemorrhage was
identified on gray-scale sonography in seven
adult patients with testicular torsion [25]. The
sonographic findings in seven pediatric pa-
American Journal of Roentgenology 2006.187:1627-1635.
tients with testicular torsion suggested a mis-
leading diagnosis of tumor or epididymitis that
resulted in delay of surgery and in testicular
loss [12–15]. Four of these cases evaluated on
color Doppler imaging showed testicular blood
minished in comparison with the asympto- creased echogenicity, was a consistent find- flow that was thought to be normal on the
matic side, is still detected on sonograms. In ing in almost all of the cases. This appearance symptomatic side. In a recent case of testicular
cases of partial torsion (180–360°), subtle was also present in the patients who were ex- torsion that we reviewed, not part of this series,
asymmetry in color blood flow may be over- amined after spontaneous or manual detor- sonography showed avascular epididymal en-
looked [20]. Bentley et al. [21] suggested that sion of the testis. Although the retrospective largement that was thought to be a tumor be-
a testicular color Doppler pattern symmetric nature of the study necessitated epididymal cause flow was present within the testis in the
with the asymptomatic testis initially may be measurements from 2D images, rather than symptomatic hemiscrotum. Diagnosis was de-
seen in patients with a thick spermatic cord and the more ideal 3D volumetric measurements, layed; a repeat study 9 hours after the first at
a long helix that is twisted. However, patients the same methodology was applied to evalu- our institution showed no testicular flow, and
with intermittent testicular torsion or spontane- ate both the symptomatic and the asympto- testicular loss occurred.
ous detorsion may undergo the study when matic hemiscrotum and the differences be- Retrospective review of the cases in our
they are pain free, so imaging may show a nor- tween the sides were highly significant. Also, study group suggests that the diagnosis would
mal testis or increased flow in the testis [2]. although the estimated measurements were have been altered or made earlier in two cases
Our sonographic study suggests that an an- necessary for statistical analysis, epididymal of testicular torsion, both of which resulted in
alysis of the appearance and vascularity of the enlargement—in conjunction with altered testicular loss. The two cases of hyperemic epi-
epididymis will add ancillary information shape and echotexture in the symptomatic didymides had potential for delay in diagnosis
that may assist in the diagnosis of testicular hemiscrotum—was visually obvious without because epididymitis with testicular ischemia
torsion in pediatric patients and that an aware- comparison of epididymal measurements and was the leading sonographic diagnosis, but tes-
ness of the associated finding of epididymal was marked in most of the cases. ticular torsion was thought to be the most likely
enlargement may avoid confusion with a In the absence of or before manipulation diagnosis after testicular scintigraphy. Al-
mass or erroneous diagnosis of epididymitis, of the testis or spontaneous detorsion, the though two additional patients were prospec-
even though the diagnosis of testicular torsion epididymis was avascular or hypovascular tively thought to have traumatic testicular con-
is still primarily based on the flow pattern in on color Doppler sonography in 95% of the tusion with epididymal hemorrhage, the
the testis. Enlargement of the spermatic cord cases of acute or late phase torsion. Surpris- outcome would not have been different be-
may also be a finding associated with testicu- ingly, the epididymis was hyperemic in 5% cause both underwent surgical exploration and
lar torsion [20–24]. of the cases of acute or late phase torsion had late phase testicular torsion.
Our study population consisted of pediatric (12% of the cases of acute torsion). Our As these cases point out, an enlarged avas-
patients with a proven diagnosis of either sonographic evaluations of patients exam- cular epididymis has the potential to change
acute or late phase testicular torsion over a ined both before and after detorsion indi- or expedite the diagnosis in cases of acute tor-
10-year period. This review showed that en- cated that return of blood flow to the epi- sion in which testicular flow is still present
largement of the epididymis in conjunction didymis can be observed in real time, similar but is decreased or is still visually normal, be-
with altered echotexture, most frequently in- to flow to the testis, and can be used as addi- cause these cases may be interpreted as a
1632 AJR:187, December 2006
Sonography of Testicular Torsion in Pediatric Patients
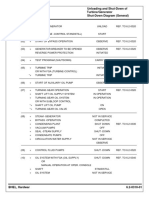
TABLE 1: Sonographic Patterns and Differential Diagnosis in Pediatric testicular flow findings, sonography depicted
Testicular Torsion the twist as a “snail shell–shaped mass.” Arce
Sonographic Pattern et al. [24] also described additional sono-
Diagnosis Epididymis Testis graphic findings related to specific color Dop-
pler assessment of the spermatic cord.
Testicular torsion Enlarged No change echotexture (A)
In our series, the surgical, pathologic, and
Hyperechoic Altered echotexture (L)
sonographic findings suggested that the extra-
Altered shape Avascular (A or L) testicular mass was primarily due to an en-
Congested or twisted spermatic Hypovascular (A or L) larged epididymis. The mass not only was su-
cord pratesticular in location, but also was frequently
Avascular (A or L) Hypervascular halo (L) paratesticular and infratesticular. Also, a sepa-
Hypovascular (A or L) Resistive index elevated rate epididymal structure was not seen, and
Hypervascular (A or L),
epididymal enlargement was present at patho-
uncommon logic examination. However, a portion or por-
Spontaneous detorsion (pain Enlarged Hypervascular or normal color tions of the tissue cephalad to the testis could
resolved or intermittent) flow possibly have been an engorged spermatic cord
Hypervascular or normal color
merged with the epididymal head, even though
flow this possibility could not be confirmed by ret-
Partial torsion or thick spermatic Enlarged Avascular, hypovascular, or
rospective review of the pathologic or surgical
cord normal color flow reports or by reanalysis of the sonograms. All
of the sonograms were of the scrotum only; the
American Journal of Roentgenology 2006.187:1627-1635.
Hypovascular or avascular
inguinal regions were not examined.
Epididymitis or torsion of Enlarged Hypervascular or normal color
appendix testis Hypervascular flow Other causes of supratesticular masses
need to be considered. Torsion of the testicu-
Extratesticular true solid mass Separate normal epididymis Normal color flow
lar appendages may be associated with a su-
Note—A = acute phase torsion, L = late phase torsion. pratesticular mass. However, the complete
constellation of findings are dissimilar to
those associated with testicular torsion; in-
TABLE 2: Suggested Management Protocol stead, a distinct 4- to 16-mm extratesticular
extraepididymal avascular mass is identified
Sonographic Diagnosis Management in most cases at the upper pole of the testis
Acute phase testicular torsion Emergent surgical exploration or may attempt manual (the epididymis testis or the appendix testis)
detorsion in conjunction with an enlarged epididymis
Late phase testicular torsion Nonemergent surgical exploration and testis with increased flow [27].
Spontaneous detorsion Nonemergent surgical exploration Isolated torsion of the epididymis has also
Partial testicular torsion Emergent surgical exploration been reported, although it seems to be a rare
Indeterminate testicular sonogram If < 12 h of symptoms, surgical exploration
occurrence. A 9-year-old boy with acute scro-
tal pain, associated with a long, tortuous epi-
If > 12 h of symptoms, scintigraphy or surgical exploration
didymis and long mesorchium, had this diag-
Epididymitis or torsion of appendix testis Nonsurgical management nosis established at surgery [28]. Clinically,
Extratesticular true solid mass Nonemergent surgical exploration tender swelling at the inferior pole of the tes-
tis was present and the testis was not tender to
palpation. A sonogram was not obtained. Two
other patients with an acute scrotum and with
false-negative. These cases are likely ones in in the affected testis. Other authors have sug- “dissociation of the testis and epididymis”
which there are fewer degrees of spermatic gested that analysis of Doppler waveform pat- have been reported, one in a 6 month old and
cord torsion (partial torsion) and the patient terns may also be helpful in cases of incom- one in an 18 year old [29]. The epididymis
presents earlier in the time course or has a plete or partial torsion [26]. was completely infarcted in the infant, requir-
thicker spermatic cord [21]. This sign theoret- A study by Baud et al. [22] of patients with ing epididymectomy.
ically has the potential to be of value when no testicular torsion showed features that paral- In most of our patients, the absence of color
testicular flow can be seen in the asympto- leled our results. They also described an extra- Doppler flow in the enlarged epididymis was
matic testis, although this did not occur in our testicular mass present in cases of testicular the key feature differentiating testicular torsion
series. Sanelli et al. [20] reported a case of torsion, but not detorsion. They indicated the from inflammatory epididymitis. However, the
partial torsion (360°) of the spermatic cord mass was due to the engorged, twisted sper- epididymis infrequently was hyperemic—
with visually normal color flow in the testis. matic cord. Kalfa et al. [23] suggested examin- even when testicular torsion was present. Spec-
They noted a masslike lobular appearance of ing the spermatic cord along its complete tral analysis was not performed in either of our
the spermatic cord with a coiled configuration length to detect a twist. They found that in all two patients with hyperemic epididymis, so
of the vessels and an elevated resistive index cases of torsion, even those with ambiguous whether the increase in flow was arterial or
AJR:187, December 2006 1633
Nussbaum Blask and Rushton
venous flow is not known. Recently, Arce et al. no anastomoses have been described. The the testis is additional evidence of successful
[24] described increased flow in the spermatic scrotal wall derives its blood supply from detorsion. After detorsion, either manual or
cord distal to the site of rotation and attributed branches of the pudendal artery, which do not spontaneous, the epididymis is frequently hy-
it to venous engorgement. That theory could pass through the spermatic cord and therefore pervascular. The appearance of the epidid-
also explain the hyperemic epididymis cases in maintain its supply during testicular torsion ymis is abnormal in both acute and late phase
our series. Those cases were a diagnostic di- [19, 32]. In late phase torsion, peritesticular in- torsion, and its appearance does help not pre-
lemma, and the possibility of epididymitis with flammatory changes occur and account for the dict testicular salvage.
secondary ischemia of the testis from venous halo of peripheral hypervascularity seen at
outflow compromise was entertained [30]. The both sonography and scintigraphy [32]. Alter- Acknowledgment
fact that the confirmed diagnosis was testicular natively, venous engorgement, due to obstruc- We thank Dr. Robert J. McCarter for per-
torsion in both of these patients suggests that tion of the distal spermatic cord as proposed by forming the statistical analysis for this project.
surgical exploration is warranted when an Arce et al. [24], is a possibility for the hyper-
avascular or hypovascular testis is seen in con- vascular epididymis.
junction with what appears to be a hyperemic Testicular viability depends on both the de- References
epididymis, distal spermatic cord, or both. gree and the duration of torsion. After 10 hours 1. Lewis AG, Bukowski TP, Jarvis PD, Wacksman J,
If a patient has undergone known manual of symptoms, most testes cannot be saved [33]. Sheldon CA. Evaluation of the acute scrotum in the
detorsion of the testis, the presence of flow Some testes that are saved at surgery atrophy emergency department. J Pediatr Surg 1995;
within an enlarged epididymis and in the tes- over time [33]. This occurred in three of our 30:277–282
tis suggests manipulation was successful, as patients. In our series, an enlarged avascular 2. Kass EJ, Stone KT, Cacciarelli AA, Mitchell B. Do
shown by the resumption of blood flow. In the epididymis was present in cases of both acute all children with an acute scrotum require explora-
patient whose acute symptoms have resolved, and late phase torsion; therefore, it was not a tion? J Urol 1993; 150:667–669
American Journal of Roentgenology 2006.187:1627-1635.
spontaneous detorsion should be considered helpful sign for predicting which testes could 3. Nussbaum Blask AR, Bulas D, Shalaby-Rana E,
when an enlarged hyperemic epididymis and be salvaged. Because we had only two cases of Rushton G, Shao C, Majd M. Color Doppler sonog-
testicular flow are present. hyperemic enlarged epididymides with testic- raphy and scintigraphy of the testis: a prospective,
An analysis of the vascular supply to the ular torsion, one with and one without testicu- comparative analysis in children with acute scrotal
scrotum and its contents explains these sono- lar salvage, whether this sign could be of any pain. Pediatr Emerg Care 2002; 18:67–71
graphic findings. The spermatic cord contains predictive value for testicular salvage is not 4. Paltiel HJ, Connolly LP, Atala A, Paltiel AD, Zura-
the testicular, deferential (artery of the ductus known. In all of our patients with manual or kowski D, Treves ST. Acute scrotal symptoms in
deferens), and cremasteric arteries. The testicu- spontaneous detorsion and reestablishment of boys with an indeterminate clinical presentation:
lar artery supplies the testis and epididymis, blood supply to the testis and epididymis, im- comparison of color Doppler sonography and scin-
and the artery of the ductus deferens and crem- mediate testicular salvage was achieved, even tigraphy. Radiology 1998; 207:223–231
asteric arteries supply the epididymis, vas def- in those cases in which testicular flow after 5. Baker LA, Sigman D, Mathews RI, Benson J,
erens, and peritesticular tissues [19, 30]. The detorsion was diminished in comparison with Docimo SG. An analysis of clinical outcomes using
testicular artery is a branch of the abdominal the asymptomatic side. color Doppler testicular ultrasound for testicular
aorta, and the artery of the ductus deferens is a The enlarged hyperechoic epididymis is a torsion. Pediatrics 2000; 105:604–607
branch of the superior vesical artery [31]. The consistent finding in pediatric testicular torsion 6. Patriquin HB, Yazbeck S, Trinh B, et al. Testicular
epididymis therefore has a dual blood supply that may assist in the diagnosis of torsion, es- torsion in infants and children: diagnosis with Dop-
via the testicular artery and via its anastomosis pecially in the prepubertal testis and in difficult pler sonography. Radiology 1993; 188:781–785
with the artery of the ductus deferens [31]. The cases in which arterial supply to the testis is 7. Zoller G, Kugler A, Ringert RH. “False positive”
venous drainage of the scrotal contents also still maintained but is decreased. Sonographic testicular perfusion in testicular torsion in power
passes through the spermatic cord. Because the findings and the associated management sug- Doppler ultrasound [in German]. Urologe A 2000;
vascular supply of the epididymis passes gestions are summarized in Tables 1 and 2. 39:251–253
through the spermatic cord, the twisting of the The primary diagnosis of testicular torsion is, 8. Coley BD, Frush DP, Babcock DS, et al. Acute tes-
spermatic cord, similar to twisting of the testis, nevertheless, still based on testicular flow pat- ticular torsion: comparison of unenhanced and con-
will compromise its blood supply and venous tern. The epididymis can resemble an extrates- trast-enhanced power Doppler US, color Doppler
drainage. This explains the presence of epi- ticular mass or hematoma. The avascular or US, and radionuclide imaging. Radiology 1996;
didymal enlargement and engorgement seen on hypovascular nature of the epididymis in most 199:441–446
sonographic examination and the ischemic cases of testicular torsion (95%) allows these 9. Bader TR, Kammerhuber F, Herneth AM. Testicu-
changes identified at pathologic examination. cases to be distinguished from epididymitis, lar blood flow in boys as assessed at color Doppler
Our patients with hypervascular epi- which can have a similar gray-scale appear- and power Doppler sonography. Radiology 1997;
didymides and lower cord complex associated ance. An enlarged hyperemic epididymis that 202:559–564
with testicular torsion are more difficult to ex- is not due to epididymitis may be seen infre- 10. Albrecht T, Lotzof K, Hussain HK, Shedden D,
plain unless the artery to the ductus deferens, quently in cases of torsion (5%). Cosgrove DO, de Bruyn R. Power Doppler US of
which travels centrally in the cord, cannot be The epididymis, in addition to the testis, the normal prepubertal testis: does it live up to its
compressed to the same degree as the testicular should be sonographically examined for re- promises? Radiology 1997; 203:227–231
artery. Theoretically, vessels that do not pass turn of color Doppler vascularity after spon- 11. Luker GD, Siegel MJ. Scrotal US in pediatric pa-
through the spermatic cord, such as the puden- taneous or manual detorsion; the presence of tients: comparison of power and standard color
dal vessels, may provide blood flow, although epididymal flow in conjunction with flow in Doppler US. Radiology 1996; 198:381–385
1634 AJR:187, December 2006
Sonography of Testicular Torsion in Pediatric Patients
12. Steinhardt GF, Boyarsky S, Mackey R. Testicular 20. Sanelli PC, Burke BJ, Lee L. Color and spectral 23:1077–1085
torsion: pitfalls of color Doppler sonography. J Urol Doppler sonography of partial torsion of the sper- 27. Baldisserotto M, de Souza JC, Pertence AP, Dora
1993; 150:461–462 matic cord. AJR 1999; 172:49–51 MD. Color Doppler sonography of normal and
13. Ingram S, Hollman AS, Azmy A. Testicular torsion: 21. Bentley DF, Ricchiuti DJ, Nasrallah PF, McMahon torsed testicular appendages in children. AJR 2005;
missed diagnosis on colour Doppler sonography. DR. Spermatic cord torsion with preserved testis 184:1287–1292
Pediatr Radiol 1993; 23:483–484 perfusion: initial anatomical observations. J Urol 28. Ravichandran S, Blades RA, Watson ME. Torsion
14. Pryor L, Watson LR, Day DL, et al. Scrotal ultra- 2004; 172(6 Pt 1):2373–2376 of the epididymis: a rare cause of acute scrotum. Int
sound for evaluation of subacute testicular torsion: 22. Baud C, Veyrac C, Couture A, Ferran JL. Spiral J Urol 2003; 10:556–557
sonographic findings and adverse clinical implica- twist of the spermatic cord: a reliable sign of testic- 29. Elert A, Hegele A, Olbert P, Heidenreich A, Hof-
tions. J Urol 1994; 151:693–697 ular torsion. Pediatr Radiol 1998; 28:950–954 mann R. Isolated epididymal torsion in dissociation
15. Allen TD, Elder JS. Shortcomings of color Doppler 23. Kalfa N, Veyrac C, Baud C, Couture A, Averous M, of testis-epididymis [in German]. Urologe A 2002;
sonography in the diagnosis of testicular torsion. J Galifer RB. Ultrasonography of the spermatic cord 41:364–365
Urol 1995; 154:1508–1510 in children with testicular torsion: impact on the sur- 30. Horstman WG, Middleton WD, Melson GL, Siegel
16. Ingram S, Hollman AS. Colour Doppler sonogra- gical strategy. J Urol 2004; 172(4 Pt 2):1692–1695 BA. Color Doppler US of the scrotum. Radio-
phy of the normal paediatric testis. Clin Radiol 24. Arce JD, Cortes M, Vargas JC. Sonographic diag- Graphics 1991; 11:941–957
1994; 49:266–267 nosis of acute spermatic cord torsion. Pediatr Ra- 31. Bartleby.com Web site. Gray’s anatomy of the hu-
17. Dogra VS, Gottlieb RH, Oka M, Rubens DJ. Sonog- diol 2002; 32:485–491 man body, 20th ed. Available at: http://bar-
raphy of the scrotum. Radiology 2003; 227:18–36 25. Vick CW, Bird K, Rosenfield AT, et al. Extratestic- tleby.com/107/. Accessed August 5, 2006
18. Leung ML, Gooding GA, Williams RD. High-res- ular hemorrhage associated with torsion of the sper- 32. Mendel JB, Taylor GA, Treves S, Cheng TH, Re-
olution sonography of scrotal contents in asympto- matic cord: sonographic demonstration. Radiology tik A, Bauer S. Testicular torsion in children:
matic subjects. AJR 1984; 143:161–164 1986; 158:401–404 scintigraphic assessment. Pediatr Radiol 1985;
American Journal of Roentgenology 2006.187:1627-1635.
19. Chen DC, Holder LE, Melloul M. Radionuclide 26. Dogra VS, Rubens DJ, Gottlieb RH, et al. Torsion 15:110–115
scrotal imaging: further experience with 210 pa- and beyond: new twists in spectral Doppler evalu- 33. Middleton WD. Scrotal sonography in 1991. Ultra-
tients. J Nucl Med 1983; 24:735–742 ation of the scrotum. J Ultrasound Med 2004; sound Q 1991; 9:61–87
AJR:187, December 2006 1635
Вам также может понравиться
- HIPOFISIS1Документ4 страницыHIPOFISIS1isela castroОценок пока нет
- Large Arachnoid Cyst: T. Mondal K. Jagdish Kumar R. Anand N.K. Dubey D. SharmaДокумент3 страницыLarge Arachnoid Cyst: T. Mondal K. Jagdish Kumar R. Anand N.K. Dubey D. SharmaJaya PrabhaОценок пока нет
- Eagle's Syndrome in An 11-Year-Old PatientДокумент4 страницыEagle's Syndrome in An 11-Year-Old Patientleeperlhan2000Оценок пока нет
- Lam 2001 Espacio Subar.Документ5 страницLam 2001 Espacio Subar.Jimmy Pino CoricazaОценок пока нет
- 10 1002@hed 20358Документ5 страниц10 1002@hed 20358Antania IsyatiraОценок пока нет
- Ultrasound Features of Spermatic Cord Hydrocele in ChildrenДокумент3 страницыUltrasound Features of Spermatic Cord Hydrocele in ChildrenEnricoFermihutagalungОценок пока нет
- 01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyДокумент3 страницы01 Testis Sparing Surgery For Epidermoid Cyst of Testis in A 3 Year Old BoyAli AhmadОценок пока нет
- Incidence of The Bell'Clapper Deformity in An Autopsy SeriesДокумент3 страницыIncidence of The Bell'Clapper Deformity in An Autopsy SeriesOttofianus Hewick KalangiОценок пока нет
- PD 879 PDFДокумент5 страницPD 879 PDFMargareta OktavianiОценок пока нет
- Ultrasonographic Appearance of Splenic Disease in 101 CatsДокумент5 страницUltrasonographic Appearance of Splenic Disease in 101 CatsdenisegmeloОценок пока нет
- Extraneural Perineurioma - Tnasicon PosterДокумент2 страницыExtraneural Perineurioma - Tnasicon PosterramkichessОценок пока нет
- Case Presentation: Baguio General Hospital and Medical Center Department of General SurgeryДокумент27 страницCase Presentation: Baguio General Hospital and Medical Center Department of General SurgeryJorge De VeraОценок пока нет
- Poster PPPДокумент1 страницаPoster PPPIndira Prawita MartAniОценок пока нет
- Original Report: Sonographic and MR Imaging Findings of Testicular Epidermoid CystsДокумент6 страницOriginal Report: Sonographic and MR Imaging Findings of Testicular Epidermoid CystsWildaHanimОценок пока нет
- Hernia Case ReportДокумент2 страницыHernia Case ReportSofie HanafiahОценок пока нет
- Cancer de Testiculo e Down 2Документ4 страницыCancer de Testiculo e Down 2paulinhamericoОценок пока нет
- Findings Osteogenesis Imperfecta Congenita: OcularДокумент5 страницFindings Osteogenesis Imperfecta Congenita: Ocularnugraha.nwcОценок пока нет
- Epithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewДокумент6 страницEpithelioid Hemangioendothelioma of The Infundibular-Hypothalamic Region: Case Report and Literature ReviewcarlosОценок пока нет
- Carrozzo 1997Документ6 страницCarrozzo 1997special spamailОценок пока нет
- Osteopathia Striata With Cranial SclerosisДокумент5 страницOsteopathia Striata With Cranial SclerosisritvikОценок пока нет
- Loshkajian 1997Документ6 страницLoshkajian 1997Ali AmokraneОценок пока нет
- Herpes Simplex PolyanglionitisДокумент5 страницHerpes Simplex PolyanglionitisReani ZulfaОценок пока нет
- Sonographic Whirlpool Sign in Ovarian Torsion: S. Boopathy Vijayaraghavan, MD, DMRDДокумент7 страницSonographic Whirlpool Sign in Ovarian Torsion: S. Boopathy Vijayaraghavan, MD, DMRDjohnalanОценок пока нет
- Hydranencephaly: Case NoteДокумент4 страницыHydranencephaly: Case NoteAndinaОценок пока нет
- Expanded Mo Bius Syndrome: David Peleg, MD, Gina M. Nelson, MD, PHD, Roger A. Williamson, MD, and John A. Widness, MDДокумент4 страницыExpanded Mo Bius Syndrome: David Peleg, MD, Gina M. Nelson, MD, PHD, Roger A. Williamson, MD, and John A. Widness, MDLUTHIEN orquideaОценок пока нет
- Ultrasonographic Diagnosis of Cystic Endometrial Hyperplasia-Pyometra in BitchesДокумент2 страницыUltrasonographic Diagnosis of Cystic Endometrial Hyperplasia-Pyometra in BitchesT Deky Rizqi AmandaОценок пока нет
- Pindborg 1967Документ6 страницPindborg 1967DIVYABOSEОценок пока нет
- Ultrasound Evaluation of Fetal Aneuploidy in The First and Second TrimestersДокумент28 страницUltrasound Evaluation of Fetal Aneuploidy in The First and Second TrimestersDwi CahyaОценок пока нет
- Intrathoracic Hibernoma: Brief Communication Communication AbrégéeДокумент2 страницыIntrathoracic Hibernoma: Brief Communication Communication AbrégéeM Ali AdrianОценок пока нет
- Giant Thoracolumbar Extradural Arachnoid Cyst A CaДокумент6 страницGiant Thoracolumbar Extradural Arachnoid Cyst A Cailmiah neurologiОценок пока нет
- The Myth of Autism: How a Misunderstood Epidemic Is Destroying Our ChildrenОт EverandThe Myth of Autism: How a Misunderstood Epidemic Is Destroying Our ChildrenРейтинг: 2.5 из 5 звезд2.5/5 (8)
- HSS Clinical Pronostic ConsiderationДокумент4 страницыHSS Clinical Pronostic ConsiderationReyes Ivan García CuevasОценок пока нет
- Cervical Cellulitis and Mediastinitis Caused by Odontogenic Infections. Report of Two Cases and Review of LiteratureДокумент6 страницCervical Cellulitis and Mediastinitis Caused by Odontogenic Infections. Report of Two Cases and Review of LiteratureJC QuezadaОценок пока нет
- Unusual Adult Porencephalic CystДокумент2 страницыUnusual Adult Porencephalic CystMifthahul IlmicaesarОценок пока нет
- Gigantismo PDFДокумент4 страницыGigantismo PDFtonyxОценок пока нет
- M: Elaine Crystine Vieira de Paiva Rua Pedro I, 1.033 Centro 60035-101 - Fortaleza - CE - BrazilДокумент2 страницыM: Elaine Crystine Vieira de Paiva Rua Pedro I, 1.033 Centro 60035-101 - Fortaleza - CE - Brazilpruebaprueba321765Оценок пока нет
- Thyroglossal Duct Cyst in Hyoid Bone: Unusual Location: The Journal of Laryngology & OtologyДокумент2 страницыThyroglossal Duct Cyst in Hyoid Bone: Unusual Location: The Journal of Laryngology & OtologyTasia RozakiahОценок пока нет
- Caudal Duplication SyndromeДокумент3 страницыCaudal Duplication Syndromekhumaira1982Оценок пока нет
- Loss of The N-Myc Oncogene in A Patient With A Small Interstitial Deletion of The Short Arm of ChromosomeДокумент5 страницLoss of The N-Myc Oncogene in A Patient With A Small Interstitial Deletion of The Short Arm of ChromosomeantonioopОценок пока нет
- AMM V 27.07Документ138 страницAMM V 27.07paul_calburean7899Оценок пока нет
- Hypospadias Tulip SignДокумент4 страницыHypospadias Tulip Signkomlanihou_890233161Оценок пока нет
- ParotitisДокумент6 страницParotitisredityoОценок пока нет
- Intracranial Aneurysms in Childhood: 27-Year Single-Institution ExperienceДокумент10 страницIntracranial Aneurysms in Childhood: 27-Year Single-Institution Experiencezrated786Оценок пока нет
- Solomon 1969Документ3 страницыSolomon 1969putu risyaОценок пока нет
- Potential Pitfalls in Cranial SonographyДокумент9 страницPotential Pitfalls in Cranial SonographyNupur SinghviОценок пока нет
- 01 Cir 57 2 278Документ8 страниц01 Cir 57 2 278KeneniОценок пока нет
- Hot Cross Bun SignДокумент4 страницыHot Cross Bun SignHenrique OliveiraОценок пока нет
- DC 2840060513Документ5 страницDC 2840060513Carmen Gomez MuñozОценок пока нет
- 121-Article Text-369-3-10-20160627Документ4 страницы121-Article Text-369-3-10-20160627rosangelaОценок пока нет
- Atypical Pituitary Adenoma: A Case ReportДокумент3 страницыAtypical Pituitary Adenoma: A Case ReportMuhammad Hafizh Islam SadidaОценок пока нет
- Factors Of: Myringoplasty in Children: Predictive OutcomeДокумент5 страницFactors Of: Myringoplasty in Children: Predictive OutcomeAcoet MiezarОценок пока нет
- Intracranial Hemangiomas Cause Childhood Temporal Lobe EpilepsyДокумент2 страницыIntracranial Hemangiomas Cause Childhood Temporal Lobe EpilepsyPrateek Kumar PandaОценок пока нет
- Dietrich Et Al-2002-Journal of Ultrasound in MedicineДокумент9 страницDietrich Et Al-2002-Journal of Ultrasound in MedicineErikaMRSiaОценок пока нет
- Kimura Disease, Pott'S Puffy - XXXXXДокумент28 страницKimura Disease, Pott'S Puffy - XXXXXHossam ThabetОценок пока нет
- 44-Day Old Infant with Ectopia CordisДокумент6 страниц44-Day Old Infant with Ectopia CordisarlitasofyanОценок пока нет
- A Giant Spinal Arterial Aneurysm in A Child Presenting As Quadriparesis (Case Reports, Vol. 2013, Issue Aug20 1) (2013)Документ4 страницыA Giant Spinal Arterial Aneurysm in A Child Presenting As Quadriparesis (Case Reports, Vol. 2013, Issue Aug20 1) (2013)negin.safari8227Оценок пока нет
- 10.1016@S00uyttgДокумент5 страниц10.1016@S00uyttgAstri AmaliaОценок пока нет
- X BibliДокумент7 страницX BibliBJ CarminatorОценок пока нет
- Hérnia talvez referenciaДокумент9 страницHérnia talvez referenciaPietra LocatelliОценок пока нет
- Tuberous Sclerosis Complex. Forty-Years of Follow-Up of A Patient AffectedДокумент3 страницыTuberous Sclerosis Complex. Forty-Years of Follow-Up of A Patient AffectedLilik FitrianaОценок пока нет
- BALLARD SCORe PDFДокумент1 страницаBALLARD SCORe PDFLilik FitrianaОценок пока нет
- From Eczema To Food To Inhalant AllergyДокумент56 страницFrom Eczema To Food To Inhalant AllergyLilik FitrianaОценок пока нет
- Buku SK Antropometri 2010Документ7 страницBuku SK Antropometri 2010Lilik FitrianaОценок пока нет
- BALLARD SCORe PDFДокумент1 страницаBALLARD SCORe PDFLilik FitrianaОценок пока нет
- Acceptable Noise Levels For Neonates in The Neonatal Intensive Care UnitДокумент59 страницAcceptable Noise Levels For Neonates in The Neonatal Intensive Care UnitLilik FitrianaОценок пока нет
- Staples - Pelengkap Poultry - Ayam Soup - SupДокумент2 страницыStaples - Pelengkap Poultry - Ayam Soup - SupLilik FitrianaОценок пока нет
- Kapadia 2017Документ7 страницKapadia 2017Anonymous dXdCD7D9UОценок пока нет
- Buku SK Antropometri 2010Документ7 страницBuku SK Antropometri 2010Lilik FitrianaОценок пока нет
- Simplified Field Tables: 1-Month Weight Increments (G) BOYSДокумент1 страницаSimplified Field Tables: 1-Month Weight Increments (G) BOYSLilik FitrianaОценок пока нет
- Buku SK Antropometri 2010Документ7 страницBuku SK Antropometri 2010Lilik FitrianaОценок пока нет
- New DokДокумент1 страницаNew DokLilik FitrianaОценок пока нет
- Grafik CDCДокумент10 страницGrafik CDCArief Budi LesmanaОценок пока нет
- Blood Pressure LevelsДокумент4 страницыBlood Pressure LevelsHeart of the Valley, Pediatric CardiologyОценок пока нет
- New Dok2Документ1 страницаNew Dok2Lilik FitrianaОценок пока нет
- See Catalog: Get A QuoteДокумент4 страницыSee Catalog: Get A QuoteahnafОценок пока нет
- Steam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)Документ1 страницаSteam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)parthibanemails5779Оценок пока нет
- Đánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardДокумент14 страницĐánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardNam NguyenHoangОценок пока нет
- Tribology - Lubricants and LubricationДокумент330 страницTribology - Lubricants and LubricationJosé Ramírez100% (2)
- Maize Package of Practices in BriefДокумент3 страницыMaize Package of Practices in Briefkomandla venkatkiran reddyОценок пока нет
- Well Serve CingДокумент140 страницWell Serve CingYounes MakОценок пока нет
- General Science EnvironmentДокумент28 страницGeneral Science EnvironmentHamza MujahidОценок пока нет
- Cryptography 01092014Документ19 страницCryptography 01092014Anshu MittalОценок пока нет
- Hufenus 2006 Geotextiles GeomembranesДокумент18 страницHufenus 2006 Geotextiles Geomembranesbkollarou9632Оценок пока нет
- Mahavir Glass Proforma InvoiceДокумент2 страницыMahavir Glass Proforma Invoicemahendra patelОценок пока нет
- Kinematics Problem SetДокумент1 страницаKinematics Problem SetMohammad JubranОценок пока нет
- Surface Roughness Measurement - MitutoyoДокумент2 страницыSurface Roughness Measurement - MitutoyoSelvaraj BalasundramОценок пока нет
- MEETING 7 OPINIONSДокумент2 страницыMEETING 7 OPINIONSLeonie Irina MutiaraОценок пока нет
- CSO Skull SeriesДокумент2 страницыCSO Skull SeriesWilchanОценок пока нет
- Medulla Oblongata Nucleus (Final)Документ7 страницMedulla Oblongata Nucleus (Final)Hassan.shehri100% (3)
- Return SectionДокумент1 страницаReturn SectionDaniel Pouso DiosОценок пока нет
- ASSIGNMENTДокумент10 страницASSIGNMENTKoleen Lopez ÜОценок пока нет
- FINS 2624 Quiz 2 Attempt 2 PDFДокумент3 страницыFINS 2624 Quiz 2 Attempt 2 PDFsagarox7Оценок пока нет
- Mercy PlansДокумент126 страницMercy Plansdharry8108Оценок пока нет
- Systematic Literature Review and Mapping of The Prediction of Pile CapacitiesДокумент12 страницSystematic Literature Review and Mapping of The Prediction of Pile CapacitiesCaio Augusto Lemke CostaОценок пока нет
- STPM Chemistry Topic 16 Haloalkanes Short Notes PDFДокумент2 страницыSTPM Chemistry Topic 16 Haloalkanes Short Notes PDFbendanОценок пока нет
- New Debashish & HemantДокумент31 страницаNew Debashish & HemantEshwar KothapalliОценок пока нет
- El DoradoДокумент12 страницEl Doradoandrewwilliampalileo@yahoocomОценок пока нет
- Pricelist Mobil Area Jabodetabek Semester 2 2022 TerbaruДокумент108 страницPricelist Mobil Area Jabodetabek Semester 2 2022 TerbarutonymuzioОценок пока нет
- TGN Level 1 No. 5 Derivation of Snow LoadДокумент4 страницыTGN Level 1 No. 5 Derivation of Snow LoadjeddijОценок пока нет
- User ManualДокумент14 страницUser ManualKhaled BellegdyОценок пока нет
- EBARA FS513CT-R0E pump manualДокумент6 страницEBARA FS513CT-R0E pump manualApriliyanto Rahadi PradanaОценок пока нет
- Wire Rope: - Bright - 6 X 19 - Fibre CoreДокумент8 страницWire Rope: - Bright - 6 X 19 - Fibre CoreQuynh NguyenОценок пока нет
- Masterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyДокумент35 страницMasterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyDemerson CamposОценок пока нет
- Swami Brahmananda - The Spiritual Son of Sri RamakrishnaДокумент7 страницSwami Brahmananda - The Spiritual Son of Sri RamakrishnaEstudante da Vedanta100% (2)