Академический Документы
Профессиональный Документы
Культура Документы
Case Study On Jaundice With Answers
Загружено:
abirami pИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Case Study On Jaundice With Answers
Загружено:
abirami pАвторское право:
Доступные форматы
CASE STUDY ON JAUNDICE
CHIEF COMPLAINT: Mrs. S – Her eyes are yellow for two days.
HISTORY OF PRESENT ILLNESS: Mrs. S is a 36 year old unemployed who presents
with yellow discoloration of her eyes which she noticed two days ago while washing her face.
At first she thought the colour was due to the lighting in her bathroom, but this morning,
when going outside of her house to retrieve the mail, she thought her hands "looked yellow."
Mrs. S further admits to feeling "sick and tired" for the past 2 -3 weeks. She has lost her
appetite and feels weak. During this time, she has been frequently nauseated and ate very
little food. Last night she developed a fever and "shook all over with a chill." This morning
she awoke after a restless night with pain and a sensation of fullness in the right upper
abdomen. She also vomited twice. The emesis was non -bloody. She has not had diarrhoea.
She has no back or shoulder pain. She thinks she lost 20 lbs during the last 3 months. She
denies having joint pain or skin rash.
Mrs. S is a chronic alcoholic who has been hospitalized on several occasions for alcohol
related problems, including a psychiatric admission. Since graduation from law school she
has had many alcohol related work problems and lost her position at a prestigious firm three
weeks ago. Since that time she has consumed approximately one fifth of vodka every day or
so.
She takes Tylenol for frequent headaches but takes no other medications. She smokes one
pack of cigarettes per day.
PHYSICAL EXAMINATION: The patient is alert but haggard looking. She is skinny and
shows prominent cheek bones. She appears much older than her stated age. Vital signs: Blood
pressure in right arm 104/60 mmHg, Heart Rate 110/minute and regular, Respiratory Rate
18/minute, Temperature 38.90 C.
HEENT: Bilateral, deep conjunctival icterus.
CHEST: Prominent ribs. Lungs are clear to percussion and auscultation.
CARDIOVASCULAR: Soft S1 and S2. No murmurs or extra cardiac sounds.
ABDOMEN: The abdomen is round and slightly tympanitic. The liver is palpable beneath the
costal margin (9 cm.) and tender. The liver span is 20 cm. There is no rebound tenderness,
shifting dullness or splenomegaly. Normal bowel sounds.
SKIN: Icteric; spider nevi noted on shoulders.
EXTREMITIES: Bilateral tremors of hands; bilateral palmar erythema.
LABORATORY DATA:
1. Complete blood cell count
o White blood cell count: 17,000 cells/mm3 with modest shift to left
o Hemoglobin 10.6 g/dL; Hematocrit 33%
o Platelets 120,000/mm3
o MCV 110/micro m3
2. Chemistries
o Aspartate arninotransferase (AST) 150 U/L
o Alanine aminotrasferase (ALT) 60 U/L
o Total Bilirubin 22 mg/dL
o Alkaline phosphatase 400 U/L
3. Prothrombin time 13.2 seconds
4. During, hospitalization WBC rose to 42,000/mm3; total bilirubin rose to 32 mg/dL
Questions
1. Identify salient historical information that may have a bearing to this patient's chief
complaint and indicate its significance.
Patient feels tired, nauseated, had fever with shaking chills
Pain in upper abdomen
Psychiatric admission
Chronic alcoholism
Sudden loss of weight in last 3 months
Tylenol use
2. What is your working diagnosis for her Jaundice based on the history and physical?
Alcoholic hepatitis
Viral hepatitis
Drug induced hepatitis
Cholelithiasis
Acute pancreatitis
3. Identify salient Laboratory findings that may have a bearing to this patient's chief
complaint and indicate its significance.
Yellow discolouration of eyes
Liver span 20 cm
Tender Liver
Skin icteric
Dishelved
Spider nevi
Fine tremors of hands
Palmar erythema
4. Cite the main clinical problem (not the diagnosis).
Jaundice
Other problems - Nausea, vomiting, fever, chills, abdominal pain
5. What patho-physiologic process does the laboratory data suggest.
The liver transferases are slightly elevated along with conjugated bilirubin.
This indicated mild hepatocellular injury with marked cholestasis.
The alkaline phosphatase level also gives evidence of the severe cholestasis
(with increase in conjugated bilirubin).
The AST level is greater than the ALT level which is classic for the disease
process that is present in this patient.
6. What is the diagnosis in this patient.
Alcoholic hepatitis.
7. Cite data from the history, physical exam and laboratory to support this diagnosis.
Recent and past history of alcoholism.
Nausea, vomiting.
Hepatomegaly
Spider nevi
AST greater than ALT. AST/ALT ratio > 1
Leukocytosis.
Worsening clinical status after hospitalization.
Palmar erythema
8. What drugs can be used to treat this patient.
A good diet can significantly improve the outcome of Alcoholic Liver
Disease.
Obesity seems to increases the risk of advanced liver disease in heavy
drinkers. Many people with this problem are severely malnourished, due to
loss of appetite and nausea.
In advanced liver disease (alcoholic hepatitis and cirrhosis) nutritional
supplements have been shown to significantly improve the liver function
tests.
A diet high in antioxidants such as vitamin E and selenium may help prevent
and treat ALD. These can be taken as supplements or by increasing dietary
fresh fruit and vegetables.
Abstinence: Even in advanced liver disease, it is still important and beneficial
to stop drinking.
Supervision may be required to safely reduce alcohol consumption. Rapid
reduction of alcohol consumption could lead to physical withdrawal
symptoms in up to 40% of people. Symptomatic treatment can include:
Corticosteroids for severe cases.
Anticytokines (infliximab and pentoxifylline).
Propylthiouracil to modify metabolism
Colchicine to inhibit hepatic fibrosis.
Antioxidants.
When all else fails and the liver is severely damaged, the only alternative is a
liver transplant.
9. What advice would you give the patient regarding the use of Tylenol.
Tylenol is Acetaminophen, which in therapeutic doses can be toxic in patients
with liver disease due to increased P-450 enzyme activity.
Tylenol should be used cautiously in these kind of patients and they should be
properly instructed about the potential toxicity of therapeutic doses of
Tylenol.
Вам также может понравиться
- Case AppendicitisДокумент30 страницCase AppendicitisSarahОценок пока нет
- Gastrointestinal Diseases and Disorders Sourcebook, Fifth EditionОт EverandGastrointestinal Diseases and Disorders Sourcebook, Fifth EditionОценок пока нет
- Caso Clínico de DislipidemiaДокумент3 страницыCaso Clínico de DislipidemiaCamiiliita Fernández La TorreОценок пока нет
- CASE STUDY FORMAT (Kidney Transplantation)Документ12 страницCASE STUDY FORMAT (Kidney Transplantation)ashnaОценок пока нет
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Oral Revalida Im Cases Dec. 12 and 13 2020Документ16 страницOral Revalida Im Cases Dec. 12 and 13 2020Bea Y. Bas-ongОценок пока нет
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Asthma2 Case StudyДокумент8 страницAsthma2 Case StudyGlenn Asuncion PagaduanОценок пока нет
- Management of CholeraДокумент69 страницManagement of CholeraNatalia LawrenceОценок пока нет
- Acute Diarrheal Disease Profound Secretory Diarrhoea Dehydration Hypovolemic Shock Native To The Ganges DeltaДокумент24 страницыAcute Diarrheal Disease Profound Secretory Diarrhoea Dehydration Hypovolemic Shock Native To The Ganges DeltacipacipaaОценок пока нет
- Diabetic NephropathyДокумент6 страницDiabetic NephropathyZulfadliZulfadliОценок пока нет
- New Fluid and Electrolytes Therapy Toyinoriginali2againДокумент55 страницNew Fluid and Electrolytes Therapy Toyinoriginali2againt.baby100% (1)
- 2011 Krok Bank SurgeryДокумент31 страница2011 Krok Bank SurgeryRahul PatilОценок пока нет
- Case PresentationДокумент20 страницCase PresentationMohamad HafyfyОценок пока нет
- Case Presentation - GASTROДокумент46 страницCase Presentation - GASTROalidudeОценок пока нет
- NCP Poststreptococcal GlomerulonephritisДокумент12 страницNCP Poststreptococcal GlomerulonephritisScarlet ScarletОценок пока нет
- Pud Case StudyДокумент8 страницPud Case Studyapi-346620455Оценок пока нет
- Pathological Changes of DM - 2023Документ53 страницыPathological Changes of DM - 2023Visura PrabodОценок пока нет
- Histopath Topic 3 PrelimДокумент103 страницыHistopath Topic 3 PrelimKatrina JornadalОценок пока нет
- DVT Case StudyДокумент2 страницыDVT Case StudyCrystal B Costa78Оценок пока нет
- CholeraДокумент5 страницCholerabishnu011978Оценок пока нет
- Health Assessment ON Gastro Intestinal System: Submitted To: Submitted byДокумент13 страницHealth Assessment ON Gastro Intestinal System: Submitted To: Submitted byAnanthibalaОценок пока нет
- Glomerulonephritis 10Документ5 страницGlomerulonephritis 10Eden Jay Calija AgoyОценок пока нет
- Final GIT Case PresentationДокумент53 страницыFinal GIT Case PresentationRovan100% (1)
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateДокумент21 страницаCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasОценок пока нет
- MR Elamin ShockДокумент70 страницMR Elamin ShockMohammed Abd AlgadirОценок пока нет
- PolycythemiaДокумент11 страницPolycythemiaBrian OchoaОценок пока нет
- IM Clinics History 2Документ4 страницыIM Clinics History 2LucyellowOttemoesoeОценок пока нет
- Case Study Anemia-1Документ6 страницCase Study Anemia-1Melsya H UtamiОценок пока нет
- Nephrotic SyndromeДокумент56 страницNephrotic SyndromeMurugesan100% (1)
- AMOEBIASISДокумент8 страницAMOEBIASISCheska ت HortelanoОценок пока нет
- Anemia IntroductionДокумент15 страницAnemia IntroductionNitesh Kotian100% (1)
- Chest Pain.Документ53 страницыChest Pain.Shimmering MoonОценок пока нет
- AmoebaДокумент24 страницыAmoebaJameh RomancapОценок пока нет
- Congestive Heart FailureДокумент14 страницCongestive Heart FailureBella Trix PagdangananОценок пока нет
- Case Presentation On Supraventricular TachycardiaДокумент64 страницыCase Presentation On Supraventricular TachycardiaHazel AsperaОценок пока нет
- Poisoning II FinalДокумент45 страницPoisoning II FinalBi PinОценок пока нет
- POLYCYTHEMIAДокумент9 страницPOLYCYTHEMIAJoeven HilarioОценок пока нет
- Tuberculosis: Dr.V. Gangadharan Professor & Hod Department of Respiratory Medicine Saveetha Medical College HospitalДокумент58 страницTuberculosis: Dr.V. Gangadharan Professor & Hod Department of Respiratory Medicine Saveetha Medical College HospitalJoanna RachelОценок пока нет
- Acute and Chronic Kidney DiseaseДокумент20 страницAcute and Chronic Kidney DiseaseCabdi WaliОценок пока нет
- BathingДокумент34 страницыBathingshannon c. lewisОценок пока нет
- GASTRITISДокумент5 страницGASTRITISmaria magdalena sagalaОценок пока нет
- BloodДокумент51 страницаBloodDrShahid Sahito100% (1)
- Poststreptococcal Glomerulonephritis - UpToDateДокумент21 страницаPoststreptococcal Glomerulonephritis - UpToDateHandre Putra100% (1)
- How Low Can You Endure The Pain, Mr. Bond?Документ70 страницHow Low Can You Endure The Pain, Mr. Bond?Venny VeronicaОценок пока нет
- Liver AbscessДокумент6 страницLiver AbscessKenneth SunicoОценок пока нет
- Anal FistulaДокумент26 страницAnal FistulaBeverly PagcaliwaganОценок пока нет
- Chronic GastritisДокумент7 страницChronic GastritisDivina AquinoОценок пока нет
- Fluid Electrolytes and Acid Base BalanceДокумент108 страницFluid Electrolytes and Acid Base BalancesayednourОценок пока нет
- Krok 2 Medicine 2014 1Документ545 страницKrok 2 Medicine 2014 1Amrut LovesmusicОценок пока нет
- Shock: Gastrointestinal Surgical Department of Affiliated Hospital of Jining Medical CollegeДокумент52 страницыShock: Gastrointestinal Surgical Department of Affiliated Hospital of Jining Medical Collegesanjivdas100% (1)
- Case StudiesДокумент59 страницCase Studiesstivana26100% (1)
- Hypertension Case StudyДокумент2 страницыHypertension Case Studyapi-344630051Оценок пока нет
- CHF, HPN and CAPДокумент17 страницCHF, HPN and CAPJhune VillegasОценок пока нет
- Case Scenario: Self-Risk AssessmentДокумент2 страницыCase Scenario: Self-Risk AssessmentAlyanna Alcazar CapateОценок пока нет
- Health AssessmentДокумент18 страницHealth AssessmentSavita Hanamsagar100% (1)
- Final Case StudyДокумент18 страницFinal Case Studyapi-487702467100% (1)
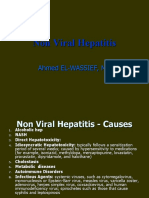
- Non Viral HepatitisДокумент40 страницNon Viral Hepatitisostaz2000100% (1)
- AtenololДокумент2 страницыAtenololabirami pОценок пока нет
- EpilepsyДокумент30 страницEpilepsyabirami pОценок пока нет
- Drugs, VD, Half Life and Loading DoseДокумент1 страницаDrugs, VD, Half Life and Loading Doseabirami pОценок пока нет
- CPPDM - Pediatrics - AbsorptionДокумент8 страницCPPDM - Pediatrics - Absorptionabirami pОценок пока нет
- CPPDM - Drug Distribution PDFДокумент17 страницCPPDM - Drug Distribution PDFabirami pОценок пока нет
- Systematic Approaches in Answering A Drug Information QueryДокумент4 страницыSystematic Approaches in Answering A Drug Information Queryabirami p100% (2)
- Case Study On Ulcerative ColitisДокумент19 страницCase Study On Ulcerative Colitisabirami pОценок пока нет
- PDP 406 Clinical Toxicology: Pharm.D Fourth YearДокумент18 страницPDP 406 Clinical Toxicology: Pharm.D Fourth Yearabirami pОценок пока нет
- Difference Between Active and Passive Transport DVДокумент3 страницыDifference Between Active and Passive Transport DVabirami pОценок пока нет
- Case Study On EpilepsyДокумент2 страницыCase Study On Epilepsyabirami pОценок пока нет
- Chapter 7basic Principles of Organic Chemistry Q1. Which Compounds Are The Simplest Organic Compounds?Документ14 страницChapter 7basic Principles of Organic Chemistry Q1. Which Compounds Are The Simplest Organic Compounds?api-233404189Оценок пока нет
- Bag Bath Return Demo For NursingДокумент4 страницыBag Bath Return Demo For Nursingjerica abesamisОценок пока нет
- Personal Development: Coping With Stress in Middle and Late AdolescenceДокумент22 страницыPersonal Development: Coping With Stress in Middle and Late AdolescenceIzanagi NomuraОценок пока нет
- Amazon Company HRM PolicyДокумент4 страницыAmazon Company HRM Policyadeeba ghani100% (2)
- Research Update: How To Conduct Fresh Cut Flower Vase Life ExperimentsДокумент2 страницыResearch Update: How To Conduct Fresh Cut Flower Vase Life ExperimentsAndrea NemenzoОценок пока нет
- Total Physical ResponseДокумент7 страницTotal Physical ResponseDesak RossyanaОценок пока нет
- Ôn luyện cấp tốc chứng chỉ Tiếng Anh B1 B2 LH:0907.286.606Документ10 страницÔn luyện cấp tốc chứng chỉ Tiếng Anh B1 B2 LH:0907.286.606Sĩ Phong100% (1)
- 2016, Yamasaki Et Al, Auditory Perceptual Evaluation of Normal and Dysphonic Voices Using The Voice Deviation Scale J VoiceДокумент5 страниц2016, Yamasaki Et Al, Auditory Perceptual Evaluation of Normal and Dysphonic Voices Using The Voice Deviation Scale J VoiceCarol PaesОценок пока нет
- One-Sample Tests of Hypothesis: Mcgraw-Hill/IrwinДокумент15 страницOne-Sample Tests of Hypothesis: Mcgraw-Hill/IrwinImam AwaluddinОценок пока нет
- Specific Heat CapacityДокумент25 страницSpecific Heat CapacityZae ZayОценок пока нет
- CHAPTER 2 Mini Ice Plant Training Module FinalДокумент6 страницCHAPTER 2 Mini Ice Plant Training Module FinalLeyzer MalumayОценок пока нет
- Scheme For The Separation of The Cations PDFДокумент1 страницаScheme For The Separation of The Cations PDFDriss DamaОценок пока нет
- Energy Pyramid: 0.1% Third-Level Consumers 1% Second-Level ConsumersДокумент2 страницыEnergy Pyramid: 0.1% Third-Level Consumers 1% Second-Level ConsumersAisha BasirОценок пока нет
- McAteer Report Says Upper Big Branch Mine Explosion PreventableДокумент126 страницMcAteer Report Says Upper Big Branch Mine Explosion PreventableThe West Virginia Examiner/WV WatchdogОценок пока нет
- ME 525: Combustion Lecture 9: Mass and Species ConservationДокумент15 страницME 525: Combustion Lecture 9: Mass and Species Conservationhiral gohilОценок пока нет
- V Unit - Wireless Network SecurityДокумент22 страницыV Unit - Wireless Network SecurityBRINDHA C it2018Оценок пока нет
- Andmeleht Alpha Continuity Plus 6kW 10kWДокумент2 страницыAndmeleht Alpha Continuity Plus 6kW 10kWAleksandar NikolicОценок пока нет
- Use of Alternative Energy Sources For The Initiation and Execution of Chemical Reactions and ProcessesДокумент21 страницаUse of Alternative Energy Sources For The Initiation and Execution of Chemical Reactions and ProcessesNstm3Оценок пока нет
- Flame RetardantsДокумент4 страницыFlame Retardants1985krОценок пока нет
- Distillation Column 2Документ6 страницDistillation Column 2vaqifОценок пока нет
- The Best Broccoli Cheese Soup (Better-Than-Panera Copycat) - Averie CooksДокумент1 страницаThe Best Broccoli Cheese Soup (Better-Than-Panera Copycat) - Averie CooksEmily WillisОценок пока нет
- PR-1159 - Commissioning and Start-UpДокумент117 страницPR-1159 - Commissioning and Start-UpIngemar David Quintero Simonpietri100% (1)
- Soekamto 2021Документ4 страницыSoekamto 2021maria astridОценок пока нет
- 5 Major Swimming Strokes: Grade 12 PE and HealthДокумент11 страниц5 Major Swimming Strokes: Grade 12 PE and HealthJack Daniel CandelarioОценок пока нет
- Dissertation On Bronchial AsthmaДокумент7 страницDissertation On Bronchial AsthmaInstantPaperWriterSpringfield100% (1)
- Kunci Jawaban Lks Ekcellent Bahasa Inggris Kelas XiiДокумент16 страницKunci Jawaban Lks Ekcellent Bahasa Inggris Kelas XiiMuhammad QurabieyОценок пока нет
- 1 MCM PDFДокумент88 страниц1 MCM PDFKingsely.shuОценок пока нет
- Become Healthy or Extinct by Darryl DsouzaДокумент281 страницаBecome Healthy or Extinct by Darryl DsouzaDip Dip DipОценок пока нет
- Marketing and Sales Promotion of PepsiДокумент58 страницMarketing and Sales Promotion of PepsiPayal Ambhore100% (1)
- TOEIC 5 - Mini Test - NO KEYДокумент4 страницыTOEIC 5 - Mini Test - NO KEYHồng Điệp LươngОценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (35)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeОт EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeРейтинг: 4.5 из 5 звезд4.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (5)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionОт EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionОценок пока нет
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsОт EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsРейтинг: 4.5 из 5 звезд4.5/5 (39)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (44)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (46)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (254)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОт EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsОценок пока нет
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!От EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Рейтинг: 5 из 5 звезд5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedРейтинг: 4 из 5 звезд4/5 (61)