Академический Документы
Профессиональный Документы
Культура Документы
Chapter 21 Cognitive Disorders: Zarrah Rose S. Alianza Bsn3A
Загружено:
JenIsananИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Chapter 21 Cognitive Disorders: Zarrah Rose S. Alianza Bsn3A
Загружено:
JenIsananАвторское право:
Доступные форматы
ZARRAH ROSE S.
ALIANZA BSN3A ^_^ ◊ Assessment
• History
CHAPTER 21 COGNITIVE DISORDERS ♣ obtain information related to medical illness, alcohol or other drugs
Cognition=brain’s ability to process, retain & use information
Cognitive abilities=include reasoning, judgment, perception, attention ♣ information about drugs should include prescribed medications, alcohol
Cognitive disorder=is a disruption or impairment in higher level functions of the brain • General Appearance & Motor Behavior
DELIRIUM ♣ have disturbances of psychomotor behavior
A syndrome that involves a disturbance of consciousness accompanied by a change in cognition ♣ may be restless, hyperactive, frequently pricking at bedclothes or making sudden, uncoordinated
Develops over a short period of time attempts to get out of bed
Clients have difficulty paying attention, are easily distracted and disoriented and may have sensory disturbances such ♣ may have slowed motor behavior, appearing sluggish and lethargic with little movement
as illusions, misinterpretations or hallucinations
DSM-IV-TR Diagnostic criteria: Symptoms of Delirium
♣ speech becomes less coherent and more difficult to understand
difficulty with attention ♣ may perseverate on a single topic or detail
easily distractible
disoriented
♣ clients may call out or scream especially at night
sensory disturbances • Mood & affect
can have sleep-awake disturbances ♣ often have rapid, unpredictable mood shifts
changes in psychomotor activity
anxiety, fear, irritability, euphoria or apathy ♣ wide range of emotional responses is possible such as anxiety, fear, irritability
♥ Etiology ♣ fearful and feel threatened, they may become combative to defend themselves
MOST COMMON CAUSES OF DELIRIUM • Thought process & content
physiologic or metabolic hypoxemia, electrolyte disturbances, renal or hepatic failure, hypoglycemia,
hyperglycemia, dehydration, sleep deprivation, thyroid or glucocorticoid
♣ thought processes often are disorganized and make no sense
disturbances, thiamine or Vitamin B12 deficiency, vitamin C, niacin, or protein ♣ thought may also be fragmented (disjointed and incomplete)
deficiency, cardiovascular shock, brain tumor, head injury and exposure to ♣ may exhibit delusions, believing their altered sensory perceptions are real
gasoline, paint solvent, insecticides and related substances
infection systemic: meningitis, encephalitis, HIV, syphilis • Sensorium & intellectual process
drug-related intoxication: anticholinergics, lithium, alcohol, sedatives and hypnotics; ♣ initial sign is an altered level of consciousness that is seldom stable
withdrawal: alcohol, sedatives, hypnotics; reactions to anesthesia, prescription
medication or illicit drugs
♣ oriented to person but frequently disoriented to time and place
◊ Risk factors include: ♣ demonstrate decreased awareness of the environment
♣ noises, people or sensory misperceptions easily distract them
• increased severity of physical illness
• older age ♣ can’t focus, sustain or shift attention effectively and there is impaired recent and immediate
memory
• baseline cognitive impairment
♥ Treatment and Prognosis ♣ frequently experience misinterpretations, illusions and hallucinations
Identify and treat any causal or contributing medical conditions • Judgment & Insight
◊ Psychopharmacology ♣ judgment is impaired
• Sedation=to prevent inadvertent self-injury ♣ can’t perceive potentially harmful situations or act in their own best interests
• Antipsychotic medications such as haloperidol (Haldol)=used to decrease agitation ♣ insight depends on the severity of the delirium
• sedatives and benzodiazepines are avoided because they may worsen delirium ♣ with mild delirium may recognize that they are confused
♥ Other Medical Treatment ♣ with severe delirium may have no insight to the situation
◊ adequate nutritious foods and fluid intake • Self-concept
◊ intravenous fluids or even total parenteral nutrition if client’s physical condition has deteriorated and cannot ♣ often are frightened or feel threatened
eat nor drink ♣ may feel helpless or powerless to do anything to change it
◊ physical restraints so that needed medical treatments can continue ♣ may feel guilt, shame, and humiliation
DRUGS CAUSING DELIRIUM
anticonvulsants, anticholinergics, antihistamines, antihypertensives, antineoplastics, antipsychotics, aspirin,
• Roles & Relationships
barbiturates, benzodiazepines, cardiac glycosides, cimetidine (tagamet), hypoglycemic agents, insulin, narcotics, ♣ unlikely to fulfill their roles
propranolol (inderal), reserpine, steroids, thiazide diuretics ♣ have no longstanding problems with roles or relationships
♥ APPLICATION OF THE NURSING PROCESS
• Physiologic consideration Echolalia=echoing what is heard
♣ disturbed sleep-wake cycles, falling asleep, daytime sleepiness, nighttime agitation or even a Palilalia=repeating words or sounds over and over
DSM-IV-TR Diagnostic criteria: Symptoms of Dementia
complete reversal of the usual daytime waking/nighttime sleeping pattern
Loss of memory
Data Analysis Deterioration of language function
◊ Nursing diagnosis commonly used when working with clients who somatize: Loss of ability to think abstractly and to plan, initiate,
• risk for injury sequence, monitor or stop complex behaviors
• acute confusion ♥ Onset and Clinical Course
• disturbed sensory perception ◊ Dementia is described in stages as follows:
• disturbed thought process • Mild= forgetfulness is the hallmark of mild dementia
• disturbed sleep pattern • Moderate=Confusion is apparent along with progressive memory loss.
♥ Outcome Identification • Severe= personality and emotional changes occur. Forget names of his/ her spouse and children and
◊ Treatment outcomes may include the following: require assistance in ADL
• client will be free of injury ♥ Etiology
• client will demonstrate increased orientation and reality contact ◊ Most common types of dementia:
• client will maintain an adequate balance of activity and rest • Alzheimer’s disease
♥ Intervention ♣ progressive brain disorder that has a gradual onset but causes an increasing decline in functioning,
NURSING INTERVENTIONS FOR DELIRIUM including loss of speech, loss of motor function and profound personality and behavioral changes.
1. promoting client’s safety
teach client to request assistance for activities ♣ Abnormal APOE gene and linkages to chromosomes 21, 14 and 19
provide close supervision to ensure safety during these activities ♣ enlargement of third & fourth ventricles
promptly respond to client’s call for assistance
2. managing client’s confusion • Vascular dementia
speak to client in calm manner ♣ symptoms similar to Alzheimer’s but onset is abrupt, following by rapid changes in functioning;
allow time for client to comprehend and respond plateau, or leveling off period
allow client to make decisions • Pick’s Disease
provide orienting verbal cues when talking to client
use supportive touch if appropriate ♣ degenerative brain disease that affects the frontal and temporal lobes
3. controlling environment to reduce sensory overload ♣ Early signs include personality changes, loss of social skills and inhibitions, emotional blunting,
keep environmental noise to minimum and language abnormalities
monitor client’s response to visitors
validate client’s anxiety and fears but do not reinforce misperceptions ♣ 50 – 60 years old (onset) and 2-5 years (death)
4. promoting sleep and proper nutrition • Creutzfeldt- Jakob disease
monitor sleep and elimination pattern ♣ a CNS disorder that develops in 40- 60 years old.
monitor food and fluid intake
provide periodic assistance to bathroom if client does not make requests • HIV infection
discourage daytime napping to help sleep at night ♣ invasion of nervous tissue by HIV
encourage some exercises during day
• Parkinson’s disease
CLIENT / FAMILY EDUCATION FOR DELIRIUM ♣ slowly progressive neurologic condition characterized by tremor, rigidity, bradykinesia, and
Monitor chronic health conditions postural instability.
Visit physician regularly
Avoid alcohol & recreational drugs
♣ Results from loss of neurons of basal ganglia.
• Huntington’s disease
DEMENTIA
A mental disorder that involves multiple cognitive deficits, primarily memory impairment and at least one of the ♣ inherited, dominant gene disease that involves cerebral atrophy, demyelination, and enlargement of
following cognitive disturbances: brain ventricles.
1. Aphasia= deterioration of language function ♣ There are choreiform movements that are continuous during waking hours and involve facial
2. Apraxia=impaired ability to execute motor functions contortions, twisting, turning and tongue movements.
3. Agnosia=inability to recognize or name objects • Head trauma
4. Disturbance in executive functioning=ability to think abstractly and to plan, initiate, sequence, monitor and stop ♥ Treatment and Prognosis
complex behavior Acetylcholine, dopamine, norepinephrine are decreased in dementia
Memory impairment=early sign of dementia ◊ Treatments include acetylcholine precursors, cholinergic agonists and cholinesterase inhibitors
◊ Cholinesterase inhibitors= have modest therapeutic effects and temporarily slow progress of dementia. ♣ Work performance suffers; deteriorating roles
• Tacrine ( Cognex)- elevates liver enzymes ♣ Inability to participate in meaningful conversations or social events
• Donepezil ( Aricept) ♣ Family members assume caregiver roles; role reversal
• Rivastigmine (Exelon) • Physiologic consideration
• Galantamine (Reminyl) ♣ Disturbed sleep- wake cycles
◊ Antipsychotics: Haloperidol ( Haldol), Olanzapine (Zyprexa), Risperidone (Risperdal) ♣ Ignore hunger or thirst
◊ Lithium carbonate, Carbamazepine ( Tegretol) and Valproic acid ( Depakote)= stabilize affective lability ♣ Bladder and bowel incontinence
and diminish aggressive outbursts ♣ Neglect bathing and grooming
◊ Benzodiazepines=may cause delirium and worsen compromised cognitive abilities ◊ Data Analysis
DRUGS USED TO TREAT DEMENTIA • Nursing diagnosis commonly used:
Name Nursing considerations ♣ risk for injury
Tacrine ( Cognex Monitor liver enzymes ♣ disturbed sleep pattern
Donepezil ( Aricept) Monitor for nausea, diarrhea & insomnia
Rivastigmine (Exelon) Monitor for nausea, vomiting, abdominal pain ♣ impaired memory
Galantamine (Reminyl) Monitor for nausea, vomiting, loss of appetite ◊ Outcome Identification
• Treatment outcomes may include the following:
♥ APPLICATION OF THE NURSING PROCESS • client will be free of injury
◊ Assessment • client will function as independently as possible
Mental status examination=provide information about the client’s cognitive abilities • client will maintain an adequate balance of activity and rest
• History ◊ Intervention
• General Appearance & Motor Behavior NURSING INTERVENTIONS FOR DEMENTIA
♣ Slurred speech; total loss of language function 1. Promoting client’s safety
Offer unobtrusive assistance
♣ Apraxia=loss of ability to perform familiar tasks such as combing hair Identify environmental triggers
♣ Cannot imitate tasks others demonstrate; gait disturbance; neglect hygiene 2. Promoting adequate sleep, proper nutrition and hygiene and activity
• Mood & affect Prepare desirable foods
Monitor bowel elimination
♣ Anxiety and fear; not express feelings; labile mood; emotional outbursts; anger and hostility; Remind client to urinate; provide pads or diapers
catastrophic emotional reactions; withdrawal, lethargic, apathetic, little attention Encourage mild physical activity such as walking
• Thought process & content 3. Structuring environment and routine
Encourage to follow regular routine and habits
♣ Loss ability to plan, sequence, monitor, initiate or stop complex behavior Monitor amount of environmental stimulation and adjust when needed.
♣ Delusions of persecutions 4. Providing emotional support
• Sensorium & intellectual process Be kind, respectful, calm
Use supportive touch when appropriate
♣ Confabulation= make up answers to fill in memory gaps 5. Promoting interaction and involvement
♣ Agnosia=another hallmark of dementia Plan activities geared to client’s interests and abilities
Reminisce the past
♣ Lose of visual spatial relationships
Remain alert to nonverbal behavior
♣ Impaired attention span, confused; disoriented • Promoting interaction and involvement
♣ Hallucinations ( usually visual hallucinations)
♣ Reminiscence therapy=thinking about or relating personally significant past experiences
• Judgment & Insight
♣ Poor judgment; insight is limited
♣ Distraction=shifting the client’s attention and energy to a more neutral topic
♣ Underestimate risks and unrealistically appraise their abilities ♣ Time away=leaving clients for a short period and then returning to them to re-engage in interaction
• Self-concept ♣ Going along=providing emotional reassurance without correcting their misperception or delusion.
CAREGIVER EDUCATION FOR DEMENTIA
♣ Angry or frustrated with themselves Encourage clients to follow usual routing
♣ Sadness at their bodies for getting old Encourage independence as much as possible
♣ Loss of self- awareness Encourage clients to participate in activities of interest
♣ Fail to recognize own reflections ♥ Mental Health Promotion
• Roles & Relationships ◊ People with elevated levels of homocysteine are at increased risk for dementia .
◊ Folate, vit. B12 , and betaine reduce plasma homocysteine levels ◊ Drink 6-8 glasses of water daily
◊ Participate in brain- stimulating activities such as reading
♥ Related Disorders
◊ Amnestic disorders=disturbance in memory that results directly from physiologic effects of a general
medical condition or alcohol and drugs
◊ Korsakoff’s syndrome=alcohol- induced amnestic disorder results from a chronic thiamine or vitamin B
deficiency
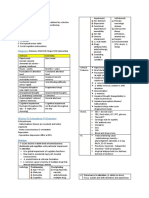
COMPARISON OF DELIRIUM AND DEMENTIA
Indicator Delirium Dementia
Onset Rapid Gradual
Duration Brief Progressive deterioration
Level of consciousness Impaired, fluctuates Not affected
Memory Short-term memory impaired Short-then-long term memory impaired
Speech Slurred, rumbling Normal in early stage, aphasia later
Thought process Temporarily disorganized Impaired thinking
Perception Visual/tactile hallucinations, delusions Absent; can have paranoia, hallucinations
Mood Anxious, fearful, weeping Depressed & anxious in early stage
SEE PAGE 479 TO 480 & 492 TO 493 FOR NURSING CARE PLAN…
ALZHEIMER’S DISEASE
progressive brain disorder that has a gradual onset but causes an increasing decline in functioning, including loss
of speech, loss of motor function and profound personality and behavioral changes.
Abnormal APOE gene and linkages to chromosomes 21, 14 and 19
enlargement of third & fourth ventricle
Acetyl butiryl=increase as Alzheimer’s progress & found in neuritic plates
♥ Etiology
◊ Genetics
◊ Environment
♥ Onset and Clinical Course
◊ Stages
• Stage I=no cognitive impairment
• Stage II=mild cognitive decline
• Stage III
• Stage IV=mild or early stage; supervision is required
• Stage V=moderately severe; there is total dependence of client
♥ Treatment
◊ Cholinesterase inhibitors
• Dopenezil
• Galantamin
◊ Adverse effects
• Insomia, fatigue, rashes, nausea & vomiting
♥ Diet
◊ Antioxidant foods
• Fruit & vegetables like squash & bell peppers
◊ Avoid refined foods like white bread
Вам также может понравиться
- Cognitive DisordersДокумент4 страницыCognitive DisordersJustine BayabosОценок пока нет
- Y.Dana Presentation Cognitive DisordersДокумент19 страницY.Dana Presentation Cognitive DisordersDana YrzabekОценок пока нет
- Cognitive DisordersДокумент105 страницCognitive DisordersNicole Keesha MataОценок пока нет
- 117 Delirium and DementiaДокумент6 страниц117 Delirium and DementiaLa VicОценок пока нет
- Cognitive DisordersДокумент4 страницыCognitive DisordersCamille Joy BaliliОценок пока нет
- Care of Older Adult in Chronic ConfusionДокумент7 страницCare of Older Adult in Chronic ConfusionClaire MachicaОценок пока нет
- CBD Team e PsychiatryДокумент44 страницыCBD Team e PsychiatrydindanovitamОценок пока нет
- Dementia KimsДокумент60 страницDementia KimssridharmotteОценок пока нет
- 9.mental Disorders Due To A General Medical Condition and Organic Brain Damages.Документ50 страниц9.mental Disorders Due To A General Medical Condition and Organic Brain Damages.chairihidayatzaОценок пока нет
- 9.mental Disorders Due To A General Medical Condition and Organic Brain Damages PDFДокумент50 страниц9.mental Disorders Due To A General Medical Condition and Organic Brain Damages PDFchairihidayatzaОценок пока нет
- Sensory Deficits in The Elderly: Their Implications and ManagementДокумент41 страницаSensory Deficits in The Elderly: Their Implications and ManagementNikky Rossel FloresОценок пока нет
- Neurocognitive DisordersДокумент13 страницNeurocognitive Disorders18105101Оценок пока нет
- HO DissociativeДокумент2 страницыHO Dissociative20210023707Оценок пока нет
- Delirum Vs DementiaДокумент1 страницаDelirum Vs Dementiaapi-577583685Оценок пока нет
- Care of Older Adults (Finals)Документ14 страницCare of Older Adults (Finals)Ax’l SisterОценок пока нет
- Evangelista Chapter 7Документ8 страницEvangelista Chapter 7Ellyza EvangelistaОценок пока нет
- Delirium and DementiaДокумент12 страницDelirium and DementiaSОценок пока нет
- Anxiety DisorderДокумент23 страницыAnxiety DisorderOliver Miguel ChavezОценок пока нет
- Cognitive DisordersДокумент56 страницCognitive DisordersROMULO NU�EZ JR.Оценок пока нет
- Cognitive DisordersДокумент5 страницCognitive DisordersCamille Joy BaliliОценок пока нет
- NeurocognitiveДокумент59 страницNeurocognitivesoran muzeyinОценок пока нет
- Dissociative DisordersДокумент13 страницDissociative DisordersMwangi LizОценок пока нет
- Bipolar Disorder: Presented By: Group 2Документ19 страницBipolar Disorder: Presented By: Group 2Pao DelossantosОценок пока нет
- Venous Disorders of The Lower LimbДокумент14 страницVenous Disorders of The Lower LimbFaris Mohd NasirОценок пока нет
- Dissociative DisordersДокумент59 страницDissociative Disordersdrsheetal.psyОценок пока нет
- Chapter 13 - Neurocognitive DisordersДокумент6 страницChapter 13 - Neurocognitive DisordersNOR AFISYA BINTI ZAKARIAОценок пока нет
- Delirium in Elderly G4 21 - 22Документ39 страницDelirium in Elderly G4 21 - 22Hannah HalimОценок пока нет
- Dementia in ServiceДокумент17 страницDementia in ServicerianabeggОценок пока нет
- CRIT4 ConfusionДокумент21 страницаCRIT4 ConfusionKen KerrОценок пока нет
- Children With Autism Have Difficulty Understanding Unspoken Social CuesДокумент4 страницыChildren With Autism Have Difficulty Understanding Unspoken Social CuesAlishbah Khan NiaziiОценок пока нет
- Understanding DementiaaДокумент6 страницUnderstanding DementiaaKent JawayОценок пока нет
- Midterm-Psych-Week 12Документ8 страницMidterm-Psych-Week 12Ladybelle GototosОценок пока нет
- Mental DisordersДокумент19 страницMental DisordersMia Charisse FigueroaОценок пока нет
- Understanding The DSM VДокумент6 страницUnderstanding The DSM VStratiatella Faith AnthonyОценок пока нет
- Videbeck Cognitive NotesДокумент6 страницVidebeck Cognitive Notesrachelle0308Оценок пока нет
- Cognitive DisordersДокумент3 страницыCognitive DisordersCailah Sofia SelausoОценок пока нет
- The Three D's and Suicide in ElderlyДокумент29 страницThe Three D's and Suicide in ElderlyIqra RazzaqОценок пока нет
- Psychiatric EmergencyДокумент26 страницPsychiatric EmergencyHoi Chung LamОценок пока нет
- Chapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersДокумент3 страницыChapter 6 Somatic-Symptom-and-Related-Disorders-and-Dissociative-DisordersAnnie SumacotОценок пока нет
- AbPsych Notes - 1Документ10 страницAbPsych Notes - 1It'sCurryAndRice PlusWaterОценок пока нет
- NSTP - LarsДокумент81 страницаNSTP - LarsShayne PenalosaОценок пока нет
- Dissociative DisordersДокумент17 страницDissociative DisordersHassanОценок пока нет
- Human Behavior 1Документ55 страницHuman Behavior 1Noe HernandezОценок пока нет
- Cognitive DisorderДокумент72 страницыCognitive DisorderJamal P. AlawiyaОценок пока нет
- NEUROMUSCULARДокумент5 страницNEUROMUSCULARIsabel HigginsОценок пока нет
- Delirium & Assessing A Confused Patient: CriteriaДокумент9 страницDelirium & Assessing A Confused Patient: CriteriaDeedz01Оценок пока нет
- Chapter 15 Neurocognitive DisordersДокумент49 страницChapter 15 Neurocognitive DisordersApril Rose ElopreОценок пока нет
- Summarized Abnormal PsychologyДокумент13 страницSummarized Abnormal PsychologyMa.Janine Torres100% (1)
- Physical Education and Sports For CWSN (Children With Special Needs - (Divyanag)Документ19 страницPhysical Education and Sports For CWSN (Children With Special Needs - (Divyanag)Saroj PandeyОценок пока нет
- Universidad de Sta. Isabel: Vincentian Learning ModuleДокумент17 страницUniversidad de Sta. Isabel: Vincentian Learning ModuleYancy TingsonОценок пока нет
- Mental State ExaminationДокумент2 страницыMental State ExaminationThomasОценок пока нет
- Neurocognitive DisorderДокумент3 страницыNeurocognitive DisorderIT’S ME HAYLAОценок пока нет
- Dissociative Disorders Involve Problems With MemoryДокумент13 страницDissociative Disorders Involve Problems With MemoryShivansh RattanОценок пока нет
- Organic Mental DisordersДокумент6 страницOrganic Mental Disorderspriya maneshОценок пока нет
- CH 15 NEUROCOGNITIVE DISORDERSДокумент6 страницCH 15 NEUROCOGNITIVE DISORDERSAgnes ValdezОценок пока нет
- Dissociative DisordersДокумент27 страницDissociative DisordersShielamae PalalayОценок пока нет
- Dissociative Disorders-1Документ20 страницDissociative Disorders-1Aishwarya RoyОценок пока нет
- Chapter 24 Cognitive DisordersДокумент7 страницChapter 24 Cognitive DisordersCatia Fernandes100% (1)
- MDD and Eating Disorders FinalДокумент31 страницаMDD and Eating Disorders FinalLanceRedanicanОценок пока нет
- IAP Guideline For Vitamin D Supplementation PDFДокумент7 страницIAP Guideline For Vitamin D Supplementation PDFBandya SahooОценок пока нет
- Analytical Method ValidationДокумент86 страницAnalytical Method ValidationRambabu komati - QA100% (12)
- Ch2 IS3 TestДокумент12 страницCh2 IS3 TestJohn Smith100% (1)
- HLH BloodДокумент13 страницHLH BloodOmyRojasОценок пока нет
- List of Minimum Requirements For Hospital ForДокумент3 страницыList of Minimum Requirements For Hospital ForTayyab Tahir Minhas67% (3)
- Discourse Community EthnographyДокумент6 страницDiscourse Community Ethnographyapi-294418947Оценок пока нет
- MPT NeurologyДокумент22 страницыMPT NeurologyDevasyaОценок пока нет
- Extravasations DiagramДокумент1 страницаExtravasations DiagramJohnОценок пока нет
- MiracleДокумент11 страницMiracleJonatasCostaОценок пока нет
- CPCSEAДокумент27 страницCPCSEAobaidОценок пока нет
- Using Statistical Process Control Chart Techniques To Ensure Quality of Care in Pharmacy Department of A HospitalДокумент5 страницUsing Statistical Process Control Chart Techniques To Ensure Quality of Care in Pharmacy Department of A HospitalRezha AmaliaОценок пока нет
- Manual de Fixação Interna Rigida Craniofacial PDFДокумент14 страницManual de Fixação Interna Rigida Craniofacial PDFFernandaJolyMacedoОценок пока нет
- Agenda: Scientific Program 6 Saudi Hematology Research DayДокумент7 страницAgenda: Scientific Program 6 Saudi Hematology Research Daynemoo80 nemoo90Оценок пока нет
- MSCT SCAN ABDOMEN PDSRI DR IraДокумент78 страницMSCT SCAN ABDOMEN PDSRI DR IraGuntur SaputraОценок пока нет
- Effectofcorestabilityexerciseonposturalstabilityinchildrenwith DownsyndromeДокумент11 страницEffectofcorestabilityexerciseonposturalstabilityinchildrenwith Downsyndrome8 nocturnalОценок пока нет
- Ich GCP: HistoryДокумент57 страницIch GCP: HistoryChandrashekhar Singh100% (1)
- Dewi Maya S (P160 Hanifah Ambang F (P16025) Nurul Yuniartanti (P160 Roni Setyawan (P16043) Wildan Aulia A (P160Документ5 страницDewi Maya S (P160 Hanifah Ambang F (P16025) Nurul Yuniartanti (P160 Roni Setyawan (P16043) Wildan Aulia A (P160hanifa ambОценок пока нет
- Autism EnglishДокумент129 страницAutism EnglishRaí Caetano de JesusОценок пока нет
- Pentalaksanaan Penyalahgunaan Benzodiazepin, Miras, Methanol-3Документ130 страницPentalaksanaan Penyalahgunaan Benzodiazepin, Miras, Methanol-3Nia PermanaОценок пока нет
- STG Final Dec 2020Документ1 215 страницSTG Final Dec 2020Bereket GGОценок пока нет
- VP Business Operations in Central South NJ Resume Diane MalkinДокумент1 страницаVP Business Operations in Central South NJ Resume Diane MalkinDianeMalkinОценок пока нет
- Jurnal Pijat 1Документ4 страницыJurnal Pijat 1Herli SahputriОценок пока нет
- Breastfeeding Policies: Martin Marasigan District HospitalДокумент2 страницыBreastfeeding Policies: Martin Marasigan District Hospitalgrace dimangondayaoОценок пока нет
- Psychiatric Nursing Questions With RationaleДокумент8 страницPsychiatric Nursing Questions With RationaleLes ChiensОценок пока нет
- Drug Design Using BioinformaticsДокумент13 страницDrug Design Using BioinformaticsAniqah Zulfa100% (3)
- ABASII Sample Report F Hr2Документ60 страницABASII Sample Report F Hr2kalla55100% (1)
- Manufacturing Drills 2Документ9 страницManufacturing Drills 2Thirdy AcostaОценок пока нет
- Histology For RetardsДокумент57 страницHistology For RetardsDavid Degaetano100% (1)
- Enbs PanelДокумент1 страницаEnbs PanelMa'am KinОценок пока нет