Академический Документы
Профессиональный Документы
Культура Документы
MedSurg Questions
Загружено:
sasha051969Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
MedSurg Questions
Загружено:
sasha051969Авторское право:
Доступные форматы
normal EF: What is the normal PSA level?
>75% <4 ng/ml - age - infections - smoking - aspiration - chronic lung probs - immobility - mechanical ventilators - immunocompromised status - alcoholic cirrhosis - viral hepatitis - ascending flaccid motor paralysis - loss of sensory function - loss of DTR's - weakness before paralysis - loss of respiratory muscle control - avoid alcohol - monitor renal fxn - monitor liver fxn - oral contraception less effective - Bicarbonate - Epinephrine - Vasopressin - Lidocaine - Amiodarone - Magnesium sulfate - Procainamide - blood - semen/vaginal fluids - saliva - NOT by tears, urine, or sweat - confusion and stupor - cyanosis - bradypnea - bradycardia - hypotension - cardiac dysrhythmias - confusion - hypoxia - cool, clammy skin - sweating - anxiety, irritability, blurred vision - weakness, seizures - cortisol - aldosterone - Na+ - blood sugar
PNA: what are the 8 risk factors?
Name 2 conditions that can result in portal HTN?
What characterizies guillan barre?
4 things to watch out for when on oral antidiabetic meds:
Meds for VF or pulseless VT: (BEV LAMP)
modes of Hep B transmission:
What are the late S&S of hypoxemia?
Two common manifestations of pna in older adults?
S&S of hypoglycemia:
What 4 things are decreased in the blood for Addison's?
What 3 things are elevated in the blood for Cushings?
- cortisol - blood sugar - Na+ - decreased breath sounds - dull percussion sounds - decreased chest wall expansion - pain - demeclocycline (Declomycin)- lithium - depressed respirations - stupor (cerebral hypoxia) - hypothermia - bradycardia (low CO) - hypotension - Dyspnea, air hunger - tachycardia - tachypnea - Anxiety - decreased O2 sat - hypotension - early activation of EMS - early CPR/defib - early ACLS - edema - bronchoconstriction - secretions - emphysema - chronic bronchitis - fatigue - weight loss - abd distension, bloating - constipation, diarrhea, change in bowel habits - anemia
Assessment findings of pleural effusion?
What 2 meds can be given to treat SIADH by blocking renal response to ADH? 5 S&S of myxedema coma:
6 common S&S of PE:
Chain of survival involves...?
3 characteristics of Asthma: COPD encompasses 2 diseases:
S&S of colon cancer:
Pts with strong hix of colorectal cancer should reduce intake - fats of what 2 things? - meats What is extracorporeal shock wave lithotripsy and to include - for renal calculi in discharge teaching? - instruct to intake lots of fluids to flush out fragments - high BP (often >200) - intense headaches - profuse sweating - feeling of doom - goosebumps - nasal stuffiness - facial erythema - high K+, P, and Na+ - low Ca++ - fluid volume overload - increased BUN & Cr - metabolic acidosis (high H+) - UO under 400ml/day (oliguria) - anemia
What are S&S of autonomic dysreflexia?
Common findings for acute renal failure:
Blood test results for malignant hyperthermia would reveal:
- high K+, P, CK, & myoglobin - low Ca++ - acidosis - hot dry skin - no sweating - N/V, abd pain - Kussmaul's breathing (fruity breath) - hyperthermia - HTN - tachydysrhythmia - delirium - vomiting - abd pain - hypotension - reflex bradycardia - diaphoresis - faintness - hypovolemia (low volume) - hypoxia (low oxygen) - hydrogen ion excess (acidosis) - hyper-/hypo-kalemia (high/low K+) - hypothermia (low body temp) - taking drugs (overdose) - tamponade (cardiac) - tension pneumothorax (oneway valve in pleural cavity) - thrombosis (pulmonary) - thrombosis (coronary) - hypoxemia that does not improve with oxygen therapy - extensive pulmonary edema (whiteout on x-ray) - IBD: age 15-40, younger - Diverticulitis: usually over 50 - immunosuppression - fluid retention - hypgerglycemia - hypokalemia - poor wound healing - initially may be up to 500ml/day, then gradually decrease overtime. - NEVER >1L/day - K+ - Ca++ - ACTH - K+ - Ca++ - BUN - Creatinine
S&S of hyperglycemia:
6 S&S of thyroid storm:
Manifestations of shock?
10 most common causes of Pulseless Electrical Activity (PEA):
Hallmarks of ARDS: Difference in age of pts with IBD versus pts with diverticulitis:
5 side effects of corticosteroids:
T-tube drainage range: What 3 things are decreased in the blood for Cushings? What 4 things are elevated in the blood for Addison's? What are some systemic effects of
guillain barre? Differentiate diet prescriptions for IBD versus diverticulitis.
- loss of sphincter control - bladder/bowel retention - sweating, sputum - SIADH - low fiber diet for IBD - high fiber diet for diverticulitis - lumbar puncture - PFT - EMG - CBC/ABG's - meats - NSAIDs - Vit. C - muscular rigidity - tachycardia - hyperthermia - hypercapnia - red-brown urine - nonproductive cough - substernal pain - nasal stuffiness - N/V - fatigue - HA - sore throat - hypoventilation - NSAIDS (e.g. ibuprofen) - Aminogylcosides (e.g. gentamycin) - ACE inhibitors (e.g. catopril) - orange/reddish pee, sweat, tears - watch for hepatotoxicity - persistent cough w/ or w/o rust/blood-colored sputum - dyspnea - unilateral wheezing - chest wall pain - persistent hypoxemia despite administration of 100% O2 - decreased pulmonary compliance - dyspnea - bilateral pulmonary edema that is noncardiac - dense pulmonary infiltrates ("ground glass" on CxR) - postinfection polyneuritis - autoimmune disorder that attacks mainly Schwann cells and destroys their myelin sheaths. - postprandial hypoglycemia - malnutrition - F&E imbalance
How do you diagnose guillain barre?
What 3 things should pts avoid in their diet 48 hours prior to FOB testing?
What are 5 S&S of malignant hyperthermia?
What are the S&S of oxygen toxicity?
Name 3 nephrotoxic drug groups: Rifampin (RIF): 2 things about RIF?
What kind of respiratory S&S do you expect to find in lung cancer pts?
5 ARDS indicators:
What's Guillain Barre?
What are 3 complications of dumping syndrome to watch out for?
Encourage foods rich in what 3 things for TB pts:? 3 characteristics of nephrotic syndrome: High pressure alarm sounds on the vent indicates?
- protein - iron - Vit C - proteinuria - HYPOalbuminemia - edema - pt biting the tube - need for suctioning - kinks in tubing - ptosis (drooping eyelid) - dysphagia - neck weakness, head bob - muscle weakness - even respiratory failure/arrest - RA is bilaterally symmetrical, OA is not - RA pain after rest, OA pain with movement - RA is autoimmune, OA is not - rapid ID of S&S - initiate circ and resp support - activate EMS - use emergency equipment - stabilize pt - Dx and Tx - restrict caffeine, vanilla, licorice for 2-3 days in advance - hold aspirin and antiHTN meds - maintain moderate acitivity - rheumatoid arthritis - SLE - ulcerative colitis - pernicious anemia - shock - peritonitis - perforated bladder - simple pneumothorax: usually no shift - tension and hemothorax: shift to contralateral (unaffected) side - spasmodic colicky pain instead of constant diffuse pain - visible peristaltic waves
Manifestations of myasthenia gravis:
Name 3 differences between osteoarthritis and rheumatoid arthritis.
Goals for management of cardiac arrest include...?
What are nursing implications for VMA testing?
Name 4 disorders associated with Myasthenia Gravis:
Monitor for which 3 complications following a paracentesis?
Tracheal shift in 3 kinds of pneumothorax: 3 characteristics that set small bowel obstruction apart from large bowel obstruction:
rather than significant abd distention - sudden projectile vomiting that relieves pain rather than infrequent vomiting The thyroid gland produces which 3 hormones? - T3 - T4 - calcitonin - tachypnea - tachycardia - restlessness - pallor - HTN - resp distress - THINS the skin - DOES NOT darken skin. - to decrease serum ammonia levels - you monitor for LOC - tobacco - alcohol - harmful chemicals (chronic exposure) - tubing disconnections - air leaks around cuff - uremia (ARF) - hepatic failure - PKU (phenylketouria) due to lack of a hepatic enzyme (genetic) - nutritional deficits - drug/alcohol w/drawal - drug/alcohol use - Usually limited to 1L in a short period of time. (Slow drainage can be used to take out >1L of fluid over several hours.) - VMA - Clonidine - phentolamine (Regitine) - watch for hepatitis - watch for neurotoxicity - take on empty stomach - take Vit B6 to prevent toxicity 0.6-1.2 (1.5) mg/dl
What are the early S&S of hypoxemia?
Topical glucocorticoids do WHAT to the skin? A pt with cirrhosis is prescribed lactulose for what? what do you monitor for to make sure it's working.
3 top risk factors for laryngeal cancer? Low pressure or low volume sounds on the vent indicates?
What 6 metabolic abnormalities can result in seizures?
How much fluid can be taken out during a paracentesis?
3 diagnostic tests for pheochromocytoma:
4 things to consider when taking Isoniazid (INH)?
Normal Creatinine range:
Amount of fluid removed via thoracentesis is limited to how much at a time? Normal INR: How long does it take for pts exposed to pathogens to exhibit S&S of infeciton?
1 L (to prevent cardiovascular collapse) 1-2 1-2 days 1. check for unresponsiveness 2. call for help 3. position client 4. open airway 5. check for breathing 6.perform ventilations 7. check circulation (pulse) 8. start compressions 9. check for spontaneous pulse 1. smoking 2. Alpha-antitrypsin (AAT) deficiency 3. air pollution 1. turn on defibrillator 2. select energy lvl ~ 200 J 3. "lead select" 4. apply gel to paddles 5. position paddles on pt 6. check monitor display and assess rhythm 7. "Charging, Stand clear!" 8. press charge 9. "Shock on 3. One, I'm clear. Two, you're clear. Three, everybody's clear" 10. apply 25 lb pressure on both paddles and shock 11. check monitor for rhythm
Proper CPR steps (list 9)
What are the leading risk factors for developing COPD?
Defibrillator Steps:
Normal urine specific gravity range: Normal Mg+ range: Ostmomy bags should be cut how much larger than the stoma? Normal BUN range:
1.001-1.030 1.5-2.5 mEq/L 1/16 to 1/8 in larger than the stoma 10-25 mg/dl
100ml/hr or less. What's the normal rate for chest tube drainage? Normal PT range: Normal Hgb range: Diabetes is diagnosed when fasting blood sugar is at what level? Normal Na+ range: Report to physician if >100ml/hr. 12-15 sec 12-18 g/dl 126 or higher 135-145 mEq/l
Suctioning should not exceed how many seconds? A decrease in FEV1 or PERF by how much is common for asthma pts? Normal plt range: How do the ABG's change as a PE progresses? For chest tubes, the water seal should be maintained at what level? TB skin test will be positive how long after exposure to TB? Normal phosphate level: How long should pressure be applied on a puncture site for a patient receiving anticoagulant therapy? TB pts are no longer considered infectious after how many negative sputum cultures? Must administer tPA drug for CVA victims within how long of onset? Normal CVP range:
15 seconds 15-20% below the expected value 150-400 billion (10^9) 1st respiratory alkalosis (initial hyperventilation) 2nd respiratory acidosis (due to hypoxemia) 2 cm
2-10 weeks. 2.8-4.5 mEq/L
20 minutes
3 hours
3-7 mmHg
or 4-10 cm Water 3.5-5.0 (5.5) mEq/L Normal K+ range: Normal albumin range: Normal APTT range: Normal Hct range: 3.8-4.5 g/dl 30-45 sec 38-54%
T/F. surfactant activity is reduced in ARDS. Prednisone class and side effects What are Miotics for and what side effect does it cause?
True. corticosteroid (antiinflammatory): Side effects include immunosuppresion, fluid retention, hypgerglycemia, hypokalemia, and poor wound healing. used for Glaucoma side effect = blurred vision - uremia (ARF) - hepatic failure - PKU (phenylketouria) due to lack of a hepatic enzyme (genetic) - nutritional deficits - drug/alcohol w/drawal - drug/alcohol use - ascending flaccid motor paralysis - loss of sensory function - loss of DTR's - weakness before paralysis - loss of respiratory muscle control they rely on their low levels of arterial oxygen to drive their breathing - cool, clammy skin - sweating - anxiety, irritability, blurred vision - weakness, seizures Cushing's triad: - widened pulse pressure - bradycardia - irregular respiratory rate == indicates increased ICP
What 6 metabolic abnormalities can result in seizures?
What characterizies guillan barre? Why be careful of giving too much oxygen to COPD patients? S&S of hypoglycemia:
What is Cushing's triad and what does it indicate?
TB skin test will be positive how long after exposure to TB? What type of trach provides a seal between the upper and lower airway and is used for pts receiving mechanical ventilation? What characterizes osteomyelitis? What characteristics differentiate BPH from prostate cancer during an digital rectal exam?
2-10 weeks. cuffed trach bone pain that is worse with movement - other signs include fever, edema, and erythema BPH: enlarged but elastic Prostate Cancer: hard, irregular
5 S&S of myxedema coma: what position do you keep the pt following a thyroidectomy?
- depressed respirations - stupor (cerebral hypoxia) - hypothermia - bradycardia (low CO) - hypotension high fowlers (to promote venous return) - Dyspnea, air hunger - tachycardia - tachypnea - Anxiety - decreased O2 sat - hypotension short term, generally <5 years lung cancer pneumothorax = hyperresonnance hemothorax = dull to r/o pneumothorax and check resolution of effusions
6 common S&S of PE:
Should hormone replacement therapy (HRT) be used on a short-term or long-term basis? What is the leading cause of cancer-related deaths? Distinguish pneumothorax from hemothorax by percussion: Post-thoracentesis CxR is for?
What is used to confirm or rule out diagnosis of renal biopsy glomerulonephritis? How do you check for laryngeal nerve damage in ask the pt to speak as soon as they awaken from pts following a thyroidectomy? anesthesia. PaO2 <60 & SaO2 <90% what ABG values indicate ARF? or PaCO2 >50 & pH <7.30 False. T/F. Pts with hyperthyroidism often experience They experience increased appetite, but their fast decreased appetite. metabolism keeps their weight down. Taking aluminum-containing antacdis concurrently does what to Ciprofloxacin absorption? - hypovolemia (low volume) - hypoxia (low oxygen) - hydrogen ion excess (acidosis) - hyper-/hypo-kalemia (high/low K+) - hypothermia (low body temp) - taking drugs (overdose) - tamponade (cardiac) - tension pneumothorax (oneway valve in pleural cavity) - thrombosis (pulmonary) - thrombosis (coronary) Why is chemotherapy not used in the case of superior vena cava syndrome caused by breast cancer tumor? Decreases Cipro absorption
10 most common causes of Pulseless Electrical Activity (PEA):
5 H's and 5 T's
chemo does not shrink size of tumor, it only halts the growth.
surgical removal is too invasive and may increase Why is surgical removal of breast cancer tumor intrathoracic pressure, which worsens the superior not suggested in case of superior vena cava vena cava syndrome. syndrome?
T/F. Organ donation must be completed within 24 hours of patient death. T/F. aluminum overload causes constipation.
False. It should be completed within 72 hours. Some can be stored for longer. True. - high BP (often >200) - intense headaches - profuse sweating - feeling of doom - goosebumps - nasal stuffiness - facial erythema a medical emergency characterized by a massive SYMPATHETIC discharge that can occur in association with spinal cord injury or disease (e.g. MS) - high K+, P, CK, & myoglobin - low Ca++ - acidosis malignant hyperthermia - muscular rigidity - tachycardia - hyperthermia - hypercapnia - red-brown urine adverse reaction to certain anesthesia lack of hormones (e.g. ACTH, CRH) from the hypothalamus or pituitary that regulate steroid production in the adrenal glands True. adrenal insufficiency - to decrease serum ammonia levels - you monitor for LOC airborne and contact - for renal calculi - instruct to intake lots of fluids to flush out fragments HYPOcalcemia (due to hyperphosphatemia) False. GI tract cleansing and a clear liquid diet are interventions for a client having a lower GI tract procedure, not an upper GI procedure. - the client should be NPO for 6-12 hours prior to an EGD.
what are S&S of autonomic dysreflexia?
what is autonomic dysreflexia?
blood test results for malignant hyperthermia would reveal: the neuromuscular blocking agent succinylcholine is a trigger for what dangerous condition? what are 5 S&S of malignant hyperthermia? what causes malignant hyperthermia/hyperpyrexia? What is secondary adrenal insufficiency?
T/F. Addison's disease is autoimmune. Addison's disease is a form of what condition? A pt with cirrhosis is prescribed lactulose for what? what do you monitor for to make sure it's working. what kind of isolation precaution is needed for SARS? what is extracorporeal shock wave lithotripsy and to include in discharge teaching? do pts with chronic renal failure have HYPO- or HYPER- calcemia? T/F. Pts who are about to undergo EGD's should be on a 24 hr clear liquid diet and have GI cleansing prior to the procedure.
T/F. the paralysis that accompanies Guillian barre is temporary. tracheal shift in 3 kinds of pneumothorax: what helps the burning pain after an IM injection? what type of MI is associated with heart failure?
True. - simple pneumothorax: usually no shift - tension and hemothorax: shift to contralateral (unaffected) side warm compress
anterior MI (causes L ventricular dysfxn) False. T/F. in treating a burn victim, remove ALL clothing Remove only those pieces of clothing that is not from the burnt areas. sticking to the skin. If it sticks, don't remove. describe what a 1st degree burn looks like: red, no blisters, dry
what are the ABCDE's of emergency are?
Airway/neck/spine Breathing Circulation Disability Exposure
Heat stroke presentation and Tx
hypotension, tac tachycardia, a confusion, b behavior, seizure
Tx w/ rapid c measure
Frostbite presentation and T
white, waxy; may partial thickness; Tx w/ warm wate 41 C), pain meds tetanus shot
define Cardiac Arrest
sudden cessation breathing and ad circulation of bloo
= no pulse and no breathing without sufficient O2 supply, the brain will suffer cell anoxia within how many minutes? goals for management of cardiac arrest include...?
within 4-6 minute
- rapid ID of S&S - initiate circ and support - activate EMS - use emergency equipment
- stabilize pt - Dx and Tx Chain of survival involves...?
- early activation - early CPR/defib - early ACLS
Meds for VF or pulseless VT: (BEV LAMP)
- Bicarbonate - Epinephrine - Vasopressin - Lidocaine - Amiodarone - Magnesium sulf - Procainamide
Defibrillator Steps:
1. turn on defibrill 2. select energy l 3. "lead select" 4. apply gel to pa 5. position paddle 6. check monitor and assess rhyth 7. "Charging, Sta 8. press charge 9. "Shock on 3. O clear. Two, you're Three, everybody 10. apply 25 lb pr both paddles and 11. check monito rhythm
Proper CPR steps (list 9)
1. check for unresponsivenes 2. call for help 3. position client 4. open airway 5. check for breat 6.perform ventilat 7. check circulatio 8. start compress 9. check for spon pulse
What are the normal ranges for ABG?
pH: 7.35-7.45 PaO2: 80-100 mm PaCO2: 35-45 m HCO3: 22-26 mE
What is Allen's test?
Allen's test verifie
of radial and ulna circulation. - compress both u radial arteries wh forms fist - have client relax go of one artery, should turn pink - repeat and let g artery how long should pressure be applied on a puncture site for a patient receiving anticoagulant therapy? what S&S should be reported to the doc following an arterial puncture? 20 minutes
ashen fingers and - tachypnea - tachycardia - restlessness - pallor - HTN - resp distress
what are the early S&S of hypoxemia?
what are the late S&S of hypoxemia?
- confusion and s - cyanosis - bradypnea - bradycardia - hypotension - cardiac dysrhyth
what are the S&S of oxygen toxicity?
- nonproductive c - substernal pain - nasal stuffiness - N/V - fatigue - HA - sore throat - hypoventilation
why be careful of giving too much oxygen to COPD patients?
they rely on their of arterial oxygen their breathing 15 seconds
suctioning should not exceed how many seconds? what do you do for ventilator patients right before you suction? what is a contraindication for a bronchoscopy? what 2 things do you check for before giving anesthetic agents to patients?
hyperoxygenate w FiO2
severe tracheal s
pt allergies & pre
dentures contraindication to chest tube insertion and thoracentesis?
severe thrombocy (due to risk for ex bleeding)
what do you do first if the chest tube tubing becomes disconnected?
place tubing in st water to restore w
S&S of pneumothorax? (similar to CHF in older adults)
dyspnea, JVD, pa coughing
Heat stroke presentation and Tx
hypotension, tach tachycardia, anxi confusion, bizarre seizures, coma.
Frostbite presentation and Tx
define Cardiac Arrest
Tx w/ rapid coolin measures white, waxy; may partial thick Tx w/ warm wate 41 C), pain me tetanus s sudden cessation breathing and ad circulation of bloo
= no pulse and no breathing
without sufficient O2 supply, the brain will suffer cell anoxia within how within 4-6 minute many minutes? - rapid ID of S&S - initiate circ and support - activate EMS goals for management of cardiac arrest include...? - use emergency equipment - stabilize pt - Dx and Tx - early activation Chain of survival involves...? - early CPR/defib - early ACLS - Bicarbonate - Epinephrine - Vasopressin Meds for VF or pulseless VT: - Lidocaine (BEV LAMP) - Amiodarone - Magnesium sulf - Procainamide
Defibrillator Steps:
Proper CPR steps (list 9)
What are the normal ranges for ABG?
What is Allen's test?
1. turn on defibrill 2. select energy l 3. "lead select" 4. apply gel to pa 5. position paddle 6. check monitor and assess rhyth 7. "Charging, Sta 8. press charge 9. "Shock on 3. O clear. Two, you're Three, everybody 10. apply 25 lb pr both paddles and 11. check monito rhythm 1. check for unresponsivenes 2. call for help 3. position client 4. open airway 5. check for breat 6.perform ventilat 7. check circulatio 8. start compress 9. check for spon pulse pH: 7.35-7.45 PaO2: 80-100 mm PaCO2: 35-45 m HCO3: 22-26 mE Allen's test verifie of radial and circulatio - compress both radial arteries w forms fis - have client rela go of one arter should turn - repeat and let g artery
how long should pressure be applied on a puncture site for a patient receiving anti-coagulant therapy? what S&S should be reported to the doc following an arterial puncture? what are the early S&S of hypoxemia? what are the late S&S of hypoxemia?
20 minut
ashen fingers a
- tachypnea - tachycardia - restlessness- pa - HTN - resp distress - confusion and s cyanosis - bradypnea- brad - hypotension
what are the S&S of oxygen toxicity?
why be careful of giving too much oxygen to COPD patients? suctioning should not exceed how many seconds? what do you do for ventilator patients right before you suction? what is a contraindication for a bronchoscopy? what 2 things do you check for before giving anesthetic agents to patients? contraindication to chest tube insertion and thoracentesis? what do you do first if the chest tube tubing becomes disconnected? S&S of pneumothorax? (similar to CHF in older adults)
- cardiac dysrhyth - nonproductive c - substernal pain - nasal stuffiness - N/V - fatigue - HA - sore throat - hypoventilation they rely on their of arterial oxygen their breathing 15 seconds
hyperoxygenate w FiO2
severe tracheal s
pt allergies & pre dentures severe thrombocy (due to risk for ex bleeding) place tubing in st to restore water s dyspnea, JVD, pa coughing
instruct the patient to do what during a chest tube removal? Assessment findings of pleural effusion? Amount of fluid removed via thoracentesis is limited to how much at a time?
perform valsalva maneuver (or take a deep breath and hold it) - decreased breath sounds - dull percussion sounds - decreased chest wall expansion - pain 1 L (to prevent cardiovascular collapse)
Sit upright with arms and shoulders raised and How to position a patient for supported on pillows on overbed table (also no talking thoracentesis? or coughing unless instructed) - hypotension - reflex bradycardia Manifestations of shock? - diaphoresis - faintness transudates - CHF, cirrhosis, nephritic syndrome exudates indications for thoracentesis: - empyema, pna chest trauma - lung/heart surgery, blunt/crushing injury sitting upright w/ arms and shoulders raised and client position for supported on pillows on overbed table. thoracentesis: No coughing or talking
after thoracentesis, place pt on which side and for how place pt on unaffected side for 1 hr. long? post-thoracentesis CxR is to r/o pneumothorax and check resolution of effusions for? T/F. It is important to assess the trach pt for risk for True. aspiration. what type of trach provides a seal between the upper and lower airway and is used for cuffed trach pts receiving mechanical ventilation? what type of trach is used for kids under 8 yrs and for those uncuffed trach who can protect the airway from aspiration? what type of trach is used for pts with long or extra-thick single-lumen tube necks? what type of trach is used metal trach permanently? for cuffed trachs, keep pressure below what level to reduce risk of tracheal below 20 mm Hg. necrosis due to prolonged compression of tracheal capillaries? provide trach care how often? what vent mode provides preset ventilator rate and tidal volume but requires pt to initiate breaths? what is SIMV mode? Q8h. AC (assisted control) mode SIMV (Synchronized Intermittent Mandatory Ventilation) has present vent rate and tidal volume. The pt can initiate breaths but tidal volume depends on client's effort. If pt does not initiate breaths, the vent takes over but synchronizes with pt's breathing pattern. Pressure Support Ventilation mode. Present pressure delivered during spontaneous inspiration to reduce work of breathing. The pt controls rate and volume. Often used as a weaning mode. However, PSV doesn't guarantee minimal minute ventilation and is often combined with other modes (SIMV, AC). Positive End Expiratory Pressure. Used to increase functional residual and improve oxygenation by opening collapsed alveoli. Must be used in combo with AC or SIMV, can't be used alone. It decreases CO and may cause trauma to lung tissue caused by high tidal volumes and increased ICP. - pt biting the tube - need for suctioning - kinks in tubing
What is PSV mode?
What is PEEP?
high pressure alarm sounds on the vent indicates?
low pressure or low volume sounds on the vent indicates? 3 characteristics of Asthma: what test is the most accurate for diagnosing asthma and its severity? a decrease in FEV1 or PERF by how much is common for asthma pts?
- tubing disconnections - air leaks around cuff - edema - bronchoconstriction - secretions PFT (pulmonary function test) 15-20% below the expected value
Albuterol: class Ipratropium (Atrovent) theophylline (Theo-dur) Prednisone class and side effects Montelukast (Singulair) cromolyn sodium (Intal) Status Asthmaticus: what is it and what to do when it happens? COPD encompasses 2 diseases: What is emphysema? What are the leading risk factors for developing COPD? T/F. Most people with emphysema also have chronic bronchitis. What is used to classify COPD as mild to very severe? Why monitor H&H in COPD pts?
short-acting beta agonist (provides rapid relief for asthma) anticholinergic: blocks parasympathetic NS and allows for sympathetic NS to exert its effects such as bronchodilation. methylxanthine - bronchodilator (cousin of caffeine) corticosteroid (antiinflammatory): Side effects include immunosuppresion, fluid retention, hypgerglycemia, hypokalemia, and poor wound healing. Leukotriene antagonist mast cell stabilizer life-threatening; often unresponsive to common tx. Prepare for emergency intubation and potent systemic bronchodilators like epinephrine as well as systemic steroid therapy. - emphysema - chronic bronchitis loss of lung elasticity that results in destruction of alveoli - hyperinflation - resp acidosis 1. smoking 2. Alpha-antitrypsin (AAT) deficiency 3. air pollution True FEV to FVC ratio. smaller ratio = worse COPD to recognize polycythemia (compensation to chronic hypoxia)
Provide COPD pts with 2-4L/min O2 via NC. For pts with chronic hypercarbia, provide more or less less. because low O2 levels are needed to drive their breathing. O2 and why? Right-sided heart failure. - blood flow through lungs is hard what is Cor Pulmonale? (resulting from alveoli stiffness or airway collapse) - thickens right side of heart - poor oxygenation inflammation of lungs that results in: characteristics of PNA? - edema - exudate PNA: what are the 8 risk factors? - age - infections - smoking - aspiration
- chronic lung probs - immobility - mechanical ventilators - immunocompromised status what does high-Fowler's position help with? what kind of O2 therapy is prescribed for pna? why give corticosteroids for pna? breathing and air exchange heated and humidified O2 decreases airway inflammation - immunosuppression - fluid retention - hypgerglycemia - hypokalemia - poor wound healing atelectasis - confusion - hypoxia 1-2 days TB
5 side effects of corticosteroids: diminished or absent breath sounds could indicate? two common manifestations of pna in older adults? how long does it take for pts exposed to pathogens to exhibit S&S of infeciton? ghon tubercles are a characteristic of what infection?
T/F. A person with TB is not contagious until S&S are present. TB skin test will be positive how long after exposure to TB? TB dx is confirmed by what? the best sputum samples should be taken when? 4 things to consider when taking Isoniazid (INH)? Rifampin (RIF): 2 things about RIF? Pyrazinamide (PZA): watch for what when taking this drug? Ethambutol (EMB): watch for what when taking this drug? Streptomycin: watch for what when taking this drug? encourage foods rich in what 3 things for TB pts:? TB pts are no longer considered infectious after how many negative sputum cultures? Hallmarks of ARDS: decreased UO with tall peaked T waves indicate: describe second degree AV block (type I): Expect what if pt is malnurished and is breaking down fats for energy?
TRUE 2-10 weeks. Positive sputum culture. - sputum smears (acid-fast) only shows how infectious it is. Early morning. - first morning specimens are the most accurate. - watch for hepatitis - watch for neurotoxicity - take on empty stomach - take Vit B6 to prevent toxicity - orange/reddish pee, sweat, tears - watch for hepatotoxicity hepatotoxicity changes in visual acuity ototoxicity - protein - iron - Vit C 3 - hypoxemia that does not improve with oxygen therapy - extensive pulmonary edema (whiteout on x-ray) hyperkalemia when PR intervals progressively lengthen and some P waves are not followed by QRS complexes. (P waves are regular) ketones in urine
Why be sure to take calcium and thyroid hormone supplements several hours apart? T/F. Thiazides reduces renal excretion of calcium. high BS, hx of pituitary tumor, and osteoporosis may indicate: What blocks coagulation by enhancing the inhibitory effects of antithrombin, which prevents conversion of prothrombin to thrombin and fibrinogen to fibrin? What interferes with the hepatic synthesis of Vit. K-dependent clotting factors, thereby reducing the supply of coagulation factors II, VII, IX, and X? modes of Hep B transmission: T/F. Acoustic neuroma results in reversible hearing loss. What is a life-threatening finding in an asthma pt that suggests severe airflow obstruction? T/F. Traction pins should be covered with dressing and changed daily. How can cardiac cath result in intrarenal renal failure?
calcium reduces absorption of thyroid hormones. But thyroid hormones do not increase need for calcium. T. So need less calcium supplementation. Cushings Heparin Warfarin/Coumadin - blood - semen/vaginal fluids - saliva - NOT by tears, urine, or sweat False. It is permanent irreversible damage to CN VIII. silent chest False. Traction pin sites should be covered initially, but then should be exposed to air. Rinsing with sterile saline is ok. the dyes used can be nephrotoxic
What distinguishes MI from angina pectoris?
Rest and Nitroglycerine do not relieve MI pain. topical glucocorticoids do WHAT to the skin? T/F. Constant bubbling in a chest tube closed water-seal system is normal. T/F. Use salt substitutes for chronic renal failure pts. Why do chronic renal failure pts need folic acids supplements? an aura precedes what type of seizure?
- THINS the skin - DOES NOT darken skin. False. Intermittent bubbling is normal. Constant bubbling indicates air leak --> tension pneumothorax. False. Salt substitutes contain high K+. to treat anemia because their erythropoietin production is inadequate. partial. - high K+, P, and Na+ - low Ca++ - fluid volume overload - increased BUN & Cr - metabolic acidosis (high H+) - UO under 400ml/day (oliguria) - anemia - NSAIDS (e.g. ibuprofen) - Aminogylcosides (e.g. gentamycin) - ACE inhibitors (e.g. catopril) 3 hours tissue plasminogen activator, a clot buster.
common findings for acute renal failure:
name 3 nephrotoxic drug groups: must administer tPA drug for CVA victims within how long of onset? what is tPA?
extreme paralysis is an indication of CVA in which hemisphere? what's Guillain Barre?
right
- postinfection polyneuritis - autoimmune disorder that attacks mainly Schwann cells and destroys their myelin sheaths. - ascending flaccid motor paralysis - loss of sensory function what characterizies guillan barre? - loss of DTR's - weakness before paralysis - loss of respiratory muscle control - loss of sphincter control what are some systemic effects of guillain - bladder/bowel retention barre? - sweating, sputum - SIADH which two CN's are not affected by CN I - olfactory Guillain barre? CN II - optic - lumbar puncture - PFT how do you diagnose guillain barre? - EMG - CBC/ABG's brady. what is one cardio side effect of Timolol? check pulse rate. True. T/F. Simple seizures do not involve a Complex seizures involve a change in change in consciousness. awareness/consciousness. - uremia (ARF) - hepatic failure - PKU (phenylketouria) due to lack of a hepatic What 6 metabolic abnormalities can result enzyme (genetic) in seizures? - nutritional deficits - drug/alcohol w/drawal - drug/alcohol use autoimmune disorder that affects skeletal muscles What is Myasthena Gravis? that manifests in weakness and fatigability. - rheumatoid arthritis Name 4 disorders associated with - SLE Myasthenia Gravis: - ulcerative colitis - pernicious anemia - ptosis (drooping eyelid) - dysphagia manifestations of myasthenia gravis: - neck weakness, head bob - muscle weakness - even respiratory failure/arrest which protein marker gives you the myoglobin (peaks 3-15 hrs) earliest diagnosis for an MI? followed CK-MB (1-2 days) followed by what else? which marker is a very sensitive indicator troponin. of MI? how long does it remain elevated it's more specific than CK-MB, and remains elevated for? for 7-10 days. Normal BUN range: 10-25 mg/dl
normal Creatinine range: normal Na+ range: normal K+ range: normal Mg+ range:
0.6-1.2 (1.5) mg/dl 135-145 mEq/l 3.5-5.0 (5.5) mEq/L 1.5-2.5 mEq/L
normal Ca++ range: normal albumin range: normal Cl- range: normal Hgb range: normal Hct range: normal WBC range: full blown AIDS CD4+ level: normal APTT range: normal PT range: normal plt range: normal INR: normal phosphate level: normal CD4+ range in healthy adult: diabetes is diagnosed when fasting blood sugar is at what level? ARF leads to metabolic acidosis or alkalosis? normal urine specific gravity range: normal CVP range: normal MAP range: normal EF: what does CVP tell us? What 3 things are elevated in the blood for Cushings?
9-11 mEq/L 3.8-4.5 g/dl 96-106 mEq/L 12-18 g/dl 38-54% 4-11 billion/L (10^9/L) less than 200 30-45 sec 12-15 sec 150-400 billion (10^9) 1-2 2.8-4.5 mEq/L 400-1600 126 or higher metabolic acidosis due to retained H+ 1.001-1.030 3-7 mmHg or 4-10 cm Water 80-100 mmHg >75% right atrial pressure & right ventricular end diastolic volume. - cortisol - blood sugar - Na+
What 3 things are decreased in the blood for Cushings?
- K+ - Ca++ - ACTH - K+ - Ca++ What 4 things are elevated in the blood for Addison's? - BUN - Creatinine - cortisol What 4 things are decreased in the blood for - aldosterone Addison's? - Na+ - blood sugar For Cushings and Addisons, which one results in fluid Cushings --> HTN, fluid overload volume overload and which one results in dehydration? Addisons --> dehydration SubQ injection of vasopressin: - if produces increased specific gravity, What is the vasopressin test used for and what does it then you have central DI. do? - if produces no increase in sp gr, then it's nephrogenic DI. What is the UO like for DI? 5-20 liters per day.
What is DDAVP for? Why is tegretol used for DI? Is vasopressin therapy lifelong for DI pts?
desmopression acetate (Vasopressin in liquid form) is for ADH replacement. it's an ADH stimulant. yes, its lifelong.
T/F. encourage DI pts to use mouthwash in response False. Encourage them to drink WATER. to thirst. tall peaked T wave, prolonged PR interval, and HYPERkalemia widened QRS indicate: flattened T wave, depressed relfexes, flabby muscles, HYPOkalemia parasthesia, and hyperglycemia indicate: lethargy, depressed reflexes, stupor/coma, N/V, fractures, and shortening of ST segment and QT HYPERcalcemia interval indicate: numbness/tingling around mouth, hyperreflexia, tetany, seizures, and elongation of ST segment and QT HYPOcalcemia interval indicate: constipation, psychotic noise, bone pain, What are the "groans, moans, bones, stones, and kidney stones, and overtones" for HYPERcalcemia: depression/confusion. neuromuscular and CNS one major characteristic of HYPOmagnesemia: HYPERirritability. depressed neuromuscular and CNS one major characteristic of HYPERmagnesemia: function phosphorous levels are opposite of what levels in the calcium (via PTH action) blood? KCL supplements should never exceed what rate? what is used to treat severe hyperkalemia? what is used to moderate hyperkalemia? T/F. Never give Calcium IM. T/F. Loop diuretics are used for hypercalcemia. always assess which 3 electrolytes together? main CNS characteristics of dehydration/hypovolemia: should NOT exceed 10-20mEq/hr IV calcium gluconate (to reverse membrane excitability) IV insulin and glucose True. give orally w/ Vit D. True. K+, Ca++, and Mg++ restlessness, irritability
main CNS characteristics of hypervolemia: what is pheochromocytoma? why should you avoid abd pressure, such as abd palpation for a pheochomocytoma pt? what is VMA?
headache, lethargy, confusion tumor of adrenal gland --> excess epinephrine and NE (catecholamines) intra-abd pressure can cause hypertensive episode. VMA (vanillylmandelic acid test) = 24hr urine collection for catecholatmines, metanephrine, and VMA. - restrict caffeine, vanilla, licorice for 2-3 days in advance - hold aspirin and anti-HTN meds - maintain moderate acitivity Used to determine if pt has pheochromocytoma. Clonidine (Catapres) is supposed to suppress catecholamine release.
What are nursing implications for VMA testing?
What is a Clonidine supression test?
3 diagnostic tests for pheochromocytoma:
- VMA - Clonidine - phentolamine (Regitine) It is diagnostic if administration of Regitine (an alpha blocker) causes rapid decrease in systolic BP of 35 mmHg or more and diastolic BP of 25 mmHg or more. True. it is lifelong. - cool, clammy skin - sweating - anxiety, irritability, blurred vision - weakness, seizures - hot dry skin - no sweating - N/V, abd pain - Kussmaul's breathing (fruity breath) give Glucagon SubQ or IM.
How is Regitine (phentolamine) used to diagnose pheochromocytoma? T/F. After bilateral adrenalectomy, glucocorticoid and mineralocorticoid replacement is required for pts with pheochromocytoma for LIFE. S&S of hypoglycemia:
S&S of hyperglycemia:
if hypoglycemic pt is unconscious, give what? via what route?
Oral antidiabetic meds may reduce blood lvls of some oral what do you advise for diabetic women of childbearing contraceptives, so they may need additional contraceptions age who are on oral antidiabetic meds and are also methods. using oral contraception? What drink should diabetics avoid in their diet, esp when taking oral antidiabetic meds? Avoid alcohol. (to avoid disulfram-like rxn) - avoid alcohol - monitor renal fxn - monitor liver fxn - oral contraception less effective Lantus/Glargine (long-acting) kidney failure hyperglycemic-hyperosmolar nonketotic syndrome. What is HHNS? most common cause of DKA: HHNS is more common in what kind of people? DKA is more common in what kind of people? T/F. There is an absence of ketones as well as acidosis in HHNS. T/F. SIADH results in renal reabsorption of sodium and water. early S&S of SIADH include: Very late S&S of SIADH include: BS>600, dehydration, absence of ketosis. Life threatening. infection. (others include illness, surgery, trauma, and stress) older adults and people w/ untreated type 2 DM. type 1 DM pts. True. False. SIADH leads to renal reabsorption of water (ADH effects) and excretion of sodium (RAAS suppression) HA, muscle cramps, weight gain, weakness confusion, Cheyne-Stokes respirations, seizures, coma
4 things to watch out for when on oral antidiabetic meds: which insulin cannot be mixed with any other type? besides, foot ulcers, cardio problems, and blindness, what else can diabetes result in?
moderate progression of SIADH can result in what S&S?
personality changes, HYPOreflexia, N//V
What 2 meds can be given to treat SIADH by blocking renal response to ADH? what's Cretinism? hypothyroidism occurs more often in what kind of people? Is serum cholesterol decreased or increased in hypothyroidism? T/F. Anemia commonly accompanies hypothyroidism. what kind of drugs is contraindicated for a pt with hypothyroidism? Is levothyroxine (Synthroid) for HYPO- or HYPERthyroidism? Is thyroid hormone therapy lifelong or temporary? what kind of diet for hypothyroidism? is cold intolerance a characteristic of HYPO- or HYPERthyroidism? 5 S&S of myxedema coma:
- demeclocycline (Declomycin) - lithium state of severe hypothyroidism in infants. women in their 40s and 50s. increased. True. CNS depressants, barbiturates, sedatives, etc. for HYPOthyroidism. lifelong. low calorie, high bulk (for constipation) HYPOthyroidism. - depressed respirations - stupor (cerebral hypoxia) - hypothermia - bradycardia (low CO) - hypotension anterior pituitary - T3 - T4 - calcitonin anterior pituitary prevents bone resorption and keeps blood calcium lvls low Graves dz blocks thyroid hormone synthesis False. They experience increased appetite, but their fast metabolism keeps their weight down. a sudden surge of large amts of thyroid hormones into bloodstream (a medical emergency!) - hyperthermia - HTN - tachydysrhythmia - delirium - vomiting - abd pain HYPERthyroidism it may indicate that the parathyroid glands are damaged. IV calcium gluconate. 50ml
T3 and T4 secretion is regulated by what gland? the thyroid gland produces which 3 hormones? TSH is secreted by which gland? what does calcitonin do? what's the most common cause of hyperthyroidism? Why is PTU given for hyperthyroidism? T/F. Pts with hyperthyroidism often experience decreased appetite. what is thyroid storm?
6 S&S of thyroid storm:
goiters appear in HYPO or HYPER thyroidism? why watch for hypocalcemia following a thyroidectomy? what do you give in case of hypocalcemia? how many milliliters of drainage do you expect in the 1st 24hrs following a thyroidectomy?
what position do you keep the pt following a thyroidectomy? how do you check for laryngeal nerve damage in pts following a thyroidectomy?
high fowlers (to promote venous return) ask the pt to speak as soon as they awaken from anesthesia.
what do you do to prevent hemorrhage in pts following a thyroidectomy? what do you monitor for in hypocalcemia? do you experience constipation or diarrhea with colon cancer? S&S of colon cancer:
avoid neck flexion/extension and always align neck with body tingling of fingers and toes, spasms, and convulsions you may experience either one or both. - fatigue - weight loss - abd distension, bloating - constipation, diarrhea, change in bowel habits - anemia - meats - NSAIDs - Vit. C colonoscopy/sigmoidoscopy reddish pink
what 3 things should pts avoid in their diet 48 hours prior to FOB testing? what is the definitive test for colorectal cancer? what color should stomas be?
pts with strong hix of colorectal cancer - fats shoulud reduce intake of what 2 - meats things? either: which positions should the pt use - supine or during a paracentesis? - upright with arms over bedside table and legs dangling volume of fluid removed during paracentesis should no more than how no more than 1L (1kg, or 2.2lb) much? what do you measure before and after abd girth a paracentesis? what do you monitor throughout the respiration rate paracentesis procedure? - shock monitor for which 3 complications - peritonitis following a paracentesis? - perforated bladder which serum level can drop dangerously low following a serum albumin paracentesis? what is the primary risk factor for portal HTN development of esophageal varices? name 2 conditions that can result in - alcoholic cirrhosis portal HTN? - viral hepatitis what is the most serious complication hypovolemic shock of esophageal varices? what's the most definitive test for EGD = diagnosing peptic ulcers? esophago-gastro-duodenoscopy how is Sucralfate (Carafate) different give 1 hr before meals instead of 1-3hrs after from other antacids? meals. what types of food should a pt with avoid milk, sweets, sugars (e.g. fruit juice, dumping syndrome avoid? sweetened fruit, milk shakes, honey, syrup, jelly) - postprandial hypoglycemia what are 3 complications of dumping - malnutrition syndrome to watch out for? - F&E imbalance - spasmodic colicky pain instead of constant diffuse pain 3 characteristics that set small bowel - visible peristaltic waves rather than significant obstruction apart from large bowel abd distention obstruction: - sudden projectile vomiting that relieves pain rather than infrequent vomiting
Differentiate WBC count for appendicitis and peritonitis.
Usually, 10-18 x10^9/L for appendicitis >20 x10^9/L for peritonitis
Differentiate temperature levels for appendicitis and peritonitis.
Usually, low fevers (<101) for appendicitis higher fevers (>101) for peritonitis Differentiate diet prescriptions for IBD versus - low fiber diet for IBD diverticulitis. - high fiber diet for diverticulitis Difference in age of pts with IBD versus pts with - IBD: age 15-40, younger diverticulitis: - Diverticulitis: usually over 50 Major complication for ulcerative colitis: major complication for Crohn's dz: T-tube drainage range: major complication of casts: major evidence that points to compartment syndrome: major complication of tractions: what characterizes osteomyelitis? the primary concept of pin care to avoid crosscontamination is: what are 3 LATE signs of neurovascular compromise in a pt with a cast/splint/traction? what are 3 EARLY signs of neurovascular compromise in a pt with a cast/splint/traction? toxic megacolon fistulas - initially may be up to 500ml/day, then gradually decrease overtime. - NEVER >1L/day compartment syndrome unrelieved pain or pain that is out of proportion to the injury. - other points include paresthesia, pallor, diminished pulses osteomyelitis bone pain that is worse with movement - other signs include fever, edema, and erythema use one cotton tip swab per pin (cotton swab soaked with peroxide or iodine) polar - cool/cold fingers/toes paralysis of fingers/toes pulses - weak pain - not relieved w/ elevation or meds paresthesia - numbness or tingling pallor - cap refill time >3 sec, blue fingers/toes - RA is bilaterally symmetrical, OA is not - RA pain after rest, OA pain with movement - RA is autoimmune, OA is not short term, generally <5 years more than 1 saturated pad per 4hrs BPH: enlarged but elastic Prostate Cancer: hard, irregular an indwelling 3-way catheter when you see bright red blood clots flow out (you need to dilute it) to keep catheter free of obstruction and to keep the irrigation pink or lighter.
name 3 differences between osteoarthritis and rheumatoid arthritis. should hormone replacement therapy (HRT) be used on a short-term or long-term basis? what is considered excess vaginal postop bleeding following a hysterectomy? what characteristics differentiate BPH from prostate cancer during an digital rectal exam? what kind of catheter is used following a prostatectomy or a TURP? when do you increase bladder irrigation rate? what is continuous bladder irrigation for?
what is the normal PSA level? what is the priority nursing action immediately following a prostectomy? what should a woman not use prior to a mammogram? when should a baseline screening mammogram be done? what are Miotics for and what side effect does it cause?
<4 ng/ml maintaining continuous bladder irrigation talcum powder or deodorant age 40 used for Glaucoma side effect = blurred vision
what happens to the CNS with multiple sclerosis? what's used for definitive diagnosis for MS? What kind of precaution should be used for pts with chicken pox (Varicella)? What kind of precaution should be used for pts with TB? What kind of precaution should be used for pts with disseminated varicella Zoster? What kind of precaution should be used for pts with measles (Rubeola)? What kind of precaution should be used for pts with HIB? What kind of precaution should be used for pts with pertussis? What kind of precaution should be used for pts with mumps? What kind of precaution should be used for pts with Rhinovirus? What kind of precaution should be used for pts with rubella? What kind of precaution should be used for pts with scarlet fever? What kind of precaution should be used for pts with C. Diff? What kind of precaution should be used for pts with congenital rubella? What kind of precaution should be used for pts with Hep A? What kind of precaution should be used for pts with shingles? What kind of precaution should be used for pts with impetigo? What kind of precaution should be used for pts with MRSA? What kind of precaution should be used for pts with herpes simplex? What kind of precaution should be used for pts with rabies? What kind of precaution should be used for pts with rheumatic fever? What kind of precaution should be used for pts with West Nile fever? acute glomerulonephritis usually commonly follows what illness?
plaque deposits in the white matter that damages myelin sheaths MRI brain and spine (for plaques) airborne airborne airborne airborne droplet droplet droplet droplet droplet droplet contact contact contact contact contact contact contact standard standard standard strep throat
what is used to confirm or rule out diagnosis of glomerulonephritis? what is nephrotic syndrome?
renal biopsy glomerular capillary damage resulting in loss of serum proteins and decreased serum osmotic pressure.
3 characteristics of nephrotic syndrome: what happens to serum cholesterol, triglycerides, and LDLs in nephrotic syndrome? Laryngeal cancer usually affects what gender and age? 3 top risk factors for laryngeal cancer? encourage what kind of diet for laryngeal cancer pts? T/F. Pts who undergo total laryngectomies will lose their natural voices. If a nodal neck dissection (radical neck) is done for laryngeal cancer, what happens to the shoulders following surgery? what's a cordectomy? aspiration can lead to the development of what respiratory condition? what is the leading cause of cancer-related deaths? what type of lung cancer is fast growing and almost always associated with the hx of smoking? most lung cancers belong in which category (small cell or non-small cell?) The TNM system for staging lung cancer stands for what?
- proteinuria - HYPOalbuminemia - edema they're all elevated men over 60 - tobacco - alcohol - harmful chemicals (chronic exposure) high protein and high calories True. shoulders drop because CN XI (spinal accessory nerve) is cut. excision of a vocal cord pneumonia lung cancer small cell lung cancer non-small cell T = tumor N = nodes M = metastasis - persistent cough w/ or w/o rust/blood-colored sputum - dyspnea - unilateral wheezing - chest wall pain high protein high calorie True. facial edema, tightness of shift collars, nosebleeds, peripheral edema, and dyspnea mental status changes, cyanosis, hemorrhage, and hypotension. DVT True. CT scan 1st respiratory alkalosis (initial hyperventilation) 2nd respiratory acidosis (due to hypoxemia) False. Onset of S&S for PE is sudden and rapid. - Dyspnea, air hunger - tachycardia - tachypnea - Anxiety
what kind of respiratory S&S do you expect to find in lung cancer pts? what kind of diet is prescribed for lung cancer pts? T/F. superior vena cava syndrome is a medical emergency. What are early signs of Superior vena cava syndrome? what are late signs of superior vena cava syndrome? what's the most common cause of pulmonary embolism? T/F. Oral contraceptives and estrogen therapies are risk factors for PE. What is commonly used to diagnose PE? How do the ABG's change as a PE progresses? T/F. Onset of S&S for PE is slow. 6 common S&S of PE:
- decreased O2 sat - hypotension why are streptokinase and alteplase used for PE? used as fibrinolytic therapy to break up blood clots
what's the highest nursing priority for a pt with PE? crystalloids are used to: dobutamine is used to: T/F. Recent surgery is a contraindication to fibrinolytic therapy. classification of acute respiratory failure (ARF) is based on what? what ABG values indicate ARF? T/F. Clients w/ ARF are always hypocapneic. T/F. ARDS is a state of ARF. mode of transmission for SARS is:
Oxygen therapy restore intravascular volume and prevent shock improve cardiac contractility True. ABG's PaO2 <60 & SaO2 <90% or PaCO2 >50 & pH <7.30 False. Client with ARF are always hypoxemic. True. droplet - persistent hypoxemia despite administration of 100% O2 - decreased pulmonary compliance - dyspnea - bilateral pulmonary edema that is noncardiac - dense pulmonary infiltrates ("ground glass" on CxR) True. PEEP False. PEEP increases intrathoracic pressure and leads to decreased cardiac output. thoracentesis deviates to the unaffected side pneumothorax = hyperresonnance
5 ARDS indicators:
T/F. surfactant activity is reduced in ARDS. which setting on mechanical ventilator is used to prevent alveolar collapse during expiration? T/F. PEEP can lead to increased cardiac output. what needs to be done to confirm hemothorax? in tension pneumothorax, tracheal deviation occurs on which side? Distinguish pneumothorax from hemothorax by percussion:
hemothorax = dull False. T/F. Increased cardiac output resulting in HTN is a Increased intrathoracic pressure with decreased CO resulting in possible complication of pneumothorax. HYPOtension is a possible complication of pneumothorax What's a definitive sign of tension pneumothorax? tracheal deviation. for chest tubes, the water seal should be 2 cm maintained at what level? T/F. continuous bubbling is expected with a water False. seal chamber. Tidaling is expected, but continuous bubbling is a sign of air leak. Taking nitrates along with Viagra can cause what severe hypotension serious problem? False. T/F. Use lotions on dry skin following radiation to Using lotions on the dry skin patches caused by radiation can prevent cracking. further irritate the skin. Taking aluminum-containing antacdis concurrently decreases Cipro absorption does what to Ciprofloxacin absorption? ostmomy bags should be cut how much larger 1/16 to 1/8 in larger than the stoma than the stoma?
T/F. Hyperkalemia decreases GI motility.
False. HYPOkalemia decreases GI motility.
T/F. An adverse rxn of furosemide is HYPOnatremia. What's the normal rate for chest tube drainage?
True. 100ml/hr or less. Report to physician if >100ml/hr.
T/F. Increased ESR occurs with any inflammatory process. how much fluid can be taken out during a paracentesis?
True. - Usually limited to 1L in a short period of time. (Slow drainage can be used to take out >1L of fluid over several hours.) Cushing's triad: - widened pulse pressure - bradycardia - irregular respiratory rate == indicates increased ICP
what is Cushing's triad and what does it indicate?
what color is a full thickness burn? what color is a 3rd degree burn? describe a 2nd degree burn? describe what a 1st degree burn looks like:
cream, tan, brown, black white, charred-looking red, blistered red, no blisters, dry
False. T/F. in treating a burn victim, remove ALL clothing from the Remove only those pieces of clothing that is not sticking burnt areas. to the skin. If it sticks, don't remove. anterior MI what type of MI is associated with heart failure? (causes L ventricular dysfxn) what helps the burning pain after an IM injection? tracheal shift in 3 kinds of pneumothorax: T/F. the paralysis that accompanies Guillian barre is temporary. T/F. Pts who are about to undergo EGD's should be on a 24 hr clear liquid diet and have GI cleansing prior to the procedure. do pts with chronic renal failure have HYPO- or HYPERcalcemia? what is extracorporeal shock wave lithotripsy and to include in discharge teaching? what kind of isolation precaution is needed for SARS? A pt with cirrhosis is prescribed lactulose for what? what do you monitor for to make sure it's working. Addison's disease is a form of what condition? T/F. Addison's disease is autoimmune. What is secondary adrenal insufficiency? what causes malignant hyperthermia/hyperpyrexia? warm compress - simple pneumothorax: usually no shift - tension and hemothorax: shift to contralateral (unaffected) side True. False. GI tract cleansing and a clear liquid diet are interventions for a client having a lower GI tract procedure, not an upper GI procedure. - the client should be NPO for 6-12 hours prior to an EGD. HYPOcalcemia (due to hyperphosphatemia) - for renal calculi - instruct to intake lots of fluids to flush out fragments airborne and contact - to decrease serum ammonia levels - you monitor for LOC adrenal insufficiency True. lack of hormones (e.g. ACTH, CRH) from the hypothalamus or pituitary that regulate steroid production in the adrenal glands adverse reaction to certain anesthesia
what are 5 S&S of malignant hyperthermia? the neuromuscular blocking agent succinylcholine is a trigger for what dangerous condition?
- muscular rigidity - tachycardia - hyperthermia - hypercapnia - red-brown urine malignant hyperthermia
blood test results for malignant hyperthermia would reveal: what is autonomic dysreflexia?
what are S&S of autonomic dysreflexia?
- high K+, P, CK, & myoglobin - low Ca++ - acidosis a medical emergency characterized by a massive SYMPATHETIC discharge that can occur in association with spinal cord injury or disease (e.g. MS) - high BP (often >200) - intense headaches - profuse sweating - feeling of doom - goosebumps - nasal stuffiness - facial erythema True. False. It should be completed within 72 hours. Some can be stored for longer. surgical removal is too invasive and may increase intrathoracic pressure, which worsens the superior vena cava syndrome. chemo does not shrink size of tumor, it only halts the growth. - hypovolemia (low volume) - hypoxia (low oxygen) - hydrogen ion excess (acidosis) - hyper-/hypo-kalemia (high/low K+) - hypothermia (low body temp) - taking drugs (overdose) - tamponade (cardiac) - tension pneumothorax (oneway valve in pleural cavity) - thrombosis (pulmonary) - thrombosis (coronary
T/F. aluminum overload causes constipation. T/F. Organ donation must be completed within 24 hours of patient death. Why is surgical removal of breast cancer tumor not suggested in case of superior vena cava syndrome? Why is chemotherapy not used in the case of superior vena cava syndrome caused by breast cancer tumor?
10 most common causes of Pulseless Electrical Activity (PEA):
Вам также может понравиться
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОт EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОценок пока нет
- Gi NclexДокумент14 страницGi NclexYoke W Khoo100% (3)
- Med Surg ReviewДокумент6 страницMed Surg ReviewSabhi Sandhu75% (4)
- MedSurg Ch30-31Документ8 страницMedSurg Ch30-31Vanessa Da Cruz100% (1)
- Answers and Rationales For NCLEX Style Review QuestionsДокумент12 страницAnswers and Rationales For NCLEX Style Review QuestionsJacinth Florido Fedelin50% (2)
- Quiz 2-Med Surg-Final Review QuestionsДокумент4 страницыQuiz 2-Med Surg-Final Review QuestionsSarah Blockno100% (2)
- Med SurgTest2Документ17 страницMed SurgTest2Becca Sanborn100% (2)
- Medical-Surgical Nursing Exam 3 (50 Items)Документ5 страницMedical-Surgical Nursing Exam 3 (50 Items)lovely_omega100% (1)
- NCLEX Exam Cardiovascular Surgery CareДокумент5 страницNCLEX Exam Cardiovascular Surgery CareHeather ClemonsОценок пока нет
- Med SurgДокумент179 страницMed Surgvinwaleed100% (1)
- NCLEX Practice QuestionsДокумент12 страницNCLEX Practice QuestionsDane WrightОценок пока нет
- Med Surg BulletsДокумент35 страницMed Surg Bulletscfournier1982Оценок пока нет
- MedSurg3 Test ReviewДокумент30 страницMedSurg3 Test ReviewAntonella Vitale100% (3)
- Advanced Med Surg Final Part 2 Everything ElseДокумент25 страницAdvanced Med Surg Final Part 2 Everything Elsejenn1722100% (1)
- Mnemonic SДокумент38 страницMnemonic Sjuel_navarroОценок пока нет
- Cardiovascular Medications NCLEX Practice QuizДокумент8 страницCardiovascular Medications NCLEX Practice QuizAngie MandeoyaОценок пока нет
- Compiled Nclex Tips and QuestionsДокумент99 страницCompiled Nclex Tips and QuestionsPaolo Balon100% (2)
- Med SurgДокумент82 страницыMed SurgRam Nik100% (4)
- MS HESI Study GuideДокумент6 страницMS HESI Study Guidejustjesko0l100% (3)
- Med SurgДокумент38 страницMed SurgEm Israel Jr.Оценок пока нет
- Medsurg ATIДокумент7 страницMedsurg ATIloveoverpride12% (17)
- Diabetes Med Surg Questions 1Документ6 страницDiabetes Med Surg Questions 1Trish Hồ0% (1)
- Nclex ExamДокумент47 страницNclex Examdamn-regret-1955Оценок пока нет
- MedSurg Medication Study Guide Test 1Документ12 страницMedSurg Medication Study Guide Test 1Sarah PlunkettОценок пока нет
- NCLEX Study MaterialДокумент40 страницNCLEX Study MaterialChristie GerconОценок пока нет
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 18Документ8 страницMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 18sarasjunk100% (1)
- Med Surg Study GuideДокумент27 страницMed Surg Study Guidetrifecta31Оценок пока нет
- NCLEXДокумент3 страницыNCLEXEternity RealОценок пока нет
- Select All That ApplyДокумент10 страницSelect All That ApplyJohnasse Sebastian NavalОценок пока нет
- GoodДокумент21 страницаGoodVanessaMUeller80% (5)
- Med Surg QuestionsДокумент62 страницыMed Surg QuestionsClarissa LurisseОценок пока нет
- Compressive Ati PDFДокумент9 страницCompressive Ati PDFsarahjaimeeОценок пока нет
- Med-Surg LEWIS 47 Final Foofed UpДокумент10 страницMed-Surg LEWIS 47 Final Foofed Uphariniliaankhen100% (1)
- ReMar Nurse University 2020 (VT) Student WorkbookДокумент50 страницReMar Nurse University 2020 (VT) Student WorkbookAnderson AlfredОценок пока нет
- Nursing-Exam-Questions-12-AR 2Документ122 страницыNursing-Exam-Questions-12-AR 2Cristel Estampador-AlcedoОценок пока нет
- Ncle X Test BankДокумент26 страницNcle X Test BankSuperDinoRedzОценок пока нет
- Exam1 100731100921 Phpapp02Документ34 страницыExam1 100731100921 Phpapp02Yaj CruzadaОценок пока нет
- Med-Surg Final Exam Study Guide Fall 2010Документ3 страницыMed-Surg Final Exam Study Guide Fall 2010Lynn Suening100% (1)
- Uworld PedsДокумент5 страницUworld PedsRubens Lazarus100% (1)
- Pedia NotesДокумент7 страницPedia NotesFreeNursingNotes100% (1)
- Blue Print Final Class Med Surg IIДокумент9 страницBlue Print Final Class Med Surg IIbaconhater100% (1)
- Nclex NCSBNДокумент6 страницNclex NCSBNNadim Khalid100% (1)
- Nclex Study GuideДокумент35 страницNclex Study Guideapi-238869635100% (3)
- Nclex Question ExamplesДокумент4 страницыNclex Question Examplesmissy23pap100% (1)
- Endocrine Nclex QuestionsДокумент9 страницEndocrine Nclex QuestionsTiffany Fain Noles100% (1)
- Janeth Cardiovascular ExamДокумент10 страницJaneth Cardiovascular ExammatthewandmaverickjeОценок пока нет
- ATI MedSurg BДокумент5 страницATI MedSurg BHeidi Monsalud100% (6)
- HESI PsyДокумент16 страницHESI PsyKrista Howe100% (14)
- Med Surge 2 Mod 3 Study Guide2Документ21 страницаMed Surge 2 Mod 3 Study Guide2Dirk Buckner100% (4)
- Elsiver NCLEX Critical CareДокумент112 страницElsiver NCLEX Critical CareHasan A AsFour100% (1)
- RNДокумент16 страницRNrunnermn100% (1)
- View AnswersДокумент4 страницыView AnswersFaith Levi Alecha AlferezОценок пока нет
- NCLEXДокумент10 страницNCLEXApril Kirstin ChuaОценок пока нет
- Lewis: Medical-Surgical Nursing, 7th Edition: Comprehensive GlossaryДокумент49 страницLewis: Medical-Surgical Nursing, 7th Edition: Comprehensive Glossarylani50% (2)
- NCLEX Study GuideДокумент2 страницыNCLEX Study GuideLogin Nurse100% (1)
- Medical Surgical Nursing Nclex Questions Integu2Документ12 страницMedical Surgical Nursing Nclex Questions Integu2dee_day_8100% (2)
- Answer KeysДокумент3 страницыAnswer Keysmaryannrichelle100% (2)
- GlaucomaДокумент26 страницGlaucomaFree Escort Service100% (1)
- Lap SC Agst 2018 DaisyДокумент294 страницыLap SC Agst 2018 DaisynitaОценок пока нет
- Drug Study ParacetamolДокумент1 страницаDrug Study ParacetamolIris BalinoОценок пока нет
- Kisu Eee NaДокумент712 страницKisu Eee Naistiahmed100% (1)
- Pathognomonic SignsДокумент12 страницPathognomonic Signsclarice_jimenezОценок пока нет
- Mock 1 Part B 26 - 8 - 2020 PDFДокумент12 страницMock 1 Part B 26 - 8 - 2020 PDFMakeesh NarayanОценок пока нет
- CombiflamДокумент1 страницаCombiflamRameshОценок пока нет
- Elsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Документ160 страницElsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Emad AdelОценок пока нет
- Aminophylline GuidelinesДокумент2 страницыAminophylline GuidelinesA. Shamshir A. MoktiОценок пока нет
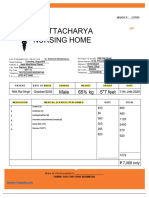
- Medical BillДокумент1 страницаMedical BillRitik Raj SinghОценок пока нет
- Clotrimazole PDFДокумент2 страницыClotrimazole PDFshajahanputhusseriОценок пока нет
- DIFFERENTIALS and MnemonicsДокумент20 страницDIFFERENTIALS and MnemonicsqurbanОценок пока нет
- Community OphthalmologyДокумент28 страницCommunity Ophthalmologynonawita0% (1)
- Bali Mandara Eye Hospital Eye Policlinic Weekly Report: 9 September 2019 - TOTAL: 207 CasesДокумент23 страницыBali Mandara Eye Hospital Eye Policlinic Weekly Report: 9 September 2019 - TOTAL: 207 CasesLipo DuoОценок пока нет
- Hyper Cvad NHLhiДокумент6 страницHyper Cvad NHLhisevag002816Оценок пока нет
- DX - Icd10Документ25 страницDX - Icd10Panji BramОценок пока нет
- K - 7 Supraventrikular Takikardia (IKA)Документ12 страницK - 7 Supraventrikular Takikardia (IKA)thomasfelixОценок пока нет
- Antifungal PDFДокумент3 страницыAntifungal PDFFaten SarhanОценок пока нет
- Pre-Employment Physical FormДокумент1 страницаPre-Employment Physical FormKarthik SОценок пока нет
- Write Cure Codes On Your Arms and Save Yourself From Incurable DiseaseДокумент3 страницыWrite Cure Codes On Your Arms and Save Yourself From Incurable DiseaseZindagiDee100% (1)
- Chronic Suppurative Otitis MediaДокумент6 страницChronic Suppurative Otitis MediaSuhas IngaleОценок пока нет
- Folic AcidДокумент1 страницаFolic Acidhazelnutski88% (8)
- Homeopathy Doctors Online ConsultationДокумент16 страницHomeopathy Doctors Online ConsultationKrishna PrasadОценок пока нет
- Intussusception Intussusception: - Repeated Crampy Belly Pain - Vomiting - Drowsiness - Passing of Currant Jelly StoolДокумент5 страницIntussusception Intussusception: - Repeated Crampy Belly Pain - Vomiting - Drowsiness - Passing of Currant Jelly StoolJustine CagatanОценок пока нет
- Dermatological HistoryДокумент5 страницDermatological HistoryßađreddińßekОценок пока нет
- Jadelle: What Is in This LeafletДокумент9 страницJadelle: What Is in This LeafletsadiaОценок пока нет
- Drug Study FinalsДокумент4 страницыDrug Study FinalsKathleen Dela CruzОценок пока нет
- ACS FianlДокумент72 страницыACS FianlmawardikaОценок пока нет
- ราคาอ้างอิงของยา เดือนมกราคม-มีนาคม 2561Документ143 страницыราคาอ้างอิงของยา เดือนมกราคม-มีนาคม 2561Tommy PanyaratОценок пока нет