Академический Документы
Профессиональный Документы
Культура Документы
Antibiotic Prophylaxis
Загружено:
Sadia GullИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Antibiotic Prophylaxis
Загружено:
Sadia GullАвторское право:
Доступные форматы
CDA Position on
Antibiotic Prophylaxis for Dental Patients at Risk
Certain categories of invasive dental treatment are known to produce significant bacteremias. Such bacteremias, although transient, may be detrimental to the health of patients with a variety of medically compromising conditions and pretreatment antibiotic prophylaxis may be indicated. Although the need to provide such chemoprophylaxis for patients with certain cardiac conditions is well known among dental practitioners, there are many other medically compromising conditions for which antibiotic prophylaxis may be appropriate. Antibiotic chemoprophylaxis prior to such dental treatment is appropriate for these selected patients. These recommendations are based upon a variety of in vitro studies, clinical experience, animal model data and an assessment of the common oral flora most likely to cause potential bacteremias. Definitive patient risk/benefit ratios for these prophylactic procedures have not been determined nor have they been medically or scientifically proven to be effective by welldesigned controlled human trials (with or without randomization). Dental procedures which may produce significant bacteremias include all procedures where significant oral bleeding and/or exposure to potentially contaminated tissue is anticipated. These procedures may include, but are not limited to, dental extractions and other oral surgery, subgingival scaling and the sub-gingival placement of dental dam clamps, restorations or orthodontic bands. Such procedures would typically require antibiotic prophylaxis in patients at risk. Simple adjustment of orthodontic appliances, tooth brushing or spontaneous loss of primary teeth do not require antibiotic prophylaxis. Patients at risk would include those with cardiac deformities, those with artificial devices in the circulatory system, and those with immunocompromising conditions (see Table 1). Patients with cardiac deformities should receive antibiotic prophylaxis according to the current guidelines of the American Heart Association (see Table 2). Consultation with the patient s physician may be required. Patients with artificial devices in the circulatory system should receive antibiotic prophylaxis using the current protocols of the American Heart Association. Such patients would include, but not be limited to, those with heart valve replacement including bioprosthetic and homograft valves, recent surgical repairs of cardiovascular defects within the past six months, and indwelling shunts or conduits (such as patients with indwelling central lines or vascular access catheters, such as Port-a-caths, for cancer chemotherapy, ventriculoarterial or ventriculovenus shunts for hydrocephalus and arteriovenus shunts for hemodialysis). Consultation with the patientphysician may be required. s
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
CDA Position on Antibiotic Prophylaxis for Dental Patients at Risk
Page 2 of 6
Patients with a variety of immunocompromising conditions should receive antibiotic prophylaxis using the current protocols of the American Heart Association. Such patients would include, but not be limited to, those with a suppressed leukocyte count (such as cancer chemotherapy, AIDS, blood dyscrasias, transplant recipients) where the white blood cell count (WBC) is less than 3500 cells/mm3 (3.5 K/mm3) or the absolute neutrophil count (ANC) is less than 500 cells/mm3 (0.5 K/mm3). Consideration for antibiotic prophylaxis should be given for other patients with an impaired immune system or those with delayed healing, such as those with, but not limited to, previous radiation therapy where planned extractions or other bony surgery is in the radiation field, an ANC less than 1000 cells/mm3 (1.0 K/mm3), uncontrolled diabetes, systemic lupus erythematosus and infection drug users. Consideration should be given for longer antibiotic prophylaxis schedules (seven to ten days or longer) for those patients where delayed healing following invasive procedures would further expose them to ongoing bacteremias. Consultation with the patientphysician may be required. s The CDA concurs with the position of the American Dental Association regarding antibiotic prophylaxis for dental patients with total joint replacement. In their advisory statement, the American Academy of Orthopaedic Surgeons and the American Dental Association have recommended the use of prophylactic antibiotics only for patients with total joint replacement (not for patients with only pins, screws, and/or plates), compromised immune system, Type I diabetes mellitus, recent (within two years) joint replacement, previous prosthetic joint infection, malnourishment or hemophilia. Consultation with the patientorthopedic surgeon may be s required. Conditions which generally do not require antibiotic prophylaxis would include, but not be limited to, physiologic, functional or innocent murmurs, a history of rheumatic fever without residual clinical heart disease, uncomplicated secundum atrial septal defect, mitral valve prolapse without mitral insufficiency, regurgitation or a murmur, coronary artery stenosis, cardiac pacemakers, atherosclerotic heart disease, well-controlled diabetes, immunocompromising conditions without decreased WBC or ANC, sickle cell anemia, cystic fibrosis or other simple orthopedic metallic devices. Consultation with the patientphysician may be required. s Patients at risk requiring antibiotic prophylaxis who are already receiving an antibiotic for a preexisting condition should receive an antibiotic for prophylaxis from a different classification. For example, a patient at risk already receiving penicillin for some other condition should receive another antibiotic for prophylaxis, such as clindamycin. Patients at risk should establish and maintain the best possible oral health to reduce potential sources of bacterial infection. Every attempt should be made to reduce gingival inflammation in patients at risk by means of brushing, flossing, topical fluoride therapy, antimicrobial rinses and professional cleaning before proceeding with routine dental treatment.
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
CDA Position on Antibiotic Prophylaxis for Dental Patients at Risk
Page 3 of 6
In order to help prevent the development of resistant strains, antibiotics should not be used indiscriminately. Complications associated with the use of antibiotics include toxic and allergic reactions, superinfections and the development of resistant organisms. It is essential that practitioners be well informed about the actions and reactions of any drugs they prescribe or administer and be prepared to handle any reasonably foreseeable complication, including anaphylaxis. Health care professionals are ultimately responsible for their own treatment decisions.
Approved CDA Board of Directors February 2005
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
CDA Position on Antibiotic Prophylaxis for Dental Patients at Risk
Page 4 of 6
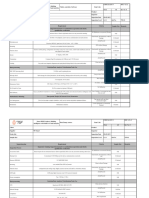
TABLE 1 ANTIBIOTIC PROPHYLAXIS FOR DENTAL PATIENTS AT RISK Conditions for which antibiotic prophylaxis is RECOMMENDED: Previous episode of infective bacterial endocarditis Heart valve replacement, including bioprosthetic and homograft valves Recent surgical repair of cardiovascular defects within the past six months Surgical systemic to pulmonary artery shunts or conduits Rheumatic heart disease or other acquired heart disease Mitral or aortic valvulitis Hypertrophic cardiomyopathy Congenital heart disease: Ventricular septal defects (unrepaired) Patent ductus arteriosus Coarctation of the aorta Tricuspid valve disease Asymmetric septal hypertrophy Tetralogy of Fallot Aortic stenosis Pulmonic stenosis Complex cyanotic heart disease Single ventrical states Transposition of the great arteries Bicuspid aortic valve Idiopathic hypertrophic subaortic stenosis (IHSS) Indwelling vascular catheter (such as Port-a-caths) Renal dialysis with arteriovenus shunt appliance Mitral valve prolapse (MVP) with mitral insufficiency, regurgitation, thickened leaflets and/or holosystolic murmur Post-mitral valve surgery Ventriculoatrial (VA) shunts for hydrocephalus Ventriculovenus (VV) shunts for hydrocephalus Immunocompromised patients where the WBC is 3500 cells/mm3 (3.5K/mm3) or less, or the ANC is 500 cells/mm3 (0.5 K/mm3) or less: Cancer chemotherapy AIDS Blood dyscrasias Transplant recipients (including organ transplants, bone marrow transplants and stem cell transplants)
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
CDA Position on Antibiotic Prophylaxis for Dental Patients at Risk
Page 5 of 6
Conditions for which antibiotic prophylaxis should be CONSIDERED:
Extractions or bony surgery planned in previous radiation field Immunocompromised patients where ANC is 1000 cells/mm3 (1.0 K/mm3) or less First two years following joint replacement in patients with immunocompromising conditions Uncontrolled or poorly controlled diabetes Systemic lupus erythematosus Injection drug users Longer antibiotic prophylaxis schedules should be considered for: Extractions or bony surgery planned in previous radiation field Uncontrolled or poorly controlled diabetes Cancer chemotherapy
Conditions for which antibiotic prophylaxis is NOT RECOMMENDED:
Physiologic, functional or innocent murmurs History of rheumatic fever without clinical heart disease Uncomplicated secundum atrial septal defect Mitral valve prolapse (MVP) without mitral insufficiency, regurgitation or a murmur Coronary artery stenosis Cardiac pacemaker Atherosclerotic heart disease Swan-Ganz catheter Well-controlled diabetes Immunocompromised patients with the ANC of 1000 cells/mm3 (1.0K/mm3) or greater Six months or longer after surgery for: Coronary artery bypass graft (CABG) Ligated patent ductus arteriosus Vascular grafts (autogenous) Surgically closed atrial or ventricular septal defects (without Dacron patches) In the absence of associated heart disease: Sickle cell anemia Cystic fibrosis Simple orthopedic metallic devices, including pins and plates
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
CDA Position on Antibiotic Prophylaxis for Dental Patients at Risk
Page 6 of 6
TABLE 2
ANTIBIOTIC PROPHYLACTIC REGIMENS FOR CERTAIN DENTAL PROCEDURES ANTIBIOTIC Amoxicillin REGIMEN Adults, 2.0 grams; Children, 50 milligrams/ kilogram orally one hour before procedure Adults, 2.0 g IM or IV ; Children, 50 mg/kg IM or IV within 30 minutes before procedure Adults, 600 mg; Children, 20 mg/kg orally one hour before procedure Adults, 2.0 g; Children, 50 mg/kg orally one hour before procedure Adults, 500 mg; Children, 15 mg/kg orally one hour before procedure Adults, 600 mg; Children, 15 mg/kg IV one hour before procedure Adults, 1.0 g; Children, 25 mg/kg IM or IV within 30 minutes before procedure
SITUATION Standard prophylaxis
Cannot use oral medications
Ampicillin
Allergic to penicillin
Clindamycin
Cephalexin or cefadroxil
Azithromycin or Clarithromycin Allergic to penicillin and unable to take oral medications Clindamycin
Cefazolin
Cephalosporins should not be used in patients with immediate-type hypersensitivity reaction (urticaria, angioedeman or anaphylaxis) to penicillins. Total childrendose should not exceed adult dose. s IM: intramuscular; IV: intravenous
These guidelines have been adapted with permission from the American Academy of Pediatric Dentistry Reference Manual 1996-1997, Antibiotic Chemoprophylaxis for Pediatric Dental Patients at Risk.
This information was created by the Canadian Dental Association for use by CDA member dentists. It should not be used as a replacement for professional dental or medical advice. If you have questions about this position statement, please consult your dentist or contact the Canadian Dental Association.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Information Security Master PlanДокумент6 страницInformation Security Master PlanMarubadi Rudra Shylesh Kumar100% (2)
- The A Etiology, Diagnosis and Management of Mandibular AsymmetryДокумент9 страницThe A Etiology, Diagnosis and Management of Mandibular AsymmetryLeonardo LamimОценок пока нет
- Assessment of Bleeding RiskДокумент25 страницAssessment of Bleeding RiskSadia GullОценок пока нет
- Alveolar Repair in AdultsДокумент17 страницAlveolar Repair in AdultsSadia GullОценок пока нет
- Comparison of Oral Versus Sub Lingual Piroxicam During Postoperative Pain Management After Lower Third Molar ExtractionДокумент6 страницComparison of Oral Versus Sub Lingual Piroxicam During Postoperative Pain Management After Lower Third Molar ExtractionSadia GullОценок пока нет
- Double-Skin Paddle RadialДокумент8 страницDouble-Skin Paddle RadialSadia GullОценок пока нет
- Diagnostic and SurgicalДокумент17 страницDiagnostic and SurgicalSadia Gull100% (1)
- Bicoronal Flap and InterpositionalДокумент4 страницыBicoronal Flap and InterpositionalSadia GullОценок пока нет
- Facial ParalysisДокумент4 страницыFacial ParalysisSadia GullОценок пока нет
- Adenoid Cystic CarcinomaДокумент4 страницыAdenoid Cystic CarcinomaSadia GullОценок пока нет
- Carotid EndartectomyДокумент5 страницCarotid EndartectomySadia GullОценок пока нет
- Carotid Cavernous FistulaДокумент3 страницыCarotid Cavernous FistulaSadia GullОценок пока нет
- Effects of Molar Tooth InvolvementДокумент4 страницыEffects of Molar Tooth InvolvementSadia GullОценок пока нет
- Cases of CherubismДокумент7 страницCases of CherubismSadia GullОценок пока нет
- "Hybrid" Lesion ofДокумент6 страниц"Hybrid" Lesion ofSadia GullОценок пока нет
- Palatal ApproachДокумент5 страницPalatal ApproachSadia GullОценок пока нет
- Palatal ApproachДокумент5 страницPalatal ApproachSadia GullОценок пока нет
- Post Op FeverДокумент6 страницPost Op FeverGiven MailaОценок пока нет
- Ablation For Pediatric PatientsДокумент5 страницAblation For Pediatric PatientsSadia GullОценок пока нет
- Cardioverter DefibrillatorДокумент3 страницыCardioverter DefibrillatorSadia GullОценок пока нет
- "Envelope" ApproachДокумент5 страниц"Envelope" ApproachSadia GullОценок пока нет
- Mastering American EnglishДокумент120 страницMastering American Englishmarharnwe80% (10)
- CA Level 2Документ50 страницCA Level 2Cikya ComelОценок пока нет
- Aluminium PasteДокумент11 страницAluminium PasteGovindanayagi PattabiramanОценок пока нет
- Quality Assurance Plan - CivilДокумент11 страницQuality Assurance Plan - CivilDeviPrasadNathОценок пока нет
- Suggestions On How To Prepare The PortfolioДокумент2 страницыSuggestions On How To Prepare The PortfolioPeter Pitas DalocdocОценок пока нет
- Rules of Bursa Malaysia Securities Clearing 2019Документ11 страницRules of Bursa Malaysia Securities Clearing 2019Evelyn SeethaОценок пока нет
- ASHRAE Final Operating Room 508 PDFДокумент13 страницASHRAE Final Operating Room 508 PDFSilisteanu AndreiОценок пока нет
- Preboard Practice PDFДокумент25 страницPreboard Practice PDFGracielle NebresОценок пока нет
- Project Success - Stakeholders 1 PDFДокумент7 страницProject Success - Stakeholders 1 PDFMoataz SadaqahОценок пока нет
- July 2014Документ56 страницJuly 2014Gas, Oil & Mining Contractor MagazineОценок пока нет
- STAB 2009 s03-p1Документ16 страницSTAB 2009 s03-p1Petre TofanОценок пока нет
- Dr. Babasaheb Ambedkar Technological UniversityДокумент3 страницыDr. Babasaheb Ambedkar Technological UniversityalfajОценок пока нет
- A Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiesДокумент21 страницаA Mini-Review On New Developments in Nanocarriers and Polymers For Ophthalmic Drug Delivery StrategiestrongndОценок пока нет
- Description About Moon: Earth SatelliteДокумент6 страницDescription About Moon: Earth SatellitePurva KhatriОценок пока нет
- SOLVING THE STEADY STATE SOLVER AND UNSTEADY or TRANSIENT SOLVER 2D HEAT CONDUCTION PROBLEM BY USINGДокумент3 страницыSOLVING THE STEADY STATE SOLVER AND UNSTEADY or TRANSIENT SOLVER 2D HEAT CONDUCTION PROBLEM BY USINGGodwin LarryОценок пока нет
- Case Studies InterviewДокумент7 страницCase Studies Interviewxuyq_richard8867100% (2)
- Project Report On HeritageДокумент39 страницProject Report On HeritageBALA YOGESH YANDAMURIОценок пока нет
- A Meta Analysis of The Relative Contribution of Leadership Styles To Followers Mental HealthДокумент18 страницA Meta Analysis of The Relative Contribution of Leadership Styles To Followers Mental HealthOnii ChanОценок пока нет
- Using MonteCarlo Simulation To Mitigate The Risk of Project Cost OverrunsДокумент8 страницUsing MonteCarlo Simulation To Mitigate The Risk of Project Cost OverrunsJancarlo Mendoza MartínezОценок пока нет
- Quality Assurance Plan-75FДокумент3 страницыQuality Assurance Plan-75Fmohamad chaudhariОценок пока нет
- - Анализ текста The happy man для ФЛиС ЮФУ, Аракин, 3 курсДокумент2 страницы- Анализ текста The happy man для ФЛиС ЮФУ, Аракин, 3 курсJimmy KarashОценок пока нет
- Matter Around Me: SC1 - Teaching Science in ElementaryДокумент27 страницMatter Around Me: SC1 - Teaching Science in ElementaryYanna Marie Porlucas Macaraeg50% (2)
- Smashing HTML5 (Smashing Magazine Book Series)Документ371 страницаSmashing HTML5 (Smashing Magazine Book Series)tommannanchery211Оценок пока нет
- ZyLAB EDiscovery 3.11 What's New ManualДокумент32 страницыZyLAB EDiscovery 3.11 What's New ManualyawahabОценок пока нет
- Ethics FinalsДокумент22 страницыEthics FinalsEll VОценок пока нет
- Growth Kinetic Models For Microalgae Cultivation A ReviewДокумент16 страницGrowth Kinetic Models For Microalgae Cultivation A ReviewJesús Eduardo De la CruzОценок пока нет
- SSC 211 ED Activity 4.1Документ4 страницыSSC 211 ED Activity 4.1bernard bulloОценок пока нет
- JLPT Application Form Method-December 2023Документ3 страницыJLPT Application Form Method-December 2023Sajiri KamatОценок пока нет
- Demand, Supply, and Market EquilibriumДокумент15 страницDemand, Supply, and Market EquilibriumAnonymous HBQ86kОценок пока нет