Академический Документы
Профессиональный Документы
Культура Документы
Steroids
Загружено:
drtasnim993Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Steroids
Загружено:
drtasnim993Авторское право:
Доступные форматы
1
Therapeutics Update - Steroids Gary E. Oliver, O.D., F.A.A.O.
I.
General Steroid Pharmacokinetics A. B. C. D. E. Steroids are synthetic glucocorticoids designed to produce similar antiinflammatory effects to endogenous glucocorticoids secreted by adrenal cortex Inhibit prostaglandin production Block enzyme phospholipase A2 Inhibit chemotaxic agents - prostaglandins, thromboxanes, leukotrienes, etc. Prevent mast cell degranulation
II.
Ocular Steroid Pharmacologic Effects A. B. C. D. E. F. G. H. I. Reduce capillary permeability Reduce cellular infiltration & exudation Suppress macrophage and neutrophil migration Inhibit fibroblast activity Inhibit mast cell degranulation Reduce overall quantity of inflammatory mediators Inhibit production of inflammatory mediators - prostaglandins, thromboxanes, leukotrienes, etc. Suppress lymphocyte proliferation Inhibit cell-mediated immune response (T-cells greater than B-cells)
III.
General Therapy Considerations and Principles A. B. C. D. E. F. G. H. I. J. Assess risks/benefits/alternatives before treatment Treatment is nonspecific Treatment goal - rapid reduction of inflammation Ocular treatment goal - prevent vision threatening complications Type and location of inflammation determines proper route of administration 1. Topical vs. systemic treatment Type and clinical severity of inflammation determines the appropriate dosage Clinical severity determines the appropriate dosage Initial dose should be adequate to suppress the inflammatory process Steroid dosage regulated by both the drug concentration and application frequency Steroid formulation indicated is determined by the inflammation site and need for 1
K. L.
tissue penetration May need to treat aggressively, particularly anterior uveitis Pulse vs. standard dosing techniques
IV.
Steroid Dosage Protocols A. Pulse dose 1. Effective for type I or IV hypersensitivity reactions and traumatic iridocyclitis 2. High initial dose followed by immediate, rapid taper of steroid 3. Short therapeutic course (typically 5-7 days) Standard dose 1. Effective for most inflammatory processes including uveitis, systemic disease related inflammation, or other more complex inflammatory reactions 2. Initial dose dependent upon severity of inflammation 3. Initial dose maintained for minimum of 72 hours, monitor for clinical improvement 4. Continue initial dose for 3-4 days after clinical improvement is noted 5. Taper steroid in step down fashion over several weeks
B.
V.
Ocular Steroid Therapy Principles A. B. C. D. E. F. Steroid dosage regulated by both drug concentration and application frequency Steroid formulation determined by inflammation site and need for tissue penetration Normal vs. inflamed tissue Always continue therapy for 3-4 days after signs and symptoms begin to resolve Always taper steroids Steroid tapering techniques 1. Reduce frequency of steroid dose 2. Reduce steroid concentration of initial medication 3. Adjust steroid potency by changing medications 4. Consider nonsteroidal anti-inflammatory agent for long term tapering Role of NSAIDS for treatment of ocular inflammation 1. Generally not as potent or as clinically effective as steroids for reduction of ocular inflammation 2. May be useful for long term tapering of anti-inflammatory agents
G.
VI.
Adverse Effects from Topical Ocular Steroid Therapy 2
A. B. C. D. E. F. G.
Elevation of intraocular pressure Secondary or reactivation of infection Masking of clinical signs Delayed wound healing Transient discomfort - burning, stinging Dry eye syndrome Posterior subcapsular cataract
VII.
Contraindications for Topical Ocular Steroids A. B. Presence of active infection examples may include bacterial disease, corneal ulcer, Herpes simplex Steroid responders use with caution, use steroid with less risk of increasing intraocular pressure, monitor IOP carefully, may need concurrent IOP lowering medication
VIII. Topical Steroid Agents A. B. C. D. E. F. G. 0.125%-1% prednisolone acetate 0.125%-1% prednisolone phosphate 0.1% fluorometholone acetate 0.1% fluorometholone alcohol 0.2%-0.5% loteprednol etabonate 1% rimexolone 0.1% dexamethasone alcohol
IX.
Steroid Efficacy A. B. C. Potency of agent Tissue penetration of agent Dosage
X.
Relative Steroid Anti-Inflammatory Activity A. Steroid Potency - decrease in inflammation after 48 hours of therapy 3
B.
C.
1% prednisolone acetate 51% 0.1% dexamethasone alcohol 40% 0.1.% fluorometholone acetate 31% 1% rimexolone, 0.5.% loteprednol may be equivalent to 1% prednisolone acetate but dosage considerations are important Steroid Dosage - decrease in inflammation after 48 hours of therapy with 1% prednisolone acetate one drop q1h 51% one drop q2h 30% one drop q4h 11% Treatment Protocols 1. External disease - minimal initial dose typically q4h 2. Anterior uveitis - minimal initial dose typically q2h
XI. Clinical Management Pearls A. Have an expected time frame for resolution of inflammation 1. External disease - expect improved symptoms in 24-48 hours, clinical signs 48-96 hours depending on the clinical entity 2. Anterior uveitis - expect improved symptoms 48-72 hours, early improvement of clinical signs by one week If not responding as expected 1. Consider if diagnosis is correct 2. Question patient compliance 3. Is dosage correct, may need to increase dosage 4. Change medication 5. Referral for second opinion Mistakes in steroid therapy 1. Under-prescribing the medication 2. Can always taper, more difficult to increase dosage 3. Undertreated cases usually are more difficult to manage 5. Steroid therapy in presence of active infectious ocular disease 6. Not monitoring intraocular pressure
B.
C.
XII.
Systemic Steroid Therapy A. B. C. Indicated for very severe anterior uveitis (adjunctive therapy) Indicated for posterior uveitis, scleritis, (possibly optic neuritis) Systemic prednisone usually not necessary for anterior segment disease due to ability to build high steroid titers from topical therapy
XIII. Nonsteroidal Anti-Inflammatory Agents (NSAIDS) A. Nonsteroidal anti-inflammatory drugs are synthetic agents designed to achieve a similar anti-inflammatory effect to the endogenous glucocorticoids secreted by the adrenal cortex 1. Inhibit the production of prostaglandins by reversibly blocking the action of the enzyme cyclooxygenase in the prostaglandin pathway 2. Most have no direct effect on leukotriene production and do not prevent mast cell degranulation 3. Inhibit platelet coagulation General Pharmacological effects 1. Analgesic 2. Anti-Inflammatory 3. Antipyretic 4. Anticoagulant Ocular Pharmacological Effects Topical Therapy 1. Improves blood-aqueous barrier 2. Prevent vasodilation 3. Reduce capillary permeability 4. Prevent migration of some inflammatory mediators 5. Reduce mild to moderate pain Adverse Effects Topical Therapy 1. Transient burning or stinging 2. Secondary or reactivation of infection 3. Masking of clinical signs 4. Headache 5. Possible central nervous system effects, such as dizziness, seizures, syncope, short term memory loss, decreased attention span General Contraindications for NSAIDS usage these are systemic principles but may have implications for topical NSAIDs depending on systemic absorption from topical application 1. Upper gastrointestinal disease 2. Bronchial asthma 3. Hypersensitivity history 4. Bleeding disorders 5. Anticoagulant therapy 6. Immediate post-op period following invasive surgery 7. Chronic renal or hepatic disease 8. Congestive heart disease 9. Pregnancy
B.
C.
D.
E.
XIV. Additional Anti-Inflammatory Agents A. 0.05% cyclosporine 1. Inhibits cytokine induced inflammation 2. Inhibits some T-cell activity 3. Increases goblet cell activity 4. Promotes rejuvenation of lacrimal gland tissue which can increase tear production Adverse Effects 1. Transient burning or stinging 2. Transient blurred vision 3. Secondary or reactivation of infectious disease, i.e. Herpes simplex
B.
XV.
Clinical Grand Rounds
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Childhood Blindness NigeriaДокумент5 страницChildhood Blindness Nigeriadrtasnim993Оценок пока нет
- LENS2Документ64 страницыLENS2drtasnim993Оценок пока нет
- Lessons From The TitanicДокумент27 страницLessons From The TitanicKevin KeefeОценок пока нет
- 2009-SCI-014 Age-Related Macular Degeneration 3Документ113 страниц2009-SCI-014 Age-Related Macular Degeneration 3drtasnim993Оценок пока нет
- Io SterilizationДокумент6 страницIo Sterilizationdrtasnim993Оценок пока нет
- 2 FRCS Neuro2 2b PDFДокумент24 страницы2 FRCS Neuro2 2b PDFdrtasnim993Оценок пока нет
- 2 FRCS Neuro2 1b PDFДокумент46 страниц2 FRCS Neuro2 1b PDFdrtasnim993Оценок пока нет
- Lessons From The TitanicДокумент27 страницLessons From The TitanicKevin KeefeОценок пока нет
- 2012-SCI-247 Local Anaesthesia in Ophthalmic Surgery 2012 1Документ38 страниц2012-SCI-247 Local Anaesthesia in Ophthalmic Surgery 2012 1Agitha Melita PutriОценок пока нет
- RCA RCO Guidelines PDFДокумент24 страницыRCA RCO Guidelines PDFdrtasnim993Оценок пока нет
- Writing Practice Test 1 IELTS Academic Model AnswersДокумент2 страницыWriting Practice Test 1 IELTS Academic Model Answersmahfuz507100% (1)
- Speaking IELTSДокумент6 страницSpeaking IELTSdrtasnim993Оценок пока нет
- Ielts Reading3 PDFДокумент0 страницIelts Reading3 PDFZargham KhanОценок пока нет
- Speaking IELTSДокумент6 страницSpeaking IELTSdrtasnim993Оценок пока нет
- Splendid Speaking Podcasts: Topic: Making Your Talks Topical (Interview 25: May Archives)Документ6 страницSplendid Speaking Podcasts: Topic: Making Your Talks Topical (Interview 25: May Archives)drtasnim993Оценок пока нет
- Holiday Barchart in UK1Документ3 страницыHoliday Barchart in UK1Wardah Tariq MalikОценок пока нет
- Exercise 1: Looking For Information at SpeedДокумент17 страницExercise 1: Looking For Information at SpeedtruongthikhaОценок пока нет
- IELTS Sample Writing Academic Task 2 6Документ3 страницыIELTS Sample Writing Academic Task 2 6Adei Srue AdeiОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- Ecg Notes RetdemДокумент2 страницыEcg Notes RetdemJerica Mae VenoyaОценок пока нет
- 03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Документ2 страницы03 Orlando D. Garcia, JR., Et Al. vs. Ranida Salvador, Et Al.Raj AtmanОценок пока нет
- Study of Lipid Profile in Coronary Heart Disease Patients in LibyaДокумент9 страницStudy of Lipid Profile in Coronary Heart Disease Patients in LibyaInternational Medical PublisherОценок пока нет
- Paul Krebaum Skunk Odor Removal RecipeДокумент2 страницыPaul Krebaum Skunk Odor Removal Recipeozzaib100% (1)
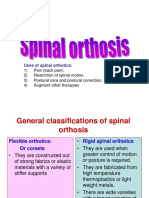
- Spinal OrthosisДокумент16 страницSpinal OrthosisChristya Ari NugrahaОценок пока нет
- ACD/Percepta: Overview of The ModulesДокумент91 страницаACD/Percepta: Overview of The ModulesTinto J AlencherryОценок пока нет
- Common Medical AbbreviationsДокумент1 страницаCommon Medical Abbreviationskedwards108Оценок пока нет
- Wyeth Laboratories - Intramuscular InjectionsДокумент36 страницWyeth Laboratories - Intramuscular InjectionsflexionОценок пока нет
- Calcium-Phosphate Metabolism: Medical Benchmarking ReportДокумент9 страницCalcium-Phosphate Metabolism: Medical Benchmarking ReportLuis Hernan Guerrero LoaizaОценок пока нет
- Palmer Ultrasound ImagingДокумент354 страницыPalmer Ultrasound ImagingRajeshPilot100% (13)
- Lay Public Stop The Bleed PresentationДокумент32 страницыLay Public Stop The Bleed PresentationCookie DooОценок пока нет
- Blood Distribution System Using Data MiningДокумент5 страницBlood Distribution System Using Data MiningRahul SharmaОценок пока нет
- Can Oral Sex Cause Throat CancerДокумент4 страницыCan Oral Sex Cause Throat CancerjyuldipОценок пока нет
- Acute Abdomen in Pediatric Patients Admitted To PDFДокумент9 страницAcute Abdomen in Pediatric Patients Admitted To PDFiwanОценок пока нет
- Appeal LetterДокумент1 страницаAppeal Letterdate6Оценок пока нет
- Msds Asam MefenamatДокумент6 страницMsds Asam MefenamatKristal Resa Diena RОценок пока нет
- Avena SativaДокумент46 страницAvena SativaJuliana VarelaОценок пока нет
- Tetracyclines: Dr. Md. Rageeb Md. Usman Associate Professor Department of PharmacognosyДокумент21 страницаTetracyclines: Dr. Md. Rageeb Md. Usman Associate Professor Department of PharmacognosyAnonymous TCbZigVqОценок пока нет
- Sport Injury DR Endang AmbarwatiДокумент44 страницыSport Injury DR Endang AmbarwatidewiulfaОценок пока нет
- Clinic Department InfoДокумент66 страницClinic Department InfoHumera ShaikhОценок пока нет
- Pharmaceutical IndustryДокумент15 страницPharmaceutical IndustrySri KanthОценок пока нет
- Aerosol TherapyДокумент25 страницAerosol TherapyMay Suchada BoonpengОценок пока нет
- The Ergot AlkaloidsДокумент9 страницThe Ergot AlkaloidsAna LucaОценок пока нет
- Levels of Organization PowerpointДокумент15 страницLevels of Organization PowerpointGloriefe QuitongОценок пока нет
- Bone Marrow BiopsyДокумент2 страницыBone Marrow BiopsySatinder SinghОценок пока нет
- Cramp Pages 1Документ10 страницCramp Pages 1masi10Оценок пока нет
- 200 Bed Hospital Project ReportДокумент59 страниц200 Bed Hospital Project ReporttonyОценок пока нет
- 2010 TFN Module Unit 06 Nursing Paradigm - NursingДокумент43 страницы2010 TFN Module Unit 06 Nursing Paradigm - NursingCamille Denise Nucum100% (1)
- Setting Fire On The MountainДокумент5 страницSetting Fire On The MountainElizabeth Durkee NeilОценок пока нет
- Psychiatric Drugs Are Neurotoxins-Power-Point-OutlineДокумент30 страницPsychiatric Drugs Are Neurotoxins-Power-Point-OutlineAugustaОценок пока нет