Академический Документы
Профессиональный Документы
Культура Документы
Articulo Neumonia
Загружено:
Ed BarajasИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Articulo Neumonia
Загружено:
Ed BarajasАвторское право:
Доступные форматы
Clinical Therapeutics/Volume 32, Number 2, 2010
Guideline-Concordant Antibiotic Use and Survival Among Patients With Community-Acquired Pneumonia Admitted to the Intensive Care Unit
Christopher R. Frei, PharmD, MSc1,2; Russell T. Attridge, PharmD1,2; Eric M. Mortensen, MD, MSc24; Marcos I. Restrepo, MD, MSc24; Yifan Yu, PharmD1,2; Christine U. Oramasionwu, PharmD, MSc1,2; Jessica L. Ruiz, RN-BSN1; and David S. Burgess, PharmD1,2
of Texas at Austin, College of Pharmacy, Austin, Texas; 2University of Texas Health Science Center at San Antonio, School of Medicine, San Antonio, Texas; 3Veterans Evidence-Based Research Dissemination Implementation Center, San Antonio, Texas; and 4South Texas Veterans Health Care System, Audie L. Murphy Division, San Antonio, Texas
AbsTrACT
Objective: This study evaluated the survival benefit of US community-acquired pneumonia (CAP) practice guidelines in the intensive care unit (ICU) setting. Methods: We conducted a retrospective cohort study of adult patients with CAP who were admitted to 5 community hospital ICUs between November 1, 1999, and April 30, 2000. The guidelines for antibiotic prescriptions were the 2007 Infectious Diseases Society of America/American Thoracic Society guidelines. Guideline-concordant antimicrobial therapy was defined as a -lactam plus fluoroquinolone or macrolide, antipseudomonal -lactam plus fluoroquinolone, or antipseudomonal -lactam plus aminoglycoside plus fluoroquinolone or macrolide. Patients with a documented -lactam allergy were considered to have received guideline-concordant therapy if they received a fluoroquinolone with or without clindamycin, or aztreonam plus fluoroquinolone with or without aminoglycoside. All other antibiotic regimens were considered to be guideline discordant. Time to clinical stability, time to oral antibiotics, length of hospital stay, and in-hospital mortality were evaluated with regression models that included the outcome as the dependent variable, guidelineconcordant antibiotic therapy as the independent variable, and the Pneumonia Severity Index (PSI) score and facility as covariates. Results: The median age of the 129 patients included in the study was 71 years (interquartile range, 6079 years). Sixty-two of 129 patients (48%) were male. Comorbidities included liver dysfunction (7 paFebruary 2010 tients [5%]), heart failure (62 [48%]), renal dysfunction (39 [30%]), cerebrovascular disease (21 [16%]), and cancer (14 [11%]). The median (25th75th percentile) PSI score was 119 (98142), and overall mortality was 19% (25 patients). Patient demographics were similar between groups. Fifty-three patients (41%) received guideline-endorsed therapies. Guideline-discordant therapy was associated with an increase in inpatient mortality (25% vs 11%; odds ratio = 2.99 [95% CI, 1.089.54]). Receipt of guideline-concordant antibiotics was not associated with reductions in time to clinical stability, time to oral antibiotics, or length of hospital stay when patients who died were excluded from the analysis. Conclusion: Guideline-concordant empiric antibiotic therapy was associated with improved survival among these patients with CAP who were admitted to 5 ICUs. (Clin Ther. 2010;32:293299) 2010 Excerpta Medica Inc. Key words: bacterial pneumonia, communityacquired pneumonia, guidelines, antibiotics, health outcomes, mortality.
This work was presented in part at the 45th Interscience Conference on Antimicrobial Agents and Chemotherapy, December 1619, 2005, Washington, DC; and at the 11th Annual International Meeting of the International Society for Pharmacoeconomics and Outcomes Research, June 2024, 2006, Philadelphia, Pennsylvania. Accepted for publication November 10, 2009. doi:10.1016/j.clinthera.2010.02.006 0149-2918/$ - see front matter 2010 Excerpta Medica Inc. All rights reserved.
1University
293
Clinical Therapeutics
iNTroduCTioN
Community-acquired pneumonia (CAP) is a common and serious illness. Pneumonia is responsible for more than 1.2 million hospitalizations annually and, in combination with influenza, is the eighth most common cause of death overall in the United States.1,2 Of patients admitted to the hospital for treatment of CAP, 9% to 26% will be admitted directly to the intensive care unit (ICU).3 Patients with CAP who are admitted to the ICU are often more severely ill, require more medical resources, and have a higher mortality rate than patients with CAP who remain in the regular hospital ward. Research based in the United States suggests that the length of hospital stay (9 vs 23 days), total hospital costs ($5700 vs $21,000), and inpatient mortality (5% vs 18%) are disproportionately greater for CAP patients admitted to the ICU than those not admitted to the ICU.3 Several clinical interventions have been associated with improved survival rates among patients with CAP, including appropriate antibiotic selection, reduced time to first antibiotic dose, blood cultures within 24 hours of admission, and oxygenation assessment.46 However, few studies have evaluated the impact of these interventions among patients with CAP in the ICU, and none has yet found that prescribing antibiotics according to recommendations set forth by national or international associations was associated with faster disease resolution or shorter time to oral antibiotics in this setting. Although antibiotic recommendations for patients in the general hospital ward have been validated in numerous investigations, recommendations for ICU patients are formed largely from expert opinion. The 2007 Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) guidelines recommend that ICU patients with CAP receive a -lactam (cefotaxime, ceftriaxone, ampicillinsulbactam, or ertapenem) plus an advanced macrolide or a -lactam plus a respiratory fluoroquinolone.7 When risk factors for Pseudomonas aeruginosa are present, the guidelines recommend an antipseudomonal -lactam plus fluoroquinolone, an antipseudomonal -lactam plus aminoglycoside plus macrolide, or an antipseudomonal -lactam plus aminoglycoside plus fluoroquinolone. If community-acquired methicillinresistant Staphylococcus aureus is a concern, vancomycin or linezolid should be added.7 The key recommendations for empiric antibiotic selection for patients with CAP who are admitted to the ICU have largely 294
remained unchanged since the 1998 and 2000 IDSA guidelines were published.8,9 With the publication of the 2007 guidelines, the only major changes in empiric therapy were the specifications of azithromycin as the macrolide of choice and 750 mg as the preferred dose of levofloxacin, as well as the removal of piperacillin/ tazobactam from the list of initial -lactam choices for patients without risk factors for Pseudomonas. Previously published studies have validated antibiotic guideline choices among patients with CAP who were admitted to medical wards and among mixed populations of patients with CAP who were admitted to medical wards and ICUs1017; however, only 1 study to date has evaluated the impact of guideline-endorsed antimicrobial choices on patients with CAP in the ICU.18 This study compares patient outcomes among patients with CAP who were admitted to the ICU and received antibiotic therapy according to accepted guidelines versus those who received therapy that did not follow guidelines.
PATieNTs ANd MeThods
This was a retrospective cohort study of all patients admitted to the ICU with CAP at 5 community hospitals within the Baptist Health System (San Antonio, Texas) from November 1, 1999, to April 30, 2000. Institutional review board approval was obtained from the Baptist Health System and the University of Texas Health Science Center at San Antonio prior to beginning the study. The study methods were similar to those used in a previous study that was limited to patients treated in the medical ward. In contrast, the present study is limited to patients treated in the ICU.19
inclusion and exclusion Criteria
We identified all adult patients admitted directly to the ICUs of the study hospitals with a principal discharge diagnosis of pneumonia (International Classification of Diseases, Ninth Revision, Clinical Modification codes 481484 and 486). Patients were excluded for the following reasons: (1) age <18 years; (2) HIV/AIDS; (3) hospitalization within the previous 7 days; (4) transfer from another hospital; or (5) active chemotherapy.
data Collection
The following information was extracted from the medical chart using a standardized data-collection form: demographics; comorbidities; antibiotic allergies; Volume 32 Number 2
C.r. Frei et al. hospital admission and discharge dates; antibiotic regimens received during hospitalization; time of entry into the system; daily vital sign measurements; daily laboratory results; oxygenation status; and radiographic findings. When multiple laboratory values or vital sign measurements were available for a given day, the most extreme value (ie, highest pulse) was recorded. The lead clinical pharmacist at the Baptist Health System verified 5% of clinical data and 100% of laboratory data by direct comparison with medical charts and laboratory reports, respectively. Severity of illness was determined in accordance with the Pneumonia Severity Index (PSI).20 All data were subsequently entered into an electronic database (Microsoft Access 2000, Microsoft Corporation, Redmond, Washington). guideline-concordant antimicrobial therapy if they received a -lactam plus fluoroquinolone or macrolide, antipseudomonal -lactam plus fluoroquinolone, or antipseudomonal -lactam plus aminoglycoside plus fluoroquinolone or macrolide. Patients with a documented -lactam allergy were considered to have received guideline-concordant therapy if they received a fluoroquinolone with or without clindamycin, or aztreonam plus fluoroquinolone with or without aminoglycoside. Patients who received all other antibiotic regimens were considered to have received guideline-discordant antibiotic therapy.
statistical Analysis
JMP 5.0 (SAS Institute Inc., Cary, North Carolina) was used for all statistical comparisons. The level for significance was P 0.05. Continuous variables were tested for normality using the Shapiro-Wilk W test. Baseline characteristics were compared using the 2 or Fisher exact test for discrete variables and the Kruskal-Wallis test for continuous variables. Time to clinical stability, time to oral antibiotics, ICU length of stay, and length of hospital stay were assessed in a Cox proportional hazards regression model; inpatient mortality was determined with a logistic regression model. In both models, the outcome was the dependent variable, guideline-concordant antibiotic therapy was the independent variable, and PSI score and facility were covariates.20 The PSI score and facility were introduced into the model first, followed by the antibiotic therapy. Patients who expired during hospitalization were excluded from the timed analyses for time to clinical stability, time to oral antibiotics, hospital length of stay, and ICU length of stay.
outcome definitions
Clinical stability was determined according to a validated rule that defined clinical stability as the first day that all 7 of the following criteria were simultaneously achieved: (1) heart rate 100 beats/min; (2) systolic blood pressure 90 mm Hg; (3) respiratory rate 24 breaths/min; (4) oxygen saturation 92% on room air; (5) temperature 99F; (6) ability to tolerate oral intake; and (7) baseline mental status.21,22 In patients noted to have altered mental status at the time of admission, a return to baseline mental status was defined as the first day after hospital admission when altered mental status was not documented or was said to have resolved. Time to clinical stability was calculated by subtracting the admission date from the first date that the patient was determined to be clinically stable. Time to oral antibiotics was calculated by subtracting the admission date from the first date that the patient received oral antibiotics. Length of ICU stay was calculated by subtracting the hospital admission date from the ICU discharge date; all patients were admitted directly to the ICU. Similarly, overall length of hospital stay was calculated by subtracting the hospital admission date from the hospital discharge date. Inpatient mortality was defined as death before hospital discharge for this CAP admission.
resulTs
A total of 129 CAP patients were admitted directly to the ICU for CAP, and 41% (53 patients) received guideline-concordant antibiotic therapy. The guidelineconcordant group was composed of patients treated with -lactam plus fluoroquinolone (24 [45%]), -lactam plus macrolide (16 [30%]), fluoroquinolone monotherapy with documented -lactam allergy (8 [15%]), antipseudomonal -lactam plus aminoglycoside plus fluoroquinolone (3 [6%]), antipseudomonal -lactam plus aminoglycoside plus macrolide (1 [2%]), or antipseudomonal -lactam plus fluoroquinolone plus aztreonam (1 [2%]). Half of the patients in the guideline-discordant group received either fluoroquino295
Guideline-Concordant and -discordant definitions
The 2007 ATS/IDSA guidelines were used to stratify CAP patients into 2 groups based on the antibiotics that they received during the first 24 hours of ICU admission.7 Patients were considered to have received February 2010
Clinical Therapeutics lone monotherapy without a documented -lactam allergy (25 [33%]) or -lactam monotherapy (11 [14%]). The next largest group was antipseudomonal -lactam plus non-antipseudomonal fluoroquinolone (10 [13%]). (If the prescriber had suspected a pseudomonal infection, then the guideline-concordant regimen would be an antipseudomonal -lactam plus an antipseudomonal fluoroquinolone [eg, ciprofloxacin or levofloxacin].) The remaining patients received 17 different regimens; no single regimen was administered to >5% of patients in the guideline-discordant group. 76 [6182] vs 69 [5779] years; P = 0.05), the 2 groups were also similar regarding severity of illness (quantified by PSI score): guideline discordant vs guideline-concordant (118 [104141] vs 122 [91 153] years; P = NS).
health Care end Points
Multivariable regression analysis indicated that nonadherence to the guidelines was independently associated with higher inpatient mortality (25% vs 11%; odds ratio [OR] [95% CI] = 2.99 [1.089.54]). Compared with guideline-discordant antibiotic therapy, guideline-concordant antibiotic therapy was associated with a 56% relative risk reduction and a 14% absolute risk reduction for inpatient mortality. Consequently, it was calculated that only 7 patients would need to be treated with guideline-concordant therapy, instead of guideline-discordant therapy, to save 1 life. Similar analyses were conducted for several secondary end points, but there were no significant associations (guideline-concordant vs guidelinediscordant values; OR [95% CI]) for median time to clinical stability (3.5 vs 3.0 days; 0.98 [0.631.54]), time to oral antibiotics (7.0 vs 7.0 days; 0.79 [0.51 1.19]), ICU length of stay (3.0 vs 2.0 days; 0.81 [0.541.21]), or length of hospital stay (8.0 vs 8.0 days;
Patient demographics
The median age of the 129 patients included in the study was 71 years (interquartile range, 6079 years). Sixty-seven patients (52%) were women. Comorbidities included liver dysfunction (7 patients [5%]), heart failure (62 [48%]), renal dysfunction (39 [30%]), cerebrovascular disease (21 [16%]), and cancer (14 [11%]). The median (25th75th percentile) PSI score was 119 (98142) (Table). Overall mortality was 19% (25 patients). Patient demographics by group (guideline concordant vs guideline discordant) were similar with respect to sex, antibiotics before admission, and comorbidities. Despite increased age in the guidelinediscordant group (median age [25th75th percentile],
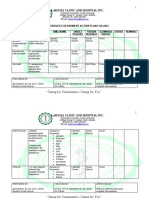
Table. Demographic characteristics of patients with community-acquired pneumonia who were admitted to 5 community hospital intensive care units between November 1, 1999, and April 30, 2000, and were initially treated with antibiotic therapy that did or did not follow the subsequently published 2007 Infectious Diseases Society of America/American Thoracic Society guidelines.7 Guideline-Concordant Antibiotics Characteristic Age, median (25th75th percentile), y Female sex, no. (%) Comorbidities, no. (%) Congestive heart failure Renal disease Cerebrovascular disease Neoplastic disease Liver disease Pneumonia Severity Index score, median (25th75th percentile)
OR = odds ratio.
Yes (n = 53) 69 (5779) 27 (51) 27 (51) 14 (26) 6 (11) 6 (11) 3 (6) 122 (91153)
No (n = 76) 76 (6182) 40 (53) 35 (46) 25 (33) 15 (20) 8 (11) 4 (5) 118 (104141)
P 0.05 0.67
OR (95% CI) 0.93 (0.461.89) 0.82 (0.411.66) 1.36 (0.632.97) 1.93 (0.695.34) 0.92 (0.302.83) 0.93 (0.204.32)
296
Volume 32 Number 2
C.r. Frei et al. 0.87 [0.571.31]). Patients lacking information for a secondary end point were not included in the analysis of that specific end point. All patients who died during hospitalization were excluded from the lengthof-ICU-stay and length-of-hospital-stay calculations (6 in the guideline-concordant group, 19 in the guideline-discordant group). For time to oral antibiotics, all 6 patients not included in the guidelineconcordant group were excluded because of death, and 19 of the 21 patients removed from the guidelinediscordant group were removed because of death. Regarding time to clinical stability, 13 patients in the guideline-concordant group and 28 patients in the guideline-discordant group were excluded; however, only 4 of the 13 patients (31%) and 10 of the 28 patients (36%) were excluded because of death. We were not able to calculate the time to clinical stability for the other 19 excluded patients because they were missing 1 daily vital sign measurement. Additionally, a sensitivity analysis was performed in which patients who died on day 1 or 2 of admission were excluded from the primary analysis. This included 1 patient from the guideline-concordant group and 2 patients from the guideline-discordant group. In this analysis, as well, guideline-discordant antibiotic therapy was associated with a greater risk of death than was guideline-concordant treatment (OR [95% CI] = 3.09 [1.0610.6]). discordant group who died; these patients might have endured longer lengths of stay if they had lived. Additionally, outcomes such as length of stay are partially dependent on hospital-specific factors such as census and occupancy rates; whereas mortality is an objective marker that is unaffected by individual facility decisions. Bod et al18 evaluated the impact of guidelineconcordant empiric therapy among CAP patients admitted to the ICU. Although the population in that study differed from the one in the present study, the study methods and findings were similar. In their prospective, multicenter, observational study, Bod et al evaluated mortality among 529 patients with CAP who were admitted to ICUs in Spain from December 1, 2000, to February 28, 2002. The authors described predictive factors for ICU admission and evaluated the impact of guideline adherence. Both studies stratified patients according to IDSA guidelines with comparable overall adherence (58% in the Bod et al study vs 40% in the present study) and utilized multivariate regression analyses; however, Bod et al used the Acute Physiology and Chronic Health Evaluation II (APACHE II) score to evaluate the severity of disease, whereas the present study used the PSI score. Both the Bod et al study and the present study concluded that nonadherence to the guidelines was independently associated with an increase in inpatient mortality: Bod et al 24% and 33% (OR [95% CI] = 1.66 [1.072.57] versus 11% and 25% (2.99 [1.08 9.54]). Although the present study provides additional evidence to support previously published studies, it is susceptible to the inherent limitations of all nonrandomized observational studies, including the inability to distribute any potential bias equally between groups. The clinical data are limited by what was recorded in the patients charts and progress notes, and the results of this study may be subject to effects of confounders that were not controlled for in regression analyses; therefore, solid conclusions regarding causality between treatment and outcomes cannot be fully ascertained. No information was collected about specific causes of death, so differences in mortality could have been the result of underlying comorbidities, medical errors, or other unknown factors. Guidelineconcordant and -discordant groups could have differed by unmeasured variables that introduced selection bias into this observational study; however, 297
disCussioN
This study evaluated the use of guideline-endorsed empiric antibiotic regimens for the treatment of CAP patients admitted to the ICU. Previously published studies found that guideline-concordant empiric antibiotic therapy was associated with improved outcomes among patients with CAP; however, many of these studies focused solely on ward patients,15,16 or they pooled ICU and ward patients collectively.1013,15,17 Two of these studies reported that guideline-concordant antibiotic therapy was associated with decreased length of stay.10,15 The remainder of these studies identified significant associations between guideline-concordant antibiotic therapy and reduced patient mortality. The present study found lower mortality rates among these patients with CAP treated in the ICU who received guideline-concordant antibiotic therapy; however, no changes were observed with regard to other measured outcomes. This finding may have been related to the exclusion of patients in the guidelineFebruary 2010
Clinical Therapeutics this may be a more accurate portrayal of real-world practices than would be observations from a controlled setting. Limited facility and physician-specific information was available, leaving us unable to account for possible differences in hospital-acquired infection rates, risk management practices, and individual physician practices including variation by day of the week or different shifts. It is also important for clinicians to consider institution- and patient-specific factors when determining the most prudent antibiotic therapy. Understanding local resistance patterns and patient risk factors is key, and strategies may differ between large urban hospitals and smaller rural hospitals or hospitals that predominantly serve younger, healthier patients. Also, given the limited sample size and scope (a single health system), additional investigation in other health systems and more diverse populations is needed. System, who assisted with data collection: Brian Barthol, PharmD; Renee Bellanger, PharmD; Donna Burgess, RPh; Paige Cuellar, PharmD; Julie Gilbert, PharmD; Jennifer Hammond, PharmD; Scott Hollis, RPh; Loretta Lemoine, RPh; Andi Lewis, PharmD; Jane Mondino, RPh; Jon Olson, PharmD; Nish Patel, PharmD; Liz Sanchez, RPh; Morris Sauter, PharmD; Thomas Shank, PharmD; Jacque Snow, PharmD; Paige Staudt, PharmD; and Mary Allyn Watson, PharmD.
reFereNCes
1. DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Hyattsville, Md: National Center for Health Statistics; 2008. National Health Statistics Report no 5. 2. Kung HC, Hoyert DL, Xu JQ, Murphy SL. Deaths: Final Data for 2005. Hyattsville, Md: National Center for Health Statistics; 2008. National Vital Statistics Reports, vol. 56, no. 10. 3. Angus DC, Marrie TJ, Obrosky DS, et al. Severe community-acquired pneumonia: Use of intensive care services and evaluation of American and British Thoracic Society Diagnostic criteria. Am J Respir Crit Care Med. 2002;166:717723. 4. Houck PM, Bratzler DW, Nsa W, et al. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. 2004;164:637644. 5. Gleason PP, Meehan TP, Fine JM, et al. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med. 1999;159:25622572. 6. Kahn KL, Rogers WH, Rubenstein LV, et al. Measuring quality of care with explicit process criteria before and after implementation of the DRG-based prospective payment system. JAMA. 1990;264:19691973. 7. Mandell LA, Wunderink RG, Anzueto A, et al, for the Infectious Diseases Society of America, American Thoracic Society. Infectious Diseases Society of America/ American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27S72. 8. Bartlett JG, Breiman RF, Mandell LA, File TM Jr, for the Infectious Diseases Society of America. Communityacquired pneumonia in adults: Guidelines for management. Clin Infect Dis. 1998;26:811838. 9. Bartlett JG, Dowell SF, Mandell LA, et al, for the Infectious Diseases Society of America. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000;31:347382. 10. Benenson R, Magalski A, Cavanaugh S, Williams E. Effects of a pneumonia clinical pathway on time to antibiotic treatment, length of stay, and mortality. Acad Emerg Med. 1999;6:12431248.
CoNClusioN
Among these patients with CAP who were admitted to 5 ICUs, antibiotic therapy that followed the 2007 ATS/IDSA guidelines was associated with improved inpatient survival.
ACkNowledGMeNTs
Dr. Frei has received research grants from OrthoMcNeil Janssen, Elan, AstraZeneca, Abbott, Merck, Roche, and Wyeth, and has served as a consultant and advisory-board member for Ortho-McNeil Janssen. Dr. Restrepo has served on speakers bureaus for Ortho-McNeil Janssen, Johnson & Johnson, and Pfizer, and on advisory boards for Ortho-McNeil Janssen and Johnson & Johnson. Dr. Mortensens work was supported by grants from the Department of Veterans Affairs Vertically Integrated Service Network and Howard Hughes Medical Institute. Dr. Burgess has received honoraria, received research grants, served as a consultant, or served on speakers bureaus for the following pharmaceutical companies: Abbott, AstraZeneca, Merck, Ortho-McNeil Janssen, Roche, sanofiaventis, and Wyeth. The authors have indicated that they have no other conflicts of interest regarding the content of this article. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. The authors acknowledge the assistance of the following clinical pharmacists from the Baptist Health 298
Volume 32 Number 2
C.r. Frei et al.
11. Capelastegui A, Espaa PP, Quintana JM, et al. Improvement of process-of-care and outcomes after implementing a guideline for the management of community-acquired pneumonia: A controlled beforeand-after design study. Clin Infect Dis. 2004;39:955963. 12. Dean NC, Silver MP, Bateman KA, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med. 2001;110:451 457. 13. Fine MJ, Stone RA, Lave JR, et al. Implementation of an evidencebased guideline to reduce duration of intravenous antibiotic therapy and length of stay for patients hospitalized with community-acquired pneumonia: A randomized controlled trial. Am J Med. 2003;115: 343351. 14. Marrie TJ, Lau CY, Wheeler SL, et al, for the CAPITAL Study Investigators. A controlled trial of a critical pathway for treatment of communityacquired pneumonia. CommunityAcquired Pneumonia Intervention Trial Assessing Levofloxacin. JAMA. 2000;283:749755. 15. Marrie TJ, Wu L. Factors influencing in-hospital mortality in communityacquired pneumonia: A prospective study of patients not initially admitted to the ICU. Chest. 2005;127: 12601270. 16. Menndez R, Ferrando D, Valls JM, Vallterra J. Influence of deviation from guidelines on the outcome of community-acquired pneumonia. Chest. 2002;122:612617. 17. Mortensen EM, Restrepo M, Anzueto A, Pugh J. Effects of guidelineconcordant antimicrobial therapy on mortality among patients with community-acquired pneumonia. Am J Med. 2004;117:726731. 18. Bod M, Rodrguez A, Sol-Violn J, et al, for the Community-Acquired Pneumonia Intensive Care Units (CAPUCI) Study Investigators. Antibiotic prescription for communityacquired pneumonia in the intensive care unit: Impact of adherence to Infectious Diseases Society of America guidelines on survival. Clin Infect Dis. 2005;41:17091716. 19. Frei CR, Restrepo MI, Mortensen EM, Burgess DS. Impact of guidelineconcordant empiric antibiotic therapy in community-acquired pneumonia. Am J Med. 2006;119:865 871. 20. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336: 243250. 21. Halm EA, Fine MJ, Marrie TJ, et al. Time to clinical stability in patients hospitalized with communityacquired pneumonia: Implications for practice guidelines. JAMA. 1998; 279:14521457. 22. Menendez R, Torres A, Rodriguez de Castro F, et al. Reaching stability in community-acquired pneumonia: The effects of the severity of disease, treatment, and the characteristics of patients. Clin Infect Dis. 2004;39:17831790.
Address correspondence to: David S. Burgess, PharmD, FCCP, University of Texas Health Science Center at San Antonio, Pharmacotherapy Education and Research Center, 7703 Floyd Curl Drive, MSC-6220, San Antonio, TX 782293900. E-mail: burgessD@uthscsa.edu 299
February 2010
Вам также может понравиться
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyОт EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyРейтинг: 4.5 из 5 звезд4.5/5 (3)
- An Case Study - WebsiteДокумент5 страницAn Case Study - Websiteapi-249707182Оценок пока нет
- Medicine American Journal of Hospice and PalliativeДокумент6 страницMedicine American Journal of Hospice and Palliativem1k0eОценок пока нет
- WSC Abstracts - 2011Документ667 страницWSC Abstracts - 2011cyber_zac52Оценок пока нет
- Infection Is Acommonproblem ForДокумент11 страницInfection Is Acommonproblem ForDitaMayasariОценок пока нет
- IDSAasdsfДокумент46 страницIDSAasdsfAnonymous d3qpXcm4xVОценок пока нет
- The Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of LifeДокумент4 страницыThe Pattern of Antimicrobial Use For Palliative Care In-Patients During The Last Week of Lifem1k0eОценок пока нет
- E20161692 FullДокумент11 страницE20161692 FullWiti Triple'sОценок пока нет
- Pneumonii 2007Документ46 страницPneumonii 2007Turcu AndreeaОценок пока нет
- Current Practice in Nutritional Support and Its Association With Mortality in Septic Patients-Results From A National, Prospective, Multicenter StudyДокумент6 страницCurrent Practice in Nutritional Support and Its Association With Mortality in Septic Patients-Results From A National, Prospective, Multicenter StudyLuis Miguel Díaz VegaОценок пока нет
- Mortality and Overall and Specific Infection Complication Rates inДокумент11 страницMortality and Overall and Specific Infection Complication Rates inKarla LapendaОценок пока нет
- CMA AntibioticsДокумент11 страницCMA AntibioticsNovita Oktavianti DehiОценок пока нет
- Ciz 1049Документ9 страницCiz 1049Justin WilliemОценок пока нет
- Treatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsДокумент5 страницTreatment Completion and Costs of A Randomized Trial of Rifampin For 4 Months Versus Isoniazid For 9 MonthsSyairah Banu DjufriОценок пока нет
- Atients Hospitalized After Initial Outpatient Treatment For Community-Acquired PneumoniaДокумент5 страницAtients Hospitalized After Initial Outpatient Treatment For Community-Acquired PneumoniaMazKha BudОценок пока нет
- Inappropriate Use of Proton Pump Inhibitors in Elderly Patients Discharged From Acute Care HospitalsДокумент6 страницInappropriate Use of Proton Pump Inhibitors in Elderly Patients Discharged From Acute Care HospitalsFitriОценок пока нет
- PIIS2666634020300064Документ47 страницPIIS2666634020300064Erick RomeroОценок пока нет
- Procalcitonin PneumoniaДокумент14 страницProcalcitonin PneumoniaMr. LОценок пока нет
- Hydrocortisone, Vitamin C, and Thiamine For The Treatment of Severe Sepsis and Septic ShockДокумент10 страницHydrocortisone, Vitamin C, and Thiamine For The Treatment of Severe Sepsis and Septic Shockmmmaw mmОценок пока нет
- Huang 2018Документ14 страницHuang 2018amazeyragОценок пока нет
- Vitamina C, Tiamina, Corticoides and Shock SepticoДокумент10 страницVitamina C, Tiamina, Corticoides and Shock SepticoNorvingОценок пока нет
- Marik 2016Документ10 страницMarik 2016PedroОценок пока нет
- Clostridium 2Документ6 страницClostridium 2Ioana AntonesiОценок пока нет
- LeprosyДокумент20 страницLeprosyHafiz Sulistio UtomoОценок пока нет
- Low Dose Prednisolone in Community Acquired PneumoniaДокумент15 страницLow Dose Prednisolone in Community Acquired PneumoniaIsaac SalazarОценок пока нет
- Pulmonary Impairment After Tuberculosis : Original ResearchДокумент8 страницPulmonary Impairment After Tuberculosis : Original ResearchPalaniappan MeyyappanОценок пока нет
- Review: The Ef Ficacy and Safety of Probiotics in People With Cancer: A Systematic ReviewДокумент11 страницReview: The Ef Ficacy and Safety of Probiotics in People With Cancer: A Systematic ReviewNatália LopesОценок пока нет
- Procalcitonin and AB DecisionsДокумент10 страницProcalcitonin and AB DecisionsDennysson CorreiaОценок пока нет
- Combined Use of Antibiotics As A Risk Factor For HДокумент15 страницCombined Use of Antibiotics As A Risk Factor For HGemala AdillawatyОценок пока нет
- Impact of Clinical Pharmacists on Pneumonia TreatmentДокумент5 страницImpact of Clinical Pharmacists on Pneumonia TreatmentDaniela HernandezОценок пока нет
- Ebn RespiДокумент17 страницEbn RespilablabkurmОценок пока нет
- G-4 Presentation DoneДокумент24 страницыG-4 Presentation DoneAbdulrhman 123Оценок пока нет
- Influenza Vaccination: Healthcare Workers Attitude in Three Middle East CountriesДокумент7 страницInfluenza Vaccination: Healthcare Workers Attitude in Three Middle East CountriesDesti EryaniОценок пока нет
- NAC Hospi UCI y SalasДокумент10 страницNAC Hospi UCI y Salasgiseladelarosa2006Оценок пока нет
- Longitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionДокумент11 страницLongitudinal Clinical Evaluation of Antibiotic Use Among Patients With InfectionMITA RESTINIA UINJKTОценок пока нет
- Risk Factors For Drug-Resistant Streptococcus Pneumoniae and Antibiotic Prescribing Practices in Outpatient Community-Acquired PneumoniaДокумент4 страницыRisk Factors For Drug-Resistant Streptococcus Pneumoniae and Antibiotic Prescribing Practices in Outpatient Community-Acquired PneumoniakingkinresmytaОценок пока нет
- 2009hetrase CCMДокумент12 страниц2009hetrase CCMgiseladelarosa2006Оценок пока нет
- Long-Stay of PICU in sepsisДокумент6 страницLong-Stay of PICU in sepsisSanti IskandarОценок пока нет
- A Prospective Study On Antibiotics-Associated Spontaneous Adverse Drug Reaction Monitoring and Reporting in A Tertiary Care HospitalДокумент8 страницA Prospective Study On Antibiotics-Associated Spontaneous Adverse Drug Reaction Monitoring and Reporting in A Tertiary Care HospitalNurul Hikmah12Оценок пока нет
- Effect of Procalcitonin-Guided AntibioticДокумент11 страницEffect of Procalcitonin-Guided AntibioticRaul ContrerasОценок пока нет
- TBC y Shock SepticoДокумент9 страницTBC y Shock Septicogiseladelarosa2006Оценок пока нет
- Pediatrics 2014 Queen E23 9Документ10 страницPediatrics 2014 Queen E23 9Desrainy InhardiniОценок пока нет
- PCT Guidance Reduces Antibiotic Use in CAPДокумент10 страницPCT Guidance Reduces Antibiotic Use in CAPmohd zonОценок пока нет
- Antibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.HДокумент2 страницыAntibiotics For Abdominal Sepsis: Richard P. Wenzel, M.D., and Michael B. Edmond, M.D., M.P.Hchebonk13Оценок пока нет
- Psychological Response COVID Renal TXДокумент5 страницPsychological Response COVID Renal TXdrshhagarОценок пока нет
- PPI Use Duration Risk Factor for Hospital-Acquired C. difficileДокумент6 страницPPI Use Duration Risk Factor for Hospital-Acquired C. difficileTeh NuraqilahОценок пока нет
- Makro LidДокумент7 страницMakro Liddoc_aswarОценок пока нет
- Cancers 08 00084Документ10 страницCancers 08 00084Benny Chris TantoОценок пока нет
- USA2016 - A Single Center Observational Study On ED Clinician Nonadherence To Clinical Practice Guidelines For Treatment of Uncomplicated UTI - 12879 - 2016 - Article - 1972Документ9 страницUSA2016 - A Single Center Observational Study On ED Clinician Nonadherence To Clinical Practice Guidelines For Treatment of Uncomplicated UTI - 12879 - 2016 - Article - 1972jessicapxeОценок пока нет
- Jamda: Original StudyДокумент6 страницJamda: Original StudyNami NakanoОценок пока нет
- PCT CAP ABiuytoДокумент10 страницPCT CAP ABiuytoAndi BintangОценок пока нет
- Stroids Meta 2023Документ14 страницStroids Meta 2023Sachin KumarОценок пока нет
- Chao Chen Et Al - Real-World Pattern of Biologic Use in Patients With Inflammatory Bowel DiseaseДокумент11 страницChao Chen Et Al - Real-World Pattern of Biologic Use in Patients With Inflammatory Bowel DiseaseJLОценок пока нет
- Treatment of Coronavirus Disease 2019 (COVID-19) Patients With Convalescent PlasmaДокумент11 страницTreatment of Coronavirus Disease 2019 (COVID-19) Patients With Convalescent PlasmaGeysel SuarezОценок пока нет
- Jurnal Interna UTIДокумент8 страницJurnal Interna UTIErdika Satria WahyuonoОценок пока нет
- The Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioДокумент7 страницThe Epidemiology, Antibiotic Resistance and Post-Discharge Course of Peritonsillar Abscesses in London, OntarioMaharaniОценок пока нет
- Treatment of Hospital-Acquired, Ventilator-Associated, and Healthcare-Associated Pneumonia in AdultsДокумент19 страницTreatment of Hospital-Acquired, Ventilator-Associated, and Healthcare-Associated Pneumonia in Adultsmd.dascalescu2486Оценок пока нет
- Ciz 1197Документ8 страницCiz 1197Lindia PrabhaswariОценок пока нет
- Polypharmacy and Drug-Related Problems Among People Living With HIV-AIDS - A Single-Center Experience (#577802) - 735759Документ8 страницPolypharmacy and Drug-Related Problems Among People Living With HIV-AIDS - A Single-Center Experience (#577802) - 735759LauraОценок пока нет
- Comprehensive Treatment of Extensively Drug-Resistant TuberculosisДокумент11 страницComprehensive Treatment of Extensively Drug-Resistant TuberculosisAnneke Nandia ParamithaОценок пока нет
- The Opioid Epidemic and the Therapeutic Community Model: An Essential GuideОт EverandThe Opioid Epidemic and the Therapeutic Community Model: An Essential GuideJonathan D. AveryОценок пока нет
- Mammograms and Other Breast Imaging Procedures: What Is A Mammogram?Документ25 страницMammograms and Other Breast Imaging Procedures: What Is A Mammogram?Marina StosicОценок пока нет
- Pathogen Reduction/Hazard Analysis Critical Control Point (HACCP) Systems Final Rule 9 CFR Part 417Документ16 страницPathogen Reduction/Hazard Analysis Critical Control Point (HACCP) Systems Final Rule 9 CFR Part 417Mili MartinezОценок пока нет
- Excessive Use of Mobile Devices and Children's Physical HealthДокумент7 страницExcessive Use of Mobile Devices and Children's Physical HealthPUÑOYLETRAОценок пока нет
- Vaishali Bujad Project..2Документ54 страницыVaishali Bujad Project..2Mitesh Prajapati 7765Оценок пока нет
- What Is AmpalayaДокумент5 страницWhat Is Ampalayarugu0% (1)
- Biology Project: Name Ajit Kumar CLASS 12 S2Документ7 страницBiology Project: Name Ajit Kumar CLASS 12 S2ajitОценок пока нет
- NO Nama Pasien Tanggal Rujukan/Tujuan RsДокумент44 страницыNO Nama Pasien Tanggal Rujukan/Tujuan RsfennyОценок пока нет
- Epos2020 PDFДокумент481 страницаEpos2020 PDFHanifa YuniasariОценок пока нет
- Questionnaire BHWДокумент2 страницыQuestionnaire BHWRogerQux100% (2)
- CureДокумент338 страницCureThiago Cavalli Azambuja100% (1)
- Body Mass IndexДокумент3 страницыBody Mass IndexSunnyVermaОценок пока нет
- Cover Letter - Selina DykesДокумент2 страницыCover Letter - Selina Dykesapi-520664738Оценок пока нет
- SOCIAL SERVICES aCTION PLAN FOR 2022Документ6 страницSOCIAL SERVICES aCTION PLAN FOR 2022Rocel Cañete Ordoyo-GabrielОценок пока нет
- Streptococcal TonsillitisДокумент8 страницStreptococcal TonsillitisNoviera LarasatiОценок пока нет
- Misty Williams How Are You Wired To Sleep UpdatedДокумент21 страницаMisty Williams How Are You Wired To Sleep UpdatedCarolyn McClendonОценок пока нет
- Gun Control PowerpointДокумент11 страницGun Control Powerpointapi-319208107Оценок пока нет
- The Effect of Social Media on Perception and Demand of Aesthetic DentistryДокумент3 страницыThe Effect of Social Media on Perception and Demand of Aesthetic DentistryMona Febiyola AzizahОценок пока нет
- Enhancing Your Skills in Stroke Quality Improvement and Data AnalysisДокумент50 страницEnhancing Your Skills in Stroke Quality Improvement and Data AnalysisRaisha Klinik Vaksinasi YogyakartaОценок пока нет
- Gender Studies Lecture 6Документ30 страницGender Studies Lecture 6Shahzaib KhanОценок пока нет
- 6610 Assignment 4Документ19 страниц6610 Assignment 4gyanendraОценок пока нет
- NoteesДокумент177 страницNoteespearlanne1292100% (1)
- Certificate For COVID-19 Vaccination: Beneficiary DetailsДокумент1 страницаCertificate For COVID-19 Vaccination: Beneficiary DetailsS M SarojОценок пока нет
- 2017 Winter Model Answer PaperДокумент9 страниц2017 Winter Model Answer PaperChetan patilОценок пока нет
- Educational Strategies For Children With Emotional and Behavioral ProblemsДокумент74 страницыEducational Strategies For Children With Emotional and Behavioral Problemsmaeydel50% (2)
- Recognised Hospitals PDFДокумент17 страницRecognised Hospitals PDFNandan YaduОценок пока нет
- Hirsch SprungДокумент4 страницыHirsch SprungRy AnneОценок пока нет
- Research Themes and Advances in MalariaДокумент11 страницResearch Themes and Advances in Malarialilibeth paola duran plataОценок пока нет
- Ielts Speaking 3Документ34 страницыIelts Speaking 3Asad GondalОценок пока нет
- Cephalexin Med CardДокумент2 страницыCephalexin Med CardAnja de VriesОценок пока нет