Академический Документы
Профессиональный Документы
Культура Документы
Ncp's
Загружено:
Duchess Kleine RafananИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Ncp's
Загружено:
Duchess Kleine RafananАвторское право:
Доступные форматы
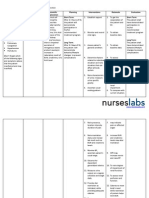
Assessment SUBJECTIVE: Napansin ko na lumalaki ang tiyan ko as verbalized by the patient.
OBJECTIVE: Anasarca Weight gain Altered electrolyte levels V/S taken as follows: T- 37.6 C P- 110 R-29 BP- 180/100
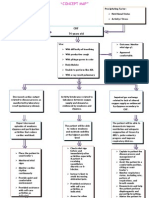
Diagnosis Fluid volume excess related to compromised regulatory mechanism as evidenced by edema and ascites formation
Planning After 8 hours of nursing interventions,the patient will demonstrate stabilized fluid volume and decreased edema.
Intervention INDEPENDENT: > Measure intake and output,weigh daily, andnote weight gainmore than 0.5kg/day. > Assess respiratory status, noting increased respiratory rate, dyspnea. >Monitor blood pressure. Auscultate lungs, noting diminished/ absent breath sounds and developing adventitious sounds. >Assess degree of peripheral/ dependent edema.
Rationale >Reflects circulating volume status. Positive balance/ weight gain often reflects continuing fluid retention. > Indicative of pulmonary congestion. >Blood pressure elevation usually associated with fluid volume excess but may not occur because of fluid shifts out of the vascular space. >Increasing pulmonary congestion may result in consolidation, impaired gas
Evaluation Goal met. After 8 hours of Nursing interventions, the patient was able to demonstratestabilized fluid volume and decreased edema.
Assessment
Diagnosis
Planning
Intervention
Rationale
Evaluation
Subjective: Mabigat at masakit ang tyan ko as verbalized by the patient. Objective: >facial grimace >with a painscale of 6/10 >irritable >with guarding behavior >with massive ascites
Acute pain and discomfort related to enlarged tender liver and ascites as evidenced by facial grimace and painscale of 6/10.
After 8 hours of effective nursing intervention, the patient will be able to demonstrate divertional activities to lessen pain.
INDEPENDENT: 1. Maintain bed rest when patient experiences abdominal discomfort. 2. Observe, record, and report presence and character of pain and discomfort.
1. Reduces metabolic demands and protects the liver.
2. Provides baseline to detect further deterioration of status and to evaluate interventions. 3. Reduce 3. Minimizes sodium and further fluid intake if formation of prescribed. ascites. 4. Teach patient divertional 4. Provide activities such venous return as deep and promotes breathing relaxation to excercises and the patient. provide reading materials. 5. Prepare patient and 5. Removal of assist with ascites fluid paracentesis. may decrease DEPENDENT: abdominal 6.Administer discomfort.
Goal met. After 8 hours of effective nursing intervention, patient seen doing the divertional activities instructed and patients pain lessened from 6/10 to 4/10.
antispasmodic and sedative agents as prescribed.
6. Reduces irritability of the gastrointestinal tract and decreases abdominal pain and discomfort.
Assessment Madalas akong hapuin lalo na kapag lagi nakahiga as verbalized by
Diagnosis Impaired Gas Exchange r/t accumulation of fluid in pleural space
Planning After 8 hours of giving effective nursing intervention and health
Intervention INDEPENDENT : 1. Position client in either
Rationale
1. Promote good ventilatio
Evaluation Goal met. After 8 hours of giving effective nursing intervention and health
the patient. Objective: >Use of accessory muscles when breathing >with labored breathing (shallow breathing) RR- 29 cycles per minute (+) crackles
secondary to underlying physiologic condition.
teaching, the patient will be able to know positioning techniques that improve ventilation.
semifowlers position or side lying position. 2. Encourag e client to cough as tolerated.
n and teaching, the breathing. patient was able to know 2. Will positioning promote techniques that mucoid or improve sputum ventilation. excretion from the lungs 3. Proper assessme nt will help identify early problems.
3. Monitor respirator y rate, depth, and effort, including use of accessory muscles, nasal flaring, and thoracic or abdomina l breathing.
4. Changes in behavior and mental status can be early signs of impaired gas
exchange. 4. Monitor clients behavior and mental status for onset of restlessne ss, agitation, confusion and in the late stages, extreme lethargy 5. Observe for cyanosis in skin: note especial color of tongue and oral mucous membran e.
5. Central cyanosis in tongue and oral mucosa is indication of serious hypoxia and is a medical emergenc y; peripheral cyanosis seen in extremitie s may not be serious. 1. To promote enough oxygen
supply Dependent: 1. Administe r oxygen inhalation appropriat ely. 2. Administe r salbutam ol 2. To provide bronchodi lation.
Subjective: Nahihirapan akong huminga, as verbalized by the patient. Objective: >flaring of nose >inadequate chest expansion >rapid shallow breathing >pallor V/S T- 37.6 C P- 110 R-29 BP- 120/90
Ineffective breathing pattern related to intra-abdominal fluid collection as evidenced by rapid shallow breathing.
After 8-hours of nursing intervention the patient will participate in actions to maximize oxygenation.
Independent: 1. Monitor respiratory rate, depth and effort.
2. Auscultate breath sounds, noting crackles, wheezes or ronchi.
1. Rapid shallow breathing may be present because of hypoxia and fluid accumulation in the abdomen. 2. Indicates developing of complications (adventitious sounds reflects accumulation of fluid; absent sounds suggest atelectasis. 3. Changes in mentation may reflect hypoxemia and respiratory failure which often accompany hepatic coma. 4. Facilitates breathing by reducing pressure on the diaphragm and minimizes risk of aspiration of secretions.
Goal met. After 8 hours of nursing intervention the patient participate in deep breathing and coughing exercises.
3. Investigate changes in the level of consciousness.
4. Keep head of the bed elevated.
5. Frequent repositioning and encourage deepbreathing exercises or coughing as appropriate. 6. Monitor
Вам также может понравиться
- NCP For Ruptured AppendicitisДокумент2 страницыNCP For Ruptured AppendicitisJansen Arquilita RiveraОценок пока нет
- NafarinДокумент2 страницыNafarinianecunar100% (2)
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NДокумент2 страницыNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaОценок пока нет
- Nursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationДокумент1 страницаNursing Care Plan: Assessment Diagnosis Planning Interventions Rationale EvaluationJhevilin RM100% (1)
- COLCHICINE pptx1800128929Документ15 страницCOLCHICINE pptx1800128929April Mergelle LapuzОценок пока нет
- SLCN Gazette Magazine, Volume 1, Issue 1, 2019Документ20 страницSLCN Gazette Magazine, Volume 1, Issue 1, 2019Mayzelle RizОценок пока нет
- Final Eb ReflectionДокумент2 страницыFinal Eb Reflectionapi-238460511Оценок пока нет
- Compartment Syndrome NCP (PAIN)Документ2 страницыCompartment Syndrome NCP (PAIN)eunica16Оценок пока нет
- MGH 8 - Ihd - NCPДокумент12 страницMGH 8 - Ihd - NCPSesinando Niez Quilao Jr.100% (1)
- Discharge Plan CapДокумент3 страницыDischarge Plan Capalexander abasОценок пока нет
- JM CarbocisteineДокумент1 страницаJM CarbocisteineKatrina MagtalasОценок пока нет
- Aspirin Drug SummДокумент2 страницыAspirin Drug SummWarren0% (1)
- TramadolДокумент1 страницаTramadolAi RouОценок пока нет
- IrbesartanДокумент3 страницыIrbesartanapi-3797941Оценок пока нет
- Drug Study SARAHДокумент2 страницыDrug Study SARAHirene Joy DigaoОценок пока нет
- Gout N C P BY BHERU LALДокумент1 страницаGout N C P BY BHERU LALBheru LalОценок пока нет
- Nursing Care Plan: Pulmonary EbolismДокумент5 страницNursing Care Plan: Pulmonary EbolismneuronurseОценок пока нет
- LOSARTANДокумент3 страницыLOSARTANReinell GoОценок пока нет
- Chloral Hydrate (Drug Study)Документ3 страницыChloral Hydrate (Drug Study)Franz.thenurse6888Оценок пока нет
- Irbesartan (Avapro)Документ1 страницаIrbesartan (Avapro)EОценок пока нет
- DS BiperidenДокумент3 страницыDS BiperidenbillyktoubattsОценок пока нет
- NCPДокумент3 страницыNCPJezza RequilmeОценок пока нет
- Nursing Care Plan. HypertensionДокумент2 страницыNursing Care Plan. HypertensionKiara Shanelle Posadas AbrioОценок пока нет
- NCP Mandibular)Документ5 страницNCP Mandibular)yellarfОценок пока нет
- Drug Study Stugeron and Kalium DuruleДокумент1 страницаDrug Study Stugeron and Kalium DuruleawesomedawnОценок пока нет
- LacipilДокумент2 страницыLacipilianecunarОценок пока нет
- Drug Study EditedДокумент5 страницDrug Study EditedfabtaciousVeelaОценок пока нет
- Drug StudyДокумент20 страницDrug StudydjanindОценок пока нет
- ETOPOSIDEДокумент4 страницыETOPOSIDEkajal guptaОценок пока нет
- College of Nursing: Cebu Normal UniversityДокумент3 страницыCollege of Nursing: Cebu Normal UniversityShiva TorinsОценок пока нет
- Altered Renal Perfusion CRFДокумент4 страницыAltered Renal Perfusion CRFKristel Anne Nillo ZepolОценок пока нет
- NCP Decreased Cardiac Output 1Документ2 страницыNCP Decreased Cardiac Output 1Arnel MacabalitaoОценок пока нет
- Aerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatec Rinovagos, Atrovent, Atrovent HFAДокумент3 страницыAerovent, Apovent Atronase, Ipraxa, Ipvent Rhinovent, Rinatec Rinovagos, Atrovent, Atrovent HFAGwyn RosalesОценок пока нет
- Ineffective Airway ClearanceДокумент6 страницIneffective Airway ClearanceBenly Grace Rebuyon MosquedaОценок пока нет
- Nursing Care Plan Rheumatoid ArthritisДокумент3 страницыNursing Care Plan Rheumatoid ArthritisJashAnia MarIe EvArdo FloresОценок пока нет
- NCPДокумент3 страницыNCPArien CaleonОценок пока нет
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesДокумент3 страницыSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaОценок пока нет
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Документ6 страницRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroОценок пока нет
- CombiventДокумент1 страницаCombiventDherick Rosas0% (1)
- NURSING CARE PLAN - SuicidalactДокумент4 страницыNURSING CARE PLAN - SuicidalactJennifer ArdeОценок пока нет
- DolcetДокумент2 страницыDolcetmarc_hansen_1312Оценок пока нет
- Risk For Ineffective Airway Clearance 1Документ8 страницRisk For Ineffective Airway Clearance 1kint manlangitОценок пока нет
- NCPДокумент3 страницыNCPJoevelyn LaynoОценок пока нет
- Drug Name Mechanism of Action Indication Contraindication Adverse Effect Nursing ResponsibilitiesДокумент4 страницыDrug Name Mechanism of Action Indication Contraindication Adverse Effect Nursing Responsibilitiesangel cenaОценок пока нет
- Drug StudyДокумент5 страницDrug Studyjanelle123 toribioОценок пока нет
- Cholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationДокумент1 страницаCholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationJess GoОценок пока нет
- Ineffective Airway ClearanceДокумент2 страницыIneffective Airway ClearancePatrick Arvin Ballesteros BarcarseОценок пока нет
- NCP PTBДокумент2 страницыNCP PTBMack Jhed AnarconОценок пока нет
- SNU49Документ2 страницыSNU49Nora BacolОценок пока нет
- Discharge PlanningДокумент1 страницаDischarge PlanningzbestgurlОценок пока нет
- Bearse Tablet InsertДокумент2 страницыBearse Tablet InsertLeonard ByunОценок пока нет
- Concept Map - Abby !Документ2 страницыConcept Map - Abby !Abegail Abaygar100% (3)
- NCP LocДокумент2 страницыNCP LocMel RodolfoОценок пока нет
- NCPДокумент5 страницNCPRose AnnОценок пока нет
- Revised NCP (Baiae)Документ9 страницRevised NCP (Baiae)Jennifer BactatОценок пока нет
- Pleural Effusion NCPsДокумент7 страницPleural Effusion NCPsJaja Nagallo100% (2)
- NCPДокумент4 страницыNCPAbegail Abaygar100% (1)
- NCP BaiaeДокумент7 страницNCP BaiaeJonathan Delos ReyesОценок пока нет
- AssesmentДокумент9 страницAssesmentmizrypОценок пока нет
- NCP Ineffective Airway ClearanceДокумент1 страницаNCP Ineffective Airway ClearanceImation DataОценок пока нет