Академический Документы
Профессиональный Документы
Культура Документы
Week 2
Загружено:
Sab IbarretaИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Week 2
Загружено:
Sab IbarretaАвторское право:
Доступные форматы
OUR LADY OF FATIMA UNIVERSITY COLLEGE OF NURSING NCM 101 COMMUNITY HEALTH NURSING The Philippine Public Health
System I. Current Health Situation Demographic Profile In 1999, the average life expectancy at birth was 68.6 years (71.28 for female and 66.03 for males). In 2001 it is 66.6 years for male & 71.9 years for female. Thirty nine (39%) of the total population in 1994 was estimated to be in the 0-14 age group. Only five percent (5%) were 60 years old and above. Given these percentages, the dependency ratio was computed to be 79, that is there are 79 people (0 to 14 and 60 years old and above) who depend on 100 people in the productive age group (15-59) (National Health Objectives). There are about 249 people for every square kilometer of the Philippine territory. Metro Manila has the highest population density (16, 051) and Cordillera Administrative Region (CAR) has the lowest (75) (according to National Health Objectives). The population in the urban areas is increasing very rapidly. From the 37% of the total population in 1984 (UNICEF, 1986) the figure increased to 44% ten years later. The annual population growth rate for the whole country is 2.3%, the growth rate in the urban areas is 3.4% per year (ESCAP). The high population density facilitates the transmission of infectious and communicable diseases and greater need for social services such as decent housing, transportation, communication, education and health services far outweighs the ability of the government and the private sector to provide these services. II. Health Profile Births and Deaths The crude birth rate (CBR) in 1997 was 28.4 per 1000 population. The crude death rate (CDR) is 6.1 per 1000 population. Based on these figures, the rate of natural increase in the country's population for the same year was 22.3 (28.4 minus 6.1 for every 1000 population (National Health Objectives). The total fertility rate (TFR) in the Philippines remains high compared to the neighboring Southeast Asian Countries. Rural women have more children than urban women. Uneducated women also have more children than those who are with college education. Those in the 25-29 age groups have the highest fertility rate. (National Demographic and Health Survey, 1999) Infant Mortality Rate (1995) was 48.9 per 1000 live births. It is within the WHO IMR global goal which is, 50/1000 live births. Under-five mortality rate or deaths of children below five years old in the same year was 67/1000 live births. The maternal mortality rate (MMR) was 1.8/1000 live births (DOH, 1995) or 18 maternal deaths for every 10,000 live births.
Causes of Morbidity and Mortality The leading causes of mortality among Filipinos (1997) are (1)Diseases of the heart (2 Disease of vascular system (3) pneumonias (4) malignant neoplasm (5) TB, all forms (6)Accidents (7) Chronic obstructive & pulmonary disease (8) Other diseases of respiratory system (9) DM (10) Diarrheal diseases (National Health Objectives). The leading causes of infants mortality (1997) are (1)respiratory conditions of fetus & newborn (2) pneumonias (3) congenital anomalies (4) birth injury and difficulty of labor (5) diarrheal diseases (6) septicemia (7) measles (8) meningitis (9)Respiratory diseases (10) Avitaminosis /nutritional deficiency (1997, Philippine Health Statistics). Infant deaths result from poor maternal conditions, unhealthy environment and inadequate health care delivery system, among others. Infant deaths result from poor maternal conditions, unhealthy environment and inadequate health care delivery system, among others. The leading causes of Maternal Mortality (1997) are (1) Normal delivery & other complications related to pregnancy occurring in the course of labor, delivery and puerperium (2) HPN complicating pregnancy, childbirth and puerperium (3) hemorrhage related to pregnancy (1997 Philippine Health Statistics). Maternal mortality as defined by the WHO as the death of a woman while pregnant or within 42 days of termination of pregnancy irrespective of the duration and the site of the pregnancy from any cause related to, or aggravated by the pregnancy or its management, but not from accidental or incidental causes. The leading causes of Morbidity (1997) are: (1) Diarrheas (2) Pnemonias (3) Bronchiolitis (4) Influenza (5) TB, all forms (6) malaria (7) Chicken pox (8) Diseases of the heart (9) Measles (10) dengue H-fever. (1997 Philippine Health Statistics). Despite the improvements in the field of public health, many of the common causes of morbidity can be prevented by improving environmental sanitation and personal hygiene. Infectious diseases remain to be the main causes of morbidity, cardiovascular diseases, diabetes and cancer, the so-called lifestyle diseases have become the top cause of deaths. Peoples lifestyle, particularly their unhealthy diet, sedentary work and lack of exercise have been identified to be the major reason why they die from the diseases which used to be associated with developed countries.
III. Reasons of Health Problems 1. Poverty Most of the leading causes of morbidity and mortality are associated with factors that could be attributed to poverty illiteracy, unfounded health beliefs, harmful practices, inadequate nutrition, poor environmental sanitation, inadequate source of potable water supply, congested housing units, limited access to basic health services, and inability to make decisions on matters which are important to health. The poverty incidence was estimated at 40.7% in 1991 which was 59% in 1985 (CRC, 1990). According to the Medium-Term Development Plan (1993-1998), more than half of the total income flows to the richest 20% of the population. The remaining 50% for sure, is not equally distributed among the majority (80%) of the population. Access to basic health services is hindered by the clients lack of financial resources and the governments inadequate financial support for public health programs and facilities.
The health budget remains to be much lower than the WHO-recommended 5% of a countrys gross national product (GNP). The budget of the Department of Health is less than 3% of the total government budget.
2. Cultural Influences on Health Many unhealthy and unsafe practices continue, particularly among poorly educated and poor people, especially those who are not reached by health education programs or messages. Culture, per se, may not be the culprit for poor health; in many instances, it is poverty and inadequacy of the health care delivery system. Although some culture practices are harmful to health, certain aspects of our culture exert positive influences on health. 3. Environmental Influences on Health An unsanitary environment is a major factor in the causation of diarrheal diseases, still one of the leading causes of morbidity in the country. It is the breeding ground of animals and insects that harbor and transmit microorganisms. The deterioration of the ecosystem has been implicated in the rapid increase of cancer cases and other health problems throughout the world. Exposure to chemicals such as pesticides and other air pollutants has been identified as ma major cause of a number of diseases such as cancer and respiratory diseases. The state of the countrys environment is the direct result of the interaction of a number of factors such as industrialization, government policies, poverty and an uncaring attitude towards environment. 4. Political Influences on Health Policies which are the outcomes of policy-making reflect the priorities of government. The health budget is the most concrete expression of the governments political will. Many Filipinos do not have full access to basic health goods and services because of the severely limited health care financing. Health spending has always been inadequate. In 1999, the amount spent for health was only 3.4% of the gross national product. The severely limited health budget is the biggest hindrance to the implementation of wellmeaning policies such as the Magna Carta of Public Health Workers (RA 7305), National Health Insurance Act (RA 7875) and the Senior Citizens Act (RA 7432). There are laws that affect the delivery of health services the Local Government Code, National Health Insurance Act and the professional practice acts of the different professions. In areas where access to medical care is difficult, nurses and midwives perform functions that are beyond the provisions of their own practice acts.
IV. The Philippine Health Care Delivery System The health care delivery system is the totality of all policies, infrastructures, facilities, equipment, products, human resources, and services that address the health needs, problems and concerns of all people. The Philippine Health Care Delivery System is composed of the public and private sectors which maintain their own health facilities (such as hospitals, clinics and diagnostic centers). Public Sector Largely finance through a tax-based budgeting system at both national and local levels and where health care is generally given free at the point of services. It is consists of the national and local government agencies providing health services.
National level the Department of Health (DOH) is mandated as the lead agency in health. It has a regional filed office in every region and maintains specialty hospitals, regional hospitals and medical centers. Local level - with the devolution of health services, local health systems are now headed by the Local Government Units (LGUs). - The provincial and district hospitals are under the provincial government. - The city/municipal government manages the health centers/rural health units (RHUs) and barangay health station (BHSs). - There is a local health board chaired by the local chief executive.
Private Sector Largely market oriented and where health care is pain through user fees at the point of service. V. The Department of Health The Department of Health remains to be the national governments biggest health care provider. The DOH used to have control and supervision over all barangay health stations, rural health units and hundreds of hospitals throughout the country. Today, only the regional hospitals, medical centers, special and specialty hospitals are directly under the DOH. The DOH exercises regulatory powers over health facilities and products. It takes the lead in the formulation of policies and standards related to health facilities, health products and health human resources. The DOH has also undergone transformation to be more responsive to its post-devolution functions.
Roles and Functions (as mandated by EO 102) 1. Leadership in Health Serves as national policy and regulatory institution from which the local government units, nongovernment organizations and other members of the health sector involved in social welfare and development will anchor their thrusts and directions for health. Provide leadership in the formulation, monitoring and evaluartion of national health policies, plans and programs. Serve as advocate in the adoption of health policies, plans and programs to address national and sectoral concerns. 2. Enabler and Capacity Builder
Innovate new strategies in health to improve effectiveness of health programs, initiate public discussion on health issues and undertaking and disseminate policy research outputs to ensure informed public participation in policy decision-making. Exercise oversight functions and monitoring and evaluation of national health plans, programs and policies. Ensure the highest achievable standards of quality health care, health promotion and health protection. 3. Administrator of Specific Services Manages selected national health facilities and hospitals with modern and advanced facilities that serves as national referral centers. Administer direct services for emergent health concerns that require new complicated technologies that it deems necessary for public welfare; administer special components of specific programs like tuberculosis etc... Administer health emergency response services, including referral and networking system for trauma, injuries and catastrophic events, in cases of epidemic and other widespread public danger, upon the direction of the President and in consultation with concerned LGU.
Vision: o HEALTH for ALL in the Philippines Mission: o Guarantee equitable, sustainable and quality health for all Filipinos, especially the poor and shall lead the quest for excellence in health.
Goal: o Health Sector Reform Agenda (HSRA) -Health Sector reform is the overriding goal of the DOH.
Rationale for Health Sector Reform: Although there has been a significant improvement in the health status of Filipinos for the last 50 years, the following conditions are still seen among the population: Slowing down in the reduction in the Infant Mortality Rate (IMR) and the Maternal Mortality Rate (MMR).
Persistence of large variations in health status across population groups and geographic areas. High burden from infectious diseases. Rising burden from chronic degenerative diseases. Unattended emerging health risks from environmental and work related factors. Burden of disease is heaviest on the poor.
Framework for Implementation of HSRA: o FOURmula ONE for Health - This is adopted as the implementation framework for health sector reforms under the current administration. - It intends to implement critical interventions as a single package backed by effective management infrastructure and financing arrangements following a sector wide approach.
Goals of FOURmula ONE for Health 1. Better health outcomes 2. More responsive health systems 3. Equitable health care financing
The Four Elements of the Strategy are: 1. Health financing the goal of this health reform area is to foster greater, better and sustained investments in health. 2. Health regulation the goal is to ensure the quality and affordability of health goods and services. 3. Health service delivery the goal is to improve and ensure the accessibility and availability of basic and essential health care in both public and private facilities and services. 4. Good governance the goal is to enhance health system performance at the national and local levels.
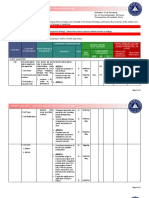
Roadmap for All Stakeholders in Health: National Objectives for Health 2005 to 2010
The NOH 2005-2010 provides the road map for stakeholders in health and health-related sectors to intensify and harmonize their efforts to attain its time-honored vision of health for all Filipinos and continue its avowed mission to ensure accessibility and quality of health care to improve the quality of life of all Filipinos, especially the poor.
Objectives of the Health Sector 1. Improve the general health status of the population 2. Reduce morbidity and mortality from certain diseases 3. Eliminate certain diseases as public health problems 4. Promote healthy lifestyle and environmental health. 5. Protect vulnerable groups with special health and nutrition needs. 6. Strengthen national and local health systems to ensure better health service delivery 7. Pursue public health and hospital reforms 8. Reduce the cost and ensure the quality of essential drugs 9. Institute health regulatory reforms to ensure quality and safety of health goods and services 10. Strengthen health governance and management support systems 11. Institute safety nets for the vulnerable and marginalized groups 12. Expand the coverage of social health insurance 13. Mobilize more resources for health 14. Improve efficiency in the allocation production and utilization of resources for health. VI. The Local Health System Devolution made local government executives responsible to operate local health care services. Each center controls a portion of the health care system as part of its political and administrative mandate. Provincial governments operate the hospital system, Provincial and District Hospitals, while city/municipal governments operate the Health Centers (HC)/Rural Health Units (RHU) and Barangay Health Station. Objectives 1. Establish local health systems effective and efficient delivery of health care services. 2. Upgrade the health care management and service capabilities of local health facilities. 3. Promote inter-LGU linkages and cost sharing schemes including local health care financing systems for better utilization of local health resources. 4. Foster participation of the private sector, non-government organizations (NGOs) and communities in local health systems development.
5. Ensure the quality of health service delivery at the local level. Inter Local Health System This system is being espoused by the Department of Health in order to ensure quality of health care services at the local level. It is a system of health care similar to a district health system in which individuals, communities and all other health care providers is well-defined geographical area participate together in providing quality equitable and accessible health care with Inter Local Government Unit (ILGU) partnership as the basic framework. The overall concept is achieved through clustering municipalities into Inter Local Health Zone (ILHZ) Expected achievement of the Inter-Local Health System 1. Universal coverage of health insurance 2. Improved quality of hospital and Rural Health Units (RHU) service 3. Effective referral system 4. Integrated planning 5. Appropriate health information 6. Improved drug management 7. Developed human resources 8. Effective leadership through Inter-LGU corporation 9. Financially visible or self sustaining hospitals 10. Integration of public health and curative hospital care 11. Strengthened cooperation between LGU and health sectors Composition of the Inter-Local Health Zone 1. People According to WHO, the ideal health district would have a population size between 100,000 and 500,000 for optimum efficiency and effectiveness. 2. Boundaries clear boundaries between Inter Local Health Zones determine the accountability and responsibility of health service providers, geographical locations and access to referral facilities are the usual basics in forming boundaries. 3. Health Facilities - District or provincial hospital (referral hospital for secondary level of health care) a number of Rural Health Units (RHU) Barangay Health Stations (BHS) and other health services deciding to work together as an integrated health system. 4. Health Workers The right unit of health providers is needed to deliver comprehensive health service. The health workers form the ILHZ team to plan joint strategies for district health care. Levels of Health Care Referral System 1. Primary Level of Care Devolved to the cities and the municipalities. The first contact between the community and other levels of health facility. Health care is provided by center physicians, public health nurses, rural health midwives, barangay health workers, traditional healers and others. Facilities could be a barangay health stations and a rural health units.
2. Secondary Level of Care This serves as referral center for primary health facilities.
Health care is rendered by physician with basic health training Facilities are either privately owned or government operated such as infirmaries, municipal and district hospitals and out-patient department of provincial hospitals Secondary facilities are capable of performing could minor surgeries and some simple laboratory examinations
3. Tertiary Level of Care This is the referral center for the secondary care facilities. Health care is rendered by specialist Facilities include medical centers, regional and provincial hospitals as well as specialized hospitals. Cases may include complicated cases and intensive care Levels of Health Care Services Problems that are beyond the capability of Barangay Health Station are referred to
Rural Health Unit (located in town or poblacion). Cases needing hospitalization are transferred to District Community Hospital Higher echelons of health services are given in Provincial, Regional and National levels. Primary Health Care Primary Health Care is an essential health care made universally accessible to individuals and families in the community by means acceptable to them through their full participation at a cost that the community and country can afford at every stage of development (WHO, 1978) Characterized by partnership and empowerment of the people that shall permeate as the core strategy Community based, accessible, acceptable and sustainable at a cost community and government can afford. Includes full participation and active involvement of the community
Leads to development of self-reliant people
History and Legal Basis Primary Health Care was declared during the First International Conference on Primary Health Care was held in Alma Ata USSR on September 6 12, 1978 by WHO and UNICEF. PHC was adopted in the Philippines as mandated by Letter of Instruction (LOI) 949 signed by President Ferdinand Marcos on October 19, 1979 and has an underlying theme of Health in the Hands of the People by 2020.
Goal: o Health for All by the year 2020 Theme: o Health in the Hands of the People by 2020 Elements/Components of Primary Health Care 1. Environmental Sanitation 2. Immunization 3. Control of Communicable Diseases 4. Health Education 5. Maternal and Child Health and Family Planning 6. Adequate Food and Proper Nutrition 7. Provision of Medical Care and Emergency Treatment 8. Treatment of Locally Endemic Diseases 9. Provision of Essential Drugs Strategies 1. Reorientation and reorganization of the national health system
2. Effective preparation and enabling process for health action at all levels 3. Mobilization of the people 4. Development and utilization of appropriate technology 5. Organization of communities 6. Increase opportunities for community participation 7. Development of intra-sectoral linkages
8. Emphasizing partnership
Four Cornerstone/Pillars in Primary Health Care 1. Active community participation 2. Intra and Inter-sectoral linkages 3. Use of appropriate technology 4. Support mechanism made available Primary Health Care Team May consist of physician, nurses, midwives, nurse auxiliaries, locally trained community health workers, traditional birth attendants and healers Basic primary health care team consists of physician, public health nurse and midwives The types vary in different communities depending upon: (1) available health manpower resources (2) local health needs and problems (3) political and financial feasibility.
Two Levels of Primary Health Care Workers 1. Village or Barangay Health Workers (V/BHWs) This refers to trained community health workers or health auxiliary volunteer or a traditional birth attendant or healer.
2. Intermediate Level Health Workers General medical practitioners or their assistants, Public Health Nurse, Rural Sanitary Inspectors and Midwives may compose this group.
Вам также может понравиться
- National Health SituationДокумент118 страницNational Health Situationmaria erika93% (56)
- The National Health SituationДокумент167 страницThe National Health SituationCes AriaОценок пока нет
- Health Profile - ThailandДокумент5 страницHealth Profile - ThailandRangaFernandoОценок пока нет
- Overview of The Philippine Health SystemДокумент10 страницOverview of The Philippine Health SystemCaryl Ann RabanosОценок пока нет
- CBTP ResearchДокумент35 страницCBTP ResearchElsaye WCUОценок пока нет
- Service Delivery Profile PhilippinesДокумент13 страницService Delivery Profile Philippines15-0001Оценок пока нет
- NUHRA National (2006 2010)Документ37 страницNUHRA National (2006 2010)Kamil PestañoОценок пока нет
- 0.1 Chapter 1 - Overview of Public Health Nursing in The PhilippinesДокумент11 страниц0.1 Chapter 1 - Overview of Public Health Nursing in The PhilippinesJerreca DasasОценок пока нет
- 0.1 Chapter 1 - Overview of Public Health Nursing in The PhilippinesДокумент11 страниц0.1 Chapter 1 - Overview of Public Health Nursing in The Philippinesaajeno10Оценок пока нет
- Philippine HealthcareДокумент16 страницPhilippine HealthcareJacq CalaycayОценок пока нет
- Primary Health CareДокумент59 страницPrimary Health CareRoxii NavarroОценок пока нет
- Introduction To Health FinancingДокумент101 страницаIntroduction To Health FinancingArianne A ZamoraОценок пока нет
- Overview of Public Health Nursing in The Philippines: Learning ObjectivesДокумент15 страницOverview of Public Health Nursing in The Philippines: Learning ObjectivesRainy DaysОценок пока нет
- Aquino Health AgendaДокумент41 страницаAquino Health AgendaJannine Mae Zaragosa MosquisaОценок пока нет
- 3 Global Health Lesson 1Документ21 страница3 Global Health Lesson 1Solomon Fallah Foa SandyОценок пока нет
- Doh ProgramsДокумент250 страницDoh Programsjoyshe111Оценок пока нет
- Doh ProgramsДокумент246 страницDoh ProgramsShengxy FerrerОценок пока нет
- Ethiopia Strategy DocumentДокумент7 страницEthiopia Strategy DocumentTes MekoОценок пока нет
- 1234 Global Health Lesson 1Документ27 страниц1234 Global Health Lesson 1Solomon Fallah Foa SandyОценок пока нет
- Health Problems in IndiaДокумент25 страницHealth Problems in Indiashubham rathod100% (1)
- DOH ProgramsДокумент248 страницDOH ProgramsMa Angelica Pineda67% (3)
- DOH Updated Programs A-FДокумент61 страницаDOH Updated Programs A-Fdeeday echavezОценок пока нет
- CHN HandoutsДокумент22 страницыCHN HandoutsPeej ReyesОценок пока нет
- Module 1 - Overview of Public Health Nursing in The PhilippinesДокумент7 страницModule 1 - Overview of Public Health Nursing in The PhilippinesKatie HolmesОценок пока нет
- Indigenous Health in AustraliaДокумент4 страницыIndigenous Health in AustraliaKerryann HuntОценок пока нет
- Social Sustainability On Maternal DeathДокумент17 страницSocial Sustainability On Maternal DeathJp YapОценок пока нет
- Primary Health Care (Review Notes)Документ87 страницPrimary Health Care (Review Notes)Rhenier S. Ilado100% (7)
- Chapter 6 SummaryДокумент3 страницыChapter 6 SummaryErica MaatubangОценок пока нет
- National HIV/STI Prevention ProgramДокумент9 страницNational HIV/STI Prevention ProgramJoezerk Jhon BielОценок пока нет
- Philippine Reproductive HealthДокумент10 страницPhilippine Reproductive HealthFrankie MacabadaОценок пока нет
- NCM 104 Lecture Chapter 2.1 Health-Care-Delivery-SystemДокумент112 страницNCM 104 Lecture Chapter 2.1 Health-Care-Delivery-SystemWilma Nierva BeraldeОценок пока нет
- Top 10 Health Agendas of The PhilippinesДокумент5 страницTop 10 Health Agendas of The PhilippinesAnne LauretaОценок пока нет
- Primary Health CareДокумент6 страницPrimary Health CareAbdulaziz KamiluОценок пока нет
- HLST 354: Class 4 - Global HealthДокумент29 страницHLST 354: Class 4 - Global HealthLenard GpОценок пока нет
- FCM3 - Health - Care - System - PPTX Filename UTF-8''FCM3 Health Care SystemДокумент49 страницFCM3 - Health - Care - System - PPTX Filename UTF-8''FCM3 Health Care SystemPria VermaОценок пока нет
- Health For All in Low-Income Settings Ecosoc March 31, 2009Документ31 страницаHealth For All in Low-Income Settings Ecosoc March 31, 2009kausar s khanОценок пока нет
- 003 Healthcare Delivery System of The PhilippinesДокумент6 страниц003 Healthcare Delivery System of The PhilippinesDIEGO APRILОценок пока нет
- UntitledДокумент57 страницUntitledsecret laОценок пока нет
- NCM 113 Final Module 8 LectureДокумент8 страницNCM 113 Final Module 8 LectureAngel Khrisna BacasmotОценок пока нет
- Community Health Nursing 1 Public Health Nursing in The PhilippinesДокумент16 страницCommunity Health Nursing 1 Public Health Nursing in The PhilippinesFlourence ZafranОценок пока нет
- Health Problems in IndiaДокумент23 страницыHealth Problems in IndiaNeethu VincentОценок пока нет
- Community Health Nursing ReviewerДокумент28 страницCommunity Health Nursing ReviewerJenie Munar RosarioОценок пока нет
- NCM 104 Lecture Chapter 2.1 Health-Care-Delivery-System 1Документ25 страницNCM 104 Lecture Chapter 2.1 Health-Care-Delivery-System 1Wilma Nierva BeraldeОценок пока нет
- Ronan Redembert R. LomongoДокумент4 страницыRonan Redembert R. LomongoRoland Awe YalonОценок пока нет
- Migration of Health WorkersДокумент23 страницыMigration of Health WorkersNufie Crunch ChicОценок пока нет
- Health System in IndiaДокумент36 страницHealth System in IndiaRishi RanjanОценок пока нет
- Determinants of HealthДокумент30 страницDeterminants of HealthRuchi YadavОценок пока нет
- Hilippines: 1. ContextДокумент16 страницHilippines: 1. ContextMilo PlacinoОценок пока нет
- Overview of The Health System in KenyaДокумент14 страницOverview of The Health System in KenyaJohnas WanderaОценок пока нет
- National Healthy Lifestyle ProgramДокумент6 страницNational Healthy Lifestyle Programmale nurseОценок пока нет
- Ii. Problems and Development Strategies: Problems of The Third World CountriesДокумент21 страницаIi. Problems and Development Strategies: Problems of The Third World CountriesMicsjadeCastilloОценок пока нет
- Health Care Delivery System 8 24 21Документ120 страницHealth Care Delivery System 8 24 21Wilma Nierva BeraldeОценок пока нет
- Overview & Community Pediatrics: DefinitionДокумент3 страницыOverview & Community Pediatrics: DefinitionJessica Febrina WuisanОценок пока нет
- Philippine Health Care Delivery SystemДокумент2 страницыPhilippine Health Care Delivery Systemhana_kimi498270Оценок пока нет
- The Aquino Health AgendaДокумент14 страницThe Aquino Health AgendaIzzah Mei CaballeroОценок пока нет
- Nurs 496 Service Learning PlanДокумент5 страницNurs 496 Service Learning Planapi-377789171Оценок пока нет
- Healthcare Delivery System in PHДокумент13 страницHealthcare Delivery System in PHLloyd SalesОценок пока нет
- Country Cooperation Strategy: IndonesiaДокумент20 страницCountry Cooperation Strategy: Indonesiafauziahputri29Оценок пока нет
- General Biology 2-136-200Документ69 страницGeneral Biology 2-136-200Sab IbarretaОценок пока нет
- Business Mathematics PDFДокумент131 страницаBusiness Mathematics PDFOscar Miranda92% (76)
- Accountancy, Business, and Management 2Документ200 страницAccountancy, Business, and Management 2Sab Ibarreta100% (2)
- Business FinanceДокумент340 страницBusiness FinanceRene Ramilo83% (6)
- Basic CalculusДокумент324 страницыBasic CalculusOrley G Fadriquel73% (11)
- General Biology 2-201-270Документ70 страницGeneral Biology 2-201-270Sab IbarretaОценок пока нет
- General Biology 2-1-135Документ134 страницыGeneral Biology 2-1-135Sab IbarretaОценок пока нет
- The Learners Demonstrate Understandin G Of... The Learners Should Be Able To..Документ3 страницыThe Learners Demonstrate Understandin G Of... The Learners Should Be Able To..Sab IbarretaОценок пока нет
- CIDAM (Gen Bio)Документ3 страницыCIDAM (Gen Bio)Sab IbarretaОценок пока нет
- CIDAM (Gen Bio) MELCДокумент4 страницыCIDAM (Gen Bio) MELCSab Ibarreta100% (1)
- The Learners Demonstrate Understandin G Of... The Learners Should Be Able To..Документ3 страницыThe Learners Demonstrate Understandin G Of... The Learners Should Be Able To..Sab Ibarreta100% (2)
- CIDAM (Religion) MELCДокумент5 страницCIDAM (Religion) MELCSab Ibarreta100% (1)
- MELCs (G7)Документ2 страницыMELCs (G7)Sab IbarretaОценок пока нет
- MELCs (G7)Документ2 страницыMELCs (G7)Sab IbarretaОценок пока нет
- CIDAM (Gen Bio) MELCДокумент4 страницыCIDAM (Gen Bio) MELCSab Ibarreta100% (1)
- MELCs (Biology 1 & 2)Документ5 страницMELCs (Biology 1 & 2)Sab Ibarreta91% (11)
- MELCs (Biology 1 & 2)Документ5 страницMELCs (Biology 1 & 2)Sab Ibarreta91% (11)
- MELCs (G7)Документ2 страницыMELCs (G7)Sab IbarretaОценок пока нет
- MELCs (G7)Документ2 страницыMELCs (G7)Sab IbarretaОценок пока нет
- MELCs (G7)Документ2 страницыMELCs (G7)Sab IbarretaОценок пока нет
- MELCs (Biology 1 & 2)Документ5 страницMELCs (Biology 1 & 2)Sab Ibarreta91% (11)
- Social Distancing GuidelinesДокумент2 страницыSocial Distancing GuidelinesSab IbarretaОценок пока нет
- CIDAM (Gen Bio)Документ3 страницыCIDAM (Gen Bio)Sab IbarretaОценок пока нет
- MELCs (Personal Development)Документ5 страницMELCs (Personal Development)Sab Ibarreta92% (12)
- Mr. and Ms. DPA Talent ScriptДокумент9 страницMr. and Ms. DPA Talent ScriptSab IbarretaОценок пока нет
- Alignment Classroom Instruction Delivery (Acid) Plan Personality Development 12Документ5 страницAlignment Classroom Instruction Delivery (Acid) Plan Personality Development 12Sab IbarretaОценок пока нет
- MELCs (Biology 1 & 2)Документ5 страницMELCs (Biology 1 & 2)Sab Ibarreta91% (11)
- MELCs (Introduction of World Religion and Belief System)Документ9 страницMELCs (Introduction of World Religion and Belief System)Sab Ibarreta84% (25)
- HRM in Higher EducationДокумент19 страницHRM in Higher EducationSab IbarretaОценок пока нет
- Alignment Classroom Instruction Delivery (Acid) Plan Personality Development 12Документ5 страницAlignment Classroom Instruction Delivery (Acid) Plan Personality Development 12Sab IbarretaОценок пока нет
- Case 1394 Moteur 1 2Документ36 страницCase 1394 Moteur 1 2ionel ianosОценок пока нет
- Topics For Oral PresentationДокумент6 страницTopics For Oral PresentationMohd HyqalОценок пока нет
- VERITAS NetBackup 4 (1) .5 On UnixДокумент136 страницVERITAS NetBackup 4 (1) .5 On UnixamsreekuОценок пока нет
- Man of The House Faq: About MothДокумент2 страницыMan of The House Faq: About MothPrapya BarmanОценок пока нет
- Catalyst 4500 SeriesДокумент1 230 страницCatalyst 4500 SeriesnvleninkumarОценок пока нет
- Minimization Z Z Z Z Maximization Z Z : LP IPДокумент13 страницMinimization Z Z Z Z Maximization Z Z : LP IPSandeep Kumar JhaОценок пока нет
- Queen - Hammer To Fall ChordsДокумент3 страницыQueen - Hammer To Fall ChordsDavideContiОценок пока нет
- Bangalore Escorts Services - Riya ShettyДокумент11 страницBangalore Escorts Services - Riya ShettyRiya ShettyОценок пока нет
- Authenticating Digital EvidenceДокумент36 страницAuthenticating Digital Evidenceatty_gie3743Оценок пока нет
- Lite Indicator Admin ManualДокумент16 страницLite Indicator Admin Manualprabakar070Оценок пока нет
- ASM NetworkingДокумент36 страницASM NetworkingQuan TranОценок пока нет
- Grounding & Bonding - The Foundation For Effective Electrical Protection PDFДокумент76 страницGrounding & Bonding - The Foundation For Effective Electrical Protection PDFFabian Nina Aguirre100% (1)
- Cavitation in Francis PDFДокумент373 страницыCavitation in Francis PDFAlberto AliagaОценок пока нет
- Consumer Price SummaryДокумент5 страницConsumer Price SummaryKJ HiramotoОценок пока нет
- PDF RR Grade Sep ProjectsДокумент46 страницPDF RR Grade Sep ProjectsjunqiangdongОценок пока нет
- Dimitris Achlioptas Ucsc Bsoe Baskin School of EngineeringДокумент22 страницыDimitris Achlioptas Ucsc Bsoe Baskin School of EngineeringUCSC Students100% (1)
- Aui2601 Exam Pack 2016 1Документ57 страницAui2601 Exam Pack 2016 1ricara alexia moodleyОценок пока нет
- BMW Engine Wiring 2 OxДокумент4 страницыBMW Engine Wiring 2 OxTomáš TdcОценок пока нет
- Problem SetsДокумент69 страницProblem SetsAnnagrazia ArgentieriОценок пока нет
- MPH EocДокумент8 страницMPH EocGalaleldin AliОценок пока нет
- Case Study StarbucksДокумент2 страницыCase Study StarbucksSonal Agarwal100% (2)
- 11 Stem P - Group 2 - CPT First GradingДокумент7 страниц11 Stem P - Group 2 - CPT First GradingZwen Zyronne Norico LumiwesОценок пока нет
- Kharrat Et Al., 2007 (Energy - Fuels)Документ4 страницыKharrat Et Al., 2007 (Energy - Fuels)Leticia SakaiОценок пока нет
- Presentacion Peaks Rms Lufs Como Usar Medidores FavorДокумент16 страницPresentacion Peaks Rms Lufs Como Usar Medidores Favorhector.obregon.martinezОценок пока нет
- Statistics 2Документ121 страницаStatistics 2Ravi KОценок пока нет
- MBF100 Subject OutlineДокумент2 страницыMBF100 Subject OutlineMARUTI JEWELSОценок пока нет
- Homework 1 Tarea 1Документ11 страницHomework 1 Tarea 1Anette Wendy Quipo Kancha100% (1)
- Chapter 1Документ20 страницChapter 1Li YuОценок пока нет
- BTL - 5000 SWT - Service Manual PDFДокумент158 страницBTL - 5000 SWT - Service Manual PDFNuno Freitas BastosОценок пока нет
- Cuerpos Extraños Origen FDAДокумент30 страницCuerpos Extraños Origen FDALuis GallegosОценок пока нет
- ChatGPT Money Machine 2024 - The Ultimate Chatbot Cheat Sheet to Go From Clueless Noob to Prompt Prodigy Fast! Complete AI Beginner’s Course to Catch the GPT Gold Rush Before It Leaves You BehindОт EverandChatGPT Money Machine 2024 - The Ultimate Chatbot Cheat Sheet to Go From Clueless Noob to Prompt Prodigy Fast! Complete AI Beginner’s Course to Catch the GPT Gold Rush Before It Leaves You BehindОценок пока нет
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicОт EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicОценок пока нет
- The Beekeeper's Lament: How One Man and Half a Billion Honey Bees Help Feed AmericaОт EverandThe Beekeeper's Lament: How One Man and Half a Billion Honey Bees Help Feed AmericaОценок пока нет
- Sully: The Untold Story Behind the Miracle on the HudsonОт EverandSully: The Untold Story Behind the Miracle on the HudsonРейтинг: 4 из 5 звезд4/5 (103)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisОт EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisРейтинг: 4 из 5 звезд4/5 (9)
- Hero Found: The Greatest POW Escape of the Vietnam WarОт EverandHero Found: The Greatest POW Escape of the Vietnam WarРейтинг: 4 из 5 звезд4/5 (19)
- Faster: How a Jewish Driver, an American Heiress, and a Legendary Car Beat Hitler's BestОт EverandFaster: How a Jewish Driver, an American Heiress, and a Legendary Car Beat Hitler's BestРейтинг: 4 из 5 звезд4/5 (28)
- The Fabric of Civilization: How Textiles Made the WorldОт EverandThe Fabric of Civilization: How Textiles Made the WorldРейтинг: 4.5 из 5 звезд4.5/5 (58)
- Reality+: Virtual Worlds and the Problems of PhilosophyОт EverandReality+: Virtual Worlds and the Problems of PhilosophyРейтинг: 4 из 5 звезд4/5 (24)
- Pale Blue Dot: A Vision of the Human Future in SpaceОт EverandPale Blue Dot: A Vision of the Human Future in SpaceРейтинг: 4.5 из 5 звезд4.5/5 (588)
- The End of Craving: Recovering the Lost Wisdom of Eating WellОт EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellРейтинг: 4.5 из 5 звезд4.5/5 (81)
- The Technology Trap: Capital, Labor, and Power in the Age of AutomationОт EverandThe Technology Trap: Capital, Labor, and Power in the Age of AutomationРейтинг: 4.5 из 5 звезд4.5/5 (46)
- A Place of My Own: The Architecture of DaydreamsОт EverandA Place of My Own: The Architecture of DaydreamsРейтинг: 4 из 5 звезд4/5 (242)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineОт EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineОценок пока нет
- How to Build a Car: The Autobiography of the World’s Greatest Formula 1 DesignerОт EverandHow to Build a Car: The Autobiography of the World’s Greatest Formula 1 DesignerРейтинг: 4.5 из 5 звезд4.5/5 (122)
- The Intel Trinity: How Robert Noyce, Gordon Moore, and Andy Grove Built the World's Most Important CompanyОт EverandThe Intel Trinity: How Robert Noyce, Gordon Moore, and Andy Grove Built the World's Most Important CompanyОценок пока нет
- Packing for Mars: The Curious Science of Life in the VoidОт EverandPacking for Mars: The Curious Science of Life in the VoidРейтинг: 4 из 5 звезд4/5 (1395)
- The Weather Machine: A Journey Inside the ForecastОт EverandThe Weather Machine: A Journey Inside the ForecastРейтинг: 3.5 из 5 звезд3.5/5 (31)
- How to Build a Car: The Autobiography of the World’s Greatest Formula 1 DesignerОт EverandHow to Build a Car: The Autobiography of the World’s Greatest Formula 1 DesignerРейтинг: 4.5 из 5 звезд4.5/5 (54)
- The Things We Make: The Unknown History of Invention from Cathedrals to Soda CansОт EverandThe Things We Make: The Unknown History of Invention from Cathedrals to Soda CansОценок пока нет
- Broken Money: Why Our Financial System is Failing Us and How We Can Make it BetterОт EverandBroken Money: Why Our Financial System is Failing Us and How We Can Make it BetterРейтинг: 5 из 5 звезд5/5 (3)