Академический Документы
Профессиональный Документы
Культура Документы
DM in Pregnancy
Загружено:
Patricia YoungИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
DM in Pregnancy
Загружено:
Patricia YoungАвторское право:
Доступные форматы
OBSTERTRICS DIABETES IN PREGNANCY Carbohydrate Metabolism in Early Pregnancy Hormonal alteration: Increased estrogen & progesterone Beta cell
ll hyperplasia Increased insulin secretion Effects Tissue glycogen storage Hepatic glucose production Peripheral glucose utilization Fasting plasma glucose Carbohydrate Metabolism in Late Pregnancy Hormonal change Human placental lactogen (HPL) Prolactin Cortisol Placental growth hormone Tumor necrosis factor Leptin Effects Insulin resistance Diabetogenic Glucose tolerance Hepatic glycogen stores Hepatic glucose production Metabolic change: Facilitated anabolism during feeding, accelerated starvation during fasting to ensure glucose & amino acids to fetus Normal Maternal Glucose Regulation Maternal tendency to develop hypoglycemia between meals & at night while fasting Levels of diabetogenic placental steroid & peptide hormones rise linearly throughout the 2nd & 3rd trimesters: Tissue resistance to maternal insulin Progressive maternal insulin resistance requires augmentation in pancreatic insulin production to maintain euglycemia Failure to augment pancreatic insulin production results in maternal & fetal hyperglycemia Classification of Diabetes during Pregnancy (NDDG) Pregestational Diabetes Type I ( Insulin deficient): Autoimmune disease Destruction of pancreatic cell No insulin production Ketoacidosis Insulin deficient Type II (Insulin Resistant) Resistance to insulin Hyperglycemia Hyperlipidemia Gestational Diabetes: Type III Pregestational Diabetes type I & II Characteristics Type I Ketoacidosis Frequent Age at onset < 40 years old Body habitus Lean HLA type DR3, DR4 Immune markers ICA, IAA Type II Rare > 40 years old Obese None None
Intermediate stage between normal glucose homeostasis & diabetes IFG: Fasting plasma glucose 110mg/dl to 126mg/dl IGT: 2 hour plasma glucose 140mg/dl to 199mg/dl Overt Diabetes Classic signs & symptoms: Polydipsia, polyuria & unexplained weight loss plus Random plasma glucose >200mg/dl or Fasting plasma glucose >/= 126 mg/dl or 2 hour plasma glucose >200mg/dl during a 75gm OGTT Gestational Diabetes Mellitus Glucose tolerance that begins or is first recognized during pregnancy Arises from significant maternal insulin resistance Preclinical Type II diabetes, unmasked by the hormonal stress of pregnancy Screening Low Risk 24-28 weeks 50gm Glucose challenge test Threshold value: 130 mg/dl High Risk 1st trimester screening (Any time it is discovered, request tests immediately) 100gm OGTT or 75gm OGTT if normal repeat at 24-28 weeks 100 gram oral glucose tolerance test (OGTT) mg/dL mmol/L Fasting 95 5.3 1 hour 180 10.0 2 hour 155 8.6 3 hour 140 7.8 Any 2 values elevated = GDM High risk Maternal age >35yrs Previous macrosomic infant Previous unexplained fetal demise Previous pregnancy with GDM Family history of DM Obesity Glucosuria Fetal effects Abortion Congenital anomalies: Cardiac & neural tube defects (Spina bifida) IUGR: Because of vasculopathy Fetal obesity Birth injury: Associated with macrosomia Preterm delivery Unexplained fetal death Maternal effects Diabetic Nephropathy Diabetic Retinopathy Diabetic Neuropathy Preeclampsia Ketoacidosis Infections Neonatal effects
Impaired Glucose Tolerance & Impaired Fasting Glucose CHRABI Page 1 of 2
Respiratory Distress Syndrome: Delays pulmonary maturity Hypoglycemia immediately after birth: High glucose in maternal blood High glucose in fetal circulation High insulin With the withdrawal of continued support of glucose source once delivered Hypoglycemia Hypocalcemia Hyperbilirubinemia Cardiac Hypertrophy Childhood Obesity Childhood Impaired Glucose Tolerance Management of Diabetes during Pregnancy Preconceptional care Metabolic control prior to pregnancy Monitoring of capillary blood glucose (CBG) levels Pre meals: 70 - 100 mg/dl 1 hr post-prandial: < 140 mg/dl 2 hr Post prandial: < 120 mg/dl Hemoglobin A1c: Represents 1-2 months level of blood glucose Smooth glucose control using insulin Folate, 400 ug/day: 1 month prior to conception & all throughout 1st trimester Diabetes in Pregnancy Diet Normal body weight: 30-35 kcal/kg/day Obese: 24 kcal/kg/d Caloric composition: Complex carbohydrates: 40 - 50% Proteins: 20% Unsaturated fats: 30 - 40% Given as 3 meals & 3 snacks daily Insulin therapy Insulin does not pass the placenta Maintain CBG levels as close to normal 1st trimester: 0.7 - 0.8 u/kg/d 2nd trimester - 0.8 -1.0 u/kg/d 3rd trimester - 0.9 - 1.2 u/kg/d Oral hypoglycemics: Not recommended because it can pass the placenta & cause fetal hypoglycemia & teratogenic effects Monitoring of glucose control Capillary glucose monitoring Fasting: </= 95 mg/dl Premeals: </=100 mg/dl 1 hour PP: < 140 mg/dl 2 hour PP: < 120 mg/dl Mean Capillary glucose levels: 100 mg/dl Hgb A1c - 6% Fetal Surveillance Accurate dating Congenital Anomaly Scanning Monitoring of fetal growth Antepartum Fetal Monitoring: Fetal movement counting (FMC), biophysical score (BPS), non-stress test (NST), contraction stress test CST) & uterine artery Doppler velocimetry Timing of Delivery CHRABI Page 2 of 2
Early delivery Vasulopathy, nephropathy, prior stillbirth & poor glucose control Amniocentesis for lung maturity Expectant management Good glucose control Not recommended beyond the estimated due date Insulin Management during Labor & Delivery Usual dose of intermediate-acting insulin is given at bedtime. Morning dose of insulin is withheld. Intravenous infusion of normal saline is begun. Once active labor begins or glucose levels decrease to <70 mg/dl, the infusion is changed to 5% dextrose & delivered at a rate of 100-150 cc/hr to achieve a glucose level of 100 mg/dl Glucose levels are checked hourly. Regular (short acting) insulin is administered by intravenous infusion at a rate of 1.25 U/h if glucose levels exceed 100 mg/dl. Breast feed Yes!!! DUHAWEE HAPPY BIRTHDAY BEEEEMWAH!!!
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Food Exchange Lists For Meal PlanningДокумент13 страницFood Exchange Lists For Meal PlanningPatricia Young63% (24)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Concept Map of DMДокумент2 страницыConcept Map of DMLeslie Marie Rendon100% (9)
- Ob SkedДокумент1 страницаOb SkedPatricia YoungОценок пока нет
- DM in PregnancyДокумент2 страницыDM in PregnancyPatricia YoungОценок пока нет
- Armynavy Menu 2011Документ1 страницаArmynavy Menu 2011Karen Joyce PinedaОценок пока нет
- Armynavy Menu 2011Документ1 страницаArmynavy Menu 2011Karen Joyce PinedaОценок пока нет
- Armynavy Menu 2011Документ1 страницаArmynavy Menu 2011Karen Joyce PinedaОценок пока нет
- Bullous ImpetigoДокумент6 страницBullous ImpetigoPatricia YoungОценок пока нет
- Cases For DiscussionДокумент2 страницыCases For DiscussionPatricia YoungОценок пока нет
- Blood Sugar 455 MG - DL (25.25mmol - L) and What It Means - BloodSugarEasy PDFДокумент4 страницыBlood Sugar 455 MG - DL (25.25mmol - L) and What It Means - BloodSugarEasy PDFSalman KhanОценок пока нет
- Daftar PustakaДокумент8 страницDaftar PustakaErmaffОценок пока нет
- Nutra Puding Buah NagaДокумент2 страницыNutra Puding Buah NagaUun RochmawatiОценок пока нет
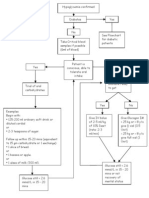
- Hypoglycaemia FlowchartДокумент1 страницаHypoglycaemia FlowchartMohammad SultanОценок пока нет
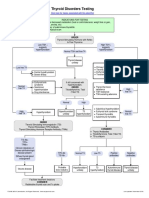
- Thyroid Disorders Testing AlgorithmДокумент1 страницаThyroid Disorders Testing AlgorithmkatОценок пока нет
- Survey of Knowledge-Attitude-Practice (KAP) Concerning Insulin Use in Adult Diabetic Patients at A Tertiary Care HospitalДокумент5 страницSurvey of Knowledge-Attitude-Practice (KAP) Concerning Insulin Use in Adult Diabetic Patients at A Tertiary Care HospitalChandresh DumatarОценок пока нет
- Clew: A37 Cg4+ & G3+ D: I-Stat® Tricontrols Level 1 ControlДокумент4 страницыClew: A37 Cg4+ & G3+ D: I-Stat® Tricontrols Level 1 ControlDominic Isaac AcelajadoОценок пока нет
- Oral Hypoglycemic Drugs2Документ4 страницыOral Hypoglycemic Drugs2علي الطياريОценок пока нет
- THYROID YunitaДокумент81 страницаTHYROID YunitaPandu KusumawardhanyОценок пока нет
- Gliclazide MR, An Efficacy and Safety: For T2DM Patients During RamadanДокумент28 страницGliclazide MR, An Efficacy and Safety: For T2DM Patients During RamadanLeonora KomboyОценок пока нет
- Endocrine Glands PathologyДокумент8 страницEndocrine Glands Pathologychrisp7Оценок пока нет
- Insulin Case Studies AACE 5-20-05Документ56 страницInsulin Case Studies AACE 5-20-05Leanne Shepherd100% (2)
- Thyroid Disorders Testing AlgorithmДокумент1 страницаThyroid Disorders Testing AlgorithmRezi HelperОценок пока нет
- List of Endocrine DiseasesДокумент6 страницList of Endocrine DiseasesPreethiHonavarОценок пока нет
- Gestational DiabetiesДокумент50 страницGestational DiabetiesAkshat Goel100% (1)
- Practical Clinical Endocrinology 2021Документ523 страницыPractical Clinical Endocrinology 2021Morozovschi VitalieОценок пока нет
- Goiter: What Is The Thyroid Gland?Документ2 страницыGoiter: What Is The Thyroid Gland?Julio LeviОценок пока нет
- Garber 2007Документ6 страницGarber 2007Diana SamuezaОценок пока нет
- Thyroid Function TestДокумент31 страницаThyroid Function TestMeno AliОценок пока нет
- Gestational Diabetes Mellitus: Definition, Aetiological and Clinical AspectsДокумент9 страницGestational Diabetes Mellitus: Definition, Aetiological and Clinical AspectsantonellamartОценок пока нет
- Endocrine Pathology LectureДокумент31 страницаEndocrine Pathology Lectureninja2007Оценок пока нет
- Dexamethasone Suppression TestДокумент2 страницыDexamethasone Suppression Testjbeans92Оценок пока нет
- 592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMДокумент2 страницы592008000011: 59000720 03-Aug-20 08:49 AM: Mrs. Veena K Arora: 03-Aug-2020 08:49 AM: Dr. Self: 03-Aug-2020 12:47PM: 48 Y 06 M 12 D / F: 03-Aug-2020 01:12PMrajanarora72Оценок пока нет
- Discuss Di Erence Between Diabetes Mellitus Type 1 and DM Type 2Документ3 страницыDiscuss Di Erence Between Diabetes Mellitus Type 1 and DM Type 2DHANNILLIE JHAIRA NU�EZОценок пока нет
- A1C InfographicДокумент1 страницаA1C Infographiclewisch81Оценок пока нет
- Endocrine Disorders Julie Mann, NP - Case StudyДокумент10 страницEndocrine Disorders Julie Mann, NP - Case Studysimonedarling75% (4)
- THYROID Nodules PPT June 2013Документ56 страницTHYROID Nodules PPT June 2013GaryОценок пока нет
- GoiterДокумент17 страницGoiterShaimaa EmadОценок пока нет
- Endemic and Sporadic GoiterДокумент13 страницEndemic and Sporadic GoiterBtwo SoelОценок пока нет