Академический Документы
Профессиональный Документы
Культура Документы
Cateterizacion Femoral en Perro
Загружено:
alebenech1570Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cateterizacion Femoral en Perro
Загружено:
alebenech1570Авторское право:
Доступные форматы
Case Series
Journal of Veterinary Emergency and Critical Care 18(3) 2008, pp 306311 doi:10.1111/j.1476-4431.2008.00309.x
Freehand ultrasound-guided femoral arterial catheterization in dogs
Steven A. Ringold, DVM and Efrat Kelmer, DVM, DACVECC
Abstract
Objective: To demonstrate that ultrasound-guided femoral artery catheterization is feasible and practical in dogs. Case series summary: Four female mixed breed dogs weighing 1423 kg were used following a terminal junior surgery laboratory and had been anesthetized before the ultrasound study. Dogs were positioned in lateral recumbency with the upper limb abducted and immobilized. The dependent limb was extended and shaved and isopropyl alcohol was applied. An ultrasound transducer was oriented transverse to the axis of the limb and, following ultrasonographic identication, the femoral artery was cannulated and a catheter was placed using the Seldinger technique. Ultrasound-guided catheterization was successful in 9 of 10 attempts; cannulization was successful in 10 of 10 attempts. Procedure time improved from 10 minutes to 1 minute during practice. Each of the 2 investigators was able to simultaneously ultrasound and cannulate the vessel. The major complication was hematoma formation, which occurred regardless of success. Information provided: Ultrasound-guided femoral artery catheterization is feasible and relatively easy to master in medium-size, anesthetized dogs. (J Vet Emerg Crit Care 2008; 18(3): 306311) doi: 10.1111/j.1476-4431.2008.00309.x
Keywords: interventional, radiology, vascular access
Introduction
Vascular access is fundamental in diagnosing and treating a multitude of conditions and diseases. Arterial catheters are used to obtain blood samples and direct arterial blood pressure measurements or to facilitate access for interventional radiology techniques. There is a particularly strong application for critical patients, anesthetized patients, and interventional cardiovascular procedures. The landmark method, which relies on recognition of anatomic landmarks by palpation and sight, is prone to inadvertent puncture of the femoral vein and is challenging in patients who are small in size, obese, or hypotensive, or who have local hematoma formation, peripheral edema, or arterial thrombosis.1 When percutaneous catheterization is unsuccessful or not feasible, a surgical approach may be indicated.
From the Department of Veterinary Medicine and Surgery, University of Missouri, College of Veterinary Medicine, Columbia, MS. Dr. Kelmers current address: College of Veterinary Medicine, The University of Tennessee, 2407 River Drive, Knoxville, TN 37996. Address correspondence and reprint requests to: Dr. Steven A. Ringold, Veterinary Medical Teaching Hospital, 379 E. Campus Dr., Columbia, MO 65211 E-mail: ringolds@missouri.edu
Surgical cutdown is invasive, may require ligation of the vessel when the position is relinquished, and may cause neuropraxia of nearby nerves.2,3 In human patients, ultrasound guidance is often employed in the critical setting or to gain vascular access for patients undergoing anesthesia and has been demonstrated to decrease catheter placement failure, decrease complications during catheter placement, decrease procedure time, and decrease the need for multiple attempts when compared to the landmark technique.48 Ultrasound-guided catheterization of the femoral artery has been shown to be feasible and safe in humans.9 The femoral artery is the distal continuation of the external iliac artery and courses along the medial aspect of the femur. Proximally, within the femoral triangle, the femoral artery lies cranial to the femoral vein and caudal or medial to the saphenous nerve. The femoral triangle is formed by the sartorius muscle cranially, the pectineus muscle caudally, and the iliopsoas and vastus medialus muscles laterally. Within the triangle, the femoral artery is covered only by the deep medial femoral fascia and a thin layer of skin and provides a convenient place for vascular access. Distal to the triangle, the vessels are covered by the caudal belly of
& Veterinary Emergency and Critical Care Society 2008
306
Ultrasound-guided femoral catherization
the semimembranosus muscle and, in relation to the femur, course caudodistally, crossing the mid to distal third of the femoral diaphysis at an angle of approximately 351.10 Using a 712 MHz ultrasound transducer, the femoral artery is easily recognized and differentiated from the adjacent femoral vein and nearby structures. The purpose of this report is to describe a technique for obtaining ultrasound-guided femoral artery access in healthy dogs.
Materials and Methods
Equipment A portable ultrasound machinea with a 12 MHz linear transducer was used for the procedure. B-mode color ow Doppler was used with the rst dog. Arterial punctures were performed using the introducer needle from a central venous catheter setb and the Seldinger technique.11 After cannulating the vessel with an introducer needle, a guide wire was placed into the vessel lumen through the introducer, which was then removed. A dilator was then passed over the wire and, following removal of the dilator, a catheter was placed and secured. Animals Four adult female mixed breed dogs of average body condition, weighing 23.1, 22.7, 22.4, and 14.5 kg, were used for this study. The dogs were used in conjunction with an ultimately terminal junior surgery laboratory and had been anesthetized 45 hours before this ultrasound study. Dogs were premedicated with atropinec (0.04 mg/kg, IM), xylazined (0.5 mg/kg, IM), and morphinee (0.5 mg/kg, IM), and induced with thiopentalf (10 mg/kg or to effect, IV). All 4 dogs had fair to poor peripheral pulse quality at the start of this investigation. The dogs were euthanized at the end of the study with a pentobarbital (390 mg/mL) and phenytoin (50 mg/mL) solutiong (0.22 mL/kg, IV). This study was approved by the Animal Care and Use Committee at the University of Missouri-Columbia. Procedure Each dog was placed in lateral recumbency with the non-dependent hind limb abducted and immobilized; a strap was wrapped around the distal tibia and metatarsus and tethered to the table. The dependent limb was extended and clipped over the femoral artery. A single investigator performed each procedure, simultaneously directing the ultrasound transducer and catheterizing the vessel. Two investigators carried out the procedures, both of whom were enrolled in residency programs, one in radiology and one in emergency and critical care, at the time of this study.
Figure 1: Orientation of the ultrasound transducer and introducer needle during catheterization of the femoral artery in a dog.
Coupled with alcohol, the transducer was applied to the skin over the femoral triangle, transverse to the axis of the limb. The femoral artery and vein were located. A 16 or 18 G introducer needle was inserted, from a distal to proximal direction, into the subcutaneous tissues, just distal to the transducer (Figure 1). The site of insertion was subjectively selected to be as far distal as possible without compromising visibility of the vessels while simultaneously sparing the proximal vessel for subsequent catheterization attempts. This area was typically located at about the level of the mid-diaphysis of the femur. Using a freehand technique, the introducer was inserted by tenting the skin and forming an angle of about 10301 between the introducer and the plane of the skin. Freehand implies alignment of the needle with the transducer and target structure in the absence of an attachable needle guide. An alternate technique uses a needle guide which connects rmly to an ultrasound transducer and simultaneously aligns a needle, subsequently attached to the guide, with the image plane and target structure to enable precise direction of the needle into the target. To locate the introducer needle, the transducer was replaced on the skin, transverse to the axis of the limb, and directly over the needle, at 901 to the plane of the needle. The introducer needle appeared as a hyperechoic focus with variable distal acoustic shadowing and reverberation. After the needle was identied, the transducer was slid proximally to identify the needle tip. The tip was then directed toward the femoral artery by advancement or lateral movement of the needle, keeping the tip in view. Once the tip was positioned over the artery, it was advanced into the vessel with a smooth yet deliberate motion. Correct placement of the catheter was veried by back ow of pulsating, arterial blood. Once the artery was cannulated, the transducer was removed and
307
& Veterinary Emergency and Critical Care Society 2008, doi: 10.1111/j.1476-4431.2008.00309.x
S.A. Ringold & E. Kelmer
Figure 2: Sagittal image of the near and far walls of the femoral artery (arrowheads) with an 18 G catheter (arrow) occupying the lumen.
vascular access was completed with the Seldinger technique.11 Ultrasound, in either the transverse or sagittal planes, was used to conrm proper catheter placement (Figure 2). External pressure was applied for no more than 5 minutes over the point of insertion following each of these steps to avoid hematoma formation. The procedure was performed 10 times, using both femoral arteries from all 4 dogs. Two femoral arteries were cannulated twice immediately after cessation of tamponade, using a more distal puncture site than the previous. Further, it was possible to apply pressure to the initial puncture site with the transducer while simultaneously using it to guide the subsequent puncture.
Figure 3: Transverse image of the femoral artery (arrowhead) and vein (arrow) with 12 MHz transducer at the level of the mid femoral diaphysis. The medial surface of the femur is seen as a curvilinear, hyperechoic line.
Results
Femoral arterial cannulization was successful on all attempts. The initial attempt took approximately 10 minutes for each investigator. Comfort with the procedure improved and procedure duration decreased quickly with subsequent attempts. For both investigators, aside from the initial attempt, the time from location of the vessel to successful cannulization varied from 1 to 6 minutes. Each investigator performed 5 catheterizations. Although subjective, there was no obvious intra-observer variation in ability or time to cannulate the vessel. To the authors knowledge, the femoral vein was not punctured in any instance. Hematoma formation was subjectively judged to be moderate or severe based on the amount of soft tissue swelling present. Swelling was more severe in cases in which pressure was applied for shorter periods of time. Tamponade was applied for no more than 5 minutes on any dog. There was difculty advancing the guide wire in one case and so catheterization was aborted. Although this attempt did not result in placement of a catheter, cannulization was successful. There was no perceived increase in difculty in cannulating the 2 arteries that
308
had previously been catheterized. In another case, a small amount of subcutaneous air, seen as a strongly hyperechoic region with indistinct distal acoustic shadowing, obfuscated the vessel and required repositioning and introduction of the needle slightly more proximal than initially intended. Sonographically, the femoral artery and vein and their anatomic relationships were easily recognized. Using a 12 MHz, linear transducer oriented transversely, the vessels were seen as two intimately associated ovoid structures, hypoechoic to the surrounding tissues (Figure 3). The femoral artery was consistently seen as a smaller, cranial, pulsating structure whereas the femoral vein was larger, caudal and failed to pulsate. On the rst attempt, B-mode color-ow Doppler was initially used, but interfered with needle visualization as the investigators attempted to puncture the artery. Therefore, its use was abandoned thereafter. In all dogs, identication of the vessels without color ow was not difcult. The femur appeared as a relatively hyperechoic, semicircular line in the far eld. Proximally, the femoral artery and vein were seen in the near eld, medial and slightly cranial to the femur. At the level of the mid third of the femur, the vessels were medial to caudomedial to the femur and, by the level of the distal third of the femur, they were caudal to the femur and deep to the semimembranosus muscle. The semimembranosus muscle was seen as a relatively
& Veterinary Emergency and Critical Care Society 2008, doi: 10.1111/j.1476-4431.2008.00309.x
Ultrasound-guided femoral catherization
hypoechoic structure with multiple hyperechoic foci and faint hyperechoic striations. If the introducer needle was not immediately apparent after inserting it through skin, it was helpful to wiggle it slightly, taking care not to damage a vessel, to discern its position as it related to the vessels in a cranial to caudal direction. The needle was most apparent at an angle of approximately 101 to the skin and close to 901 to the transducer. In order to manipulate the introducer, it was necessary to increase this angle to 20301 to the skin (effectively, a 20301 to the femoral artery) reducing the angle with the transducer to 60701 and slightly decreasing needle conspicuity. To restore needle distinction, it was possible to angle the probe 10151 distally before adversely affecting transducerskin contact and impairing the image. This change re-established a 70801 angle between the needle and transducer, slightly improving needle conspicuity.
Discussion
This study demonstrates that obtaining ultrasoundguided femoral artery catheterization is feasible and relatively easy in anesthetized medium-sized dogs. Access to the femoral artery in veterinary patients permits continuous direct blood pressure measurements and sample collection for lab work and arterial blood gas analysis in emergent, critical, and anesthetized patients as well as research dogs. Many interventional radiology procedures, such as angiocardiography, vascular occlusion, stenting, and embolization require arterial access. Additionally, some research procedures rely on arterial catheterization. Typically, catheterization of the femoral artery is achieved using palpation and landmarks or by a surgical cut-down procedure. Ultrasound guidance is quick and effective in establishing a femoral arterial position and may be particularly benecial in patients with complicating conditions. Several studies in the human literature comparing ultrasound-guided to the landmark technique for venous access demonstrate that the former technique is associated with higher success rates during the rst attempt and shorter procedure times.1,8,12,13 In this study, all vessels were easily identied and were in their expected anatomic locations. B-mode color ow Doppler may aid in the initial identication of the vessels, particularly in small and hypovolemic patients, but in this study it interfered with needle tip identication at the moment of arterial puncture. If the femoral artery and vein are difcult to distinguish from each other due to altered anatomical relationship or other cause, pulsed wave Doppler may allow this determination to be made. Arteries and veins can be
identied by their characteristic Doppler ow indices noted with pulsed wave Doppler. Pulsed wave Doppler uses sound pulses coupled with measurement of the time delay for echoes to return to the transducer. This information enables determination of the precise location of a structure. Echoes from this precise location can be selectively listened for, in this case at the location of the vessel lumen, to produce an echo pattern consistent with the blood ow of that vessel.14 A freehand method of needle direction was used for this study as it was deemed more practical for application in a veterinary emergency and critical care practice due to its simplicity and exibility relative to the more cumbersome, but theoretically more precise, method of using a needle guide. Sonographic recognition of the introducer needle requires an understanding of some basic ultrasound principles. Ultrasound imaging is based on a combination of sound transmission, reection, and refraction. Transmission, reection, or refraction of sound is determined by the angle of the sound beam and the acoustic impedance of the substances in which it is travels. Acoustic impedance is a product of the density of the substance and the velocity at which sound travels within that substance. Sound travels at 1540 m/s in the average soft tissue and at approximately 6400 m/s in metals, imparting a great variation in acoustic impedance between the 2 substances.14,15 This difference is known as acoustic mismatch and the larger the mismatch, the more sound is reected at the interface of the 2 substances. The large acoustic mismatch between a needle and soft tissue creates specic artifacts that facilitate recognition of the needle when sound, traveling through that tissue, encounters the needle. On transverse section, the needle will appear as an intensely hyperechoic focus with varying degrees of distinct, distal acoustic shadowing and reverberation (Figure 4). Distal acoustic shadowing occurs from nearly complete reection of the sound pulse wave by the needle, creating an area of relative hypoechogenicity deep to the reecting structure. Reverberation appears as a series of equally spaced, hyperechoic lines, deep to the reector and is created by sound bouncing back and forth between the transducer and the reector.16 When puncturing the artery, it was necessary to advance the needle with a smooth yet deliberate motion. Otherwise the needle tended to roll off the artery. A relief incision to facilitate vascular puncture was not considered for this study, but may have facilitated the procedure. Optimal needletransducer angles have been previously assessed.17,18 All angles described in this study are subjective as it was not the primary intent of this paper to assess optimal needle
309
& Veterinary Emergency and Critical Care Society 2008, doi: 10.1111/j.1476-4431.2008.00309.x
S.A. Ringold & E. Kelmer
Figure 4: Reverberation artifact (arrowheads) off the tip of an introducer needle (arrow).
transducer angles. Optimal needle conspicuity occurs at an angle of 901 between the needle and transducer and decreases with decreasing angle.19 However, needles are still seen clearly with an angle of 601 to the transducer. Therefore, by positioning the needle at 20301 to the skin and the transducer perpendicular to the skin, an angle of 60901 between the transducer and needle is achieved, producing good needle conspicuity. The needle tip conspicuity is greatest with the bevel facing the transducer or 1801 to it.18 Wiggling the needle does make it more apparent, but one must do so cautiously and minimally to avoid lacerating the vessel.19 The most common complication that was encountered in our study was hematoma formation, which occurred after each puncture. Hematomas were subjectively judged to be more severe in cases with shorter tamponade times. Hematomas did not appear to be more severe in the 2 vessels that were punctured more than once and additional punctures were not encumbered by prior cannulation. It is possible that the severity of hematoma formation could have been reduced by avoiding dilation of the artery. It has been our clinical experience during venous catheterization that dilation is not always necessary for successful catheterization. Another possibility would be to use a pediatric or micropuncture introducer needle. In humans, hematoma formation is comparable in both the landmark and ultrasound guided techniques.8 To obtain hemostasis, it is recommended that rm
310
pressure be applied for 1520 minutes to the arterial puncture site after a canula or catheter has been removed.2 In this series, pressure was applied for less than 5 minutes after the procedure, resulting in severe hematoma formation in some instances. A hematoma may also form if the femoral vein is inadvertently punctured; this complication was not observed in this study. One of the presumed benets of ultrasound guidance is decreased incidence of femoral vein puncture. By observing the needle tip before and during advancement, this problem can be minimized. Severe thrombocytopenia, thrombocytopathia, coagulopathies, hypercoagulable states, and disease at the site of insertion are contraindications for arterial catheter placement. A patients coagulation status should be assessed before catheter placement to avoid life-threatening hemorrhage following the procedure.2 Another complication that was seen in this study was the inadvertent introduction of air into subcutaneous tissues. In one case, when attaching a syringe to the introducer hub after the needle was already placed through the skin, a small amount of air was deposited subcutaneously. There is a substantial acoustic mismatch between soft tissue, which transmits sound at 1540 m/s, and air, which transmits sound at 331 m/s.14,15 Because of this mismatch, sound is almost entirely reected at the soft tissue gas interface, creating distal acoustic shadowing and reverberation artifacts and thus obscuring the sonographic image of the vessels. In this study with medium size dogs, this occurrence was not a problem as it was easy to insert the introducer and observe the artery proximal to the subcutaneous gas, although doing so did require an additional skin puncture. In smaller animals with a more limited vessel length, subcutaneous air could sufciently degrade an image, interfering with canula guidance. To address this difculty, a saline lled syringe may be attached to the introducer hub before puncture. This practice has the added benet of preventing blood clot formation in the needle lumen, but may prevent recognition of arterial puncture as a pulsating blood backow will not be as likely to occur. Difculty passing the wire occurred in 1 instance after feeding it approximately 5 cm proximally for an unknown reason. Possible explanations include subendothelial insertion, suboptimal needle angle, or blood clot. Keeping the angle of the introducer o451 to the artery will facilitate smooth passage of the guide wire and decrease the possibility of passing the wire intramurally.20 It is the authors opinion that this complication was not related to the method of cannulization and that it may have occurred just as easily using the landmark method.
& Veterinary Emergency and Critical Care Society 2008, doi: 10.1111/j.1476-4431.2008.00309.x
Ultrasound-guided femoral catherization
This study has some limitations. Because the dogs were part of a terminal study, they were not recovered from anesthesia and therefore assessment of catheter placement effect on gait or neurological function of the limb could not be made. Additionally, all the dogs in this study were medium-sized dogs with average body condition and presumed mild to moderate hypotension, representing relatively close to ideal conditions. Ultrasound-guided femoral arterial catheterization in patients with complicating factors may not be as easy to perform. Hypotension was not quantitatively documented in these dogs and is open to question, but was presumed to be present in all 4 dogs based on pulse quality and the duration of the anesthetic period before initiation of this investigation. Hypotension should be quantied in future studies. Femoral artery catheterization has many clinical applications in addition to research applications. Ultrasound-guided canalization provides an efcient means of establishing arterial access with minimal complications. Future direction for study should include comparisons between the landmark and freehand ultrasound-guided methods of femoral arterial catheterization to evaluate the complication rate, failure rate, and length of procedure. Future studies could evaluate application of the technique described here in dogs that are severely hypotensive, small in size, or obese. Ultrasound guidance for establishing carotid artery and central venous access should also be investigated.
Footnotes
a b c d e f g
GE Logic 500 Ultrasound System, General Electric, Faireld, CT. Central Venous Catheter, Cook Incorporated, Bloomington, IN. Atropine, Phoenix, St. Joseph, MO. Xyla-ject, Phoenix. Morphine, Baxter, Deereld, IL. Pentothal, Abbott, North Chicago, IL. Ethasol solution, Virbac Animal Health, Fort Worth, TX.
Acknowledgements
The authors would like to thank Drs. Jimi Cook and Tony Mann for providing the subjects used in this study.
References
1. Schwemmer U, Arzet HA, Trautner H, et al. Ultrasound-guided arterial cannulation in infants improves success rate. Eur J Anaesthesiol 2006; 23(6):476480.
2. Beal MW, Hughes D. Vascular access: theory and techniques in the small animal emergency patient. Clin Tech Small Anim Pract 2000; 15(2):101109. 3. Parsa MH, Parsa CJ, Sampath AC. Intravenous and intra-arterial access, In: Grenvik AKE, Ayres SM, Holbrook PR, Shoemaker WC, eds. Textbook of Critical Care, 4th edn. Philadelphia: W. B. Saunders Company; 2000, pp. 5974. 4. Brederlau J, Greim C, Schwemmer U, et al. Ultrasound-guided cannulation of the internal jugular vein in critically ill patients positioned in 30 degrees dorsal elevation. Eur J Anaesthesiol 2004; 21(9):684687. 5. Randolph AG, Cook DJ, Gonzales CA, et al. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med 1996; 24(12):20532058. 6. Levin PD, Sheinin O, Gozal Y. Use of ultrasound guidance in the insertion of radial artery catheters. Crit Care Med 2003; 31(2):481 484. 7. Verghese ST, McGill WA, Patel RI, et al. Ultrasound-guided internal jugular venous cannulation in infants: a prospective comparison with the traditional palpation method. Anesthesiology 1999; 91(1):7177. 8. Miller AH, Roth BA, Mills TJ, et al. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Acad Emerg Med 2002; 9(8):800805. 9. Yeow KM, Toh CH, Wu CH, et al. Sonographically guided antegrade common femoral artery access. J Ultrasound Med 2002; 21(12):14131416. 10. Hermanson J, Evans H. Muscles of the pelvic limb, In: Evans H. ed. Millers Anatomy of the Dog, 3rd edn. Philadelphia: W. B. Saunders; 1993, pp. 349384. 11. Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta radiol 1953; 39(5): 368376. 12. Farrell J, Gellens M. Ultrasound-guided cannulation versus the landmark-guided technique for acute haemodialysis access. Nephrol Dial Transplant 1997; 12(6):12341237. 13. Chuan WX, Wei W, Yu L. A randomized-controlled study of ultrasound prelocation vs anatomical landmark-guided cannulation of the internal jugular vein in infants and children. Paediatr Anaesth 2005; 15(9):733738. 14. Nyland T, Matoon J, Herrgesell E, et al. Physical principles, instrumentation, and safety of diagnostic ultrasound, In: Nyland T, Matoon J. eds. Small Animal Diagnostic Ultrasound, 2nd edn. Philadelphia: W. B. Saunders; 2002, pp. 118. 15. Wells P. Physical Principles of Ultrasonic Diagnosis. New York: Academic Press Inc.; 1969, 5pp. 16. Pennick D. Artifacts, In: Nyland T, Matoon J. eds. Small Animal Diagnostic Ultrasound, 2nd edn. Philadelphia: W. B. Saunders Company; 2002, pp. 1929. 17. Bradley MJ. An in-vitro study to understand successful freehand ultrasound guided intervention. Clin Radiol 2001; 56(6): 495498. 18. Hopkins RE, Bradley M. In-vitro visualization of biopsy needles with ultrasound: a comparative study of standard and echogenic needles using an ultrasound phantom. Clin Radiol 2001; 56(6):499 502. 19. Bisceglia M, Matalon TA, Silver B. The pump maneuver: an atraumatic adjunct to enhance US needle tip localization. Radiology 1990; 176(3):867868. 20. Axelrod DJ, Freeman H, Pukin L, et al. Guide wire perforation leading to fatal perirenal hemorrhage from transcortical collaterals after renal artery stent placement. J Vasc Interv Radiol 2004; 15(9):985987.
& Veterinary Emergency and Critical Care Society 2008, doi: 10.1111/j.1476-4431.2008.00309.x
311
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Trauma C1 C2Документ8 страницTrauma C1 C2Karen OrtizОценок пока нет
- FJMCW Lahore MbbsДокумент9 страницFJMCW Lahore MbbsRayan ArhamОценок пока нет
- Nutritional assessment pregnancy lactationДокумент11 страницNutritional assessment pregnancy lactationKathleen Martinez100% (1)
- Hamer - Five Laws - Cancer Congress PDFДокумент23 страницыHamer - Five Laws - Cancer Congress PDFFelipe Gomes100% (1)
- BD TTM Neuro Brochure Update Feb 2020 - v1Документ2 страницыBD TTM Neuro Brochure Update Feb 2020 - v1Hanh NguyenОценок пока нет
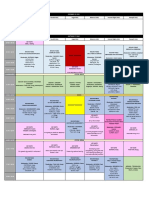
- 2019 International Symposium on Pediatric Audiology ScheduleДокумент3 страницы2019 International Symposium on Pediatric Audiology ScheduleEulalia JuanОценок пока нет
- New Microsoft Office Word DocumentДокумент2 страницыNew Microsoft Office Word DocumentAnam BukhariОценок пока нет
- 1.01 Introduction To EpidemiologyДокумент3 страницы1.01 Introduction To EpidemiologyPim AramОценок пока нет
- Understanding BenzodiazepinesДокумент7 страницUnderstanding BenzodiazepinesChris Patrick Carias StasОценок пока нет
- Prosthetic Management - Transtibial Amputation Part 12Документ25 страницProsthetic Management - Transtibial Amputation Part 12Marizandi BothaОценок пока нет
- G128 0066721 MSDSДокумент8 страницG128 0066721 MSDSfiguev2208Оценок пока нет
- FOR35 5crAB06 PDFДокумент32 страницыFOR35 5crAB06 PDFFleRexОценок пока нет
- Biology 1610 E-Portfolio Assignment PDFДокумент4 страницыBiology 1610 E-Portfolio Assignment PDFapi-437601454Оценок пока нет
- Grievous WoundsДокумент3 страницыGrievous WoundsBsalesОценок пока нет
- Steroid Tapering and Supportive Treatment Guidance V1.0 PDFДокумент1 страницаSteroid Tapering and Supportive Treatment Guidance V1.0 PDFNthutagaol TrusОценок пока нет
- Hubungan Antara Abdominal Perfusion Pressure: (App) Dengan Outcome Post OperasiДокумент17 страницHubungan Antara Abdominal Perfusion Pressure: (App) Dengan Outcome Post OperasidrelvОценок пока нет
- Chapter 33 Prescott Innate Immunity PDFДокумент7 страницChapter 33 Prescott Innate Immunity PDFneeru.bhagatОценок пока нет
- Merged Document 14 PDFДокумент9 страницMerged Document 14 PDFMurali SmatОценок пока нет
- CHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.Документ2 страницыCHC Jawa Hub: Jawa, Rewa, Madhya Pradesh Rewa Madhya Pradesh - 486223 Phone No.MAHESH GAUTAMОценок пока нет
- Venous Leg UlcersДокумент28 страницVenous Leg UlcersamurachОценок пока нет
- Anxiety Disorder: Student Name: Malinda SirueДокумент9 страницAnxiety Disorder: Student Name: Malinda SirueEsmareldah Henry SirueОценок пока нет
- Reading Task 1-Breast Cancer and The ElderlyДокумент6 страницReading Task 1-Breast Cancer and The ElderlyJats_Fru_1741100% (5)
- Gingival Periodontal IndexДокумент23 страницыGingival Periodontal Indexxodia_04100% (3)
- Propofol Infusion SyndromeДокумент7 страницPropofol Infusion SyndromewadejackОценок пока нет
- Postpartum Hemorrhage Nursing CareДокумент3 страницыPostpartum Hemorrhage Nursing CareClaire Canapi BattadОценок пока нет
- Endovenous Microwave Ablation of Great Saphenous VeinДокумент3 страницыEndovenous Microwave Ablation of Great Saphenous VeinMalekseuofi مالك السيوفيОценок пока нет
- Vastarel MR 35mgДокумент1 страницаVastarel MR 35mgPhil Edgar Contreras RNОценок пока нет
- Achilles Tendon Conditions Signs and SymptomsДокумент1 страницаAchilles Tendon Conditions Signs and SymptomsTessa DagutОценок пока нет
- Schizophrenia - Practice Essentials, Background, PathophysiologyДокумент10 страницSchizophrenia - Practice Essentials, Background, PathophysiologydilaОценок пока нет
- Glossary of EMTДокумент5 страницGlossary of EMTErnan BaldomeroОценок пока нет