Академический Документы
Профессиональный Документы
Культура Документы
Integrative Physiology Approach to Salt and Water Balance Disorders
Загружено:
diomer123Исходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Integrative Physiology Approach to Salt and Water Balance Disorders
Загружено:
diomer123Авторское право:
Доступные форматы
Crit Care Clin 18 (2002) 249 272
Clinical approach to disorders of salt and water balance Emphasis on integrative physiology
Mitchell L. Halperin, MD, FRCPC a,*, Desmond Bohn, MB, FRCPC b
a Division of Nephrology, St. Michaels Hospital and the University of Toronto, St. Michaels Hospital Annex, 38 Shuter Street, Toronto, Ontario, M5B 1A6, Canada b Department of Critical Care Medicine of the Hospital for Sick Children, and the Department of Anaesthesia, The University of Toronto, 555 University Ave., Toronto, Ontario, M5G 1X8 Canada
With our current emphasis on subspecialty medicine, consultants suggest possible diagnoses and treatments for patients who have abnormalities within their areas of expertise. The medical team responsible for the care of that patient must integrate these suggestions into an overall management plan. Therefore, teamwork is especially important for the care of a patient. The underlying basis for a given disorder may be revealed when an integrative analysis is performed. Some defects may only become evident during therapy. These challenges are especially important for problems in fluid and electrolyte balance in an intensive care unit (ICU) setting because they may become lifethreatening very rapidly. How to anticipate and avoid these dangers is illustrated in the context of case examples selected for presentation in this article. There are two different, but not mutually exclusive, ways to arrive at a clinical diagnosis and to design its therapy when the problem is in the salt and water area. The more traditional approach begins with data from the history, physical examination, and laboratory tests. This information is used to generate a list of possible causes of the disorder. Our approach differs in that it begins with the application of simple principles of physiology at the bedside (Table 1) [5]. It relies on deductive reasoning and a quantitative analysis. The starting point is defined by the consulting service what they believe to be most critical for their patient.
* Corresponding author. E-mail addresses: mitchell.halperin@utoronto.ca (M.L. Halperin), dbohn@sickkids.ca (D. Bohn). 0749-0704/02/$ - see front matter D 2002, Elsevier Science (USA). All rights reserved. PII: S 0 7 4 9 - 0 7 0 4 ( 0 1 ) 0 0 0 0 8 - 2
250
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
Table 1 Physiologic principles used at the bedside Physiologic principle Polyuria Urine volume = Osm/UOsm Use at the bedside Divide polyuria into: Osmotic diuresis if > 1000 mOsm/d Organic solutes Examine filtered load Seek metabolic origin (e.g., urea) Electrolytes (were they infused?) Water diuresis (Uosm < Posm) UOsm a osm excretion and flow rate Main threat is change in brain ICF volume Na+ content reflects the ECF volume Basis revealed by tonicity balance Identify cause for the release of vasopressin NaCl, K+ wasting and concentrating defect Can be induced by cations (gentamicin) Confirmed by urea (572 mmol/100 g protein) Therapy with exogenous protein anabolics Ask if acute ( < 48 h) = increased brain ICF volume Risk factors = young age, women, increased ECF volume Urgent therapy 3% saline Retained lavage fluid = different Most are chronic (danger is ODS) Seek reason for vasopressin, especially if a reversible cause might be present Treat slowly ( < 9 mmol/L/d); slower if K+ deficit or malnourished
Impact of a change in PNa PNa inversely related to ICF volume Hypernatremia Caused by Na+ gain or water deficit Calcium receptor in the loop of Henle Creates furosemide-like effect Catabolic state Protein oxidation causes urea appearance Hyponatremia Find source of EFW and vasopressin Calculate new ICF volume Calculate ECF Na+ content Assess possible K+ deficiency
Abbreviations: U = urine; P= plasma.
To make this article interactive, we pause periodically and ask the reader questions to consider prior to providing our discussion of that issue. In each case, there is an abnormal plasma sodium (Na+ ) concentration (PNa) in an ICU setting.
Polyuria and hypernatremia Illustrative case 1 Polyuria (current urine flow rate 10 ml/min) developed suddenly in a 14-year-old boy (weight 50 kg, total body water 30 liters) during resection of a craniopharyngeoma. His PNa rose from 140 to 155 mmol/ over 6 hours. He was given 3 liters of isotonic saline intravenously and his urine output was 4 liters. He had also received an infusion of mannitol. The aim of the consult was to define goals of therapy for this patient.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
251
Initial quantitative analysis The urine flow rate of 10 ml/min, if extrapolated over 24 hours, is equivalent to 14.4 liters per day. This volume exceeds the patients extracellular fluid (ECF) volume and is virtually equal to half of total body water. Faced with this medical emergency, we ask the reader: What was responsible for this massive polyuria? What was responsible for this massive polyuria? Physiology principle 1. The urine flow rate is a function of two factors (Eq. 1). Hence polyuria has two causes, a larger than normal solute excretion rate (osmotic diuresis) and/or an inability to raise the concentration of solutes in the urine appropriately (water diuresis). In an osmotic diuresis, each liter of urine contains at least 300 milliosmoles of the causative solute (and other solutes as well) [32]. Urine f low rate liters=day Number of Solutes excreted=Solutesurine 1
Return to the bedside. Using the values from surgery, 3 milliosmoles of extra solutes (10 ml/min a minimum of 300 milliosmoles/l in an osmotic diuresis) would need to be excreted each minute if this was a glucose, urea, or mannitolinduced osmotic diuresis. This would require the presence of very high concentrations of these organic solutes in plasma if one of them caused the polyuria. If the urine composition were not available, the following calculation could be performed to determine whether enough solutes were filtered to cause the osmotic diuresis. With a normal glomerular filtration rate (GFR), the concentration of glucose in the filtrate would have to be 27 mmol/l (486 mg/dl) higher than the renal threshold of 10 mmol/l (180 mg/dl) to filter 3 mmol of glucose per min to permit it to cause this degree of osmotic diuresis (24 mmol/l 0.125 l/min). Hence the blood sugar levels would need to be 666 mg/dl (37 mmol/l) for this to be a glucose-induced osmotic diuresis [14]. If urea were the principal urine osmole, its concentration in plasma would have to be close to 60 mmol/l (BUN 168 mg/dl) because close to half of the filtered urea is normally reabsorbed [9]. Even higher plasma concentrations would be needed if the GFR were lower than 125 ml/min. For mannitol, at least 50 g ( $ 290 mmol) would have to be infused for every liter of urine excreted. Based on this, extra information was sought. Because the blood sugar and BUN were both in the normal range and the quantity of mannitol infused was too small, an osmotic diuresis due to organic solutes was ruled out. The fact that the urine Na+ + potassium (K+ ) concentration was only 50 mmol/l ruled out a salineinduced osmotic diuresis. Therefore the basis for the polyuria was a water diuresis, a diagnosis that was confirmed when his urine osmolality was known (120 mOsm/kg H2O). The next question is, What was the cause of the large water diuresis? It is essential to recall that his PNa was 155 mmol/l during the polyuria.
252
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
What was the cause of the large water diuresis? Physiology principle 2. The control system for water has its sensor (specialized area of the hypothalamus) in a different location from one of its response elements (excretion of water by the kidney). Therefore a messenger (vasopressin) must communicate between these two locations (Fig. 1). The cell volume of the central osmostat shrinks sufficiently when the PNa exceeds 140 mmol/l and this leads to an augmented release of vasopressin. Vasopressin causes the distal segments of the nephron to become permeable to water due to the insertion of water channels [27], causing the urine to become maximally concentrated (the urine osmolality should be 3 4-fold higher than the plasma osmolality) [29]. Return to the bedside. A lesion releasing vasopressinase was unlikely in this patient. There were two factors suggesting that the likely diagnosis was central diabetes insipidus (DI). First, there was the neurosurgery and a disease process (craniopharyngeoma) that could have compromised the ability to release vasopressin from the hypothalamus. Second, there was a large water diuresis (the urine osmolality was 120 mOsm/kg H2O) despite the presence of a stimulus for the release of vasopressin (hypernatremia). To confirm that the DI was central rather than nephrogenic in origin, vasopressin was administered. Bearing in mind that vasopressin acts in a matter of minutes [27], we ask the reader, How low should the urine flow rate be when vasopressin acts? The measured value for this urine flow rate was 6 ml/min.
Fig. 1. Control system for water excretion. The circles represent structures in the hypothalamus. The tonicity stat (osmostat) detects a change in the PNa. Because of hypernatremia (box on the left), this center leads to the release of vasopressin (VP). Vasopressin acts on the distal nephron to cause it to become permeable to water leading to the excretion of concentrated urine. There are also non-osmotic stimuli that influence the release of vasopressin.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
253
How low should the urine flow rate be when vasopressin acts? Application of physiology principle 1. First, the urine flow rate depends on two factors, the number of impermeable solutes (effective or non-urea osmoles) in the lumen of the terminal collecting duct and the effective osmolality (non-urea osmolality) of the papillary medullary interstitium (Eq. 1) [11]. Second, a typical diet leads to the excretion of 800 mosmoles/day, with half being urea and the other half, electrolytes. Third, because the non-urea osmolality can rise to 600 mOsm/kg H2O when vasopressin acts, the expected urine flow rate is close to 0.67 ml/min under these conditions (400 mosmoles of electrolytes excreted at a concentration of 600 mosmoles per liter). Fourth, the maximum total and effective osmolalities in the renal interstitial compartment decline during a prior water diuresis and it takes time to reconstitute this environment after vasopressin acts. Return to the bedside. A urine osmolality of 120 mOsm/kg H2O is not the expected value during a water diuresis when the urine flow rate is 10 ml/min. Rather, the urine osmolality should have been 50 60 mOsm/kg H2O if 800 milliosmoles were excreted in 1440 min (0.5 0.6 milliosmoles/min) [5]. Moreover, in a water diuresis, water is largely impermeable in the distal nephron. Therefore a high rate of excretion of osmoles should not influence the urine flow rate when there is a lack of vasopressin. In contrast, when vasopressin acts, the osmole excretion rate will exert a major effect on the urine flow rate (Eq. 1). A change in urine flow rate is obvious at the bedside whereas a delay is expected before the laboratory reports the urine osmolality. Therefore clinical decision making will be based initially on the decline in urine flow rate. On the one hand, normal subjects have a minimum urine flow rate of close to 0.5 ml/min when vasopressin acts [30]. Accordingly, one might anticipate that the urine volume should fall to 0.5 ml/min after vasopressin was given. A surprise is in store if this were the logic used. The error would be to rely on data obtained from one setting (normal subjects) and apply them to this patient in the ICU. Comment. Had a physiologic analysis been performed at the time when the urine flow rate was 10 ml/min, the observed decrease to 6 ml/min after vasopressin administration could have been anticipated if three facts were taken into account. First, the patient was excreting effective osmoles (urine electrolytes) at a rate that was close to 3-fold that of subjects consuming a typical Western diet (10 ml/min 50 mmol Na+ + K+ /l = 0.5 mmol/min) vs. the expected 225 mmol Na+ + K+ /day or 0.15 mmol/min. Second, the huge water diuresis that occurred prior to the administration of vasopressin should diminish the medullary interstitial osmolality and this would take time to be reconstituted. Thus the maximum urine osmolality would be similarly reduced. Third, the peak natriuresis might not have been reached at the time that the first urine osmolality was measured. Indeed, the rate of osmole (Na+ + K+ ) excretion continued to rise after vasopressin was given. Thus a urine flow rate after vasopressin that was more than 10-fold that of subjects consuming a typical Western diet was a more realistic expectation. Hence, by not applying physiologic principles to the bedside, a series of compounding errors were set into motion that had grave consequences for the patient. One of the errors was to give multiple doses of a long-acting preparation of vasopressin,
254
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
dDAVP. The grave consequences of this error in therapy will be discussed in the response to the question, what was the occult threat to survival? Now we ask the reader to consider, What is the basis of hypernatremia in this patient with central DI? What is the basis of hypernatremia in this patient with central DI? Physiology principle 3. To raise the PNa by 10%, there must either be a gain of Na+ and/or a deficit of water in the ECF compartment (Table 1). In quantitative terms, the gain of Na+ is calculated in total body water terms so a rise in PNa of 15 mmol/l requires a positive balance of approximately 450 mmoles of Na+ (15 mmol/l 30 liters total body water (i.e., 60% of body weight in this patient). On the other hand, because water distributes across all body fluid compartments in proportion to their volumes [33], the deficit of water must be close to 10% of total body water (10% 30 liters, or 3 liters) to cause the observed 10% rise in PNa. Return to the bedside. We begin with an analysis based on electrolyte-free water (water without Na+ + K+ ) to illustrate its limitations (Fig. 2). To think in electrolyte-free water terms [10,23,28], an imaginary calculation is performed where the 4 liters of urine in our patient are divided into 1.3 liters of isotonic saline (use 150 mmol of Na+ + K+ /liter for simplicity) and the remaining 2.7 liters is called electrolyte-free water (Fig. 2). It is important to calculate an electrolytefree water balance rather than focus on either excretion or input to determine why the PNa changed. This can easily be done in our patient because the input contained 0 liters of electrolyte-free water while 2.7 liters of electrolyte-free water were excreted. This negative balance of 2.7 liters of electrolyte-free water should raise the PNa by close to 15 mmol/l (140 mmol/l (30/27.3 liters). If an electrolyte-free water balance were used to design therapy, a positive balance of
Fig. 2. Calculation of electrolyte-free water. The urine volume in Case 1 was 4 liters (large rectangle) and its Na+ + K+ concentration was 50 mmol/l (left of arrow). This solution can be divided into two imaginary components, 1.3 liters of isotonic saline (150 mmol Na+ + K+ /liter) and 2.7 liters of electrolyte-free water (EFW). (From RossMark Medical Publishers, The Acid Truth and Basic Facts, 4th ed, 1997; with permission) [13].
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
255
2.7 liters of electrolyte-free water should be induced to correct the hypernatremia. Notwithstanding, there are many ways to achieve a negative balance of 2.7 liters of electrolyte-free water [3]. For example, if we made a change only to the volume of isotonic saline infused during the period in which hypernatremia developed (now 4 liters instead of 3 liters), there is still no electrolyte-free water administered so the balance for electrolyte-free water is still minus 2.7 liters. Therefore the rise in PNa would be identical, but its basis would be different (Table 2). Obviously, the goals of therapy should also be different in these examples despite the fact that the negative balance of electrolyte-free water and rise in PNa were identical. Therefore one cannot rely on an electrolyte-free water balance to guide therapy (Table 2). [3]. A better way to determine why the PNa changed is to calculate a tonicity balance (Fig. 3) where all inputs and outputs are also divided into two components, total volume of water and Na+ + K+ each of which is analyzed separately [3]. Mass balance for Na+ plus K+ rather than just Na+ must be included because Na+ may enter cells in conjunction with the exit of K+ [8]. Thus the loss of K+ with chloride (Cl ) or bicarbonate can be thought of as a loss of their Na+ salts from the ECF compartment. When considering Na+ + K+ in isolation, for every mmol retained per liter of total body water, the rise in PNa will be 1 mmol/l [33]. Similarly, a gain of 1 liter of water, when considered in isolation should lower the PNa by the formula: PNa (1/total body water). In addition to predicting the rise in PNa [3], the tonicity balance also provides reliable information about its cause (Table 2). In our patient, the volume of water infused was 1 liter less than the urine volume. Recall that 3 liters of net water loss would be required to raise the PNa by 10%. Therefore hypernatremia in our patient was not due solely to a water deficit despite the large electrolyte-free water diuresis. Since the patient was given 450 mmol Na+ and excreted 200 mmol Na+ (+ K+ ) in his urine, there was a net gain of 250 mmol of Na+ + K+ . The
Table 2 Hypernatremia and a negative balance of 2.7 L of electrolyte-free water a Na+ + K+ (mmol) Case 1 Input Output Balance 450 200 + 250 Therapy from balances Water (L) 3 4 1 EFW (L) 0 2.7 2.7 EFW Tonicity
+ 2.7 L H2O
+ 1 L H2O
250 mmol Na+
Change IV to 4L of isotonic saline Input 600 4 Output 200 4 Balance + 400 0
0 2.7 2.7
+ 2.7 L H2O
0 L H2O
400 mmol Na+
a The PNa rose from 140 to 155 mmol/L in each setting. The only difference is the volume of isotonic saline infused over the time period of observation. In both settings, there is a negative balance of 2.7 liters of electrolyte-free water (EFW). The goals of therapy to correct the hypernatremia were clear only after a tonicity balance was calculated.
256
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
Fig. 3. Calculation of a tonicity balance. The rectangle represents the body with its concentration of Na + . The input of Na+ + K+ and of water are shown on the left; the output of Na+ + K+ and of water are shown on the right of this rectangle in Case 1. Balances are shown in dashed boxes inside the rectangle.
combination of a deficit of 1 liter of water and a gain of 250 mmol of Na+ would explain the rise in PNa. In contrast to information provided by an electrolyte-free water balance, the tonicity balance revealed the goals for therapy create a negative balance of 250 mmol of Na+ (+ K+ ) along with a positive balance of 1 liter of water (Table 2). This therapy will correct hypernatremia and return both the ICF and ECF compartment volumes to normal. Moreover, the tonicity balance provides a physiologic basis for the clinical implications of hypernatremia. When a tonicity balance is used in the hypothetical example (i.e., when 4 liters of isotonic saline were administered), it is clear that the goals of therapy are to create a negative balance for Na+ + K+ of 400 mmol and a nil balance of water. Given the short time interval, insensible losses would be relatively small. Therefore, because of the absence of fever, we would not include them in this patient. Clinical course. After administration of vasopressin, the measured concentrations of Na+ + K+ in the urine rose to 175 mmol/l. The intravenous fluid therapy was half-isotonic saline (close to 75 mmol Na+ /liter) at volumes equal to the urine output this caused a deficit of almost 100 mmol of Na+ per liter of throughput. After the excretion of 2.5 liters of urine, the desired negative balance of 250 mmol of Na+ would have occurred. The other goal of therapy was to expand his body water by 1 liter and this was achieved by giving a positive balance of 1 liter of electrolyte-free water (i.e., 1 liter of D5W if hyperglycemia was not present). At this point, both his ICF and ECF volumes and composition would be restored to normal (PNa would be 140 mmol/l). A successful clinical outcome was anticipated. We ask the reader,What is the occult threat to survival? What was the occult threat to survival? Application of physiology principle 3. The PNa is used to reflect the volume of the ICF compartment for three reasons (Fig. 4). First, water crosses cell
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
257
Fig. 4. PNa Concentration reflects the ICF volume in the absence of hyperglycemia and mannitol infusion. The circle represents the ICF compartment that contains macromolecular anions (P ) and its major effective osmole, the cation K+ . Urea, shown on the left, is not an effective osmole because it virtually always has an equal concentration in the ECF and ICF compartments. The osmoles restricted to the ECF compartment are Na+ and its attendant anions. Osmotic equilibrium is achieved because water can cross this cell membrane rapidly.
membranes rapidly to achieve osmotic equilibrium. Second, the number of effective osmoles (osmoles other than urea) in the ICF compartment remains constant in most acute settings. Third, in the absence of hyperglycemia and/or mannitol accumulation in the ECF compartment, the effective ECF osmoles are Na+ and its attendant anions, Cl and bicarbonate. Therefore when hypernatremia develops, the volume of cells will be smaller unless there was a gain in ICF osmoles in muscle for example due to a recent seizure [36] or rhabdomyolysis [15]. The target organ of clinical importance is the brain because it is in a confined rigid space and it cannot gain intracellular particles in an acute setting. The main danger in this setting is an intracerebral hemorrhage. In contrast, hyponatremia usually implies that its ICF volume is expanded and ultimately may lead to cerebral herniation because of the rigidity of the skull and the fact that close to 67% of total brain water is in its ICF compartment. Return to the bedside. Once the PNa has returned to 140 mmol/l, progressive acute hyponatremia from ongoing negative Na+ balance is a real danger unless therapy is modified quickly. One can anticipate that the urine Na+ concentration may be almost as high as the medullary interstitial Na+ + K+ concentration when vasopressin acts because of the low urea concentration in the renal medullary interstitium (the result of the low urine urea concentration). Because a long-acting ( $ 10 h) form of vasopressin (dDAVP) was given and the vast majority of urine osmoles were Na+ + K+ salts, it is not surprising that the urine Na + concentration rose to 300 mmol/l (Fig. 5). Therefore it is easy to anticipate why hyponatremia would develop during therapy to correct hypernatremia because half-isotonic saline (75 mmol Na+ /l) was given at a rate equal to urine
258
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
Fig. 5. Options of therapy to prevent the development of hyponatremia. The actions of vasopressin led to the urinary excretion of 1 liter of hypertonic saline (300 mmol/l) in Case 1. To avoid the development of hyponatremia, the intravenous infusion and urine output must have the same concentrations of Na+ (+ K+ ) and the same volume. Thus either the concentration of saline infused must be 300 mmol/l or the urine must be adjusted so that it becomes close to isotonic saline (give a loop diuretic). (From RossMark Medical Publishers, The Acid Truth and Basic Facts, 4th ed, 1997; with permission.)
output. Because this strategy was not changed when the PNa fell to 140 mmol/l, the patient became progressively hyponatremic and died due to brain swelling that led to herniation. We ask the reader, How could this fatal outcome be avoided? How could this fatal outcome be avoided? Application of physiology principle 3. To prevent a change in the PNa, the input must be identical to the output both in terms of volume and electrolyte content (Fig. 5). Return to the bedside. There are two ways to achieve a tonicity balance (Fig. 5). First, one could infuse saline at the same concentration and flow rate as in the urine; second, one could administer a loop diuretic to lower urine Na + + K+ concentration to approximate that of plasma. With this latter strategy, giving isotonic saline at the same rate as the urine output could have replaced all renal losses other than K+ while preventing a fall in the PNa. At any point before the tragic end, his PNa could have been raised to a non-threatening level easily by the administration of 1 mmol Na+ (without water) per liter of total body water times the desired change in the PNa. Raising his PNa from 125 mmol/l to 130 mmol/l would have required a positive balance of 150 mmol of Na+ (5 mmol/l 30 liters) which could have been accomplished by the rapid infusion of close to 0.3 liters of 3% NaCl. It is important to recognize that a reasonably rapid rate of correction of hyponatremia is not a risk factor for osmotic demyelination in a patient with acute hyponatremia [31]. Concluding remarks for case 1 Using simple whole body physiology (Table 1), deductive reasoning, and a quantitative analysis emphasizing mass balance, the basis of the polyuria was
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
259
clearly a water diuresis due to central DI. By calculating the osmole excretion rate and deducing that there was an excessive excretion of electrolytes, it was important to predict that the urine flow rate might only decline to around 6 ml/min after vasopressin was given. Armed with these insights, the patient would not have been given so large a dose of this hormone. For therapy, the objectives were also clear return the body compartment volumes and composition to normal. Using a tonicity balance, the basis of hypernatremia was a positive balance of 250 mmol of Na+ (and Cl ) and a deficit of 1 liter of water. Accordingly, the design of therapy was to create a negative balance for Na+ (250 mmol) while increasing water balance by 1 liter. Moreover, the dangers in this setting could be anticipated. Once the PNa returned to normal, one must maintain Na+ and water balances. Because the urine Na+ concentration was high and the urine flow rate was also large, intravenous solutions should be given at the same rate as the urine output while ensuring that their overall Na+ concentration was equal to that of the urine (Fig. 5). Perhaps the simple take-home message is that a physiological approach should be the one used at the bedside in the ICU. There are two other points that merit emphasis. First, from a practical and safety perspective, it is critical to monitor the PNa closely during and after therapy to be sure the goals of therapy are indeed being achieved. Second, because hypernatremia developed so acutely, it should not be dangerous to return the PNa to normal over a period of one day. Illustrative case 2 Three problems prompted the transfer of a 70-kg male to the ICU following a recent bone marrow transplant. First, he was heavily immunosuppressed and developed an acute respiratory tract infection for which he was treated with antibiotics including gentamicin. Second, he became hypotensive (blood pressure nadir was 65/40 mm Hg) yet he developed non-oliguric acute renal failure (plasma creatinine rose from 0.9 to 4.6 mg/dl (100 to 412 mmol/l), BUN rose from 14 to 213 mg/dl, urea 5 to 76 mmol/l). Third, his PNa rose from 140 to 157 mmol/l over several days in the ICU. Balance data were available for the day his PNa rose from 147 to 155 mmol/l. They revealed a positive balance of both 1 liter of water and 378 mmol Na+ + K+ (7 liters of hypotonic saline (Na+ + K+ of 90 mmol/l) were infused and he excreted 6 liters of urine (Na+ + K+ concentration of 42 mmol/l) (Fig. 6). His urine osmolality was 524 mOsm/kg H2O. At this point, we ask the reader to consider the following questions. What was the basis of the polyuria and hypernatremia? Why was the urine Na+ + K+ concentration so low? What was the basis of the polyuria? Physiology principle 4. Function of the thick ascending limb of the loop of Henle (TAL) is needed to concentrate the urine and for conservation of Na+ and Cl by the kidney. These cells have a calcium receptor on their basolateral aspect (facing the blood side, Fig. 7). When this receptor is occupied by a
260
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
Fig. 6. Tonicity balance in case 2. For details, see text and the legend to Fig. 3.
cationic ligand such as calcium or gentamicin, the kidney behaves as if it were under the influence of a loop diuretic because of an intracellular signal transduction cascade that leads to inhibition of K+ movement from these cells into the lumen. The net result is a renal concentrating defect and a high rate of excretion of Na+ (and Cl ).
Fig. 7. Physiology of the calcium receptor in the loop of Henle. A cell in the thick ascending limb of the loop of Henle (TAL) is depicted on the right portion of the Figure. When the calcium receptor on its basolateral aspect is occupied, its luminal ROM-K channel is inhibited. When fewer K+ enter the lumen, there is insufficient K+ for the luminal Na+ , K+ , 2 Cl cotransporter and less positive luminal voltage to drive the paracellular reabsorption of Na+ , Ca2+ and Mg2+ .
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
261
Return to the bedside. Using the physiological principles illustrated in Table 1, it is clear that the basis for the polyuria was an osmotic diuresis (very high daily osmole excretion rate, 6 liters 524 mOsm/liter = 3144 mosmoles per day). The bulk of these osmoles were non-electrolytes (2 (Na+ + K+ ) = 84 mOsm/kg H2O). Only one solute (urea) was filtered in sufficient quantity to cause this osmotic diuresis. Hence the presumptive diagnosis was a urea-induced osmotic diuresis (confirmed later by direct analysis of urea). Notwithstanding, two other features contributed to this polyuria. First, there was a high daily rate of excretion of Na+ + K+ (6 liters 42 mmol/l = 252 mmol/day). Second, the furosemide-like effect due to gentamicin (Fig. 7) could have led to a lower renal medullary interstitial tonicity and thereby a lower than expected urine osmolality in the face of a calculated plasma osmolality of 390 mOsm/kg H2O (2 157 mmol Na+/l + 76 mmol urea/l). What was the basis of the hypernatremia? A tonicity balance calculation (Fig. 6) revealed that the basis for the hypernatremia was the positive balance of 378 mmol of Na+ + K+ because there was also a positive balance of 1 liter of water. Thus his ECF volume was expanded (Na+ gain) rather than being contracted (a deficit of water will cause hypernatremia with a contracted ECF volume). Why was the urine Na + + K + concentration so low if vasopressin is acting? When there is a lesion that limits the rise in the urine osmolality (furosemidelike effect attributable to gentamicin, Fig. 7), a higher rate of excretion of organic solutes (urea in this case) obligates a lower concentration of electrolytes in each liter of urine (Fig. 8). At this point, we again ask the reader to pause and consider, What is the next threat to survival in this patient? What is the next threat to survival in this patient? Physiology principle 5. The catabolism of proteins leads to the production of urea, the major nitrogenous waste product [18] (Fig. 9). Because lean body mass has water as its main constituent (80% of weight), these tissues contain 180 g of protein per kg. For every 100 g of protein oxidized, 16 g of nitrogen is converted to urea (572 mmol of urea) [16]. Therefore the appearance in the urine of close to 1100 mmol of urea from endogenous sources represents the net catabolism of 1 kg of lean body mass. Because of its size, muscle catabolism is the major contributor when there is a very high rate of appearance of urea. This can cause a problem because muscle function is needed to clear respiratory secretions. Return to the bedside. On the day the tonicity balance was carried out, the patient excreted 6 liters of urine with a urea concentration of close to 400 mmol/l. Therefore 2400 mmol of urea were excreted, representing the net catabolism of close to 200 g of protein. On that day, he was given 60 g of protein by nasogastric
262
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
Fig. 8. Exacerbation of polyuria by a renal medullary lesion. The rectangle on the left represents 1 liter of urine excreted per day when vasopressin acts, the medullary interstitial osmolality is 900 mOsm/kg H2O, and half of the urine solutes are urea (the other half are electrolytes (lytes)). With a major concentrating defect limiting the maximum urine osmolality to 300 mOsm/kg H2O as the only change, the urine volume will now be 3 liters per day and the urine Na+ + K+ concentration will be hypotonic as shown to the right of the arrow.
tube so he catabolized approximately 140 g of endogenous protein. This was likely derived from almost 0.8 kg of lean body mass (Fig. 9). Should this
Fig. 9. Catabolism of lean body mass to cause a urea-induced osmotic diuresis. With low levels of anabolic hormones and high levels of catabolic factors, there is net breakdown of muscle protein and release of amino acids. Amino acids are delivered to the liver where their nitrogen is converted to urea while carbon/hydrogen is converted to glucose by a common pathway for the most part. The urea soformed becomes the principal urinary nitrogen waste. A quantitative analysis is shown by the numbers in parentheses. Control exerted at site 1.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
263
continue, he would ultimately undergo marked muscle wasting (and he did). Protein wasting could make his lung infection worse by compromising efforts to clear secretions from his respiratory tract as well as diminishing his immunological responses to infection [20]. Summary. Had the true basis for polyuria and hypernatremia been recognized, efforts would have been more vigorous at the nutritional level in this patient. On the one hand, more exogenous calories including protein could have been given. On the other hand, anabolic hormones such as high dose insulin with glucose to avoid hypoglycemia and/or provision of nutritional supplements such as glutamine [20] might have been tried to minimize protein catabolism. One might also have questioned the use of high doses of catabolic hormones such as glucocorticoids at this point because of his extreme degree of catabolism. Concluding remarks for case 2 Perhaps the simple message in Case 2 is to perform a balance of all major constituents of the urine. From the Na+ and water perspective, a ureainduced osmotic diuresis caused polyuria. Hypernatremia developed because isotonic saline was infused whereas the urine had a much lower concentration of Na+ + K+. More importantly, from an integrative physiology point of view, these salt and water issues were the clues to reveal the very large endogenous protein catabolism with its potential threats for survival.
Hyponatremia The first decision one must make when dealing with a patient with hyponatremia (PNa less than 136 mmol/l) is to determine whether it represents an acute condition (documented course is less than 48 hours). The reason for this emphasis is that the main danger in acute hyponatremia results from brain cell swelling whereas the main danger with chronic hyponatremia is the osmotic demyelination syndrome (ODS) that occurs secondary to its treatment [35]. In fact, one usually begins with therapeutic considerations in acute hyponatremia and with diagnostic considerations in chronic hyponatremia. If even mild symptoms begin in a patient with acute hyponatremia, clinical deterioration may be very rapid so treatment must be prompt and vigorous.
Acute hyponatremia Illustrative case 3 A 17-month-old infant weighing 10 kg had a 2-day history of gastroenteritis. Physical examination revealed a normal ECF volume, but one observer said that he was somewhat dry. There was a mild degree of hyponatremia (PNa 134 mmol/l)
264
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
and a urine osmolality of 320 mOsm/kg H2O; the urine volume was not recorded throughout his hospital course. Despite these minor abnormalities, he was given a bolus of isotonic saline (200 ml, 30 mmol Na+ ) and a maintenance infusion of 2/3 D5W and 1/3 isotonic saline at 40 ml/h for the next 20 hours (total volume, 750 ml, 37.5 mmol Na+ ). He received an estimated 200 ml of water as ice chips because of a dry mouth. He improved initially, but 20 hours after the start of therapy, a seizure occurred. His PNa at this time was 121 mmol/l. We ask the reader to consider: Why did acute hyponatremia develop? What would your therapy be bearing in mind that he has had a seizure? To prevent the development of hyponatremia, what should the initial therapy be? Are there specific risk factors for hyponatremia in certain patients who receive electrolyte-free water? Why did acute hyponatremia develop? Physiology principle 6. To develop hyponatremia, there must be both a source of electrolyte-free water and a means to decrease its rate of excretion (Table 1); the latter is due to renal actions of vasopressin [27]. The quantity of Na+ in the ECF compartment is close to 30 mmol/kg body weight (Table 1); a 10-kg normal infant has 2 liters of ECF and 280 mmol of Na+. Return to the bedside. Vasopressin could have been released in response to a number of non-osmotic stimuli including the underlying GI disturbance (Table 3). He had three source of electrolyte-free water. First, hypotonic solutions were infused. Second, electrolyte-free water was given orally in the form of ice chips. Third, electrolyte-free water was generated by the kidney by a process that we call desalination of infused isotonic saline (Fig. 10); this process requires a large natriuresis [34]. Because he was given close to 7 mmol of Na+ per kg, his ECF volume would be expanded by 20% providing a stimulus for Na+ excretion.
Table 3 High vasopressin levels in patients with hyponatremia Readily reversible causes Low effective circulating volume Anxiety, stress pain, nausea Drugs causing nausea (e.g., chemotherapeutic agents), the central release of vasopressin (e.g., morphine) or enhancement of the renal effects of vasopressin (e.g., certain oral hypoglycemics, nonsteroidal anti-inflammatory drugs) Endocrine causes (e.g., hypothyroidism, adrenal insufficiency) Exogenous DDAVP, oxytocin Not easily reversible causes Vasopressin-producing tumors Central nervous system or lung lesions (may cause reset osmostat) Granulomas Certain metabolic lesions (e.g., porphyria)
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
265
Fig. 10. Generation of electrolyte-free water by the kidney. The larger rectangle to the left of the arrows represents the infusion of 2 liters of isotonic saline; the content of Na + (300 mmol) is shown in the oval inside that rectangle. A similar depiction is used for the excretion of Na + and water and they are shown to the right of the arrows. To have a concentration of Na + in the urine that is 300 mmol/l, vasopressin (VP) must act and there must be a reason to excrete NaCl. The remaining 1 liter of electrolyte-free water is retained in the body.
What should your therapy be bearing in mind that he has had a seizure? Application of physiology principle 3. The ICF volume is inversely proportional to the PNa (Fig. 4). To lower the ICF volume, one must give solutes such as Na+ (and Cl ) or mannitol that are restricted to the ECF compartment. To draw water out of the skull by osmosis to reduce intracranial pressure, the solute given must not readily cross cerebral capillaries. Hypertonic Na+ and mannitol cause osmotic shrinking of the brain because they do not readily cross the blood-brain barrier [26]. Return to the bedside. Treatment must be aggressive even if only mild symptoms were present. Hypertonic saline (3%) should be given intravenously to raise the PNa by 5 mmol/l in 1 2 hours; this should alleviate significant cerebral swelling and hopefully prevent irreversible damage. The calculated dose of NaCl depends upon body weight (10 kg) and in infants, water is 70% of body weight. Because total body water is approximately 7 liters, he would need 35 mmol (5 mmol/l 7 liters) to raise his PNa by 5 mmol/l. This is equivalent to close to 80 ml of 3% saline ($ 500 mmol/l). A potential danger of this infusion is over-expansion of his ECF volume, but this risk is minor. Longer-term treatment would depend on the volume and tonicity of the urine. Having said all this, the emphasis should have been on correct therapy when the child was admitted.
266
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
To prevent the development of hyponatremia, what should the initial therapy be? Application of physiology principles 1 and 3. The excretion of Na+ is increased when the ECF volume is expanded. If vasopressin is present, the concentration of Na+ + K+ in the urine can be very high, generating electrolyte-free water that will be retained in the body (Fig. 10). Return to the bedside. Acute hyponatremia in hospitalized patients should be a problem of the past. Prevention depends upon limiting the access to electrolytefree water in a patient likely to have vasopressin acting. The administration of hypotonic infusions is contraindicated in our patient because his PNa is less than 138 mmol/l. Since electrolyte-free water can be generated by the kidney as a result of a large natriuresis when vasopressin acts (Fig. 10), one should give only as much isotonic saline as needed for hemodynamic purposes. It is not advisable to administer a large volume of isotonic saline to achieve a good urine output because the good urine output may really be a danger sign if the urine tonicity is high. If the urine were hypertonic, it should be replaced with the same volume and tonicity as was excreted or, alternatively, the composition of this urine could be changed to near-isotonic saline with a loop or osmotic diuretic and again its total volume replaced with isotonic saline (Fig. 5). Are there specific risk factors for the development of acute hyponatremia in certain patients who receive electrolyte-free water? Application of physiology principle 3. Close to 50% of body water is in skeletal muscles. The major constituent (80%) of the brain is water. Approximately 2/3 of this water is in cells and this volume increases with hyponatremia. Therefore for a given % swelling, the larger the brain cell/total volume in the skull, the greater the rise in intracranial pressure. On the other hand, hyponatremia that is due to the addition of an iso-osmotic mannitol solution will expand the ECF volume but it will not cause brain cell swelling (the plasma osmolality is not appropriately low, Table 4). Return to the bedside. The following major risk factors can be anticipated for developing brain swelling with acute hyponatremia. First, even less electrolytefree water is needed to cause a lower PNa in patients with a small muscle mass. Second, patients who have a larger brain cell mass (younger age) are at greater risk from a given volume of water retained in the body. Third, patients given an acute bolus of saline intravenously will have an expanded blood volume (higher hydrostatic pressure) and a lower colloid osmotic pressure. Hence they might have a higher intracerebral ECF volume and develop symptoms from increased intracranial pressure with a smaller reduction in their PNa. Fourth, patients with an underlying brain lesion (seizure disorder) may be more prone to develop seizures with a smaller degree of hyponatremia.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272 Table 4 Acute hyponatremia due to lavage solutions EFW Unit Before the excretion of the organic solute ICF volume L ECF volume L PNa mmol/L Plasma osmolality mOsm/L Original 20 10 140 290 Final 22 11 127 264 Lavage solution Original 20 10 140 290
267
Final 20 13 108 290
After the excretion of the organic solute (as 3 L of isotonic urine) ICF volume L 22 ECF volume L 11 PNa mmol/L 127 Plasma osmolality mOsm/L 264
20 10 140 290
Each subject with 30L of total body water has a 3L positive water balance. The patient who received the isosmotic lavage solution also has a positive balance of 900 mOsm of a solute with a distribution restricted to the ECF compartment. The plasma osmolality is not depressed in the patient who retained the isotonic lavage solution, and the ICF volume is normal, despite a PNa of 108 mmol/L. When the lavage solution is excreted as an isotonic solution, there is a large increase in the PNa and no change in the ICF volume.
It is said that young women are less able to regulate brain cell volume in response to acute hyponatremia [1]. This ides has arisen because of poor outcomes in young women compared with men who develop postoperative hyponatremia. Nevertheless, this is not a closed issue for two reasons. First, postoperative hyponatremia in males most frequently occurs during transuretheral resection of the prostate (TURP). Males undergoing TURP are typically older and could have a smaller brain cell/total intracranial volume. Second, the composition of the fluid retained with the commonest surgery in females and males is different electrolyte-free intravenous water after gynecological surgery and lavage solutions during a TURP (Table 4). During a TURP, acute hyponatremia may be due to the absorption of isotonic or half-iso-osmotic lavage solutions containing glycine, sorbitol, and/or mannitol [12]. Neurological manifestations in this setting might be due to toxic metabolic products such as ammonium (NH4+) produced during the metabolism of glycine rather than to brain cell swelling. It follows that one should not use aggressive therapy for this type of acute hyponatremia if the measured plasma osmolality is reduced by less than 10%. On the other hand, if the plasma osmolality is less than 260 mOsm/kg H2O, therapy reverts to that described above for a gain of electrolyte-free water.
Chronic hyponatremia (time course >48 hours) Illustrative case 4 The usual diet of a 78-year-old, 60 kg, cheerful lady was tea (a large cup), toast, and jam. A thiazide diuretic was prescribed because of the recent discovery
268
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
of high blood pressure (160/90 mm Hg). She became lethargic and slower in mentation over several weeks, but there were no focal neurologic signs. Blood pressure fell to 140/90 mm Hg suggesting that her ECF volume was contracted. Laboratory investigations are shown in Table 5. We ask the reader the following questions: If an emergency is present, what is it? What dangers to you anticipate with therapy? On a quantitative analysis, what changes occurred in the volumes and electrolyte composition in her ICF and ECF compartments? What is the chronic therapy for hyponatremia due to SIADH? If an emergency is present, what is it? Other physiology principles. Cardiac arrhythmias are more common if hypokalemia is severe in degree and if there is underlying heart disease. If KCl is given to treat hypokalemia, think of it as a form of NaCl for the ECF compartment because when K+ enters cells, Na+ (and H + ) will exit cells for the most part. Return to the bedside. The major emergency to anticipate is hypokalemia if it is accompanied by prolonged QT interval in the EKG recording. The absolute value for her PNa, while alarming, should not be considered an emergency. Because of absence of an ominous EKG, KCl was given slowly to raise her PK to the low 3 mmol/l range over 24 hours. The oral route was used because bowel sounds were present. One cannot accurately predict how much of K+ will be needed over the next 24 hours, but we anticipated that at least 100 mmol of KCl would be required changes in her PK dictate the actual dose given. Glucose and bicarbonate containing infusions should not be given for fear of an unwanted acute shift of K+ into cells. Notwithstanding, there is a danger with KCl therapy too rapid correction of her hyponatremia. This can occur for two reasons. First, giving hypertonic KCl will raise her PNa and thereby could lead to too rapid a rise in PNa. Second, because K+ will enter the ICF compartment and Na+ will move in the opposite direction, the ECF volume will expand. This in turn could suppress the release of vasopressin and lead to the excretion of a large volume of dilute urine.
Table 5 Laboratory values in case 4 Parameter Na K+ Cl Glucose Urea Osmolality
a +
Unit mmol/L mmol/L mmol/L mg/dL (mmol/L) mg/dL (mmol/L) mOsm/kg H2O
Plasma 107 2.2 67 90(5) 11(4) 220
Urinea 10 25 10 0 320 402
Random sample.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
269
What dangers do you anticipate with therapy? Application of physiology principle 3. The physical examination to detect a mild degree of ECF volume contraction is not reliable [4,24]. Return to the bedside. As discussed above, in the short-term, there is a danger that hyponatremia may be corrected too rapidly because of suppression of the release of vasopressin. As a result, a large water diuresis could lead to a rapid increase in PNa and cause the ODS. Clues suggesting that her ECF volume was low are found in the history (low-salt diet and the thiazide diuretic). The laboratory data are often difficult to interpret with respect to the ECF volume status. For example, some laboratory data did suggest that her ECF volume was contracted (urine Na+ and Cl concentrations were both < 15 mmol/l), but these data are not entirely convincing in someone on a low-salt diet who should have a low electrolyte excretion rate. Other laboratory values that may be of help in this regard are a frankly high plasma urea (may not be high because of her low-protein diet), high level of creatinine (not present because of low muscle mass), metabolic alkalosis with hypokalemia (present in this case), and/or a plasma anion gap that is higher than expected even when corrected for albumin level [19]. There was a danger sign with therapy in this patient her urine output rose dramatically with an infusion of saline. Because this was a water diuresis, vasopressin was given to reduce the urine output temporarily so that the desired slow rate of rise in the PNa could be achieved (4 mmol/l/24 hour because of her K+ deficit) [2,22]. The main threat is brain cell volume shrinkage and the development of an ODS following therapy that resulted in too rapid a rise in the PNa [21,35]. The danger of ODS is greater in patients with a deficit of K+ and those whose nutritional state is poor [2,22] probably because they are unable to regenerate brain ICF particles quickly enough to prevent their cell volume from shrinking. In attempts to correct PNa of patients in this high-risk group, the correction rate should be much less than our usual recommendation of 8 mmol/l per 24 hours [25]. The PNa should rise at a rate that is slow enough to avoid the ODS in every patient. The emphasis should be on magnitude of correction of hyponatremia, remaining within our 4 mmol/liter/24 hours [25]. Raising the PNa above 125 mmol/l is rarely necessary in the first few days. What changes occurred in her ICF and ECF compartment volumes and composition? With a body weight of 60 kg, her normal total body water (TBW) is close to 30 liters (50% of body weight distributed as 20 liters ICF and 10 liters ECF). If there was no change in the number of osmoles in her ICF compartment, the calculated ICF volume with a PNa of 107 mmol/l is 26 liters ((140 mmol/l/ 107 mmol/l) 20 liters). If her ECF volume was close to 10 liters on admission, there was a negative balance of 330 mmoles of Na+ in her ECF compartment
270
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
(fall in PNa of 33 mmol/l 10 liters). Because her plasma K + concentration was so low (2.2 mmol/l), her ICF compartment probably gained a cation (Na + or H + ). It is not possible at present to assign quantitative values to these changes in ICF ion composition. What is the chronic therapy with hyponatremia due to SIADH? If the patient has an on-going defect in the excretion of electrolyte-free water, there are two options for therapy to prevent a further decline in PNa. Either less water must be consumed (water restriction) or the urine must be large in volume and isotonic to the intake. To lower the urine Na+ + K+ concentration, one can ingest urea [6]; a typical dose for urea is 10 30 g per day. If the urine Na+ + K+ concentration is very high, administration of a loop diuretic can reduce these concentrations an isotonic level [7,17]. We do not recommend the use of drugs such as vasopressin antagonists because of the possibility of causing a large water diuresis and an excessively rapid rise in PNa.
Summary Our purpose was to illustrate the utility of an approach that begins with simple principles of physiology to patients who have a disturbance in salt and water balance (Table 1). At times, the physiology is restricted to the kidney and body fluid compartments. In these settings, the goals of therapy are defined by calculating a tonicity balance electrolyte-free water balances simply do not provide the needed information [3]. At other times, performing balances of other solutes such as urea reveal that another critically important problem is present (tissue catabolism). Thus the physiologic analysis becomes more integrative, extending beyond renal issues. Goals for therapy become clearer once the integrative physiology is known. More modern contributions from molecular studies permit a revised interpretation of the physiology. An example presented was the possible role of gentamicin-like drugs as a cause of high output renal failure that is basically a persistent loop diuretic-like effect. In the patient presenting with hyponatremia, the first step is to determine if the time course is less than 48-hours because emergency therapy is different in this setting. With acute hyponatremia, the objective is to diminish brain cell swelling especially if even mild symptoms are present. In contrast, the objective in the patient with chronic hyponatremia is to prevent ODS. An even slower rate of rise of the PNa is required in patients who are malnourished and/or K+ depleted.
References
[1] Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med 1986;314:1529 35.
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
271
[2] Bahr M, Sommer N, Peterson D, Wietholter H, Dichgans J. Central pontine myelinolysis associated with low potassium levels in alcoholism. J Neurol 1990;237:275 6. [3] Carlotti APCP, Bohn D, Mallie J-P, et al. Tonicity balance and not electrolyte-free water calculations more accurately guides therapy for acute changes in natremia. Intensive Care Med 2001;27:921 4. [4] Chung HM, Kluge R, Schrier RW. Clinical assessment of extracellular fluid volume in hyponatremia. Am J Med 1987;83:905 8. [5] Davids MR, Edoute Y, Halperin ML. Approach to a patient with acute polyuria and hypernatremia: A need for the physiologic approach of McCance at the bedside. Netherlands J Med 2001;58:103 10. [6] Decaux G, Brimioulle S, Genette F, et al. Treatment of the syndrome of inappropriate secretion of antidiuretic hormone by urea. Am J Med 1980;69:99 106. [7] Decaux G, Waterlot Y, Genette F, et al. Treatment of the syndrome of inappropriate secretion of antidiuretic hormone with furosemide. N Engl J Med 1981;304:329 30. [8] Edelman IS, Leibman J, OMeara MP, et al. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest 1958;37:1236 56. [9] Gamble JL, McKhann CF, Butler AM, et al. An economy of water in renal function referable to urea. Am J Physiol 1934;109:139 54. [10] Goldberg M. Hyponatremia. Med Clin North Am 1981;65:251 69. [11] Gowrishankar M, Lenga I, Cheung RY, et al. Minimum urine flow rate during water deprivation: importance of the permeability of urea in the inner medulla. Kidney Int 1998;53:159 66. [12] Hahn RG. The transurethral resection syndrome. Acta Anaesthesiol Scand 1991;35:557 67. [13] Halperin ML. The ACID truth and BASIC facts with a Sweet Touch, an enLYTEnment. In: Stirling, ON, Canada: RossMark Medical Publishers; 1997. [14] Halperin ML, Goguen JM, Scheich AM, et al. Clinical consequences of hyperglycemia and its correction. In: Seldin DW, Giebisch G, editors. Clinical disturbances of water metabolism. New York: Raven Press; 1993. p. 249 72. [15] Halperin M.L, Goldstein MB. Fluid, electrolyte and acid-base physiology; a problem-based approach. Philadelphia: W.B. Saunders; 1998. [16] Halperin M.L, Rolleston FS. Clinical detective stories: a problem-based approach to clinical cases in energy and acid-base metabolism. In: London, England: Portland Press; 1993. p. 273 4. [17] Hantman D, Rossier B, Zohlman R, et al. Rapid correction of hyponatremia in the syndrome of inappropriate secretion of antidiuretic hormone. Ann Int Med 1973;78:870 5. [18] Jungas RL, Halperin ML, Brosnan JT. Lessons learnt from a quantitative analysis of amino acid oxidation and related gluconeogenesis in man. Physiol Rev 1992;72:419 48. [19] Kamel KS, Cheema-Dhadli S, Halperin FA, et al. Anion gap: do the anions restricted to the intravascular space have modifications in their valence? Nephron 1996;73:382 9. [20] Labow BI, Souba WW. Glutamine. World J Surg 2000;24:1503 13. [21] Laureno R, Karp BI. Myelinolysis after correction of hyponatremia. Ann Int Med 1997;126:57 62. [22] Lohr JW. Osmotic demyelination syndrome following correction of hyponatremia: association with hypokalemia. Am J Med 1994;96:408 13. [23] Mallie J-P., Bichet DG, Halperin ML. Effective water clearance and tonicity balance: the excretion of water revisited. Clin Invest Med 1997;20:16 24. [24] McCance RA. Medical problems in mineral metabolism. III. Experimental human salt deficiency. Lancet 1936;230:823 30. [25] Oh MS, Kim HJ, Carroll HJ. Recommendations for treatment of symptomatic hyponatremia. Nephron 1995;70:143 50. [26] Porzio P, Halberthal M, Bohn D, et al. Design of a treatment for acute symptomatic hyponatremia: ensuring the excretion of a predictable amount of electrolyte-free water. Crit Care Med 2000;28:1905 10. [27] Robertson GL. Vasopressin. In: Seldin DW, Giebisch G, editors. The kidney: physiology & pathophysiology. Philadelphia PA: Lippincott Williams & Wilkins; 2000. p. 1133 52.
272
M.L. Halperin, D. Bohn / Crit Care Clin 18 (2002) 249272
[28] Rose BD. New approach to disturbances in the plasma sodium concentration. Am J Med 1986; 81:1033 40. [29] Sands JM, Layton HE. Urine concentrating mechanism and its regulation. In: Seldin DW, Giebisch G, editors. The kidney: physiology & pathophysiology. Philadelphia PA: Lippincott Williams & Wilkins; 2000. p. 1175 216. [30] Soroka SD, Chayaraks S, Cheema-Dhadli S, et al. Minimum urine flow rate during water deprivation: importance of the urea and non-urea osmole concentration and excretion rate. J Am Soc Nephrol 1997;8:880 6. [31] Soupart A, Decaux G. Therapeutic recommendations for management of severe hyponatremia: current concepts on pathogenesis and prevention of neurologic complications. Clin Nephrol 1996;46:149 69. [32] Spira A, Gowrishankar M, Halperin ML. Factors contributing to the degree of polyuria in a patient with diabetes mellitus in poor control. Am J Kidney Dis 1997;30:829 35. [33] Spital A, Sterns RD. The paradox of sodiums volume of distribution: Why an extracellular solute appears to distribute over total body water. Arch Intern Med 1989;149:1255 7. [34] Steele A, Gowrishankar M, Abrahmson S, et al. Postoperative hyponatremia despite isotonic saline infusion: A phenomenon of desalination. Ann Int Med 1997;126:20 5. [35] Sterns RH, Silver SM, Spital A. Hyponatremia. In: Seldin DW, Giebisch G, editors. The kidney: physiology & pathophysiology. Philadelphia PA: Lippincott Williams & Wilkins; 2000. p. 1217 38. [36] Welt LG, Seldin DW, Nelson WP, et al. Role of the central nervous system in metabolism of electrolytes and water. Arch Int Med 1952;90:355 78.
Вам также может понравиться
- Fluid and Electrolytes for Nursing StudentsОт EverandFluid and Electrolytes for Nursing StudentsРейтинг: 5 из 5 звезд5/5 (12)
- Electrolyte DisordersДокумент10 страницElectrolyte DisordersSlavicaОценок пока нет
- Apollo TyresДокумент78 страницApollo TyresADITYA33% (3)
- Aircraft Design Project 2Документ80 страницAircraft Design Project 2Technology Informer90% (21)
- Hyperbaric WeldingДокумент17 страницHyperbaric WeldingRam KasturiОценок пока нет
- Demystifying HyponatremiaДокумент10 страницDemystifying HyponatremiaJavier Vivanco100% (1)
- Fluid and Electrolyte Imbalance in EvacueesДокумент15 страницFluid and Electrolyte Imbalance in EvacueesDyanne Bautista100% (1)
- Fluid and Electrolyte Nursing Care Management 112Документ7 страницFluid and Electrolyte Nursing Care Management 112anne marieОценок пока нет
- Fluids and Electrolytes-2Документ82 страницыFluids and Electrolytes-2Jem Loterte100% (1)
- Elevator Traction Machine CatalogДокумент24 страницыElevator Traction Machine CatalogRafif100% (1)
- Canon imageFORMULA DR-X10CДокумент208 страницCanon imageFORMULA DR-X10CYury KobzarОценок пока нет
- Lec. 3 - Fluid and ElectrolyteДокумент16 страницLec. 3 - Fluid and Electrolyteمجيب سلطانОценок пока нет
- CP 343-1Документ23 страницыCP 343-1Yahya AdamОценок пока нет
- Lyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticДокумент13 страницLyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticJayr Mercado0% (1)
- Medical Surgical Fluid and Electrolytes FVD FVEДокумент7 страницMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadОценок пока нет
- Medical-Surgical: Fluids & ElectrolytesДокумент65 страницMedical-Surgical: Fluids & Electrolytesɹǝʍdןnos100% (32)
- Fluid Therapy FinalДокумент3 страницыFluid Therapy Finallaureeate100% (1)
- Medical Surgical Nursing: Fluids and ElectrolytesДокумент28 страницMedical Surgical Nursing: Fluids and ElectrolytesDhen MarcОценок пока нет
- Fluid, Electrolyte, and Acid-Base BalanceДокумент41 страницаFluid, Electrolyte, and Acid-Base BalanceRn nadeenОценок пока нет
- Under The Guidance Of: Dr. B.Shashidharan. Professor and Chief Unit-III By, Dr. Henley Punnen AndrewsДокумент63 страницыUnder The Guidance Of: Dr. B.Shashidharan. Professor and Chief Unit-III By, Dr. Henley Punnen AndrewsHenley AndrewsОценок пока нет
- Fluids Electrolytes NotesДокумент23 страницыFluids Electrolytes NotesHamza AdriОценок пока нет
- Fluid Balance in Clinical PracticeДокумент8 страницFluid Balance in Clinical Practicefernando_vaz2010100% (1)
- Urine Serum Ratio To Predict Response To Fluid RestrictionДокумент8 страницUrine Serum Ratio To Predict Response To Fluid Restrictionkromatin9462Оценок пока нет
- Liquidos y Electrolitos 2Документ4 страницыLiquidos y Electrolitos 2Jorge MBОценок пока нет
- Fispatologjia e CreegullimeveДокумент16 страницFispatologjia e CreegullimeveArmar MendoОценок пока нет
- Fluid Electrolytes and Nutrition Physiological and Clinical AspectsДокумент14 страницFluid Electrolytes and Nutrition Physiological and Clinical AspectsPaulynhiita FashyOnОценок пока нет
- Emergency Fluid TherapyДокумент7 страницEmergency Fluid TherapyAnaОценок пока нет
- Intravenous Fluid TherapyДокумент10 страницIntravenous Fluid TherapyAnonymous ysrxggk21cОценок пока нет
- VET343 Urinary Lecture Notes 2014Документ35 страницVET343 Urinary Lecture Notes 2014walczakcОценок пока нет
- What Is Plasma Osmolality?:, 23 Mei 2007 Fluid and Electrolyte TherapyДокумент17 страницWhat Is Plasma Osmolality?:, 23 Mei 2007 Fluid and Electrolyte TherapyRani ChesarОценок пока нет
- Fluid and Electrolyte DisordersДокумент9 страницFluid and Electrolyte DisordersRehab weridaОценок пока нет
- PN Composition CompilationДокумент15 страницPN Composition CompilationAnonymous rDD9I2Оценок пока нет
- 3 Fluid and ElectrolyteДокумент7 страниц3 Fluid and ElectrolyteStephen HDОценок пока нет
- AssignmentДокумент6 страницAssignmentleone shikukuОценок пока нет
- Guidelines For Management Of: HypernatremiaДокумент7 страницGuidelines For Management Of: HypernatremiaSarly Puspita AriesaОценок пока нет
- Fluid and Electrolyte Balance: Presenter: Dr. Siyum Mathewos (Omfs-Ri) Modulator: Dr. Dereje (Omfs, Consultant)Документ87 страницFluid and Electrolyte Balance: Presenter: Dr. Siyum Mathewos (Omfs-Ri) Modulator: Dr. Dereje (Omfs, Consultant)Siyum MathewosОценок пока нет
- Fluid and Electrolyte Disorders: Dr. Chandra Kant Pandey Dr. R. B. SinghДокумент8 страницFluid and Electrolyte Disorders: Dr. Chandra Kant Pandey Dr. R. B. SinghMok Chu ZhenОценок пока нет
- Fluid and Electrolyte ImbalanceДокумент85 страницFluid and Electrolyte ImbalanceAdarshBijapurОценок пока нет
- Australian Naturopathic Network: Departments Medical Sciences A&P FluidДокумент4 страницыAustralian Naturopathic Network: Departments Medical Sciences A&P FluidFathur Rahman Mutiara HikmahОценок пока нет
- Lect 02Документ5 страницLect 02Iptysam Al-AlawiОценок пока нет
- METABOLISME AIR DAN MINERALДокумент15 страницMETABOLISME AIR DAN MINERALKlara SintaОценок пока нет
- Water Metabolism (Welch)Документ10 страницWater Metabolism (Welch)Prisky ChriselawatiОценок пока нет
- A Review of PH and OsmolarityДокумент5 страницA Review of PH and OsmolarityMuhammad Rizki SaidОценок пока нет
- Diagnosis and Management of Hyponatremia in Acute Illness PDFДокумент13 страницDiagnosis and Management of Hyponatremia in Acute Illness PDFMihaela MocanОценок пока нет
- METABOLISME AIRДокумент15 страницMETABOLISME AIRAyu FadhilahОценок пока нет
- Module 2 Fluid Electrolyte Disorders Acid Base Notes 9th EdДокумент15 страницModule 2 Fluid Electrolyte Disorders Acid Base Notes 9th EdSara FОценок пока нет
- Principles of Dialysis: Diffusion, Convection, and Dialysis MachinesДокумент6 страницPrinciples of Dialysis: Diffusion, Convection, and Dialysis MachinesD'phiLea EyFfaОценок пока нет
- Body Fluid DistributionДокумент56 страницBody Fluid DistributionZoya Morani100% (1)
- Hipo e HipernatremiaДокумент23 страницыHipo e HipernatremiaMary DiazОценок пока нет
- Hemorrhagic ShockДокумент2 страницыHemorrhagic ShockPharhana PuterieОценок пока нет
- Perioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediДокумент8 страницPerioperative Intravenous Fluid Therapy For Adults: Rob Mac Sweeney, Rachel Alexandra Mckendry, Amit BediAnnisa Chaerani BurhanuddinОценок пока нет
- Basic of Fluid Therapy ImaДокумент69 страницBasic of Fluid Therapy Imal Made ArtawanОценок пока нет
- 7 FullДокумент9 страниц7 FullNoniqTobingОценок пока нет
- Fluids and Electrolyte Balance: Understanding Intracellular and Extracellular Fluid CompartmentsДокумент17 страницFluids and Electrolyte Balance: Understanding Intracellular and Extracellular Fluid CompartmentsSydney DeringОценок пока нет
- Lect15&16 Fluids&ElectrolytesДокумент77 страницLect15&16 Fluids&Electrolyteskhurram na100% (1)
- Fluids and Electrolytes - PaediatricsДокумент52 страницыFluids and Electrolytes - PaediatricsZweОценок пока нет
- Chapter 25 Fluid, Electrolyte, and Acid-Base BalanceДокумент5 страницChapter 25 Fluid, Electrolyte, and Acid-Base BalanceDawlat SalamaОценок пока нет
- Fluid Electrolyte BalanceДокумент19 страницFluid Electrolyte BalanceRatna VimalОценок пока нет
- Fluid Therapy for Dehydrated HorseДокумент5 страницFluid Therapy for Dehydrated HorsePrabina SahuОценок пока нет
- Intravenous Fluid ManagementДокумент14 страницIntravenous Fluid ManagementSALSABILA RAHMA REFFANANAОценок пока нет
- The Hyponatremic Patient: A Systematic Approach To Laboratory DiagnosisДокумент7 страницThe Hyponatremic Patient: A Systematic Approach To Laboratory DiagnosisJuen LohОценок пока нет
- Dry Weight in HemodialysisДокумент12 страницDry Weight in HemodialysisAnik PriyaniОценок пока нет
- 5 Volume and Electrolyte Management: Concezione TommasinoДокумент20 страниц5 Volume and Electrolyte Management: Concezione TommasinoTayyab SiddiquiОценок пока нет
- Metabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentОт EverandMetabolic Disorders and Critically Ill Patients: From Pathophysiology to TreatmentCarole IchaiОценок пока нет
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?От EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?Оценок пока нет
- 2014 AHA CX No CardioДокумент107 страниц2014 AHA CX No Cardiodiomer123Оценок пока нет
- Anestesia para UrologiaДокумент7 страницAnestesia para Urologiadiomer123Оценок пока нет
- 9 Anaesthetic Considerations For Laparoscopic Surgery in Neonates and Infants: A Practical ReviewДокумент13 страниц9 Anaesthetic Considerations For Laparoscopic Surgery in Neonates and Infants: A Practical Reviewdiomer123Оценок пока нет
- Coronary-Artery Bypass Surgery in Patients WithДокумент2 страницыCoronary-Artery Bypass Surgery in Patients Withdiomer123Оценок пока нет
- Acute Decompensated Heart FailureДокумент22 страницыAcute Decompensated Heart Failurediomer123Оценок пока нет
- Evaluation Pre Opera TiДокумент8 страницEvaluation Pre Opera Tidiomer123Оценок пока нет
- AI Model Sentiment AnalysisДокумент6 страницAI Model Sentiment AnalysisNeeraja RanjithОценок пока нет
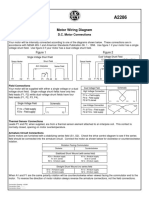
- Motor Wiring Diagram: D.C. Motor ConnectionsДокумент1 страницаMotor Wiring Diagram: D.C. Motor Connectionsczds6594Оценок пока нет
- F-16c.1 Ginkgo Ginkgolic AcidДокумент2 страницыF-16c.1 Ginkgo Ginkgolic AcidNarongchai PongpanОценок пока нет
- STS Chapter 1 ReviewerДокумент4 страницыSTS Chapter 1 ReviewerEunice AdagioОценок пока нет
- CG Module 1 NotesДокумент64 страницыCG Module 1 Notesmanjot singhОценок пока нет
- Monodisperse Droplet Generators As Potential Atomizers For Spray Drying Technology PDFДокумент11 страницMonodisperse Droplet Generators As Potential Atomizers For Spray Drying Technology PDFfishvalОценок пока нет
- Idioms & Phrases Till CGL T1 2016Документ25 страницIdioms & Phrases Till CGL T1 2016mannar.mani.2000100% (1)
- Metal Framing SystemДокумент56 страницMetal Framing SystemNal MénОценок пока нет
- ML AiДокумент2 страницыML AiSUYASH SHARTHIОценок пока нет
- PDFViewer - JSP 3Документ46 страницPDFViewer - JSP 3Kartik ChaudharyОценок пока нет
- HVCCI UPI Form No. 3 Summary ReportДокумент2 страницыHVCCI UPI Form No. 3 Summary ReportAzumi AyuzawaОценок пока нет
- Daftar Spesifikasi Teknis Pembangunan Gedung Kantor BPN BojonegoroДокумент6 страницDaftar Spesifikasi Teknis Pembangunan Gedung Kantor BPN BojonegoroIrwin DarmansyahОценок пока нет
- Essentials For Professionals: Road Surveys Using SmartphonesДокумент25 страницEssentials For Professionals: Road Surveys Using SmartphonesDoly ManurungОценок пока нет
- ADIET Digital Image Processing Question BankДокумент7 страницADIET Digital Image Processing Question BankAdarshОценок пока нет
- India - Wikipedia, The Free EncyclopediaДокумент40 страницIndia - Wikipedia, The Free EncyclopediaPrashanth KrishОценок пока нет
- LSUBL6432AДокумент4 страницыLSUBL6432ATotoxaHCОценок пока нет
- Design of Fixed Column Base JointsДокумент23 страницыDesign of Fixed Column Base JointsLanfranco CorniaОценок пока нет
- Pharmacokinetics and Drug EffectsДокумент11 страницPharmacokinetics and Drug Effectsmanilyn dacoОценок пока нет
- 07.03.09 Chest Physiotherapy PDFДокумент9 страниц07.03.09 Chest Physiotherapy PDFRakesh KumarОценок пока нет
- Chain Surveying InstrumentsДокумент5 страницChain Surveying InstrumentsSachin RanaОценок пока нет
- Math 202: Di Fferential Equations: Course DescriptionДокумент2 страницыMath 202: Di Fferential Equations: Course DescriptionNyannue FlomoОценок пока нет
- Letter of MotivationДокумент4 страницыLetter of Motivationjawad khalidОценок пока нет
- 1"a Study On Employee Retention in Amara Raja Power Systems LTDДокумент81 страница1"a Study On Employee Retention in Amara Raja Power Systems LTDJerome Samuel100% (1)