Академический Документы
Профессиональный Документы
Культура Документы
Cardiac Cycle
Загружено:
n_nkИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cardiac Cycle
Загружено:
n_nkАвторское право:
Доступные форматы
CVS MODULE II PHASE MEDICINE 2009-2010 CARDIAC CYCLE / PHYSIOLOGY MECHANICAL EVENTS OF THE CARDIAC CYCLE Events in Late
Diastole Late in diastole, the mitral and tricuspid valves between the atria and ventricles are open and the aortic and pulmonary valves are closed. Blood flows into the heart throughout diastole, filling the atria and ventricles. The rate of filling declines as the ventricles become distended, andespecially when the heart rate is lowthe cusps of the atrioventricular (AV) valves drift toward the closed position. The pressure in the ventricles remains low. Atrial Systole Contraction of the atria propels some additional blood into the ventricles, but about 70% of the ventricular filling occurs passively during diastole. Contraction of the atrial muscle that surrounds the orifices of the superior and inferior vena cava and pulmonary veins narrows their orifices, and the inertia of the blood moving toward the heart tends to keep blood in it; however, there is some regurgitation of blood into the veins during atrial systole. Ventricular Systole At the start of ventricular systole, the mitral and tricuspid (AV) valves close. Ventricular muscle initially shortens relatively little, but intraventricular pressure rises sharply as the myocardium presses on the blood in the ventricle. This period of isovolumetric
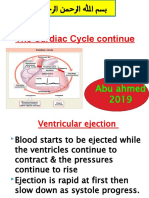
(isovolumic, isometric) ventricular contraction lasts about 0.05 s, until the pressures in the left and right ventricles exceed the pressures in the aorta (80 mm Hg; 10.6 kPa) and pulmonary artery (10 mm Hg) and the aortic and pulmonary valves open. During isovolumetric contraction, the AV valves bulge into the atria, causing a small but sharp rise in atrial pressure. When the aortic and pulmonary valves open, the phase of ventricular ejection begins. Ejection is rapid at first, slowing down as systole progresses. The intraventricular pressure rises to a maximum and then declines somewhat before ventricular systole ends. Peak left ventricular pressure is about 120 mm Hg, and peak right ventricular pressure is 25 mm Hg or less. Late in systole, the aortic pressure actually exceeds the ventricular, but for a short period momentum keeps the blood moving forward. The AV valves are pulled down by the contractions of the ventricular muscle, and atrial pressure drops. The amount of blood ejected by each ventricle per stroke at rest is 70-90 mL. The end-diastolic ventricular volume is about 130 mL. Thus, about 50 mL of blood remains in each ventricle at the end of systole (end-systolic ventricular volume), and the ejection fraction, the percent of the end-diastolic ventricular volume that is ejected with each stroke, is about 65%. The ejection fraction is a valuable index of ventricular function. Early Diastole Once the ventricular muscle is fully contracted, the already falling ventricular pressures drop more rapidly. This is the period of protodiastole. It lasts about 0.04 s. It ends when the momentum of the ejected blood is overcome and the aortic and pulmonary valves close, setting up transient vibrations in the blood and blood vessel walls. After the valves are closed, pressure continues to drop rapidly during the period of isovolumetric ventricular relaxation. Isovolumetric relaxation ends when the ventricular pressure falls below the atrial pressure and the AV valves open, permitting the ventricles to fill. Filling is rapid at first, then slows as the next
cardiac contraction approaches. Atrial pressure continues to rise after the end of ventricular systole until the AV valves open, then drops and slowly rises again until the next atrial systole.
Timing Although events on the two sides of the heart are similar, they are somewhat asynchronous. Right atrial systole precedes left atrial systole, and contraction of the right ventricle starts after that of the left. However, since pulmonary arterial pressure is lower than aortic pressure, right ventricular ejection begins before left ventricular ejection. During expiration, the pulmonary and aortic valves close at the same time; but during inspiration, the aortic valve closes slightly before the pulmonary. The slower closure of the pulmonary valve is due to lower impedance of the pulmonary vascular tree. When measured over a period of minutes, the outputs of the two ventricles are, of course, equal, but transient differences in output during the respiratory cycle occur in normal individuals. Length of Systole & Diastole Cardiac muscle has the unique property of contracting and repolarizing faster when the heart rate is high, and the duration of systole decreases from 0.27 s at a heart rate of 65 to 0.16 s at a rate of 200 beats/min. The shortening is due mainly to a decrease in the duration of systolic ejection. However, the duration of systole is much more fixed than that of diastole, and when the heart rate is increased, diastole is shortened to a much greater degree. For example, at a heart rate of 65, the duration of diastole is 0.62 s, whereas at a heart rate of 200, it is only 0.14 s. This fact has important physiologic and clinical implications. It is during diastole that the heart muscle rests, and coronary blood flow to the subendocardial portions of the left ventricle occurs only during
diastole. Furthermore, most of the ventricular filling occurs in diastole. At heart rates up to about 180, filling is adequate as long as there is ample venous return, and cardiac output per minute is increased by an increase in rate. However, at very high heart rates, filling may be compromised to such a degree that cardiac output per minute falls and symptoms of heart failure develop. Because it has a prolonged action potential, cardiac muscle is in its refractory period and will not contract in response to a second stimulus until near the end of the initial contraction. Therefore, cardiac muscle cannot be tetanized like skeletal muscle. The highest rate at which the ventricles can contract is theoretically about 400/min, but in adults the AV node will not conduct more than about 230 impulses/min because of its long refractory period. A ventricular rate of more than 230 is seen only in paroxysmal ventricular tachycardia. . Atrial Pressure Changes & the Jugular Pulse Atrial pressure rises during atrial systole and continues to rise during isovolumetric ventricular contraction when the AV valves bulge into the atria. When the AV valves are pulled down by the contracting ventricular muscle, pressure falls rapidly and then rises as blood flows into the atria until the AV valves open early in diastole. The atrial pressure changes are transmitted to the great veins, producing three characteristic waves in the record of jugular pressure. The a wave is due to atrial systole. As noted above, some blood regurgitates into the great veins when the atria contract, even though the orifices of the great veins are constricted. In addition, venous inflow stops, and the resultant rise in venous pressure contributes to the a wave. The c wave is the transmitted manifestation of the rise in atrial pressure produced by the bulging of the tricuspid valve into the atria during isovolumetric ventricular contraction. The v wave mirrors the rise in atrial pressure before the tricuspid valve opens during diastole.
Вам также может понравиться
- The Cardiac CycleДокумент19 страницThe Cardiac CycleRebi NesroОценок пока нет
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisОт EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisРейтинг: 5 из 5 звезд5/5 (1)
- Cardiovascular Physiology 3Документ69 страницCardiovascular Physiology 3maxmus4Оценок пока нет
- High Blood Pressure: Natural Self-help for Hypertension, including 60 recipesОт EverandHigh Blood Pressure: Natural Self-help for Hypertension, including 60 recipesОценок пока нет
- The Cardiac CycleДокумент9 страницThe Cardiac CycleKaylababy Hamilton BlackОценок пока нет
- CARDIAC CYCLE-laДокумент12 страницCARDIAC CYCLE-latehillahkabwe100Оценок пока нет
- Cardiac CycleДокумент18 страницCardiac CycleKundan GuptaОценок пока нет
- Cardiovascular Physiology: October 25, 2010Документ51 страницаCardiovascular Physiology: October 25, 2010VinuPrakashJ.Оценок пока нет
- Cardiac CycleДокумент30 страницCardiac CycleCarrine Liew100% (2)
- 04-The Cardiac Cycle - Wigger's Diagram (J Swanevelder)Документ6 страниц04-The Cardiac Cycle - Wigger's Diagram (J Swanevelder)Patrick WilliamsОценок пока нет
- The Cardiac Cycle: Describing The Sequence of Events in One Heart BeatДокумент14 страницThe Cardiac Cycle: Describing The Sequence of Events in One Heart BeatAswathy KrishnaОценок пока нет
- Cardiac CycleДокумент6 страницCardiac Cyclearavind kishanОценок пока нет
- The Cardiac Cycle: Describing The Sequence of Events in One Heart BeatДокумент14 страницThe Cardiac Cycle: Describing The Sequence of Events in One Heart BeatLaiba AsimОценок пока нет
- Oral PathologyДокумент23 страницыOral PathologyRuba AbbassОценок пока нет
- The Cardiac Cycle: Describing The Sequence of Events in One Heart BeatДокумент14 страницThe Cardiac Cycle: Describing The Sequence of Events in One Heart BeatMadds06Оценок пока нет
- Lecture-5 Cardiac CycleДокумент28 страницLecture-5 Cardiac Cyclettalhalatif99Оценок пока нет
- Cardiac Cycle - Atrial Contraction (Phase 1)Документ10 страницCardiac Cycle - Atrial Contraction (Phase 1)Fatima KhanОценок пока нет
- CV Physio-IntroductionДокумент33 страницыCV Physio-IntroductionHanaОценок пока нет
- The Cardiac CycleДокумент14 страницThe Cardiac CycleShreeraj ShahОценок пока нет
- Cardiac Cycle: Right Atrial SystoleДокумент6 страницCardiac Cycle: Right Atrial SystoleBeatriz De Vicente MartinezОценок пока нет
- Electrical Conduction in The HeartДокумент35 страницElectrical Conduction in The HeartNormasnizam Mohd NoorОценок пока нет
- Cardiac Cycle - Atrial Contraction (Phase 1) : A-V Valves Open Semilunar Valves ClosedДокумент10 страницCardiac Cycle - Atrial Contraction (Phase 1) : A-V Valves Open Semilunar Valves ClosedFatima KhanОценок пока нет
- Cardiac CycleДокумент30 страницCardiac CycleAdel100% (1)
- Cardiac Cycle by Bala GoyalДокумент14 страницCardiac Cycle by Bala Goyaltee su lingОценок пока нет
- Cardiac Cycle: DR Rida Ajmal KhanДокумент29 страницCardiac Cycle: DR Rida Ajmal KhanMooma fatimaОценок пока нет
- Cvs PPT 2) BpehssДокумент35 страницCvs PPT 2) BpehssAmbreen GhafoorОценок пока нет
- Cardiac CycleДокумент4 страницыCardiac CycleDivya RanasariaОценок пока нет
- Cardiac CycleДокумент2 страницыCardiac CyclevamshidhОценок пока нет
- The Cardiac Cycle 2Документ7 страницThe Cardiac Cycle 2Abigail ChristisnОценок пока нет
- CVS - IiДокумент12 страницCVS - IiBinta Elsa JohnОценок пока нет
- Heart As A Pump: Departemen Fisiologi Fakultas Kedokteran Universitas Sumatera UtaraДокумент33 страницыHeart As A Pump: Departemen Fisiologi Fakultas Kedokteran Universitas Sumatera UtaraXeniel AlastairОценок пока нет
- Cardiac Physiology PDFДокумент17 страницCardiac Physiology PDFAli Aborges Jr.Оценок пока нет
- Cardiac CycleДокумент12 страницCardiac Cycleanupam manu100% (1)
- Cardiovascular Physiology: Lawrence A. Olatunji ReaderДокумент46 страницCardiovascular Physiology: Lawrence A. Olatunji ReaderMaryam Ogunade0% (1)
- Body Fluids and Circulation Mea 8 JulyДокумент22 страницыBody Fluids and Circulation Mea 8 JulyAstrick StoosОценок пока нет
- The Circulatory System in MammalsДокумент29 страницThe Circulatory System in MammalsKeanna RaphaelОценок пока нет
- TtttttygbhbДокумент4 страницыTtttttygbhbNeeraj JainОценок пока нет
- Cardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)Документ21 страницаCardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)minesh prajapatiОценок пока нет
- The Cardiac CycleДокумент4 страницыThe Cardiac CycleAlvinОценок пока нет
- DR Rahimah Zakaria Dept of PhysiologyДокумент31 страницаDR Rahimah Zakaria Dept of PhysiologyChokJunHoongОценок пока нет
- The Cardiac Cycle Continue: Abu Ahmed 2019Документ19 страницThe Cardiac Cycle Continue: Abu Ahmed 2019Khalid AbdullahОценок пока нет
- The Cardiac Cycle Continue: Abu Ahmed 2019Документ19 страницThe Cardiac Cycle Continue: Abu Ahmed 2019Khalid AbdullahОценок пока нет
- KP 1.3.2.1 Aktivitas Mekanik Jantung (2 Jam)Документ68 страницKP 1.3.2.1 Aktivitas Mekanik Jantung (2 Jam)Try MutiaraОценок пока нет
- Transport in Animals: The Cardiac CycleДокумент2 страницыTransport in Animals: The Cardiac CyclejennieОценок пока нет
- Physiology of The Cardiac SystemДокумент41 страницаPhysiology of The Cardiac SystemRoh JitenОценок пока нет
- K3 - CardiacCycle and Heart Sound Physiology-Cv13Документ40 страницK3 - CardiacCycle and Heart Sound Physiology-Cv13Raka Notgoing Anywherebut AlwayseverywhereОценок пока нет
- Amboss - Cradiac CycleДокумент18 страницAmboss - Cradiac CycleAllysahОценок пока нет
- Heart Sounds PDFДокумент38 страницHeart Sounds PDFZennon Blaze ArceusОценок пока нет
- Cardiac CycleДокумент31 страницаCardiac CycleAdwaitha KrОценок пока нет
- Cardiac CycleДокумент7 страницCardiac Cycletewogbadeomobuwajo005Оценок пока нет
- Study FastДокумент49 страницStudy FastmbbsporalekhaОценок пока нет
- The Sequence of Events That Occur in The Heart During Cardiac CycleДокумент13 страницThe Sequence of Events That Occur in The Heart During Cardiac CycleADITYAROOP PATHAKОценок пока нет
- Assign MNTДокумент13 страницAssign MNTADITYAROOP PATHAKОценок пока нет
- Comparative Rates of Conduction System FiringДокумент3 страницыComparative Rates of Conduction System FiringSulochana ChanОценок пока нет
- Physiology Cardiology RCR1Документ17 страницPhysiology Cardiology RCR1eamcrawleyОценок пока нет
- Heart Sounds and Arteriovenous Pulses: DR Chandana HewageДокумент48 страницHeart Sounds and Arteriovenous Pulses: DR Chandana HewagePrasad HewawasamОценок пока нет
- Cardiac Cycle ExplainedДокумент5 страницCardiac Cycle ExplainedCai Peng FeiОценок пока нет
- The Cardiac Cycle NotesДокумент5 страницThe Cardiac Cycle NotesAsad Khan Khalil100% (1)
- Cardiovascular PhysiologyДокумент88 страницCardiovascular Physiologykhorrami4Оценок пока нет
- Coc Exam ModelДокумент44 страницыCoc Exam ModelYeshi AbebeОценок пока нет
- Common Diseases of NewbornДокумент162 страницыCommon Diseases of NewbornMichelle ThereseОценок пока нет
- April PhysiologyДокумент2 страницыApril Physiologyapi-284800663Оценок пока нет
- Chemistry of Blood Colours 2015Документ1 страницаChemistry of Blood Colours 2015o3uz3s333tОценок пока нет
- B.SC Botany Sem 1 To 6 2017Документ72 страницыB.SC Botany Sem 1 To 6 2017Jay ShethОценок пока нет
- Digestion Rate On FishДокумент8 страницDigestion Rate On FishMellya RizkiОценок пока нет
- BISC403 Sample Exam 4 W - Answers 20SpДокумент5 страницBISC403 Sample Exam 4 W - Answers 20SpGrace MillsОценок пока нет
- Perfusionist Job DescriptionДокумент3 страницыPerfusionist Job DescriptionNouman IshaqОценок пока нет
- PenisilinДокумент11 страницPenisilinHaruka KanataОценок пока нет
- Coronary Artery Disease and HypertensionДокумент8 страницCoronary Artery Disease and HypertensionsnehaОценок пока нет
- Patel 2014Документ7 страницPatel 2014Javiera Munizaga MuñozОценок пока нет
- Overactivebladder 160426102342Документ53 страницыOveractivebladder 160426102342Tô Hoàng DũngОценок пока нет
- Organic AcidsДокумент25 страницOrganic Acidssatti_indianОценок пока нет
- Specialization of Cerebral Hemispheres in Humans: December 2013Документ9 страницSpecialization of Cerebral Hemispheres in Humans: December 2013Huy NgoОценок пока нет
- Wim Hof HandoutДокумент2 страницыWim Hof HandoutAryan AhlawatОценок пока нет
- Nursing Review BulletsДокумент125 страницNursing Review BulletsROBERT C. REÑA, BSN, RN, MAN (ue)96% (46)
- Gbio 2122 Week 1 10 by Kuya CharlesДокумент18 страницGbio 2122 Week 1 10 by Kuya CharlesChoe Yoek Soek100% (2)
- Pupillary Light ReflexДокумент2 страницыPupillary Light ReflexJohn OsborneОценок пока нет
- %pecta (: P'erfectedДокумент5 страниц%pecta (: P'erfectedjuan perez arrikitaunОценок пока нет
- ABG ElectrolytesДокумент48 страницABG ElectrolytesDRwaqas Gulzar100% (1)
- Anti-Depressant Drugs: Presented by L.Nithish Shankar Ii Year Mbbs KGMCДокумент17 страницAnti-Depressant Drugs: Presented by L.Nithish Shankar Ii Year Mbbs KGMCÑiťhišh Śhankąŕ LóganáthánОценок пока нет
- Mitosis Meiosis ComparedДокумент1 страницаMitosis Meiosis ComparedDURU ALTINKAYA100% (1)
- 0046 8177 (93) 90013 7Документ12 страниц0046 8177 (93) 90013 7Carmen Gomez MuñozОценок пока нет
- Anatomy and Physiology of Respiratory System Tutorial2Документ1 страницаAnatomy and Physiology of Respiratory System Tutorial2Jhullian Frederick Val VergaraОценок пока нет
- Jaw RelationДокумент48 страницJaw RelationBharanija100% (1)
- Basic of Cardiovascular and Respiratory SystemДокумент59 страницBasic of Cardiovascular and Respiratory SystemMonika ChaikumarnОценок пока нет
- Soothing The Traumatized Brain: WorksheetsДокумент5 страницSoothing The Traumatized Brain: WorksheetsAlguémОценок пока нет
- Cardiotonic Drugs Revised DheryanДокумент16 страницCardiotonic Drugs Revised Dheryanlinnet17Оценок пока нет
- Cell and Its Structure and Functions: Q1. Write Down The Main Differences Between The Animal Cell and The Plant CellДокумент5 страницCell and Its Structure and Functions: Q1. Write Down The Main Differences Between The Animal Cell and The Plant CellMuhhammed AliОценок пока нет
- Botany Report - Chap 7Документ35 страницBotany Report - Chap 7Seannel CruzОценок пока нет
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)От EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Рейтинг: 3 из 5 звезд3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 4.5 из 5 звезд4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryОт EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryРейтинг: 4 из 5 звезд4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaОт EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsОт EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsРейтинг: 4 из 5 звезд4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossОт EverandThe Obesity Code: Unlocking the Secrets of Weight LossРейтинг: 4 из 5 звезд4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesОт EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesРейтинг: 4.5 из 5 звезд4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsОт EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsРейтинг: 5 из 5 звезд5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.От EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Рейтинг: 4.5 из 5 звезд4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsОт EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsРейтинг: 4.5 из 5 звезд4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisОт EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisРейтинг: 5 из 5 звезд5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessОт EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessРейтинг: 4.5 из 5 звезд4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassОт EverandTroubled: A Memoir of Foster Care, Family, and Social ClassРейтинг: 4.5 из 5 звезд4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingОт EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingРейтинг: 4 из 5 звезд4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeОт EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeРейтинг: 4.5 из 5 звезд4.5/5 (254)